Maat 09 I 1 P 10
Diunggah oleh
Achmad Deza FaristaJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Maat 09 I 1 P 10
Diunggah oleh
Achmad Deza FaristaHak Cipta:
Format Tersedia
Original Article
Maternal Factors for Low Birth Weight Babies
Lt Col G Singh*, Capt R Chouhan+, Maj K Sidhu#
Abstract
Background: Low birth weight is defined as the live births with less than 2.5 kg weight. It is a key determinant of infant survival,
health and development. Low birth weight infants are at a greater risk of having a disability and for diseases such as cerebral
palsy, visual problems, learning disabilities and respiratory problems. To reduce the low birth weight deliveries, we studied the
maternal factors which adversely affect the fetus in utero and their impact on fetus.
Methods: A retrospective study was carried out on 40 low birth weight pregnancies out of 650 deliveries from July 2005 to Jun 2006.
Maternal factors like age, parity, pre pregnancy body mass index, hemoglobin levels, bad obstetric history (history of stillbirth/
neonatal death in previous pregnancies, three or more spontaneous consecutive abortions), pre eclampsia, fetal distress, mode of
deliveries were studied. These results were compared with a random sample of 300 pregnant ladies taken from rest of the
deliveries. Cases of multiple pregnancies and stillbirths were excluded.
Result: We found that prepregnancy maternal body mass index (p<0.01 for BMI <20), unbooked status (p<0.01), pre eclampsia (p
<0.01) and bad obstetric history (p<0.01) were the maternal factors which resulted in low birth weight babies in most of the cases.
However in 10 (25%) cases, no contributory maternal factor was found.
Conclusion: Prepregnancy maternal body mass index, unbooked status, pre eclampsia and bad obstetric history are significant
maternal factors resulting in low birth weight babies.
MJAFI 2009; 65 : 10-12
Key Words : Prepregnancy maternal body mass index; Unbooked status; Pre eclampsia; Bad obstetric history
Introduction
ow birth weight (LBW) is the dominating risk factor
for infant morbidity and mortality, (36% of all
mortality in children <5 years of age), constituting about
4 million deaths per year. Some term and preterm small
babies are healthy, with weight and length according to
their genetic potential, while others are smaller due to
factors impeding growth during fetal life. This
phenomenon is called intrauterine growth restriction
(IUGR) and is the second leading cause of perinatal
morbidity and mortality, after prematurity.
Low birth weight lower than that expected from the
genetic potential might be caused by fetal, maternal or
placental factors or a combination of risk factors,
resulting in an impaired placental transport of nutrients
or reduced growth potential of the fetus. Constitutional,
gender and hereditary factors explain up to 40% of the
variability of birth weight. Maternal age (<20 or >35
yrs), ethnicity, marital status, birth interval, educational
level and socio-economic conditions are other
explanatory factors. Common fetal factors are genetic
and/or chromosomal aberrations. Medical risk factors
for LBW before pregnancy are chronic conditions like
hypertension, renal insufficiency, cardio-respiratory,
autoimmune, endocrine or infectious disorders. The risk
factors for LBW during pregnancy are hypertensive
disorders, diabetes, malnutrition, bleeding, anemia,
infection, placental or fetal anomalies and multiple
pregnancies. The morbidities of term and moderately
preterm (>32 weeks) LBW are mainly related to uteroplacental insufficiency and poor energy substrate
transfer, resulting in neonatal complications like birth
asphyxia, hypothermia, meconium aspiration,
polycythaemia, hypoglycemia, hypocalcaemia and
thrombocythaemia.
LBW infants are forty times more likely to die within
their first four weeks of life than normal birth weight
infants. LBW infants are also three times more likely
than normal birth weight infants to have
neurodevelopmental complications and congenital
abnormalities [1].The neonatal course in LBW infants
born preterm (<32 weeks) is dominated by complications
caused by anatomic and physiological immaturity e.g.
birth asphyxia, hypothermia, respiratory distress due to
delayed alveolar clearance of water and surfactant
deficiency, delayed postnatal circulatory adaptation with
pulmonary hypertension, systemic hypotension and
delayed closure of fetal shunts. Immaturity and reduced
substrate stores explain high prevalence of hypo/
hyperglycemia, jaundice and coagulopathy. Immature
Classified Specialist (Obstetric & Gynaecology), Military Hospital, Gwalior, Pin-474006. +MO (Paediatrics), Military Hospital, Amritsar
Cantt 143001. #GD Matron, 174 MH, C/o 56 APO.
