Igm 9
Diunggah oleh
Nutriologo Luis Garcia CampechanoJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Igm 9
Diunggah oleh
Nutriologo Luis Garcia CampechanoHak Cipta:
Format Tersedia
Special Series: Practical Diagnosis and Management of Immunodeficiency
Patients with abnormal IgM levels: assessment,
clinical interpretation, and treatment
Hans D. Ochs, MD
INTRODUCTION
This review of the role of IgM in cognate immunity is part of
a series on ambulatory diagnoses and management of primary
immune deficiency diseases edited by Chitra Dinakar, University of Missouri.1 IgM is phylogenetically the earliest
antibody class identified and the first immunoglobulin isotype to appear in the circulation after exposure to a new
antigen. IgM plays an important role in the ontogeny of B
cells and in early cognate immune responses.2 VDJ rearrangement of the immunoglobulin heavy chain occurs at the pre
B-cell stage, when light chains are still of the surrogate type
(5/VpreB). Further maturation leads to immature B cells,
which express surface IgM and IgD and carry and light
chains, creating a functional B-cell receptor that allows antigen recognition and further development into unswitched
memory B cells (IgM/D, CD27). After interaction with
the T-cell receptor of antigen-specific CD4 T cells via major
histocompatibility complex II and costimulatory molecules
(CD40 ligand [CD40L]/CD40, inducible costimulator
[ICOS]/ICOS ligand), mature B cells undergo isotype switching, resulting in B cells expressing CD27 and IgG, IgA, or
IgE. Whereas IgM is responsible for rapid and early generation of antibody, long-term humoral immunity is initiated by
the production of high-affinity IgG or IgA antibody. The
demonstration of IgM antibodies to a specific infectious agent
can be used as an indicator of recent infection. The presence
of IgM in cord blood (20 mg/dL) may indicate prenatal
infection because IgM antibody cannot be acquired from the
mother by transplacental passage. In infants, IgM serum
levels increase rapidly from a mean of 11 mg/dL at term to 55
mg/dL at 1 year of age. By 2 years, IgM concentration is
approximately 60% of that in adults.
IgM is expressed as a monomer on the surface of nave and
mature unswitched B cells, where it forms the antigen receptor complex together with the coreceptors Ig and Ig. If
secreted, most IgM forms a pentameric complex, which stays
Affiliations: Department of Pediatrics, University of Washington School
of Medicine, Childrens Hospital and Regional Medical Center, Seattle
Childrens Hospital Research Institute, Seattle, Washington.
Disclosures: Author has nothing to disclose.
Funding Sources: Funded by an unrestricted educational grant from
Talecris Biotherapeutics.
Received for publication December 20, 2007; Received in revised form
February 20, 2008; Accepted for publication February 28, 2008.
VOLUME 100, MAY, 2008
mostly (70% to 80%) intravascular. Its half-life is approximately 6 days, in contrast to IgG, which has a half-life of 21
to 28 days. IgM antibodies are uniquely efficient in agglutination and are highly avid because of their multimeric nature
and strong complement fixation.
IgM LEVELS AND DISEASE
Because of the central role of IgM in the development of B
cells and because class switch recombination (CSR) and
somatic hypermutation (SH) require sophisticated intrinsic
and extrinsic mechanisms, evaluation of serum IgM levels
provides an informative insight into primary and secondary
immunodeficiency disorders. Quantitation of serum immunoglobulin is generally performed by nephelometry that detects
IgM at concentrations as low as 6 mg/dL. IgM is age dependent during childhood but otherwise stable over time. If
abnormal, IgM levels, like all tests, should be rechecked to
avoid laboratory errors. Loss of serum proteins can occur
through the gut, in the kidneys, or by excessive drainage from
the thoracic or peritoneal cavities and may lead to hypogammaglobulinemia, affecting low-molecular-weight immunoglobulins (eg, IgG and IgA) more than IgM, which is
secreted as a 900,000-molecular-weight protein. Since the
pentameric structure of IgM favors agglutination, quantitation of isohemagglutinin titers is an excellent test for functional IgM. Low serum IgM levels in the context of hypogammaglobulinemia may indicate molecular defects that
disrupt cell signaling or gene expression directly, thus interfering with B- and T-cell development. On the other hand,
mutations of genes required for CSR and SH result frequently
in increased serum IgM levels.
