Management of Wound
Diunggah oleh
progiezHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Management of Wound
Diunggah oleh
progiezHak Cipta:
Format Tersedia
19 CME REVIEWARTICLE
Volume 60, Number 7
OBSTETRICAL AND GYNECOLOGICAL SURVEY
Copyright 2005
by Lippincott Williams & Wilkins
CHIEF EDITORS NOTE: This article is part of a series of continuing education activities in this Journal through which a total
of 36 AMA/PRA category 1 credit hours can be earned in 2005. Instructions for how CME credits can be earned appear on
the last page of the Table of Contents.
Management of Wound Complications
From Cesarean Delivery
Sue Ellen Sarsam, CNM,* John P. Elliott, and Garrett K. Lam, MD
*Nurse Practitioner, Phoenix Perinatal Associates, an Affiliate of Obstetrix Medical Group of Phoenix, PC,
Phoenix, Arizona; Associate Director of Perinatal Services, Phoenix Perinatal Associates, an Affiliate of
Obstetrix Medical Group of Phoenix, PC, Phoenix, Arizona and Clinical Professor, University of Arizona
School of Medicine, Tucson, Arizona; and Associate Director of Perinatal Services, Phoenix Perinatal
Associates, an Affiliate of Obstetrix Medical Group of Phoenix, PC, Phoenix, Arizona and Clinical Assistant
Professor, University of Arizona School of Medicine, Tucson, Arizona
Multiple factors account for the increasing number of cesarean delivery wound complications in
the United States; among them are an increase in cesarean delivery and an increase in the
number of overweight and obese patients. This article reviews the pathophysiology of acute
wound healing. Risk factors for cesarean delivery wound complications are identified and
described. Clinical practices that can reduce the risk of developing wound complications,
including Centers for Disease Control and Prevention guidelines, are considered. Treatment
guidelines to accelerate wound healing such as secondary closure and negative pressure
wound therapy in disrupted wounds are proposed. Older guidelines for management of wounds
using secondary intention are critiqued. Historical methods of wound care such as the practice
of using certain cleansers and the practice of wet to dry dressings are outdated. Modern wound
healing products are described.
Target Audience: Obstetricians & Gynecologists, Family Physicians
Learning Objectives: After completion of this article, the reader should be able to describe the effects
of obesity on cesarean delivery wound healing, to improve methods of wound healing in the obese patient,
and to explain why wet to dry dressing changes are not effective wound management.
Wound complications from cesarean delivery are a
significant emotional and economic burden in obstetric
care. The postpartum period is a challenging time for
women, as a result of stressors such as fluctuations in
hormone levels, caring for a newborn baby, and recovery from the actual delivery process. A postoperative
wound complication further intensifies an already difThe authors have disclosed that they have no financial relationships with or interests in any commercial companies pertaining to
this educational activity.
Wolters Kluwer Health has identified and resolved all faculty
conflicts of interest regarding this educational activity.
Reprint requests to: Garrett K. Lam, MD, Phoenix Perinatal
Associates, an affiliate of Obstetric Medical Group of Phoenix, PC,
1331 N. 7th Street, Suite 275, Phoenix, AZ 85006. E-mail:
Garrett_Lam@obstetrix.com.
ficult period of adjustment. The economic burden is
difficult to quantify but is likely significant.
A recent review of obstetric practice in the
United States revealed that cesarean delivery accounted for 26.1% of all births in 2002 (1). Concurrently, the number of overweight and obese
patients (an independent risk factor for wound
complications (2)) is increasing rapidly. The National Health and Nutrition Examination Survey
calculate that, as of 2000, 64% of American adults
were either overweight or obese (3). These factors
can potentially lead to an increase in cesarean
delivery wound complications. This article identifies clinical practices that may reduce the risk of
cesarean delivery wound complications and pro-
462
Management of Wound Complications From Cesarean Delivery Y CME Review Article
poses treatment guidelines that may help accelerate wound healing in disrupted wounds.
BACKGROUND
Wound complications include wound separation
without infection, superficial wound infection, deep
wound infection, wound dehiscence, and rarely, necrotizing fasciitis (see Appendix 1 for Centers for
Disease Control and Prevention [CDC] definitions of
wound infection). The incidence of wound complications in the obstetric population varies in the literature, with rates ranging from 2.8% to 26.6% (2,4
14). Although wound disruptions are frequently
preceded by infection, Martens et al (8) found a
wound disruption rate of 1.7% without infection.
Fascial dehiscence occurs in 0.3% of all cesarean
deliveries. The incidence of necrotizing fasciitis is
slightly less, with one review establishing a rate of
1.8 women per 1000 cesarean deliveries (5).
PATHOGENS
Microorganisms originating from the patient
and/or the patients immediate environment are the
primary sources for postpartum wound infections.
The genital tract and skin are the most influential
reservoirs for bacterial contamination. In a study by
Martens et al (8), the most prevalent pathogens cultured from infected cesarean wounds are Staphylococcus epidermidis, Staphylococcus aureus, Escherichia coli, and Proteus mirabilis. In another study of
wound microbiology, Roberts et al (14) identified the
most prominent pathogens as cervicovaginal flora
such as Ureaplasma species and Mycoplasma species.
WOUND HEALING PHYSIOLOGY
Wound healing occurs as a complex interplay of
multiple biologic and cellular processes, which are
codependent. A review of these complexities will aid
in understanding how wound healing is disrupted and
thus, how best to support the physiology of healing.
Full-thickness wound healing is carried out in three
phases (Fig. 1): inflammation, proliferation, and remodeling. The inflammatory phase occurs in response to the initial injury and is manifested by the
signs and symptoms of erythema, edema, warmth,
and drainage. The purpose of this phase is to control
bleeding and establish a clean wound bed. Hemostasis is initiated by activating the intrinsic and extrinsic
coagulation pathways and platelet aggregation. After
463
hemostasis is established, the platelets break down,
releasing cytokines and growth factors such as platelet-derived growth factors, transforming growth factors B1 and B2, platelet-derived epidermal growth
factor, platelet-activating factor, insulin-like growth
factor-1, fibronectin, and serotonin. These cytokines
and growth factors then attract inflammatory cells
such as neutrophils and monocytes to the wound site,
which prevent infection by phagocytizing microorganisms. These white blood cells also release growth
factors such as fibroblast growth factor, epidermal
growth factor, vascular endothelial growth factor,
tumor necrosis factor, interleukin-1, and interferongamma, which trigger the activation of fibroblasts
and keratinocytes to aid in healing. In a clean wound,
the inflammatory phase lasts approximately 3 days.
