R Idelalisib V1 11.14
Diunggah oleh
GabrielJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
R Idelalisib V1 11.14
Diunggah oleh
GabrielHak Cipta:
Format Tersedia
R-IDELALISIB FOR CLL
For relapsed CLL in patients who are not suitable for cytotoxic chemotherapy and who meet the CDF criteria
Individual funding for idelalisib must be agreed before treatment may start
All patients should be screened for hepatitis B virus before starting treatment
Drugs/Dosage:
Other Drugs:
Rituximab
375mg/m2
IV
fractionated over Day 1 and Day 2 of the course
(see Administration section)
2
then, starting 2 weeks after the 375mg/m dose;
Rituximab
500mg/m2
IV
every 2 weeks for 4 doses (on week 2, week 4,
(dose banded
week 6 & week 8), then every 4 weeks for
as table below)
3 doses (on week 12, week 16 & week 20)
Idelalisib
150mg
PO
twice daily, continuous until disease progression or
unacceptable toxicity
Rituximab Premedication (to be administered before all infusions):
Paracetamol 1000mg po
60 minutes before rituximab
Chlorphenamine 10mg IV
15 minutes before rituximab
Dexamethasone 8mg IV
15 minutes before rituximab
Allopurinol 300mg po daily, ideally starting 24 hours before treatment - review after 4 weeks.
For patients with high initial counts (WBC > 100) or bulky disease, it is suggested that at least
1 litre of IV N/saline is administered before starting treatment.
Loperamide as required for management of idelalisib-associated diarrhoea (note that the
onset of diarrhoea may not be immediate but may first occur months after starting treatment)
Frequency:
Rituximab 2 weekly for 5 doses, then 4 weekly for 3 doses (total 8 doses)
i.e. Rituximab on week 0, week 2, week 4, week 6, week 8, week 12, week 16 & week 20
Idelalisib twice daily dosing continuously, until disease progression or unacceptable toxicity
Administration:
Idelalisib available as 100mg and 150mg tablets.
The tablets should be swallowed whole, either with or without food.
It is assumed that the majority of patients will present with WBC > 25 x 109/L, which requires
rituximab to be administered with caution at a reduced rate, and with careful monitoring, as
there is an increased risk of severe cytokine release syndrome. Ensure all patients are well
hydrated before starting treatment. The following fractionated schedule over 2 days complies
with the UK CLL advisory board advice, and is in line with current RMH practice:
Dose 1:
Give rituximab over 2 days as follows:
Day 1: rituximab 50mg/m2 in 50ml sodium chloride 0.9% IV infusion at 50mg/hr fixed rate
throughout.
Day 2: rituximab 325mg/m2 in 250-500ml sodium chloride 0.9% IV infusion, start at
50mg/hr, escalate in 50mg/hr increments every 30 minutes to max 400mg/hr.
Dose 2:
If WBC < 25 x 109/L;
Give rituximab 500mg/m2 in 500ml sodium chloride 0.9% total dose on one day.
If no problems with Dose 1 infusions, start at 100mg/hr; escalate in 100mg/hr increments every
30 minutes to a maximum of 400mg/hr.
If reactions occurred with Dose 1, infuse as for Day 2 of Dose 1.
Reason for Update: new CDF drug
Version: 1
Supersedes: None
Prepared by: S Taylor
Approved by Chair of Alliance TSSG: Dr A Laurie
Date: 27.11.14
Review date: December 2016
Checked by: C Tucker
Page 1 of 4
If WBC > 25 x 109/L, consider fractionating again as follows:
Day 1: rituximab 125mg/m2 in 100-250ml sodium chloride 0.9%
Day 2: rituximab 375mg/m2 in 500ml sodium chloride 0.9%
If no problems with Dose 1 infusions, start both fractions at 100mg/hr; escalate in 100mg/hr
increments every 30 minutes to a maximum of 400mg/hr.
If reactions occurred with Dose 1, give both fractions as for Day 2 of Dose 1.
Dose 3 onwards:
*Assuming tolerated all previous infusions at standard rates, and WBC < 25*
Give rituximab 500mg/m2 in 500ml N/saline as a single dose.
Give 20% of dose (i.e. 100ml) over 30 minutes, then the remaining 80% (i.e. 400ml) over 1
hour, to give a total infusion time of 90 minutes.