SELECTIVE IgM DEFICIENCY
Isolated absence or reduction of serum IgM in view of otherwise normal immunoglobulin isotypes and T-cell function
is known as selective IgM deficiency. Some patients with
selective IgM deficiency are asymptomatic. Selective IgM
deficiency has been defined as IgM levels of less than 2 SDs
or less than 10% of the mean for age (eg, 5 to 15 mg/dL in
infants and children and 20 mg/dL in adults). Considering
the importance of IgM in the ontogeny of B-cell development, the selective absence of IgM in the presence of normal
numbers of circulating B cells is difficult to explain. In vitro
studies have identified defective B-cell function35 or the
509
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Assignment On Diesel Engine OverhaulingDokumen19 halamanAssignment On Diesel Engine OverhaulingRuwan Susantha100% (3)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
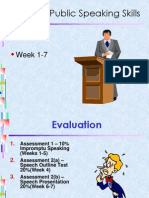
- TOPIC 1 - Public Speaking SkillsDokumen72 halamanTOPIC 1 - Public Speaking SkillsAyan AkupBelum ada peringkat
- Introduction To Pharmacy ManagementDokumen28 halamanIntroduction To Pharmacy ManagementSirry HidayaniBelum ada peringkat
- Violent Extremism in South AfricaDokumen20 halamanViolent Extremism in South AfricaMulidsahayaBelum ada peringkat
- Antenna Tilt GuidelinesDokumen24 halamanAntenna Tilt GuidelinesJorge Romeo Gaitan Rivera100% (5)
- DC-DC Converter Reliability Design and TestingDokumen16 halamanDC-DC Converter Reliability Design and TestinggirisanaBelum ada peringkat
- Dysphagia in The Elderly (Marco Teoìrico)Dokumen12 halamanDysphagia in The Elderly (Marco Teoìrico)Nutriologo Luis Garcia CampechanoBelum ada peringkat
- Recto Law and Maceda LawDokumen3 halamanRecto Law and Maceda Lawjulie cairo0% (1)
- AripiprazoleDokumen2 halamanAripiprazoleKrisianne Mae Lorenzo FranciscoBelum ada peringkat
- Dysphagia in The Elderly 2015Dokumen11 halamanDysphagia in The Elderly 2015Nutriologo Luis Garcia CampechanoBelum ada peringkat
- Implantes Reacciones DrogasDokumen47 halamanImplantes Reacciones DrogasNutriologo Luis Garcia CampechanoBelum ada peringkat
- Rofes Et Al-2014-Neurogastroenterology & MotilityDokumen10 halamanRofes Et Al-2014-Neurogastroenterology & MotilityNutriologo Luis Garcia CampechanoBelum ada peringkat
- 1364 13Dokumen11 halaman1364 13Nutriologo Luis Garcia CampechanoBelum ada peringkat
- 818979Dokumen14 halaman818979Nutriologo Luis Garcia CampechanoBelum ada peringkat
- IPAQ English Self-Admin ShortDokumen3 halamanIPAQ English Self-Admin ShortDavid Curtis MintahBelum ada peringkat
- Ipaq PDFDokumen4 halamanIpaq PDFNutriologo Luis Garcia CampechanoBelum ada peringkat
- X-Linked Hyper-Igm Syndrome With Cd40Lg Mutation: Two Case Reports and Literature Review in Taiwanese PatientsDokumen6 halamanX-Linked Hyper-Igm Syndrome With Cd40Lg Mutation: Two Case Reports and Literature Review in Taiwanese PatientsNutriologo Luis Garcia CampechanoBelum ada peringkat
