Management of Cyanide Toxicity in Patients With Burns 2015 Burns
Diunggah oleh
Patrick JohnHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Management of Cyanide Toxicity in Patients With Burns 2015 Burns
Diunggah oleh
Patrick JohnHak Cipta:
Format Tersedia
burns 41 (2015) 1824
Available online at www.sciencedirect.com
ScienceDirect
journal homepage: www.elsevier.com/locate/burns
Review
Management of cyanide toxicity in patients with
burns
Louise MacLennan *, Naiem Moiemen
UK Healing Foundation Centre for Burns Research, Queen Elizabeth Hospital Birmingham, Birmingham, UK
article info
abstract
Article history:
The importance of cyanide toxicity as a component of inhalational injury in patients with
Accepted 4 June 2014
burns is increasingly being recognised, and its prompt recognition and management is vital
Keywords:
by a lack of randomised controlled trials in humans, and in addition consideration must be
Cyanide
given to the concomitant pathophysiological processes in patients with burns when inter-
for optimising burns survival. The evidence base for the use of cyanide antidotes is limited
Inhalation injury
preting the literature. We present a literature review of the evidence base for cyanide
Burns
antidotes with interpretation in the context of patients with burns. We conclude that
Hydroxycobalamin
hydroxycobalamin should be utilised as the first-line antidote of choice in patients with
Sodium thiosulphate
burns with inhalational injury where features consistent with cyanide toxicity are present.
# 2014 Elsevier Ltd and ISBI. All rights reserved.
Sodium nitrite
Dicobalt edetate
Contents
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
Introduction . . . . . . . . . . . . . . . . . . . .
Methods . . . . . . . . . . . . . . . . . . . . . . .
Biochemistry . . . . . . . . . . . . . . . . . . .
Clinical features and diagnosis . . . . .
Management . . . . . . . . . . . . . . . . . . .
Hydroxycobalamin. . . . . . . . . . . . . . .
Sodium thiosulphate . . . . . . . . . . . . .
Sodium nitrite, amyl nitrite, 4DMAP .
Dicobalt edetate . . . . . . . . . . . . . . . . .
Choice of antidote . . . . . . . . . . . . . . .
Discussion . . . . . . . . . . . . . . . . . . . . .
Conclusion . . . . . . . . . . . . . . . . . . . . .
References . . . . . . . . . . . . . . . . . . . . .
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
19
19
19
19
19
20
20
21
21
21
22
22
23
* Corresponding author at: UK Healing Foundation Centre for Burns Research, Queen Elizabeth Hospital Birmingham, Mindelsohn Way,
Edgbaston, Birmingham B15 2WB, United Kingdom. Tel.: +44 7738 399472.
E-mail address: leamaclennan@gmail.com (L. MacLennan).
http://dx.doi.org/10.1016/j.burns.2014.06.001
0305-4179/# 2014 Elsevier Ltd and ISBI. All rights reserved.
burns 41 (2015) 1824
1.
Introduction
Inhalational injury is one of the major predictors of mortality
in patients with burns [1], and is estimated to be present in
2030% of patients with burns who undergo hospitalisation [2].
Advances in fluid resuscitation, surgery and antibiotics have
improved the management of burn shock and sepsis [3], with
fire and burn mortality in the USA dropping from 3.0 to 1.2 per
100,000 population in the 25-year period from 1981 to 2006 [4].
However, the management of inhalational injury remains one
of the greatest challenges of burn care, and its presence is
reported to double the mortality by burn [5,6].
Inhalation injury comprises direct thermal injury, chemical
irritation of lung parenchyma and the systemic effects of
absorption of the toxic products of combustion, such as carbon
monoxide and cyanide. There is increasing evidence that
cyanide toxicity plays an important role in smoke inhalation
injury and its associated mortality [79], with smoke inhalation reportedly the most common cause of cyanide toxicity
[10,11]. It is difficult to accurately determine the true incidence
of cyanide toxicity due to smoke inhalation as blood cyanide
levels are often not measured; however, it has been reported to
have been found in as many as 76% of patients with smoke
inhalation injury [9]. This paper aims to appraise the evidence
base for the pharmacological management of cyanide toxicity
in the context of smoke inhalation and burn injuries, in order
to guide management in this clinical setting.
2.
Methods
A search of Medline (1950June 2013), EMBASE (1980June
2013) and CINAHL (1981June 2013) databases was undertaken
using the NHS Evidence Interface. The search terms cyanide
plus smoke inhalation, and also cyanide plus either
hydroxycobalamin, sodium thiosulphate, nitrite, or dicobalt edetate were used.
3.
Biochemistry
Cyanide refers to any substance that contains the cyano (CN)
group. This includes inorganic cyanides with a negatively
charged cyanide ion, such as sodium cyanide, and organic
cyanides with a covalent CN group such as methyl cyanide.
Inorganic cyanides are salts of hydrocyanic acid, also known
as hydrogen cyanide, and are highly toxic. Hydrogen cyanide is
a volatile liquid that forms a colourless gas at 26 8C and has a
distinctive odour of bitter almonds; however, 2040% of people
are genetically unable to detect this [12,13]. Cyanide compounds are used in the production of acrylic, rubber and
plastic; for industrial processes including electroplating, steel
production and metal extraction from ores; and for fumigation. In smoke inhalation injury, cyanide toxicity is thought to
occur from exposure to the products of combustion of those
cyanide-containing synthetic substances.
Cyanide acts by binding to the ferric ions in cytochrome c
oxidase, thus inhibiting its action in the electron transport
chain in mitochondria. This disruption of the electron
19
transport chain blocks cellular aerobic respiration, which
can rapidly become fatal. Whole blood cyanide levels above
0.51.0 mg/L (1940 mmol/L) are regarded as toxic [7,9,14], and
untreated levels above 2.53 mg/L (96115 mmol/L) are potentially fatal [12,14].
