Untitled
Diunggah oleh
hassanien221271Deskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Untitled
Diunggah oleh
hassanien221271Hak Cipta:
Format Tersedia
First Aid for Neck/Spine Injury
© American Institute for Preventive Medicine
________________________________________
Anything that puts too much pressure or force on the neck or back can result in
a neck and/or spinal injury. Common causes are:
• Accidents - with cars, motorcycles, snowmobiles, toboggans, rollerblades
, etc.
• Falls - especially from high places
• Diving mishaps - from diving into water that is too shallow
• A hard blow to the neck or back while playing a contact sport such as fo
otball
• Violent acts such as a gunshot wound that penetrates the head, neck or t
runk
Suspect a neck injury, too, if a head injury has occurred.
Some neck and spinal injuries can be serious because they could result in paraly
sis. These need emergency medical care. Others, such as whiplash, can be tempora
ry, minor injuries.
A mild whiplash typically causes neck pain and stiffness the following day. Some
people, though, have trouble raising their heads off the pillow the next mornin
g. Physical therapy and a collar to support the neck are the most common types o
f treatment. It often takes three to four months for all symptoms to disappear.
Prevention
• Use padded headrests in your car to prevent whiplash.
• Drive carefully and defensively.
• Wear seatbelts, both lap belts and shoulder harnesses.
• Buckle children into approved car seats appropriate for their age.
• Wear a helmet whenever you ride a bicycle or motorcycle or when you roll
er skate or roller blade.
• Wear the recommended safety equipment for contact sports.
• Take care when jumping up and down on a trampoline, climbing a ladder or
checking a roof.
• Check the depth of the water before diving into it. Do not dive into wat
er that is less that 9 feet deep. Never dive into an above-ground pool.
NOTE: IF YOU SUSPECT A NECK OR BACK INJURY IN YOU OR SOMEONE ELSE, YOU MUST KEEP
THE NECK AND/OR BACK PERFECTLY STILL UNTIL AN EMERGENCY CREW ARRIVES. DO NOT MO
VE SOMEONE WITH A SUSPECTED NECK OR SPINE INJURY UNLESS THE PERSON MUST BE MOVED
BECAUSE HIS OR HER SAFETY IS IN DANGER. ANY MOVEMENT OF THE HEAD, NECK OR BACK
COULD RESULT IN PARALYSIS OR DEATH. IMMOBILIZE THE NECK BY HOLDING THE HEAD, NEC
K AND SHOULDERS PERFECTLY STILL. USE BOTH HANDS, ONE ON EACH SIDE OF THE HEAD.
Questions to Ask
Is the injured person not breathing and has no pulse?
Perform CPR, but without moving the neck or spine and Seek Emergency Car
e. (See "CPR") But when you do the "Airway and Breathing" part of CPR, do not ti
lt the head back or move the head or neck. Instead, pull the lower jaw (chin) fo
rward to open the airway.
Is the injured person not breathing, but has a pulse?
Perform "Rescue Breathing" without moving the neck or spine and Seek Eme
rgency Care.(See "Airway and Breathing".) But do not tilt the head back or move
the head or neck. Instead, pull the lower jaw (chin) forward to open the airway.
Spinal injury: First aid
If you suspect a back or neck (spinal) injury, do not move the affected person.
Permanent paralysis and other serious complications can result. Assume a person
has a spinal injury if:
There's evidence of a head injury with an ongoing change in the person's
level of consciousness.
The person complains of severe pain in his or her neck or back.
The person won't move his or her neck.
An injury has exerted substantial force on the back or head.
The person complains of weakness, numbness or paralysis or lacks control
of his or her limbs, bladder or bowel.
The neck or back is twisted or positioned oddly.
If you suspect someone has a spinal injury:
Dial 911 or call for emergency medical assistance.
Keep the person still. Place heavy towels on both sides of the neck or h
old the head and neck to prevent movement. The goal of first aid for a spinal in
jury is to keep the person in much the same position as he or she was found.
Provide as much first aid as possible without moving the person's head o
r neck. If the person shows no signs of circulation (breathing, coughing or move
ment), begin CPR, but do not tilt the head back to open the airway. Use your fin
gers to gently grasp the jaw and lift it forward.
If you absolutely must roll the person because he or she is vomiting, ch
oking on blood or in danger of further injury, use at least two people. Work tog
ether to keep the person's head, neck and back aligned while rolling the person
onto one side.
Spinal cord injury
ARTICLE SECTIONS
Introduction
Signs and symptoms
Causes
Risk factors
When to seek medical advice
Screening and diagnosis
Complications
Treatment
Prevention
Coping skills
Introduction
In 1995, actor Christopher Reeve fell off a horse and severely damaged his spina
l cord, leaving him paralyzed from the neck down. From then until his death in 2
004, the silver screen Superman became the most famous face of spinal cord injur
y.
Most spinal cord injury causes permanent disability or loss of movement (paralys
is) and sensation below the site of the injury. Paralysis that involves the majo
rity of the body, including the arms and legs, is called quadriplegia or tetrapl
egia. When a spinal cord injury affects only the lower body, the condition is ca
lled paraplegia.
Christopher Reeve's celebrity and advocacy raised national interest, awareness a
nd research funding for spinal cord injury. Many scientists are optimistic that
important advances will occur to make the repair of injured spinal cords a reach
able goal. In the meantime, treatments and rehabilitation allow many people with
spinal cord injury to lead productive, independent lives.
Signs and symptoms
CLICK TO ENLARGE
Spinal cord injuries
Spinal cord injury symptoms depend on two factors:
The location of the injury. In general, injuries that are higher in your
spinal cord produce more paralysis. For example, a spinal cord injury at the ne
ck level may cause paralysis in both arms and legs and make it impossible to bre
athe without a respirator, while a lower injury may affect only your legs and lo
wer parts of your body.
The severity of the injury. Spinal cord injuries are classified as parti
al or complete, depending on how much of the cord width is damaged.
In a partial spinal cord injury, which may also be called an incomplete injury,
the spinal cord is able to convey some messages to or from your brain. So people
with partial spinal cord injury retain some sensation and possibly some motor f
unction below the affected area.