- Mouse DisthrophyDokumen12 halamanMouse DisthrophyNutriologo Luis Garcia CampechanoBelum ada peringkat
- Diseases MusculsarDokumen21 halamanDiseases MusculsarNutriologo Luis Garcia CampechanoBelum ada peringkat
- IGM2Dokumen11 halamanIGM2Nutriologo Luis Garcia CampechanoBelum ada peringkat
- Igm 5Dokumen9 halamanIgm 5Nutriologo Luis Garcia CampechanoBelum ada peringkat
- Igm 11Dokumen7 halamanIgm 11Nutriologo Luis Garcia CampechanoBelum ada peringkat
- Period On CIADokumen586 halamanPeriod On CIANutriologo Luis Garcia CampechanoBelum ada peringkat
- A Photograph Poem Summary in EnglishDokumen6 halamanA Photograph Poem Summary in Englishpappu kalaBelum ada peringkat
- Maintain Records and Bond EmployeesDokumen5 halamanMaintain Records and Bond EmployeesAngel Frankie RamosBelum ada peringkat
- Beacon Finland JAK ATB Coupling System PDFDokumen6 halamanBeacon Finland JAK ATB Coupling System PDFsyahrir anasBelum ada peringkat
- Princes of the Apocalypse Locations IndexDokumen2 halamanPrinces of the Apocalypse Locations IndexPedroManzelaDuarteBelum ada peringkat
- Impact of Technology On Future JobsDokumen29 halamanImpact of Technology On Future Jobsmehrunnisa99Belum ada peringkat
- Song Grade XiDokumen12 halamanSong Grade XiM Ridho KurniawanBelum ada peringkat
- CSE 191 Homework Proposition LogicDokumen5 halamanCSE 191 Homework Proposition LogicJyothi AnkumBelum ada peringkat
- Reporter Matt Rudd Goes On An Extraordinary Plane RideDokumen2 halamanReporter Matt Rudd Goes On An Extraordinary Plane RideHAnhh TrầnnBelum ada peringkat
- Touw 1982 Roses MedievalDokumen14 halamanTouw 1982 Roses MedievalВладан СтанковићBelum ada peringkat
- MKTG10001Dokumen38 halamanMKTG10001Jessica KokBelum ada peringkat
- Executive Summary WynnDokumen5 halamanExecutive Summary Wynnapi-505730347Belum ada peringkat
- Physics 5th Edition Walker Test BankDokumen24 halamanPhysics 5th Edition Walker Test BankKathyHernandeznobt100% (31)
- The Bible in Picture and Story (1889)Dokumen250 halamanThe Bible in Picture and Story (1889)serjutoBelum ada peringkat
- Mathematical Language and Symbols ExplainedDokumen5 halamanMathematical Language and Symbols Explainedcyra6flores6verderaBelum ada peringkat
- Vector DifferentiationDokumen2 halamanVector DifferentiationJayashree MisalBelum ada peringkat
- Capoeira and The Politics of InequalityDokumen411 halamanCapoeira and The Politics of InequalityPipoca AngoleraBelum ada peringkat
- RUN ON SENTENCES AND FRAGMENTS GUIDEDokumen17 halamanRUN ON SENTENCES AND FRAGMENTS GUIDEWAHEED-UL -ISLAMBelum ada peringkat
- Eq 1Dokumen4 halamanEq 1jppblckmnBelum ada peringkat
- Coils and InductanceDokumen6 halamanCoils and InductanceJoseGarciaRuizBelum ada peringkat
- Mayans.M.C.S05E03.720p.WEB .x265-MiNX - SRTDokumen44 halamanMayans.M.C.S05E03.720p.WEB .x265-MiNX - SRTmariabelisamarBelum ada peringkat
- Physics: PAPER 1 Multiple ChoiceDokumen20 halamanPhysics: PAPER 1 Multiple Choicelulz.l.n.sBelum ada peringkat
- Parle Sales DistributionDokumen21 halamanParle Sales Distributionkakki1088Belum ada peringkat