Nep FGB
Diunggah oleh
icaeeJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Nep FGB
Diunggah oleh
icaeeHak Cipta:
Format Tersedia
Approach to Hypokalemia
12 : 6
Hemant Mehta, Mumbai
Potassium is an important ion in body, which is required for functions of cells, especially nerve and
muscle cells. It comes in body through food and the kidneys remove excess of potassium to keep a
proper balance of mineral in the body. Hypokalemia is a disorder that occurs when the serum potassium
(Sk) in the blood drops to < 3.5 mEq/L.
Physiology
Daily potassium load is 50-150 mEq out of which 90% is excreted in urine and remaining through
stool and sweat. When renal function is compromised, the GI tract can eliminate up to 30% of the
intake; enteric loss of potassium in diarrheal conditions can be substantial. K secretion by colon and
sweat gland is stimulated by aldosterone.
Sk is a general indicator of total body potassium. However, because only about 2% of total body K
is in the extracellular fluid and 98% is in the cells, small losses or gains by the cells can cause large
changes in Sk.
Acid-Base balance
Metabolic acidosis promotes hyperkalemia whereas alkalosis promotes hypokalemia.
Insulin
Insulin deficiency impairs cellular K uptake and promotes hyperkalemia, probably through the lack
of stimulation of Na-K-ATPase. Increased Sk stimulates pancreatic insulin release while hypokalemia
has an inhibitory (diabetogenic) effect.
Catecholamines
Catecholamines, particularly beta-2 agonists e.g. terbutaline, stimulates the cellular Na-K pump and
can result in moderate hypokalemia.
Aldosterone
Aldosterone stimulates cellular potassium uptake and facilitates renal K excretion. It stimulates Na-K
pump, not only in the renal collecting ducts, but in other organs as well.
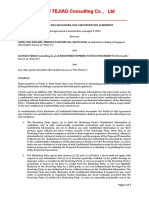
Renal regulation of potassium (Figure 1)
Almost 90% of the K eliminated in the urine is due to secretion in the cortical collecting duct. It is
influenced by conditions like adrenal insufficiency, hyperaldosteronism and Cushings syndrome. K
secretion by the collecting duct is stimulated by high Sk, increased tubular fluid flow and diuretics.
Reduction in the dietary K intake results in renal conservation of K both by decreasing K secretion
in the cortical collecting duct and enhancing reabsorption in the medullary collecting duct.
What are the causes of hypokalemia?
Renal losses: diuretics (loop and thiazide), renal tubular acidosis (RTA), excess aldosterone
GI losses: diarrhea, laxative abuse, villous adenoma
628
Approach to Hypokalemia
Nephron
breath, diarrhea, vomiting, fasting, dysuria, fever etc which
can account for lethargy.
K+
Past history: Similar episodes or neurological disease or renal
disease?
K+
Proximal
Tubule
K+
K+
Collecting
Duct
K+
Drug history: diuretics, laxatives, alternative or recreational
medicines
Loop of Henle
Personal history: constipation, smoking, alcohol
Na+ K+ 2Cl- Luminal
Loop
diuretics
Family history: renal disease, periodic paralysis, neurological
problems
Investigations on initial assessment: after careful
examination which includes assessment of hydration, BP and
neurological examination, following investigations are asked
for: CBC, Routine urinalysis, Urinary electrolytes on a spot
sample (urine sample must be collected before treatment is
started for correction of Sk), renal and liver function tests,
CRP, ECG, CXR, ABG
ClNa+
ATP
K+
Basolateral
Thiazide
Luminal
Distal Nephron
K+
ATP
ClATP
ATP
H+
H+
Intercalated Cell
Na+
Na+
ENaC
K+ Cl-
Principal Cell
HCO
Na+
Cl-
K+
Aldosterone
Additional tests which are useful: Serum magnesium level,
Aldosterone, Renin and Cortisol levels
Amiloride
Alkalosis: hydrogen ions transported out of cells at the expense
of K+ flowing in
It is first necessary to determine whether hypokalemia is an
emergency or non emergency. It is also important to find out
whether hypokalemia is artefactual, the result of redistribution
of K or a result of true K depletion. Artefactual values may be
seen in leukemic patients with a WBC value > 100,000/mm3.
