Epidurals and Cesareans Link Remains Unclear
Diunggah oleh
oanamemoJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Epidurals and Cesareans Link Remains Unclear
Diunggah oleh
oanamemoHak Cipta:
Format Tersedia
CONTINUING EDUCATION MODULE
Epidurals: Do They or Dont They
Increase Cesareans?
Henci Goer
ABSTRACT
The controversy over whether epidurals increase the risk of cesarean has raged since the 1970s. This article
provides a history of of the early observational research designed to answer this question and an in-depth
analysis of the most recent randomized control trials. Based on the research, the author concludes that we
cannot assure women that epidurals do not increase the risk of cesarean.
The Journal of Perinatal Education, 24(4), 209212, http://dx.doi.org/10.1891/1058-1243.24.4.209
Keywords: cesarean birth, clinical outcomes, evidence-based practice, interventions, complications, labor
and birth
Lets start with a bit of background for those of you
who didnt personally live through the early controversy over whether epidurals increased the cesarean
rate. As epidurals began to achieve popularity in the
late 1970s and 1980s, one researcher sounded the
alarm when he and his group published a study of
714 first-time mothers showing that even after excluding women with big babies and women whose
labor pattern was abnormal prior to having an epidural, epidurals remained a potent factor in cesarean
rates for delayed progress (Thorp, Parisi, Boylan, &
Johnston, 1989). Everyone pooh-poohed his finding on grounds that observational studies cant truly
determine whether epidurals lead to more cesareans
or women experiencing more prolonged, painful labors, and therefore at higher risk for cesarean, were
more likely to want epidurals. The chicken versus
egg question, they argued, couldnt be resolved
without a randomized controlled trial (RCT), and it
wasnt likely that women would agree to be assigned
by chance to have an epidural or not. In point of fact,
that same year saw publication of a small Danish
RCT (107 women, 104 of them first-time mothers;
Philipsen & Jensen, 1989). It reported that having
an epidural nearly tripled the cesarean rate (16% vs.
6%) for cephalopelvic disproportion despite no
clinical evidence of CPD being a requirement for
inclusion. The investigators ignored this, however,
concluding only that instrumental vaginal delivery
rates were similar, and epidurals provided better
pain relief. In any case, the anesthetic dose was much
higher than was already becoming the norm, so it
could be reasonably argued that the trials findings
wouldnt apply to modern-day practice.
Thorp, meanwhile, took up the RCT challenge.
He and his colleagues carried out an epidural versus
no epidural trial in 93 first-time mothers and found
that epidurals did, in fact, lead to cesareans (25% vs.
2%), not vice versa (Thorp et al., 1993). That bit of
unwelcome news precipitated a stampede to perform
w
An earlier version of this
column was published on
Science & Sensibility
(January 27, 2015).
Accessed at http://www
.scienceandsensibility.org/
epidurals-do-they-or-dontthey-increase-cesareans/
Epidurals: Do They or Dont They Increase Cesareans? | Goer 209
JPE24-4_Final_A3_209-212.indd 209
9/27/15 9:48 AM
The finding that epidurals dont increase cesareans is puzzling
because they increase likelihood of factors associated with them
more RCTs, and when enough of those had accumulated, to a series of systematic reviews pooling their
data (meta-analysis), of which the Cochrane review,
Anim-Somuah, Smyth, and Jones (2011), is the latest. These reached the more comfortable conclusion
that epidurals didnt increase likelihood of cesarean,
and pro-epiduralists breathed a collective sigh of
relief and went back, if they had ever stopped, to
unreservedly recommending epidurals. (This rather
sweeps under the rug the other problems epidurals
can cause, but thats a topic for another day.)
