CKD Guidelines 2005
Diunggah oleh
Stefania WidyaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
CKD Guidelines 2005
Diunggah oleh
Stefania WidyaHak Cipta:
Format Tersedia
Evidence Based Practice Guidelines for Nutritional
Management of Chronic Kidney Disease
Developed by the Australia and New Zealand Renal Guidelines Taskforce
(ANZRGT)
Revised May, 2005
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Table of Contents
INTRODUCTION
AIM
GUIDELINE DEVELOPMENT PROCESS
CONSULTATION PROCESS
USE OF GUIDELINES
REVIEW PROCESS
TASK FORCE MEMBERS
3
3
3
4
4
5
EVIDENCE BASED PRACTICE GUIDELINE FRAMEWORK
CHRONIC KIDNEY DISEASE STAGE 3 (GFR 30-59)
1
2
3
SCOPE
EVIDENCE BASED RECOMMENDATIONS
SUMMARY OF RECOMMENDATIONS
7
7
10
CHRONIC KIDNEY DISEASE STAGE 4 (GFR 15- 29)
11
1
2
3
11
11
14
SCOPE
EVIDENCE BASED RECOMMENDATIONS
SUMMARY OF RECOMMENDATIONS
CHRONIC KIDNEY DISEASE STAGE 5 - HAEMODIALYSIS
15
1
2
3
15
15
17
SCOPE
EVIDENCE BASED RECOMMENDATIONS
SUMMARY OF RECOMMENDATIONS
CHRONIC KIDNEY DISEASE STAGE 5 - PERITONEAL DIALYSIS
18
1
2
3
18
18
21
SCOPE
EVIDENCE BASED RECOMMENDATIONS
SUMMARY OF RECOMMENDATIONS
REFERENCES
22
APPENDIX 1: SUMMARY OF RECOMMENDATIONS FOR MANAGEMENT OF CHRONIC KIDNEY DISEASE 23
APPENDIX 2: SUMMARY OF RECOMMENDATIONS FOR NUTRITION PRESCRIPTION IN CHRONIC KIDNEY
DISEASE
24
APPENDIX 3: DESCRIPTIONS OF LEVELS OF EVIDENCE CITED FROM ORIGINAL SOURCES
25
APPENDIX 4: STAGES OF CHRONIC KIDNEY DISEASE
25
APPENDIX 5: CALCULATIONS
26
APPENDIX 6: BMI RANGES
28
APPENDIX 7: MALNUTRITION SCREENING TOOL
29
APPENDIX 8: SUBJECTIVE GLOBAL ASSESSMENT
30
APPENDIX 9: GLOSSARY
32
Australia & New Zealand Renal Guidelines Taskforce
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Introduction
Aim
A working party of Dietitians from Australia and New Zealand has developed evidence based practice guidelines for the
dietetic management of chronic kidney disease. The purpose of these guidelines is to provide dietitians in Australia and
New Zealand with a user-friendly summary of evidence based clinical guidelines related to the dietetic management of
adult patients with chronic kidney disease.
Guideline Development Process
The evidence based practice guidelines for the dietetic management of chronic kidney disease were developed by
summarising the nutrition components of the following published guidelines:
Caring for Australians with Renal Impairment (CARI) Guidelines
Kidney Disease Outcomes Quality Initiative (K/DOQI) Clinical Practice Guidelines
American Dietetic Association (ADA) Medical Nutrition Therapy Evidence-Based Guides for Practice:
Chronic Kidney Disease (non-dialysis) Medical Nutrition Therapy Protocol
ADA Guidelines for Nutritional Care of Renal Patients (3rd ed)
European Dialysis and Transplant Nurses Association and European Renal Care Association (EDTNA/ERCA)
Guidelines for the Nutritional Care of Adult Renal Patients.
Levels of evidence or opinion have been cited from the above documents and referenced in each guideline. Descriptions
of the levels of evidence are listed in Appendix 3. The relevant guidelines and articles were identified by Medline
database and Internet key word searches between April 2002 and October 2003.
Where conflicting guidelines answering the same clinical question existed, the guideline with the strongest level of
evidence was included. When conflicting supporting evidence was equal in quality and depth, CARI guidelines were
selected preferentially as more relevant to the local environment. If similar information was proposed from more than
one set of guidelines, all sources were acknowledged. Aspects of nutritional management not included in any of the
guidelines were omitted, however some aspects deemed important by the taskforce have been included as practice tips.
Due to the difficulties associated with research into nutritional management of kidney disease, an evidence-based
approach could not be adopted for all aspects. For published guidelines based on opinion or agreed best practice without
supporting research, recommendations have still been included to complete the document but are acknowledged as
being open for wider variance in practice. In particular, adherence to process type guidelines may be strictly resource
dependant.
The selected guidelines were reformatted into the following components: definition of disease, diagnostic criteria,
clinical questions to be addressed, referral criteria, nutrition assessment, nutrition prescription and outcome measures, in
line with established nutritional management process. Dietetic management of acute renal failure, transplantation,
nephrotic syndrome or kidney disease in paediatrics is not included.
These guidelines include information taken from existing sets of guidelines based on scientific evidence, and where no
evidence exists, published guidelines stating consensus opinion from experienced practitioners including dietitians have
been included. These guidelines do not address many issues concerning the implementation of dietetic practice, such as
using groups or individual consultations, educational strategies or counselling techniques. This is beyond the scope of
these guidelines and neither the evidence nor consensus opinion currently exists to promote one form of practice over
another.
The practice tips sections were added to provide further assistance to Dietitians and go beyond the scope of the
guidelines themselves. These sections are not evidence based but are included as a guide only, and are intended to
provide extra information about patient management.
These guidelines have been developed as a quality activity without funding, therefore there is no external influence on
the content of the guidelines. No member of the guideline taskforce has any conflict of interest to declare relating to the
development of these guidelines.
Consultation Process
These practice guidelines have undergone several stages of peer and expert review using the Appraisal of Guidelines for
Research and Evaluation (AGREE) instrument (The AGREE Collaboration). The rigour of scientific process varies
between guidelines. The K/DOQI and CARI guidelines have documented systematic search and review processes in
place, which meet the NH&MRC and AGREE criteria for quality. The ADA and EDTNA/ERCA guidelines are less
rigorous, but the information extracted from these documents is based on expert opinion and is unable to be assessed
using an evidence based practice tool.
Australia & New Zealand Renal Guidelines Taskforce
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
The first draft of these guidelines was presented at the Dietitians Association of Australia (DAA) 21st National
Conference in Cairns in May 2003 and achieved support in principle. A national panel of experts was defined at the
conference, the Australia and New Zealand Renal Guidelines Taskforce (ANZRGT) to oversee further development and
formulation of the final document. Consultation with nephrologists and renal nurses was undertaken when the
guidelines were presented at the 31st Annual Renal Society of Australasia Conference in Brisbane, also in May 2003.
The second draft was reviewed by the ANZRGT in August 2003 with comments incorporated into the final document.
ANZRGT launched the guidelines in Queensland on October 30, 2003 with the assistance of the Queensland Health
Core Practice Group. Following the launch of the 2003 Guidelines, a workshop was conducted at the DAA 22nd
National Conference in Melbourne in May 2004, on implementing the guidelines, and the taskforce gathered feedback
from the 6 month pilot period since launching the guidelines. Currently, the guidelines are published on the Queensland
Health Electronic Publishing Service (QHEPS) Internet site and are undergoing the endorsement process by DAA..
As part of the DAA endorsement process, consumer input was sourced from Kidney Health Australias regional
Advocacy Committees, which are comprised of CKD patients. A standardised feedback form was developed based on
recommendations from the Charter of Patient Rights. Feedback from consultation in two states has indicated that overall
consumers felt the guidelines provided a standardised approach to care, however were concerned that in their current
format were too technical to be understood by consumers. Consumers would have liked to have been involved from the
outset and were particularly interested that minority groups such as Indigenous people and those from non English
speaking backgrounds be considered in any educational material and that those in rural and remote areas receive the
same access to dietetic care as people in metropolitan areas. Discussion at both the National DAA workshops in 2003
and 2004 recognised the importance of involving consumers particularly from Indigenous backgrounds in the
development of education materials.
Use of Guidelines
These guidelines are meant to serve as a general framework for handling patients with particular health problems. It
may not always be appropriate to use these guidelines to manage clients because individual circumstances may vary.
The independent skill and judgement of the health care provider must always dictate treatment decisions. These
guidelines for practice are provided with the express understanding that they do not establish or specify particular
standards of care, whether legal, medical or other. (Adapted from Splett, 2000)
Review Process
These guidelines are based on other published guidelines and should be reviewed annually to ensure they remain
current. Responsibility for review lies with Royal Brisbane and Womens Hospital in conjunction with the Australia
and New Zealand Renal Guidelines Taskforce.
Next Review Date:
October 2005
References
The AGREE Collaboration. 2001. Appraisal of Guidelines for Research and Evaluation (AGREE) Instrument.
www.agreecollaboration.org (accessed 31/03/2003)
Splett, P.L. 2000. Developing and Validating Evidence Based Guides for Practice: A Tool Kit for Dietetics
Professionals, American Dietetic Association: United States of America.
Australia & New Zealand Renal Guidelines Taskforce
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Australia and New Zealand Renal Guidelines Taskforce (ANZRGT)
NAME
POSITION
LOCATION
STATE
PHONE
Susan Ash
Associate Professor,
Dietitian
Renal Dietitian
Queeensland University of
Technology
Greenslopes Private Hospital
Qld
(07) 3864 3524
s.ash@qut.edu.au
Qld
(07) 3394 7363
trevorthomas@powerup.com.au
(07) 3636 7997
katrina_campbell@health.qld.gov.au
Kathryn Anderson
Katrina Campbell
PhD Student, Dietitian
RBWH
Qld
Maria Chan
Renal Dietitian
St George Hospital
NSW
Suzie Chesterfield
Renal Dietitian
RBWH
Qld
Chanm@sesahs.nsw.gov.au
(07) 3636 7997
suzie_chesterfield@health.qld.gov.au
Karen Corke
Renal Dietitian
Canberra Hospital
ACT
(02) 6244 2211
Karen.corke@act.gov.au
Ruth Dumont
Renal Dietitian
Royal Perth Hospital
WA
(08) 9224 3203
Ruth.dumont@health.wa.gov.au
Kristin Gay
Renal Dietitian
Monash Medical Centre
Vic
(03) 9594 6666
k.gay@southernhealth.org.au
Lyn Lloyd
Renal Dietitian
Auckland City Hospital
NZ
64 9 5357 137
Lyn.lloyd@xtra.co.nz
Helen MacLaughlin
Renal Dietitian
Abbey Community
UK
(07) 3636 7997
helen.maclaughlin@abbeycommunity.org
Ellen McCoy
Renal Dietitian
RBWH
Qld
(07) 3636 7997
ellen_mccoy@health.qld.gov.au
Anthony Meade
Renal Dietitian
Queen Elizabeth Hospital
SA
(08) 8222 6000
Anthony.meade@nwahs.sa.gov.au
Robyn Montgomery
Renal Dietitian
Townsville Hospital
Qld
(07) 4796 2950
Tracey Tasker
Renal Dietitian
Royal Hobart Hospital
Tas
(03) 6222 8503
robyn.montgomeryjohnson@health.qld.gov.au
Tracey.tasker@dhhs.tas.gov.au
Paulett Thrift
Renal Dietitian
Area Renal, Tamworth
NSW
(02) 6767 8448
pthrift@doh.health.nsw.gov.au
Bernadeen Trotter
Renal Dietitian
Top End Renal Service
NT
(08) 8948 9000
bernadeen.trotter@nt.gov.au
Australia & New Zealand Renal Guidelines Taskforce
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
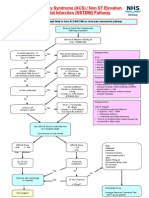
Evidence Based Practice Guideline Framework
Nutrition Care Process
Clinical Questions Related to Stage of Care Process
Criteria for referral to Dietitian
Objectives
At what level of GFR should
patients be referred to the dietitian
in order to maximise nutritional
intervention opportunities?