A complete spinal cord injury is defined by total or near-total loss of motor fu
nction and sensation below the area of injury. However, even in a complete injur
y, the spinal cord is almost never completely cut in half. Doctors use the term
"complete" to describe a large amount of damage to the spinal cord. It's a key d
istinction because many people with partial spinal cord injuries are able to exp
erience significant recovery, while those with complete injuries are not.
Spinal cord injuries of any kind may result in one or more of the following sign
s and symptoms:
Pain or an intense stinging sensation caused by damage to the nerve fibe
rs in your spinal cord
Loss of movement
Loss of sensation, including the ability to feel heat, cold and touch
Loss of bowel or bladder control
Exaggerated reflex activities or spasms
Changes in sexual function, sexual sensitivity and fertility
Difficulty breathing, coughing or clearing secretions from your lungs
Emergency signs and symptoms
Emergency signs and symptoms of spinal cord injury after a head injury or accide
nt may include:
Fading in and out of consciousness
Extreme back pain or pressure in your neck, head or back
Weakness, incoordination or paralysis in any part of your body
Numbness, tingling or loss of sensation in your hands, fingers, feet or
toes
Loss of bladder or bowel control
Difficulty with balance and walking
Impaired breathing after injury
An oddly positioned or twisted neck or back
Spinal cord injuries
Paralysis of the lower half of the body is called paraplegia. Paralysis of both
arms and legs is called quadriplegia.
Causes
Your brain and central nervous system
Together, your spinal cord and your brain make up your central nervous system, w
hich controls most of the functions of your body. Your spinal cord runs approxim
ately 15 to 17 inches from the base of your brain to your waist and is composed
of long nerve fibers that carry messages to and from your brain.
These nerve fibers feed into nerve roots that emerge between your vertebrae — th
e 33 bones that surround your spinal cord and make up your backbone. There, the
nerve fibers organize into peripheral nerves that extend to the rest of your bod
y.
Injury may be traumatic or nontraumatic
A traumatic spinal cord injury may stem from a sudden, traumatic blow to your sp
ine that fractures, dislocates, crushes or compresses one or more of your verteb
rae. It may also result from a gunshot or knife wound that penetrates and cuts y
our spinal cord. Additional damage usually occurs over days or weeks because of
bleeding, swelling, inflammation and fluid accumulation in and around your spina
l cord.
Nontraumatic spinal cord injury may be caused by arthritis, cancer, blood vessel
problems or bleeding, inflammation or infections, or disk degeneration of the s
pine.
Damage to nerve fibers
Whether the cause is traumatic or nontraumatic, the damage affects the nerve fib
ers passing through the injured area and may impair part or all of your correspo
nding muscles and nerves below the injury site. Spinal injuries occur most frequ
ently in the neck (cervical) and lower back (thoracic and lumbar) areas. A thora
cic or lumbar injury can affect leg, bowel and bladder control, and sexual funct
ion. A cervical injury may affect breathing as well as movements of your upper a
nd lower limbs.
The spinal cord ends at the lower border of the first vertebra in your lower bac
k — known as a lumbar vertebra. So injuries below this vertebra actually don't i
nvolve the spinal cord. However, an injury to this part of your back or pelvis m
ay damage nerve roots in the area and may cause some loss of function in the leg
s, as well as difficulty with bowel and bladder control and sexual function.
Common causes of spinal cord injury
The most common causes of spinal cord injury in the United States are:
Motor vehicle accidents. Auto and motorcycle accidents are the leading c
ause of spinal cord injuries, accounting for almost 50 percent of new spinal cor
d injuries each year.
Acts of violence. About 15 percent of spinal cord injuries result from v
iolent encounters, often involving gunshot and knife wounds.
Falls. Spinal cord injury after age 65 is most often caused by a fall. O
verall, falls make up approximately 22 percent of spinal cord injuries.
Sports and recreation injuries. Athletic activities such as impact sport
s and diving in shallow water cause about 8 percent of spinal cord injuries.
Diseases. Cancer, infections, arthritis and inflammation of the spinal c
ord also cause spinal cord injuries each year
Risk factors
Although a spinal cord injury is usually the result of an unexpected accident th
at can happen to anyone, some groups of people have a higher risk of sustaining
a spinal cord injury. These include:
Men. Spinal cord injury affects a disproportionate amount of men. In fac
t, women account for only about 20 percent of spinal cord injuries in the United
States.
Young adults and seniors. People are most often injured between ages 16
and 30. But there is another peak in people older than 60. Motor vehicle crashes
are the leading cause of spinal cord injury for young people, while falls cause
most injuries in older adults. However, in some cities, acts of violence — such
as gunshot wounds, stabbings and assaults — are a major cause of spinal cord in
jury.
People who are active in sports. Sports and recreational activities caus
e 8 percent of the 11,000 spinal cord injuries in the United States each year, a
lthough sports-related spinal cord injury is becoming less common. High-risk ath
letic activities include football, rugby, wrestling, gymnastics, diving, surfing
, ice hockey and downhill skiing.
People with predisposing conditions. A relatively minor injury can cause
spinal cord injury in people with conditions that affect their bones or joints,
such as arthritis or osteoporosis.
When to seek medical advice
Spinal cord injury isn't always obvious. Numbness or paralysis may result immedi
ately after a spinal cord injury or gradually as bleeding or swelling occurs in
or around the spinal cord. In either case, the time between injury and treatment
is a critical factor that can determine the extent of complications and the lev
el of recovery.
Anyone who has experienced significant trauma to the head or neck needs immediat
e medical evaluation for the possibility of spinal cord injury. In fact, it's sa
fest to assume that trauma victims have a spinal cord injury until proved otherw
ise.
If you suspect that someone has a back or neck injury, don't move the injured pe
rson. Permanent paralysis and other serious complications may result. Instead, t
ake these steps:
Dial 911 or call for emergency medical assistance.
Keep the person still.
Place heavy towels on both sides of the neck or hold the head and neck t
o prevent it from moving, until emergency care arrives.
Provide basic first aid, such as stopping any bleeding and making the pe
rson comfortable, without moving the head or neck.
Screening and diagnosis
Paramedics and emergency workers are trained to treat people who have suffered a
traumatic head or neck injury as if they have a spinal cord injury or an unstab
le spinal column, until a thorough screening and diagnosis can be completed. A k
ey step in the initial treatment is immobilizing the spine.
