Toll-Like Receptors and Skin: Jeadv
Diunggah oleh
Benor Amri MustaqimJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Toll-Like Receptors and Skin: Jeadv
Diunggah oleh
Benor Amri MustaqimHak Cipta:
Format Tersedia
JEADV
DOI: 10.1111/j.1468-3083.2011.04049.x
REVIEW ARTICLE
Toll-like receptors and skin
A.T. Ermertcan,* F. Ozturk, K. Gunduz
Department of Dermatology, Faculty of Medicine, Celal Bayar University, Manisa, Turkey
*Correspondence: A.T. Ermertcan. E-mail: draylinturel@hotmail.com
Abstract
Toll-like receptors are important pattern recognition receptors which have key roles in both innate and adaptive
immune responses. They are strongly associated with the pathogenesis of inflammatory and autoimmune diseases.
Furthermore, Toll-like receptors have also been implicated in the pathogenesis of several skin diseases such as skin
infections, psoriasis, acne vulgaris, lichen planus, Behcets disease, leprosy, syphilis, Lyme disease, atopic
dermatitis and allergic contact dermatitis, mycosis fungoides, non-melanoma skin cancers and melanoma. In this
manuscript, the structure and functions of Toll-like receptors in immune responses, their impact on skin diseases
and recent advances on therapeutic usage have been reviewed.
Received: 18 January 2011; Accepted: 16 February 2011
Conflict of interest
None declared.
Introduction
All living organisms are continuously exposed to foreign entities
including food, micro-organisms and unnecessary self metabolites.
There is a continuing need to discriminate dangerous non-self
from safe self, particularly when life-threatening microorganisms
invade the body. Two arms of immune defences against invading
pathogens: innate (natural) and adaptive (acquired) immunity
have been defined.1
Innate immunity is the first line of host defence. The innate
immune response utilizes both physical barriers such as skin and
mucosal epithelium for avoiding infection and rapid cellular
responses. Inflammatory responses by innate immune cells such
as granulocytes and macrophages that can be triggered in minutes
and are then followed by activation of dendritic cells and natural
killer (NK) cells.2,3 Adaptive (acquired) immune responses are
slower processes that are mediated by T cells and B cells, whose
highly diverse antigen receptors are generated by complex DNA
rearrangement events and thus have the potential to recognize
novel antigens as well as conserved ones. In contrast to adaptive
immunity, innate immunity had been regarded as a relatively nonspecific system, with its main roles being to engulf and destroy
pathogens, to trigger proinflammatory responses, and to help
present antigen, thereby priming adaptive immune responses.1
However, recent studies showed that the innate immune system
has a great degree of specificity that enables it to discriminate efficiently between self and foreign entities, including microorganisms
and unnecessary self molecules.1,4 Innate immune system recognizes pathogens by pathogen-associated molecular patterns
(PAMPs), including molecules from Gram-positive and -negative
JEADV 2011, 25, 9971006
bacteria, DNA and RNA viruses, fungi and protozoa and they
show target specificity.2,5 The mammalian receptors responsible
for recognition of PAMPs are called pattern recognition receptors
(PRRs). The failure of the immune system to recognize a pathogens PAMP could lead to a delay or blunting of the immune
response, resulting in unchecked invasion by the microbe.6 The
major pattern recognition receptors of the innate immune system
are Toll-like receptors (TLRs), Nod-like receptors (NLRs) and
RIG-I-like receptors (RLRs). Unlike the T-cell and B-cell antigen
receptors, these PRRs are entirely germline-encoded and are
expressed constitutively by both immune and non-immune cells.1
Following PAMP recognition, PRR activate specific signalling
pathways that lead to robust but highly defined innate immune
responses. These innate responses then help prime subsequent
protective adaptive (antigen-specific) immune responses to the
inciting pathogens.
In addition to their primary function of fighting invading
microbes, PRRs are also involved in the pathogenesis of many
diseases. In particular, PRR recognition of self-molecules derived
from the host (e.g. nucleic acids) may be linked to autoimmune
diseases and possibly to other immunological disorders. In
humans, PRRs and their mutations have recently been linked to
susceptibility, not only to infectious diseases, but also to chronic
inflammatory diseases, such as atherosclerosis and asthma.1,7 It
has been reported that TLRs play an important role in the pathophysiology of autoimmune, central nervous system (CNS), lung,
gastrointestinal tract, kidney diseases and cancer.2,811 There have
been significant advances in our understanding of TLRs in skin
inflammation, cutaneous malignancies and defence mechanisms.