* Patients who did not tolerate their previous infusion at the standard rate *
Infuse as per Day 2 of first infusion, or at a slower rate if required.
Monitoring:
For all rituximab infusions, monitor and record patients vital signs (blood pressure, pulse,
temperature and O2 saturation) at baseline and then every 30 minutes (before each increase
in infusion rate for escalating infusions) until the end of the infusion.
If reactions occur at any time, stop the infusion. If symptoms improve, restart at half the
previous infusion rate, and escalate as tolerated.
Calculating infusion
rates:
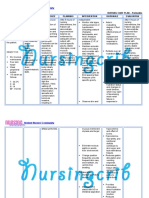
For rituximab doses in 500ml volume only, you may use the table below, or a locally
locally approved method of calculating infusion rates.
50
Rituximab banded
dose
500mg
525mg
550mg
575mg
600mg
650mg
675mg
700mg
750mg
800mg
825mg
850mg
900mg
950mg
1000mg
1050mg
1100mg
1150mg
100
150
Infusion Rate (mg/hour)
200
250
300
350
400
Infusion Rate (ml/hour) for rituximab in 500ml volume only
50
48
45
43
42
38
37
36
33
31
30
29
28
26
25
24
23
22
100
95
90
87
83
77
74
71
67
62
61
59
56
53
50
48
45
43
150
143
136
130
125
115
111
107
100
94
91
88
83
79
75
71
68
65
200
190
182
174
167
154
148
143
133
125
121
118
111
105
100
95
91
87
250
238
227
217
208
192
185
178
167
156
152
147
139
132
125
119
114
109
300
286
273
261
250
231
222
214
200
187
182
176
167
158
150
143
136
130
350
333
318
304
292
269
259
250
233
219
212
206
194
184
175
167
159
152
400
381
364
348
333
308
296
286
267
250
242
235
222
210
200
190
182
174
For rituximab in smaller volumes (50ml, 100ml or 250ml), do not refer to the table; you may
again use a locally approved method, or the following equation:
Infusion rate in ml/hr = required infusion rate in mg/hr x total volume (ml)
dose of rituximab (mg)
Reason for Update: new CDF drug
Version: 1
Supersedes: None
Prepared by: S Taylor
Approved by Chair of Alliance TSSG: Dr A Laurie
Date: 27.11.14
Review date: December 2016
Checked by: C Tucker
Page 2 of 4
Main Toxicities:
Rituximab:
severe cytokine release syndrome usually occurs within 12 hours of the
first rituximab infusion (see Comments) and consists of fever, headache, rigors, flushing,
nausea, rash, URTI symptoms; increased risk of infections
tumour lysis syndrome (ensure pre-medicated with allopurinol and good hydration)
transient hypotension and bronchospasm are usually infusion rate related;
Idelalisib:
increased transaminases;
diarrhoea;
pneumonitis;
rash
Anti - emetics:
mildly emetogenic (anti-emetic not usually required)
Extravasation:
rituximab is a non-vesicant
Regular
FBC
Investigations:
LFTs, including AST
U&Es
LDH
Comments:
Full resuscitation equipment must be available, with immediate access to clinical staff trained
in resuscitation for the first hour of the first rituximab infusion. Blood pressure, pulse,
temperature and O2 saturation must be measured and recorded at regular intervals as
specified above.
Interactions:
Avoid co-administration with CYP3A inducers (e.g. rifampicin, phenytoin, St Johns wort,
carbamazepine) as this may result in reduced plasma concentrations of idelalisib.
before every rituximab dose, then monthly for the first 6 months, then
up to every 3 months in stable patients
every 2 weeks for 3 months, then as clinically indicated
every 4 weeks
every 8 weeks
The primary metabolite of idelalisib, GS-563117, is a strong CYP3A4 inhibitor, and so the
concomitant use of idelalisib with medicinal products metabolised by CYP3A may lead to
increased serum concentrations of the other product. When idelalisib is co-administered with
other medicinal products, the Summary of Product Characteristics (SPC) for the other product
must be consulted for the recommendations regarding co-administration with CYP3A4
inhibitors. Concomitant treatment of idelalisib with CYP3A substrates with serious and/or lifethreatening adverse reactions (e.g., alfuzosin, amiodarone, cisapride, pimozide, quinidine,
ergotamine, dihydroergotamine, quetiapine, lovastatin, simvastatin, sildenafil, midazolam,
triazolam) should be avoided and alternative medicinal products that are less sensitive to
CYP3A4 inhibition should be used if possible.