Preventing further damage
Immobilizing the spine can prevent injury to the spine or prevent worsening of a
ny injury that is already present. For this reason, emergency personnel receive
training in handling an injured person without moving the neck and back. They us
e rigid collars around the injured person's neck and place the injured person on
a rigid board, until a complete evaluation can take place.
In the emergency room, a doctor may be able to rule out spinal cord injury by ca
refully inspecting an injured person, testing for sensory function and movement,
and asking some questions about the accident. But if the injured person complai
ns of neck pain, isn't fully awake, or has obvious signs of weakness or neurolog
ical injury, emergency diagnostic tests may be needed.
These tests may include:
X-rays. Medical personnel typically order these tests on all trauma vict
ims suspected of having a spinal cord injury. X-rays can reveal vertebral proble
ms, tumors, fractures or degenerative changes in your spine.
Computerized tomography (CT) scan. A CT scan may provide a better look a
t abnormalities seen on an X-ray. This scan uses computers to form a series of c
ross-sectional images that can define bone, disk and other problems.
Magnetic resonance imaging (MRI). MRI uses a strong magnetic force and r
adio waves to produce computer-generated images. This test is extremely helpful
for looking at the spinal cord and identifying herniated disks, blood clots or o
ther masses that may be compressing the spinal cord. But MRI can't be used on pe
ople with pacemakers or on trauma victims who need certain life-support machines
or cervical traction devices.
Myelography. Myelography allows your doctor to visualize your spinal ner
ves more clearly. After a special dye is injected into your spinal canal, X-rays
or CT scans of your vertebrae can suggest a herniated disk or other lesions. Th
is test is used when MRI isn't possible or when it may yield important additiona
l information that isn't provided by other tests.
If your doctor suspects a spinal cord injury, he or she may prescribe traction t
o immobilize your spine, as well as high doses of the corticosteroid drug methyl
prednisolone (Medrol). There is some controversy about the use of this medicatio
n due to the small benefits noted in research studies and the possible risks. Ho
wever, there are no other medications available at this time. So, methylpredniso
lone is often given as soon as possible, and it must be given within eight hours
of injury.
Diagnosis doesn't stop there, though. A few days after injury, your doctor will
conduct a neurological exam to determine the severity of the injury and to predi
ct the likely extent of recovery. This may involve more X-rays, MRIs or more adv
anced imaging techniques.
Complications
If you recently experienced a spinal cord injury, it might seem like every aspec
t of life just became a lot more complicated. After all, adapting to life with a
disability — often in a wheelchair — is no easy task.
You'll likely experience many thoughts and emotions after the injury. And you'll
likely have concerns about how your injury will affect your lifestyle, your fin
ancial situation and your personal relationships. Grieving and emotional stress
are normal and common. However, if your grief and sadness are affecting your per
sonal care, causing you to isolate yourself from others, or prompting you to abu
se alcohol or other drugs, it's time to seek help. People with spinal cord injur
y are at increased risk of suicide, especially in the first 10 years following t
he injury.
Other complications of a spinal cord injury may include:
Urinary tract problems. A spinal cord injury that affects nerves that ru
n to your bladder can cause urinary incontinence — the inability to control the
release of urine from your bladder. Loss of bladder control increases your risk
of urinary tract infections. It may also cause kidney infection and kidney or bl
adder stones. Drinking plenty of clear fluids and using a catheter — a thin, sof
t tube that you insert into your urethra and bladder to drain your urine — sever
al times a day may help.
Bowel management difficulties. After a spinal cord injury, voluntary con
trol of your bowels may be lost or impaired. This can make it difficult for stoo
l to move through your intestines, or it can result in fecal incontinence — the
inability to control your bowel movements. Eating a high-fiber diet can help reg
ulate your bowels. Medications and other products are also available to manage w
aste elimination.
Pressure sores. Sitting or lying in the same position for a long period
of time can cause pressure sores, which are also called decubitus ulcers or beds
ores. People with a spinal cord injury are particularly susceptible to pressure
sores because the injury reduces or eliminates sensations, making it difficult t
o know when a sore is developing. Changing positions frequently — with help, if
needed — is the best way to prevent these sores.
Deep vein thrombosis and pulmonary embolism. Sitting for long periods of
time can decrease blood flow through your veins and cause blood clots to form.
These blood clots can develop in a vein deep within a muscle (deep vein thrombos
is), and they can lead to a blocked pulmonary artery in your lungs (pulmonary em
bolism). Large clots that block blood flow can be fatal, so people with spinal c
ord injury may need devices or medications to try to prevent clotting.
Lung and breathing problems. It's more difficult to breathe and cough wi
th weakened abdominal and chest muscles, so people with cervical and thoracic sp
inal cord injury may develop pneumonia or other lung problems. Medications and t
herapy can treat these problems. In some instances, people with spinal cord inju
ry may also need a yearly flu shot or other immunizations.
Autonomic dysreflexia. Spinal cord injury above the middle of your chest
may cause a condition called autonomic dysreflexia. This dangerous condition oc
curs when an irritation or pain below the level of the injury sends a signal tha
t fails to reach your brain, producing a reflex action that can constrict blood
vessels. The result is a rise in blood pressure and a drop in heart rate that ca
n result in stroke or seizure. Changing positions or eliminating the cause of th
e irritation — which can be something as simple as a full bladder or tight cloth
es — can help.
Spasticity. Some people with spinal cord injury develop muscle spasms an
d jumping of their arms and legs. Unfortunately, this doesn't mean that they're
recovering. These exaggerated reflexes occur because some of the nerves in the l
ower spinal cord become more sensitive after injury and cause muscle contraction
s. However, because of the spinal cord injury, the brain can no longer send sign
als to the lower nerves to regulate the contractions. Medical treatments may be
needed if spasms become severe.
Weight control issues. After a spinal cord injury, weight loss and muscl
e atrophy are common. But the change in lifestyle and activities may eventually
cause weight gain, which can make it difficult for you to lift yourself — or be
lifted — from place to place and put you at risk of heart disease and other prob
lems. It's a good idea to develop an exercise and diet plan with assistance from
a dietitian and rehabilitation therapist.