Many factors, however, can disrupt this cascade of
cellular events, including infection, diabetes, hypertension, and immunosuppression, thus causing a delay in wound healing.
The proliferative phase occurs next and consists of
3 components: angiogenesis, collagen synthesis, and
epithelialization. The purpose of angiogenesis is to
create new vasculature to supply blood to the damaged area to aid healing. Collagen synthesis fills the
open wound with new connective tissue, depositing a
matrix material to serve as the basis for wound closure and scar formation. These processes occur simultaneously and are codependent.
When wounds heal by primary intention, like in
sutured incisions, the rate of collagen formation
reaches a peak around the fifth postoperative day. It
is possible to feel a ridge under the suture line, called
the healing ridge, which is produced by the newly
formed collagen. If this ridge is not palpable, impaired healing is likely, therefore placing the wound
at risk for disruption (15).
The amount of collagen necessary to fill the wound
is related to the volume of the defect to be filled.
Wounds that are closed by approximating the incision with suture only need a small amount of collagen. Wounds healed by secondary intention need
greater amounts of collagen and require a prolonged
proliferative phase. Collagen production continues
for weeks or months and is dependent on specific
oxygen and nutritional requirements. If the hosts
nutritional or vascular status is compromised, wound
healing is delayed. This aspect of healing is addressed in another section of this article.
Initially, the bed of a healing wound is filled with
red, vascular granulation tissue. Over time, the healing wound experiences a contraction of the wound
bed with the opposing edges slowly pulling together.
464
Obstetrical and Gynecological Survey
Fig. 1. Normal healing response in full-thickness wounds.
There are several theories as to how this is mediated.
One theory proposes that wound contraction is triggered by myofibroblasts (modified fibroblasts) that
release factors that cause contraction of the skin and
tissue around the defect. Another theory suggests that
fibroblast cells are actually moving among the collagen matrix, causing a reorganization of the matrix,
producing the wound bed contraction (16).
Epithelialization is the third component in the proliferative phase. Epithelial cells migrate, proliferate,
and differentiate to resurface the wound defect, and
can only work over a moist, vascular wound surface.
This fact was addressed in the work of Winter (17)
and then Hinman (18), forming the basis for the
concept of moist wound healing. Dry or necrotic
wound surfaces thus impede epithelialization. In sutured wounds, epithelialization occurs concurrently
with collagen synthesis, whereas in open wounds,
epithelialization takes place after granulation tissue is
formed.
The final phase of wound healing is remodeling,
which can continue for over 1 year. In this phase, the
entire scar is reinforced through a process of collagen
maturation. Collagen fibers in nonwounded skin
have a basketweave pattern. In wounded and scarred
tissue, the collagen produced is biochemically distinct from that in nonwounded tissue and is laid down
in a pattern parallel to the skin. The repaired scar
requires time to strengthen. Studies have shown that
after 1 week, the strength of the scar is only 3% of
normal skin, after 3 weeks the strength is 20%, and
after 3 months 80%. Thus, scar tissue is never as
strong as nonwounded tissue (16).
RISK FACTORS FOR POSTCESAREAN
WOUND COMPLICATIONS
Wound healing is distinctly shorter, more efficient,
and organized when done through the process of
primary intention. Infection, inhospitable character-
Management of Wound Complications From Cesarean Delivery Y CME Review Article
istics of the host (such as vascular or chronic disease), suboptimal perioperative conditions (hypothermia), and surgical technique that traumatizes
tissue can all impede the normal phases of wound
repair (19,20). Risk factors for postcesarean wound
complication will also impede wound healing. These
factors are described subsequently, and are summarized
with recommendations for prevention in Table 1.
Obesity
Obesity is a major risk factor for postcesarean
wound complications (7). The etiology of wound
complications in obese women is probably related to
the poor vascularity of subcutaneous fat, serous fluid
collection, and hematoma formation. The obese gravida is prone to more frequent wound complications
even with the use of prophylactic antibiotics (2).
Cetin and Cetin (10) found that the wound disruption
rate increased significantly with thickened subcutaneous tissue. Women with subcutaneous tissue
greater than 2 cm had a wound disruption rate of
27.2% compared with 18.7% of controls. Studies
have shown that using a subcutaneous suture in all
patients with greater than 2-cm subcutaneous depth
significantly reduces the risk of wound disruption
(4,5,10,2123). Specifically, closure of excess subcutaneous tissue eliminates dead space, thus reducing
the formation of seromas.
Diabetes
Impaired wound healing is frequently seen in patients with diabetes. Cruse and Foord (24) reviewed
infection rates in 23,649 patients and found that
465
diabetics had 5 times the risk of infection of nondiabetics, even with clean incisions. Although increased
levels of HgA1c were not shown to be positively
correlated to surgical site infections in a study (25),
diabetes and postoperative hyperglycemia were independent risk factors for a surgical site infection.
Another study, by Zerr et al (26), compared infection
rates before and after implementation of stricter
blood glucose goals and found that the rate of infection before implementation was 2.4% and after implementation, the rate was 1.5%. Zerr demonstrated
that glucose levels above 200 mg/dL in the immediate postoperative period were associated with an
increased surgical site infection rate. Additionally,
blood glucose levels above 200 mg/dL at 48 hours
postsurgery were significantly associated with deep
wound infection.
The explanation for the difference in diabetic wound
healing is complex. The disparity starts with alterations
in the inflammatory response generated by injury or
incision. These differences in enzyme secretion and
growth factor affect all the aspects of normal wound
healing such as collagen synthesis and deposition, leukocyte function, and tissue perfusion. Although a growing body of research in experimental models of diabetes
exists to investigate the use of vitamin A, exogenous
growth factors, and nitric oxide supplementation to
increase wound repair in diabetic patients, there are no
specific recommendations other than meticulous avoidance of hyperglycemia and strict regulation of insulin to
assist in wound healing. Specific blood glucose target
levels have not been identified, although as previously
mentioned in the Zerr study, blood glucose over 200
mg/dL were shown to increase surgical site infections.