WEAKNESSES OF THE EPIDURAL VERSUS
NO EPIDURAL TRIALS
The finding that epidurals dont increase cesareans
is puzzling because they increase likelihood of factors associated with them (Anim-Somuah et al.,
2011). For one thing, they increase use of oxytocin
to augment labor, which implies they slow labor. For
another, more women run fevers, and it stands to
reason that a woman progressing slowly who starts
running a fever is a likely candidate for cesarean. For
a third, the difference in fetal malposition (occiput
posterior) rates at delivery comes close to achieving
statistical significance, meaning the difference is unlikely to be due to chance. Persistent OP is strongly
associated with cesarean delivery (Cheng, Shaffer,
Caughey, 2006; Fitzpatrick, McQuillan, & OHerlihy,
2001; Phipps et al., 2014; Ponkey, Cohen, Heffner,
Lieberman, 2003; Sencal, Xiong, & Fraser, 2005;
Sizer & Nirmal, 2000). Epidurals even increase cesareans for fetal distress by 40%, although the absolute
difference didnt amount to much (1 more per 100
women). Could a difference exist and meta-analysis
of RCTs fail to detect it?
A string of well-conducted observational studies
over the years have suggested that they could
(Eriksen, Nohr, & Kjaergaard, 2011; Kjaergaard,
Olsen, Ottesen, Nyberg, & Dykes, 2008; Lieberman
First-time mothers are much more susceptible to factors that
impede progress, so including women with prior vaginal births can
make it appear that epidurals are less problematic for first-time
mothers than they really are.
210
JPE24-4_Final_A3_209-212.indd 210
et al., 1996; Nguyen et al., 2010), the most recent of
which is a very large, very convincing study published in fall of 2014 (Bannister-Tyrrell, Ford, Morris, & Roberts, 2014). Its authors point out, as have
others before them, the weaknesses of the RCTs,
weaknesses serious enough to nullify their results or
make them inapplicable to typical community practice (external validity).
To begin with, in most trials, substantial percentages of women allocated to the non-epidural group
ended up having epidurals, and some women allocated to the epidural group ended up not having
one. Since RCTs analyze results according to group
assignment (to do otherwise would negate the point
of random assignment, which is to avoid bias), not
what actually happened, this diminishes differences
between groups. In addition, trials were mostly
confined to women with no medical or obstetric
complications who were treated according to strict
protocols for labor management and indications for
cesarean surgery. Neither is the case in most hospitals. To these I would add that many trials lumped
together first-time mothers and women with prior
births when reporting outcomes. First-time mothers
are much more susceptible to factors that impede
progress, so including women with prior vaginal
births can make it appear that epidurals are less problematic for first-time mothers than they really are.
In addition, three of the trials were carried out in a
hospital where participants were mostly attended by
midwives, and cesarean rates were much lower than
is common for women attended by obstetricians.
All of this means that any null results in metaanalyses of the trials can be taken with a grain of salt,
any findings of significant differences probably represent a minimal value, and first-time moms may be
harder hit than appears. To cite one example, AnimSomuah et al. (2011) reported that 5 more women
per 100 having epidurals had a malpositioned baby
at delivery (18% vs. 13%) in the 4 trials reporting
this outcome, a difference, as I said, that just missed
achieving statistical significance. But when I confined results to the two trials in first-time mothers
alone in which 10% or fewer of the women in the
no-epidural group had an epidural, the gap widened to 9 more per 100 (11% vs. 2%).
SUMMARY OF THE BANNISTER-TYRRELL
ET AL. (2014) ANALYSIS
Bannister-Tyrrell and colleagues (2014) drew their
population from a database of 210,700 Australian
women with no prior cesareans who were laboring at
The Journal of Perinatal Education | Fall 2015, Volume 24, Number 4
9/27/15 9:48 AM
term with a singleton, head-down baby. A strength of
the database was that, unlike most, it distinguished
epidurals for labor from epidurals for delivery. Using
a long list of factors, investigators constructed a propensity score for how likely a woman was to have an
epidural, matched women according to their score,
and compared results according to whether women
with the same score had or didnt have an epidural.
Matched controls were found for 52,600 women
who had an epidural and were found across the full
range of propensity scores. Women having epidurals were 2.5 times more likely to have a cesarean
(20% vs. 8%), or put another way, 12 more women
per 100 having epidurals had a cesarean (absolute
excess), which amounts to 1 additional cesarean for
every 8.5 women having an epidural (number needed
to harm). Among first-time mothers, women having
epidurals were 2.4 times more likely to have a cesarean. Study authors didnt provide cesarean rates
for this subgroup, but the raw cesarean rates overall
were 18% in first-time mothers versus 2% in women
with prior births, so the effect on this more vulnerable population could be dire.