Received : 20.06.07; Accepted : 12.03.08
E-mail: gurneeshellora@hotmail.com
Maternal Factors for Low Birth Weight Babies
11
intestinal function makes enteral feeding problematic and
nutrition insufficient. Immature vascular development
in the central nervous system and in the retina
predisposes for serious intraventricular bleeding and
retinopathy. Immature skin and mucosa barrier and
immaturity of cellular and humeral immune function,
predisposes for early neonatal sepsis and increased
prevalence of nosocomial infections. LBW infants are
at risk of developing complications that impose risks for
permanent sequelae. The risk increases both by lower
gestational age and weight. Preterm small for gestational
age (SGA) are more susceptible than preterm infants
with adequate intrauterine growth.
or parity between the LBW and control groups. The mean
age of the mothers in both groups was 24.68 years and 25.15
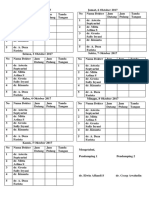
years respectively. Table 1 shows comparison between LBW
group and control for varying levels of prepregnant BMI. As
the BMI increase from < 20 to >25, there is a fall in risk levels
for LBW neonates. Fisher exact test was applied and difference
in incidence of LBW neonates for BMI <20 & >25 was
statistically highly significant (p< 0.01).
Table 2 shows fetal outcome in LBW group and control
group. There was higher association of preterm delivery (15%
vs 6.33%), malpresentation (5% vs 2.33%), caesarean section
(27.5 % vs 22.67 %), tuberculosis (2.5% vs 0.67%), anemia
(20% vs 18%) in LBW group, but none of them were
statistically significant. However unbooked status (12.5% vs
2%, p<0.01), bad obstetric history (17.5% vs 4%, p< 0.01),
and pre eclampsia (32.5% vs 5.33%, p<0.01) were highly
significant in this study.
Material and Methods
A retrospective study of all newborns weighing less than
2.5 kg born between July 2005 to Jun 2006 was carried out in
650 deliveries which occurred during this period. Multiple
pregnancies and stillbirths were excluded. Maternal factors
like age, parity, pre-pregnancy body mass index (BMI),
hemoglobin levels, bad obstetric history (history of stillbirth/
neonatal death in previous pregnancies, three or more
spontaneous consecutive abortions), pre eclampsia, fetal
distress, mode of deliveries were studied. These results were
compared with a random sample of 300 pregnant ladies.
Statistical analysis was done using Fisher Exact test.
Discussion
The frequency of LBW found in this study was 6.16%,
the reported incidence of which varies from 6-18% [13]. Maternal nutritional status both before and during
pregnancy is a well-recognized determinant of birth
outcomes [4]. BMI is a simple, useful index for
evaluating prepregnancy nutritional status. Although
prepregnancy BMI has a genetic as well as nutritional
component, a low prepregnancy BMI is considered a
marker for minimal tissue nutrient reserves [5]. Women
with low prepregnancy weight for height or BMI are at
increased risk for a number of adverse pregnancy
Results
During the study period, 40 (6.16%) pregnancies resulted
in LBW neonates out of total 650 singleton pregnancies.
