Treating Depression in Prison Nursing Home
Diunggah oleh
Andreea NicolaeJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Treating Depression in Prison Nursing Home
Diunggah oleh
Andreea NicolaeHak Cipta:
Format Tersedia
Clinical
Case Studies
http://ccs.sagepub.com/
Treating Depression in the Prison Nursing Home : Demonstrating
Research-to-Practice Translation
Suzanne Meeks, Robin Sublett, Irene Kostiwa, James R. Rodgers and Donna Haddix
Clinical Case Studies 2008 7: 555 originally published online 25 July 2008
DOI: 10.1177/1534650108321303
The online version of this article can be found at:
http://ccs.sagepub.com/content/7/6/555
Published by:
http://www.sagepublications.com
Additional services and information for Clinical Case Studies can be found at:
Email Alerts: http://ccs.sagepub.com/cgi/alerts
Subscriptions: http://ccs.sagepub.com/subscriptions
Reprints: http://www.sagepub.com/journalsReprints.nav
Permissions: http://www.sagepub.com/journalsPermissions.nav
Citations: http://ccs.sagepub.com/content/7/6/555.refs.html
>> Version of Record - Nov 10, 2008
Proof - Jul 25, 2008
What is This?
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
Treating Depression in the Prison
Nursing Home
Clinical Case Studies
Volume 7 Number 6
December 2008 555-574
2008 Sage Publications
10.1177/1534650108321303
http://ccs.sagepub.com
hosted at
http://online.sagepub.com
Demonstrating Research-to-Practice
Translation
Suzanne Meeks
University of Louisville
Robin Sublett
Kentucky State Reformatory
Irene Kostiwa
James R. Rodgers
University of Louisville
Donna Haddix
Kentucky State Reformatory
We describe a theoretically grounded and empirically developed intervention for depression with
older men in a state reformatory nursing home. As the number of prisoners aging in place rises,
there is a critical need for research on mental health interventions in prison nursing homes where
inmates may be at high risk for depression and suicide. The participants in this project were four
male residents in the Kentucky state prison system nursing home; all four had diagnoses of major
depressive episodes. BE-ACTIV, a behavioral treatment for depression, is a hybrid approach that
combines one-to-one sessions with the depressed resident and work with staff. One-to-one sessions motivate the resident to engage in new activities, while meetings with nursing home staff
break down barriers to completion of pleasant events. Over the 10-week treatment, depressive
symptoms declined, and global functioning increased an average of 13 points per participant. Two
of the participants showed improved self-reported negative affect. Study results suggest that
BE-ACTIV is feasible in the prison nursing home and has the potential to improve the quality of
life for medically frail prisoners by helping them to identify meaningful or pleasant activities. The
cases illustrate importance of therapeutic relationships in the context of improving depressive
symptoms, and the possibility of building effective relationships in a setting with multiple barriers to effective treatment.
Keywords:
nursing homes; prisoners; depression; treatment
1 Theoretical and Research Basis
In this case study, we describe the application of a theoretically grounded and empirically developed intervention for depression to a specific population of older adults: older
men in a state reformatory nursing home. In recent years, researchers and funding agencies
555
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
556
Clinical Case Studies
have increasingly recognized the importance of translating research findings to clinical
settings as critical to the vitality and utility of any clinical science (e.g., National Institutes
of Health [NIH], 2007; Vernig, 2007). From the perspective of funding agencies, such
translation ensures that investment in scientific research results in advancements in direct
patient care; from the perspective of researchers, working in clinical settings stimulates new
research questions and enables real-world tests of theoretical models. The evidence-based
treatment movement encourages use of empirically tested interventions in practice settings,
but often the process of developing evidence-based treatments does not address the many
barriers to translating those treatments to varied practice settings. Older adults in particular
enter mental health treatment through a variety of settings that ranges from traditional mental health venues and outpatient medical practices to long-term care settings, such as
assisted living and nursing homes. Each of these settings presents novel challenges to treatment delivery that must be tested and overcome if treatments are to be widely available.
This study is part of a larger program of research for developing and testing the BE-ACTIV
intervention specifically designed for nursing home clients. This small demonstration project came about following an inquiry by the second author regarding whether BE-ACTIV
might be applicable to the prison nursing home setting. A demonstration of this nature not
only provides information to meet site-specific clinical needs, but also adds to the foundation of ecological validation for a treatment approach.
Mental Health Needs Among Older Prisoners
Despite the fact that the elderly appear to be a rapidly growing segment of the prison
population in the United States and other countries, there is relatively little work done to
date addressing the mental health issues related to aging in place in prisons. The general
population of prisoners in federal, state, and private facilities grew 28% between 1995 and
2000 (Bureau of Justice Statistics, 2003), but although elderly prisoners are still a minority
of the corrections population, the rate of older prisoners is growing at a much higher rate
(Aday, 1994). Little is known about these older prisoners; we found only a 1983 review of
federal data, case reports, and other nonresearch reports compiled by Goetting describing
this population. Her review indicated that the majority of elderly prisoners were men with
multiple incarcerations who were likely to have histories of violence.
Data from the Bureau of Prison Statistics suggest that the rate of mental illness among
prisoners is very high, with approximately half reporting symptoms (James & Glaze,
2006). Most symptoms were related to mood disorders. Prisoners with mental illness were
at higher risk than other prisoners for injury and victimization, as well as for longer prison
stays. Although rates of mental illness diminished with age, the percentage for older adults
remained significantly higher than for elders outside of prison. In one of the few epidemiological studies of psychiatric morbidity in prisons, Fazel, Hope, ODonnell, and Jacoby
(2001) surveyed 203 men over the age of 60 in 15 British prisons with populations of at
least 10 older prisoners. Diagnoses were determined by structured psychiatric interviews.
Approximately one third of the sample had Axis I diagnoses from the Diagnostic and
Statistical Manual of Mental Disorders (4th ed.) (DSM-IV; American Psychiatric
Association, 1994), and nearly all of these had diagnoses of a depressive disorder. Risk for
depressive disorder was related to medical condition, similar to other populations of older
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
Meeks et al. / Treating Depression in the Prison Nursing Home
557
adults that have been studied, but because the overall risk was much higher than for community-residing elders, it seems likely that older prisoners in nursing homes are at particular risk for depressive illness. When treatment needs of this same sample were examined,
it appeared that depressive disorders were medically undertreated (Fazel, Hope, ODonnell,
& Jacoby, 2004). Prisoners of all ages with mental illnesses are at risk for suicidal behavior (Senior et al., 2007), and suicide risk is correlated with age. Prisoners who have been in
prison longer are at higher risk for suicide (Konrad et al., 2007). In their comparison of
British prisoners with and without charted suicide risk, Senior and colleagues (2007) found
that those at risk had higher unmet support needs in the areas of safety, psychological
distress, and daily activities.
In their 2005 review of research on mental disorders in prison, Fazel and Lubbe conclude
that although epidemiological work and work on attention to interventions for violent
behaviors constitute a starting point, there is a critical need for research into what interventions can be effectively implemented in prison settings. There is some evidence that
prisoners do receive antidepressant medication (Baillargeon, Black, Contreras, Grady, &
Pulvino, 2002), although approximately 20% of prisoners diagnosed with major depression
did not receive antidepressants in this study, and there were gender, racial, and ethnic disparities in who received antidepressants and what type of antidepressants were prescribed.
Most state prisons, and all federal prisons, offer psychological and psychiatric services
(Bureau of Justice Statistics, 2003). Although some therapists have written about treating
prisoners (e.g., Pollock, Stowell-Smith, & Gpfert, 2006; Saunders, 2001), there is virtually no research on mental health interventions for this population, and the effectiveness of
interventions used with prisoners, particularly older prisoners, is unknown.
The BE-ACTIV Program for Depression in Nursing Homes
The BE-ACTIV program has been described in two previous publications (Meeks,
Looney, Van Haitsma, & Teri, 2008; Meeks, Teri, Van Haitsma, & Looney, 2006), and the
conceptual basis was described in a third article (Meeks & Depp, 2002). Briefly,
BE-ACTIV is a behavioral treatment that derives from the work of Lewinsohn and his colleagues (Lewinsohn, Hoberman, Teri, & Hautzinger, 1985). In this work, the central feature of depression is the combination of reduced positive reinforcement and positive impact
that arise in the context of disrupted routine, loss of control, and stress. The primary goal
of treatment is to interrupt the cycle of high negative affect and low positivity by systematically increasing opportunities for positive reinforcement. Empirical support for an activity-related intervention in nursing homes comes from a body of evidence accumulated by
Lawton and his colleagues (e.g., Lawton, 1997) that links resident activity level, affective
tone of activities, and levels of positive and negative affect to depression. This research
strongly suggests that participation in activities perceived as positive should be an important focus for intervention.