But theres still more. Investigators further adjusted for confounding factors not captured in their
database. These included differences in health-care
settings (same state but not same city), care provider (women without epidurals are more likely to
be attended by midwives), and for confounding interventions more likely with epidurals (continuous
fetal monitoring). Relative risk of cesarean with an
epidural remained at 2.5. Investigators then adjusted
for the association between occiput posterior baby
and cesarean by setting estimates of the risk ratio
to exceed the strongest associations reported in the
literature, and they assumed that the prevalence of
severe labor pain was 3 to 4 times higher in women
having epidurals. Factoring these into their statistical analysis reduced the risk ratio, but women having
epidurals still were 50% more likely to have a cesarean. This means that with a baseline cesarean rate of
8% in women without an epidural, 12% of women
with an epidural will have one or 4 more women per
100 or 1 more cesarean for every 25 women.
THE TAKE-HOME
At the very least we cannot assure women with confidence that epidurals dont increase the likelihood
of cesarean. For this reason and because of their
numerous other drawbacks and considering that
comfort measures and other strategies have been
shown to be both effective for most women and free
At the very least we cannot assure women with confidence that
epidurals dont increase the likelihood of cesarean.
of adverse effects (Declercq, Sakala, Corry, & Applebaum, 2006; Jones et al., 2012), women may want
to make epidurals Plan B rather than Plan A. That
being said, whatever their choice, women can minimize their chance of cesareanwith or without an
epiduralby choosing a midwife or doctor whose
policies and practices promote spontaneous vaginal
birth http://www.lamaze.org/HealthyBirthPractices.
REFERENCES
Anim-Somuah, M., Smyth, R. M., & Jones, L. (2011). Epidural versus non-epidural or no analgesia in labour. Cochrane Database of Systematic Reviews, (12), CD000331.
http://dx.doi.org/10.1002/14651858.CD000331.pub3
Bannister-Tyrrell, M., Ford, J. B., Morris, J. M., & Roberts,
C. L. (2014). Epidural analgesia in labour and risk of
caesarean delivery. Paediatric and Perinatal Epidemiology, 28(5), 400411. Retrieved from http://www.ncbi
.nlm.nih.gov/pubmed/25040829
Cheng, Y. W., Shaffer, B. L., & Caughey, A. B. (2006). Associated factors and outcomes of persistent occiput
posterior position: A retrospective cohort study from
1976 to 2001. Journal of Maternal-Fetal & Neonatal
Medicine, 19(9), 563568. Retrieved from http://www
.ncbi.nlm.nih.gov/pubmed/16966125?dopt=Citation
Declercq, E., Sakala, C., Corry, M. P., & Applebaum, S.
(2006). Listening to Mothers II: Report of the Second National U.S. Survey of Womens Childbearing Experiences.
New York, NY: Childbirth Connection. Retrieved from
http://childbirthconnection.org/pdfs/LTMII_report.pdf
Eriksen, L. M., Nohr, E. A., & Kjaergaard, H. (2011). Mode
of delivery after epidural analgesia in a cohort of lowrisk nulliparas. Birth, 38(4), 317326. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/22112332
Fitzpatrick, M., McQuillan, K., & OHerlihy, C. (2001).
Influence of persistent occiput posterior position on
delivery outcome. Obstetrics and Gynecology, 98(6),
10271031. Retrieved from http://www.ncbi.nlm.nih
.gov/pubmed/11755548?dopt=Citation
Jones, L., Othman, M., Dowswell, T., Alfirevic, Z., Gates,
S., Newburn, M., . . . Neilson, J. P. (2012). Pain management for women in labour: An overview of systematic
reviews. Cochrane Database of Systematic Reviews, (3),
CD009234. Retrieved from http://www.ncbi.nlm.nih
.gov/pubmed/22419342
Kjaergaard, H., Olsen, J., Ottesen, B., Nyberg, P., &
Dykes, A. K. (2008). Obstetric risk indicators for
labour dystocia in nulliparous women: A multicentre cohort study. BMC Pregnancy Childbirth, 8,
45. Retrieved from http://www.ncbi.nlm.nih.gov/
pubmed/18837972?dopt=Citation
Lieberman, E., Lang, J. M., Cohen, A., DAgostino, R.,
Jr., Datta, S., & Frigoletto, F. D., Jr. (1996). Association of epidural analgesia with cesarean delivery in
Epidurals: Do They or Dont They Increase Cesareans? | Goer 211
JPE24-4_Final_A3_209-212.indd 211
9/27/15 9:48 AM
nulliparas. Obstetrics and Gynecology, 88(6), 993
1000. Retrieved from http://www.ncbi.nlm.nih.gov/
pubmed/8942841
Nguyen, U. S., Rothman, K. J., Demissie, S., Jackson,
D. J., Lang, J. M., & Ecker, J. L. (2010). Epidural analgesia and risks of cesarean and operative vaginal
deliveries in nulliparous and multiparous women.