There were no significant difference in the maternal age, race
Table 1
Comparison between low birth weight (LBW) and control group in prepregnancy body mass index (BMI)
Pre pregnancy BMI
Weight (kg)/Height (m)2
<20
20-25
>25
**
significant,
LBW group
n=40
Control group
n=300
14 (35%)
24 (60%)
2 (5%)
50 (16.67%)
133 (44.33%)
117 (39.00%)
p value
(Fisher exact test)
0.009**
0.066
0.000**
Odds ratio
(95%CI)
Odds ratio
(baseline strata
BMI >25 as one)
2.692 (1.328-5.470)
1.883 (0.970-3.656)
0.082 (0.022-0.315)
32.829
22.963
1.000
confidence interval
Table 2
Comparison between low birth weight (LBW) and control group in pregnancy complications
Unbooked*
Bad obstetric history##
Anemia (Hb <11gm%)
Pre eclampsia
Preterm delivery
Tuberculosis on treatment
PROM***
Malpresentation
Fetal distress###
LSCS
*
LBW group n=40
Control group n=300
5 (12.5%)
7 (17.5%)
5 (12.5%)
13 (32.5%)
6 (15%)
1 (2.5%)
3 (7.5%)
2 (5%)
2 (5%)
11 (27.5%)
6 (2%)
12 (4%)
54 (18%)
16 (5.33%)
19 (6.33%)
2 (0.67%)
31 (10.33%)
7 (2.33%)
26 (8.67%)
68 (22.67%)
p value (Fisher exact test)
0.005**
0.003**
0.507
0.000**
0.097
0.314
0.781
0.286
0.554
0.550
Odds ratio (95% CI)
7.000 (2.152-22.84)
5.091 (1.931-13.488)
0.651 (0.252-1.687)
8.546 (3.771-19.418)
2.610 (1.006-6.813)
3.821 (0.491-30.015)
0.704 (0.219-2.280)
2.203 (0.504-9.756)
0.555 (0.141-2.202)
1.294 (0.623-2.696)
less than three antenatal visits,** significant, *** premature rupture of membranes, # confidence interval, ## history of recurrent abortions,
stillbirth, neonatal death in last pregnancy, ### as manifested by fetal bradycardia, variable or late decelerations
MJAFI, Vol. 65, No. 1, 2009
12
outcomes, including preterm birth and IUGR [6]. In this
study, high percentage of LBW (35 %) newborns were
born to women with BMI <20 as compared to 16.67%
of normal birth weight newborns in control group. The
mechanisms of association between prepregnancy BMI
and IUGR and preterm delivery are not clear, but probably
the relationship between a low prepregnancy BMI and
adverse pregnancy outcomes is mediated by protein
energy availability. One explanation for the lower mean
neonate birth weight in women with low prepregnancy
weight may be that the fetus was prevented from
receiving an adequate supply of nutrients from the
mother because of changes in maternal hemodynamic
status [7]. These studies suggested that in malnourished
underweight women, lower volume expansion related to
decreased micronutrient status might be associated with
reduced fetal growth.
Unbooked status of mother is a significant independent
risk factor for LBW babies [8,9]. In this study, 12.5 %
of LBW neonates were born to unbooked mothers as
compared to 2% in control. Unbooked status contributes
to maternal undernourishment and inadequate care during
pregnancy, thus compromising both baby and the mother.
In this study, bad obstetric history was a significant
contributory factor towards LBW babies (17.5% vs 4%,
p<0.01). Mothers with bad obstetric history were 4 times
likely to deliver a LBW baby [9]. Perhaps genetic factors
and socioeconomic factors were the reasons for this
phenomenon leading to repeat adverse obstetric outcome.
In this study, anemia was not a significant factor (18%
vs 20%, p>0.05) but contribution of anemia leading to
LBW babies is controversial [7,9]. However, substantial
iron deficiency anemia (usually <80g/L) is associated
with an increased incidence of LBW. The mechanism
by which anemia could produce this effect is unknown,
but other nutrient deficiencies are important contributing
factors [10]. One study even reported harmful effects
of iron supplementation [11]. In this study women with
pre eclampsia were six times more likely to have LBW
babies as compared to control (p<0.01). Pre eclampsia
by reducing plasma volume reduces the supply of nutrient
to the fetus thus affecting fetal growth [12,13].
Higher incidence of preterm delivery was seen in
LBW babies (15% vs 6.33%, p>0.05), which was not
statistically significant. In literature, two-thirds of infants
born weighing less than 2,500 grams are preterm [14].
Low incidence of preterm in this study may be due to
exclusion of multiple births. The incidence of tuberculosis,
malpresentation, fetal distress and cesarean section rates
were higher in LBW group, but statistically insignificant.
