Sexual Precocity PDF
Diunggah oleh
mist73Deskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Sexual Precocity PDF
Diunggah oleh
mist73Hak Cipta:
Format Tersedia
Sexual Precocity
Basics
DESCRIPTION
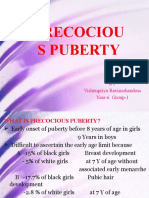
Sexual precocity has traditionally been defined as physical signs of sexual development before age 8 years in girls
and age 9 in boys.
Recently, new guidelines were proposed for lowering the age considered to be normal for sexual development in
girls:
1. Signs of puberty as young as age 7 in white girls and age 6 in black girls may be normal.
2. These new guidelines have not been universally adopted.
The entire clinical picture, including rate of progression and the presence of neurologic symptoms, must be taken
into account.
EPIDEMIOLOGY
Precocious puberty is 56 times more common in girls.
8090% of affected girls have central precocious puberty.
Precocious puberty in boys is more likely to be associated with underlying pathology.
~50% of affected boys have central precocious puberty.
Increased incidence seen in internationally adopted children and in children born premature or small for gestational
age
Incidence
Precocious puberty occurs in 1 in 5,000 children
RISK FACTORS
Genetics
Familial male precocious puberty (testitoxicosis): Sex-limited, autosomal dominant inheritance of activating
mutation in the luteinizing hormone (LH) receptor
McCuneAlbright syndrome: Sporadic, postzygotic, somatic mutation in the stimulatory subunit of G-protein
receptor; more common in girls
PATHOPHYSIOLOGY
Central precocious puberty can be associated with CNS disorders
Peripheral precocious puberty is associated with gonadal and adrenal disorders.
Peripheral precocious puberty can progress to central precocious puberty due to maturation of the hypothalamic
pituitary axis by sex steroids.
ETIOLOGY
Central precocious puberty (gonadotropin-releasing hormone [GnRH]dependent):
Associated with gonadotropin (LH and/or follicle-stimulating hormone [FSH]) levels that are elevated beyond the
normal prepubertal range. Results from activation of hypothalamicpituitarygonadal axis.
Peripheral precocious puberty (GnRH-independent): Gonadotropin-independent elevation of sex steroids arising (i)
directly from gonads and/or adrenals, (ii) through stimulation of gonads by GnRH-independent mechanism, or (iii)
from an exogenous source
Diagnosis
SIGNS AND SYMPTOMS
Careful chronology of physical changes, growth spurt, onset of menses
Presence of neurologic, visual, or behavioral changes to suggest a CNS lesion
History
Family history of early puberty
Presence of exogenous sex steroids in the home
Physical Exam
Plot accurate height (using wall-mounted stadiometer), weight, and growth velocity.
Carefully stage breasts, color of vaginal mucosa, and pubic hair in girls.
Carefully stage testicular volume (with Prader gonadometer), penile size, and pubic hair in boys.
Carefully evaluate for abdominal masses.
Examine skin for acne and caf au lait spots.
Perform comprehensive neurologic evaluation to assess for possible CNS pathology.
TESTS
LABORATORY
Sex steroids: Estradiol, testosterone
Adrenal steroids: 17-OH progesterone, dehydroepiandrosterone sulfate (DHEA-S), androstenedione
Gonadotropins: FSH, LH (ultrasensitive or immunochemiluminometric [ICMA]-LH most accurate)
Prolactin: May be elevated with CNS tumors
Thyroid-stimulating hormone (TSH) and free thyroxine (T4)
Human chorionic gonadotropin levels
Provocative tests should be done when the aforementioned tests are abnormal or equivocal:
1. GnRH test for central precocious puberty; prepubertal GnRH response is predominately FSH, whereas
pubertal response is predominately LH
2. Adrenocorticotropic hormone (ACTH) stimulation test for adrenal abnormalities. Exogenous
corticosteroid therapy will interfere with ACTH test, but does not interfere with GnRH test of pituitary
gonadal axis.
IMAGING
Bone age: If advanced, further studies are warranted, guided by history and physical examination. If not advanced,
or if the patient has only mild breast or pubic hair development (but not both), premature thelarche or premature
adrenarche, respectively, is the most likely diagnosis.