Although the affinity of cyanide for ferric ions is strong, the
process is reversible. Cyanide disassociates from cytochrome
c oxidase by binding with sulphur transferred from endogenous thiosulphate by the catalyst rhodanese. The resultant
thiocyanate undergoes renal excretion. Observational studies
have shown a half-life of between 1 and 3 h [7,15].
4.
Clinical features and diagnosis
Early clinical manifestations of cyanide toxicity include those
of sympathetic activation namely tachycardia, hypertension,
palpitations, tachypnoea and anxiety, as well as nausea,
headache and dizziness. As the toxicity becomes more severe,
signs include confusion, drowsiness, seizures, bradycardia,
bradypnoea, hypotension and pulmonary oedema, progressing to loss of consciousness, fixed pupils, cardiovascular
collapse and ultimately death. The patients breath classically
smells of bitter almonds to the majority of clinicians able to
detect this odour. One study found that 67% of smoke
inhalation victims without major burns but with neurological
impairment had toxic cyanide levels above 39 mmol/L (1.0 mg/
L) [9].
Although blood cyanide concentration can be measured, it
is not of use for diagnosis in the acute setting as few
laboratories perform the assay and results cannot be obtained
rapidly. Diagnosis is therefore clinical; however, plasma
lactate has been found to correlate with the severity of
cyanide toxicity due to lactic acidosis from the prevailing
anaerobic metabolism [7,16,17]. In victims of smoke inhalation
with burns <15% total body surface area (TBSA), a plasma
lactate level >10 mmol/L (90 mg/dL) has been found to be a
sensitive indicator of cyanide toxicity suggesting blood
cyanide levels >40 mmol/L (1.0 mg/L) [7].
A panel endorsed by the European Society for Emergency
Medicine recently developed algorithms for both prehospital
and in-hospital management of possible cyanide toxicity in
smoke inhalation. Empiric antidotal treatment was recommended in the prehospital setting for those with a history of
smoke inhalation and either a Glasgow Coma Scale (GCS) <14
or abnormal haemodynamics; and in the hospital setting for
those with a history of smoke inhalation and a lactate above
90 mg/dL (10 mmol/L) [18].
5.
Management
Management of cyanide toxicity in patients with burns with
smoke inhalation injury includes both supportive measures
and specific antidotes. Supportive measures include high-flow
oxygen, monitoring of vital signs including cardiac monitoring, circulatory support, mechanical ventilation and correction of metabolic acidosis with sodium bicarbonate.
Hyperbaric oxygen has been advocated as a potential adjunct
for cyanide toxicity; however, the evidence for its efficacy in
20
burns 41 (2015) 1824
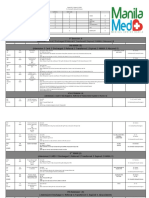
Table 1 Cyanide antidote properties.
Antidote
Mechanism of action
Hydroxycobalamin
Binds cyanide directly
5 g IV over 15 min
Sodium thiosulphate
Upregulates bodys
natural excretion
mechanism of forming
thiocyanate
Convert haemoglobin to
methaemoglobin which
binds cyanide
12.5 g IV over 10 min
Sodium nitrite, Amyl
nitrite, 4DMAP
Dicobalt edetate
Binds cyanide directly
Dose and route
Sodium nitrite: 300 mg
IV over 520 min
Amyl nitrite: 0.3 ml
ampoules crushed and
inhaled
4DMAP: 250 mg IV over
1 min
300 mg IV over 1 min
this situation is limited and conflicting [1922]. In addition, it is
not widely available and the chamber presents a difficult
environment in which to resuscitate the patient.
Several antidotes have been postulated, with differing
mechanisms of action and variable evidence of efficacy. These
antidotes include hydroxycobalamin, sodium thiosulphate,
methaemoglobin-producing nitrites and dicobalt edetate
(Table 1).
6.
Hydroxycobalamin
Hydroxycobalamin binds cyanide by substituting a hydroxyl
group for a CN group, forming cyanocobalamin, a non-toxic
substance that can be excreted by the kidneys. It is thought a
5-g dose can bind blood cyanide levels up to 40 mmol/L (1.0 mg/
L) [23]. It also has the additional effect of scavenging nitric
oxide thus raising blood pressure, which can potentially offset
the hypotension induced by the cyanide toxicity.
Hydroxycobalamin has been shown to reduce cyanide
levels in smokers [24]. In addition, animal studies by Bebarta
[2527] and Riou [28] support the efficacy of hydroxycobalamin
in reversing the effects of cyanide toxicity in swine and rat
models.
Hydroxycobalamin has been utilised in France as the firstline antidote for cyanide toxicity for many years, and is often
administered at the scene of injury following smoke inhalation
by emergency physicians who form part of the prehospital care
team within the fire service. Fortin and Borron have published
large case series which demonstrate mean survival of 4267%
following hydroxycobalamin administration to smoke inhalation victims with presumed [29] or confirmed [9] cyanide
toxicity. Borron has shown 62% and 64% survival in patients
with blood cyanide concentration over 100 mmol/L (2.6 mg/L), a
level usually regarded as fatal, when treated with hydroxycobalamin for cyanide toxicity due to smoke inhalation [9] and
other causes [30], respectively. Fortin noted statistically
significant differences in mean hydroxycobalamin dose in
those who had cardiac arrest without recovery, cardiac arrest
with early recovery but later death and cardiac arrest with
recovery [31], and concluded that hydroxycobalamin should be
Side effects
Transient hypertension, headache,
bradycardia, skin and urine
discolouration
Nausea and vomiting, headache
Reduction in oxygen carrying capacity
of blood, vasodilation, hypotension
Anaphylaxis, hypotension, cardiac
arrhythmias; more severe in absence of
cyanide toxicity
administered presumptively and as quickly as possible when
cyanide toxicity is suspected, and in the event of cardiac arrest
the dose should be increased or repeated unless a rapid
response is observed. As there were no significant adverse
effects of hydroxycobalamin administration in any of these
case series, they conclude that hydroxycobalamin is safe to use
empirically for suspected cyanide toxicity in prehospital care.