BE-ACTIV was adapted from a manualized treatment for depression in cognitively
impaired elders, developed and tested by Teri and colleagues (Teri, 1994, 1997; Teri,
Logston, & Uomoto, 1991; Teri, Logsdon, Uomoto, & Curry, 1997). Their research demonstrated that a behavioral intervention can be used successfully with impaired elders, and that
caregivers can learn to collaborate in increasing pleasant events and producing successful
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
558
Clinical Case Studies
outcomes for the elders they care for. Our preliminary work adapting this intervention to
the nursing home setting is summarized in two previous articles (Meeks et al., 2006; Meeks
et al., 2008). In place of family caregivers, BE-ACTIV requires that the therapist form a
working relationship with the activities staff of the nursing facility. This hybrid approach
to mental health care involves a combination of one-to-one sessions with the depressed resident and involvement of staff in implementing the plan for increasing pleasant events. Oneto-one sessions serve to motivate the resident to engage in new activities, while meetings
with nursing home staff help to break down barriers to the implementation of pleasant
events. In the pilot work, BE-ACTIV shows promise of improving depressive diagnoses,
increasing positive affect, and increasing activity levels of nursing home residents as compared to residents randomly assigned to treatment as usual (Meeks et al., 2008). Given that
prisoners in a correctional nursing home environment are at high risk for depression and suicide, and the prison environment affords few opportunities for pleasant daily activities, it
seems logical that BE-ACTIV could be a useful intervention for that setting.
2 Case Presentation
The participants in this demonstration project were four male prisoners who were residents in the nursing facility for the Kentucky state prison system. The participants volunteered to participate as part of a research project; the chief psychologist of the nursing
facility identified all residents who were presenting with depressed mood, had diagnoses of
depression, or were being treated with antidepressants. Of the 78 inmates on the unit, the
chief psychologist identified approximately 46 as potentially eligible (meeting criteria for
a depressive disorder and having a Mini-Mental Status Exam [MMSE] score of 14 or
above). Of these, 21 consented to screening, but only 6 were found to meet criteria for the
study after the initial research assessment. One of these men was transferred off the unit
and another died before they could receive the intervention; we completed the intervention
with the other four.
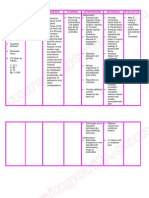
Table 1 shows the ages, race, and diagnostic status of the participants at baseline assessment. The youngest participant was 47,1 the oldest was 81, but they all had considerable
medical morbidity and all but one had some mild cognitive impairment. After baseline
assessment, they received weekly sessions of BE-ACTIV for 10 weeks, with a follow-up
assessment at the end of the 10 weeks. The therapists were two doctoral students in clinical psychology, one male and one female, with prior clinical experience in both inpatient
and nursing home settings, but with no prior experience in forensic settings. The staff member who collaborated in the treatment was a female recreational therapist assigned to the
nursing unit for several hours per week. Prior to her participation, she received a 3-hr
in-service training by the first author about the BE-ACTIV program, depression in general,
and her role in implementing pleasant events (see Meeks & Burton, 2004).
The prison nursing unit is configured more like a nursing home than a prison ward, with
a centrally located nursing station, semiprivate rooms, a mess hall, and a lounge area with
a TV. There is also a fenced, secure, outdoor patio with a small garden. Inmates of the nursing home are generally not allowed to be on the yard with the general prison population.
Recreational activities are usually held in the mess hall. Weekly sessions were held either
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
Meeks et al. / Treating Depression in the Prison Nursing Home
559
Table 1
Participant Baseline Characteristics
Age
Race
DSM-IV diagnosis
GAF
GDS
MMSE
COOP
Positive affecta
Negative affecta
Mr. A
Mr. B
61
African
American
MDD recurrent,
in partial
remission
47
African
American
Bipolar disorder,
current episode
MDE, severe,
without psychotic
features
53
21
29
10
14
10
60
18
24
7
5
10
Mr. C
Mr. D
58
White
81
White
MDD recurrent, in
partial remission
MDD, single
episode, severe,
without psychotic
features
53
25
26
8
14
15
45
22
23
13
9
20
Note: COOP, Dartmouth COOP Scales of Functioning; DSM-IV, Diagnostic and Statistical Manual of Mental
Disordersfourth edition; GAF, global assessment of functioning; GDS, Geriatric Depression Scale; MDD,
major depressive disorder; MDE, major depressive episode; MMSE, Mini-Mental Status Exam.
a. Positive and negative affect are sums of five items for baseline week.
in the residents room or in available office space on the nursing or psychiatric units. Care
was taken to optimize privacy but at times staff may have been within earshot of the shared
office space, or a roommate may have been present. During the 10 weeks of treatment,
therapists recorded weekly self-reported mood ratings, pleasant events, and the time that
the recreational therapist spent with the residents. The therapists completed diagnostic and
symptom assessments in the week following the tenth session for all except Mr. D, who was
in solitary confinement at the end of the treatment.
3 Presenting Complaints and History
All four participants were experiencing major depressive episodes (MDEs) at baseline,
two severe and two in partial remission (see Table 1). We deliberately did not request
information about the participants criminal background or convictions aside from the
length of time they had been incarcerated, choosing instead to treat depressive symptoms
in the context of the residents current situation. Individual presenting issues and history are
presented in the following paragraphs.
Mr. A
Mr. A was an African American male who had been in and out of the prison system in the
past and was incarcerated for a little more than a year at the time of the study because of a
violation of his parole. Staff reported that he was irritable, quiet, and withdrawn, rarely
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
560
Clinical Case Studies
participating in activities, spending much of his time in his room watching television or sleeping. He admitted that he had been hibernating because of ongoing worries about his health,
parole, and marriage. He also complained of nerves and said that he did not like being in
crowds or around other people, especially his fellow inmates. Mr. A reported having strained
relationships with most of his family members, although his aunt and cousin remained in contact with him. During the initial interview and early sessions, his speech was relatively quiet
and he appeared somewhat guarded in his responses. Mr. A was placed on the nursing unit following the loss of his leg resulting from poorly controlled diabetes mellitus and peripheral vascular disease. He had triple bypass surgery approximately 4 years prior to treatment. He
suffered a heart attack just a year before his incarceration, which he felt marked the beginning
of his current depressive episode. His health status and access to adequate health care were key
concerns for him; he feared dying in prison. Symptoms of depressed mood, weight gain,
insomnia, lack of energy, and difficulty concentrating endorsed at the initial interview contributed to a diagnosis of recurrent major depressive disorder (MDD) in partial remission.
Mr. B
Mr. B was an African American who had been incarcerated for 2 years. He was referred to
the program because staff members reported that he rarely spoke, did not attend activities, and
left his room only to eat or when instructed to do so. He would constantly lie in bed and watch
television even though only one TV channel was available to him. During the initial assessment, Mr. B was reserved and quiet, rarely making eye contact or speaking except to answer
direct questions. He stated that he didnt have much energy and that he felt really down
almost all of the time. His medical record included a diagnosis of schizophrenia, but based on
his endorsements on the Structured Clinical Interview for DSM-IV (SCID), he met criteria for
a history of mania and reported no psychosis outside of the context of affective episodes; so he
received the diagnosis of bipolar disorder, most recent episode depressed. His current episode
was rated as severe, but there was no evidence of current psychotic features. He agreed to participate in the project in hopes that he would feel better.
Mr. B stated that he felt that he had a normal childhood and had played football in high
school but that he always felt different than other people. He had no immediate family and
was divorced from his only wife. This was his second time in prison and he was determined
that his behavior would be such that he would be assured of parole at the earliest possible
opportunity. He reported that he had been moved to the prison nursing home to monitor and
care for his diabetes. Mr. B had many friends on the yard (in the general prison population),
and the move to the nursing home had isolated him from these friends because visits
between units required a special request sanction by the wardens office. Mr. B noted that
the larger rooms in the nursing facility were nice but that he missed his friends.
Mr. C
Mr. C was a white man who had been incarcerated for approximately 13 years. Staff suggested that he might be a good candidate for the study because of ongoing difficulties with
depressed mood, sleep disruption, and irritability. Despite these symptoms, Mr. C maximized
his daily routine by participating in available activities and remaining engaged with staff and
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
Meeks et al. / Treating Depression in the Prison Nursing Home
561
fellow inmates. He embodied the essence of behavioral activation even before his participation
in the study, and often stated I have to stay busy and hinted of a looming deeper depression.