MRI of head: As indicated by history, physical examination, and laboratory tests; almost always done in boys
because they are much less likely than are girls to have idiopathic sexual precocity
Ultrasound of gonads/adrenals: As indicated by examination and studies. Look for tumors in both sexes; in girls,
ultrasound can also evaluate development of ovaries and uterus.
CLINICAL:
Obese children often have advanced bone age.
Palpation of breast tissue (buds) can be difficult due to adiposity.
DIFFERENTIAL DIAGNOSIS
Causes of central precocious puberty:
1. Often idiopathic (girls more often than boys)
2. Any cause of peripheral precocious puberty
3. Tumors:
1. CNS tumors
2. Hypothalamic hamartoma: Most common CNS mass to cause precocious puberty; benign
(nonprogressive), congenital malformation of neurons that secrete GnRH
3. Hypothalamic-chiasmatic glioma: Often associated with neurofibromatosis
4. Astrocytoma
5. Ependymoma
4. Post-CNS trauma or damage:
1. Surgery
2. Radiation: May occur after 18-Gy exposure
3. Hydrocephalus and other CNS malformations
4. Infection: Brain abscess, meningitis, encephalitis, granuloma. Lesions may result in stimulation
or lack of inhibition of the GnRH-secreting area of the hypothalamus, resulting in early activation
of the pituitary
Causes of peripheral precocious puberty:
1. Tumors:
1. Human chorionic gonadotropin-secreting tumors: May arise from pineal gland or liver
2. Gonadal tumors
3. Adrenal tumors
2. Environmental: Exogenous estrogens (creams and oral forms) and/or exogenous androgens (anabolic
steroids or testosterone formulations)
3. Congenital adrenal hyperplasia: Poorly controlled CAH can activate the hypothalamicpituitarygonadal
axis in either gender
4. Severe acquired hypothyroidism: High levels of TSH may cross-stimulate gonadal FSH and/or LH
receptors.
5. McCuneAlbright syndrome: Triad of precocious puberty, caf au lait spots, and polyostotic fibrous
dysplasia
6. Familial male precocious puberty (familial testitoxicosis)
7. Refeeding after severe malnutrition during early development (such as adopted children who had
kwashiorkor)
Other disorders:
1. Premature thelarche
2. Premature adrenarche
3. Obesity
Treatment
GENERAL MEASURES
As indicated by cause of the precocious puberty, removal of CNS lesions or cessation of exogenous sex steroids
MEDICATIONS
Central precocious puberty: GnRH agonists such as leuprolide (Lupron) are the treatment of choice. Adjunctive
therapy with growth hormone may improve final adult height.
Calcium supplementation may preserve bone mass accretion during GnRH agonist therapy.
Peripheral precocious puberty: Aromatase inhibitors and antiandrogens (spironolactone or ketoconazole).
Glucocorticoids for congenital adrenal hyperplasia
SURGERY
Removal of CNS lesions if present
Follow-up Recommendations
When to expect improvement:
1. Depends on cause. For example, sexual changes of McCuneAlbright syndrome are due to autonomously
functioning ovarian cysts, which regress variably over time.
2. Treatment of central precocious puberty with a GnRH agonist usually results in cessation of menses within
2 months, slowing or nonprogression of pubertal changes over 46 months, and decreased acceleration of
bone age within 12 months.
Typically, GnRH agonists are given in a depot form every 28 days. Some children require shortening of this
interval, often prompted by reports of moodiness, development of acne, or breakthrough menses.
EXPECTED COURSE/PROGNOSIS
With treatment, improvement in predicted height is achieved, but most children do not reach target height predicted
by midparental height measurements. Earlier treatment results in improved final height.
Effect of GnRH agonists on fertility has not been fully elucidated.
POSSIBLE COMPLICATIONS
Short stature
Psychosocial stresses of early puberty
Frequently Asked Questions
Q: If my child is treated with GnRH agonists, will he/she go through puberty when we stop the medication?
A: Yes, children on GnRH agonist treatment do proceed through normal puberty when the medication is stopped.
Effects on fertility have not been fully studied long-term.
Q: If my child already has some pubertal changes, can they be reversed?
A: If GnRH agonists are used, menses will cease, and breast tissue and pubic hair will often regress.