Hydroxycobalamin has a very mild side effect profile:
transient hypertension, bradycardia, headache and skin and
urine discolouration have been documented but no major
adverse effects have been reported [9,2932].
A number of recent review articles have also concluded,
based on the limited efficacy data available, as well as the
more widely documented safety data, that hydroxycobalamin
is a safe and effective first-line antidote for cyanide toxicity
[14,18,3339].
7.
Sodium thiosulphate
Endogenous thiosulphate forms part of the bodys normal
excretion mechanism of cyanide, by transferring sulphur to
cyanide to form thiocyanate which is excreted by the kidneys,
under the action of the catalyst rhodanese. Administration of
sodium thiosulphate is thought to upregulate the bodys
natural excretion of cyanide by increasing the availability of
substrate, thus limiting toxicity. Sodium thiosulphate is
generally well tolerated with only minor side effects such as
nausea, vomiting and headache being reported [3941].
Much of the evidence in the literature assesses the efficacy
of sodium thiosulphate when given in conjunction with other
antidotes [39]. Evidence for the efficacy of sodium thiosulphate
as a sole agent is confined to case reports and animal models,
and outcomes are mixed. It has been shown to reverse the
effects of cyanide in sheep when given at triple the standard
human dose [42], and to reverse the effects of cyanide in rats at
standard human doses [43]. One study in a dog model
demonstrated reduced plasma cyanide levels compared to
the control but differences were only seen after 1 h [44]. This
apparent slow onset of action may explain why some studies
do not show clinical efficacy, as either the study period may be
burns 41 (2015) 1824
too short [45] or the severity of the cyanide toxicity so great as
to cause death before a response is seen [46].
Several literature reviews conclude that there is reasonable
evidence that sodium thiosulphate is effective in cyanide
toxicity [37,38,40]; however, the slower onset of action
compared to other antidotes is also generally accepted [37
40,47]. Considering the rapid half-life of cyanide, it is postulated
that in the period prior to the onset of action of sodium
thiosulphate the cyanide would either prove fatal or reduce to
non-critical concentrations; thus, this slow onset of action
limits the usefulness of sodium thiosulphate as an antidote for
the acute cyanide toxicity seen in smoke inhalation.
8.
Sodium nitrite, amyl nitrite, 4DMAP
Nitrites such as sodium nitrite or amyl nitrite oxidise iron in
haemoglobin from ferrous to ferric iron, forming methaemoglobin. 4-dimethylaminopyridine (4DMAP) works by a similar
mechanism via methaemoglobin. Oxygen cannot bind to the
ferric iron in methaemoglobin, but cyanide binds preferentially with methaemoglobin over cytochrome c oxidase,
forming cyanmethaemoglobin, thus releasing cytochrome c
oxidase so that aerobic metabolism can resume.
Nitrites have been used as a cyanide antidote since their
efficacy was demonstrated in animal models in the 1930s [48
52]. These studies popularised a regime of amyl nitrite and
sodium nitrite given together with sodium thiosulphate.
However, 2030% of haemoglobin needs to be converted to
methaemoglobin for adequate efficacy [47], which has an
adverse effect on the oxygen carrying capacity of blood,
making this an unsafe choice in patients with smoke
inhalation injury who may also have concurrent carbon
monoxide toxicity [14,37,39,53]. In addition, nitrites cause
vasodilation and consequently hypotension which can worsen circulatory stability [53,54], a side effect which could be
particularly dangerous in patients with major burns.
9.
Dicobalt edetate
Dicobalt edetate also acts by binding cyanide, and it has been
used as a cyanide antidote for over 100 years. Once again,
evidence of efficacy is derived from animal models and case
reports [41] rather than human clinical trials. It is associated
with a number of serious side effects, including anaphylaxis,
hypotension and cardiac arrhythmias [55,56]. These side
effects may be even more pronounced if dicobalt edetate is
administered in the absence of cyanide toxicity; therefore, it is
generally recommended that it is only used as an antidote in
severe confirmed cases of cyanide toxicity [38]. In practical
terms, this precludes it from being used as a cyanide antidote
in patients with burns with smoke inhalation as cyanide
toxicity can rarely be absolutely confirmed in these cases.
10.
Choice of antidote
There are no randomised controlled human trials to evaluate
the efficacy of cyanide antidotes in the literature, only animal
21
models and case series. There are a number of factors to
account for this, including the relative rarity of cyanide
poisoning, the lack of a rapid test to confirm the presence of
cyanide toxicity and ethical issues which would prevent the
use of a placebo when cyanide toxicity is suspected. In the
absence of controlled human studies, these animal models
and case series become the only evidence on which we can
base our practice. The only randomised controlled trial in
humans in the literature is a safety study of hydroxycobalamin in healthy human subjects [32]; however, this provides no
information on efficacy.
There is evidence of efficacy in the literature for every
cyanide antidote in our review; however, not all of these
antidotes appear to be suitable in the context of smoke
inhalation injury.
Antidotes such as sodium nitrite, amyl nitrite and 4DMAP,
which act by forming methaemoglobin, reduce the oxygen
carrying capacity of blood. The coexistence of carbon
monoxide toxicity in smoke inhalation injury may also
simultaneously reduce the oxygen carrying capacity of blood,
making methaemoglobin-forming antidotes potentially dangerous in this context, and there have been reports of fatal
reductions in oxygen carrying capacity when sodium nitrite
has been given in the presence of carbon monoxide toxicity
[40,53]. In addition, we postulate that the reduction in
oxygenation of the blood in these vital first few hours post
injury could potentially have an adverse effect on coexisting
burns, and the side effect of hypotension with nitrite use could
worsen circulatory stability in patients with burn shock.
