Research
Diunggah oleh
Shuaib AkramHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Research
Diunggah oleh
Shuaib AkramHak Cipta:
Format Tersedia
Shuaib Akram
Is it better to give people mosquito nets or
make them pay?
desire for better health' and 'are governments to
blame'
Links: http://www.pooreconomics.com/data/country/home
Rafae low hanging fruit
Rizki: health trap
Akash: under-utilised miracles
Shuaib: desire for better health
Akash: money for nothing
Shuaib: are governments to blame
Adya: Does free mean worthless
Khalil: Faith
Khalil: Weak beliefs + necessity of hope
http://nairobi.usembassy.gov/itns_fact_sheet.html
Nowadays, the governments of the US and Australia, along with many other
countries which do not have malaria, still assist in the fight against malaria by
funding malaria control programs in other countries, either directly (for example, the
US funds international health projects through the US Agency for International
Development) or indirectly, through international organisations like the World Health
Organisation and the Global Fund for HIV, TB and Malaria. They also provide
training in technical expertise to scientists, doctors and clinicians from malariaendemic countries.
The governments of countries which have malaria are also deeply engaged in
fighting the disease, mostly through their respective Ministries of Health, which often
have specific malaria departments. In India, for example, malaria control is carried
out by the National Vector Borne Disease Control Programme (NVBDCP), which is
part of the Directorate General of Health Services. The NVBDCP carries out a multi-
Shuaib Akram
pronged strategy to combat malaria, including early case detection and treatment,
vector control (with spraying, biological control and personal protection), community
participation, etc. In Uganda, the Malaria Control Programme also carries out the
above activities, and also provides intermittent preventative treatment against
malaria for young children and pregnant women and has in the past engaged in
large-scale distribution of long-lasting insecticide treated bednets. Both countries
also explicitly include monitoring and evaluation as part of their control strategies, to
make sure that any interventions or control efforts they make are having a positive
impact on reducing malaria morbidity and mortality.
Malaria imposes substantial costs to both individuals and governments.
Costs to individuals and their families include purchase of drugs for treating malaria at home;
expenses for travel to, and treatment at, dispensaries and clinics; lost days of work; absence
from school; expenses for preventive measures; expenses for burial in case of deaths.
Costs to governments include maintenance, supply and staffing of health facilities; purchase of
drugs and supplies; public health interventions against malaria, such as insecticide spraying or
distribution of insecticide-treated bed nets; lost days of work with resulting loss of income; and
lost opportunities for joint economic ventures and tourism.
Direct costs (for example, illness, treatment, premature death) have been estimated to be at least
US$ 12 billion per year. The cost in lost economic growth is many times more than that.
Presidents malaria intitiative
PSI (population services international) http://www.nothingbutnets.net/partners/psi.html?
referrer=https://www.google.co.uk/
And look at fact sheet
Can talk about how Kenya has benefited from the PSI and had caused to creat PMI
Health policy plan journal Evans
Impressive results in Kenya, achieved by means of the new WHOrecommended strategy, show that free mass distribution of long-lasting
insecticidal nets is a powerful way to quickly and dramatically increase
coverage, particularly among the poorest people.
Shuaib Akram
In Kenya, from 2004 to 2006, a near ten-fold increase in the number of young children
sleeping under insecticide-treated mosquito nets was observed in targeted districts,
resulting in 44% fewer deaths than among children not protected by nets, according
to preliminary data from the Government of Kenya. This is the first demonstration of
the impact of large-scale distribution of insecticide treated mosquito nets under
programme conditions, rather than in research settings, where, in different parts of
Africa, reduction observed in overall mortality has ranged from 14 % up to 60 %.
These achievements can be attributed to three principal ingredients, which all need to
be present for malaria control efforts to succeed - high political commitment from the
government, strong technical assistance from WHO, and adequate funding from
bilateral and multilateral donors.
http://www.who.int/mediacentre/news/releases/2007/pr43/en/
Check PSI ITN case study
The PMI is expanding access to free or highly subsidized nets while also creating commercial
markets in African countries. It supports the provision of free nets to those at highest risk from
malaria-pregnant women and children under age 5, particularly infants-and to those who cannot
afford to purchase a mosquito net. It also provides low-cost ITNs where they are needed most and
sells subsidized nets to increase demand, availability, and affordability among vulnerable
populations.