TABLE 1
Risk factors for cesarean section wound complication practice recommendations to reduce risk
Risk factor
Obesity
Diabetes
Intrapartum chorioamnionitis
Postoperative endometritis
Prolonged rupture of membranes
Severe anemia
Stressphysiological or psychologic
Smoking
Anticoagulation therapy
Perioperative hypothermia
Severe hypertension
Inadequate nutrition
Practice recommendations
Subcutaneous suture
Stringent glucose control, insulin therapy
Decrease number of vaginal examinations
Judicious use of internal fetal monitoring
Prophylactic antibiotics at cord clamping
Prophylactic antibiotics
Correct anemia
Appropriate pain control/stress reduction
Smoking cessation or nicotine patch
Consider placement of closed drain system to avoid hematoma or seroma
formation
Maintenance of normal body temperature in operating room and recovery
room (use electric warming blanket)
Correct hypertension
Adequate protein, vitamin A, C, and zinc
466
Obstetrical and Gynecological Survey
Chorioamnionitis
Tissue infection and clinical circumstances that
predispose to infection comprise the other major
reasons for suboptimal wound healing. Specifically,
long labors, prolonged rupture of membranes, and
frequent vaginal examinations are all known risk
factors for increasing the rate of infection. Indeed,
the intrauterine environment during labor can tremendously impact postpartum healing. Tran et al (9)
showed that chorioamnionitis increases the risk for
wound infection by a factor of 10.
Corticosteroids
Patients on chronic corticosteroid therapy are especially at risk for poor wound healing. Corticosteroids increase the risk of infection by suppressing
inflammation, inhibiting leukocyte function, retarding wound contraction, decreasing collagen matrix
deposition, and delaying epithelialization. Several
studies support the assertion that vitamin A can counteract some of the effects of corticosteroids (27,28).
Specifically, vitamin A restores the inflammatory
response, promotes epithelialization and the synthesis of collagen, further promoting wound healing and
remodeling (27). Interestingly, vitamin A does not
restore the process of contraction in a healing wound.
The recommended dose of vitamin A has not been
specifically researched, although current recommendations for supplementation for those patients on
steroids are 10,000 to 15,000 IU per day orally (29).
Vitamin A may also be administered topically so as
not to reverse the systemic therapeutic effects of
steroids (28). According to Drugs in Pregnancy and
Lactation (30), it is estimated that topically applied
retinoic acid is not detected in breast milk in clinically significant amounts. Furthermore, vitamin A
naturally occurs in breast milk. The recommended
daily allowance (RDA) for oral intake of vitamin A
during lactation is 4000 IU; adverse affects to the
nursing infant are unknown.
Stress
Stress, both physiological and psychologic, has a
deleterious impact on wound healing. In a study by
Kiecolt-Glaser et al (31), wound healing was significantly longer in women who were caregivers for
relatives with dementia than controls. Broadbent et al
(32) studied wound fluid for levels of interleukin-1,
interleukin-6 and matrix metalloproteinase-9, cytokines, and enzymes that are required to attract phago-
cytes and regulate collagen matrix production for
wound healing. Patients reporting higher stress had
significantly lower levels of interleukin-1, interleukin-6, and matrix metalloproteinase-9. Stress also
causes endogenous hypercortisolemia from the sympathetic stimulation of adrenal glands to release their
glucocorticoid steroid reserves, which blunts the inflammatory phase of wound healing. There is some
evidence that psychoeducational therapy, stress reduction techniques, hypnosis, music therapy, and
acupuncture could reduce stress and reduce the risk
of wound complications (3335).
In animal and human models, postoperative pain
has been shown to have a negative influence on
immune function and wound healing (36); however,
the impact on wound healing using postoperative
pain relief in humans is mixed. The stress response
produced by surgery includes changes in the pituitary
and adrenal systems as well as metabolic changes,
which suppresses the immune system (37). It is interesting to note that regional anesthesia (rather than
general anesthesia) has the most support in the literature to decrease the stress response from surgical
procedures. Specifically, in a study by Koltun (38),
there was a significantly larger level of cortisol measured in the urine for 24 hours postoperatively in
patients who had received general anesthesia over
that of patients who received epidural anesthesia.
Another finding showed natural killer cell cytotoxicity to be significantly depressed in the general anesthesia group over the epidural anesthesia group. Epidural anesthesia may block the afferent pain stimuli
suppressing the stress response, whereas general anesthesia may not.
Nutrition
Nutrition and nutritional supplementation to improve wound healing has been written about extensively, especially in the area of chronic wounds.
Many recommendations have been made particularly
with regard to vitamin C, A, and zinc. The problem
is that few human studies are available that identify
optimal levels of nutrients for wound healing and
whether nutritional supplementation has any impact
at all on the rate of healing. Adequate nutrition does
seem essential to proper wound healing (39,40). This
fact is frequently overlooked but should be a priority
of postoperative management. Protein requirements
during pregnancy are approximately 60 to 80 grams
per day (41). Lactation increases those requirements
by 5 grams per day. Surgical procedures increase
protein requirements above these levels, yet also
Management of Wound Complications From Cesarean Delivery Y CME Review Article
cause ileus, which further worsens a patients nutritional status (15). Protein deficit has been directly
correlated with wound dehiscence (39). Serum prealbumin can be used as a guide to nutritional status.
It has a half-life of 2 days and can therefore be used
as a short-term guide to protein levels (normal values
1938 mg/dL, severe protein depletion 05 mg/dL,
moderate protein depletion 510 mg/dL, mild protein
depletion 1015 mg/dL) (42). Although serum prealbumin levels are routinely ascertained in the elderly
at risk for malnutrition, it may be an area for future
study in the obstetric population. For patients who
have been kept nothing by mouth during a protracted
course of labor, it may be useful to determine protein
status and if found deficient, treat with high protein
supplement postoperatively. Clear liquid protein supplements are now available for those patients who
require clear liquids.
Vitamin supplementation is another consideration
for those patients who are at risk for a wound complication. Vitamin C is necessary for collagen synthesis, capillary wall integrity, fibroblast function,
and immunologic function. Vitamin C deficiency can
delay wound healing, although there is no strong
evidence for supplementation in patients who do not
have scurvy. The RDA for vitamin C during pregnancy and lactation is 70 and 90 mg, respectively.
Supplemental doses of 1000 to 2000 mg per day are
suggested in the chronic wound literature (43).
Zinc supplementation for accelerating healing
wounds has been studied with conflicting results
(44). Low serum zinc levels have been associated
with impaired healing. Zinc aids collagen formation
and supports immune function. The RDA in preg-
467
nancy and lactation for zinc is 15 and 19 mg per day,
respectively. There are no evidenced-based recommendations at this time for zinc supplementation.
Vitamin A is also frequently cited as necessary for
wound healing. Vitamin A is necessary for a normal
inflammatory response, increasing the number of
monocytes and macrophages as well as stabilizing
the intracellular lysosomes of the white blood cells
(29). Vitamin A has also been shown to accelerate
collagen production in animals (40). Doses and lactation implications have been discussed previously.