2011 The Authors
Journal of the European Academy of Dermatology and Venereology 2011 European Academy of Dermatology and Venereology
Ermertcan et al.
998
Skin conditions associated with Toll-like receptors include acne,
rosacea, psoriasis, atopic dermatitis, systemic lupus erythematosus, mycosis fungoides, syphilis, leprosy, candidiasis, bacterial
and viral skin infections, such as herpes simplex and varicella
zoster, wound healing, non-melanoma skin cancers and melanoma.1217
Agonists and antagonists for TLRs, NLRs and RLRs, as well as
inhibitors of their signalling molecules, are presently under development for a variety of therapeutic applications. Choosing highly
effective and proper but safer PRR-agonists antagonists is
critical for the development of improved vaccine adjuvant and
immunostimulatory agents. PRR antagonists or inhibitors of PRRsignalling molecules, however, may provide another opportunity
for the development of drugs to prevent and or treat diseases in
which PRRs are involved in the aetiology or pathogenesis.1
In this review, the role of Toll-like receptors in immune
responses, their impact on human diseases, especially skin diseases
and recent advances on therapeutic usage will be discussed.
Toll-like receptors: discovery and structure
The importance of TLRs in immune responses was first recognized
with the discovery of the host defence role of the Toll pathway in
Drosophila melanogaster.1 Drosophila have no adaptive immune
responses as they do not possess any lymphocytes or antibodies.
Therefore, they rely on innate immunity and the production of
antimicrobial peptides to defend themselves against pathogens.4
Toll is a German slang and it means fantastic. Toll mutant was
discovered in the early 1980s by Nusslein-Volhard and Anderson
(two investigators working in Tuebingen, Germany) during a
mutagenesis screen aimed at unravelling the genes involved in the
establishment of dorso-ventral axis of Drosophila embryo.
Hashimoto and colleagues cloned the Toll gene in 1988 and found
it to encode a novel type of transmembrane receptor.10 Subsequent
studies showed that the activation of the Toll pathway in Drosophila resulted in the production of antimicrobial peptides that were
essential in host defence against fungal and bacterial pathogens.
Soon after the discovery of the host defence function of Toll in
Drosophila, a number of structurally related proteins were identified in mammals and were thus named Toll-like receptors.4,14 In
1997, the successful cloning of a human homologue of Drosophila
Toll was reported by Janeway and Medzhitov, and this TLR was
shown to activate NFjB.10
TLRs are a group of glycoproteins that function as surface
transmembrane receptors located mostly in cellular membranes
and permit cells to recognize self from non-self in immune activation.12,13 Immune cells such as monocytes, macrophages, dendritic
cells, granulocytes, NK cells, B cells, T cells and non-immune cells
like keratinocytes, fibroblasts, epithelial cells express TLRs.1 TLRs
are mostly found in cells that iniate the primary immune response.
They are located on the cell surface, in the cellular plasma membrane, in intracellular compartments, including endoplasmic reticulum and endosomes.13
JEADV 2011, 25, 9971006
TLRs have ectodomains containing leucine-rich repeats that
mediate the recognition of PAMPs, transmembrane domains and
intracellular Toll-interleukin 1 (IL-1) receptor (TIR) domains
required for downstream signal transduction. Elucidation of structure of several TLR ectodomains has provided structural insights
suggesting that several PAMPs act as ligands for TLRs. PAMPs recognized by TLRs include lipids, lipoproteins, proteins and nucleic
acids derived from bacteria, viruses, parasites and fungi.12,14
TLRs can be classified into subfamilies based on their genetic
tree. The TLR1, TLR2, TLR6 and TLR10 subfamily recognizes
lipoproteins derived from bacteria, viruses, fungi and parasites,
whereas TLR3 and the highly related TLR7, TLR8, and TLR9 subfamily recognize nucleic acids.3 TLR4 recognizes lipopolysaccharides and TLR5 is the receptor for bacterial flagellin. TLR11
recognizes a profilin-like molecule in Toxoplasma gondii. Direct
interaction of a TLR-ligand recognition can be flexible, permitting
the recognition of a diverse range of molecules. For example,
although TLR4 is associated with recognition of lipopolysaccharides, it also recognizes the fusion protein of respiratory syncytial
virus, fibronectin and heat-shock proteins. Similarly, TLR9 recognizes haemozoin, the heme-polymeric metabolite of the malaria
parasite as well as nucleic acids.1 TLR subfamilies and their ligands
are summarized in Table 1.