Sexual dysfunction. Many men with a spinal cord injury still have erecti
ons, even men with little sensation in the genital area. But the erections may n
ot be firm enough or last long enough for sexual activity. Fertility also can be
affected. Ninety percent of men with a spinal cord injury aren't able to ejacul
ate during intercourse. However, this doesn't mean that men with a spinal cord i
njury can't be sexually active or father a child. Doctors, urologists and fertil
ity specialists who specialize in spinal cord injury can offer options for bette
r sexual functioning and fertility.
Women with a spinal cord injury also may benefit from seeing a doctor about chan
ges in their sexuality and fertility. There's usually no physical change in wome
n with a spinal cord injury that inhibits sexual intercourse or pregnancy. But w
omen may lose the ability to produce vaginal lubrication or experience orgasm, a
nd many experience changes in body image that affect sexuality. In addition, any
pregnancy will likely be considered high risk. It's important to talk with a do
ctor before becoming pregnant.
Pain. You may experience pain as a result of damage to your spinal cord
or other parts of your body during your accident. It's possible to feel pain in
areas of your body where there's little or no sensation. You may also experience
pain from overusing muscles in one part of your body. For example, many people
develop shoulder tendinitis from manually operating a wheelchair for a long peri
od of time. Any kind of pain can have a negative impact on daily living. Medicat
ions and modified activities can help manage pain.
New injuries. Having a spinal cord injury makes you susceptible to injur
y of any part of your body that has impaired sensation. You may even receive a b
urn or cut without realizing it. Take steps to prevent new injuries and to inspe
ct your body for any cuts or sores that need medical attention.
Treatment
Fifty years ago, a spinal cord injury was usually fatal. At that time, most inju
ries were severe, complete injuries and little treatment was available.
Today, there's still no way to reverse damage to the spinal cord. But modern inj
uries are usually less severe, partial spinal cord injuries. And advances in rec
ent years have improved the recovery of people with a spinal cord injury and sig
nificantly reduced the amount of time survivors must spend in the hospital. Rese
archers are working on new treatments, including innovative treatments, prosthes
es and medications that may promote nerve cell regeneration or improve the funct
ion of the nerves that remain after a spinal cord injury.
In the meantime, spinal cord injury treatment focuses on preventing further inju
ry and enabling people with a spinal cord injury to return to an active and prod
uctive life within the limits of their disability. This requires urgent emergenc
y attention and ongoing care.
Emergency actions
Urgent medical attention is critical to minimizing the long-term effects of any
head or neck trauma. So treatment for a spinal cord injury often begins at the s
cene of the accident.
If you suffer a head or neck injury, you'll likely be treated by paramedics and
emergency workers who will attend to three immediate concerns:
Maintaining your ability to breathe
Keeping you from going into shock
Immobilizing your neck to prevent further spinal cord damage
Emergency personnel typically immobilize the spine as gently and quickly as poss
ible using a rigid neck collar and a rigid carrying board, which they'll use to
transport you to the hospital.
In the emergency room, doctors focus on maintaining your blood pressure, breathi
ng and neck stabilization and avoiding possible complications, such as stool or
urine retention, respiratory or cardiovascular difficulty, and formation of deep
vein blood clots in the extremities. You may be sedated so that you don't move
and sustain more damage while undergoing diagnostic tests for spinal cord injury
.
If you do have a spinal cord injury, you'll usually be admitted to the intensive
care unit for treatment. You may even be transferred to a regional spine injury
center that has a team of neurosurgeons, orthopedic surgeons, spinal cord medic
ine specialists, psychologists, nurses, therapists and social workers with exper
tise in spinal cord injury.
Early stages of treatment
In the early stages of paraplegia or quadriplegia, your doctor will treat the in
jury or disease that caused the loss of function. Immediate treatment may includ
e:
Medications. Methylprednisolone (Medrol) is a treatment option for acute
spinal cord injury. This corticosteroid seems to cause some recovery in people
with a spinal cord injury if given within eight hours of injury. Methylprednisol
one works by reducing damage to nerve cells and decreasing inflammation near the
site of injury.
Immobilization. You may need traction to stabilize your spine and bring
the spine into proper alignment during healing. Sometimes, traction is accomplis
hed by placing metal braces, attached to weights or a body harness, into your sk
ull to hold it in place. In some cases, a rigid neck collar also may work.
Surgery. Often, emergency surgery is necessary to remove fragments of bo
nes, foreign objects, herniated disks or fractured vertebrae that appear to be c
ompressing the spine. Surgery may also be needed to stabilize the spine to preve
nt future pain or deformity. Controversy exists regarding the best time to perfo
rm surgery. Some surgeons believe it should be performed as soon as possible in
most circumstances, while others believe it's safer to wait for several days bef
ore attempting any surgery. Research has not clearly proved which approach is be
tter.
Ongoing care
After the initial injury or disease stabilizes, doctors turn their attention to
problems that may arise from immobilization, such as deconditioning, muscle cont
ractures, bedsores, urinary infection and blood clots. Early care will likely in
clude range-of-motion exercises for paralyzed limbs, help with your bladder and
bowel functions, applications of skin lotion, and use of soft bed coverings or f
lotation mattresses, as well as frequently changing your position.
Hospitalization can last from several days to several weeks, depending on the ca
use and extent of the paralysis and the progress of your therapy. But treatment
doesn't stop when you check out of the hospital.
Here are some of the ongoing treatments you can expect.
Rehabilitation. During your hospital stay, a rehabilitation team will work with
you to improve your remaining muscle strength and to give you the greatest possi
ble mobility and independence. Your team may include a physical therapist, occup
ational therapist, rehabilitation nurse, rehabilitation psychologist, social wor
ker, dietitian recreation therapist and a doctor who specializes in physical med
icine (physiatrist) or spinal cord injury.
During the initial stages of rehabilitation, therapists usually emphasize regain
ing leg and arm strength, redeveloping fine-motor skills and learning adaptive t
echniques to accomplish day-to-day tasks. A program typically includes exercise,
as well as training on the medical devices you'll need to assist you, such as a
wheelchair or equipment that can make it easier to fasten buttons or dial a tel
ephone.
Therapy often begins in the hospital and continues in a rehabilitation facility.