The clinical setting and the blood pH will determine whether
hypokalemia is secondary to redistribution.
Manifestations of hypokalemia include:
Once these are ruled out, start with urinary K values.
Muscle weakness, cramps, tetany
If urinary K is <15mEq/d: Look at ABG.
Fatigue
If metabolic acidosis: diarrhea, GI fistula, fasting/starvation.
Constipation, ileus
If neutral pH: profuse sweating, inadequate intake.
Arrhythmias and predisposition to digitalis toxicity
If metabolic alkalosis: remote vomiting or remote diuretics.
Muscle damage, rhabdomyolysis
If variable pH: laxative abuse, villous adenoma.
Paralysis (which can include the lungs)
If urinary K is > 15 mEq/d, estimate TTKG.
ECG changes: T wave flattening, U waves, ST segment
depression
TTKG = (Urine K / Serum K) / (Urine Osm / Serum Osm)
Renal: Polyuria (nephrogenic diabetes insipidus), polydipsia
ATP
ATP
K+
Cl-
Cl-
K+
Basolateral
Fig. 1 : Renal potassium handling
Approach to a patient with hypokalemia:
History:
The search for etiology of hypokalemia should begin with a
careful history and physical examination concentrating on the
drug history and the state of hydration (vomiting and diarrhea).
Definition
A calculated measurement which estimates the tubular
fluid potassium concentration at the end of the cortical
collecting tubule, the site responsible for most of potassium
secretion. In simplest terms, think of the TTKG as a
rough measurement of aldosterone activity in the kidney.
TTKG = 8-9 in normal subject on a normal diet
Practical Application
Duration of symptoms
Hyperkalemia (typically persistent high Sk)
What is meant by weakness? Is it focal neurological or
generalized? Rule out symptoms like cough, shortness of
Use the TTKG to determine if high K+ is from low aldosterone
states or from decreased effective circulating volume (in CHF,
629
Medicine Update 2012 Vol. 22
etc.)
In low aldosterone states, K+ in the cortical collecting tubule
should be low and thus the TTKG should be low.
If hypoaldosterone state, TTKG < 5
If urinary chlorides are < 10 mEq/d: vomiting, chloridorrhea,
nasogastric drainage
If urinary chlorides are > 20 mEq/d; do urinary calcium to
creatinine ratio*.
Hypokalemia (Persistent)
* Values are expressed in mMol/L. For conversion: Creatinine
1 mg/dl = 0.080 mMol/L and
calcium 1 mg/dl =
0.25 mMol/L.
Use the TTKG to determine renal vs. non-renal loss of
potassium.
If UCa/Cr ratio >0.2, consider loop diuretics or Barters
syndrome
If loss is renal, assume hyperaldosterone state and thus K+ at
the cortical collecting duct should be high and thus the TTKG
should be high.
If UCa/Cr ratio < 0.15, consider thiazide diuretics or
Gitelmans syndrome
If decreased ECV, TTKG > 7
If renal loss of K+, TTKG > 7
If non-renal loss, TTKG < 5 (should be hypoaldo from low
K+)
Simply think of the TTKG as a rough measurement of
aldosterone activity in the kidney. As aldosterones action
is retention of Nawith excretion of K, tubular fluid K
concentration is high ifthere is aldosterone action,and
so is TTKG. Division by (urine osmo/plasma osmo) is
toadjust the urinary potassium for the concentrating effects
that occur in the collecting tubule, where water is removed
from the urine. Note that this formula is valid only when
Uosm >300 and UNa >25.A high TTKG suggests that the
kidney is wasting potassium, which may be appropriate (in
the setting of hyperkalemia) or inappropriate (in the setting
of hypokalemia). Normally,hypokalemia should produce a
TTKG < 3. The expected TTKG in hyperkalemia is > 10.
In hyper K, if the TTKG is high, it means that there ishigh
aldosterone action (appropriate), e.g. from low effective
circulating volume in CHF. If TTKG is < 5, it means that
aldosterone activity is low, and the reason for hyper K is due
to abnormal renal handling of K, e.g. in type IV renal tubular
acidosis.