Dicobalt edetate is associated with frequent and severe side
effects such as anaphylaxis, hypotension and arrhythmias.
These side effects can be amplified when it is administered in
the absence of cyanide toxicity [57]. Consequently, its use is
usually limited to cases where cyanide toxicity has been
confirmed such as ingestion of a known cyanide-containing
substance [40]. In the context of patients with burns with
smoke inhalation, cyanide toxicity can be suspected but
cannot be definitively confirmed in the immediate resuscitation period, therefore precluding the use of dicobalt edetate as
a cyanide antidote in smoke inhalation injury.
Hydroxycobalamin and sodium thiosulphate are both
associated with a mild side-effect profile and are regarded
as safe to use in smoke inhalation patients. Sodium
thiosulphate however appears to have a slower onset of
action which may limit its usefulness as a sole agent in the
urgent reversal of severe cyanide toxicity. Sodium thiosulphate has traditionally been used in conjunction with other
more rapid acting antidotes [39,41], particularly sodium nitrite
[26], and evidence in the literature of its efficacy as a sole agent
is limited. Recent guidance on antidote availability from the
UK College of Emergency Medicine recommends that hydroxycobalamin be considered in smoke inhalation victims
showing signs associated with cyanide toxicity, and that
sodium thiosulphate generally be used as an adjuvant to other
antidotes [58].
There has been a lack of good quality comparative studies
in the literature comparing the relative efficacy of cyanide
antidotes; however, Bebarta et al. have recently published two
randomised controlled comparative studies in a swine model
[25,26]. In the first study, hydroxycobalamin with sodium
22
burns 41 (2015) 1824
thiosulphate was compared to sodium nitrite with sodium
thiosulphate, and found that hydroxycobalamin with sodium
thiosulphate reversed hypotension more rapidly but there were
no statistically significant differences in mortality, acidosis or
lactate [25]. In the second study, hydroxycobalamin, sodium
thiosulphate and hydroxycobalamin plus sodium thiosulphate
were compared, and whereas the cyanide toxicity was reversed
in the hydroxycobalamin and combined groups, all the subjects
died in the sodium thiosulphate group [26]. In addition, no
difference in outcome measures was seen in the combined
group compared to hydroxycobalamin alone. These results
suggest that hydroxycobalamin is significantly more effective
than sodium thiosulphate for cyanide toxicity, as there was a
profound difference in survival demonstrated in this model.
Clearly, the applicability of an animal model to a human
population has its limits; however, as a similar study in humans
would be ethically unfeasible, increased reliance on animal
models may be necessary. We therefore recommend that
hydroxycobalamin is used as the antidote of choice in patients
with burns with cyanide toxicity due to smoke inhalation.
11.
Discussion
It has been suggested that the low flashpoint of hydrogen
cyanide of 18 8C (0 8F), which is the lowest temperature at
which cyanide will ignite, means that most hydrogen cyanide
will combust and therefore not be present in significant levels
in smoke in a domestic fire [47]. However, the lower flammable
limit, the minimum concentration at which a substance can
ignite, is 5.6% (56,000 ppm) which is a level immensely higher
than the immediate danger to life or health value of 50 ppm
[59], suggesting that dangerous cyanide levels could still be
present before the threshold for ignition is reached. The
highest concentration of cyanide appears to occur in the first
few minutes following fire ignition [60,61], which may explain
why one study did not find dangerous exposure levels using
measuring devices attached to coats of firefighters who will
have arrived on scene after cyanide levels have dropped [62].
Studies of smoke inhalation victims measuring cyanide levels
at the fire scene have demonstrated blood cyanide levels
significantly higher than controls [7], with levels above
39 mmol/L in 67% of victims [9].
The necessity to use specific cyanide antidotes for blood
cyanide concentrations which in isolation are generally
regarded as toxic but not fatal has also been questioned
[47]. Although it may not be necessary to use antidotes in this
situation when the cyanide toxicity is an isolated injury, in the
context of a patient with burns with smoke inhalation injury
we believe that a more aggressive approach with early use of a
specific antidote is warranted. Animal studies have shown
that in the presence of concomitant major atmospheric
oxygen depletion, the fatal dose of blood cyanide was one
tenth of that expected [8]. Even if the cyanide toxicity alone is
not sufficient to be fatal, it could potentially confer a worse
outcome on a concomitant major burn injury. Optimal
perfusion of the burnt skin during the resuscitation period
can affect the survival of tissue in the zone of stasis [63]. We
postulate that the ischaemia and acidosis caused by cyanide
toxicity may reduce perfusion of the burnt tissue, and in
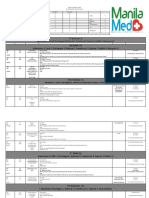
History of Smoke Inhalation
100% O2
Pre-hospital:
In hospital:
GCS < 14 and/or cardiovascular
instability
Plasma lactate > 10mmol/L
5g IV hydroxycobalamina
5g IV hydroxycobalaminb
Consider 10g dose in the event of cardiac arrest.
Further 5g dose can be given up to 10g total dose.
Fig. 1 Flowchart for assessment and management of
cyanide toxicity in patients with burns.
Source: Modified from Anseeuw et al. [18].
patients with major burns aggressive reversal of even mild
cyanide toxicity may improve burn tissue perfusion and
consequently could potentially indirectly improve survival
from the burn injury. We therefore recommend treatment
with hydroxycobalamin for any burn victim with a history of
smoke inhalation who has clinical features consistent with
cyanide toxicity (Fig. 1).