As therapy continues, you and your family members will receive counseling and a
ssistance on a wide range of topics, from dealing with urinary tract infections
and skin care to modifying your home and car to accommodate your disability. The
rapists will encourage you to resume your favorite hobbies, participate in athle
tic activities and return to the workplace, if possible. They'll even help deter
mine what type of assistive equipment you'll need for these vocational and recre
ational activities and teach you how to use it.
Medications. You may benefit from medications that manage the signs, symptoms an
d complications of spinal cord injury. These include medications to control pain
and muscle spasticity, as well as medications that can improve bladder control,
bowel control and sexual functioning. You may also need short-term medications
from time to time, such as antibiotics for urinary tract infections.
New technologies. Inventive medical devices can help people with a spinal cord i
njury become more independent and more mobile. Some apparatuses may also restore
function. These include:
Modern wheelchairs. Improved, lighter weight wheelchairs are making peop
le with spinal cord injury more mobile and more comfortable. Some wheelchairs ca
n even climb stairs, travel over rough terrain and elevate a seated passenger to
eye level to reach high places without help.
Computer devices. Computer-driven tools and gadgets can help with daily
routines. You can use voice-activated computer technologies to answer and dial a
phone, or to use a computer and pay bills. Computer-controlled technologies can
also help with bathing, dressing, grooming, cleaning and reading.
Electrical stimulation devices and neural prostheses. These sophisticate
d devices use electrical stimulation to produce actions. Some are implanted unde
r the skin and connect with the nervous system to supplement or replace lost mot
or and sensory functions. Others are outside the body. They are often called fun
ctional electrical stimulation (FES) systems, and they use electrical stimulator
s to control arm and leg muscles to allow people with a spinal cord injury to st
and, walk, reach and grip.
These systems are composed of computer-controlled electrodes that are taped to t
he skin or implanted under the skin and controlled by the user. One of the syste
ms allows someone with a spinal cord injury to trigger hand and arm movements. T
hese devices require more research, but they've gained a great deal of attention
, in part because the actor Christopher Reeve was able to rely primarily on an F
ES bicycle that used computer-controlled electrodes to stimulate his legs to cyc
le. He also had a system implanted to stimulate his breathing.
Prognosis and recovery
It's often impossible for your doctor to make a precise prognosis right away. Re
covery, if it occurs, typically starts between a week and six months after injur
y. Impairment remaining after 12 to 24 months is likely to be permanent.
However, some people experience small improvements for up to two years or longer
. At one point, Christopher Reeve made national headlines when he regained the a
bility to move his fingers and wrists and feel sensations more than five years a
fter he was paralyzed in a horse accident. But many not-so-famous folks with a s
pinal cord injury have made similar strides away from the media spotlight. And d
octors are researching ways to improve late recovery.
Prevention
Following this advice may reduce your risk of a spinal cord injury:
Drive safely. Motor vehicle accidents are the leading cause of spinal co
rd injuries. Wear a seat belt every time you drive. Make sure that your children
wear a seat belt or, if they're very young, use an age- and weight-appropriate
child safety seat. Children under age 12 should always ride in the back seat to
avoid air bag injuries. Don't drive while intoxicated.
Be safe with firearms. Lock up firearms and ammunition in a safe place t
o prevent accidental discharge of weapons. Store guns and ammunition separately.
Prevent falls. Use a stool or stepladder to reach objects in high places
. Add handrails along stairways. Place nonslip mats on your bathroom and shower
floor. For young children, use safety gates to block stairs and consider install
ing window guards.
Take precautions when playing sports. Always wear recommended safety gea
r. Avoid headfirst moves, such as diving into shallow water, spear tackling in f
ootball, sliding headfirst in baseball and skating headfirst into the boards in
ice hockey. Use a spotter in gymnastics.
Coping skills
An accident that results in paralysis is a life-changing event. The sudd
en presence of disability can be frightening and confusing. You may wonder how s
pinal cord injury will affect your everyday activities, job, relationships and l
ong-term happiness.
Recovery from such an event takes time, but many people who are paralyze
d move on to lead productive and fulfilling lives. The will to live in humans is
amazingly strong, and the creativity with which many affected people lead their
lives is great. It's essential to stay motivated and get the support you need.
Grieving
If you're newly injured, you and your family will likely experience a period of
mourning and grief that's similar to the period after the death of a loved one.
Although the grieving process is different for everyone, it's common to experien
ce denial or disbelief, then sadness, anger, bargaining, and, finally, acceptanc
e.
The grieving process is a common, healthy part of your recovery. It's na
tural — and important — to grieve the loss of the way you were. But it's also ne
cessary to set new goals and find a way to move forward with your life.
Taking control
One of the best ways to regain control of your life is to educate yourself about
your injury and your options for reclaiming an independent life. A wide range o
f driving equipment and vehicle modifications is available today. The same is tr
ue of home modification products. Ramps, wider doors, special sinks, grab bars a
nd easy-to-turn doorknobs make it possible for you to assert your autonomy.
Because the costs of a spinal cord injury can be overwhelming, you may w
ant to find out if you are eligible for economic assistance or support services
from the state or federal government or from charitable organizations. Your reha
bilitation team can help you identify resources in your area.
Talking about your disability
Your friends and family may respond to your disability in different ways. Some m
ay be unfazed by your injury. Others may be uncomfortable and unsure if they are
saying or doing the right thing. And some may have a difficult time adjusting t
o the change. They may grieve for the loss of the way your life was before the a
ccident. They may be scared about the financial challenges and stress that are s
ure to arise. Or they may be nervous about their new role as caregiver.
Educating people about your disability is often the best solution. Child
ren are naturally curious and sometimes adjust rather quickly if their questions
are answered in a clear, straightforward way. Adults can also benefit from lear
ning the facts. Explain the effects of your injury and what your family and frie
nds can do to help. At the same time, don't hesitate to tell friends and loved o
nes when they're helping too much. Although it may be uncomfortable at first, ta
lking about your injury often strengthens your relationships with family and fri
ends.
Dealing with intimacy
Many men and women with a spinal cord injury wonder if they can maintain a roman
tic, intimate relationship with a partner. The answer is yes.