We conclude that prepregnancy maternal BMI,
unbooked pregnancy, pre eclampsia and bad obstetric
Singh, Chouhan and Sidhu
history are significant factors resulting in LBW babies.
Conflicts of Interest
None identified
Intellectual Contribution of Authors
Study Concept : Lt Col G Singh
Drafting & Manuscript Revision : Lt Col G Singh
Statistical Analysis : Lt Col G Singh
Study Supervision : Lt Col G Singh, Capt R Chouhan, Maj K Sidhu
References
1. Zlot A, Smith N, Miller J, Janes G, Coltin K. The
Massachusetts low birth weight project: the level of agreement
of low birth weight status between managed care claims data
and birth certificates. Abstr Book Assoc Health Serv Res Meet
1999; 16: 67.
2. United Nations Childrens Fund and World Health Organization.
Low Birth weight: Country, regional and global estimates.
UNICEF, New York, 2004.
3. Kapoor SK, Kumar G, Pandav CS, Anand K. Incidence of low
birth weight in Rural Ballabgarh, Haryana. Indian Pediatrics
2001; 38: 271-5.
4. Osrin D, De L, Costello A. Maternal nutrition and fetal growth:
practical issues in international health. Semin Neonatol 2000;
5: 20919.
5. Schieve LA, Cogswell ME, Scanlon KS, et al. Prepregnancy
body mass index and pregnancy weight gain: associations with
preterm delivery. Obstet Gynecol 2000; 96: 194200.
6. Neggers Y, Goldenberg RL. Some Thoughts on Body Mass
Index, Micronutrient Intakes and Pregnancy Outcome. J Nutr
2003;133:1737-40.
7. Philip JS. Maternal hemoglobin concentration and birth weight.
American Journal of Clinical Nutrition 2000; 71:1285-7.
8. Loto OM, Ezechi OC, Kalu BKE, et al. Poor obstetric
performance of teenagers: is it age- or quality of care-related?
Journal of Obstetrics and Gynecology, 2004; 24:395 - 8.
9. Anand K, Garg BS. A Study of Factors Affecting LBW. Indian
Journal of Community Medicine 2000; 25: 4-6.
10. Ronnenberg AG, Wood RJ, Wang X, et al. Preconception
Hemoglobin and Ferritin Concentrations are associated with
pregnancy outcome in a prospective cohort of Chinese women.
J Nutr 2004; 134: 2586-91.
11. Ziaei S, Norrozi M, Faghihzadeh S, Jafarbegloo E. A randomised
placebo-controlled trial to determine the effect of iron
supplementation on pregnancy outcome in pregnant women
with haemoglobin 13.2 g/dl. BJOG: An International Journal
of Obstetrics and Gynaecology. 2007; 114: 6848.
12. Odegard RA, Vatten LJ, Nilsen ST, Salvesen KA, Austgulen R.
Preeclampsia and Fetal Growth. Obstetrics & Gynecology
2000;96:950-5.
13. Walker BR, McConnachie A, Noon JP, Webb DJ, Watt GCM.
Contribution of parental blood pressures to association between
low birth weight and adult high blood pressure: cross sectional
study. BMJ 1998; 316:834-7.
14. Scholl TO, Johnson WG. Folic acid influence on the outcome
of pregnancy. American Journal of Clinical Nutrition 2000; 71
(suppl):1295S-1303S.