Achieve and
maintain
desirable
weight and
adequate
nutritional
status
Nutrition Assessment
Which specific measures best
reflect nutritional status or change
in nutritional status in Chronic
Kidney Disease?
Optimise
status of comorbidities
Normalise or
stabilise
biochemical
markers
Nutrition
Prescription/Intervention
What is (are) the appropriate
nutritional intervention(s) to
optimise nutritional status in
Chronic Kidney Disease and
prevent malnutrition?
Maintain
skeletal
muscle stores
and strength
Patients to
achieve
individual
goals
Implementation and
Management
What is the optimal method of
implementation and follow up to
ensure nutritional status is
maintained or improved?
Australia & New Zealand Renal Guidelines Taskforce
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Chronic Kidney Disease Stage 3 (GFR 30-59)
1 Scope
1.1 Definition
Chronic Kidney Disease (CKD) is defined as the presence of kidney damage for 3 months or more, as defined by
structural or functional abnormalities, with or without decreased glomerular filtration rate (GFR), OR, GFR less
than 60ml/min for more than 3 months with or without kidney damage. (3)
1.2 Diagnostic Criteria
Chronic Kidney Disease stages are defined by level of kidney function, irrespective of diagnosis. Stage 3
Chronic Renal Insufficiency (CRI) is described as moderate decrease in GFR, defined as GFR < 60 ml/min,
irrespective of the presence or absence of kidney damage. (3 - (R) & (O))
1.3 Patient Target Group
Any adult patient fulfilling the definition and diagnostic criteria, excluding those with nephrotic syndrome. These
guidelines by definition also exclude acute renal failure and transplantation.
2 Evidence Based Recommendations
2.1
Criteria for referral to Dietitian
GFR < 60ml/min (1 - level C evidence; 3 - (C) and (S))
Protein energy malnutrition develops during the course of chronic kidney disease and is associated with adverse
outcomes. Low protein and calorie intake is an important cause of malnutrition in chronic kidney disease. (3 - (C) and
(S))
PRACTICE TIPS:
1. Dietetic Management of Stage 3 CKD is focused on prevention of malnutrition and co-morbidity
management.
2. Prioritise patients who are malnourished or at risk of malnutrition. Use the Malnutrition Screening Tool
(Appendix 7) to determine who is at risk.
3. Manage co-morbidities or refer on to those who specialise in Overweight/Obesity, Diabetes or Coronary
Heart Disease Management.
2.2
Nutrition Assessment CKD Stage 3
Anthropometry
Measure
Outcome
Oedema-free (dry) actual body weight and
body mass index (BMI) (1 evidence, 3 evidence & opinion) and/or
BMI 18.5-25 (1) or as appropriate for
cultural group (see appendix 6)
Subjective global assessment (SGA) and/or
% ideal body weight (IBW) (3 - evidence &
opinion)
SGA optimise weight, muscle and fat
stores (4 opinion)
IBW within healthy weight range
(appendix 6)
Use total body nitrogen, dual x-ray
absorptiometry (DEXA) or bioelectrical
impedance (BIA) to measure long term
nutritional adequacy (1 - evidence & opinion) if
available and/or appropriate
Within the
population
Australia & New Zealand Renal Guidelines Taskforce
normal
ranges
for
the
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Biochemistry
and Clinical
Measure
Outcome
Serum albumin (3 evidence)
Within the normal range at individual
facilities (ANZRGT - opinion)
Creatinine and thus GFR (4 opinion)
Monitor rate of decline
Address modifiable factors (BP control;
glucose control in DM) (3 - R)
Haemoglobin (4 grade II evidence)
>120mg/L (males)
>110mg/L (females)
K+ and PO4 (4 - grade II evidence)
Maintained within or progressed towards
normal range at individual facilities
Plasma PTH (12 evidence)
Blood glucose (with Diabetes) (1- level A
evidence
3.85-7.7 pmol/L (12 Opinion)
4.4-6.7 (pre-prandial)
HbA1c (with Diabetes) (1 - level A evidence)
<7%
Blood pressure (4 grade II evidence)
<125/75 if >1 gram proteinuria/24hr or
diabetic nephropathy,
<130/85 without proteinuria
Serum cholesterol and triglycerides (1 level C
evidence)
Total cholesterol <5.0mmol/L (1 - level C
evidence)
TG - no level given
Note medications including antihypertensives, diuretics, phosphate binders and
vitamin/mineral supplements (4 opinion)
Diet
Lifestyle
Measure
normalised
protein
nitrogen
appearance (nPNA) (3 evidence & opinion) if
available, Or
No level given
Conduct dietary interview or analyse patient
food record (3 evidence & opinion) to ascertain
current intake
See 4.3 Nutrition Prescription
/Intervention
Determine current level of physical activity
and exercise habits (4 opinion)
Patient/client to maintain current
functional level and achieve individual
physical activity goals
Determine physical or motivational limitations
to exercise (4 opinion)
PRACTICE TIPS:
1. If you do use DEXA or BIA, ensure the patient is oedema-free prior to measurement or account for fluid
overload; see Appendix 9 for prediction equations.
2. Albumin: the presence of acute or chronic systemic inflammation limits the specificity of serum albumin as a
nutritional marker
3. GFR: see Appendix 5 for calculating GFR from serum creatinine
4. PTH: there is an inverse relationship between PTH levels and GFR, which is subsequently linked with lowturnover bone disease. This occurs in the absence of raised serum PO4 levels. Monitoring of PTH is
recommended at least every 12 months. (12)
5. Triglycerides recommend use normal acceptable levels, CKD is high risk category for heart disease
6. nPNA: see appendix 5 for calculating nPNA from 24hr urine collection. NB: nPNA related to protein intake
only when protein and KJ intake are constant and the patient is metabolically stable (2)
Australia & New Zealand Renal Guidelines Taskforce
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
2.3
Nutrition Prescription/Intervention CKD Stage 3
Energy
Ideal kilojoule/calorie energy intake determined for their age, gender, BMI and level of
physical activity
A nutritionally balanced diet with adequate energy intake to maintain a healthy weight
should be prescribed. (1 - level C evidence)
Protein
A normal protein diet, consisting of 0.75-1.0g/kg IBW/day, is recommended. The
clinically unimportant benefit of low protein diets (<0.6g/kg/day) on renal failure
progression is not justified when weighed against the concomitant significant declines in
clinical and biochemical parameters of nutrition. (1 - level A evidence)
Fat and
Carbohydrate
Priority should be given to a diet aimed at avoidance of protein-energy malnutrition, and
reducing fat intake to <30% of daily energy intake, with the saturated fat component
limited to 10%. Carbohydrates should be utilised to make up the balance of the required
daily energy intake. (1- level C evidence)
Sodium
<100mmol/day if hypertensive and CKD is progressive. (1 - level C evidence)
Potassium
Not usually restricted in renal insufficiency (4 - opinion)
If > 6.0mmol/L a reduced potassium diet should be commenced. (1 level C evidence)
Phosphate
Dietary phosphate restriction (800-1000 mg/d) and/or use of phosphate binders, if PO4
>1.49mmol/L (12 opinion) and/or PTH >7.7pmol/L on more than 2 consecutive
measurements (12 evidence).
Fluid
Intake should be adjusted to the degree of CKD, and prevention of renal disease, oedema
and hypertension management. Once fluid management requires diuretics a liberal fluid
intake should be curbed. Management of hypertension includes limiting fluid intake. (1
level C evidence)
Supplementation
Patients with chronic kidney disease with GFR < 50ml/min, and an elevated parathyroid
hormone (PTH) level or histological evidence of osteodystrophy, should receive
supplementation with vitamin D (calcitriol). (1 level A evidence)
Lifestyle
Dietitian to encourage physical activity as outlined in the National Physical Activity
Guidelines for Australians (5). Refer patient to medical team and exercise physiologist /
physiotherapist as appropriate
PRACTICE TIPS:
1. for IBW ranges see appendix 6
2. Energy: Weight loss is appropriate if BMI > 30 in order to manage co-morbidities (3 - opinion)
3. Protein: focus on achieving ideal intake and avoid the terms restriction or low protein
4. Fat: On occasions the fat intake may need to be increased to above 30% to prevent undesired weight loss.
Unsaturated fats are to be used in preference to saturated fat sources. (ANZRGT - opinion)
5. Potassium: A reduced potassium diet limits K+ intake to 1mmol/kg IBW/day. (ANZRGT opinion). Before
commencing this diet, ensure that hyperkalaemia is not a result of an acute response to conditions such as
uncorrected acidosis or raised haematocrit (ANZRGT opinion).
6. Phosphate: If PO4 >1.49mmol/L and/or PTH >7.7pmol/L, phosphate intake should be maintained between
<1000mg/day, in combination with use of PO4 binder medication (12 evidence and opinion). Care must be
taken when restricting PO4 intake, as to not compromise recommended protein intake (ANZRGT opinion).
7. The medical team should prescribe supplementation of vitamin D. The guideline on supplementation is
included for information purposes and the Dietitian may recommend supplementation.
Australia & New Zealand Renal Guidelines Taskforce
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
2.4 Implementation and Management CKD Stage 3
Education
Patients with decreased dietary intake or malnutrition should undergo dietary
modification, counselling and education or specialised nutrition therapy (3-R)
Nutrition counselling should encompass adequate protein and energy intake, blood
glucose control in DM, fluid and sodium control in hypertension (3 - evidence),
phosphate control in hyperparathyroidism (12 evidence), lipid control if indicated (1
level C evidence), weight management if indicated (3 - opinion), meal plans, recipe
modification, self monitoring and reading food labels (4 opinion).