Hypothermia
It has been hypothesized that mild perioperative
hypothermia (defined as 2C below the normal core
body temperature of 36.5C) can promote postoperative wound infection by causing vasoconstriction
and impaired immune function. There is some controversy in the literature as to the validity of this
theory (19,45,46). Recent research, on balance, does
show a relationship between mild perioperative hypothermia and wound infection. Although an evidenced-based recommendation cannot be made at
this time, active perioperative warming with a forced
air blanket seems theoretically warranted.
PREVENTION OF WOUND
COMPLICATIONS
The first step in prevention of wound infection
starts with the preparation of the operative site. Table
2 presents the guidelines (modified from those proposed by the CDC) for prevention of wound infection. Important to these suggestions is the fact that
TABLE 2
Prevention of surgical site infections
When
Guideline
24 h preprocedure
Immediately before operation
In the operating room
Shower 2 within 24 h using chlorhexidine
If hair removal necessary, use clippers
Prepare patient skin using:
Alcohol (most rapid action, best against Gram-positive and Gram-negative bacteria) or,
Iodine/iodophors (intermediate rapidity of action, best against Gram-positive bacteria)
Antimicrobial prophylaxis
Asepsis and surgical technique:
Hemostasis
Gentle handling of tissues
Remove devitalized tissues
Eradicate dead space
Monofilament sutures
Closed suction drains removed no longer than 24 h after procedure
Maintain normothermia
Incision care
Cover with sterile dressing for 24 to 48 h
Postoperative
Modified from the 1999 Centers for Disease Control and Prevention guidelines for prevention of surgical site infection (65).
468
Obstetrical and Gynecological Survey
use of antibacterial wash needs to start before surgical preparation of the patient in the operating room.
In fact, Hayek (47) showed a reduction in postoperative infection rates when patients showered twice in
24 hours before surgery with chlorhexidine wash.
The rate of Staphylococcus aureus-infected wounds
(attributable to skin contamination) dropped by 50%
in the chlorhexidine group compared with the bar
soap group. Other studies have shown a decrease in
skin colonization after showering with chlorhexidine
(48). Additionally, the manner in which the skin is
prepared is also important. Specifically, avoidance of
shaving the skin is emphasized, because the use of a
razor increases the risk of skin breakage, which can
allow pathogens direct access to the bloodstream.
Fig. 2. Secondary closure technique.
WOUND MANAGEMENT
Despite prophylactic measures and good surgical
technique, a small percentage of patients will still
experience wound complications. Wound management should consider strategies that expedite healing,
minimize complications and cost. Furthermore, principles of wound management should provide treatment to decrease cofactors that impede healing. Hematomas and seromas are commonly observed
problems after a cesarean delivery. These types of
situations require manual opening of the wounds to
allow drainage. After infection has been treated and
all of the hematoma/seroma evacuated, an open
wound can be managed in 3 ways: secondary closure,
secondary intention with dressings, and secondary
intention using negative pressure wound therapy.
intention required a mean of 71 days of wound care
to heal. In a study by Dodson et al (50), patients who
were treated with secondary closure required a mean
of 17 days to heal, whereas those patients who were
allowed to heal by secondary intention took 61 days
to complete wound healing. The results of these
studies are striking. Wounds healed on average 7
weeks sooner in the secondary closure group.
Healing by Secondary Intention Using Dressings
Healing through secondary intention has historically been the most common way to manage wound
disruption. The rise in the incidence of chronic
wounds has encouraged the development of new
wound care strategies and products to improve on the
old wet to dry dressings.
Secondary Closure
Secondary closure can be performed once a wound
is free of infection or necrotic tissue and has started
to granulate. This procedure, which may be performed at the bedside using local anesthesia and/or
sedation, is done within 1 to 4 days after disruption
or evacuation of hematoma or seroma. A wound
cleanser is first needed to prep the area, and then a
polypropylene mattress suture is used to close the
skin and subcutaneous tissue en bloc. An illustration
of secondary closure technique is shown in Figure 2.
The suture may be removed 7 days after reclosure.
The practice of using secondary closure to repair
superficial wound dehiscence is supported by several
studies. Walters et al (49) found secondary closure to
be successful in 85% of cases. The mean time to
complete healing was 15.8 days in successful cases.
Those patients randomized to healing by secondary
MISCONCEPTIONS OF WOUND HEALING
It is important to describe several historical tenets
of wound care that are outdated before proceeding in
a discussion of healing by secondary intention. Many
studies have documented that the use of products
such as povidone iodine (51), Daikens solution (52)
iodophor gauze, and hydrogen peroxide (53) are cytotoxic to white blood cells and other vital wound
healing components. The use of these products can
delay wound healing. Irrigation with normal saline or
commercial wound-cleansing solutions, which do not
contain any of the aforementioned components, will
adequately remove surface bacteria without disrupting the beneficial physiological process.
Another myth is that moist wounds are more prone to
delayed healing because they are more likely to become
infected or break down and that keeping a wound dry
Management of Wound Complications From Cesarean Delivery Y CME Review Article
promotes healing. Research, in the early 1960s (17,18),
proved that in fact, wounds that are kept moist at all
times are significantly quicker to heal than dry wounds.
Moist wounds promote autolytic debridement, support
epithelial cell migration, and make dressing removal
easier, causing less trauma to viable tissue (54). In wet
to dry dressings, saline-soaked gauze is allowed to dry
and then removed. This causes new tissue, which had
adhered to the gauze, to be pulled away, consequently
destroying healthy tissue. This technique is more appropriate for necrotic tissue debridement, and its validity is debated by wound care experts who state that it
should be used on very necrotic tissue and stopped
when there is viable tissue (55).
MODERN WOUND CARE
Historically, dressing changes have been described
as frequently as 4 times daily. Frequent dressing
changes will slow wound healing by reducing wound
temperature, disrupting cellular function and chemical reactions necessary for tissue repair. A study by
Thomas (56) has shown that it takes a wound 40
minutes after dressing change to return to optimal
temperature. Additionally, mitosis and leukocyte activities can be slowed for up to 3 hours after wound
cleansing. Temperature in humans must be kept between 97.5o to 99oF (36.4o to 37.2oC) for cellular
processes to be optimal. Understanding wound heal-
469
ing physiology and wound products allows wound
care to be chosen appropriately for each wound.
Dressing changes can then be reduced to once daily
or even every other day, which enables the wound to
maintain a physiological environment.
Modern wound care dressing selection considers factors such as the phase of healing, the volume of exudate,
and the presence of necrotic tissue to determine the type
of dressing that will be most supportive of wound
healing. Dressing selection should optimize the wound
bed by decreasing the risk of infection, removing necrotic tissue, managing exudate, eliminating dead
space, and maintaining wound temperature.