Mr. C related a history of severe depressive episodes and alcohol abuse that began in his late
20s; he had a history of at least one grave suicide attempt. Mr. C was on the nursing unit primarily because of visual impairment combined with other medical problems. During the
initial interview, he complained of visions of bright lights and images of arbitrary floating
objects, which interfered with his concentration during the day and prevented him from
obtaining restorative sleep at night. He said these obtrusive visions began subsequent to a surgical procedure on his eyes. During the initial interview, his symptoms of depressed mood,
weight gain, insomnia, fatigue, thoughts of death, and significant ongoing distress contributed
to a diagnosis of MDD in partial remission. Interpersonally, Mr. C was very pleasant and agreeable but was noted to have a low frustration tolerance. He became visibly irritated when discussing his lack of control in terms of an inability to accomplish certain tasks either because
of his blindness or because of the restrictive environment of the prison.
Mr. D
Mr. D was a white man who had served more than 30 years in the prison system. The
staff noted that Mr. D was not liked by other inmates on the unit and that his problematic
and often oppositional behavior made him difficult to treat. Mr. D showed signs of memory loss and his score on the MMSE was a 23, indicating significant cognitive impairment.
He was often incontinent and resisted attempts by the staff to help him with self-care.
Usually, such resistance was met by calling the prison guard who would order him to bathe
and change clothes on the threat of punishment involving solitary confinement and loss of
privileges. On the SCID, Mr. D met threshold for all major depression items, earning him
a diagnosis of MDE, severe, without psychotic features. He had no recollection of a prior
episode, nor were any documented in his medical record.
Mr. D reported that he was a self-taught engineer and that he designed heating and air conditioning systems. He had worked for many years in a supervisory position in the prison
mechanical shop and had been involved in training other prisoners in skilled trades that could
be useful in and out of the prison system. Mr. D noted that because of his prison jobs, he felt
that his life had been useful. He put a great deal of emphasis on his ability to do real work.
As his memory difficulties progressed he was gradually removed from the teaching positions
and then from the prison shop. Ultimately, (probably because of his cognitive decline) he was
placed in the prison nursing home where he spent his time occasionally watching TV, eating
food from the prison commissary, and sleeping. Because of the sale of his home and belongings following the death of his wife, Mr. D had some money in the bank; he believed that
other prisoners only talked to him so that they could borrow money or share in his food. He
did not have any positive social relationships with other inmates on the unit.
4 Assessment
Diagnoses were determined using a modified version of the SCID (First, Spitzer,
Gibbon, & Williams, 2002). Either the first author or one of the therapists administered the
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
562
Clinical Case Studies
SCID 2 weeks prior to the first therapy session, and then again in the week following session 10. Depressive symptoms were also assessed using the Geriatric Depression Scale
(GDS; Brink et al., 1982), a 30-item, self-report scale designed for use with older adults.
We also administered the MMSE (Folstein, Folstein, & McHugh, 1975) as a screen for cognitive impairment, and the Dartmouth COOP Scales of Functioning (Nelson, Wasson,
Johnson, & Hays, n.d.). The COOP chart method of assessing functional status was developed by the Dartmouth Primary Care Cooperative Information Project (COOP) to provide
researchers and clinicians with a quick but valid means to assess adult and adolescent functioning in primary care (Nelson et al., 1987). COOP charts used included interference with
daily activities, interference with social activities, health changes, and overall self-rated
health, yielding a functional impairment scale ranging from 4 to 25 with higher scores indicating higher impairment. Participants rated their mood weekly using the Philadelphia
Geriatric Center Positive and Negative Affect Rating Scale (PNAR; Lawton, Kleban, Dean,
Rajagopal, & Parmelee, 1992). The PNAR produces positive and negative affect scales
each with a possible range of 5-25. We obtained demographic information, medical diagnoses, and medications from the prison health records. Results of baseline assessments are
shown in Table 1.
During the first session of BE-ACTIV, the therapist completes the initial version of the
Pleasant Events ScheduleNursing Home Version (PES-NH; Meeks, Heuerman, Ramsey,
Welsh, & White, 2005). This instrument helps the therapist and resident identify potentially
pleasant events that could be incorporated into the residents daily routine. An activity staff
member is invited to attend these first sessions. In this project, the recreational therapist
was present at all four first sessions to help the therapists determine what activities were
feasible within the prison nursing home. The follow-up version of the PES-NH was used
weekly during the therapy sessions to determine the number and pleasantness of the mens
activities during the time between sessions.
5 Case Conceptualization
With the exception of Mr. C, each of these men presented with pronounced reduction in
daily activities and a sense of hopelessness about the possibility of engaging in any activities that might be pleasant. As a result of placement on the nursing unit, all the men had
experienced significant losses related to meaningful social contact, including opportunities
to interact with friends and relatives on the yard (A, B, and C), and the opportunity to
engage in meaningful work including teaching others (D). They also reported reduction in
opportunities for leisure activities such as access to a weight room and library, and loss of
control over the availability of supplies or materials such as books, newspapers, art supplies, or television stations. Thus, each was experiencing reduced opportunities for positive
affect, in combination with increasing experiences of negative affect related to increased
health problems and disability, worries about parole (for A and B), and family stressors (A
and C). Figure 1 depicts these circumstances within the context of the conceptual basis of
BE-ACTIV from the work of Lewinsohn and colleagues (Lewinsohn et al., 1985). The
shaded box indicates the primary target of the intervention to increase opportunities for, and
control over, pleasant events so that the participants will experience increased positive
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
Meeks et al. / Treating Depression in the Prison Nursing Home
563
Figure 1
Conceptual Model of BE-ACTIV in the Prison Setting
Reduced opportunities for
social interaction and work
Loss of control over daily
activities
Increased negative affect
Antecedents:
Increased physical/cognitive
disability
Move to more restrictive
prison unit
Reduced positive
reinforcement
Reduced positive
affect
Increased negative
self-awareness
(negative cognitions)
Increased depression
(Persistent Dysphoria)
Vulnerabilities
Negative consequences
of Depression: Reduced
activity, negative
interpersonal interactions,
poorer health, more need
for care
affect. Note that although it is unavoidable that there will be some attention to reducing
negative affect and negative events associated therewith, this is not the focus of BE-ACTIV
because many sources of negative affect in nursing homes, and particularly in a prison nursing home, are unavoidable and largely immutable.
6 Course of Treatment and Assessment of Progress
Figure 2 shows increases in pleasant events for all participants over the course of therapy, with slight decreases apparent at therapy termination. Graphs of weekly mood ratings
(Figures 3-6) over the 12 weeks of the study suggest that the participants mood was unstable and highly reactive to environmental events, particularly at the beginning of the treatment period, but that as treatment progressed, around the fifth or sixth session, there was a
stabilization of negative affect for three out of four participants. The participants relationships with the staff recreational therapist showed both greater contact and greater trust over
the 10 weeks of treatment. Participants also reported a feeling of having more control over
their moods and choices of activities. Tables 1 and 2 show characteristics of the participants
at pre- and posttreatment assessments. These data suggest, contrary to our expectations,
that overall self-reported positive affect did not increase much over the course of treatment,
but that at least in the case of two of the participants, negative affect declined. Levels of
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
564
Clinical Case Studies
Table 2
Posttreatment Outcomes
Mr. A
DSM-IV diagnosis
MDD recurrent,
in partial
remission
GAF
GDS
MMSE
COOP
Positive affecta
Negative affecta
70
12
25
7
5
13
Mr. B
BPI, most recent
episode depressed,
in partial
remission
60
18
26
10
16
7
Mr. C
MDD recurrent,
in partial
remission
75
10
26
5
14
10
Mr. D
Unable to
complete
final
SCID
NA
NA
NA
NA
NA
NA
Note: See note to Table 1. NA, not available; SCID, Structured Clinical Interview for DSM-IV.
a. Positive and negative affect are sums of the final week of therapy.
physical disability remained stable across the 10 weeks. Depressive symptoms declined for
all participants for whom we were able to assess outcomes, and global functioning
increased an average of 13 points per participant. Specific characteristics of treatment
course for the participants are summarized in the following paragraphs.
Course of Treatment for Mr. A
Gaining a sense of mastery over his daily routine appeared to be a major theme for
Mr. A over the course of therapy, who stated that his mood problems were a matter of control. Control issues might be expected in a prison setting where inmates have few choices,
but Mr. A in particular found great relief and pleasure in the notion that he had some control, even if it was in the smallest facet of his daily routine. At the beginning of therapy, his
attention was largely focused on his upcoming parole hearing. Any excitement or positive
feelings concerning his possible release were undermined by significant worry about
returning to the free world with an amputated leg, that his marriage was deteriorating, and
that his former home and life would no longer be available to him. Thus, during the first
several sessions, Mr. As negative affect increased significantly reflecting his ongoing anxiety about an upcoming parole hearing and intense disappointment and anger on denial of
parole. Despite his past tendency to withdraw and isolate in the face of such negative feelings, Mr. A identified and engaged in activities that he found pleasurable as a part of the
study. Mr. A was highly creative and found pleasure in reading stories, writing, painting,
and listening to music. He described in vivid detail the pleasure that he felt when painting
or taking a hot bath which involved a type of mental escape from the confines of the
prison and an overall sense of well-being. He drew a strong connection between his chosen
activities and these positive feelings, and he often framed this in terms of a renewed sense
of control. As a result, he became highly committed to participating in these activities, independently increased the frequency of his baths, and never missed an opportunity to paint.