MJAFI, Vol. 65, No. 1, 2009
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Journal Reading 1 A. Deza FaristaDokumen9 halamanJournal Reading 1 A. Deza FaristaAchmad Deza FaristaBelum ada peringkat
- Maurice Nicoll The Mark PDFDokumen4 halamanMaurice Nicoll The Mark PDFErwin KroonBelum ada peringkat
- Absens IDokumen16 halamanAbsens IAchmad Deza FaristaBelum ada peringkat
- Asma LuluDokumen25 halamanAsma LuluBrenda KarinaBelum ada peringkat
- No Day Destination KeteranganDokumen2 halamanNo Day Destination KeteranganAchmad Deza FaristaBelum ada peringkat
- Referat Gna DezaDokumen37 halamanReferat Gna DezaAchmad Deza FaristaBelum ada peringkat
- ITENERARYDokumen2 halamanITENERARYAchmad Deza FaristaBelum ada peringkat
- ITINDokumen3 halamanITINAchmad Deza FaristaBelum ada peringkat
- Schengen Visa Application January2017Dokumen3 halamanSchengen Visa Application January2017Meiliana AnggeliaBelum ada peringkat
- No Day Destination KeteranganDokumen2 halamanNo Day Destination KeteranganAchmad Deza FaristaBelum ada peringkat
- FishboneDokumen1 halamanFishboneAchmad Deza FaristaBelum ada peringkat
- Absensi SeminarDokumen9 halamanAbsensi SeminarAchmad Deza FaristaBelum ada peringkat
- ContentServer 51Dokumen6 halamanContentServer 51Achmad Deza FaristaBelum ada peringkat
- Orbital Lymphoma Diagnostic TreatmentDokumen7 halamanOrbital Lymphoma Diagnostic TreatmentAchmad Deza FaristaBelum ada peringkat
- ContentServer 52Dokumen7 halamanContentServer 52Achmad Deza FaristaBelum ada peringkat
- Topical Corticosteroid Vs Oral Zinc-Topical Corticosteroid in Patients With VitiligoDokumen5 halamanTopical Corticosteroid Vs Oral Zinc-Topical Corticosteroid in Patients With VitiligoAan AnharBelum ada peringkat
- Lim FomaDokumen7 halamanLim FomaAchmad Deza FaristaBelum ada peringkat
- Azithromycin Pulse Therapy Effective in Acne TreatmentDokumen3 halamanAzithromycin Pulse Therapy Effective in Acne TreatmentreyBelum ada peringkat
- Maternal BMI's impact on pre-eclampsia phenotypeDokumen7 halamanMaternal BMI's impact on pre-eclampsia phenotypeAchmad Deza FaristaBelum ada peringkat
- Seminar Pre-Eclamsi PDFDokumen14 halamanSeminar Pre-Eclamsi PDFLydia Fe SphBelum ada peringkat
- OBESITY AND PREGNANCY OUTCOMESDokumen5 halamanOBESITY AND PREGNANCY OUTCOMESAchmad Deza FaristaBelum ada peringkat
- Publication 519Dokumen7 halamanPublication 519Achmad Deza FaristaBelum ada peringkat
- ContentServer 37.ASPaaaaaDokumen6 halamanContentServer 37.ASPaaaaaAchmad Deza FaristaBelum ada peringkat
- Screen para Hie Doppler y MarcadoresDokumen8 halamanScreen para Hie Doppler y MarcadoresAchmad Deza FaristaBelum ada peringkat
- Hypertension 2013 Li 873 9aaaaaDokumen8 halamanHypertension 2013 Li 873 9aaaaaAchmad Deza FaristaBelum ada peringkat
- PreeDokumen6 halamanPreeAchmad Deza FaristaBelum ada peringkat
- Weight Gain Recommendations in PregnancyDokumen4 halamanWeight Gain Recommendations in PregnancyEirna Syam Fitri IIBelum ada peringkat
- Nutritional Status Among Women With Pre-Eclampsia and Healthy Pregnant and Non-Pregnant Women in A Latin American CountryDokumen7 halamanNutritional Status Among Women With Pre-Eclampsia and Healthy Pregnant and Non-Pregnant Women in A Latin American CountryAchmad Deza FaristaBelum ada peringkat
- Yclnu1789 PDFDokumen14 halamanYclnu1789 PDFAchmad Deza FaristaBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- NCM 107 - LM 7 Assessing Blood Loss, Identifying LOCHIADokumen8 halamanNCM 107 - LM 7 Assessing Blood Loss, Identifying LOCHIAJewel Ramos GalinatoBelum ada peringkat