Management
Recommended time for the initial consultation is 45-60 minutes (4 opinion)
Recommended time for review consultations is 20-30 minutes (4 opinion)
Monthly
Oedema-free (dry) body weight & BMI calculated (1 evidence)
6-12
monthly
For patients with GFR 30-60 ml/min (CKD stage 3) nutritional status
should be monitored every 6-12 months if there is no evidence of
malnutrition (3 opinion) and more frequently if malnourished
PRACTICE TIPS:
1. For patients with poorly controlled co-morbidities (hyperglycaemia, hypertension & hyperlipidaemia) refer to
the appropriate medical specialist for management of co-morbidities. (ANZRGT - opinion)
2. It is important to recognise this stage of CKD requires nutritional management to maximise health and
prevent nutritional deterioration. Individualised management with 6-12 monthly reviews is recommended. If
resources are not available to see patients, then documentation of referrals is advised, for future lobbying for
resources. (ANZRGT - opinion)
3. Consultation times account for patient contact time only and do not include additional time spent in associated
administrative tasks such as making patient-associated telephone calls, obtaining biochemistry results or
writing letters. (ANZRGT opinion)
3 Summary of Recommendations
-
See Appendix 1 and 2
Australia & New Zealand Renal Guidelines Taskforce
10
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Chronic Kidney Disease Stage 4 (GFR 15- 29)
1 Scope
1.1 Definition
Chronic Kidney Disease (CKD) is defined as the presence of kidney damage for 3 months or more, as defined by
structural or functional abnormalities, with or without decreased glomerular filtration rate (GFR), OR, GFR less
than 30ml/min for more than 3 months with or without kidney damage. (3)
1.2. Diagnostic Criteria
Chronic Kidney Disease stages are defined by level of kidney function. Stage 4 is described as a severe decrease
in GFR, defined as GFR 15-29 ml/min, with or without kidney damage. (3)
1.3 Patient Target Group
Any adult patient fulfilling the definition and diagnostic criteria, excluding those with nephrotic syndrome. These
guidelines by definition also exclude acute renal failure and transplantation.
2 Evidence Based Recommendations
2.1
Criteria for referral to Dietitian
GFR < 30ml/min (1 - level C evidence; 3 - (C) and (S))
PRACTICE TIPS:
1. Dietetic Management of Stage 4 CKD is focused on optimisation of protein and energy intake to reduce
symptoms of uremia and malnutrition.
2. Prioritise those patients who are malnourished or at risk of malnutrition.
3. These guidelines also apply to patients with GFR < 15 ml/min who are not undergoing dialysis treatment.
2.2
Nutrition Assessment CKD Stage 4
Anthropometry
Biochemistry
and Clinical
Measure
Outcome
Oedema-free (dry) actual body weight and
body mass index (BMI) (1 evidence, 2 evidence & opinion)
BMI 18.5-25 (1) or as appropriate for
cultural group (see appendix 6)
Subjective global assessment (SGA) and/or
% ideal body weight (IBW) (2- evidence &
opinion)
SGA optimise muscle stores, weight and
fat stores (4 opinion)
IBW within healthy weight range
(appendix 6)
Use total body nitrogen, dual x-ray
absorptiometry (DEXA) or bioelectrical
impedance (BIA) to measure long term
nutritional adequacy (1 - evidence & opinion) if
available and/or appropriate
Within the
population
Serum albumin (2 evidence)
Within the normal range at individual
facilities (ANZRGT - opinion)
Creatinine and thus GFR (4 opinion)
Monitor rate of decline
Address modifiable factors (BP control;
glucose control in DM) (3 - R)
Haemoglobin (4 grade II evidence)
>120mg/L (males)
>110mg/L (females)
Australia & New Zealand Renal Guidelines Taskforce
normal
ranges
for
the
11
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Measure
Biochemistry
and Clinical
(cont)
Outcome
K and PO4 (4 - grade II evidence)
K+ < 6.0mmol/L (1 level C evidence)
PO4 0.87 1.49 mmol/L (12 evidence
and opinion)
Plasma PTH (12 evidence)
Blood glucose (with Diabetes) (1 - level A
evidence)
HbA1c (with Diabetes) (1 - level A evidence)
7.7 12.1 pmol/L (12 opinion)
4.4-6.7 (pre-prandial)
Blood pressure (4 grade II evidence)
<125/75 if >1g proteinuria or diabetic
nephropathy, <130/85 if no proteinuria
Serum cholesterol and triglycerides (1 level C
evidence)
TC <5.0mmol/L (1 - level C evidence)
TG - no level given
<7%
Note medications including antihypertensives, diuretics, phosphate binders and
vitamin/mineral supplements (4 opinion)
Diet
Lifestyle
Measure
normalised
protein
nitrogen
appearance (nPNA) (2 evidence & opinion) if
available Or
No level given
Conduct dietary interview or analyse patient
food record (2 evidence & opinion) to ascertain
current intake
See 4.3 Nutrition Prescription
/Intervention
Determine current level of physical activity
and exercise habits (4 opinion)
Patient/client to maintain current
functional level and achieve individual
physical activity goals
Determine physical or motivational limitations
to exercise (4 opinion)
PRACTICE TIPS:
1. If you do use DEXA or BIA, ensure the patient is oedema-free prior to measurement or account for fluid
overload; see Appendix 9 for prediction equations
2. Albumin: the presence of acute or chronic inflammation limits the specificity of serum albumin as a
nutritional marker
3. GFR: see Appendix 5 for calculating GFR from serum creatinine
4. PTH: there is an inverse relationship between PTH levels and GFR, which is subsequently linked with lowturnover bone disease. This occurs in the absence of raised PO4 levels. Monitoring of PTH is recommended
at least every 3 months. (12 opinion)
5. Triglycerides recommend use normal acceptable levels, CKD is high risk category for heart disease
6. nPNA: see appendix 5 for calculating nPNA from 24hr urine collection. NB: nPNA related to protein intake
only when protein and KJ intake are constant and the patient is metabolically stable (2)
Australia & New Zealand Renal Guidelines Taskforce
12
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
2.3
Nutrition Prescription/Intervention CKD Stage 4
Energy
An energy intake of at least 146kJ (35kcal)/kg IBW/day must accompany a moderate
protein restriction to minimise protein energy malnutrition. (1 - level A evidence)
For patients > 60 years, with a moderate protein restriction, an energy intake of 125146kJ (30-35kcal)/kg IBW is recommended. (2 evidence and opinion)
Protein
For patients with progressive chronic kidney disease (GFR < 25ml/min), the protein
content of the diet should not be less than 0.75g/kg IBW/day. (1 - level A evidence)
At least 50% of the protein should be of high biological value. (1 - level A evidence)
Fat and
Carbohydrate
Priority should be given to a diet aimed at avoidance of protein-energy malnutrition, and
reducing fat intake to <30% of daily energy intake, with the saturated fat component
limited to 10%. Carbohydrates should be utilised to make up the balance of the
required daily energy intake. (1- level C evidence)
Sodium
<100mmol/day if hypertensive and CKD is progressive. (1 level C evidence)
Potassium
If K+ > 6.0mmol/L a reduced potassium diet should be commenced. (1 level C evidence)
Phosphate
Dietary phosphate restriction (800-1000 mg/d) and/or use of phosphate binders, if PO4
>1.49mmol/L (12 opinion) and/or PTH > 12.1 pmol/L on more than 2 consecutive
measurements (12 evidence)
Fluid
Fluid intake should be adjusted to the degree of CKD, oedema and hypertension
management. Once fluid management requires diuretics a liberal fluid intake should be
curbed. Management of hypertension includes limiting fluid intake. (1 level C
evidence)
Supplementation
Patients with chronic kidney disease following a protein restricted diet (<0.75g/kg
IBW/day) should receive supplementation with thiamine (>1mg/day), B2 (1-2mg/day)
and B6 (1.5-2mg/day). (1 level B evidence)
Patients with chronic kidney disease with GFR < 50ml/min, and an elevated parathyroid
hormone (PTH) level or histological evidence of osteodystrophy, should receive
supplementation with vitamin D (calcitriol). (1 - level A evidence)
Lifestyle
Dietitian to encourage physical activity as outlined in the National Physical Activity
Guidelines for Australians (5).
Refer patient to medical team and exercise
physiologist/physiotherapist as appropriate.
PRACTICE TIPS:
1. for IBW ranges see appendix 6
2. Energy: maximise unsaturated fats and sugars or modular supplements to achieve energy intake of 125146kJ/kg IBW/day if in HWR. Weight loss is appropriate if BMI > 30 in order to manage co-morbidities (3 opinion).
3. Protein: The protein content should also not be greater than 1.0g/kg IBW/day. (ANZRGT opinion)
4. Fat: On occasions the fat intake may need to be increased to above 30% to prevent undesired weight loss.
Unsaturated fats are to be used in preference to saturated fat sources. (ANZRGT - opinion)
5. Potassium: A reduced potassium diet limits K+ intake to 1mmol/kg IBW/day. (ANZRGT opinion)
6. Phosphate: try to optimise compliance with PO4 binder medication in conjunction with maintaining phosphate
intake between 800mg and 1000mg/day, (12 evidence and opinion)
7. The medical team should prescribe supplementation of vitamins. The guidelines on supplementation are
included for information purposes and the Dietitian may recommend supplementation.
Australia & New Zealand Renal Guidelines Taskforce
13
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
2.4 Implementation and Management CKD Stage 4
Education
Pre end stage kidney disease education forms an important part of the management
strategy to slow the progression of renal disease and may have an independent beneficial
effect. (1 level A evidence)
Nutrition counselling should encompass appropriate protein and energy intake (2
evidence and opinion), fluid, sodium and potassium intake (1 level C evidence), weight
management if indicated (1 & 3 - opinion), meal plans, recipe modification, self
monitoring and reading food labels (4 opinion).
Management
Recommended time for the initial consultation is 45-60 minutes (4 opinion)
Recommended time for review consultations is 20-30 minutes (4 opinion)
Monthly
Oedema-free (dry) body weight measured and BMI calculated (1 evidence)
3 monthly
Recent nutrient intake assessment (diet evaluation or nPNA) (1 evidence
and opinion)
especially if GFR < 15ml/min, concomitant illness, inadequate nutrient
intake or malnutrition (2 evidence & opinion)
6-12 monthly
SGA (1 - opinion)
Assessment of long term nutritional adequacy with total body nitrogen,
DEXA or BIA (1 evidence and opinion) if available or appropriate
PRACTICE TIPS:
1. It is important to recognise this stage of CKD requires nutritional management to prevent malnutrition by
optimising protein, energy and fluid intake. Individualised management with 3 monthly reviews is
recommended. If resources are not available to see patients, then documentation of referrals is advised, for
future lobbying for resources. (ANZRGT - opinion)
2. For Patients with poorly controlled co-morbidities (hyperglycaemia, hypertension & hyperlipidaemia)
education should also address improving blood glucose control, weight management and blood lipids.