However, people with a spinal cord injury often need to address physical
and emotional changes that can affect sexuality. You may need medical treatment
s or medications to have sexual intercourse. In some cases, intercourse may not
be possible and you and your partner may need to explore and experiment with dif
ferent ways to be romantic and intimate. A professional counselor can help you a
nd your partner communicate your needs and feelings so that you're more comforta
ble talking about sex and discovering what is fulfilling for both of you.
Taking care of yourself
As you adjust to your disability, allow yourself time to rest and time to proces
s your thoughts and feelings about your disability. This is also a good time to
concentrate on eating a healthy diet and reducing stress.
Good nutrition will help you build enough strength to fully participate
in daily activities. A balanced diet will also help you fight infections and mai
ntain proper body weight. Plus, it will help maintain regular bladder and bowel
functioning and assist in preventing pressure ulcers.
Looking ahead
By nature, a spinal cord injury has a sudden impact on your life and the lives o
f those closest to you. When you first hear your diagnosis, you may start making
a mental list of all of the things you can't do anymore. However, as you learn
more about your injury and your treatment options, you may be surprised at all o
f the things you can do.
Thanks to new technologies, treatments and devices, people with a spinal
cord injury play basketball and participate in track meets. They paint and take
photographs. They get married, raise children and have rewarding jobs.
Today, advances in stem cell research and nerve cell regeneration give h
ope for a greater recovery for people with a spinal cord injury. Several experim
ental treatments are being tested around the world. At the same time, new medica
tions are being developed for people with long-standing spinal cord injuries. No
one knows exactly when new treatments will become available, but you can remain
hopeful about the future of spinal cord research, while living your life to the
fullest today.
Spinal cord injury
From Wikipedia, the free encyclopedia
This article may require cleanup to meet Wikipedia's quality standards.
Please improve this article if you can. (September 2007)
Spinal cord injury
Classification & external resources
ICD-10
G95.9, T09.3
DiseasesDB
12327 29466
eMedicine
emerg/553 neuro/711 pmr/182 pmr/183 orthoped/425
MeSH
D013119
Spinal cord injury causes myelopathy or damage to white matter or myelinated fib
er tracts that carry sensation and motor signals to and from the brain. It also
damages gray matter in the central part of the spinal, causing segmental losses
of interneurons and motorneurons. Spinal cord injury can occur from many causes,
including:
Trauma such as automobile accidents, falls, gunshots, diving accidents,
war injuries, etc.
Tumor such as meningiomas, ependymomas, astrocytomas, and metastatic can
cer.
Ischemia resulting from occlusion of spinal blood vessels, including dis
secting aortic aneurisms, emboli, arteriosclerosis.
Developmental disorders, such as spina bifida, meningomyolcoele, and oth
er.
Neurodegenerative diseases, such as Friedreich's ataxia, spinocerebellar
ataxia, etc.
Demyelinative diseases, such as Multiple Sclerosis.
Transverse myelitis, resulting from spinal cord stroke, inflammation, or
other causes.
Vascular malformations, such as arteriovenous malformation (AVM), dural
arteriovenous fistula (AVF), spinal hemangioma, cavernous angioma and aneurysm.
Contents
[hide]
1 Classification
2 The Effects of Spinal Cord Injury
2.1 The Location of the Injury
2.1.1 Cervical injuries
2.1.2 Thoracic injuries
2.1.3 Lumbar and Sacral injuries
2.1.4 Central Cord and Other Syndromes
3 Treatment
4 References
5 External links
[edit] Classification
The American Spinal Cord Injury Association or ASIA defined an international cla
ssification based on neurological levels, touch and pinprick sensations tested i
n each dermatome, and strength of ten key muscles on each side of the body, i.e.
shoulder shrug (C4), elbow flexion (C5), wrist extension (C6), elbow extension
(C7), hip flexion (L2), knee extension (L3), ankle dorsiflexion (L4), long toe e
xtension (L5), and ankle plantar flexion (S1). Each muscle is graded on a scale
of 0-5 where 0 is paralyzed, 1 is slight movement, 2 is definite movement, 3 is
movement against gravity, 4 is movement against manual resistance, and 5 is norm
al. The scores of the muscles add up to 100. The pinprick and touch sensations a
re grade separately for each dermatome on a scale of 0-2 where 0 is absent sensa
tion, 1 is abnormal sensation, and 2 is normal. These add up to 112 points each
for pinprick and touch.
Traumatic spinal cord injury is classified into five types by the American Spina
l Injury Association (ASIA) and the International Spinal Cord Injury Classificat
ion System.
A indicates a "complete" spinal cord injury where no motor or sensory fu
nction is preserved in the sacral segments S4-S5. A complete injury is one in wh
ich there is some neurological level below which there is no motor or sensory fu
nction. Since the S4-S5 segment is the lower segmental, absence of motor and sen
sory function indicates "complete" spinal cord injury.
B indicates an "incomplete" spinal cord injury where sensory but not mot
or function is preserved below the neurological level and includes the sacral se
gments S4-S5. This is typically a transient phase and if the person recovers any
motor function below the neurological level, that person essentially becomes a
motor incomplete, i.e. ASIA C or D.
C indicates an "incomplete" spinal cord injury where motor function is p
reserved below the neurological level and more than half of key muscles below th
e neurological level have a muscle grade of less than 3.
D indicates an "incomplete" spinal cord injury where motor function is p
reserved below the neurological level and at least half of the key muscles below
the neurological level have a muscle grade of 3 or more.
E indicates "normal" where motor and sensory scores are normal. Note tha
t it is possible to have spinal cord injury and neurological deficit with comple
tely normal motor and sensory scores.
In addition, there are several clinical syndromes associated with incomplete spi
nal cord injuries.
The Central Cord syndrome is associated with greater loss of upper limb
function compared to lower limbs.
The Brown-Séquard syndrome results from injury to one side with the spin
al cord, causing weakness and loss of proprioception on the side of the injury a
nd loss of pain and thermal sensation of the other side.
The Anterior Spinal syndrome results from injury to the anterior part of
the spinal cord, causing weakness and loss of pain and thermal sensations below
the injury site but preservation of proprioception that is usually carried in t
he posterior part of the spinal cord.
Tabes Dorsalis results from injury to the posterior part of the spinal c
ord, usually from infection diseases such as syphilis, causing loss of touch and
proprioceptive sensation.