When faced with divorce from his wife around the Session 7, rather than follow his past
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
Meeks et al. / Treating Depression in the Prison Nursing Home
Figure 2
Change in Pleasant Activities (Frequency Pleasantness)
Over 12 Weeks for Each Prisoner
60.00
50.00
Frequency x pleasantness
40.00
30.00
20.00
10.00
0.00
Session1
Session 2
Session 3
Session 4
Session 5
Mr. A
Session 6
Mr. B
Session 7
Mr. C
Session 8
Session 9 Session 10
Mr. D
Figure 3
Change in Positive and Negative Affect Over 12 Weeks for Mr. A
4.50
4.00
3.50
3.00
2.50
2.00
1.50
1.00
B1
B2
T1
T2
T3
Mr. A Pos Affect
T4
T5
T6
T7
T8
Mr. A Neg Affect
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
T9
T10
565
566
Clinical Case Studies
Figure 4
Change in Positive and Negative Affect Over 12 Weeks for Mr. B
4.50
4.00
3.50
3.00
2.50
2.00
1.50
1.00
B1
B2
T1
T2
T3
T4
T5
Mr. D Pos Affect
T6
T7
T8
T9
T10
Mr. D Neg Affect
Figure 5
Change in Positive and Negative Affect Over 12 Weeks for Mr. C
4.50
4.00
3.50
3.00
2.50
2.00
1.50
1.00
B1
B2
T1
T2
T3
Mr. C Pos Affect
T4
T5
T6
T7
T8
Mr. C Neg Affect
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
T9
T10
Meeks et al. / Treating Depression in the Prison Nursing Home
567
Figure 6
Change in Positive and Negative Affect Over 12 Weeks for Mr. D
4.50
4.00
3.50
3.00
2.50
2.00
1.50
1.00
B1
B2
T1
T2
T3
Mr. B Pos Affect
T4
T5
T6
T7
T8
T9
T10
Mr. B Neg Affect
pattern of withdrawal, he continued to participate in activities and his negative affect
remained low. Nonetheless, as he felt better about himself, Mr. A also engaged in a pleasurable activity that had negative consequences for his health: eating sweets and high fat
snacks. With diabetes and cardiovascular problems, this increased snacking affected his
blood sugar and physical health. As he experienced physical discomfort, his worry about
his health and negative affect increased around Session 9. Despite the physical illness, he
continued to increase the frequency of his baths and also identified additional activities of
interest, such as writing a novel.
Course of Treatment for Mr. B
At baseline, Mr. B rarely participated in any activities or left his room. Figure 4 shows
that Mr. B experienced a relatively small range of both positive and negative affect. As the
intervention progressed, he found interests in numerous events including attending the regular Monday afternoon unit coffee, going to bingo games, taking a second weekly shower,
sitting outside, and listening to nature. Mr. B discovered an avid interest in listening to the
sounds of nature. During the sessions, he would describe in detail the appearance of the birds
that landed in the prison yard and would occasionally attempt to whistle like them. At the
conclusion of these exchanges, a rare smile would appear on his face. Toward the end of the
intervention, Mr. B was beginning to spend a small amount of time each day out on the patio
under a shady overhang attempting to hear whatever sounds were available including the
cows in the pasture beyond the wall, men working in the yard, and the blowing of the wind.
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
568
Clinical Case Studies
The weekly visit from the therapist appeared to become a pleasant event in itself. His
response to the therapist is evident in both activity level (Figure 2) and negative affect
(Figure 4). Mr. B noted that he looked forward to the meeting each week. Early in the
intervention, his compliance with planned activities seemed to be mainly the result of his
stated desire to fulfill the therapists requests, illustrating how the one-to-one relationship
can serve as a motivator to encourage depressed residents to try activities that they otherwise would not. As time progressed, the pleasure Mr. B gained from activity participation
appeared to become the impetus for his continued activity participation, even resulting in
participation in spontaneous activities such as talking to people on the unit, attending movie
night, and going outside more often than requested.
Course of Treatment for Mr. C
From the outset of the therapy, Mr. C emphasized his need to stay busy and engaged
in all available activities, except those that required vision, such as crafts, because of his
visual impairment. Rather than focusing on the enjoyment he received from these activities, however, he attributed his high level of engagement in activities and with others as an
avoidance of being alone in an empty room, where he believed he would inevitably focus
on his problems and become deeply depressed. Over the course of therapy, discussion of
activities as pleasant events and a source of positive affect appeared to help him derive
more satisfaction from the activities in which he already engaged. Identification of additional activities was challenging because he was so highly active, therefore much of the
work at baseline focused on increasing simple interactions with the staff and advocating for
his own needs. Like Mr. A, Mr. C expressed feelings of frustration regarding his lack of
control. For Mr. C this related to his inability to meet his own needs, in part because of his
visual impairment. He reported frustration regarding his unfulfilled requests of staff members. For example, he requested that his tape recorder be fixed so that he could listen to
books on tape, requested visits from his brother who was also an inmate but who resided
in the general population, and he requested that he be baptized. In the past, his requests
were largely passive, wherein he would ask once and then wait for it to be fulfilled. He
became quickly impatient when these things did not happen, and his negative feelings prevented him from further pursuing his needs. Thus, pleasant events identified at the beginning of the therapy involved interacting with staff and checking on the status of his
requests. Mr. C was generally very social in that he enjoyed talking to other inmates and to
staff. He was personable and appreciative of others, therefore the staff responded well to
him, further establishing these interactions as pleasant events. Thus, the activity of checking in with staff members helped him build better relationships and provided reminders to
staff about his needs, both of which gave him a sense of control. He often expressed his
genuine positive regard and respect for the recreational therapist, and in building this relationship, expressed a feeling of being supported, which he previously lacked. As a result of
his activity of checking in with staff regularly, he received a new tape recorder, received
approval for regularly scheduled visitation with his brother, and was baptized. Thus, his
interactions with staff led to further reinforcement via fulfillment of his requests, and in
turn an increase in other events, such as listening to books on tape and visiting with his
brother. A sharp increase in negative affect was noted in sessions 3 and 4, wherein Mr. C
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
Meeks et al. / Treating Depression in the Prison Nursing Home
569
discussed frustrations with unfulfilled needs such as not being able to get his laundry done,
not finding a chair to sit in at church, and most importantly his worry about his brothers
legal issues. These setbacks were addressed by focusing Mr. C on those things that were
within his control, such as the activities that he scheduled and in which he engaged.
Course of Treatment for Mr. D
Because of his dementia, although Mr. D could remember the majority of activities in
which he participated he had difficulty remembering the affect associated with those activities. He often lived in the moment and would interpret the past in light of his present mood.
However, there were a few activities about which he would give account in great detail and
which seemed to supersede his mood-specific interpretation. He consistently perceived
social activities such as coffees and bingo as negative events and felt they were unworthy
of his time. The one exception was whenever the activities director would place a cookie in
his mouth during coffee. He would remember this with great pleasure and enjoyed recounting this event. He appeared to enjoy going outside but reported that he was too old to
stand the summer heat. Mr. D attached great importance to events or activities that he considered worth his time. Attending religious services fell into this category, not so much
for the religious content as for the musical content. Mr. D described himself as a former
musician and attending religious service with the accompanying music seemed to restore
the affect associated with his memories of those days. Prior to the intervention, he rarely
associated with other residents in a positive manner and rarely took part in any activities.
Near the end of his time in the study, there was a rare live musical concert and hamburger
cookout that produced a spike of positive affect for Mr. D (see T6 in Figure 6) because it
combined, food, going outside, and his love of music.
As with Mr. B, the weekly therapy meetings appeared to become a pleasant event for
Mr. D. He enjoyed and responded to one-on-one interactions with both the therapist and the
recreational therapist. Along with his determination of activity meaningfulness, this type of
interaction seemed to underlie his compliance with therapy and his willingness to participate in any activity. Despite his bitter skepticism about participating in anything meaningful, Mr. D made an effort seemingly just to please the therapists, and his positive affect
appears to have increased somewhat over the course of treatment. However, Mr. Ds cognitive decline within a prison nursing home setting significantly affected the outcome of his
treatment. As an example, on two occasions, Mr. D initially refused his scheduled sessions
because of incontinence and a lack of clean clothing. Prisoners are issued a uniform and if
the uniform becomes soiled it is sometimes difficult to acquire new clothing. This may be
because clothing is limited and the necessary articles may not be readily available or it
could be because the unit is understaffed and certified nursing assistants (CNAs) have other
more pressing duties. In the first instance, the therapist was able to resolve the issue by finding new clothing for Mr. D, and in the second instance, Mr. D agreed to continue therapy
within the confines of his room. The other issue brought about by Mr. Ds cognitive decline
was his behavioral infractions on the unit and with the staff. These were often combative
and sometimes viewed as vindictive. In a prison population, problematic behaviors may be
dealt with in a punitive fashion and according to accepted prison protocols and standards. In
Mr. Ds case, his behavioral infractions resulted in segregation from the prison population.