(ANZRGT - opinion)
3. Consultation times account for patient contact time only and do not include additional time spent in associated
administrative tasks such as making patient-associated telephone calls, obtaining biochemistry results or
writing letters (ANZRGT opinion)
3 Summary of Recommendations
-
see Appendix 1 and 2
Australia & New Zealand Renal Guidelines Taskforce
14
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Chronic Kidney Disease Stage 5 - Haemodialysis
1 Scope
1.1 Definition
Chronic Kidney Disease (CKD) is defined as the presence of kidney damage for 3 months or more, as defined by
structural or functional abnormalities, with or without decreased glomerular filtration rate (GFR), OR, GFR less
than 60ml/min for more than 3 months with or without kidney damage. (3)
1.2 Diagnostic Criteria
Chronic Kidney Disease stages are defined by level of kidney function. Stage 5 is described as kidney failure,
with renal replacement therapy such as haemodialysis. (3)
1.3 Patient Target Group
Any adult patient fulfilling the definition and diagnostic criteria. These guidelines by definition also exclude acute
renal failure and transplantation, unless the transplant has failed and the patient is undergoing dialysis treatment.
2 Evidence Based Recommendations
2.1
Criteria for referral to Dietitian
For haemodialysis patients, nutritional status should be routinely assessed at commencement of haemodialysis
and at regular intervals thereafter. (1 evidence; 2 evidence)
PRACTICE TIP:
1. Prioritise those patients with poorly controlled co-morbidities or malnutrition. (ANZRGT - opinion)
2.2
Nutrition Assessment CKD Stage 5 - Haemodialysis
Anthropometry
Biochemistry
and Clinical
Measure
Outcome
% Ideal oedema free (dry) body weight (2
opinion) and body mass index (BMI) (1
evidence)
IBW within range BMI 23-26
(ANZRGT - opinion) or as appropriate for
cultural group (see appendix 6)
Subjective global assessment (SGA) (1&2 opinion)
SGA maintained or improved (8 - no level
cited)
Use total body nitrogen, dual x-ray
absorptiometry (DEXA) or bioelectrical
impedance (BIA) to measure long term
nutritional adequacy (1 - evidence & opinion) if
available &/or appropriate
Within range for normal population
Pre dialysis serum albumin (1 evidence; 2 evidence)
Within the normal range at individual
facilities (ANZRGT - opinion)
Pre dialysis serum potassium (8 - no level cited)
< 5.5mmol/L
Pre dialysis serum urea (7 level B evidence)
21-39mmol/L correlates with reduced
relative risk of morbidity
Pre dialysis serum phosphate (12 evidence)
1.13-1.78 mmol/L target range (12
evidence)
16.5-33.0 pmol/L (12 evidence)
<5.8 (mmol/L)2 or 2.9 if ionised calcium,
(iCa) is used
Ideal target is less than 4.2 or 2.6
(mmol/L)2 (iCa) (1 - level B evidence)
Pre dialysis PTH (12 evidence)
Pre dialysis corrected calcium x phosphate
product (1 - level B evidence)
Pre dialysis serum lipids (11 - evidence)
TC<5.2mmol/L; LDL<2.6mmol/L; TG
<1.7mmol/L
Australia & New Zealand Renal Guidelines Taskforce
15
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Biochemistry
and Clinical
(cont)
Measure
Outcome
Post dialysis serum urea (8 - no level cited)
65% reduction from pre dialysis value
indicates adequate haemodialysis (1 - level
B evidence)
Ascertain dialysis adequacy (1 - level B
evidence)
Ascertain dialysis frequency and fluid gains (8
- no level cited)
Target Kt/V should be 1.2 (9 evidence)
HbA1c (for persons with diabetes) (8 - no level
cited)
<7%
Blood pressure (8 no level cited)
Appropriate control maintained
Achieve interdialytic fluid gains 2-5%
IBW
Note medications including antihypertensives, diuretics, phosphate binders and
vitamin/mineral supplements (8 no level cited)
Diet
Lifestyle
Measure normalised protein nitrogen
appearance (nPNA) (1 - evidence & opinion, 2
evidence) if available
nPNA 0.8 (8 - no level cited)
Conduct dietary interview or analyse patient
food record (1 evidence & opinion; 2
evidence & opinion) to ascertain current intake
See 4.3 Nutrition Prescription
/Intervention
Determine current level of physical activity
and exercise habits (8 no level cited)
Patient/client to maintain current
functional level and achieve individual
physical activity goals
Determine physical or motivational limitations
to exercise (8 no level cited)
PRACTICE TIPS:
1. If you do use DEXA or BIA, ensure that measurement is performed at dry weight; see Appendix 9 for
prediction equations.
2. Biochemistry stated as pre dialysis indicates blood tests to be taken immediately prior to the dialysis session.
3. Albumin: the presence of acute or chronic inflammation limits the specificity of serum albumin as a
nutritional marker
4. Phosphate: < 30% of dialysis patients are able to maintain PO4 in the target range. The goal should be for
levels <2.2 mmol/L for lower risk of mortality. (12 evidence), and increase the percentage of patients in the
target range. (12 opinion).
5. Adequacy of dialysis can be assessed in several ways. The most common acceptable methods are: formal
urea-kinetic Kt/V, URR (urea reduction ratio), natural log Kt/V and the Daugirdas second generation formula.
A renal unit should be consistent in the method it applies. (1- Level C evidence)
6. nPNA: see appendix 5 for calculating nPNA from post and pre dialysis biochemistry. NB: nPNA related to
protein intake only when protein and KJ intake are constant and the patient is metabolically stable (2)
2.3
Nutrition Prescription/Intervention CKD Stage 5 - Haemodialysis
Energy
For haemodialysis patients, it seems prudent to follow published recommendations of
125-146 kJ (30-35kcal)/kg ideal body weight (IBW)/day. (1 level C evidence)
Recommended energy intake when acutely ill is at least 146kJ (35kcal)/kg IBW/day for
those < 60 yrs and at least 125-146kJ (25-35kcal)/kg IBW/day for those 60 years and
older. (2 - evidence and opinion)
Protein
For haemodialysis patients, it seems prudent to follow published recommendations of
1.2-1.4g protein/kg IBW /day. (1 level C evidence)
At least 50% of the dietary protein should be of high biological value. (2 evidence and
opinion)
Recommended protein intake when acutely ill is at least 1.2g/kgIBW/day. (2 opinion)
Fat and
Carbohydrate
Saturated fat <7%, poly-unsaturated fat 10%, mono-unsaturated fat 20% of total kJ
CHO 50-60% of total kJ (11 evidence and opinion)
Australia & New Zealand Renal Guidelines Taskforce
16
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Sodium
80 110 mmol/day (6 evidence and agreed best practice)
Potassium
1mmol/kg IBW/day (8 no level cited)
Phosphate
Dietary phosphate restriction (800-1000 mg/d) and/or use of phosphate binders, if PO4
>1.8mmol/L (12 opinion) and/or PTH >33.3pmol/L (12 evidence).
Fluid
500ml + previous days urine output (PDUO). (6 evidence and agreed best practice)
Supplementation
not specifically addressed by any guidelines for haemodialysis
Lifestyle
Dietitian to encourage physical activity as outlined in the National Physical Activity
Guidelines for Australians (5). Refer patient to medical team and exercise
physiologist/physiotherapist as appropriate.
PRACTICE TIPS:
1. Energy and Protein: IBW range for HD is BMI 22-25 (1 - opinion, ethnic group or age not specified), for
IBW ranges see Appendix 6; aim to achieve weight in IBW range
2. Phosphate: Care must be taken to make the diet as low as possible in phosphate whilst maintaining adequate
protein. To ensure a reasonable level, calculate 10-12mg phosphate per gram of recommended protein. (12
opinion).
3. Supplementation: The medical team manages prescription of vitamins and minerals. Supplementation as in
CKD stages 3 and 4 is still applicable. (ANZRGT - opinion)
4. Fibre intake should be encouraged, as constipation can be common in haemodialysis. (ANZRGT - opinion)
2.4
Implementation and Management CKD Stage 5 - Haemodialysis
Education
Every haemodialysis patient should receive intensive nutritional counselling based on an
individualised care plan (2 opinion), focusing on adequate protein and energy intake (1
level C evidence), fluid and electrolyte management (8 no level cited), self monitoring and
meal plans (8 no level cited).
Management
Recommended time for initial consultation is 45-60 mins (8 - no level cited)
Recommended time for review sessions is 30-45 minutes for initial review and then 45-60
minutes every 6 months (8 no level cited)
Monthly
Oedema-free (dry body weight) and BMI (1 - evidence)
Serum albumin (1 opinion)
3 6 monthly
Dialysis adequacy (Kt/V) (1 - Level C evidence)
nPNA (1 evidence and opinion)
Dietary interviews (more frequently if clinically indicated) (1 opinion)
SGA (1&2 - opinion)
6-12 monthly
Assessment of long term nutritional adequacy with total body nitrogen,
DEXA or BIA (1 opinion) if available or appropriate
PRACTICE TIPS:
1. Consultation times account for patient contact time only and do not include additional time spent in associated
administrative tasks such as making patient-associated telephone calls, obtaining biochemistry results or
writing letters (ANZRGT opinion)
2. If resources are not available to see patients as frequently as recommended, then documentation is advised,
for future lobbying for resources. (ANZRGT - opinion)
3 Summary of Recommendations
-
See Appendix 1 and 2
Australia & New Zealand Renal Guidelines Taskforce
17
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Chronic Kidney Disease Stage 5 - Peritoneal Dialysis
1 Scope
1.1 Definition
Chronic Kidney Disease (CKD) is defined as the presence of kidney damage for 3 months or more, as defined by
structural or functional abnormalities, with or without decreased glomerular filtration rate (GFR), OR, GFR less
than 60ml/min for more than 3 months with or without kidney damage (3).
1.2 Diagnostic Criteria
Chronic Kidney Disease stages are defined by level of kidney function. Stage 5 is described as kidney failure,
with renal replacement therapy such as peritoneal dialysis (3).
1.3 Patient Target Group
Any adult patient fulfilling the definition and diagnostic criteria. These guidelines by definition also exclude acute
renal failure and transplantation, unless the transplant has failed and the patient is undergoing dialysis treatment.
2 Evidence Based Recommendations
2.1
Criteria for referral to Dietitian
For peritoneal dialysis patients, nutritional status should be routinely assessed at commencement of peritoneal
dialysis and at regular intervals thereafter. (1 & 2 evidence)
PRACTICE TIP:
1. Prioritise those patients with poorly controlled co-morbidities or malnutrition. (ANZRGT - opinion)
2.2
Nutrition Assessment CKD Stage 5 Peritoneal Dialysis
Anthropometry
Biochemistry
and Clinical
Measure
Outcome
The nutritional status of peritoneal dialysis
patients should be monitored by methods
appropriate to assess total body stores and
detect early changes of malnutrition.