Conus Medullaris syndrome results from injury to the tip of the spinal c
ord, located at L1 vertebra.
Cauda Equina syndrome is, strictly speaking, not really spinal cord inju
ry but injury to the spinal roots below the L1 vertebra.
One can have spine injury without spinal cord injury. Many people suffer transie
nt loss of function ("stingers") in sports accidents or pain in "whiplash" of th
e neck without neurological loss and relatively few of these suffer spinal cord
injury sufficient to warrant hospitalization. In the United States, the incidenc
e of spinal cord injury has been estimated to be about 35 cases per million per
year, or approximately 10,500 per year (35 * 300). In China, the incidence of sp
inal cord injury was recently estimated to be as high as 65 cases per million pe
r year in urban areas. If so, assuming a population of 1.3 billion, this would s
uggest an incidence of 84,500 per year (65 * 1300).
The prevalence of spinal cord injury is not well known in many large countries.
In some countries, such as Sweden and Iceland, registries are available. About 4
50,000 people in the United States live with spinal cord injury (one in 670), an
d there are about 11,000 new spinal cord injuries every year (one in 30,000). Th
e majority of them (78%) involve males between the ages of 16-30 and result from
motor vehicle accidents (42%), violence (24%), or falls (27%). Perhaps this can
be attributed to the willingness of males to try dangerous things, when compare
d to females.
[edit] The Effects of Spinal Cord Injury
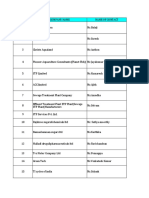
Divisions of Spinal Segments
Segmental Spinal Cord Level and Function
Level Function
Cl-C6
Neck flexors
Cl-Tl
Neck extensors
C3, C4, C5
Supply diaphragm (mostly C4)
C5, C6
Shoulder movement, raise arm (deltoid); flexion of elbow (biceps); C6 externally
rotates the arm (supinates)
C6, C7
Extends elbow and wrist (triceps and wrist extensors); pronates wrist
C7, T1
Flexes wrist
C7, T1
Supply small muscles of the hand
T1 -T6
Intercostals and trunk above the waist
T7-L1
Abdominal muscles
L1, L2, L3, L4
Thigh flexion
L2, L3, L4
Thigh adduction
L4, L5, S1 Thigh abduction
L5, S1, S2
Extension of leg at the hip (gluteus maximus)
L2, L3, L4
Extension of leg at the knee (quadriceps femoris)
L4, L5, S1, S2
Flexion of leg at the knee (hamstrings)
L4, L5, S1
Dorsiflexion of foot (tibialis anterior)
L4, L5, S1
Extension of toes
L5, S1, S2
Plantar flexion of foot
L5, S1, S2
Flexion of toes
The exact effects of a spinal cord injury vary according to the type and level i
njury, and can be organized into two types:
In a complete injury, there is no function below the "neurological" leve
l, defined as the lowest level that has intact neurological function. If a perso
n has some level below which there is no motor and sensory function, the injury
is said to be "complete". Recent evidence suggest that less than 5% of people wi
th "complete" spinal cord injury recover locomotion.
A person with an incomplete injury retains some sensation or movement be
low the level of the injury. The lowest spinal cord level is S4-5, representing
the anal sphincter and peri-anal sensation. So, if a person is able to contract
the anal sphincter voluntarily or is able to feel peri-anal pinprick or touch, t
he injury is said to be "incomplete". Recent evidence suggest that over 95% of p
eople with "incomplete" spinal cord injury recover some locomotory ability.
In addition to a loss of sensation and motor function below the point of injury,
individuals with spinal cord injuries will often experience other complications
of spinal cord injury:
Bowel and bladder function is regulated by the sacral region of the spin
e, so it is very common to experience dysfunction of the bowel and bladder, incl
uding infections of the bladder, and anal incontinence.
Sexual function is also associated with the sacral region, and is often
affected.
Injuries of the C-1, C-2 will often result in a loss of breathing, neces
sitating mechanical ventilators or phrenic nerve pacing.
Inability or reduced ability to regulate heart rate, blood pressure), sw
eating and hence body temperature.
Spasticity (increased reflexes and stiffness of the limbs).
Neuropathic pain.
Autonomic dysreflexia or abnormal increases in blood pressure, sweating,
and other autonomic responses to pain or sensory disturbances.
Atrophy of muscle.
Osteoporosis (loss of calcium) and bone degeneration.
Gallbladder and renal stones.
[edit] The Location of the Injury
Knowing the exact level of the injury on the spinal cord is important when predi
cting what parts of the body might be affected by paralysis and loss of function
.
Below is a list of typical effects of spinal cord injury by location (refer to t
he spinal cord map to the right). Please keep in mind that while the prognosis o
f complete injuries are predictable, incomplete injuries are very variable and m
ay differ from the descriptions below.
[edit] Cervical injuries
Cervical (neck) injuries usually result in full or partial tetraplegia. Dependin
g on the exact location of the injury, one with a spinal cord injury at the cerv
ical level may retain some amount of function as detailed below, but are otherwi
se completely paralyzed.
C3 vertebrae and above : Typically lose diaphragm function and require a
ventilator to breathe.
C4 : May have some use of biceps and shoulders, but weaker
C5 : May retain the use of shoulders and biceps, but not of the wrists o
r hands.
C6 : Generally retain some wrist control, but no hand function.
C7 and T1 : Can usually straighten their arms but still may have dexteri
ty problems with the hand and fingers. C7 is generally the level for functional
independence.
[edit] Thoracic injuries
Injuries at the thoracic level and below result in paraplegia. The hands, arms,
head, and breathing are usually not affected.
T1 to T8 : Most often have control of the hands, but lack control of the
abdominal muscles so control of the trunk is difficult or impossible. Effects a
re less severe the lower the injury.
T9 to T12 : Allows good trunk and abdominal muscle control, and sitting
balance is very good.
[edit] Lumbar and Sacral injuries
The effect of injuries to the lumbar or sacral region of the spinal canal are de
creased control of the legs and hips, urinary system, and anus.
[edit] Central Cord and Other Syndromes
Central cord syndrome (picture 1) is a form of incomplete spinal cord injury cha
racterized by impairment in the arms and hands and, to a lesser extent, in the l
egs. This is also referred to as inverse paraplegia, because the hands and arms
are paralyzed while the legs and lower extremities work correctly.