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
570
Clinical Case Studies
Segregation takes place in a small cell where the prisoner is kept for 23 hr per day, with little contact with others and only few possessions (Bender, 2005). Mr. D was in segregation
during the final week of treatment and was unable to have his final assessment or meeting
with his therapist, as it was expected that he would be there for some time.
7 Complicating Factors
Clearly, prison nursing homes have characteristics that pose unique barriers to successful treatment of and recovery from depressive disorders. Some of the barriers we encountered are shared with other nursing homes. For example, the recreational therapist had very
little access to or budget for supplies that might enhance activities such as art projects, reading, and movies. Frequently this lack of an activities budget is found in nursing homes in
the private sector as well, although not surprisingly we found the lack of supplies to be
more extreme in the correctional setting. The limited amount of time the recreational therapist could be on the unit was also a problem, and staff shortages are frequently found in
private sector nursing homes as well. Lack of a private place to hold therapy sessions is a
problem that frequently occurs in all nursing homes, but this is significantly more of an
issue in the prison because of security considerations. Such lack of privacy may, especially
in prisons, impede open communication between the therapist and the client, and therefore
limit the power of the therapy relationship to effect change through motivating the client.
Nevertheless, all four of these men appear to have developed good working relationships
with their therapists, and all commented on the importance of the visits to them and for
motivating them to try new activities.
As nursing home patients are typically medically at risk and struggle with multiple
chronic health problems, the threat of illness events may have an impact on fluctuations in
mood, therapy compliance, and outcomes. We saw this in the prison setting as well. Mr. A,
B, and C were younger than the average nursing home resident, but all three suffered from
multiple chronic illnesses and disabilities and were significantly impaired in their ability to
navigate in their environments. Mr. A was particularly sensitive to changes in his health and
worried extensively about dying in prison. All four perceived, and complained of, poorer
medical care than they believed they would have received outside of prison. Although
Mr. B and C had relatively stable health over the time we worked with them, both Mr. A
and especially Mr. D showed medical instability that affected their mood and activity participation. Mr. Ds declining cognitive capacity was especially problematic because it
resulted in behavioral symptoms that within the prison context were interpreted and dealt
with as disciplinary infractions. This more punitive response was probably exacerbated by
both Mr. Ds premorbid personality and the type of crime for which he had been convicted;
simply put, he was not an easy person to like. His case, however, illustrates the effectiveness of individual therapy sessions for building a positive relationship that can lead to positive change against this backdrop of unstable or declining health.
Other life stressors also complicated the course of treatment for these men. Perhaps the
most powerful of these was the worry about parole hearings; in the case of Mr. A, denial of
parole constituted a major challenge to his improving mood, but he was able to use the
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
Meeks et al. / Treating Depression in the Prison Nursing Home
571
treatment process to work through his disappointment and manage his mood following the
denial. Additionally, Mr. A and C reported multiple family stressors, including legal problems of other family members, family illness, and the limited access to see or talk to family members. The presence of ongoing life stressors of this nature potentially not only
impedes the progress of therapy, but also provides opportunities to test the capacity of the
resident to use skills taught in the treatment to improve mood.
A final complication that we encountered in this project was the low participation by
inmates identified as potentially eligible. The refusal rate for this project was not noticeably different than refusal rates we have encountered for depressed residents in nursing
homes outside of prison. However, despite the fact that the mental health staff at the facility used their own knowledge of the inmates to nominate them for participation, the
majority of inmates who consented to be screened did not meet criteria for major or
minor depressive episodes when interviewed with the SCID. This led us to wonder
whether there was a reluctance among the residents to admit to depression, particularly
to strangers. It is possible that, had the screenings been conducted with staff members
with whom inmates had already developed some form of relationship, we would have
identified more depression.
8 Follow-Up
Participants continued to be monitored by the prisons chief psychologist, with the following outcomes approximately 6 months after termination of therapy.
Mr. A
Unfortunately, Mr. As worries about dying in prison were borne out. Approximately 1
month after the completion of the program, Mr. A died as a result of complications following a fall. Mr. A had been medically unstable for some time. However, prior to his death,
Mr. As mood improved noticeably, he was happier, and he shared more. In addition, he
continued to participate in arts and crafts as well as bingo.
Mr. B
At the beginning of the program Mr. B only rarely left his room. Though he has not
regressed to that level, Mr. B continues to spend an excessive amount of time in his room
sleeping and staring at the television. His participation in group activities has declined but
he does attend bingo. Another previously identified pleasurable activity that he has maintained is taking regular showers. His church attendance and writing have declined though
not to preprogram levels. His affect remains primarily flat though he does occasionally
smile and his eye contact has improved from what it was at the beginning of the study. A
particular pleasurable activity for Mr. B was to go outside and observe nature.
Unfortunately, he has not been able to engage in this for some time because of a prolonged
period of inclement weather.
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
572
Clinical Case Studies
Mr. C
Mr. C continues to come to bingo and enjoys his books on tape. He has had some visits from
his brother which is another identified pleasurable event. He has maintained his previous level
of high activity and has added a job of wiping down the hand rails in the nursing care unit.
He has a roommate with whom he gets along and he continues to be social, visiting with other
inmates on a regular basis. Mr. C appears upbeat and describes his mood as good.
Mr. D
Mr. D has significantly decreased in cognitive functioning since the end of the program.
In addition, his health has declined. He spends most of his time in his room sleeping. He
now requires a wheel chair for ambulation. He continues to be disliked by staff and other
inmates and is now serving segregation time for displaying threatening behavior toward his
roommate. Despite this, Mr. D can respond pleasantly when treated with compassion.
9 Treatment Implications of the Cases
These four cases suggest that, once cases are identified, BE-ACTIV is feasible in the prison
nursing home and has the potential to improve the quality of life for medically frail prisoners
by helping them to identify meaningful or pleasant activities. The cases illustrate how the relationship with the therapist is an important aspect of the intervention, despite its behavioral
emphasis. In addition, BE-ACTIV encourages the development of a productive and positive
relationship with recreational staff members, giving them explicit tasks that can help structure
their work with prisoners and allowing prisoners to have an ally within the prison system. The
cases show how relatively few resources can be brought to make a difference in the activity
levels and satisfaction of inmates, and that increases in activity levels can lead to improvements
in negative affect, depressive symptoms, and psychiatric functioning. The intervention uses relatively few resources that are already available in most prison settings, and therefore, to the
extent that treatment for depression may reduce morbidity, activities of daily life (ADL) dependency, and excess mortality, such a treatment may be seen as a cost-effective means of preventing other problems that might arise for depressed inmates. The cases studies presented
here, therefore, suggest that it may be appropriate to further evaluate BE-ACTIV in the prison
setting in a larger, controlled research study.
10 Recommendations to Clinicians and Students
Clinicians working in prison settings face numerous barriers that have been explored in
recently published books (Pollock et al., 2006; Saunders, 2001). Despite these barriers, our
cases illustrate that a useful therapistinmate relationship can be established relatively quickly
in the context of a structured, manualized, behavioral treatment. We found that it was not necessary to explore the prisoners past experiences or criminal activity to treat their depression
effectively. A working partnership with nonmental health staff in the prison unit is a critical
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
Meeks et al. / Treating Depression in the Prison Nursing Home
573
part of BE-ACTIV and serves two purposes: (a) to ensure that pleasant events are implemented and (b) to provide the inmate with an ally whose function extends beyond mental
health care to enjoyment of day-to-day life. Furthermore, the alliance with a recreational therapist helps increase the likelihood that activities will be maintained once active mental health
treatment is ended, although we did not test this assumption in the present project.
Note
1. To protect the anonymity of the participants, inmates actual ages are not given in the case descriptions.
References
Aday, R. (1994). Golden years behind bars: Special programs and facilities for elderly inmates [Electronic version]. Federal Probation, 58(2), 47.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.).
Washington, DC: Author.