Methods such as nPNA (1 - level C evidence; 2
evidence & opinion), total body nitrogen (1 level C evidence), DEXA (1&2 evidence &
opinion) or SGA (1 level C evidence; 2
evidence and opinion) should be used.
nPNA >0.9 (10 - opinion)
total body nitrogen & DEXA within the
range for normal population
SGA maintained or improved (8 no level
cited)
% Ideal dry body weight (2 opinion) and
body mass index (BMI) (1 evidence)
IBW within range BMI 23-26
(ANZRGT opinion) or as appropriate for
cultural group (see appendix 6)
Serum Albumin (1 evidence; 2 - evidence).
Within the normal range at individual
facilities (ANZRGT - opinion)
Serum urea and/or creatinine (1 - evidence)
Stabilise
If urea and /or creatinine are low patient
should be further evaluated for
malnutrition. (1 evidence)
Serum K
K: 3.5 5.5 mmol/L
HbA1c (for persons with diabetes) (8 - no level
cited
<7%
Blood pressure (8 no level cited)
Appropriate control maintained
Australia & New Zealand Renal Guidelines Taskforce
18
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Biochemistry
and Clinical
(cont)
Measure
Outcome
Serum lipids (11 - evidence)
TC<5.2mmol/L; LDL<2.6mmol/L; TG
<1.7mmol/L
Serum PO4 (12 evidence)
1.13-1.78 mmol/L target range (12
evidence)
16.5-33.0 pmol/L (12 evidence)
<5.8 (mmol/L)2 or 2.9 if ionised calcium,
(iCa) is used
Ideal target is less than 4.2 or 2.6
(mmol/L)2 (iCa) (1 - level B evidence)
Plasma PTH (12 evidence)
Serum albumin corrected calcium x phosphate
product (1 - level B evidence)
Dialysis adequacy (Kt/V) (10 - evidence)
Weekly target 2.0 with a minimum of
1.7/week
Ascertain type of peritoneal dialysis and prescription (8 - no level cited)
Note medications including antihypertensives, diuretics, phosphate binders and
vitamin/mineral supplements (8 no level cited)
Diet
Lifestyle
Measure protein equivalent of normalised
protein nitrogen appearance (nPNA) if
available (1 - evidence & opinion, 2 evidence)
nPNA > 0.9 (10 - opinion)
Conduct dietary interview and/or review
patient food record (1 evidence & opinion; 2
evidence & opinion) to ascertain current intake
See 4.3 Nutrition Prescription
/Intervention
Determine current level of physical activity
and exercise habits (8 opinion)
Patient/client to maintain current
functional level and achieve individual
physical activity goals
Determine physical or motivational limitations
to exercise (8 opinion)
PRACTICE TIPS:
1. nPNA: see appendix 5 for calculating nPNA from biochemistry. NB: nPNA related to protein intake only
when protein and KJ intake are constant and the patient is metabolically stable (2)
2. If you do use DEXA or BIA, ensure that measurement is performed at dry weight; see Appendix 9 for
prediction equations.
3. Albumin: the presence of acute or chronic inflammation limits the specificity of serum albumin as a
nutritional marker
4. Phosphate: < 30% of dialysis patients are able to maintain PO4 in the target range. The goal should be for
levels <2.2 mmol/L for lower risk of mortality. (12 evidence), and increase the percentage of patients in the
target range. (12 opinion).
5. Adequacy of dialysis can be assessed in several ways. The most common acceptable methods are: formal
urea-kinetic Kt/V, URR (urea reduction ratio), natural log Kt/V and the Daugirdas second generation formula.
A renal unit should be consistent in the method it applies. (1- Level C evidence)
4.3
Energy
Nutrition Prescription/Intervention CKD Stage 5 Peritoneal Dialysis
For peritoneal dialysis patients, total energy intake of 146kJ (35kcal)/kg ideal body
weight (IBW)/day should be achieved. (1 level C evidence)
The recommended energy intake for acutely ill peritoneal dialysis patients is at least
146kJ (35kcal)/kg IBW/day for those < 60 yrs and at least 125-146kJ (30-35kcal)/kg/day
for those 60 years and older (2 - evidence and opinion)
NB: The recommended total energy intake includes energy from the dialysate. To account for
glucose load of dialysate when calculating energy requirements. Approximately 60% of the
glucose in the dialysate is absorbed (2).
Australia & New Zealand Renal Guidelines Taskforce
19
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Protein
For peritoneal dialysis patients, recommendation of 1.2-1.4g protein/kg IBW /day. (1
level C evidence)
At least 50% of the dietary protein should be of high biological value (2 evidence and
opinion)
Recommended protein intake for a peritoneal dialysis patient who is acutely ill is at least
1.3g/kg IBW/day. (2 opinion)
A higher intake of 1.5g/kg IBW/day is recommended for patients with peritonitis. (6
evidence and agreed best practice)
Fat and
Carbohydrate
Saturated fat <7%, poly-unsaturated fat 10%, mono-unsaturated fat 20% of total kJ
CHO 50-60% of total kJ (11 evidence and opinion)
Sodium
Individualised treatment recommended based on oedema and hypertension
If restriction required, 80-110 mmol/day. (6 evidence and agreed best practice)
Potassium
Individualised treatment recommended based on biochemistry
Phosphate
Dietary phosphate restriction (800-1000 mg/d) and/or use of phosphate binders, if PO4
>1.8mmol/L (K/DOQI bone, opinion) and/or PTH >33.3pmol/L (12 evidence).
Fluid
Individualised treatment recommended based on oedema and hypertension
If fluid overloaded: limit fluid intake to 800ml + previous days urine output (PDUO). (6
evidence and agreed best practice)
Supplementation
not specifically addressed by any guidelines for peritoneal dialysis
Lifestyle
Dietitian to encourage physical activity as outlined in the National Physical Activity
Guidelines for Australians (5). Refer patient to medical team and exercise
physiologist/physiotherapist as appropriate.
PRACTICE TIPS:
1. Energy & Protein: IBW range for PD is BMI 23-26 (opinion, ethnic group or age not specified), for IBW
ranges see Appendix 6; aim to achieve weight in IBW range
2. Energy: To calculate the energy from a peritoneal dialysis bag based on dextrose, estimate 60-100%
absorption of dextrose. For example for a 1500mL bag, 15% dextrose, will give 250-420kJ. Common
practise is to estimate absorption of up to 2000kJ/day from the diasylate, if a patient is on 4 bags per day.
(ANZRGT opinion).
3. Potassium: If restriction required, suggested level is 1mmol/kg IBW/day. (ANZRGT - opinion)
4. Phosphate: Care must be taken to make the diet as low as possible in phosphate whilst maintaining adequate
protein. To ensure a reasonable level, calculate 10-12mg phosphate per gram of recommended protein. (12
opinion).
5. Supplementation: The medical team manages prescription of vitamins and minerals. Multivitamin
supplementation may be required, and supplementation as in CKD stages 3 and 4 is still applicable.
(ANZRGT - opinion)
6. Encourage fibre intake. Constipation in PD can affect catheter position and increase risk of peritonitis.
(ANZRGT - opinion)
Australia & New Zealand Renal Guidelines Taskforce
20
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
2.4 Implementation and Management CKD Stage 5 Peritoneal Dialysis
Education
Every peritoneal dialysis patient should receive intensive nutritional counselling based on
an individualised care plan (2 opinion) focusing on adequate protein intake and
appropriate energy intake (1 level C evidence), maintenance of muscle stores (1 level C
evidence), self monitoring and meal plans (8 no level cited).
Management
Recommended time for initial consultation is 45-60 mins (8 - no level cited)
Recommended time for review sessions is 30-45 minutes for initial review and then 45-60
minutes every 6 months (8 no level cited).
Monthly
Oedema-free (dry body weight) and BMI (1 - evidence)
Serum albumin (1 opinion)
6 monthly
SGA (1 level C evidence)
nPNA (1 level C evidence)
Dietary interviews (more frequently if clinically indicated) (1 opinion)
weekly Kt/V (1 level C evidence)
total body nitrogen or DEXA (1 opinion) if available
PRACTICE TIPS:
1. Consultation times account for patient contact time only and do not include additional time spent in associated
administrative tasks such as making patient-associated telephone calls, obtaining biochemistry results or
writing letters (ANZRGT opinion)
2. If resources are not available to see patients as frequently as recommended, then documentation is advised,
for future lobbying for resources. (ANZRGT - opinion)
3 Summary of Recommendations
-
See Appendix 1 and 2
Australia & New Zealand Renal Guidelines Taskforce
21
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
References
1. The CARI Guidelines (Caring for Australians with Renal Impairment). 2003. Australian
Kidney Foundation & Australia New Zealand Society of Nephrology.
2. Clinical practice guidelines for nutrition in chronic renal failure. K/DOQI, National Kidney
Foundation. 2000. American Journal of Kidney Diseases, 35 (supp 2), s1-s140.
3. National Kidney Foundation Kidney Disease Outcome Quality Initiative (K/DOQI) Advisory
Board. 2002. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation,
classification and stratification. American Journal of Kidney Diseases, 39 (supp 2), s1-s246.
4. American Dietetic Association. 2002. Medical Nutrition Therapy Evidence-Based Guides for
Practice: Chronic Kidney Disease (non-dialysis) Medical Nutrition Therapy Protocol.
Chicago: American Dietetic Association.
5. National Physical Activity Guidelines for Australians. 1999. Canberra: Australian Department
of Health and Ageing.
6. European Guidelines for the Nutritional Care of Adult Renal Patients. 2003. European
Dialysis and Transplantation Nurses Association/European Renal Care Association (EdtnaErca) Journal, 29(1), s1-s23.
7. Lowrie, EG & Lew, NL. 1990. Death risk in haemodialysis patients: the predictive value of
commonly measured variables and an evaluation of death rate differences between facilities.
American Journal of Kidney Diseases, 15, 458-482.
8. Wiggins, K.L. 2002. Guidelines for Nutritional Care of Renal Patients (3rd ed). Renal
Dietitians Dietetic Practice Group, American Dietetic Association. Chicago: American Dietetic
Association.
9. NKF-K/DOQI clinical practice guidelines for hemodialysis adequacy: update 2000. 2001.
American Journal of Kidney Diseases, 37 (supp 1), s7-s64.
10. NKF-K/DOQI clinical practice guidelines for peritoneal dialysis adequacy: update 2000. 2001.
American Journal of Kidney Diseases. 37 (supp 1), s65-s136.
11. K/DOQI Clinical Practice Guidelines for Managing Dyslipidemias in Chronic Kidney Disease.
2003. American Journal of Kidney Diseases, 41(supp 3), s1 s79.
12. K/DOQI Clinical Practice Guidelines for bone metabolism and disease in chronic kidney
disease. American Journal of Kidney Disease, 42(4), S7 S169.