The clinical features suggestive of cyanide toxicity are
similar to those of carbon monoxide toxicity, and it is possible
that clinical features in a patient warranting empiric cyanide
antidote treatment are in fact attributable to carbon monoxide
toxicity. However, we believe the risk of treatment of cyanide
toxicity in a patient with only carbon monoxide toxicity is
outweighed by the potential benefit of early empiric treatment
for cyanide toxicity. High-flow oxygen is indicated for both
toxins, and empiric hydroxycobalamin treatment has a safe
side-effect profile even in the absence of cyanide toxicity. In
addition, a correlation between blood concentrations of
carbon monoxide and cyanide has been shown in smoke
inhalation victims [7] suggesting that most patients in actual
fact suffer toxicity of both simultaneously. The possibility that
the clinical features may be attributable to another cause
should of course always be considered when resuscitating a
patient, and it should not be assumed that cyanide toxicity is
the sole cause of the patients clinical condition.
The time delay to administration of a cyanide antidote is
thought to have a significant impact on outcome [64]. Early
empiric treatment at the scene of injury with hydroxycobalamin for patients suspected to have cyanide toxicity is
utilised in France [9,2931]. Early administration of hydroxycobalamin is possible in France as prehospital care includes
a physician-led ambulance team. We postulate the earlier
intervention has an important role in improving survival, and
that feasibility studies of early empiric treatment of cyanide
toxicity with hydroxycobalamin administered at the scene of
injury are warranted in other countries.
12.
Conclusion
The nature of cyanide toxicity in patients with burns precludes
the possibility of randomised controlled human trials to
burns 41 (2015) 1824
provide strong clinical evidence for the efficacy of antidotes;
therefore, pharmacological theory must be combined with the
available evidence in the literature from animal models and
case series, despite the limitations of this type of evidence, in
order to determine optimal treatment strategies. Dicobalt
edetate and methaemoglobin-forming agents such as sodium
nitrite have side-effect profiles that render them unsafe to use
in patients with burns with smoke inhalation injury. There is
evidence of efficacy for both hydroxycobalamin and sodium
thiosulphate and both are well tolerated; however, comparative studies in the literature found hydroxycobalamin to be
substantially more efficacious than sodium thiosulphate, and
in addition concerns have been raised regarding the slow
onset of action of sodium thiosulphate. We therefore
recommend that hydroxycobalamin is used as the first-line
antidote of choice in patients with burns with inhalational
injury where features consistent with cyanide toxicity are
present. In addition, we suggest that protocols are developed
in the prehospital and emergency care setting that facilitate
the most timely administration of hydroxycobalamin in order
to maximise efficacy.
Conflict of interest
There are no conflicts of interest to declare.
references
[1] Belgian Outcome in Burn Injury Study Group. Development
and validation of a model for prediction of mortality in
patients with acute burn injury. Br J Surg 2009;96(1):1117.
[2] Smith DL, Cairns BA, Ramadan F, Dalston JS, Fakhry SM,
Rutledge R, et al. Effect of inhalation injury, burn size, and
age on mortality: a study of 1447 consecutive burn patients.
J Trauma 1994;37(4):6559.
[3] Mlcak RP, Suman OE, Herndon DN. Respiratory
management of inhalation injury. Burns 2007;33(1):213.
[4] Peck MD. Epidemiology of burns throughout the world. Part
I: Distribution and risk factors. Burns 2011;37(7):1087100.
[5] Palmieri TL, Gamelli RL. Diagnosis and management of
inhalation injury. In: Jeschke MG, Kamolz LP, Sjoberg F,
Wolf SE, editors. Handbook of burns. Vienna: Springer;
2012. p. 16372.
[6] Colohan SM. Predicting prognosis in thermal burns with
associated inhalational injury: a systematic review of
prognostic factors in adult burn victims. J Burn Care Res
2010;31(4):52939.
[7] Baud FJ, Barriot P, Toffis V, Riou B, Vicaut E, Lecarpentier Y,
et al. Elevated blood cyanide concentrations in victims of
smoke inhalation. N Engl J Med 1991;325(25):17616.
[8] Alarie Y. Toxicity of fire smoke. Crit Rev Toxicol
2002;32(4):25989.
[9] Borron SW, Baud FJ, Barriot P, Imbert M, Bismuth C.
Prospective study of hydroxocobalamin for acute cyanide
poisoning in smoke inhalation. Ann Emerg Med
2007;49(6):794801.
[10] Walsh DW, Eckstein M. Hydrogen cyanide in fire smoke: an
underappreciated threat. Emerg Med Serv 2004;33:1603.
[11] Eckstein M, Maniscalco PM. Focus on smoke inhalation: the
most common cause of acute cyanide poisoning. Prehosp
Disaster Med 2006;21(2):s4955.
23
[12] Kulig K. Case studies in environmental medicine: cyanide
toxicity. Atlanta, GA: Agency for Toxic Substances and
Disease Registry, US Department of Health and Human
Services; 1991.
[13] Kirk RL, Stenhouse NS. Ability to smell solutions of
potassium cyanide. Nature 1953;171(4355):6989.
[14] Shepherd G, Velez LI. Role of hydroxocobalamin in acute
cyanide poisoning. Ann Pharmacother 2008;42(5):6619.
[15] Kirk MA, Gerace R, Kulig KW. Cyanide and methemoglobin
kinetics in smoke inhalation victims treated with the
cyanide antidote kit. Ann Emerg Med 1993;22(9):14138.
[16] Singh BM, Coles N, Lewis P, Braithwaite RA, Nattrass M,
Fitzgerald MG. The metabolic effects of fatal cyanide
poisoning. Postgrad Med J 1989;65(770):9235.
[17] Baud FJ, Borron SW, Megarbane B, Trout H, Lapostolle F,
Vicaut E, et al. Value of lactic acidosis in the assessment of
the severity of acute cyanide poisoning. Crit Care Med
2002;30(9):204450.