Baillargeon, J., Black, S. A., Contreras, S., Grady, J., & Pulvino, J. (2002). Anti-depressant prescribing patterns
among prison inmates with depressive disorders. U.S. Department of Justice Document #194054. Retrieved
January 16, 2008, from the National Criminal Justice Reference Service Web site: http://www.ncjrs.gov/pdffiles1/nij/grants/194054.pdf
Bender, E. (2005). Prison punishment exacerbates inmates psychiatric illness. Psychiatric News, 40, 15-16.
Bureau of Justice Statistics. (2003). Census of state and federal correctional facilities, 2000. Revised 2003.
Retrieved January 16, 2008, from http://www.ojp.usdoj.gov/bjs/pub/pdf/csfcf00.pdf
Brink, T. L., Yesavage, J. A., Owen, L., Heersema, P., Aey, M., & Rose, T. L. (1982). Screening tests for geriatric depression. Clinical Gerontologist, 1, 37-43.
Fazel, S., Hope, T., ODonnell, I., & Jacoby, R. (2001). Hidden psychiatric morbidity in elderly prisoners
[Electronic version]. British Journal of Psychiatry, 179, 535-539.
Fazel, S., Hope, T., ODonnell, I., & Jacoby, R. (2004). Unmet treatment needs of older prisoners: A primary
care survey. Age and Ageing, 33, 396-398.
Fazel, S., & Lubbe, S. (2005). Prevalence and characteristics of mental disorders in jails and prisons. Current
Opinion in Psychiatry, 18, 550-554.
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (2002, November). Structured Clinical Interview
for DSM-IV-TR Axis I disorders, research version, patient edition (SCID-I/P). New York: Biometrics
Research, New York State Psychiatric Institute.
Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). Mini-mental state: A practical method for grading
the cognitive state of patients for the clinician. Journal of Psychiatry Research, 12, 189-198.
Goetting, A. (1983). The elderly in prison. Journal of Research in Crime and Delinquency, 20, 291-309.
James, D. J., & Glaze, L. E. (2006). Mental health problems of prison and jail inmates. U. S. Department of
Justice, Bureau of Justice Statistics, NCJ 213600, September. Retrieved January 16, 2008, from
http://www.ojp.usdoj.gov/bjs/pub/pdf/mhppji.pdf
Konrad, N., Daigle, M. S., Daniel, A. E., Dear, G. E., Frottier. P., Hayes, L. M., et al. (2007). Preventing suicide in prisons, Part I. Recommendations from the International Association for Suicide Prevention Task
Force on Suicide in Prisons. Crisis, 28, 113-131.
Lawton, M. P. (1997). Positive and negative affective states among older people in long-term care. In R. L.
Rubinstein & M. P. Lawton (Eds.), Depression in long-term and residential care (pp. 29-54). New York:
Springer.
Lawton, M. P., Kleban, M. H., Dean, J., Rajagopal, D., & Parmelee, P. A. (1992). The factorial generality of
brief positive and negative affect measures. Journal of Gerontology: Psychological Sciences, 47, 228-237.
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
574
Clinical Case Studies
Lewinsohn, P. M., Hoberman, H., Teri, L., & Hautzinger, M. (1985). An integrative theory of depression. In S. Reiss
& R. R. Bootzin (Eds.), Theoretical issues in behavior therapy (pp. 331-359). New York: Academic Press.
Meeks, S., & Burton, E. G. (2004). Nursing home staff characteristics and knowledge gain from a didactic
workshop on depression and behavior management. Gerontology and Geriatrics Education, 25, 57-66.
Meeks, S., & Depp, C. A. (2002). Pleasant-events based behavioral intervention for depression in nursing home
residents: A conceptual and empirical foundation. Clinical Gerontologist, 25, 125-148.
Meeks, S., Heuerman, A., Ramsey, S., Welsh, D., & White, K. (2005, November). The Pleasant Events
ScaleNursing Home Version: Development and validation. Paper presented at the Annual Meeting of the
Gerontological Society of America, Orlando, FL.
Meeks, S., Looney, S. W., Van Haitsma, K., & Teri, L. (2008). BE-ACTIV: A staff-assisted, behavioral intervention for depression in nursing homes. The Gerontologist, 48, 105-114.
Meeks, S., Teri, L., Van Haitsma, K., & Looney, S.W. (2006). Increasing pleasant events in the nursing home:
Collaborative behavioral treatment for depression. Clinical Case Studies, 5, 287-304.
Nelson, E. C., Wasson, J., Johnson, D. J., & Hays, R. D. (n.d.). Dartmouth COOP functional health assessment
charts: Brief measures for clinical practice. Retrieved June 16, 2005, from the Dartmouth University COOP
Project Web site: http://www.dartmouth.edu/~coopproj/more_charts.html
Nelson, E. C., Wasson, J., Kirk, J., Keller, A., Clark, D., Dietrich, A., et al. (1987). Assessment of function in
routine clinical practice: Description of the COOP chart method and preliminary findings. Journal of
Chronic Diseases, 40, 55S-63S.
National Institutes of Health. (2007). Re-engineering the clinical research enterprise. Retrieved January 9,
2008, from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp
Pollock, P. H., Stowell-Smith, M., & Gpfert, M. (Eds.). (2006). Cognitive analytic therapy for offenders.
London: Routledge.
Saunders, J. W. (Ed.). (2001). Life within hidden worlds. Psychotherapy in prisons. London: Karnac Books.
Senior, J., Hayes, A. J., Pratt, D., Thomas, S. D., Fahy, T., Leese, M., et al. (2007). The identification and management of suicide risk in local prisons. Journal of Forensic Psychiatry and Psychology, 18, 368-380.
Teri, L. (1994). Behavioral treatment of depression in patients with dementia. Alzheimers Disease and
Associated Disorders, 8, 66-74.
Teri, L. (1997). The relation between research on depression and a treatment program: One model. In R. L. Rubinstein
& M. P. Lawton (Eds.), Depression in long-term and residential care (pp. 129-153). New York: Springer.
Teri, L., Logsdon, R., & Uomoto, J. (1991). Treatment of depression in patients with Alzheimers disease.
Therapist Manual. Seattle: University of Washington School of Medicine.
Teri, L., Logsdon, R. G., Uomoto, J., & McCurry, S. M. (1997). Behavioral treatment of depression in dementia patients: A controlled clinical trial. Journal of Gerontology: Psychological Sciences, 52B, P159-P166.
Vernig, P. M. (2007). From science to practice: Bridging the gap with translational research. APS Observer, 20(2).
Retrieved January 19, 2008, from http://www.psychologicalscience.org/observer/getArticle.cfm? id=2133
Suzanne Meeks, PhD, is a professor of clinical psychology in the Department of Psychological and Brain
Sciences at the University of Louisville. She has been involved in clinical work and research in nursing homes
for more than 20 years as part of her broader research focus on mental illness in late life.
Robin Sublett, PhD, is the chief psychologist at the Kentucky State Reformatory. She currently provides clinical services in the Nursing Care Facility as well as supervises the General Psychological Services.
Irene Kostiwa, MA, is a doctoral student in clinical psychology at the University of Louisville. Her research
interests include sleep and mood problems among long-term care residents.
James R. Rodgers, MA, is a doctoral student in clinical psychology at the University of Louisville, completing his internship at the Southwest Texas Veterans Health Center during the 2008-2009 academic year. His
research and clinical interests focus on end-of-life care.
Donna Haddix is a recreation leader at the Kentucky State Reformatory. She supervises recreation services in
the Correctional Psychiatric Unit as well as the Nursing Care Facility.