Australia & New Zealand Renal Guidelines Taskforce
22
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Appendix 1: Summary of Recommendations for Management of Chronic Kidney
Disease
Chronic Kidney
Disease Stage 3
(GFR 30-59)3
GFR<60ml/min1,3
Chronic Kidney
Disease Stage 4
(GFR 15-29)3
GFR<30ml/min2
Chronic Kidney
Disease Stage 53
Haemodialysis
Upon commencement
Chronic Kidney
Disease Stage 53
Peritoneal Dialysis
Upon commencement
45-60 mins4
45-60 mins4
45-60 mins8
45-60 mins8
Alb3, K4, PO4,4 cr4,
bld glucose &
HbA1c(for persons
with diabetes) 4,
PTH12, BP4, lipids1,
GFR4, Hb4,
medications inc
supplements4
dry wt1,3, BMI1,
%IBW/SGA3, diet
assessment/nPNA1,3,
activity level and
limitations4
Alb2, K4, PO44, cr4,
bld glucose &
HbA1c(for persons
with diabetes)4,
PTH12, BP4, lipids1,
GFR4, Hb4,
medications inc
supplements4,
dry wt1,2, BMI1,
%IBW/SGA2, diet
assessment/nPNA1,2,
activity level and
limitations4
Pre dial: Alb1,2, urea1,
K8, PO41, CaxPO41,
lipids11, PTH12,
Post dial: urea8 HbA1c
(if diab)8, HD freq &
fluid gains8, BP8,
medications8, Kt/V
Alb1,2, K8, PO48,
lipids11, PTH12,
CaxPO41, urea &/or
cr1, HbA1c (if diab) 8,
PD prescription &
fluid gains8, BP8,
medications8, Kt/V
Dry wt1, BMI1,
%IBW2, SGA1,2, diet
assessment1,2 or
nPNA1,2
Dry wt1, BMI1,
%IBW2, SGA1,2, diet
assessment1,2 or
nPNA1,2
Nutrition
counselling
adequate protein and
energy1,3, bld glucose
control in DM3, fluid
and Na control in
HT3, lipid1 & weight3
control, meal plan4,
self monitoring4,
physical activity4
protein and energy
intake1,2, Na, K &
fluid intake1, wt
control1,4, meal
plan4,recipe
modification, self
monitoring4, physical
activity4
individual care plan2,
adequate protein and
energy intake1, fluid
& electrolyte
management8, self
monitoring8, meal
plan8, physical
activity8
individual care plan2,
adequate protein
intake1, appropriate
energy intake1, self
monitoring8, meal
plan8, physical
activity8
Review &
frequency of
follow up
Dry wt & BMI
monthly1, 20-30 min4
r/v every 6-12 months
if no evidence of
malnutrition, more
frequently if
malnourished3
Dry wt & BMI
monthly1, 20-30 min4
r/v every 1-3
months1, more
frequently if
inadequate intake,
concomitant illness,
GFR < 15 or
malnourished2; SGA
every 6-12 months1
Dry wt, BMI & alb
monthly1, 45-60 min8
r/v every 3-6 months
inc nPNA, Kt/V, diet
assessment & SGA1,
more frequently if
clinically indicated1
Dry wt, BMI & alb
monthly1, 45-60 min8
r/v every 6 months
inc nPNA, Kt/V, diet
assessment & SGA1,
more frequently if
clinically indicated1
Point of
referral
Time for
consultation
Biochemistry
and Clinical
Nutrition
assessment
References
The CARI Guidelines (Caring for Australians with Renal Impairment). 2003. Australian Kidney Foundation & Australia New Zealand Society
of Nephrology.
2.
Clinical practice guidelines for nutrition in chronic renal failure. K/DOQI, National Kidney Foundation. 2000. American Journal of Kidney
Diseases, 35 (supp 2), s1-s140.
3.
National Kidney Foundation Kidney Disease Outcome Quality Initiative (K/DOQI) Advisory Board. 2002. K/DOQI clinical practice guidelines
for chronic kidney disease: evaluation, classification and stratification. American Journal of Kidney Diseases, 39 (supp 2), s1-s246.
4.
American Dietetic Association. 2002. Medical Nutrition Therapy Evidence-Based Guides for Practice: Chronic Kidney Disease (nondialysis) Medical Nutrition Therapy Protocol. Chicago: American Dietetic Association.
5.
National Physical Activity Guidelines for Australians. 1999. Canberra: Australian Department of Health and Ageing.
6.
European Guidelines for the Nutritional Care of Adult Renal Patients. 2003. European Dialysis and Transplantation Nurses Association/
European Renal Care Association (Edtna/Erca) Journal, 29(1), s1-s23.
7.
Lowrie, EG & Lew, NL. 1990. Death risk in haemodialysis patients: the predictive value of commonly measured variables and an evaluation of
death rate differences between facilities. American Journal of Kidney Diseases, 15, 458-482.
8.
Wiggins, K.L. 2002. Guidelines for Nutritional Care of Renal Patients (3rd ed). Renal Dietitians Dietetic Practice Group, American Dietetic
Association. Chicago: American Dietetic Association.
9.
NKF-K/DOQI clinical practice guidelines for hemodialysis adequacy: update 2000. 2001. American Journal of Kidney Diseases, 37 (supp
1), s7-s64.
10. NKF-K/DOQI clinical practice guidelines for peritoneal dialysis adequacy: update 2000. 2001. American Journal of Kidney Diseases, 37
(supp 1), s65-s136.
11. K/DOQI Clinical Practice Guidelines for Managing Dyslipidemias in Chronic Kidney Disease. 2003. American Journal of Kidney Diseases,
41(supp 3), s1 s79.
12. K/DOQI Clinical Practice Guidelines for bone metabolism and disease in chronic kidney disease. American Journal of Kidney Disease, 42(4),
S7 S169.
1.
Australia & New Zealand Renal Guidelines Taskforce
23
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Appendix 2: Summary of Recommendations for Nutrition Prescription in Chronic
Kidney Disease
CKD Stage 3
GFR 59-30ml/min
CKD Stage 4
GFR <30ml/min
CKD Stage 5
Haemodialysis
CKD Stage 5
Peritoneal Dialysis
Biochemistry
& Clinical
monitor creat &
GFR3; normal alb,
K+ & PO44, normal
TG & chol1; HbA1c
<7%4; goal BP4
monitor creat &
GFR3; normal alb,
K+ & PO44, normal
TG & chol1; HbA1c
<7%4; goal BP4
stabilise urea &
creatinine1; norm
alb1; norm lipids11, K
3.5 -5.58; PO4< 2.21;
HbA1c <7%8
Energy
Ideal for age, gender,
BMI and phys
activity level1
At least 146kJ/kg
IBW (BMI 18.5-25)
1
, 125-146kJ/kg IBW
>60 yr2
Protein
0.75-1.0g/kg
IBW/day1
0.75-1.0g/kg IBW1
with adequate kJ
intake1
>50% HBV1
Pre dial: urea 21-397;
K+<5.58; PO4 <2.21;
norm alb1, norm
lipids11
Post dial: urea >65%
reduction8;
HbA1c < 7%8
125-146kJ/kg IBW
(BMI 22-25)1
acute illness:
>146kJ/kg IBW if
<60yr 2, >125kJ
/kg IBW if > 60yr2
1.2-1.4g/kg IBW1
>50% HBV2
acute illness: > 1.2 g
/kg IBW2
Sodium
<100mmol if
hypertensive and
CKD is progressive1
<100mmol if
hypertensive and
CKD is progressive1
80 110 mmol/day6
Potassium
Not usually
restricted, If K+ > 6.0
limit intake1 to
1mmol/kg IBW/ day
If K+>6.0 limit
intake1 to 1mmol/ kg
IBW/day (ANZRGT)
1mmol/kg IBW/day8
if >1.49 mmol/L, (or
>target PTH) restrict
to 800-1000mg/day
(adj for protein) &/or
binders 12
Individualised based
on CKD, oedema and
hypertension1
if >1.78 mmol/L, (or
>target PTH) restrict
to 800-1000mg/day
(adj protein) &/or
binders 12
500ml + PDUO6
146kJ (35kcal)/kg
IBW (BMI 22-25)1
inc glucose from
dialysate8
acute illness: >146
kJ/kg IBW /day2
min 1.2g/kg IBW1;
>50% HBV2
acute illness: >1.3g
/kgIBW2; peritonitis:
1.5g/kg IBW6
Indiv treatment
recommended, if
restricted 80-110
mmol/day6
Indiv treatment
recommended, if
restricted 1mmol/ kg
IBW/day (ANZRGT)
(ANZRGT)
Phosphate
Fluid
if >1.49 mmol/L, (or
>target PTH) restrict
to 800-1000mg/day
(adj for protein) &/or
binders 12
Individualised based
on CKD, oedema and
hypertension1
if >1.78 mmol/L, (or
>target PTH) restrict
to 800-1000mg/day
(adj for protein) &/or
binders 12
Indiv treatment
recommended, if
fluid overloaded or
hypertensive: 800ml
+ PDUO6
References
The CARI Guidelines (Caring for Australians with Renal Impairment). 2003. Australian Kidney Foundation & Australia New Zealand Society
of Nephrology.
2.
Clinical practice guidelines for nutrition in chronic renal failure. K/DOQI, National Kidney Foundation. 2000. American Journal of Kidney
Diseases, 35 (supp 2), s1-s140.
3.
National Kidney Foundation Kidney Disease Outcome Quality Initiative (K/DOQI) Advisory Board. 2002. K/DOQI clinical practice guidelines
for chronic kidney disease: evaluation, classification and stratification. American Journal of Kidney Diseases, 39 (supp 2), s1-s246.
4.
American Dietetic Association. 2002. Medical Nutrition Therapy Evidence-Based Guides for Practice: Chronic Kidney Disease (nondialysis) Medical Nutrition Therapy Protocol. Chicago: American Dietetic Association.
5.
National Physical Activity Guidelines for Australians. 1999. Canberra: Australian Department of Health and Ageing.
6.
European Guidelines for the Nutritional Care of Adult Renal Patients. 2003. European Dialysis and Transplantation Nurses Association/
European Renal Care Association (Edtna/Erca) Journal, 29(1), s1-s23.
7.
Lowrie, EG & Lew, NL. 1990. Death risk in haemodialysis patients: the predictive value of commonly measured variables and an evaluation of
death rate differences between facilities. American Journal of Kidney Diseases, 15, 458-482.
8.
Wiggins, K.L. 2002. Guidelines for Nutritional Care of Renal Patients (3rd ed). Renal Dietitians Dietetic Practice Group, American Dietetic
Association. Chicago: American Dietetic Association.
9.
NKF-K/DOQI clinical practice guidelines for hemodialysis adequacy: update 2000. 2001. American Journal of Kidney Diseases, 37 (supp
1), s7-s64.