Most often the damage is to the cervical or upper thoracic regions of the spinal
cord, and characterized by weakness in the arms with relative sparing of the le
gs with variable sensory loss.
This condition is associated with ischemia, hemorrhage, or necrosis involving th
e central portions of the spinal cord (the large nerve fibers that carry informa
tion directly from the cerebral cortex). Corticospinal fibers destined for the l
egs are spared due to their more external location in the spinal cord.
This clinical pattern may emerge during recovery from spinal shock due to prolon
ged swelling around or near the vertebrae, causing pressures on the cord. The sy
mptoms may be transient or permanent.
Anterior cord syndrome (picture 2) is also an incomplete spinal cord injury. Bel
ow the injury, motor function, pain sensation, and temperature sensation is lost
; touch, proprioception (sense of position in space), and vibration sense remain
intact. Posterior cord syndrome (not pictured) can also occur, but is very rare
.
Brown-Séquard syndrome (picture 3) usually occurs when the spinal cord is hemise
ctioned or injured on the lateral side. On the ipsilateral side of the injury (s
ame side), there is a loss of motor function, proprioception, vibration, and lig
ht touch. Contralaterally (opposite side of injury), there is a loss of pain, te
mperature, and deep touch sensations.
[edit] Treatment
Treatment for acute traumatic spinal cord injuries have consisted of giving high
dose methylprednisolone if the injury occurred within 8 hours. The recommendati
on is primarily based on the National Acute Spinal Cord Injury Studies (NASCIS)
II and III. Some of the claims of the studies have been challenged as being from
faulty interpretation of the data.
Breakthrough medical research shows Chondroitinase treatment [1] and stem cell t
ransplants could have the potential to help or cure paralysis caused by spinal i
njury. Stem cells are primal cells found in all multi-cellular organisms. They c
an be made to differentiate into a range of specialized cells including nerve ce
lls, which can be transplanted into the body.
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Irrigation SchedulingDokumen3 halamanIrrigation SchedulingLuojisi CilBelum ada peringkat
- Corpus Alienum PneumothoraxDokumen3 halamanCorpus Alienum PneumothoraxPratita Jati PermatasariBelum ada peringkat
- Pediatric Blood PressureDokumen28 halamanPediatric Blood PressureGenta Syaifrin Laudza0% (1)
- India's #1 Nroute Daily Whey Protein Powder Online 2022Dokumen3 halamanIndia's #1 Nroute Daily Whey Protein Powder Online 2022NRoute ProteinBelum ada peringkat
- CodanDokumen4 halamanCodanPetar RajicBelum ada peringkat
- Activity 1: Write Your Answer On The Space ProvidedDokumen4 halamanActivity 1: Write Your Answer On The Space ProvidedEki OmallaoBelum ada peringkat
- Coma ManagementDokumen5 halamanComa ManagementElena DocBelum ada peringkat
- 16-23 July 2011Dokumen16 halaman16-23 July 2011pratidinBelum ada peringkat
- Planning PlaygroundDokumen16 halamanPlanning PlaygroundAdnan AliBelum ada peringkat
- BM Waste Color CodingDokumen23 halamanBM Waste Color Codingpriyankamote100% (1)
- Banner AT FM 10k PDFDokumen14 halamanBanner AT FM 10k PDFDamian RamosBelum ada peringkat
- Karakteristik Penderita Mioma Uteri Di Rsup Prof. Dr. R.D. Kandou ManadoDokumen6 halamanKarakteristik Penderita Mioma Uteri Di Rsup Prof. Dr. R.D. Kandou ManadoIsma RotinBelum ada peringkat
- Job Shadowing PresentationDokumen12 halamanJob Shadowing Presentationapi-462381810Belum ada peringkat
- SAFed Tests PDFDokumen88 halamanSAFed Tests PDFDanBelum ada peringkat
- Tinetti Assessment BalanceDokumen2 halamanTinetti Assessment Balancesathish Lakshmanan100% (1)
- Technical Manual: RTS Automatic Transfer SwitchDokumen28 halamanTechnical Manual: RTS Automatic Transfer SwitchKrīztīän TörrësBelum ada peringkat
- Talentadong Kabataan (National Children's Month)Dokumen4 halamanTalentadong Kabataan (National Children's Month)Prince Joshua Sumagit100% (1)
- TTS 16 80 400 Septic Tank DesingsDokumen16 halamanTTS 16 80 400 Septic Tank DesingsJeffrey James100% (2)
- FR 2011 02 23Dokumen275 halamanFR 2011 02 23Ngô Mạnh TiếnBelum ada peringkat
- The CSI Effect - Google FormsDokumen12 halamanThe CSI Effect - Google FormsZivi DegenBelum ada peringkat
- Mosh RoomDokumen21 halamanMosh RoomBrandon DishmanBelum ada peringkat
- Analytical Customer UpdationDokumen16 halamanAnalytical Customer UpdationSathish SmartBelum ada peringkat
- Altius Annual Leave Policy Wef 1st January 2012 Ver 1.1Dokumen11 halamanAltius Annual Leave Policy Wef 1st January 2012 Ver 1.1Mudassar HakimBelum ada peringkat
- Urosepsis-Sepsis - (KeithRN-Unfolding THIGPEN PDFDokumen11 halamanUrosepsis-Sepsis - (KeithRN-Unfolding THIGPEN PDFOLga A. Thigpen100% (4)
- Communication in Palliative CareDokumen7 halamanCommunication in Palliative CareIhsan NudinBelum ada peringkat
- Wa0094.Dokumen9 halamanWa0094.lider vigilanciaBelum ada peringkat
- WASH in CampsDokumen13 halamanWASH in CampsMohammed AlfandiBelum ada peringkat
- Allergist OIT Packet 180913 NutsDokumen74 halamanAllergist OIT Packet 180913 Nutsmuaz.rizviBelum ada peringkat
- Qand ADokumen5 halamanQand AJoshua PascasioBelum ada peringkat
- Diffuse Large B-Cell Lymphoma: The History, Current View and New PerspectivesDokumen14 halamanDiffuse Large B-Cell Lymphoma: The History, Current View and New PerspectivesPepe PintoBelum ada peringkat