Downloaded from ccs.sagepub.com by Andreea Nicoleta Nicolae on October 12, 2011
Anda mungkin juga menyukai
- HNR 3700 - Community Perceptions of Prison Health Care Final ProposalDokumen18 halamanHNR 3700 - Community Perceptions of Prison Health Care Final Proposalapi-582630906Belum ada peringkat
- Running Head: Annotated Bibliography Tomkins 1Dokumen9 halamanRunning Head: Annotated Bibliography Tomkins 1api-303232478Belum ada peringkat
- 13 PGDokumen13 halaman13 PGSamson MbuguaBelum ada peringkat
- KFP Part 4Dokumen14 halamanKFP Part 4api-726694735Belum ada peringkat
- Mental Health and Palliative Care Literature ReviewDokumen4 halamanMental Health and Palliative Care Literature ReviewafdtbwkhbBelum ada peringkat
- Running Head: Confinement and Mental Illness in U.S Prisoners 1Dokumen19 halamanRunning Head: Confinement and Mental Illness in U.S Prisoners 1Tonnie KiamaBelum ada peringkat
- Inpatient Geriatric Psychiatry: Optimum Care, Emerging Limitations, and Realistic GoalsDari EverandInpatient Geriatric Psychiatry: Optimum Care, Emerging Limitations, and Realistic GoalsHoward H. FennBelum ada peringkat
- 140.editedDokumen19 halaman140.editedTonnie KiamaBelum ada peringkat
- Example Review and Critique of A Qualitative StudyDokumen6 halamanExample Review and Critique of A Qualitative StudyWinnifer KongBelum ada peringkat
- Centre For Policy On Ageing Information Service Selected ReadingsDokumen62 halamanCentre For Policy On Ageing Information Service Selected ReadingsC Hendra WijayaBelum ada peringkat
- 2017, Family Intervention in A Prison Environment A Systematic Literature ReviewDokumen17 halaman2017, Family Intervention in A Prison Environment A Systematic Literature ReviewEduardo RamirezBelum ada peringkat
- Scholarly PaperDokumen6 halamanScholarly Paperapi-430368919Belum ada peringkat
- RecommendedDokumen9 halamanRecommendedMaya Putri Haryanti100% (1)
- Mental Health FacilitiesDokumen11 halamanMental Health FacilitiesMiKayla PenningsBelum ada peringkat
- Nursing Annotated BibliographyDokumen7 halamanNursing Annotated BibliographyAssignment Help Australia100% (1)
- 675-Article Text-2218-2-10-20130830Dokumen22 halaman675-Article Text-2218-2-10-20130830Marijana PsihoBelum ada peringkat
- Running Head: Health Care Setting Impact On Patients With Neurodegenerative DiseasesDokumen14 halamanRunning Head: Health Care Setting Impact On Patients With Neurodegenerative DiseasesJackie WilsonBelum ada peringkat
- Ageing Prisoners: An Introduction To Geriatric Health-Care Challenges in Correctional FacilitiesDokumen24 halamanAgeing Prisoners: An Introduction To Geriatric Health-Care Challenges in Correctional FacilitiesepraetorianBelum ada peringkat
- Evaluation of A Comedy Intervention To Improve Coping and Help-Seeking For Mental Health Problems in A Women ' S PrisonDokumen8 halamanEvaluation of A Comedy Intervention To Improve Coping and Help-Seeking For Mental Health Problems in A Women ' S PrisonGINA ZEINBelum ada peringkat
- Policy BriefDokumen10 halamanPolicy Briefapi-607761527Belum ada peringkat
- Negative Impacts That Prison Has On Mentally Ill PeopleDokumen15 halamanNegative Impacts That Prison Has On Mentally Ill PeopleIAN100% (1)
- The Role of Family Empowerment and Family Resilience On Recovery From PsychosisDokumen12 halamanThe Role of Family Empowerment and Family Resilience On Recovery From PsychosisSyahwira ramadhanBelum ada peringkat
- Peer Victimization PaperDokumen21 halamanPeer Victimization Paperapi-249176612Belum ada peringkat
- 8.2.1 Rosenhan (1973) On Being Sane in Insane Places.: Studies Clinical PsychologyDokumen3 halaman8.2.1 Rosenhan (1973) On Being Sane in Insane Places.: Studies Clinical PsychologySara AbrahamBelum ada peringkat
- Walker 2020Dokumen22 halamanWalker 2020Stella GašparušBelum ada peringkat
- Major mental disorders linked to higher criminality and violence ratesDokumen20 halamanMajor mental disorders linked to higher criminality and violence ratesAndrés Rojas OrtegaBelum ada peringkat
- A Literature Review Psychiatric BoardingDokumen13 halamanA Literature Review Psychiatric Boardingn0nijitynum3100% (1)
- 15stefaan de Smet PDFDokumen9 halaman15stefaan de Smet PDFJorge PlanoBelum ada peringkat
- Three Propositions For An Evidence-Based Medical AnthropologyDokumen16 halamanThree Propositions For An Evidence-Based Medical AnthropologypatriciamadariagaBelum ada peringkat
- Gender Differences Among Prisoners in Drug TreatmentDokumen22 halamanGender Differences Among Prisoners in Drug TreatmentlosangelesBelum ada peringkat
- An Anatomy of LonelinessDokumen4 halamanAn Anatomy of LonelinessTheodore LiwonganBelum ada peringkat
- Archives of Psychiatric Nursing: Krystyna de Jacq, Allison Andreno Norful, Elaine LarsonDokumen9 halamanArchives of Psychiatric Nursing: Krystyna de Jacq, Allison Andreno Norful, Elaine LarsonleticiaBelum ada peringkat
- Coleman Et Al. - JPRDokumen7 halamanColeman Et Al. - JPRWitrisyahPutriBelum ada peringkat
- Senior FinalDokumen23 halamanSenior Finalapi-350348558Belum ada peringkat
- Research PaperDokumen12 halamanResearch Paperapi-451581488Belum ada peringkat
- Behaviour Research and Therapy: Alan E. KazdinDokumen12 halamanBehaviour Research and Therapy: Alan E. KazdinDroguBelum ada peringkat
- Literature Review Suicide in PrisonDokumen4 halamanLiterature Review Suicide in Prisonafmzrvaxhdzxjs100% (1)
- Tiro IdesDokumen12 halamanTiro IdesArturo MelgarBelum ada peringkat
- St. Denis - Forensic Psych in ChileDokumen8 halamanSt. Denis - Forensic Psych in ChileKendall RunyanBelum ada peringkat
- Pt. B. D. Sharma University of Health Sciences, RohtakDokumen30 halamanPt. B. D. Sharma University of Health Sciences, RohtaknikhilBelum ada peringkat
- Psychology Assessment - I - M1Dokumen42 halamanPsychology Assessment - I - M1Brinda ChughBelum ada peringkat
- Literature Review DeliriumDokumen7 halamanLiterature Review Deliriumafmzadevfeeeat100% (1)
- Literature ReviewDokumen11 halamanLiterature Reviewapi-582875150Belum ada peringkat
- Running Head: Effects of Follow-Up Psychiatric Care 1Dokumen20 halamanRunning Head: Effects of Follow-Up Psychiatric Care 1api-409577818Belum ada peringkat
- 22 Depression Alliance Abstracts, July 09Dokumen6 halaman22 Depression Alliance Abstracts, July 09sunkissedchiffonBelum ada peringkat
- Sosial Capital's Link to Depression, Pain & SymptomsDokumen9 halamanSosial Capital's Link to Depression, Pain & SymptomsSiti Anisa FatmawatiBelum ada peringkat
- Neurobehavioural and cognitive function linked to childhood trauma in homeless adultsDokumen13 halamanNeurobehavioural and cognitive function linked to childhood trauma in homeless adultsReal NoloseBelum ada peringkat
- A Time-Series Study of The Treatment of Panic DisorderDokumen21 halamanA Time-Series Study of The Treatment of Panic Disordermetramor8745Belum ada peringkat
- Cognitive-Behavioral Interventions With Older AdulDokumen38 halamanCognitive-Behavioral Interventions With Older AdulMARIELA LIZETH VALENTE CORTEZBelum ada peringkat
- Long Term Effects of Anabolic SteroidsDokumen3 halamanLong Term Effects of Anabolic SteroidsMadelaine EvangelioBelum ada peringkat
- Module 5 PaperDokumen8 halamanModule 5 PaperWinterBelum ada peringkat
- Racial Differences in Self-Reports of Sleep Duration in A Population-Based StudyDokumen8 halamanRacial Differences in Self-Reports of Sleep Duration in A Population-Based StudyRivhan FauzanBelum ada peringkat
- 5 Western Models For Mental Health BentallDokumen4 halaman5 Western Models For Mental Health BentallimanuelcBelum ada peringkat
- Intelligence and Personality As PredictorsDokumen96 halamanIntelligence and Personality As PredictorsTrifan DamianBelum ada peringkat
- Psych 3Dokumen17 halamanPsych 3austinviernes99Belum ada peringkat
- A CritiqueDokumen9 halamanA Critiquewangarichristine12Belum ada peringkat