10. NKF-K/DOQI clinical practice guidelines for peritoneal dialysis adequacy: update 2000. 2001. American Journal of Kidney Diseases, 37
(sup 1), s65-s136.
11. K/DOQI Clinical Practice Guidelines for Managing Dyslipidemias in Chronic Kidney Disease. 2003. American Journal of Kidney Diseases,
41 (supp 3), s1 s79.
12. K/DOQI Clinical Practice Guidelines for bone metabolism and disease in chronic kidney disease. American Journal of Kidney Disease, 42(4),
S7 S169.
1.
Australia & New Zealand Renal Guidelines Taskforce
24
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Appendix 3: Descriptions of levels of evidence cited from original sources
Source
American Dietetic Association
Medical Nutrition Therapy
Evidence-Based Guides for
Practice: Chronic Kidney Disease
(non-dialysis) Medical Nutrition
Therapy Protocol
The CARI Guidelines
K/DOQI Clinical practice
guidelines for chronic kidney
disease 2000, 2001, 2003
K/DOQI Clinical practice
guidelines for chronic kidney
disease: evaluation, classification
and stratification 2002
Guidelines for Nutritional Care of
Renal Patients (3rd ed)
European Guidelines for the
Nutritional Care of Adult Renal
Patients
Description
Grade I The evidence consists of results from studies of strong design
for answering the questions addressed. The results are both clinically
important and consistent with minor exceptions at most. The results
are free of serious doubts about generalisability, bias, and flaws in
research design. Studies with negative results have sufficiently large
samples to adequate statistical power.
Grade II The evidence consists of results from studies of strong
design for answering the questions addressed, but there is uncertainty
attached to the conclusion because of inconsistencies among the
results for different studies or because of doubts about
generalisability, bias, research design flaws or adequacy of sample
size. Alternatively, the evidence consists solely of studies from
weaker designs for the questions addressed, but the results have been
confirmed in separate studies and are consistent with minor
exceptions at most.
Grade III The evidence consists of results from limited studies of
weak design for answering the questions addressed. Evidence from
studies of strong design is either unavailable because no studies of
strong design have been done or because the studies that have been
done are inconclusive due to lack of generalisability, bias, design
flaws or inadequate sample sizes.
Grade IV The support of the conclusion consists solely of the
statements of informed medical commentators based on their clinical
experience, unsubstantiated by the results of any research studies.
Level A Randomised controlled trials and meta analyses
Level B Descriptive Studies
Level C Consensus or opinion
A rating of "evidence" was defined as "mainly convincing scientific
evidence, limited added opinion";
"Opinion" was defined as "mainly opinion, limited scientific
evidence";
"Evidence and Opinion" was defined as "about equal mixtures of
scientific evidence and opinion."
S Analysis of individual patient data from a single large, generalisable
study of high methodological quality (for example NHANES III)
C Compilation of original articles into evidence tables
R Review of reviews and selected original articles
O Opinion
No levels of evidence or opinion provided
Examination of the scientific literature shows a paucity of evidence
on dietary advice in renal failure. Therefore the guidelines are based
on scientific evidence, where available, and on a consensus of what
constitutes best practice where not.
Appendix 4: Stages of Chronic Kidney Disease
Stage
Description
GFR (mL/min/1.73m2)
1
Kidney damage with normal or GFR
90
2
60-89
Kidney damage with mild GFR
3
30-59
Moderate GFR
4
15-29
Severe GFR
5
Kidney failure
< 15 (or dialysis)
Chronic kidney disease is defined as either kidney damage or GFR 60 mL/min/1.73m2 for 3 months. Kidney
damage is defined as pathologic abnormalities or markers of damage, including abnormalities in blood or urine tests or
imaging studies (K/DOQI 2002).
Australia & New Zealand Renal Guidelines Taskforce
25
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Appendix 5: Calculations
1. GFR
Cockcroft-Gralt Formula for estimating creatinine clearance / GFR
GFR (ml/min) = (140 - age in years) x weight in kg
814 x serum creatinine in mmol/L
Multiply by 0.85 for women
GFR should be corrected for body surface area (BSA).
BSA may be calculated by the Du Bois formula
BSA = 0.007184 x [height (cm)]0.725 x [weight (kg)]0.425 (Du Bois and Du Bois 1916).
Use GFR rather than creatinine levels or other measures of renal impairment in referral criteria and assessment of
patients for the following reasons:
this is the measure used to define the stages of kidney disease
this is used by all nephrologists
it is the measure used in all referenced guidelines
it does account for age, weight and renal function
2.
Prediction Equations for BIA and DEXA
BIA
Use Kushner formula for calculation of total body water (TBW)
Males:
TBW=8.399+0.396(H2/R) + (0.143W)
Females:
TBW=8.315+0.382(H2/R) +(0.105W)
R is resistance in ohms
H is the Height in cm
W is the weight in kg
Kushner, R.F. & Schoeller, D.A. 1986. Estimation of total body water by bioelectrical impedance analysis. Am J Clin Nutr 44:417-424.
DEXA
Use Lukaski formula for fat free mass (FFM) which is roughly equivalent to lean body mass (LBM)
FFM = -4.03+(0.734H2/R) +(0.116W) +(0.096Xc) +(0.878 x 1 for males or 0 for females)
Xc= compacitents
Lukaski, H. C., Bolonchuk, W. W., Hall, C. B. & Siders, W.A. 1986. Validation of tetrapolar bioelectrical impedance method to assess human body
composition. J Appl Physiol 60:1327-1332.
3.
Calculation of normalised protein nitrogen appearance (nPNA) (adapted from The CARI Guidelines)
Chronic renal failure
nPNA may be approximated by the Randerson formula
nPNA (g/kg/day) = [[urea excretion (mmol/day) x 0.209] + 15.71] weight (kg) (Kopple et al 1993 in CARI).
Peritoneal dialysis
Given that daily changes in body nitrogen are usually negligible in stable patients on peritoneal dialysis, the UNA is
usually represented as the sum of dialysate and urinary losses. The protein equivalent of total nitrogen appearance
(PNA) expresses the nitrogen appearance in terms of protein.
PNA (grams of protein/24hrs) = TNA (grams of nitrogen/24 hrs) x 6.25.
Because of the constant relationship between the measured UNA and the total nitrogen appearance, the protein
equivalent of total nitrogen appearance (PNA) is determined from the UNA, or from the urea appearance (UA) by the
following formulae [13 in 1].
PNA (g/day) = 20.1 + 7.5 x UNA (g/24 hrs)
or
PNA (g/day) = 20.1 + 0.209 x UA (mmol/24 hrs)
Several alternative equations have been derived to calculate the PNA in CAPD patients. Comparisons performed by
Keshaviah and Nolph [14 in 1] have shown that all equations correlate closely with each other and do not show any
Australia & New Zealand Renal Guidelines Taskforce
26
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
significant difference to the measured protein intake. However, if dialysate protein loss is excessive (greater than 10-15
g protein per day), this needs to be additionally accounted for in making an estimate of protein intake [15 in 1]. In this
case it is recommended that the protein intake be determined from the UNA by determining the protein equivalent of
nonprotein nitrogen appearance (PNPNA), which in the individual patient, is equal to the PNA minus protein losses.
This should reflect the net protein intake under steady state conditions, i.e. the total intake of protein minus dialysate
and urinary protein losses [13 in 1]. Thus by determining the PNPNA (see below) and adding dialysate and urinary
protein loss, a more accurate estimate of the PNA may be made.
PNPNA (g/day) = 15.1+ 6.95 x UNA (g/24 hrs)
or
PNPNA(g/day)=15.1+0.195xUA (mmol/24 hrs)
The terminology is often loosely applied, so that the terms used in applying urea kinetic modelling to nutrition in CAPD
have recently been redefined [16 in 1]. For practical purposes the PNA can be substituted for the older terminology
referring to it as the protein catabolic rate or PCR. Studies assessing the benefits of the kinetically derived protein intake
suggest that relaying the information back to the patient results in an improved compliance with dietary
recommendations [17 in 1].
Haemodialysis
The methods used to determine the PNA differ in the HD and PD population, The most widely used method calculates
the urea generation rate from the end of the first dialysis to/the beginning of the second dialysis and relies
predominantly on the difference between the post and pre dialysis urea values .
Several methods are used to calculate the urea generation rate from which the PNA are calculated.
PNA = UGR (g/24 hrs) + 1.7 + Urinary protein losses
0.154
UGR
UGR (g/24 hrs) = Urea (mmol/24 hrs) x 0.028
(mmol/24 hrs) =
- V2C2 - V3C3 x 24
interdialytic time (hrs)
V2 C2 = Vdurea and concentration of urea post dialysis
V3 C3 = Vdurea and concentration of urea pre dialysis.
Note: In all cases urinary urea and protein losses need to be measured and included in the calculations used to
estimate protein intake.
Australia & New Zealand Renal Guidelines Taskforce
27
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Appendix 6: BMI Ranges
Suggested table of BMI
ranges
Underweight
Healthy
Overweight
Obese
Pre-Dialysis
<18.5
20-25
25-30
>30
Dialysis (Haemodialysis,
Peritoneal Dialysis)
<18.5
23-26
26-32
>32
The Council for Renal Nutrition (American Kidney Foundation) recommend an ideal body weight of BMI 20-25 for
pre-dialysis patients and BMI 23-26 for dialysis patients. They do not address ethnicities or age groups in defining
these levels.
Calculation of Ideal Body Weight (IBW)
Aim for weight to be within BMI of 20-25 if GFR 15-59 and a BMI of 23-26 on a dialysis modality. A patients ideal
body weight can be adjusted (as per the equation below), particularly if a patient is obese BMI>30.
Adjusted Body Weight = [(Actual Weight Ideal Weight) x 0.25] + Ideal Body Weight (IBW).
When to use actual or adjusted body weight:
1. Use actual body weight (dry weight for dialysis patients) when:
Weight is within reasonable range of ideal or standard body weight (recommended BMI range).
Recent weight change has not occurred.
The patient is not malnourished.
The patient has been slightly overweight or underweight almost all of their lives.
2. Use adjusted body weight when patients are overweight/obese, using clinical judgement.
Kopple, J.D., 2002, Rocket Guide to Nutritional Assessment of the Patient with Chronic Kidney Disease 3rd Ed, Lippincott Williams & Wikins,
Philadelphia
Koople, J.D., Zhu, X., Lew, N.L., Lowrie, E.G., 1999. Body weight for height relationships predict mortality in maintenance haemodialysis patients
Kidny Int 56:1136-1148.
Mitch, WE., Klahr, S., 2002, Handbook of Nutrition and the Kidney, 4th Ed, Lippincott Williams & Wikins, Philadelphia
Australia & New Zealand Renal Guidelines Taskforce
28
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Appendix 7: Malnutrition Screening Tool
Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Ferguson
M, Capra S, Bauer J and Banks M. Nutrition 15:458-464. 1999
Have you lost weight recently without trying?