Anda mungkin juga menyukai
- Precociou S Puberty: BY Vishnupriya Ravimohandoss Year-6 Group-1Dokumen31 halamanPrecociou S Puberty: BY Vishnupriya Ravimohandoss Year-6 Group-1Priya RaviBelum ada peringkat
- Treatment and Outcomes of Precocious Puberty: An UpdateDokumen11 halamanTreatment and Outcomes of Precocious Puberty: An UpdateAbdurrahman Hasanuddin100% (1)
- Puberty Normal and AbnormalDokumen41 halamanPuberty Normal and AbnormalTonyScariaBelum ada peringkat
- Precocious PubertyDokumen30 halamanPrecocious PubertyNeha SharmaBelum ada peringkat
- Idiopathic Central Precocious Puberty A Case ReportDokumen8 halamanIdiopathic Central Precocious Puberty A Case ReportCarolyn CapisnonBelum ada peringkat
- Physiology and PubertyDokumen8 halamanPhysiology and PubertynofiajahBelum ada peringkat
- Puberty: Normal Development and Causes of Precocious PubertyDokumen8 halamanPuberty: Normal Development and Causes of Precocious Pubertyclear mindBelum ada peringkat
- 3 - Precocious PubertyDokumen9 halaman3 - Precocious PubertyJohnM.GiraldoBelum ada peringkat
- Tall StatureDokumen24 halamanTall StaturedianmutiaBelum ada peringkat
- Growth & Development of An Adolescent (2380)Dokumen8 halamanGrowth & Development of An Adolescent (2380)ta CBelum ada peringkat
- And Tab 1Dokumen4 halamanAnd Tab 1Bella SuratmonoBelum ada peringkat
- Am I Normal - A Systematic Review and Construction of Nomograms For Flaccid and Erect Penis Length and Circumference in Up To 15 521 MenlDokumen9 halamanAm I Normal - A Systematic Review and Construction of Nomograms For Flaccid and Erect Penis Length and Circumference in Up To 15 521 MenlBlack HoleBelum ada peringkat
- Precocious VS Early Puberty, SiskaDokumen21 halamanPrecocious VS Early Puberty, SiskapuspaBelum ada peringkat
- Gynecology AbnormalPubertyandGrowthProblemsDokumen6 halamanGynecology AbnormalPubertyandGrowthProblemsBhi-An BatobalonosBelum ada peringkat
- Precocious PUBERTYDokumen4 halamanPrecocious PUBERTYjprakashjjBelum ada peringkat
- Penile Length Study Finds No Patients With Severely Short PenisDokumen4 halamanPenile Length Study Finds No Patients With Severely Short PenisNunuh Sulaeman100% (1)
- Precosious Puberty Case StudyDokumen27 halamanPrecosious Puberty Case Studynishavohreh100% (1)
- Abnormal Development of Female Genital TractDokumen69 halamanAbnormal Development of Female Genital TractJerry CreedBelum ada peringkat
- Mikropenis NcbiDokumen7 halamanMikropenis NcbiIceBearBelum ada peringkat
- Management of Foreskin ConditionsDokumen26 halamanManagement of Foreskin ConditionsSarif CassanovaBelum ada peringkat
- Proper Circumcision Techniques for Infants and AdultsDokumen6 halamanProper Circumcision Techniques for Infants and Adultsntambik21Belum ada peringkat
- Precocious PubertyDokumen27 halamanPrecocious PubertyManesha PutraBelum ada peringkat
- Fertilisasi Askeb IDokumen19 halamanFertilisasi Askeb IPutry Utami0% (1)
- PenisDokumen23 halamanPenisWira DharmaBelum ada peringkat
- Sign of Hyperandrogenism PDFDokumen6 halamanSign of Hyperandrogenism PDFmisbah_mdBelum ada peringkat
- Circumcision Using The Mogen ClampDokumen4 halamanCircumcision Using The Mogen ClampJorge AndrésBelum ada peringkat
- Tuberculous Otitis Media 20100326Dokumen32 halamanTuberculous Otitis Media 20100326Riska Nur AiniBelum ada peringkat