Maternal Child Health Journal, 14(5), 705712. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/
19760498?dopt=Citation
Philipsen, T., & Jensen, N. H. (1989). Epidural block or parenteral pethidine as analgesic in labour: A randomized
study concerning progress in labour and instrumental
deliveries. European Journal of Obstetrics, Gynecology,
and Reproductive Biology, 30(1), 2733. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/2924990
Phipps, H., Hyett, J. A., Graham, K., Carseldine, W. J.,
Tooher, J., & de Vries, B. (2014). Is there an association between sonographically determined occipitotransverse position in the second stage of labor and
operative delivery? Acta Obstetricia et Gynecologica
Scandinavica, 93(10), 10181024. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/25060716
Ponkey, S. E., Cohen, A. P., Heffner, L. J., & Lieberman, E.
(2003). Persistent fetal occiput posterior position: Obstetric outcomes. Obstetrics and Gynecology, 101(5, Pt. 1),
915920. Retrieved from http://www.ncbi.nlm.nih.gov/
pubmed/12738150?dopt=Citation
Sencal, J., Xiong, X., & Fraser, W. D. (2005). Effect of fetal
position on second-stage duration and labor outcome.
Obstetrics and Gynecology, 105(4), 763772. Retrieved
from http://www.ncbi.nlm.nih.gov/pubmed/15802403
Sizer, A. R., & Nirmal, D. M. (2000). Occipitoposterior
position: Associated factors and obstetric outcome
in nulliparas. Obstetrics and Gynecology, 96(5, Pt. 1),
212
JPE24-4_Final_A3_209-212.indd 212
749752. Retrieved from http://www.ncbi.nlm.nih
.gov/pubmed/11042312?dopt=Citation
Thorp, J. A., Hu, D. H., Albin, R. M., McNitt, J., Meyer,
B. A., Cohen, G. R., & Yeast, J. D. (1993). The effect of
intrapartum epidural analgesia on nulliparous labor:
A randomized, controlled, prospective trial. American Journal of Obstetrics and Gynecology, 169(4), 851
858. Retrieved from http://www.ncbi.nlm.nih.gov/
pubmed/8238138?dopt=Citation
Thorp, J. A., Parisi, V. M., Boylan, P. C., & Johnston, D.
A. (1989). The effect of continuous epidural analgesia
on cesarean section for dystocia in nulliparous women.
American Journal of Obstetrics and Gynecology, 161(3),
670675. Retrieved from http://www.ncbi.nlm.nih
.gov/pubmed/2782350
HENCI GOER, award-winning medical writer and internationally known speaker, is an acknowledged expert on
evidence-based maternity care. Her first book, Obstetric
Myths Versus Research Realities, was given Lamaze International Presidents Award in recognition of its value as a
resource for childbirth educators. Its successor, Optimal Care
in Childbirth: The Case for a Physiologic Approach, won
the American College of Nurse-Midwives Best Book of the
Year award. Goer has also written The Thinking Womans
Guide to a Better Birth, unique in that it gives pregnant
women access to the research evidence. Goer has written
consumer education pamphlets and numerous articles for
trade, consumer, and academic periodicals as well. Nearing
completion, Goers latest project is Childbirth U, a website
that will sell narrated slide presentations at modest cost to
help pregnant women make informed decisions about care.