Toll-like receptor signalling
TLRs have an ectodomain that consists of 19-25 tandem copies
of leucine-rich repeats. They possess a transmembrane domain
which spans the cell membrane or membranes of intracellular
compartments. Some TLRs (TLRs 1,2,4-6) are found on the cell
membrane and become internalized into phagosomes after
interaction with their ligands. Some of them (TLRs 3,7,9) are
only found on membranes of intracellular compartments such
as endosomes and lysosomes. At the beginning of intracellular signalling, TLRs have a homologous cytoplasmic tail that
is highly conserved on both TLRs and members of the
Table 1 TLR subfamilies, their ligands and species
TLR subfamily Natural ligand
Species
References
TLR1 + TLR2
Triacyl lipopeptides Bacteria
(1,3)
TLR2
Zymosan
Fungi
(1,26,38)
TLR3
dsRNA
Viruses
TLR4
Lipopolysaccharide Gram-negative
bacteria
(3,8,12,26)
TLR5
Flagellin
Bacteria
(1,9,38)
TLR6 + TLR2
Diacyl lipopeptides
Mycoplasma
(1,14,18)
TLR7
ssRNA
Virus, host
(1,9,12,14,39)
TLR8
ssRNA
Virus, host
(1,9,12,14)
TLR9
DNA, hemozoin
Bacteria, virus, (1,14,18)
plasmodium
TLR10
Not known
Bacteria
(1,38)
TLR11
Profilin-like protein
Toxoplasma,
bacteria
(1,10,14)
(3,12)
2011 The Authors
Journal of the European Academy of Dermatology and Venereology 2011 European Academy of Dermatology and Venereology
TLRs and skin
999
interleukin-1 (IL-1) receptor family and is thus called the Toll
IL-1 receptor (TIR) domain. Once a TLR is activated by its
corresponding ligand, the TIR domain of the TLR interacts
with an adapter molecule.14 TIR domain-containing adaptor
molecules including MyD88 (Myeloid differentiation factor-88),
TIRAP (Mal) (Toll-IL-1R domain-containing adaptor protein),
TRIF (Toll-IL-1R domain-containing adaptor-inducing interferon b) and TRAM (TRIF related adaptor molecule) are
recruited by distinct TLRs and activate distinct signalling pathways. MyD88, the first identified member of this TIR family, is
used by all TLRs except TLR3, and activates the transcription
factor NFjB and mitogen-activated protein kinases (MAPKs) to
induce inflammatory cytokines.18 MyD88 is not required for
recognition of some microbial ligands, and not all TLR signalling is completely MyD88-dependent. TLR3 and TLR4 also trigger a MyD88-independent pathway called TRIF pathway that
lead to activation of the transcription factors IRF-3 (interferon
regulatory factor 3) and NFjB to ultimately produce interferon
(IFN)-b and inflammatory cytokines. TRAM and TIRAP function as sorting adaptors that recruit TRIF to TLR4 and MyD88
to TLR2 and TLR4, respectively.14,18 TRIF pathway activating
IRF3 leads the production of type I IFN (IFN-a b), which is
important in antiviral immune responses.14
Thus, TLR signalling pathways can be largely classified as
either MyD88-dependent pathways, which drive the induction
of inflammatory cytokines, or TRIF-dependent pathways, which
are responsible for the induction of type I interferon as well as
inflammatory cytokines. TLR4 is the only TLR that uses all
four adaptors and activates both the MyD88 and TRIF dependent pathways.18
The MyD88-dependent pathway
After recognition of PAMPs by TLRs, MyD88 recruits the IL-1R
associated kinases IRAK1, IRAK2, IRAK4 and IRAK-M. IRAK
activation results in an interaction with TRAF6 (tumour necrosis
factor receptor associated factor 6), an E3 ligase.18 Additional scaffolding and binding proteins join the complex and several phosphorylation and ubiquitylation steps occur leading to the
phosphorylation of the IKK complex (inhibitor of NFjB [IjB]
kinase complex), which results in the degradation of IjB allowing
NFjB translocation to the nucleus and induction of transcription