- Kelainan Penis Pada AnakDokumen23 halamanKelainan Penis Pada AnakAndrew SoerijadiBelum ada peringkat
- Kegel Handout PDFDokumen1 halamanKegel Handout PDFMini ManojBelum ada peringkat
- Scrotal Disease - 2Dokumen47 halamanScrotal Disease - 2Hillary BushnellBelum ada peringkat
- Amputation of The Penis: A.Venugopalan PG 212 LAS. 164Dokumen14 halamanAmputation of The Penis: A.Venugopalan PG 212 LAS. 164Shayan JuttBelum ada peringkat
- Partograph 1Dokumen22 halamanPartograph 1SIRBENZBelum ada peringkat
- PubertyDokumen2 halamanPubertyana8stesia8suarfiBelum ada peringkat
- Kipp Mandatory Penis InspectionDokumen1 halamanKipp Mandatory Penis InspectionJeff barkerBelum ada peringkat
- Primary and Secondary AmenorrhoeaDokumen72 halamanPrimary and Secondary Amenorrhoead clarkeBelum ada peringkat
- PenisDokumen2 halamanPenismichelle labaoBelum ada peringkat
- Investigation InfertilityDokumen44 halamanInvestigation InfertilityDenisBelum ada peringkat
- Lecture 124 MALE INFERTILITY by Dr. NayyerDokumen63 halamanLecture 124 MALE INFERTILITY by Dr. NayyerRizwan AhmedBelum ada peringkat
- I-3 Pediatric and Adolescent GynecologyDokumen8 halamanI-3 Pediatric and Adolescent GynecologyuvioscribdBelum ada peringkat
- Kuliah Penis & ScrotumDokumen13 halamanKuliah Penis & ScrotumEmallia Phypiet FitrianiBelum ada peringkat
- 2012 Longer Penis OrgasmsDokumen10 halaman2012 Longer Penis OrgasmsLucano Alvares100% (1)
- Pediatric RadiologyDokumen59 halamanPediatric RadiologyNguyễn Tiến ĐồngBelum ada peringkat
- Prostate and Seminal VesiclesDokumen83 halamanProstate and Seminal Vesiclesgreg_enricoBelum ada peringkat
- Azoospermia Guidelines PDFDokumen7 halamanAzoospermia Guidelines PDFafifberlianBelum ada peringkat
- Human Sexual IntercourseDokumen22 halamanHuman Sexual Intercoursetajuddin0786gmailcomBelum ada peringkat
- Sexual Medicine Committee Newsletter 3Dokumen11 halamanSexual Medicine Committee Newsletter 3Khushi Shukla100% (1)
- Anatomy and Blood Supply of the PenisDokumen7 halamanAnatomy and Blood Supply of the PenisalexBelum ada peringkat
- The Reproductive SystemDokumen266 halamanThe Reproductive SystemNatia DemetradzeBelum ada peringkat
- Rare Congenital Genitourinary AnomaliesDokumen27 halamanRare Congenital Genitourinary Anomaliesد. محمد عبد الباقي فهميBelum ada peringkat
- StratOG Vaginal BreechDokumen17 halamanStratOG Vaginal BreechNalin AbeysingheBelum ada peringkat
- C Ovid 19 Treatment GuidelinesDokumen356 halamanC Ovid 19 Treatment GuidelinesSebastian LozanoBelum ada peringkat
- Case Presentation Testicular TorsonDokumen16 halamanCase Presentation Testicular TorsonMestikarini AstariBelum ada peringkat
- Menopause GuideDokumen26 halamanMenopause GuideSofia Pranacipta0% (1)
- McCoy - Reasons For Pretending Orgasm InventoryDokumen11 halamanMcCoy - Reasons For Pretending Orgasm InventoryCsanyi EditBelum ada peringkat
- Sperm Count and Male InfertilityDokumen4 halamanSperm Count and Male Infertilitynica_ocampoBelum ada peringkat
- Hypospadias Surgery: An Illustrated GuideDari EverandHypospadias Surgery: An Illustrated GuideAhmed HadidiPenilaian: 5 dari 5 bintang5/5 (1)
- Anejaculation, (Absence of Ejaculate) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandAnejaculation, (Absence of Ejaculate) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Handbook of Current and Novel Protocols for the Treatment of InfertilityDari EverandHandbook of Current and Novel Protocols for the Treatment of InfertilityMichael H. DahanBelum ada peringkat