The Journal of Perinatal Education | Fall 2015, Volume 24, Number 4
9/27/15 9:48 AM
Anda mungkin juga menyukai
- Spin Doctoring The ResearchDokumen6 halamanSpin Doctoring The ResearchszopfaszBelum ada peringkat
- Lit Review NealeDokumen9 halamanLit Review Nealeapi-726948535Belum ada peringkat
- 1 s2.0 S0266613816000401 MainDokumen8 halaman1 s2.0 S0266613816000401 MainBeth TorresBelum ada peringkat
- Endometriosis-Associated Infertility: Surgery and IVF, A Comprehensive Therapeutic ApproachDokumen8 halamanEndometriosis-Associated Infertility: Surgery and IVF, A Comprehensive Therapeutic ApproachRangga AdityaBelum ada peringkat
- Pregnancy After Caesarean Section: Fewer or Later?: J.J.H. Eijsink, L. Van Der Leeuw-Harmsen and P.J.Q. Van Der LindenDokumen5 halamanPregnancy After Caesarean Section: Fewer or Later?: J.J.H. Eijsink, L. Van Der Leeuw-Harmsen and P.J.Q. Van Der LindenSamuel Albert Andrian SiagianBelum ada peringkat
- Running Head: HEALTH POLICY PAPER 1Dokumen10 halamanRunning Head: HEALTH POLICY PAPER 1api-283540594Belum ada peringkat
- Pone 0054858 PDFDokumen7 halamanPone 0054858 PDFfiameliaaBelum ada peringkat
- Womens Experiences of Childbirth and PosDokumen7 halamanWomens Experiences of Childbirth and PosMirjana14Belum ada peringkat
- The External Version in Modern Obstetrics: An Alternative to Cesarean DeliveryDokumen21 halamanThe External Version in Modern Obstetrics: An Alternative to Cesarean DeliveryCitrast NursyahidahBelum ada peringkat
- Debate GUIDE PDFDokumen8 halamanDebate GUIDE PDFBlesse PateñoBelum ada peringkat
- Friedman EA (2000) : Labor: Clinical Evaluation and Management, P 23, 2nd Ed. New York, Appleton-Century-CroftsDokumen5 halamanFriedman EA (2000) : Labor: Clinical Evaluation and Management, P 23, 2nd Ed. New York, Appleton-Century-CroftsJuliane ItliongBelum ada peringkat
- StratOG Vaginal BreechDokumen17 halamanStratOG Vaginal BreechNalin AbeysingheBelum ada peringkat
- Fertil Ster IlDokumen6 halamanFertil Ster IlAstrina SupandyBelum ada peringkat
- Ijwh 5 811Dokumen8 halamanIjwh 5 811Anonymous ORleRrBelum ada peringkat
- Ultrasound in Prenatal DiagnosisDokumen11 halamanUltrasound in Prenatal DiagnosisValentina Grajales RestrepoBelum ada peringkat
- Laborinduction: Areviewof Currentmethods: Mildred M. RamirezDokumen11 halamanLaborinduction: Areviewof Currentmethods: Mildred M. RamirezRolando DiazBelum ada peringkat
- Articulo EndometriosisDokumen7 halamanArticulo EndometriosisMaIt VeFloBelum ada peringkat
- Research Summar4Dokumen2 halamanResearch Summar4api-238818738Belum ada peringkat
- Anti-Choice Claims About Abortion and Breast CancerDokumen6 halamanAnti-Choice Claims About Abortion and Breast CancerProgressTXBelum ada peringkat
- DP 203Dokumen63 halamanDP 203charu parasherBelum ada peringkat
- HuffmanShwartzSwanson2015 PDFDokumen9 halamanHuffmanShwartzSwanson2015 PDFIrene De La CruzBelum ada peringkat
- Seijmonsbergenschermers 2013Dokumen9 halamanSeijmonsbergenschermers 2013Febyan AbotBelum ada peringkat
- Pi Is 0002937816462733Dokumen6 halamanPi Is 0002937816462733muhammad maadaBelum ada peringkat
- Research Article: Pregnancy Outcome of Multiparous Women Aged Over 40 YearsDokumen4 halamanResearch Article: Pregnancy Outcome of Multiparous Women Aged Over 40 YearsChristine Laurenza SBelum ada peringkat