In hypo K, ifTTKG is still > 7, it means that there is inappropriately
highaldosterone activity despite the hypo K, and thus renal
loss of K is the cause of thehypo K, e.g. hyperaldosteronism,
Cushings syndrome (pseudohyperaldosteronism).If TTKG
is < 5, it means that aldosterone activity is appropriately low
to conserve K, and thus the hypo K is not due to renal loss,
i.e. non-renal loss.
If TTKG is high with hypokalemia, look at BP.
If BP is low/normal: Look at ABG.
Low/normal BP with metabolic acidosis: RTA type I and II,
diabetic ketoacidosis
Low/normal BP with metabolic alkalosis: Look at urinary
chlorides.
If TTKG is high and BP is high: do serum aldosterone level.
High BP with low aldosterone level: to do Serum cortisol
level. Low cortisol level: Liddles syndrome; high cortisol
level: Cushings syndrome.
If high BP with high aldosterone level; do plasma renin activity.
If renin level is high: renal artery stenosis, malignant
hypertension, accelerated hypertension, juxta-glomerular
apparatus tumor
If renin level is low: primary hypoaldosteronism or other
problems of adrenal gland
Treatment of hypokalemia
Although Sk is not an exact indicator of the total body K deficit,
a decrease (below 4 mEq/L) of 0.27 mEq/L is approximately
equivalent to 100 mEq/L of K deficit (upto a total deficit of
500 mEq/L). Sk levels of <2.0 mEq/L may reflect deficit of
>1000 mEq/L.
Four factors should be taken into account for correction:
Acid-base status: correction of coexisting metabolic acidosis without concomitant K replacement can cause the
Sk to fall lower.
Intravenous glucose administration: can cause K levels
to fall: in life threatening hypokalemia, initial K replacement should be given in glucose free solutions.
Overzealous administration of K can result in hyperkalemia.
Coexisting hypomagnesemia prevents correction of hypokalemia.
Intravenous K is reserved for patients unable to take K orally
or in severe life threatening situations, e.g. paralysis, digitalis
intoxication (with arrhythmias); hypokalemia induced hepatic
coma and those with ECG abnormalities.
Oral therapy is preferred because it rarely causes overshoot
hyperkalemia, in presence of normal renal function. Oral
supplement is given in doses of 20-120 mEq/day. Over the
630
Approach to Hypokalemia
counter salt substitutes is an economical source of K and
contain 3.5-7.5 mEq/Gm (5 gm is approximately 1 teaspoon).
K is available as K chloride, phosphate, bicarbonate, gluconate,
acetate and citrate. In general, KCl is appropriate to correct K
depletion and is the only preparation effective when there is
chloride depletion (metabolic alkalosis).
Oral K supplements come in a variety of liquids, powders
and tablets, containing 5-40 mEq/dose. Liquid preparations
are associated with gastrointestinal irritation. Enteric coated
KCl tablets are associated with GI ulcerations.
Intravenous K can be given safely at rates of 10mEq/
hour by peripheral vein without ECG monitoring and in
concentrations of upto 30mEq/L (to avoid pain/phlebitis).
If Sk is <2.5 mEq/L associated with ECG abnormalities
and/or severe neuromuscular complications, doses upto 40
mEq/hr can be given through a central vein with continuous
ECG monitoring. Doses up to this level are rarely necessary.
Frequent estimations of Sk (every 4-6 hrs) is the best guide
to replacement therapy. Once indications for intravenous/
emergent therapy have been resolved, less aggressive therapy
should be given.
Therapeutic measures in the treatment of chronic hypokalemia
include the use of oral K supplements and the K sparing diuretics
spironolactone, triamterene and amiloride. Combined use of
K supplements and K-sparing diuretics is contraindicated.
Following cases will exemplify how a systematic approach
can resolve the issue of hypokalemia and lead to appropriate
diagnosis.
Case 1:
36 yr old policeman presented with sudden onset weakness
of both lower & upper limbs for 2 days, more in lower
limbs & more in the morning hrs.
He was able to walk without support but had difficulty
in climbing stairs & to stand from sitting position. He
also felt difficulty in raising his arms overhead.
On the day of admission weakness increased & he was
not able to get up from bed without support in the
morning after a good sleep.