- JPOG December 2014 HK PDFDokumen58 halamanJPOG December 2014 HK PDFmist73Belum ada peringkat
- Scheduling GuideDokumen33 halamanScheduling GuideSeetal Kaur0% (1)
- 40Dokumen16 halaman40mist73Belum ada peringkat
- Intussusception PDFDokumen3 halamanIntussusception PDFmist73100% (1)
- Cigna Senior Life Plan Details PDFDokumen1 halamanCigna Senior Life Plan Details PDFmist73Belum ada peringkat
- Skilled Migration Update PDFDokumen44 halamanSkilled Migration Update PDFmist73Belum ada peringkat
- Cme201511 PDFDokumen30 halamanCme201511 PDFmist73Belum ada peringkat
- Wesley Lodge Accommodation - Information Sheet PDFDokumen1 halamanWesley Lodge Accommodation - Information Sheet PDFmist73Belum ada peringkat
- Template Form Updates UD8 Provision of Medical Services Statement - PDF 32836586 PDFDokumen1 halamanTemplate Form Updates UD8 Provision of Medical Services Statement - PDF 32836586 PDFmist73Belum ada peringkat
- Intestinal Obstruction PDFDokumen7 halamanIntestinal Obstruction PDFmist73Belum ada peringkat
- Jaundice PDFDokumen6 halamanJaundice PDFmist73Belum ada peringkat
- Enuresis PDFDokumen7 halamanEnuresis PDFmist73Belum ada peringkat
- FFTDokumen7 halamanFFTmist73Belum ada peringkat
- HT PDFDokumen5 halamanHT PDFmist73Belum ada peringkat
- Cystic Fibrosis PDFDokumen6 halamanCystic Fibrosis PDFmist73Belum ada peringkat
- Hirschsprung DiseaseDokumen5 halamanHirschsprung Diseasemist73Belum ada peringkat
- Cushing SyndromeDokumen5 halamanCushing Syndromemist73Belum ada peringkat
- GN Types, Causes, Symptoms & TreatmentDokumen5 halamanGN Types, Causes, Symptoms & Treatmentmist73Belum ada peringkat
- Bronchiolitis PDFDokumen9 halamanBronchiolitis PDFmist73Belum ada peringkat
- Pneumonia PDFDokumen7 halamanPneumonia PDFmist73Belum ada peringkat
- Asthma PDFDokumen11 halamanAsthma PDFmist73Belum ada peringkat
- Epilepsy PDFDokumen6 halamanEpilepsy PDFmist73Belum ada peringkat
- Behavioral or Psychiatric Problems PDFDokumen5 halamanBehavioral or Psychiatric Problems PDFmist73Belum ada peringkat
- Cerebral PalsyDokumen7 halamanCerebral Palsymist73Belum ada peringkat
- Anorexia Nervosa PDFDokumen6 halamanAnorexia Nervosa PDFmist73Belum ada peringkat
- Otago Distance Learning Prospectus 2016Dokumen35 halamanOtago Distance Learning Prospectus 2016mist73Belum ada peringkat
- Allergy and Immunology Melanie Wong LO 2015Dokumen1 halamanAllergy and Immunology Melanie Wong LO 2015mist73Belum ada peringkat
- Osteomyelitis: Osteomyelitis Is Infection in The Bone. Osteomyelitis Can Occur in InfantsDokumen4 halamanOsteomyelitis: Osteomyelitis Is Infection in The Bone. Osteomyelitis Can Occur in Infantstiban_07Belum ada peringkat
- Pacres SpeechDokumen3 halamanPacres SpeechJohn Emmanuel PacresBelum ada peringkat
- Effects of Drug Abuse on Health and SocietyDokumen9 halamanEffects of Drug Abuse on Health and SocietyAditya guptaBelum ada peringkat
- Maria Thomas PDFDokumen143 halamanMaria Thomas PDFElizabeth Sinchana100% (2)
- Miasm IntroductionDokumen11 halamanMiasm IntroductionsurabhiBelum ada peringkat
- Table 2: Endocrine Disorders Disorders Symptoms Lab Test ResultsDokumen3 halamanTable 2: Endocrine Disorders Disorders Symptoms Lab Test ResultsRamil BondadBelum ada peringkat