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Top Muscle Building and Weight Gain SecretsDokumen8 halamanTop Muscle Building and Weight Gain SecretsKarl Gallagher83% (6)
- Attending Physician Statement (APS) - TPD - FamilyDokumen3 halamanAttending Physician Statement (APS) - TPD - FamilyTaufik Hameed SultanBelum ada peringkat
- Community Health NursingDokumen14 halamanCommunity Health Nursingyasira0% (1)
- The Dangers of Sitting - Why Sitting Is The New Smoking - Better Health ChannelDokumen10 halamanThe Dangers of Sitting - Why Sitting Is The New Smoking - Better Health ChannelTHE PRATHAM SRIVASTAVA.Belum ada peringkat
- 4832 Concept Map On Failure To Thrive-Desktop-1dptoe6Dokumen11 halaman4832 Concept Map On Failure To Thrive-Desktop-1dptoe6api-603346045Belum ada peringkat
- Ssp-Appendix 07 Smsts CDMDokumen24 halamanSsp-Appendix 07 Smsts CDMAnonymous L0bC6SJBelum ada peringkat
- Cultural Competence or Cultural Humility Moving Beyond The DebateDokumen4 halamanCultural Competence or Cultural Humility Moving Beyond The DebateEstela MedinaBelum ada peringkat
- RLE-level-2-Learning-packet-2-Blue-week-2 (Sanaani, Nur-Fatima, M.)Dokumen29 halamanRLE-level-2-Learning-packet-2-Blue-week-2 (Sanaani, Nur-Fatima, M.)Nur SanaaniBelum ada peringkat
- OHS-PR-09-03-F02 RISK ASSESSMENT For INSTALLATION OF WALL MOUNTED JIB CRANEDokumen21 halamanOHS-PR-09-03-F02 RISK ASSESSMENT For INSTALLATION OF WALL MOUNTED JIB CRANEmohammed tofiqBelum ada peringkat
- Cognitive Behavioral Guided Self Help For The Treatment Od Recurrent Binge EatingDokumen19 halamanCognitive Behavioral Guided Self Help For The Treatment Od Recurrent Binge EatingIsmael RodriguezBelum ada peringkat
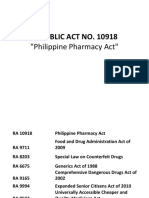
- PharmacyDokumen78 halamanPharmacyGelie BundocBelum ada peringkat
- The Right To Die: Pre-ReadingDokumen8 halamanThe Right To Die: Pre-ReadingGiovanni EscobarBelum ada peringkat
- TFN ReviewerDokumen18 halamanTFN Reviewerkiki park100% (1)
- LP 20 Health Q3Dokumen8 halamanLP 20 Health Q3Hazel Rubas SamsonBelum ada peringkat
- Outpatients Unit - Guideline Section - International Health Facility GuidelinesDokumen23 halamanOutpatients Unit - Guideline Section - International Health Facility GuidelinesSebastian laierBelum ada peringkat
- NIH Document Production Cover Letter 2021.10.20 McMorris RodgersDokumen2 halamanNIH Document Production Cover Letter 2021.10.20 McMorris RodgersAl StatiliusBelum ada peringkat
- JournalDokumen1 halamanJournaljasper pachingelBelum ada peringkat
- Research ProposalDokumen6 halamanResearch ProposalAhmad NajjarBelum ada peringkat
- Opt WorkshopDokumen15 halamanOpt WorkshopMhel Daz BabaysonBelum ada peringkat
- Jesse Smith Letter of ReccDokumen1 halamanJesse Smith Letter of Reccapi-510425013Belum ada peringkat
- An Overview of The Role of Nurses and Midwives in Leadership and Management in EuropeDokumen44 halamanAn Overview of The Role of Nurses and Midwives in Leadership and Management in EuropeTCBelum ada peringkat
- Intradermal Delivery Vaccines Report 2009 SeptDokumen94 halamanIntradermal Delivery Vaccines Report 2009 SeptSantoso CokroBelum ada peringkat
- 50 Item Integumentary Exam-BudekDokumen8 halaman50 Item Integumentary Exam-BudekLj FerolinoBelum ada peringkat
- Heutagogy Learning Beyond The Classroom Vijaya Bhanu IndiaDokumen24 halamanHeutagogy Learning Beyond The Classroom Vijaya Bhanu IndiaVijayaBhanuKoteBelum ada peringkat
- Calcium CarbideDokumen8 halamanCalcium CarbidetaraBelum ada peringkat
- Chronic Renal Failure Nursing Care PlanDokumen6 halamanChronic Renal Failure Nursing Care PlanRuva Oscass JimmyBelum ada peringkat
- Meniere' S Disease: (Endolymphatic Hydrops)Dokumen9 halamanMeniere' S Disease: (Endolymphatic Hydrops)WillieBelum ada peringkat
- Sequalae of Wearing Complete DenturesDokumen34 halamanSequalae of Wearing Complete DenturesAyeshaAslamBelum ada peringkat
- P RM 01 Incident Reporting PolicyDokumen44 halamanP RM 01 Incident Reporting PolicypatientsafetyBelum ada peringkat
- Wound Forum 14Dokumen12 halamanWound Forum 14Lia Mar'atush SholihahBelum ada peringkat