Dose Modifications
Haematological
Toxicity:
If counts become low during treatment, this may be due to marrow infiltration and should be
discussed with Consultant before any further treatment is given.
Elevated liver transaminases:
ALT / AST
>3 5 x ULN
First occurrence of
>5 x ULN
Second occurrence of
>5 x ULN
Reason for Update: new CDF drug
Version: 1
Supersedes: None
Prepared by: S Taylor
Management
Increase monitoring of LFTs, including AST, to every week until
the values fall to 3 x ULN
Withhold idelalisib until ALT/AST 3 x ULN.
Then re-start idelalisib treatment at 100 mg twice daily.
If this event does not recur at 100mg bd, the dose can be
increased to 150 mg twice daily again, at the discretion of the
Consultant.
Withhold idelalisib until ALT/AST 3 x ULN.
Re-initiation at 100 mg twice daily may be considered, at the
discretion of the Consultant.
Approved by Chair of Alliance TSSG: Dr A Laurie
Date: 27.11.14
Review date: December 2016
Checked by: C Tucker
Page 3 of 4
Diarrhoea/colitis:
Idelalisib must be withheld in the event of Grade 3 or 4 diarrhoea/colitis. Once diarrhoea/colitis
has returned to Grade 1, idelalisib can be resumed at 100 mg bd. If diarrhoea/colitis does
not recur, the dose can be re-escalated to 150 mg bd, at the discretion of the Consultant.
Pneumonitis:
Idelalisib must be withheld in the event of suspected pneumonitis, and the patient treated
accordingly. Once pneumonitis has resolved and if re-treatment is considered appropriate,
resume at 100 mg bd.
Treatment must be discontinued for moderate or severe symptomatic pneumonitis.
Rash:
Idelalisib must be withheld in the event of Grade 3 or 4 rash. Once rash has returned to
Grade 1, treatment can be resumed at 100 mg bd. If rash does not recur, the dose can be reescalated to 150 mg bd, at the discretion of the Consultant.
Renal Impairment:
No idelalisib dose adjustments are required for patients with mild, moderate or severe renal
impairment.
Hepatic Impairment:
No dose adjustment of idelalisib is required when initiating treatment in patients with mild or
moderate hepatic impairment, but an intensified monitoring of adverse reactions is
recommended, as drug exposure is expected to be increased.
There is insufficient data to make dose recommendations for patients with severe hepatic
impairment. Therefore, caution and extra monitoring is recommended if using idelalisib in this
population.
Patient Information:
Macmillan leaflet for Rituximab
Idelalisib patient information leaflet available from Gilead
References:
Furman, R et al; NEJM 2014; 370: 997 - 1007
Reason for Update: new CDF drug
Version: 1
Supersedes: None
Prepared by: S Taylor
Approved by Chair of Alliance TSSG: Dr A Laurie
Date: 27.11.14
Review date: December 2016
Checked by: C Tucker
Page 4 of 4
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Cycloid Psychosis An Examination of The Validy of The ConceptDokumen9 halamanCycloid Psychosis An Examination of The Validy of The ConceptjoaogarcesBelum ada peringkat
- Spina BifidaDokumen27 halamanSpina BifidaSandy VillarBelum ada peringkat
- Physiotherapy - Scar MassageDokumen2 halamanPhysiotherapy - Scar MassageAlinaBelum ada peringkat
- WHO Classification of Head and Neck TumoursDokumen349 halamanWHO Classification of Head and Neck TumoursdrAlbertoVV100% (2)
- Nursing Care Plan For Peritonitis NCPDokumen2 halamanNursing Care Plan For Peritonitis NCPderic86% (7)
- Tretinoin (All Trans Retinoic Acid)Dokumen2 halamanTretinoin (All Trans Retinoic Acid)GabrielBelum ada peringkat