[18] Anseeuw K, Delvau N, Burillo-Putze G, De Iaco F, Geldner G,
Holmstrom P, et al. Cyanide poisoning by fire smoke
inhalation: a European expert consensus. Eur J Emerg Med
2013;20(1):29.
[19] Lawson-Smith P, Jansen EC, Hilsted L, Hyldegaard O. Effect
of hyperbaric oxygen therapy on whole blood cyanide
concentrations in carbon monoxide intoxicated patients
from fire accidents. Scand J Trauma Resusc Emerg Med
2010;18:32.
[20] Lawson-Smith P, Olsen NV, Hyldegaard O. Hyperbaric
oxygen therapy or hydroxycobalamin attenuates surges in
brain interstitial lactate and glucose; and hyperbaric
oxygen improves respiratory status in cyanide-intoxicated
rats. Undersea Hyperb Med 2011;38(4):22337.
[21] Hart GB, Strauss MB, Lennon PA, Whitcraft 3rd DD.
Treatment of smoke inhalation by hyperbaric oxygen. J
Emerg Med 1985;3(3):2115.
[22] Way JL, End E, Sheehy MH, De Miranda P, Feitknecht UF,
Bachand R, et al. Effect of oxygen on cyanide intoxication.
IV. Hyperbaric oxygen. Toxicol Appl Pharmacol
1972;22(3):41521.
[23] Houeto P, Hoffman JR, Imbert M, Levillain P, Baud FJ.
Relation of blood cyanide to plasma cyanocobalamin
concentration after a fixed dose of hydroxocobalamin in
cyanide poisoning. Lancet 1995;346(8975):6058.
[24] Forsyth JC, Mueller PD, Becker CE, Osterloh J, Benowitz NL,
Rumack BH, et al. Hydroxocobalamin as a cyanide antidote:
safety, efficacy and pharmacokinetics in heavily smoking
normal volunteers. J Toxicol Clin Toxicol 1993;31(2):27794.
[25] Bebarta VS, Tanen DA, Lairet J, Dixon PS, Valtier S, Bush A.
Hydroxocobalamin and sodium thiosulfate versus sodium
nitrite and sodium thiosulfate in the treatment of acute
cyanide toxicity in a swine (Sus scrofa) model. Ann Emerg
Med 2010;55(4):34551.
[26] Bebarta VS, Pitotti RL, Dixon P, Lairet JR, Bush A, Tanen DA.
Hydroxocobalamin versus sodium thiosulfate for the
treatment of acute cyanide toxicity in a swine (Sus scrofa)
model. Ann Emerg Med 2012;59(6):5329.
[27] Bebarta VS, Pitotti RL, Dixon PS, Valtier S, Esquivel L, Bush
A, et al. Hydroxocobalamin and epinephrine both improve
survival in a swine model of cyanide-induced cardiac
arrest. Ann Emerg Med 2012;60(4):41522.
[28] Riou B, Baud FJ, Astier A, Barriot P, Lecarpentier Y. In vitro
demonstration of the antidotal efficacy of
hydroxocobalamin in cyanide poisoning. J Neurosurg
Anesthesiol 1990;2(4):296304.
[29] Fortin JL, Giocanti JP, Ruttimann M, Kowalski JJ. Prehospital
administration of hydroxocobalamin for smoke inhalationassociated cyanide poisoning: 8 years of experience in the
Paris Fire Brigade. Clin Toxicol (Phila) 2006;44(Suppl. 1):
3744.
24
burns 41 (2015) 1824
[30] Borron SW, Baud FJ, Megarbane B, Bismuth C.
Hydroxocobalamin for severe acute cyanide poisoning by
ingestion or inhalation. Am J Emerg Med 2007;25(5):5518.
[31] Fortin JL, Desmettre T, Manzon C, Judic-Peureux V,
Peugeot-Mortier C, Giocanti JP, et al. Cyanide poisoning and
cardiac disorders: 161 cases. J Emerg Med 2010;38(4):46776.
[32] Uhl W, Nolting A, Golor G, Rost KL, Kovar A. Safety of
hydroxocobalamin in healthy volunteers in a randomized,
placebo-controlled study. Clin Toxicol (Phila)
2006;44(Suppl. 1):1728.
[33] Thompson JP, Marrs TC. Hydroxocobalamin in cyanide
poisoning. Clin Toxicol (Phila) 2012;50(10):87585.
[34] OBrien DJ, Walsh DW, Terriff CM, Hall AH. Empiric
management of cyanide toxicity associated with smoke
inhalation. Prehosp Disaster Med 2011;26(5):37482.
[35] Lawson-Smith P, Jansen EC, Hyldegaard O. Cyanide
intoxication as part of smoke inhalation: a review on
diagnosis and treatment from the emergency perspective.
Scand J Trauma Resusc Emerg Med 2011;19:14.
[36] Hamel J. A review of acute cyanide poisoning with a
treatment update. Crit Care Nurse 2011;31(1):7281.
[37] Borron SW, Baud FJ. Antidotes for acute cyanide poisoning.
Curr Pharm Biotechnol 2012;13(10):19408.
[38] Hall AH, Saiers J, Baud F. Which cyanide antidote? Crit Rev
Toxicol 2009;39(7):54152.
[39] Reade MC, Davies SR, Morley PT, Dennett J, Jacobs IC.
Review article: management of cyanide poisoning. Emerg
Med Australas 2012;24(3):22538.
[40] Megarbane B, Delahaye A, Goldgran-Toledano D, Baud FJ.
Antidotal treatment of cyanide poisoning. J Chin Med Assoc
2003;66(4):193203.