The risk of infection can be reduced by using a
nontoxic solution to cleanse the wound. Necrotic
tissue can be removed by sharp debridement or daily
applications of enzymatic debriders that act on necrotic tissue but have no effect on healthy tissue.
Drainage can be managed by using highly absorbent
dressing material. Calcium alginate and foam are
examples of 2 newer materials used in wound care
that are highly absorbent and have been shown to be
less painful during dressing changes than gauze. According to the Cochrane Database (57), existing research is inadequate to show whether foam or calcium alginate accelerates wound healing time.
Wound care products are described in Table 3. A
source guide is provided in Table 4.
TABLE 3
Wound care product descriptions
Product
Antifungal cream
Calcium alginate
Enzymatic dbrider
Film
Foam
Gauze
Hydrogel
Silver nitrate
Description
Topical cream used as treatment for superficial fungal infections of the periwound skin; contains 2%
miconazole nitrate
Spun fibers derived from brown seaweed composed of calcium salts of alginic acid; calcium alginate is a
solid that exchanges calcium ions for sodium ions when it contacts any substance containing sodium
such as wound fluid; the resulting sodium alginate is a gel; nonadhesive, nonocclusive, conformable to wound bed; indicated for moderately or highly draining wounds; not indicated for deep
tunnels as a result of difficulty in retrieval; do not moisten before use; needs cover dressing
Topical solution that breaks down necrotic tissue by directly digesting the components of slough or
by dissolving the collagen that holds the necrotic tissue to the underlying wound bed; applied 1 to
3 times daily with dressing changes; little data is available to help guide product selection
Thin, transparent polyurethane sheets coated on one side with acrylic, hypoallergenic adhesive; the
adhesive will not stick to moist surfaces; impermeable to fluids and bacteria but semipermeable to
oxygen and water vapor; indicated in superficial wounds with little or no exudate
Polyurethane sheets containing open cells capable of holding fluids and pulling them away from the
wound bed; foams provide absorbency while keeping the wound moist; manufacturers vary in the
formulation; some include wound cleansers, moisturizers, and absorbing agents; indicated in
moderately or highly draining wounds; may be cut to conform to wound beds; not indicated for
narrow tunnels
Woven or nonwoven cotton or synthetic blends; nonimpregnated or impregnated with normal saline
or other substances
Formulated in sheets or gels; glycerin, saline, or water-based to hydrate the wound; indicated in dry
or minimally draining wounds; not intended to fill wound spaces
Used to treat overgrown granulation tissue; apply stick to hypergranulation tissue
470
Obstetrical and Gynecological Survey
Vacuum-Assisted Closure
Negative pressure wound therapy (NPWT), also
known as vacuum-assisted closure, received U.S.
Food and Drug Administration approval in 1995. It
uses controlled levels of negative pressure to assist
and accelerate wound healing by evacuating localized edema with negative pressure. Bacterial colonization is reduced along with the evacuation of wound
drainage (58). Intermittent negative pressure causes
in periodic release of cytokines and inflammatory
factors important to the previously mentioned phases
of wound healing (59). Negative pressure also increases localized blood flow and oxygenation,
thereby promoting a nutrient-rich environment that
stimulates granulation tissue growth (60). Such cellular proliferation encourages angioneogenesis, uniform wound size reduction, and reepithelialization
(58). This therapy has been used in chronic wounds
such as diabetic foot ulcers (61). NPWT accelerated
wound closure significantly over traditional gauze
dressings in a study by Eginton et al (62). Recent
research in gynecologic oncology has looked at
NPWT as a reliable and safe method to treat wound
failures (63,64). The results thus far have been encouraging.
The dressing used for negative pressure wound
therapy is polyurethane foam that is trimmed to fit
the entire surface of the wound. Once the foam is
placed, evacuation tubing is laid on top of the
foam. A clear, adhesive dressing is placed over the
foam and tubing to secure the unit to the wound
site. The evacuation tubing has slits cut into the
proximal end, which will evacuate the wound fluid
into a collection chamber located on the computerized vacuum pump. The collection canister
can be emptied as needed. Controlled negative
pressure is then applied by the vacuum-assisted
closure device, which is a small computerized
pump (4 inches by 2 inches, weighing 2 pounds)
with a rechargeable battery. The tubing can be
clamped and disconnected for short periods of time
(no more than 2 hours at a time for a maximum of
6 hours per day). Dressing changes are needed
every 48 hours. Indications, contraindications, and
precautions are noted in Figure 3. Illustrations of
the NPWT dressing and the wound vacuum are
seen in Figures 4 and 5.
Although negative pressure wound therapy is
considerably more costly (approximately $100 per
day) than gauze dressings, the time to complete
healing is significantly reduced (62). Home health
nursing visits can be reduced to 3 times weekly
instead of everyday for gauze-dressing changes.
Our practice has seen significantly improved healing for patients who have used the wound vacuum,
particularly in obese patients. Closure of wound
dehiscence by secondary intention in such women
can take months. Their deep subcutaneous layer
also makes secondary closure technically difficult
to perform. NPWT ensures that the subcutaneous
TABLE 4
Wound care product source sheet
Product
category
3M
Antifungal cream
Film
Tegaderm
Calcium alginate Tegagen HG,
Tegagen HI
Foam
3M Foam
Hydrogel
Soft cloth tape
(hypoallergenic)
Wound cleansers
Tegagel
Midipore
J&J
Molnlycke
Ferris
Coloplast Corp
Care-Tech Labs
Smith & Nephew
Baza cream
Bioclusive, Select
Nu-Derm Alginate
Mefilm
Melgisorb
Sof-Foam
Meplilex
Nu-Gel
Normigel
Mefix
Polymem,
Polywic
Hypafix
Saline spray
Technicare
Comfeel SeaCleans
Clinical Care spray
Enzymatic
dbrider
3M, 3M Center, St. Paul, MN 551441000
Coloplast Corp, Holtedam 1, RK-3050 Humlebaek, Denmark
Johnson & Johnson, One Johnson & Johnson Plaza, New Brunswick, NJ 08933
Care Tech Labs, 3224 S. Kingshighway Blvd, St. Louis, MO 63139
Molnlycke, Gotenborg, Sweden
Smith & Nephew Inc, 11775 Starkey Rd, Largo, FL 337791970
Ferris Mfg Corp, 16W300 83rd St, Burr Ridge, IL 605275848
Collagenase
Management of Wound Complications From Cesarean Delivery Y CME Review Article
471
Fig. 5. Dressing application. A clear adhesive dressing is
placed over the foam to secure the unit to the wound site.
CONCLUSION
Fig. 3. Indications, contraindications, and precautions for negative pressure wound therapy.