- R GCVP V2 2.15Dokumen3 halamanR GCVP V2 2.15GabrielBelum ada peringkat
- R Bendamustine 90 For Low Grade NHL V2 2.15Dokumen2 halamanR Bendamustine 90 For Low Grade NHL V2 2.15GabrielBelum ada peringkat
- Pentostatin V4 6.14Dokumen2 halamanPentostatin V4 6.14GabrielBelum ada peringkat
- Nilotinib V4 4.13Dokumen2 halamanNilotinib V4 4.13GabrielBelum ada peringkat
- Melphalan Oral V3 7.11Dokumen2 halamanMelphalan Oral V3 7.11GabrielBelum ada peringkat
- Intravenous Mel Dex July 08 Checked in Date Oct 2011Dokumen2 halamanIntravenous Mel Dex July 08 Checked in Date Oct 2011GabrielBelum ada peringkat
- Flag V7 3.15Dokumen2 halamanFlag V7 3.15GabrielBelum ada peringkat
- Presentation HaemoparasiteDokumen112 halamanPresentation HaemoparasiteMedicine 0786Belum ada peringkat
- Cardiovascular Disease EssayDokumen9 halamanCardiovascular Disease EssayW.flores07Belum ada peringkat
- CytopathologyDokumen19 halamanCytopathologyማላያላም ማላያላም100% (2)
- Shubham Das English Project Term 2Dokumen17 halamanShubham Das English Project Term 2Sukalpo BanerjeeBelum ada peringkat
- Hypocalcemia: Author: Christopher B Beach, MD, FACEP, FAAEM, Associate Professor and ViceDokumen65 halamanHypocalcemia: Author: Christopher B Beach, MD, FACEP, FAAEM, Associate Professor and ViceronelnBelum ada peringkat
- Combined Pulmonary Fibrosis and Emphysema - Case Report and Literature ReviewDokumen6 halamanCombined Pulmonary Fibrosis and Emphysema - Case Report and Literature ReviewAMALIAHAKIMBelum ada peringkat
- Test Bank For Emergency Care Emt 13th EditionDokumen30 halamanTest Bank For Emergency Care Emt 13th EditionCharles Pando100% (36)
- Globus PharyngusDokumen10 halamanGlobus PharyngusamalBelum ada peringkat
- Ineffective Airway ClearanceDokumen6 halamanIneffective Airway ClearanceKarl Angelo MontanoBelum ada peringkat
- Ectopic-Pregnancy - Assign - Khan AliDokumen8 halamanEctopic-Pregnancy - Assign - Khan AliMohammad KhanBelum ada peringkat
- OCD Lecture NotesDokumen4 halamanOCD Lecture NotesAustin Higgins67% (3)
- HEENT Case Study 2Dokumen5 halamanHEENT Case Study 2AlexanderWarrenBelum ada peringkat
- Blood Product Transfusion in Adults: Indications, Adverse Reactions, and ModificationsDokumen9 halamanBlood Product Transfusion in Adults: Indications, Adverse Reactions, and ModificationsDiego MerchánBelum ada peringkat
- Salmonellosis 2021Dokumen36 halamanSalmonellosis 2021mehrshad Farahpour Gp5Belum ada peringkat
- Journal Reading FixDokumen20 halamanJournal Reading FixElsa MayoraBelum ada peringkat
- Hypertensive Crisis: Syed RazaDokumen45 halamanHypertensive Crisis: Syed RazaAndika HBelum ada peringkat
- TURP SyndromeDokumen13 halamanTURP SyndromeWindy Ari WijayaBelum ada peringkat
- Nursing Care Plan For Ineffective Cerebral Tissue PerfusionDokumen2 halamanNursing Care Plan For Ineffective Cerebral Tissue PerfusionKate CruzBelum ada peringkat
- V 5 N 1Dokumen190 halamanV 5 N 1Jorge RodriguezBelum ada peringkat
- Case Report: 2 NovemberDokumen22 halamanCase Report: 2 NovemberandrianyBelum ada peringkat
- Bulimia NervosaDokumen12 halamanBulimia NervosaNehaBelum ada peringkat
- RME Child at 1 MonthDokumen20 halamanRME Child at 1 MonthhafizBelum ada peringkat
- FFFFFFF: Health Declaration Form Health Declaration Form Health Declaration FormDokumen1 halamanFFFFFFF: Health Declaration Form Health Declaration Form Health Declaration FormLeny Goyo LaurenteBelum ada peringkat
- Anxiety DisorderDokumen44 halamanAnxiety DisorderKemal AmanoBelum ada peringkat
- Health Vocabulary - Unit 6Dokumen2 halamanHealth Vocabulary - Unit 6Hind BenelgamraBelum ada peringkat