- Cesarean Delivery After InductionDokumen5 halamanCesarean Delivery After InductionKIBIR TEMESGENBelum ada peringkat
- Vaginal Misoprostol Prior To Insertion of An Intrauterine Device: An RCTDokumen17 halamanVaginal Misoprostol Prior To Insertion of An Intrauterine Device: An RCTIndra Budi PutraBelum ada peringkat
- Jurnal IDokumen24 halamanJurnal IAgustin LindaBelum ada peringkat
- Vaginal ultrasound reduces IUD expulsion rates less than 40 charactersDokumen3 halamanVaginal ultrasound reduces IUD expulsion rates less than 40 charactersAgustin GonzalezBelum ada peringkat
- Home BirthDokumen33 halamanHome BirthMarlon Royo100% (2)
- Induction of Labor and Risk of Postpartum Hemorrhage in Low Risk ParturientsDokumen8 halamanInduction of Labor and Risk of Postpartum Hemorrhage in Low Risk ParturientsRudolf Fernando WibowoBelum ada peringkat
- Endometriosis EurDokumen5 halamanEndometriosis EurReynaldi AbdullahBelum ada peringkat
- PRINT - Decrease Unintended Pregnancy-PIIS0015028214022092Dokumen7 halamanPRINT - Decrease Unintended Pregnancy-PIIS0015028214022092nurBelum ada peringkat
- Interventions For The Prevention of Pain Associated With The Placement of Intrauterine Contraceptives: An Updated ReviewDokumen14 halamanInterventions For The Prevention of Pain Associated With The Placement of Intrauterine Contraceptives: An Updated ReviewLeonardo Daniel MendesBelum ada peringkat
- Drugs in LabourDokumen9 halamanDrugs in LabourWhira CahbaliBelum ada peringkat
- Jurnal Placenta PreviaDokumen9 halamanJurnal Placenta Previasheva25Belum ada peringkat
- PII002822438690167XDokumen11 halamanPII002822438690167XChristian VieryBelum ada peringkat
- Keberhasilan Post SCDokumen12 halamanKeberhasilan Post SCAprilliaBelum ada peringkat
- Declining FertilityDokumen17 halamanDeclining FertilityNanda PerdanaBelum ada peringkat
- Pneumonia and Pregnancy Outcomes: A Nationwide Population-Based StudyDokumen7 halamanPneumonia and Pregnancy Outcomes: A Nationwide Population-Based StudyAdrin Mahmuddin HarahapBelum ada peringkat
- Is Fetal Growth Restriction Associated With A More Severe Maternal Phenotype in The Setting of Early Onset Pre-Eclampsia? A Retrospective StudyDokumen6 halamanIs Fetal Growth Restriction Associated With A More Severe Maternal Phenotype in The Setting of Early Onset Pre-Eclampsia? A Retrospective StudyYessie ErBelum ada peringkat
- Chouinard2019 PDFDokumen8 halamanChouinard2019 PDFanggunBelum ada peringkat
- Application of Ultrasonography in Female Infertility: A Comprehensive ReviewDokumen11 halamanApplication of Ultrasonography in Female Infertility: A Comprehensive ReviewNur Fitryanti Lubis100% (1)
- Hard Arson 2008Dokumen7 halamanHard Arson 2008elda zulkarnainBelum ada peringkat
- Effects of Labor Support On Mothers, Babies, and Birth OutcomesDokumen10 halamanEffects of Labor Support On Mothers, Babies, and Birth OutcomesLuvi AprilianaBelum ada peringkat
- Hum. Reprod.-2001-Tur-2124-9Dokumen0 halamanHum. Reprod.-2001-Tur-2124-9masdipoBelum ada peringkat
- Impact of A Multiple, IVF Birth On Post-Partum Mental Health: A Composite AnalysisDokumen8 halamanImpact of A Multiple, IVF Birth On Post-Partum Mental Health: A Composite AnalysisMirjana14Belum ada peringkat
- Misoprostol Facilitates IUD Insertion in Nulliparous WomenDokumen8 halamanMisoprostol Facilitates IUD Insertion in Nulliparous WomenPutri Nilam SariBelum ada peringkat