- Exploring The - Near-Suicide - Phenomenon Using Mindsponge TheoryDokumen3 halamanExploring The - Near-Suicide - Phenomenon Using Mindsponge TheoryLuyện TrầnBelum ada peringkat
- Sa Psy150-28Dokumen2 halamanSa Psy150-28api-438183736Belum ada peringkat
- Eugenics as a Factor in the Prevention of Mental DiseaseDari EverandEugenics as a Factor in the Prevention of Mental DiseaseBelum ada peringkat
- Addiction Recovery Management: Theory, Research and PracticeDari EverandAddiction Recovery Management: Theory, Research and PracticeBelum ada peringkat
- Animalele - Material Terapie ABADokumen17 halamanAnimalele - Material Terapie ABAAndreea NicolaeBelum ada peringkat
- David Gordon - Phoenix - Therapeutic Patterns of Milton H. EricksonDokumen203 halamanDavid Gordon - Phoenix - Therapeutic Patterns of Milton H. EricksonNora Grigoruta100% (9)
- Time Limited Psychotherapy PDFDokumen52 halamanTime Limited Psychotherapy PDFlara_2772Belum ada peringkat
- 3 Full PDFDokumen21 halaman3 Full PDFAndreea NicolaeBelum ada peringkat
- Behavioral Therapy For Anxiety DisordersDokumen18 halamanBehavioral Therapy For Anxiety DisordersAndreea NicolaeBelum ada peringkat
- 555 Full PDFDokumen21 halaman555 Full PDFAndreea NicolaeBelum ada peringkat
- An Investigation of Health Anxiety in FamiliesDokumen12 halamanAn Investigation of Health Anxiety in FamiliesAndreea NicolaeBelum ada peringkat
- 382 Full PDFDokumen22 halaman382 Full PDFAndreea NicolaeBelum ada peringkat
- Behavioral Therapy For Anxiety DisordersDokumen18 halamanBehavioral Therapy For Anxiety DisordersAndreea NicolaeBelum ada peringkat
- A Time-Series Study of The Treatment of Panic DisorderDokumen21 halamanA Time-Series Study of The Treatment of Panic Disordermetramor8745Belum ada peringkat
- Oppositional Defiant DisorderDokumen13 halamanOppositional Defiant DisorderAndreea NicolaeBelum ada peringkat
- Behavioral Therapy For Anxiety DisordersDokumen18 halamanBehavioral Therapy For Anxiety DisordersAndreea NicolaeBelum ada peringkat
- Cognitive InterventionDokumen13 halamanCognitive InterventionAndreea NicolaeBelum ada peringkat
- Behavioral Activation in Breast Cancer PatientsDokumen14 halamanBehavioral Activation in Breast Cancer PatientsAndreea NicolaeBelum ada peringkat
- Don't Kick Me OutDokumen14 halamanDon't Kick Me OutAndreea NicolaeBelum ada peringkat
- RADDokumen25 halamanRADAndreea NicolaeBelum ada peringkat
- Relation ASD - ADHDDokumen16 halamanRelation ASD - ADHDAndreea NicolaeBelum ada peringkat
- The Role of Attention - ASDDokumen13 halamanThe Role of Attention - ASDAndreea NicolaeBelum ada peringkat
- Behavioral Activation As An Intervention For Coexistent Depressive and Anxiety SymptomsDokumen13 halamanBehavioral Activation As An Intervention For Coexistent Depressive and Anxiety SymptomsAndreea NicolaeBelum ada peringkat
- Assessment and Behavioral Treatment of Selective MutismDokumen22 halamanAssessment and Behavioral Treatment of Selective MutismAndreea NicolaeBelum ada peringkat
- 9 Feeding Therapy in A Child With Autistic DisorderDokumen12 halaman9 Feeding Therapy in A Child With Autistic DisorderArden AriandaBelum ada peringkat
- The Five Therapeutic RelationshipsDokumen16 halamanThe Five Therapeutic RelationshipsAndreea Nicolae100% (2)
- The Use of Homework Success For A Child With Attention-Deficit/ Hyperactivity Disorder, Predominantly Inattentive TypeDokumen14 halamanThe Use of Homework Success For A Child With Attention-Deficit/ Hyperactivity Disorder, Predominantly Inattentive TypeAndreea NicolaeBelum ada peringkat
- Internet-Related Psychopathology Clinical Phenotypes and PerspectivesDokumen138 halamanInternet-Related Psychopathology Clinical Phenotypes and PerspectivesAndreea NicolaeBelum ada peringkat
- Behavioral Therapy For Anxiety DisordersDokumen18 halamanBehavioral Therapy For Anxiety DisordersAndreea NicolaeBelum ada peringkat
- Trating Food Refusal in Adolescent With Asperger's DisorderDokumen14 halamanTrating Food Refusal in Adolescent With Asperger's DisorderAndreea NicolaeBelum ada peringkat
- Behavioral Therapy For Anxiety DisordersDokumen18 halamanBehavioral Therapy For Anxiety DisordersAndreea NicolaeBelum ada peringkat
- Therapist As Trauma SurvivorsDokumen16 halamanTherapist As Trauma SurvivorsAndreea NicolaeBelum ada peringkat
- The Role of Attention - ASDDokumen13 halamanThe Role of Attention - ASDAndreea NicolaeBelum ada peringkat
- Thrombocytopenia in PregnancyDokumen12 halamanThrombocytopenia in PregnancyzoyaBelum ada peringkat
- CetirizineDokumen2 halamanCetirizinelintangBelum ada peringkat
- Appstat PDFDokumen197 halamanAppstat PDFrfactor0976Belum ada peringkat
- Opini-Can Hemoglobin-Hematocrit Relationship Be Used To Assess Hydration StatusDokumen4 halamanOpini-Can Hemoglobin-Hematocrit Relationship Be Used To Assess Hydration StatusBoby ShéBelum ada peringkat
- 05 Abpg2103 Topic 1Dokumen14 halaman05 Abpg2103 Topic 1Ummu SolihahBelum ada peringkat
- Adhd Case Study by Martial Arts Master Greg MoodyDokumen11 halamanAdhd Case Study by Martial Arts Master Greg MoodyMaster Greg Moody100% (1)
- Psychiatric Medication Guidelines Pregnancy LactationDokumen27 halamanPsychiatric Medication Guidelines Pregnancy LactationSunija SelvamBelum ada peringkat
- Team 2 Presents Vital SignsDokumen44 halamanTeam 2 Presents Vital Signswiwin100% (1)
- Critical Thinking Exercise NCM 106Dokumen5 halamanCritical Thinking Exercise NCM 106Julienne Sanchez-SalazarBelum ada peringkat
- Otomicroscopy (Adult, Peds)Dokumen4 halamanOtomicroscopy (Adult, Peds)Carmen EneaBelum ada peringkat
- Urology Instrumentation A Comprehensive GiudeDokumen185 halamanUrology Instrumentation A Comprehensive GiudeJade Kenneth Gonzales Lomansoc93% (15)
- TylenolDokumen2 halamanTylenolAle_deCastroBelum ada peringkat
- AyusynkDokumen2 halamanAyusynknahar570Belum ada peringkat
- Jurnal Case Report Carcinoma Maxillaris PDFDokumen3 halamanJurnal Case Report Carcinoma Maxillaris PDFEnvhy WinaBelum ada peringkat
- Sean Barnett-Nurs362resumeDokumen2 halamanSean Barnett-Nurs362resumeapi-252467227Belum ada peringkat
- 3.guía CLSI Documento H3 - A6Dokumen56 halaman3.guía CLSI Documento H3 - A6Majo Tovar67% (3)
- ResumeDokumen3 halamanResumeDeviprasad MahantaBelum ada peringkat
- Access For Dialysis - Surgical and Radiologic ProceduresDokumen436 halamanAccess For Dialysis - Surgical and Radiologic ProceduresAriadna Mariniuc100% (1)
- Yin Yang MedicineDokumen78 halamanYin Yang Medicineashutosh2501100% (2)
- Nursing Care Plan Cesarian DeliveryDokumen2 halamanNursing Care Plan Cesarian Deliveryderic97% (39)
- Principles of Management of Poisoned Patient: 09/09/1440 DR Abdelmonem G. Madboly 1Dokumen19 halamanPrinciples of Management of Poisoned Patient: 09/09/1440 DR Abdelmonem G. Madboly 1JyotiBelum ada peringkat
- Vanessa Perez ResumeDokumen2 halamanVanessa Perez Resumeapi-247302506Belum ada peringkat
- Anodontia of Permanent Teeth - A Case ReportDokumen3 halamanAnodontia of Permanent Teeth - A Case Reportanandsingh001Belum ada peringkat
- Acute Tonsil Lo Pharyngitis Slide ShowDokumen9 halamanAcute Tonsil Lo Pharyngitis Slide ShowVine Millan GarciaBelum ada peringkat
- Homeopathic Treatment of MigraineDokumen3 halamanHomeopathic Treatment of MigraineRPh Krishna Chandra JagritBelum ada peringkat
- Wellington ICU Drug Manual 2013Dokumen444 halamanWellington ICU Drug Manual 2013khangsiean89Belum ada peringkat
- Flea Allergy DermatitisDokumen3 halamanFlea Allergy DermatitisDhea Febrianty OllybriieBelum ada peringkat
- Pencegahan Dan Pengendalian Infeksi Di Rumah Sakit Dan FasyankesDokumen60 halamanPencegahan Dan Pengendalian Infeksi Di Rumah Sakit Dan FasyankesNesa MuktariBelum ada peringkat
- AAOS Abstracts GuidelinesDokumen6 halamanAAOS Abstracts GuidelinesNuno PaisBelum ada peringkat
- Carmarthen in SpotlightDokumen1 halamanCarmarthen in SpotlightDigital MediaBelum ada peringkat