Past history: No past h/o similar illness, no h/o any chronic
illness i.e. HT, DM, Thyroid disorder. No h/o fever, headache,
vomiting. No h/o any drug intake
Family history: His twin brother had h/o similar symptoms,
was diagnosed as hypokalemic paralysis & treated with
potassium supplements but was not worked up for the
etiology of hypokalemia.
In view of this history, he was diagnosed as a case of familial
hypokalemic periodic paralysis.
On examination: Anxious, Pulse 104/min, regular; BP 140/80
mm of Hg, RR 24/min. Power in B/L LL & UL: proximal 2/5,
distal 5/5. Rest other systemic examination was unremarkable.
Patients motor weakness improved to normal power within
hours after supplementation of K i.e. when Sk reached to
normal value i.e. 4 mEq/L.
Investigations: Serum Na/K/Cl/TCO2 = 141/1.8/102/24
mEq/L,
ABG: pH 7.53, HCO3 27.8, pCO2 34, pO2 85.1, S. Creatinine
0.73mg/dl, S. Magnesium 2.3mg/dl and CPK was 1426 U/L.
Urinary K was13.7mEq/L when Sk was low, but after
correction of Sk, it was 56.7mEq/L. TTKG was 6.4. Urinary
chloride was 111,7mEq/L on admission. Urinary calcium/
creatinine ratio was 0.516. 24 hours urinary calcium was
high. Thus this was diagnosed to have Barters syndrome.
Episodic weakness beginning after age 25 is almost never due
to primary periodic paralysis. Further, low serum potassium
between attacks and absence of a similar family history should
raise strong suspicion of a secondary disorder.
Case 2:
As opposed to Case 1, this was a case of 70 years female.
She was diagnosed to have acute leukemia. She was admitted
to ICU with pulmonary edema and received intravenous
furosemide 40mg once and developed severe hypo K, leading
to life threatening cardiac arrhythmias. She had difficult to
treat hypo K and was referred to nephrology service. She
was investigated like the above case, and was found to
have high TTKG, high urinary chlorides and urine calcium/
creatinine ratio of 0.12 which would go in favor of thiazide
diuretics or Gitelmans syndrome. She had never received
thiazide diuretics and it was unlikely to have presentation of a
hereditary defect like Gitelmans syndrome at this age. Further
investigations revealed that she had lysozymuria secondary to
her leukemia which was causing hypokalemia.
The clinical features of Bartters syndrome (and possibly also
Gitelmans syndrome) are to a large extent caused by raised
concentrations of prostaglandins. By direct action and through
stimulation of natriuresis, these compounds stimulate renin
secretion, thereby promoting potassium wasting. They also
have a direct effect on aldosterone biosynthesis. Indomethacin
has been used in both syndromes, but especially Bartters, for
the beneficial effects of inhibiting prostaglandin synthesis.
631
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Agenda StyleDokumen48 halamanAgenda StyleUday KanthBelum ada peringkat
- BGFV CFDokumen11 halamanBGFV CFicaeeBelum ada peringkat
- Tree Infographics PGo 4 - 3Dokumen4 halamanTree Infographics PGo 4 - 303067okBelum ada peringkat
- Tree Infographics PGo 4 - 3Dokumen4 halamanTree Infographics PGo 4 - 303067okBelum ada peringkat
- Geriatric Functional AssessmentDokumen17 halamanGeriatric Functional Assessmentm2r71964Belum ada peringkat
- 4 5947281651888292650 PDFDokumen286 halaman4 5947281651888292650 PDFicaeeBelum ada peringkat
- DiabetesDokumen31 halamanDiabetesicaeeBelum ada peringkat
- Porter's 5 Forces Slide TemplateDokumen3 halamanPorter's 5 Forces Slide TemplategokulkBelum ada peringkat