- WatermarkDokumen6 halamanWatermarkAna AdamBelum ada peringkat
- Bangresearch 301 RevisedDokumen4 halamanBangresearch 301 Revisedapi-356371162Belum ada peringkat
- The Natural History of The Normal First Stage Of.6 PDFDokumen6 halamanThe Natural History of The Normal First Stage Of.6 PDFreioctabianoBelum ada peringkat
- Low-Risk Planned Caesarean Versus Planned Vaginal Delivery at Term: Early and Late Infantile OutcomesDokumen11 halamanLow-Risk Planned Caesarean Versus Planned Vaginal Delivery at Term: Early and Late Infantile OutcomesEduarda QuartinBelum ada peringkat
- Family History As A Risk Factor For Pelvic Organ Prolapse: Original ArticleDokumen7 halamanFamily History As A Risk Factor For Pelvic Organ Prolapse: Original ArticlepakemainmainBelum ada peringkat
- Ritgen ManueverDokumen2 halamanRitgen ManueverGustavo Gonzalez CabreraBelum ada peringkat
- ContrafactsheetDokumen3 halamanContrafactsheetCBCP for LifeBelum ada peringkat
- Forveps y VacuumDokumen6 halamanForveps y VacuumSaul Gonzalez HernandezBelum ada peringkat
- Parturition Events and Risk of Urinary Incontinence in Later LifeDokumen16 halamanParturition Events and Risk of Urinary Incontinence in Later LifeMutia LailaniBelum ada peringkat
- English Progress Program: Nama: Nurul Hidayah NIM: 21117091Dokumen12 halamanEnglish Progress Program: Nama: Nurul Hidayah NIM: 21117091nurul4hidayah-99Belum ada peringkat
- Getting Pregnant in the 1980s: New Advances in Infertility Treatment and Sex PreselectionDari EverandGetting Pregnant in the 1980s: New Advances in Infertility Treatment and Sex PreselectionBelum ada peringkat
- On Autumn's Wing, A Story of Birth Trauma, Brain Injury and Miracles.Dari EverandOn Autumn's Wing, A Story of Birth Trauma, Brain Injury and Miracles.Belum ada peringkat
- Contraception for the Medically Challenging PatientDari EverandContraception for the Medically Challenging PatientRebecca H. AllenBelum ada peringkat
- P-Stim™ Auricular Electroacupuncture Stimulation Device For Pain ReliefDokumen10 halamanP-Stim™ Auricular Electroacupuncture Stimulation Device For Pain ReliefoanamemoBelum ada peringkat
- TestDokumen1 halamanTestoanamemoBelum ada peringkat
- Journal of Perinatal EducationDokumen3 halamanJournal of Perinatal EducationoanamemoBelum ada peringkat
- Robin Predare Catre MediciDokumen1 halamanRobin Predare Catre MedicioanamemoBelum ada peringkat
- VBAC or Repeat CDokumen26 halamanVBAC or Repeat CoanamemoBelum ada peringkat
- Bagajul de SpitalDokumen1 halamanBagajul de SpitaloanamemoBelum ada peringkat
- Nursing 212 Final Exam Review - Fall 2017Dokumen12 halamanNursing 212 Final Exam Review - Fall 2017Marc LaBarbera100% (1)
- Final Output - Montuerto, Julius Nixell B.Dokumen3 halamanFinal Output - Montuerto, Julius Nixell B.Jayvee Pellazar BernatBelum ada peringkat
- Community Medicine 2022Dokumen8 halamanCommunity Medicine 2022Ashirwad DadeiaBelum ada peringkat
- Dental Auxiliary: Presented By-Sneha Patil (Final Year BDS Student)Dokumen36 halamanDental Auxiliary: Presented By-Sneha Patil (Final Year BDS Student)Mumin RashidBelum ada peringkat
- Managing Drug SupplyDokumen36 halamanManaging Drug SupplyLisna K. RezkyBelum ada peringkat
- OGDokumen385 halamanOGMin MawBelum ada peringkat