Recent developments using evidence-based research can decrease postcesarean morbidity for
women. Modern wound care strategies and products
developed to support wound healing physiology can
minimize healing time if a wound complication occurs. The information provided here can be useful to
improve clinical outcomes in other surgical procedures as well.
APPENDIX 1
Criteria for Defining a Surgical Site Infection
Superficial Incisional Surgical Site Infection
Fig. 4. Negative pressure using a foam dressing and evacuation tubing increases localized blood flow and oxygenation.
wound environment remains free from seroma and
hematoma formation, thus assisting in maintaining
an environment in which healing is optimized.
Infection occurs within 30 days after the operation
and infection involves only skin or subcutaneous
tissue of the incision and at least one of the following
(65):
1. Purulent drainage, with or without laboratory
confirmation, from the superficial incision.
2. Organisms isolated from an aseptically obtained culture of fluid or tissue from the superficial
incision.
3. At least one of the following signs or symptoms
of infection: pain or tenderness, localized swelling,
redness, or heat and superficial incision is deliberately opened by surgeon, unless the incision is
culture-negative.
4. Diagnosis of superficial incisional surgical site
472
Obstetrical and Gynecological Survey
infection (SSI) by the surgeon or attending physician.
Do not report the following conditions as SSI:
l. Stitch abscess (minimal inflammation and discharge confined to the points of suture penetration).
2. Infection of an episiotomy or newborn circumcision site.
3. Infected burn wound.
4. Incisional SSI that extends into the fascial and
muscle layers (see deep incisional SSI).
Note: Specific criteria are used for identifying infected episiotomy and circumcision sites and burn
wounds.
the incision, which was opened or manipulated during an operation and at least one of the following:
1. Purulent drainage from a drain that is placed
through a stab wound into the organ/space.
2. Organisms isolated from an aseptically obtained culture of fluid or tissue in the organ/space.
3. An abscess or other evidence of infection involving the organ/space that is found on direct
examination, during reoperation, or by histopathologic or radiologic examination.
4. Diagnosis of an organ/space SSI by a surgeon
or attending physician.
REFERENCES
Deep Incisional Surgical Site Infection
Infection occurs within 30 days after the operation
if no implant is left in place or within 1 year if
implant is in place and the infection appears to be
related to the operation and infection involves deep
soft tissues (eg, fascial and muscle layers) of the
incision and at least one of the following:
1. Purulent drainage from the deep incision but
not from the organ/space component of the surgical site.
2. A deep incision spontaneously dehisces or is
deliberately opened by a surgeon when the patient
has at least one of the following signs or symptoms: fever (38C), localized pain or tenderness,
unless the site is culture-negative.
3. An abscess or other evidence of infection involving the deep incision is found on direct examination, during reoperation, or by histopathologic
or radiologic examination.
4. Diagnosis of a deep incisional SSI by a surgeon
or attending physician.
Notes
1. Report infection that involves both superficial
and deep incision sites as deep incisional SSI.
2. Report an organ/space SSI that drains through
the incision as a deep incisional SSI.
Organ/Space Surgical Site Infection
Infection occurs within 30 days after the operation
if no implant is left in place or within I year if
implant is in place and the infection appears to be
related to the operation and infection involves any
part of the anatomy (eg, organs or spaces), other than
1. National Center for Health Statistics: Faststats. Births
method of delivery (CDC web site, data for US in 2002).
Available at: http://www.cdc.gov/nchs/fastats/delivery.htm.
2. Myles TD, Gooch J, Santolaya J. Obesity as an independent
risk factor for infectious morbidity in patients who undergo
cesarean delivery. Obstet Gynecol 2002;100:959964.
3. National health and Nutrition Examination Survey. Healthy
weight, overweight, and obesity among US adults. Available
at: http://www.cdc.gov/nchs/about/major/nhanes/Databriefs.
htm. Accessed December 14, 2004.
4. Naumann RW, Hauth JC, Owen J, et al. Subcutaneous tissue
approximation in relation to wound disruption after cesarean
delivery in obese women. Obstet Gynecol 1995;85:412416.
5. Chelmow D, Huang E, Strohbehn K. Closure of the subcutaneous dead space and wound disruption after cesarean delivery. J Matern Fetal Neonatal Med 2002;11:403408.
6. Manann EF, Chauhan SP, Rodts-Palenik S, et al. Subcutaneous stitch closure versus subcutaneous drain to prevent
wound disruption after cesarean delivery: a randomized clinical trial. Am J Obstet Gynecol 2002;186:11191123.
7. Vermillion ST, Lamoutte C, Soper DE, et al. Wound infection
after cesarean: effect of subcutaneous tissue thickness. Obstet Gynecol 2000;95:923926.
8. Martens MG, Kolrud BL, Faro S, et al. Development of wound
infection or separation after cesarean delivery; prospective
evaluation of 2,431 cases. J Reprod Med 1995;40:171175.
9. Tran TS, Jamulitrat S, Chongsuvivatwong V, et al. Risk factors
for post cesarean surgical site infection. Obstet Gynecol 2000;
95:367371.
10. Cetin A, Cetin M. Superficial wound disruption after cesarean
delivery: effect of depth and closure of subcutaneous tissue.
Int J Gynaecol Obstet 1997;57:1721.
11. Killian CA, Graffunder EM, Vinciguerra TJ, et al. Risk Factors
for surgical-site infections following cesarean section. Infect
Control Hosp Epidemiol 2001;22:613617.
12. Pelle H, Jepsen O, Larsen S, et al. Wound infection after
cesarean section. Infect Control 1986;7:456461.
13. Moir-Bussy BR, Hutton RM, Thompson JR. Wound infection
after caesarean section. J Hosp Infect 1984;5:359370.
14. Roberts S, Maccato M, Faro S, et al. The microbiology of
post-cesarean wound morbidity. Obstet Gynecol 1993;81:
383386.
15. Bryant R. Acute surgical and traumatic wound healing. In:
Acute & Chronic Wounds: Nursing Management, 2nd ed. St
Louis: Mosby, 2000:189196.
16. Witte MB, Barbul A. General principles of wound healing. Surg
Clin North Am 1997;77:509528.
17. Winter G. Formation of the scab and the rate of epithelization
of superficial wounds in the skin of the young domestic pig.
Nature 1962;4812:293294.
Management of Wound Complications From Cesarean Delivery Y CME Review Article
18. Hinman CD, Maibach H. Effect of air exposure and occlusion on
experimental human skin wounds. Nature 1963;4904:377378.
19. Kurz A, Sessler D, Lenhardt R. Perioperative normothermia to
reduce the incidence of surgical-wound infection and shorten
hospitalization. N Engl J Med 1996;334:12091216.