- Agenda StyleDokumen48 halamanAgenda StyleUday KanthBelum ada peringkat
- 10 1001@jamainternmed 2018 5394 PDFDokumen7 halaman10 1001@jamainternmed 2018 5394 PDFicaeeBelum ada peringkat
- What Exactly Are PFTS?: - SpirometryDokumen67 halamanWhat Exactly Are PFTS?: - SpirometryicaeeBelum ada peringkat
- Increased Risk of Latent TB Infection in Pre-Diabetes and DiabetesDokumen9 halamanIncreased Risk of Latent TB Infection in Pre-Diabetes and DiabetesicaeeBelum ada peringkat
- Idf Diabetes Atlas: Sixth EditionDokumen160 halamanIdf Diabetes Atlas: Sixth EditionEverton Xavier RodriguesBelum ada peringkat
- 4 5947281651888292650 PDFDokumen286 halaman4 5947281651888292650 PDFicaeeBelum ada peringkat
- Thoracic CT Findings in Birt-Hogg-Dubé SyndromeDokumen4 halamanThoracic CT Findings in Birt-Hogg-Dubé SyndromeicaeeBelum ada peringkat
- Hallmarks of Cancer: The Next GenerationDokumen29 halamanHallmarks of Cancer: The Next GenerationAllanM.SchiffmanBelum ada peringkat
- CDC Tuberculosis - What The Physician Should KnowDokumen320 halamanCDC Tuberculosis - What The Physician Should KnowbillyBelum ada peringkat
- 17 - Cystic Lung Disease Achieving A Radiologic Diagnosis PDFDokumen8 halaman17 - Cystic Lung Disease Achieving A Radiologic Diagnosis PDFicaeeBelum ada peringkat
- GedvgDokumen7 halamanGedvgicaeeBelum ada peringkat
- HHS Public Access: The Immunology of Tuberculosis: From Bench To BedsideDokumen30 halamanHHS Public Access: The Immunology of Tuberculosis: From Bench To BedsideicaeeBelum ada peringkat
- HHS Public Access: The Immunology of Tuberculosis: From Bench To BedsideDokumen30 halamanHHS Public Access: The Immunology of Tuberculosis: From Bench To BedsideicaeeBelum ada peringkat
- ErsfcDokumen10 halamanErsfcicaeeBelum ada peringkat
- Diabetes, oxidative stress, and TB outcomesDokumen4 halamanDiabetes, oxidative stress, and TB outcomesicaeeBelum ada peringkat
- Treatment of Latent Tuberculosis Infection: Patrick Tang, MD, PHD James Johnston, MDDokumen9 halamanTreatment of Latent Tuberculosis Infection: Patrick Tang, MD, PHD James Johnston, MDicaeeBelum ada peringkat
- 31 - Multi-Institutional Oncogenic Driver Mutation Analysis in Lung Adenocarcinoma The Lung Cancer Mutation Consortium Experience PDFDokumen10 halaman31 - Multi-Institutional Oncogenic Driver Mutation Analysis in Lung Adenocarcinoma The Lung Cancer Mutation Consortium Experience PDFicaeeBelum ada peringkat
- 30 - Characteristics and Outcomes of Patients With Lung Cancer Harboring Multiple Molecular Alterations Results From The IFCT Study Biomarkers France PDFDokumen31 halaman30 - Characteristics and Outcomes of Patients With Lung Cancer Harboring Multiple Molecular Alterations Results From The IFCT Study Biomarkers France PDFicaeeBelum ada peringkat
- FervDokumen9 halamanFervicaeeBelum ada peringkat
- 5 - Lung Cancer in Never-Smokers A Case-Control Study in A Radon-Prone Area (Galicia, Spain) PDFDokumen8 halaman5 - Lung Cancer in Never-Smokers A Case-Control Study in A Radon-Prone Area (Galicia, Spain) PDFicaeeBelum ada peringkat
- H 5 XFRTDokumen11 halamanH 5 XFRTicaeeBelum ada peringkat
- Tilburg Frailty Indicator (TFI) : Part A Determinants of FrailtyDokumen3 halamanTilburg Frailty Indicator (TFI) : Part A Determinants of FrailtyicaeeBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- 621F Ap4405ccgbDokumen8 halaman621F Ap4405ccgbAlwinBelum ada peringkat