- HIV Lecture Handout 2021Dokumen10 halamanHIV Lecture Handout 2021Jimilyn GallowayBelum ada peringkat
- Nursing Informatics (Terminal Requirement 17)Dokumen1 halamanNursing Informatics (Terminal Requirement 17)Lyza MateoBelum ada peringkat
- Mental health and HIV in IndiaDokumen7 halamanMental health and HIV in IndiaAyu RajikanBelum ada peringkat
- Ethics Gtu 301 Final Exam.14.15 1Dokumen2 halamanEthics Gtu 301 Final Exam.14.15 1JebatAl-KelantaniBelum ada peringkat
- Robsons Ten Group Classification of Cesarean Section at A Tertiary Center in NepalDokumen6 halamanRobsons Ten Group Classification of Cesarean Section at A Tertiary Center in NepalgehanathBelum ada peringkat
- 5.Mr Lode Vedonk - Vietnam Oktober 2023Dokumen11 halaman5.Mr Lode Vedonk - Vietnam Oktober 2023Tran Khanh TrangBelum ada peringkat
- DR Moshiri - Class II Correction by Leveraging Molar Rotation - 2Dokumen4 halamanDR Moshiri - Class II Correction by Leveraging Molar Rotation - 2Enea NastriBelum ada peringkat
- Tieraona Low Dog, MD, With and Marc S. Micozzi, MD, PHD (Auth.) - Women's Health in Complementary and Integrative Medicine. A Clinical Guide (2005)Dokumen353 halamanTieraona Low Dog, MD, With and Marc S. Micozzi, MD, PHD (Auth.) - Women's Health in Complementary and Integrative Medicine. A Clinical Guide (2005)Marfu'ah Mar'ahBelum ada peringkat
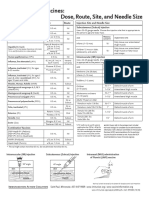
- Injection Site and Needle Size Vaccine Dose RouteDokumen1 halamanInjection Site and Needle Size Vaccine Dose RouteDr Ambana GowdaBelum ada peringkat
- Extension Toxicology Network ExplainedDokumen6 halamanExtension Toxicology Network Explainedjohnrey_lidresBelum ada peringkat
- Overweight 2Dokumen1 halamanOverweight 2Trần NhânBelum ada peringkat
- SLE-CME SlidesDokumen70 halamanSLE-CME Slidesrossi434614Belum ada peringkat
- BJOG - 2023 - Lee - Tranexamic Acid As An Adjunct To Oxytocin Prophylaxis in The Prevention of Postpartum Haemorrhage inDokumen9 halamanBJOG - 2023 - Lee - Tranexamic Acid As An Adjunct To Oxytocin Prophylaxis in The Prevention of Postpartum Haemorrhage inHayfa LayebBelum ada peringkat
- Periodic Health ExamDokumen23 halamanPeriodic Health ExamPernel Jose Alam MicuboBelum ada peringkat
- School Contingency Plan For COVID-19 Pandemic: Department of EducationDokumen14 halamanSchool Contingency Plan For COVID-19 Pandemic: Department of EducationMaria Rose Tariga AquinoBelum ada peringkat
- CV Maggies - HungDokumen4 halamanCV Maggies - HungDoni HardiansyahBelum ada peringkat
- HW 2Dokumen16 halamanHW 2api-371944008Belum ada peringkat
- Torch InfectionsDokumen13 halamanTorch InfectionsOmeBelum ada peringkat
- Ozone Therapy Conference at Bombay Hospital Focuses On Shared ExperiencesDokumen4 halamanOzone Therapy Conference at Bombay Hospital Focuses On Shared ExperiencesDr Saxena Centre for Progressive MedicineBelum ada peringkat
- Medication ReconciliationDokumen9 halamanMedication ReconciliationHoly DishBelum ada peringkat
- CertificateDokumen1 halamanCertificateDrazarBelum ada peringkat
- Clubfoot Deformities ExplainedDokumen3 halamanClubfoot Deformities ExplainedKim GalamgamBelum ada peringkat
- Bayi Baru LahirDokumen43 halamanBayi Baru LahirBRI KUBelum ada peringkat
- NCM 119 Safety Case Study Extended StayDokumen4 halamanNCM 119 Safety Case Study Extended StayMaria Victoria A. PraxidesBelum ada peringkat