20. Owen J, Andrews WW. Wound complications after cesarean
sections. Clin Obstet Gynecol 1994;37:842855.
21. Allaire AD, Fish J, McMahon MJ. Subcutaneous drain vs.
suture in obese women undergoing cesarean delivery. A prospective, randomized trial. J Reprod Med 2000;45:327331.
22. Kore SS, Vyavaharkar MM, Akolekar RR. Comparison of closure of subcutaneous tissue versus non-closure in relation to
wound disruption after abdominal hysterectomy in obese patients. J Postgrad Med 2000;46:2628.
23. Soisson AP, Olt GO, Soper JT. Prevention of superficial
wound separation with subcutaneous retention sutures. Gynecol Oncol 1993;51:330334.
24. Cruse PJE, Foord R. A prospective study of 23,649 surgical
wounds. Arch Surg 1973;107:206210.
25. Latham R, Lancaster AD, Covington JF, et al. The association
of diabetes and glucose control with surgical site infections
among cardiothoracic surgery patients. Infect Control Hosp
Epidemiol 2001;22:607612.
26. Zerr KJ, Furnary AP, Grunkemeier GL, et al. Glucose control
lowers the risk of wound infections in diabetics after open
heart operations. Ann Thorac Surg 1997;63:356361.
27. Anstead GM. Steroids, retinoids, and wound healing. Adv
Wound Care 1988;11:277285.
28. Wicke C, Halliday B, Allen D. Effects of steroids and retinoids
on wound healing. Arch Surg 2000;135:12651270.
29. Scholl D, Lankgamp-Henken B. Nutrient recommendations
for wound healing. J Int Nurs 2001;24:124132.
30. Briggs GG, Freeman R, Yaffe SJ. Drugs in Pregnancy and
Lactation, 6th ed. Philadelphia: Lippincott Williams & Wilkins,
2002:13761379, 14701477.
31. Kiecolt-Glaser JK, Marucha PT, Malarkey WB, et al. Slowing
of wound healing by psychological stress. Lancet 1995;346:
11941196.
32. Broadbent E, Petrie KJ, Alley PG, et al. Psychological stress
impairs early wound repair following surgery. Psychosom Med
2003;65:865869.
33. Andersen BL, Farrar WB, Golden-Kreuts DM, et al. Psychological, behavioral, and immune changes after a psychological
intervention: a clinical trial. J Clin Oncol 2004;22:35703580.
34. Pelletier CL. The effect of music on decreasing arousal due to
stress: a meta-analysis. J Music Ther 2004;41:192214.
35. Urizar GG Jr, Milzzo M, Le HN, et al. Impact of stress reduction instructions on stress and cortisol levels during pregnancy. Biol Psychol 2004;67:275282.
36. Kiecolt-Glaser JK, Page GG, Marucha PT, et al. Psychological influences on surgical recovery. Am Psychol 1998;53:12091218.
37. Kehlet H. Surgical stress: the role of pain and analgesia. Br J
Anaesth 1989;63:189195.
38. Koltun W, Bloomer M, Tilberg A, et al. Awake epidural anesthesia
is associated with improved natural killer cell cytotoxicity and a
reduced stress response. Am J Surg 1996;171:6873.
39. Riou JP, Cohen JR, Johnson H. Factors influencing wound
dehiscence. Am J Surg 1992;163:324.
40. Hunt TK. Vitamin A and wound healing. J Am Acad Dermatol
1986;15:817821.
41. National Research Council. Recommended daily dietary allowance for women before and during pregnancy and lactation. National Research Council, 1989.
42. Fischbach F. Chemistry studies. In: A Manual of Laboratory
and Diagnostic Tests, 7th ed. Philadelphia: Lippincott Williams & Wilkins, 2004:348349.
43. Levenson SM, Demetriou AA. Metabolic factors. In: Cohen IK,
Diegelmann RF, Lindblad WJ, eds. Wound Healing Biochem-
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
473
ical and Clinical Aspects. Philadelphia: WB Saunders Co,
1992:248273.
Lansdown AB. Zinc in the healing wound. Lancet 1996;347:
706707.
Flores-Maldonado A, Medina-Escobedo CE, Rios-Rodriguez
HM. Mild perioperative hypothermia and the risk of wound
infection. Arch Med Res 2001;32:227231.
Munn MB, Rouse DJ, Owen J. Intraoperative hypothermia and
post-cesarean wound infection. Obstet Gynecol 1998;91:
582584.
Hayek LJ, Emerson JM, Gardner AM. A placebo-controlled
trial of the effect of two preoperative baths or showers with
chlorhexidine detergent on postoperative wound infection
rates. J Hosp Infect 1987;10:165172.
Kaiser AB, Kernodle DS, Barg NL, et al. Influence of preoperative
showers on staphylococcal skin colonization: a comparative trial
of antiseptic skin cleansers. Ann Thorac Surg 1988;45:3538.
Walters MD, Dombroski RA, Davidson SA, et al. Reclosure of disrupted abdominal incisions. Obstet Gynecol 1990;76:597602.
Dodson MD, Magann EF, Meeks GR, et al. A randomized
comparison of secondary closure and secondary intention in
patients with superficial wound dehiscence. Obstet Gynecol
1992;80:321324.
Kramer SA. Effect of povidoneiodine on wound healing: a
review. J Vasc Nurs 1999;17:1723.
Bennett LL, Rosenblum RS, Perlov C, et al. An in vivo comparison of topical agents on wound repair. Plast Reconstr
Surg 2001;108:675683.
OToole EA, Goel M, Woodley DT. Hydrogen peroxide inhibits
human keratinocyte migration. Dermatol Surg 1996;22:525529.
Watret L, White R. Surgical wound management: the role of
dressings. Nursing Standard 2001;15:5969.
Bryant R. Skin pathology and types of damage. In: Acute &
Chronic Wounds: Nursing Management, 2nd ed. St Louis:
Mosby, 2000:125156.
Thomas S. Functions of a wound dressing. In: Thomas S, ed.
Wound Management and Dressings. London: Pharmaceutical
Press, 1990.
Vermeulen H, Ubbink D, Goossens A, et al. Dressings and
topical agents for surgical wounds healing by secondary intention. Cochrane Database Syst Rev 2004;3:151.
Morylkas MJ, Argenta LC, Shelton-Brown EL, et al. Vacuumassisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg
1997;38:553562.
Fabian TS, Kaufman HJ, Lett ED, et al. The evaluation of
subatmospheric pressure and hyperbaric oxygen in ischemic
full-thickness wound healing. Am Surg 2000;66:11361143.