- @medicalbookpdf Preeclampsia PDFDokumen286 halaman@medicalbookpdf Preeclampsia PDFgalihsupanji111_2230Belum ada peringkat
- Ultrasound Measurement During PregnancyDokumen14 halamanUltrasound Measurement During PregnancyMohammed IbrahimBelum ada peringkat
- Percentages For MRCOG1Dokumen3 halamanPercentages For MRCOG1jmoBelum ada peringkat
- Tugas 1Dokumen20 halamanTugas 1lastia meilinaBelum ada peringkat
- Types and Complication of C-SectionDokumen13 halamanTypes and Complication of C-SectionMeghaUnniBelum ada peringkat
- Female Reproductive SystemDokumen3 halamanFemale Reproductive SystemKai AsuncionBelum ada peringkat
- E TacticsDokumen22 halamanE Tacticsmaximus leodonus100% (2)
- Leg Med - Preganancy, Abortion, Paternity and Filiation (Nov - May 2021)Dokumen8 halamanLeg Med - Preganancy, Abortion, Paternity and Filiation (Nov - May 2021)Shia LevyBelum ada peringkat
- Tantra and Female Ejaculation: The Sacred Nectar AmritaDokumen4 halamanTantra and Female Ejaculation: The Sacred Nectar AmritaRockdorkBelum ada peringkat
- Impact of Teen Pregnancy on Academic PerformanceDokumen86 halamanImpact of Teen Pregnancy on Academic PerformanceCaroline ValenzuelaBelum ada peringkat
- Different Types of Family in IndiaDokumen5 halamanDifferent Types of Family in IndiaDavid VarteBelum ada peringkat
- Chlamydia GonorrheaDokumen3 halamanChlamydia GonorrheaAugene ToribioBelum ada peringkat
- WordDokumen49 halamanWordMarko ShabanofOzz0% (1)
- The Columbus Foundation-NARALDokumen4 halamanThe Columbus Foundation-NARALCheryl SullengerBelum ada peringkat
- Pregnancy Calendar and Calculator Tool - BabyMedDokumen2 halamanPregnancy Calendar and Calculator Tool - BabyMedImran MullaBelum ada peringkat
- KEMH Obstetric Cholestasis GuidelineDokumen11 halamanKEMH Obstetric Cholestasis GuidelineTuna AhsanBelum ada peringkat
- 3 2 24 791 PDFDokumen4 halaman3 2 24 791 PDFKeerti PathakBelum ada peringkat
- Obstetrical Procedures Forceps Delivery Cesarean SectionDokumen3 halamanObstetrical Procedures Forceps Delivery Cesarean SectionRosnalia HariyantoBelum ada peringkat
- Make Sex HotterDokumen21 halamanMake Sex Hotterjack2207100% (1)
- Guide To The FemaleOrgasmDokumen7 halamanGuide To The FemaleOrgasmrishav kumar agarwal0% (1)
- 1st Quarter 2023Dokumen16 halaman1st Quarter 2023blairBelum ada peringkat
- MRCOG Short Answer Questions September 2013Dokumen1 halamanMRCOG Short Answer Questions September 2013Dr.Marva YusafzaiBelum ada peringkat
- STDS: Trichomoniasis: Trichomonas Vaginalis, Which Can Be Found in The Female Vagina or Urethra and in TheDokumen2 halamanSTDS: Trichomoniasis: Trichomonas Vaginalis, Which Can Be Found in The Female Vagina or Urethra and in TheSupermarsopaMarsopitaMarsoperaBelum ada peringkat
- PreeclampsiaDokumen21 halamanPreeclampsiaRitamariaBelum ada peringkat
- Nate Roundy Polmeth 2022 PosterDokumen1 halamanNate Roundy Polmeth 2022 Posterapi-467836735Belum ada peringkat
- Lesson 10Dokumen10 halamanLesson 10Charmaine Gorge DangsiBelum ada peringkat
- Bio DoopDokumen6 halamanBio DoopAnaconda Warriors 12 ABelum ada peringkat
- Science 10 Q3 - M2Dokumen14 halamanScience 10 Q3 - M2Avha CortesBelum ada peringkat
- Chestnut's Obstetric Anesthesia Principles and Practice, Fifth EditionDokumen2 halamanChestnut's Obstetric Anesthesia Principles and Practice, Fifth EditionYohanes TjandraBelum ada peringkat