No
Unsure
Yes
see below
If yes, how much weight (kg) have you lost?
1.0 5.0
6.0 10.0
11.0 15.0
> 15.0
No
Yes
Have you been eating poorly because of a decreased appetite?
Total Score :
IF THE TOTAL SCORE IS 2 OR MORE, PATIENT IS AT RISK OF MALNUTRITION
Australia & New Zealand Renal Guidelines Taskforce
29
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Appendix 8: Subjective Global Assessment
Name:
Date:
A
Medical History
WEIGHT
Wt change past 6 months
0-<5% loss
5-10% loss
>10% loss
Usual weight.
Amount weight loss....
Current weight...
% weight loss.
*
*
*
Amount.
Weight change past 2 weeks
No change; normal weight
Increase to within 5%
Increase (1 level above)
No change, but below usual wt
Increase to within 5-10%
Decrease
*
*
*
*
*
*
*
DIETARY INTAKE
No change; adequate
No change; inadequate
*
*
Duration of change...
Change
Suboptimal diet
Full liquid
Hypocaloric liquid
Starvation
*
*
*
*
Intake borderline; increasing
Intake borderline; decreasing
Intake poor; no change
Intake poor; increasing
Intake poor decreasing
*
*
*
*
*
*
GASTROINTESTINAL SYMPTOMS
Frequency (never, daily, no. of times/week)
Nausea
Vomiting
Diarrhoea
Anorexia
Duration (<2wk, >2wk)
..
..
...
...
None; intermittent
Some (daily >2 week)
All (daily >2 week)
*
*
*
FUNCTIONAL
CAPACITY
No dysfunction
Difficulty with ambulation/normal activities
Bed/chair-ridden
Duration of change ..
Change past 2 week
Improved
No change
Regressed
*
*
*
*
*
*
Australia & New Zealand Renal Guidelines Taskforce
30
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Physical examination
SUBCUTANEOUS FAT
Under the eyes
Slightly bulging area
Triceps
Large space between
fingers
Biceps
Large space between
fingers
MUSCLE WASTING
Temple
Well-defined
muscle/flat
Not visible in Males;
may be visible but not
prominent in females
Rounded
Clavicle
Shoulder
Scapula/ribs
Calf
Bones not prominent;
no significant
depressions
Well rounded; no
depressions
Well developed
Knee
Bones not prominent
Quadriceps
Hollowed look,
depression, dark circles
Very little space
between fingers, or
fingers touch
Very little space
between fingers, or
fingers touch
Slight depression
Hollowing, depression
Some protrusion; may
not be all the way along
Protruding/prominent
bone
No square look;
acromion process may
protrude slightly
Mild depressions or
bone may show
slightly; not all areas
Mild depression
Square look; bones
prominent
Bones prominent;
significant depressions
Depression; thin
Thin; no muscle
definition
Bones prominent
Interosseous muscle between thumb
and forefinger
Muscle protrudes;
could be flat in females
OEDEMA (related to malnutrition)
No sign
Mild to moderate
Severe
ASCITES (related to malnutrition)
No sign
Mild to moderate
Severe
OVERALL SGA RATING
Flat or depressed area
Adapted from: Detsky et al., 19948; Baxter Healthcare Corporation, 1993; McCann, 1996
(Ferguson, Bauer, Banks, Capra, 1996)
Australia & New Zealand Renal Guidelines Taskforce
31
Evidence Based Practice Guidelines for the Nutritional Management of Chronic Kidney Disease
Appendix 9: Glossary
Adult: any person over the age of 18
BIA: Bio-electrical impedance analysis is a method of measuring body composition based on the difference in
conductivity of body fat and fat-free tissue.
Body weight: use dry, oedema-free, post dialysis or non-dwelling body weight for all calculations
DEXA: Dual x-ray absorptiometry is a method of measuring body composition using x-ray technology.
Kt/V: Kt/V is a measure of dialysis adequacy. K is the urea clearance of the dialyser, t is the time between drawings of
blood (in minutes) and V is the patients total body water volume. Kt/V is regularly calculated for al dialysis patients.
This measure can be adversely affected by many patient related or dialysis associated variables.
nPNA: Normalised Protein equivalent of Total Nitrogen Appearance normalised to ideal body weight. See Appendix 6
to calculate nPNA.
Urea Reduction Ratio (URR): A method used to calculate adequacy of haemodialysis is the urea reduction ratio,
where adequate dialysis is a reduction of 65% or more between the pre and post dialysis serum urea values.
Australia & New Zealand Renal Guidelines Taskforce
32
Anda mungkin juga menyukai
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Who Iycf Questionnaire Guidelines PDFDokumen91 halamanWho Iycf Questionnaire Guidelines PDFStefania WidyaBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Antro Anak PDFDokumen21 halamanAntro Anak PDFStefania WidyaBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- WHO Child Growth Standards Idi SAMDokumen12 halamanWHO Child Growth Standards Idi SAMShivalkar Reddy VanchaBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Acend 2017Dokumen18 halamanAcend 2017Stefania WidyaBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Weight Loss PerceptionDokumen8 halamanWeight Loss PerceptionStefania WidyaBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Antro Anak PDFDokumen21 halamanAntro Anak PDFStefania WidyaBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Leptin N GhrelinDokumen14 halamanLeptin N GhrelinStefania WidyaBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- In Vitro Fluoride Toxicity in Human Spermatozoa - Reproductive Toxicology, Vol. 8, No. 2, Pp. 155-159, 1994 PDFDokumen5 halamanIn Vitro Fluoride Toxicity in Human Spermatozoa - Reproductive Toxicology, Vol. 8, No. 2, Pp. 155-159, 1994 PDFStefania WidyaBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Bmi Asia Strategies PDFDokumen7 halamanBmi Asia Strategies PDFHevi NetyaBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Food and Nutrition in EmergencyDokumen44 halamanFood and Nutrition in EmergencyStefania WidyaBelum ada peringkat
- In Vitro Fluoride Toxicity in Human Spermatozoa - Reproductive Toxicology, Vol. 8, No. 2, Pp. 155-159, 1994 PDFDokumen5 halamanIn Vitro Fluoride Toxicity in Human Spermatozoa - Reproductive Toxicology, Vol. 8, No. 2, Pp. 155-159, 1994 PDFStefania WidyaBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Pancreatic PolypeptideDokumen5 halamanPancreatic PolypeptideStefania WidyaBelum ada peringkat
- The Mayo Clinic Diet by Mayo Clinic PDFDokumen7.690 halamanThe Mayo Clinic Diet by Mayo Clinic PDFStefania Widya0% (4)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Food Culture in Southeast AsiaDokumen173 halamanFood Culture in Southeast Asiacekrik100% (3)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Must FullDokumen6 halamanMust FullStefania WidyaBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Manual For Charge NursesDokumen99 halamanManual For Charge NursesHazelina Villamor100% (1)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Beltran - Diagnostic Challenges Musculoskeletal RadiologyDokumen181 halamanBeltran - Diagnostic Challenges Musculoskeletal RadiologyAndrei GianinaBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Solving Math Word Problems: Steps Tips For Success ExampleDokumen3 halamanSolving Math Word Problems: Steps Tips For Success ExampleDhiman NathBelum ada peringkat
- BleedingDokumen14 halamanBleedingRhomizal MazaliBelum ada peringkat
- Alice Final Draft EthicsDokumen8 halamanAlice Final Draft Ethicsapi-254093121Belum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- 2 Marks Q & ADokumen11 halaman2 Marks Q & AJayaprakash JayaramanBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Sydney M PRPDokumen23 halamanSydney M PRPapi-465406877Belum ada peringkat
- OD Diagnosis: J. Michael Sammanasu JIMDokumen34 halamanOD Diagnosis: J. Michael Sammanasu JIMCorina IcaBelum ada peringkat
- In-Patient Claim Form - ConventionalDokumen2 halamanIn-Patient Claim Form - ConventionalAbdul Qayyum Sipra Madduki50% (2)
- Acs Nstemi PathwayDokumen3 halamanAcs Nstemi PathwayAliey's SKeplek NgeNersBelum ada peringkat
- UNIMA72 ProjectDokumen10 halamanUNIMA72 ProjectJan KowalskiBelum ada peringkat
- Recurrent Pregnancy LossDokumen40 halamanRecurrent Pregnancy LossJagannath MaaleBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Annexure C: Medical and Dental Professions BoardDokumen2 halamanAnnexure C: Medical and Dental Professions BoardK ValdesBelum ada peringkat
- Implant FailureDokumen6 halamanImplant FailureNajeeb UllahBelum ada peringkat
- Bioethics Unit IiiDokumen4 halamanBioethics Unit IiiShannel J. DabalosBelum ada peringkat
- Legalizing MarijuanaDokumen3 halamanLegalizing MarijuanaAlyssa MabalotBelum ada peringkat
- Practical Manual On Veterinary Clinical Diagnostic Approach 2157 7579 1000337Dokumen10 halamanPractical Manual On Veterinary Clinical Diagnostic Approach 2157 7579 1000337Shravankumar Gaddi100% (1)
- 20th Century NurseDokumen5 halaman20th Century NurseMisch Yeen100% (1)
- Health Education - Quiz 1 Midterms Summer 2012-2013Dokumen8 halamanHealth Education - Quiz 1 Midterms Summer 2012-2013Lizette Leah Ching100% (1)
- SurveillanceDokumen64 halamanSurveillancePalwasha KhanBelum ada peringkat
- Nxlex 6Dokumen50 halamanNxlex 6Arvin CamposBelum ada peringkat
- NCP 1Dokumen3 halamanNCP 1itsmeayaBelum ada peringkat
- 1978 Caramazza Berndt PBDokumen21 halaman1978 Caramazza Berndt PBEddiesvoiceBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Ubat Bah Ini :)Dokumen172 halamanUbat Bah Ini :)Eckry SilverBelum ada peringkat
- Lung AbscessDokumen2 halamanLung Abscessoxidalaj100% (1)
- 1) CORRECT - Assess For Patency of The NG Tube Muscle Spasms Associated With VomitingDokumen39 halaman1) CORRECT - Assess For Patency of The NG Tube Muscle Spasms Associated With VomitingJujuBelum ada peringkat
- Nursing Care Plan For Postpartum HemorrhageDokumen2 halamanNursing Care Plan For Postpartum HemorrhageDianne Mae100% (1)
- Comprehensive Healthcare Simulation. Grant and Cheng.Dokumen417 halamanComprehensive Healthcare Simulation. Grant and Cheng.charlsandroid01Belum ada peringkat
- Post Depravity by SupervertDokumen250 halamanPost Depravity by SupervertJeremy VaughnBelum ada peringkat
- Final SPR 10 Student SyllabusDokumen61 halamanFinal SPR 10 Student SyllabusHilux23Belum ada peringkat
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDari EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedPenilaian: 5 dari 5 bintang5/5 (80)