Morykwas MF, David LR, Schneider AM, et al. Use of subatmospheric pressure to prevent progression of partial thickness
burns in a swine model. J Burn Care Rehabil 1999;20:1521.
Page JC, Newswander B, Schwenke CD, et al. Retrospective
analysis of negative pressure wound therapy in open foot
wounds with significant soft tissue defects. Adv Skin Wound
Care 2004;17:354364.
Eginton MT, Brown KR, Seabrook GR, et al. A prospective
randomized evaluation of negative pressure wound dressings
for diabetic foot wounds. Ann Vasc Surg 2003;17:645649.
Schimp VL, Worley C, Brunello S, et al. Vacuum-assisted
closure in the treatment of gynecologic oncology wound failures. Gynecol Oncol 2004;92:586591.
Argenta PA, Rahaman J, Gretz HF, et al. Vacuum-assisted
closure in the treatment of complex gynecologic wound failures. Obstet Gynecol 2002;99:497501.
Mangram AJ, Horan TC, Pearson ML, et al. Guideline for
prevention of surgical site infection, 1999. Infect Control Hosp
Epidemiol 1999;20:247280.
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Digital AmputationsDokumen60 halamanDigital AmputationsprogiezBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Fat Embolism SyndromeDokumen6 halamanFat Embolism SyndromeprogiezBelum ada peringkat
- Journal Terapi UTIDokumen6 halamanJournal Terapi UTIprogiezBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Journal Terapi UTIDokumen6 halamanJournal Terapi UTIprogiezBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Jurnal AirwayDokumen2 halamanJurnal AirwayprogiezBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- A Guide To Medicinal Plants in North AfricaDokumen2 halamanA Guide To Medicinal Plants in North Africakenpersky100% (1)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Tugas BioStatistikDokumen3 halamanTugas BioStatistikfrankyBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Obg Unit-1Dokumen28 halamanObg Unit-1madhu.BBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Una CoalesDokumen394 halamanUna Coalesabuzeid5100% (1)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Med Surg Bullets 1Dokumen21 halamanMed Surg Bullets 1Jor GarciaBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Pediatrics Clinics 2006 (Vol 53, No 4, Aug 2006) (Elsevier) WWDokumen249 halamanPediatrics Clinics 2006 (Vol 53, No 4, Aug 2006) (Elsevier) WWGeorgiana Combei Ungureanu100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- 2016 - All Phases TNPG Allotment ListDokumen35 halaman2016 - All Phases TNPG Allotment ListAshok PaskalrajBelum ada peringkat
- DAFTAR PUSTAKA AnestesiDokumen2 halamanDAFTAR PUSTAKA AnestesiauliyaanandaBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Leiomioma - Miomectomia LaparoscopicaDokumen20 halamanLeiomioma - Miomectomia LaparoscopicaNella SolanoBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Local Health Referral System ManualDokumen72 halamanThe Local Health Referral System ManualRuth Hazel Galang100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Books With Download LinksDokumen16 halamanBooks With Download LinksJeffery Samuel73% (11)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Malposition Malpresentation Abnormal LieDokumen41 halamanMalposition Malpresentation Abnormal Lieapi-3705046100% (1)
- RSCM - Profil - UkreineDokumen13 halamanRSCM - Profil - UkreineprimastyoanggataBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Maternal and Child NursingDokumen46 halamanMaternal and Child NursingDarnell Adrian Estobio100% (2)
- DR RajaSabapathy CVDokumen120 halamanDR RajaSabapathy CVWara Samsarga GedeBelum ada peringkat
- SketchyIM Check List PDFDokumen5 halamanSketchyIM Check List PDFhectorBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Maternal Child NursingDokumen14 halamanMaternal Child NursingTina TalmadgeBelum ada peringkat
- Perceived Competence in Cardiopulmonary Resuscitation, Knowledge and Skills, Amongst 50 Qualified NursesDokumen6 halamanPerceived Competence in Cardiopulmonary Resuscitation, Knowledge and Skills, Amongst 50 Qualified NursesYannis ZoldenbergBelum ada peringkat
- NOTICE (Revised Syllabi) : (WRITTEN TEST & SYLLABI For The Posts - Advt. No. 01, 02 and 03 of 2016)Dokumen123 halamanNOTICE (Revised Syllabi) : (WRITTEN TEST & SYLLABI For The Posts - Advt. No. 01, 02 and 03 of 2016)wani ashBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Generic Name TizanidineDokumen3 halamanGeneric Name TizanidinemadamcloudnineBelum ada peringkat
- Dr. Muh. Ardi MunirDokumen6 halamanDr. Muh. Ardi MunirRahmanBelum ada peringkat
- Application For Registration Licence Renewal of Registration and Licence Under Sections 7 and 8 of The Sikkim Clinical Establishments Act. 1995Dokumen2 halamanApplication For Registration Licence Renewal of Registration and Licence Under Sections 7 and 8 of The Sikkim Clinical Establishments Act. 1995kabuldasBelum ada peringkat
- Brody 2006 Prolactin BPDokumen4 halamanBrody 2006 Prolactin BPBassu RazvanBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- 1 - Introduction of CytopathologyDokumen41 halaman1 - Introduction of CytopathologyAyu Rizky Fitriawan AyuBelum ada peringkat
- Pregnancy and Yoga PDFDokumen9 halamanPregnancy and Yoga PDFSpurthi MagdumBelum ada peringkat
- Anticoagulant Therapy For Deep Vein Thrombosis (DVT-2Dokumen7 halamanAnticoagulant Therapy For Deep Vein Thrombosis (DVT-2Rahma AnwarBelum ada peringkat
- Clubfoot - Ponseti Management. Editor Lynn Stahelli (2003)Dokumen32 halamanClubfoot - Ponseti Management. Editor Lynn Stahelli (2003)amalia_utami_1Belum ada peringkat
- Understanding Corrected AgeDokumen2 halamanUnderstanding Corrected Ages_ton77Belum ada peringkat
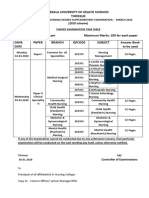
- Kerala University of Health Sciences Thrissur: (2010 Scheme)Dokumen1 halamanKerala University of Health Sciences Thrissur: (2010 Scheme)subiBelum ada peringkat
- Semi-Rigid Ureteroscopy: Indications, Tips, and Tricks: Lily A. Whitehurst Bhaskar K. SomaniDokumen7 halamanSemi-Rigid Ureteroscopy: Indications, Tips, and Tricks: Lily A. Whitehurst Bhaskar K. SomaniUmar FarooqBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)