- Unit-1: Introduction: Question BankDokumen12 halamanUnit-1: Introduction: Question BankAmit BharadwajBelum ada peringkat
- Bluetooth TutorialDokumen349 halamanBluetooth Tutorialjohn bougsBelum ada peringkat
- Book Networks An Introduction by Mark NewmanDokumen394 halamanBook Networks An Introduction by Mark NewmanKhondokar Al MominBelum ada peringkat
- NAT Order of Operations 82Dokumen39 halamanNAT Order of Operations 82Kike PadillaBelum ada peringkat
- C6 RS6 Engine Wiring DiagramsDokumen30 halamanC6 RS6 Engine Wiring DiagramsArtur Arturowski100% (3)
- Sysmex Xs-800i1000i Instructions For Use User's ManualDokumen210 halamanSysmex Xs-800i1000i Instructions For Use User's ManualSean Chen67% (6)
- CAS-GEC04 Module11 Food-SecurityDokumen6 halamanCAS-GEC04 Module11 Food-SecurityPermalino Borja Rose AnneBelum ada peringkat
- ABP - IO Implementing - Domain - Driven - DesignDokumen109 halamanABP - IO Implementing - Domain - Driven - DesignddoruBelum ada peringkat
- August 03 2017 Recalls Mls (Ascpi)Dokumen6 halamanAugust 03 2017 Recalls Mls (Ascpi)Joanna Carel Lopez100% (3)
- House Rules For Jforce: Penalties (First Offence/Minor Offense) Penalties (First Offence/Major Offence)Dokumen4 halamanHouse Rules For Jforce: Penalties (First Offence/Minor Offense) Penalties (First Offence/Major Offence)Raphael Eyitayor TyBelum ada peringkat
- To Introduce BgjgjgmyselfDokumen2 halamanTo Introduce Bgjgjgmyselflikith333Belum ada peringkat
- Describing-Jobs-British-English StudentDokumen3 halamanDescribing-Jobs-British-English Studentrenata pedroso100% (1)
- Non Circumvention Non Disclosure Agreement (TERENCE) SGDokumen7 halamanNon Circumvention Non Disclosure Agreement (TERENCE) SGLin ChrisBelum ada peringkat
- Reader's Digest (November 2021)Dokumen172 halamanReader's Digest (November 2021)Sha MohebBelum ada peringkat
- Good Ethics Is Good BusinessDokumen9 halamanGood Ethics Is Good BusinesssumeetpatnaikBelum ada peringkat
- New Education Policy 2019Dokumen55 halamanNew Education Policy 2019Aakarshanam VenturesBelum ada peringkat
- PRODUCTDokumen82 halamanPRODUCTSrishti AggarwalBelum ada peringkat
- Yellowstone Food WebDokumen4 halamanYellowstone Food WebAmsyidi AsmidaBelum ada peringkat
- Sentinel 2 Products Specification DocumentDokumen510 halamanSentinel 2 Products Specification DocumentSherly BhengeBelum ada peringkat
- Pub - Essentials of Nuclear Medicine Imaging 5th Edition PDFDokumen584 halamanPub - Essentials of Nuclear Medicine Imaging 5th Edition PDFNick Lariccia100% (1)
- Catalogoclevite PDFDokumen6 halamanCatalogoclevite PDFDomingo YañezBelum ada peringkat
- Briana SmithDokumen3 halamanBriana SmithAbdul Rafay Ali KhanBelum ada peringkat
- National Standard Examination in Astronomy 2018-19 (NSEA) : Question Paper Code: A423Dokumen1 halamanNational Standard Examination in Astronomy 2018-19 (NSEA) : Question Paper Code: A423VASU JAINBelum ada peringkat
- Attributes and DialogsDokumen29 halamanAttributes and DialogsErdenegombo MunkhbaatarBelum ada peringkat
- GATE ECE 2006 Actual PaperDokumen33 halamanGATE ECE 2006 Actual Paperkibrom atsbhaBelum ada peringkat
- C6030 BrochureDokumen2 halamanC6030 Brochureibraheem aboyadakBelum ada peringkat
- John Titor TIME MACHINEDokumen21 halamanJohn Titor TIME MACHINEKevin Carey100% (1)
- Case Study Hotel The OrchidDokumen5 halamanCase Study Hotel The Orchidkkarankapoor100% (4)
- Requesting A Query in Zemanta Using PHPDokumen10 halamanRequesting A Query in Zemanta Using PHPAther SajjadBelum ada peringkat