[41] Meredith TJ, Jacobsen D, Haines JA, Berger J-C, van Heijst
ANP. International program on chemical safety/
commission of the European Communities evaluation of
antidotes series. Antidotes for poisoning by cyanide, vol. 2.
Cambridge: Cambridge University Press; 1993.
[42] Burrows GE. Cyanide intoxication in sheep; therapeutics.
Vet Hum Toxicol 1981;23(1):228.
[43] Renard C, Borron SW, Renaudeau C, Baud FJ. Sodium
thiosulfate for acute cyanide poisoning: study in a rat
model. Ann Pharm Fr 2005;63(2):15461.
[44] Vesey CJ, Krapez JR, Varley JG, Cole PV. The antidotal action
of thiosulfate following acute nitroprusside infusion in
dogs. Anesthesiology 1985;62:41521.
[45] Breen PH, Isserles SA, Westley J, Roizen MF, Taitelman UZ.
Effect of oxygen and sodium thiosulfate during combined
carbon monoxide and cyanide poisoning. Toxicol Appl
Pharmacol 1995;134(2):22934.
[46] Paulet G, Dassonville J. Value of dimethylaminophenol
(DMAP) in the treatment of cyanide poisoning:
experimental study. J Toxicol Clin Exp 1985;5:10511
[French].
[47] Barillo DJ. Diagnosis and treatment of cyanide toxicity. J
Burn Care Res 2009;30(1):14852.
[48] Hug E. Compt. rend. Soc de biol 1932;111:519.
[49] Hug E. Action of sodium nitrite with sodium thiosulphate in
the treatment of poisoning provoked by potassium cyanide
in the rabbit. Rev Soc Argent Biol 1933;9:917 [Spanish].
[50] Chen K, Rose C, Clowes G. Amyl nitrite and cyanide
poisoning. J Am Med Assoc 1933;100(24):19202.
[51] Chen K, Rose C, Clowes G. Methylene blue, nitrites, and
sodium thiosulphate against cyanide poisoning. Proc Soc
Ex Bio Med 1933;31:2503.
[52] Chen K, Rose C, Clowes G. Comparative values of several
antidotes in cyanide poisoning. Am J Med Sci 1934;188:
76781.
[53] Hall AH, Kulig KW, Rumack BH. Suspected cyanide
poisoning in smoke inhalation: complications of sodium
nitrite therapy. J Toxicol Clin Exp 1989;9(1):39.
[54] Ivankovich AD, Braverman B, Kanuru RP, Heyman HJ,
Paulissian R. Cyanide antidotes and methods of their
administration in dogs: a comparative study.
Anesthesiology 1980;52(3):2106.
[55] Hillman B, Bardhan KD, Bain JTB. The use of dicobalt
edetate (Kelocyanor) in cyanide poisoning. Postgrad Med J
1974;50:1714.
[56] Naughton M. Acute cyanide poisoning. Anaesth Intensive
Care 1974;2(4):3516.
[57] National Poisons Informations Service. Dicobalt edetate
(antidote); 2012, http://www.toxbase.org/General-Info/
Antidotesdoses-and-sources/Dicobalt-edetate/ [accessed
8.1.14].
[58] College of Emergency Medicine and National Poisons
Information Service. Guideline on Antidote Availability for
Emergency Departments; 2013, http://
secure.collemergencymed.ac.uk/code/
document.asp?ID=7559 [accessed 8.1.14].
[59] Centers for Disease Control and Prevention.
Documentation for Immediately Dangerous To Life or
Health Concentrations (IDLHs): Hydrogen cyanide; 1994,
http://www.cdc.gov/niosh/idlh/74908.html [accessed
16.3.14].
[60] Madrzykowski D, Bryner NP, Grosshandler WL, Stroup DW.
Fire spread through a room with polyurethane foamcovered walls. In: Interflam 2004. International Interflam
Conference, 10th Proceedings, Volume 2; 2004. p. 112738.
[61] Davies JWL. Toxic chemicals versus lung tissue-an aspect
of inhalation injury revisited. J Burn Care Rehabil
1986;7:21322.
[62] Burgess WA, Treitman RD, Gold A. Air contaminants in
structural firefighting.National Technical Information
Service Publication PB 299017 Springfield, VA: US
Department of Commerce; 1979.
[63] Jackson DM. The diagnosis of the depth of burning. Br J Surg
1953;40:58896.
[64] Guidotti T. Acute cyanide poisoning in prehospital care:
new challenges, new tools for intervention. Prehosp
Disaster Med 2006;21(2):s408.