- Medical Billing ProcessDokumen24 halamanMedical Billing ProcessNajamHass100% (5)
- Contoh Soal Bahasa InggrisDokumen17 halamanContoh Soal Bahasa InggrisYuli KurniawatiBelum ada peringkat
- The same questions apply as aboveDokumen29 halamanThe same questions apply as aboveمحمد عزيز حسن ماضيBelum ada peringkat
- Salicylic Acid and Sulfur (Topical Route) : Commonly Used Brand Name(s)Dokumen9 halamanSalicylic Acid and Sulfur (Topical Route) : Commonly Used Brand Name(s)Gutu DoinaBelum ada peringkat
- Lumbar PunctureDokumen18 halamanLumbar PunctureJaspreet KangBelum ada peringkat
- Impact of Small-Scale Mining To The ResidentsDokumen15 halamanImpact of Small-Scale Mining To The ResidentsAngelIgualdoSagapiBelum ada peringkat
- Peace Corps Mefloquine Policy March 2015 Letter To DirectorDokumen7 halamanPeace Corps Mefloquine Policy March 2015 Letter To DirectorAccessible Journal Media: Peace Corps DocumentsBelum ada peringkat
- P T of Comm NSGDokumen27 halamanP T of Comm NSGBabita DhruwBelum ada peringkat
- Pe Reviewer PrelimDokumen2 halamanPe Reviewer PrelimCumberbatch Depp KaiBelum ada peringkat
- Lab Report: 2743025 LAB/20N/121831 27/jan/2022 Mr. Naman Thapliyal 13649512 StatusDokumen2 halamanLab Report: 2743025 LAB/20N/121831 27/jan/2022 Mr. Naman Thapliyal 13649512 StatusM Abdul MoidBelum ada peringkat
- Sbo and Ecf (Doc Gallo) SGD SurgeryDokumen113 halamanSbo and Ecf (Doc Gallo) SGD SurgeryNikki MacasaetBelum ada peringkat
- Standards For Sanitation: What, Why and How?: Kate Hurley, DVM, MPVMDokumen26 halamanStandards For Sanitation: What, Why and How?: Kate Hurley, DVM, MPVMKaren SalcedoBelum ada peringkat
- Critical Care TransportDokumen7 halamanCritical Care TransporttaqinosBelum ada peringkat
- Chief complaint dental historyDokumen6 halamanChief complaint dental historyralucaBelum ada peringkat
- Curative COVID-19 Test Results ReportDokumen1 halamanCurative COVID-19 Test Results ReportIsabella FonsecaBelum ada peringkat
- YL Camping Consent and Health FormDokumen4 halamanYL Camping Consent and Health Formmcronin1970Belum ada peringkat
- Neonates: Clinical Syndromes and Cardinal Fea-Tures of Infectious Diseases: Approach To Diagnosis and Initial ManagementDokumen7 halamanNeonates: Clinical Syndromes and Cardinal Fea-Tures of Infectious Diseases: Approach To Diagnosis and Initial ManagementFatma ElzaytBelum ada peringkat
- Pneumonia AnswersDokumen5 halamanPneumonia AnswersColeen Mae CamaristaBelum ada peringkat
- Factors Associated With Compassion Satisfaction, Burnout, andDokumen30 halamanFactors Associated With Compassion Satisfaction, Burnout, andpratiwi100% (1)
- Group1 - BSN2-C - ASYNCHRONOUS ACTIVITY INFOGRAPHICSDokumen3 halamanGroup1 - BSN2-C - ASYNCHRONOUS ACTIVITY INFOGRAPHICSJollan Marie BuenvenidaBelum ada peringkat
- Healthy Delights Magazine Filled With 42 Quick RecipesDokumen8 halamanHealthy Delights Magazine Filled With 42 Quick RecipesYasser NazmyBelum ada peringkat
- Career CounselingDokumen13 halamanCareer CounselingPooja PatelBelum ada peringkat
- NHS Patient Safety SyllabusDokumen22 halamanNHS Patient Safety SyllabusMubeenRahmanBelum ada peringkat
- EITC HSE Qualifications CalendarDokumen15 halamanEITC HSE Qualifications Calendarm_othman_4Belum ada peringkat