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Cardiology I WorkbookDokumen68 halamanCardiology I WorkbookPharmacist DinaBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- PT, Aptt, TTDokumen44 halamanPT, Aptt, TTswaraj sharmaBelum ada peringkat
- Organic AcidsDokumen25 halamanOrganic Acidssatti_indianBelum ada peringkat
- Pharmacology HandoutDokumen84 halamanPharmacology Handoutnanashimii100% (4)
- Nadi Literally MeansDokumen9 halamanNadi Literally MeansThomas Dürst100% (1)
- Occupational Therapy - Play, SIs and BMTsDokumen3 halamanOccupational Therapy - Play, SIs and BMTsAnnbe Barte100% (1)
- Big Book of Kaiju #0Dokumen17 halamanBig Book of Kaiju #0Boracchio Pasquale100% (1)
- Msds Buffer AsetatDokumen6 halamanMsds Buffer AsetatAnnisa SeptianiBelum ada peringkat
- SH Lecture 2018 - Respiratory System DevelopmentDokumen23 halamanSH Lecture 2018 - Respiratory System DevelopmentAna-Maria-Cecilia DurduiBelum ada peringkat
- Census August2 - August 3, 2020Dokumen5 halamanCensus August2 - August 3, 2020Patrick JohnBelum ada peringkat
- Census August 28 - August 29, 2020Dokumen5 halamanCensus August 28 - August 29, 2020Patrick JohnBelum ada peringkat
- Census August 30 - August 31, 2020Dokumen6 halamanCensus August 30 - August 31, 2020Patrick JohnBelum ada peringkat
- Census August 24 - August 25, 2020Dokumen6 halamanCensus August 24 - August 25, 2020Patrick JohnBelum ada peringkat
- Census August 26 - August 27, 2020Dokumen5 halamanCensus August 26 - August 27, 2020Patrick JohnBelum ada peringkat
- Census August 20 - August 21, 2020Dokumen5 halamanCensus August 20 - August 21, 2020Patrick JohnBelum ada peringkat
- Census August 22 - August 23, 2020Dokumen5 halamanCensus August 22 - August 23, 2020Patrick JohnBelum ada peringkat
- Census August 14 - August 15, 2020Dokumen6 halamanCensus August 14 - August 15, 2020Patrick JohnBelum ada peringkat
- Census August 18 - August 19, 2020Dokumen5 halamanCensus August 18 - August 19, 2020Patrick JohnBelum ada peringkat
- Census August 16 - August 17, 2020Dokumen5 halamanCensus August 16 - August 17, 2020Patrick JohnBelum ada peringkat
- Census August 12 - August 13, 2020Dokumen6 halamanCensus August 12 - August 13, 2020Patrick JohnBelum ada peringkat
- Census August 8 - August 9, 2020Dokumen6 halamanCensus August 8 - August 9, 2020Patrick JohnBelum ada peringkat
- 9 Extension: (5) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Dokumen7 halaman9 Extension: (5) (Admission: 0 Card: 0 Discharged: 0 Referral: 0 Transferred: 0 Expired: 0 HAMA: 0 Abscond: 0Patrick JohnBelum ada peringkat
- Census August 6 - August 7, 2020Dokumen6 halamanCensus August 6 - August 7, 2020Patrick JohnBelum ada peringkat
- Census August 10 - August 11, 2020Dokumen6 halamanCensus August 10 - August 11, 2020Patrick JohnBelum ada peringkat
- Circulatory System AssessmentDokumen4 halamanCirculatory System Assessmentapi-98991203Belum ada peringkat
- B9780702031458000636 WebDokumen13 halamanB9780702031458000636 WebChristopher BermeoBelum ada peringkat
- Detection of Leukemia in Human Blood Sample Based On Microscopic Images: A StudyDokumen8 halamanDetection of Leukemia in Human Blood Sample Based On Microscopic Images: A StudySaku RaBelum ada peringkat
- Wingate Anaerobic Test PercentileDokumen10 halamanWingate Anaerobic Test PercentileFernando Rojas LopezBelum ada peringkat
- List of Medical Roots, Suffixes and Prefixes - Wikipedia, The Free EncyclopediaDokumen35 halamanList of Medical Roots, Suffixes and Prefixes - Wikipedia, The Free EncyclopediaHoward GouldBelum ada peringkat
- Ulkus Pedis and DM Type 2 Case KarawangDokumen28 halamanUlkus Pedis and DM Type 2 Case KarawangFathia RachmatinaBelum ada peringkat
- Essencial Phrasal VerbsDokumen4 halamanEssencial Phrasal VerbsalvereBelum ada peringkat
- CHAPTER 2 - Textbook ExerciseDokumen8 halamanCHAPTER 2 - Textbook ExerciseLeena HingBelum ada peringkat
- Case Report Myoma Uterine: Supervised By: Dr. Hesty Duhita Permata, SP - OGDokumen12 halamanCase Report Myoma Uterine: Supervised By: Dr. Hesty Duhita Permata, SP - OGNiki Rizqi rachmawatiBelum ada peringkat
- MICROBIOLOGY - Microbial Taxonomy, Cell Structure and Bacterial Metabolism, Growth & GeneticsDokumen16 halamanMICROBIOLOGY - Microbial Taxonomy, Cell Structure and Bacterial Metabolism, Growth & GeneticsRobie LeañoBelum ada peringkat
- The MoneraDokumen19 halamanThe MoneraNaufal Taufiq AmmarBelum ada peringkat
- Specialization of Cerebral Hemispheres in Humans: December 2013Dokumen9 halamanSpecialization of Cerebral Hemispheres in Humans: December 2013Huy NgoBelum ada peringkat
- 47pages METHAMPHETAMINE TOXICITY AND MESSENGERS OF DEATHDokumen47 halaman47pages METHAMPHETAMINE TOXICITY AND MESSENGERS OF DEATHDenise MathreBelum ada peringkat
- Pelvic Floor MuscleDokumen11 halamanPelvic Floor MuscleSonia guptaBelum ada peringkat
- PM Artifacts WEBDokumen20 halamanPM Artifacts WEBSalman MemonBelum ada peringkat
- Unstable Angina Differential DiagnosesDokumen5 halamanUnstable Angina Differential DiagnosesSanda-ana BogdanBelum ada peringkat
- Overactivebladder 160426102342Dokumen53 halamanOveractivebladder 160426102342Tô Hoàng DũngBelum ada peringkat
- Reports 2Dokumen10 halamanReports 2Tejaswini ReddyBelum ada peringkat
- Talley & O'Connor Quiz SampleDokumen5 halamanTalley & O'Connor Quiz SamplefilchibuffBelum ada peringkat
- Toxic A History of Nerve Agents From Nazi Germany To Putins Russia 1St Edition Edition Dan Kaszeta Download 2024 Full ChapterDokumen23 halamanToxic A History of Nerve Agents From Nazi Germany To Putins Russia 1St Edition Edition Dan Kaszeta Download 2024 Full Chaptermari.artrip178100% (9)
- SYOK HipovolemikDokumen31 halamanSYOK HipovolemikAmaliahHarumiKarimBelum ada peringkat