of target genes. Simultaneously, the TRAF6 complex also activates
members of the MAPK (mitogen-activated protein kinase) family
such as the stress-activated protein kinase, p38 and Jun N-terminal
kinase, leading to the transcription of additional target genes. As
the result of this pathway, cytokines such as TNFa, IL-1, IL-6 and
IL-12, chemokines such as IL-8 and MIP2, and up-regulation of
costimulatory molecules such as CD40, CD80, CD86 and adhesion
molecules such as ICAM-1 are produced.14,19,20
TLRs 1,2,4-9 utilize the MyD88-dependent pathway to iniate
signalling. TLRs 2 and 4 also utilize TIRAP in the MyD88-dependent pathway.14
JEADV 2011, 25, 9971006
The TRIF-dependent pathway
The TRIF-dependent pathway culminates in the activation of
NFjB and IRF3 (interferon regulatory factor 3). TRIF recruits
TRAF6 for NFjB activation similar to those of the MyD88-dependent pathway. TRIF recruits a signalling complex which catalyse
the phosphorylation of IRF3 and induce its nuclear translocation.
TRAF3 is an important factor in this pathway. While TRAF3 promoting IRF3 activation and interferon b transcription, it inhibits
the MyD88-dependent pathway.18 TLRs 3 and 4 utilize TRIF pathway.14
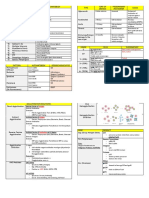
The MyD88-dependent and TRIF-dependent pathways are
summarized in Fig. 1.
Balanced production of inflammatory cytokines and type I
interferon might have key roles in controlling tumour cell growth
and autoimmune diseases. The negative regulation of TLRinduced responses is important for suppressing inflammation and
deleterious immune responses. So far, many negative regulators
that suppress TLR signalling pathways at multiple levels have been
identified. These include splice variants for adaptors or their
related proteins, ubiquitin ligases, deubiquitinases, transcriptional
regulators and microRNAs.18,2124
TLRs and dermatological diseases
In the human skin, TLRs are expressed in different cell types from
the epidermis to the adipose tissue, with great variations in the
expression and functionality depending on the cell type. The most
important epidermal cells expressing TLRs include keratinocytes,
which express TLRs 1-6 and 9, and Langerhans cells which can
express all TLRs, particularly TLRs 1, 2, 3, 5, 6 and 10. Other cells
expressing TLRs include dermal monocytes macrophages, dendritic cells, T and B cells, and mast cells in the dermis, endothelial
cells of the skin microvasculature, and skin stromal cells such as
fibroblasts and adipocytes.1315,2527
TLRs are increasingly being implicated in many immune and
inflammatory diseases, cancer and wound healing.2,8,12,17,28 Besides
infectious and autoimmune diseases, it has been shown that TLRs
have also important roles in CNS, lung, gastrointestinal tract and
kidney diseases.2 The CNS diseases reported to be related with
TLRs are Alzheimers disease29,30 and multiple sclerosis31,32 The
lung diseases that TLRs are important are asthma, C. pneumoniae,
M. tuberculosis, L. pneumophila, C. neoformans and Influenza A
virus infections.33 Expression of TLRs have been elevated in
inflammatory bowel disease, comprising Crohns disease and
ulcerative colitis. Especially TLR4 and TLR5 were reported to be
responsible in inflammatory bowel disease.8,34,35 Elevated TLR4
expression in gastric mucosa has been reported in H. pylori
induced gastritis, too.36 Bacterial pyelonephritis, renal diseases
associated with viral infection such as HIV, CMV, HCV and EBV
virus, immune complex glomerulonephritis or renal vasculitis are
renal diseases that TLR play a role in the pathogenesis of them.37
Recent reports have suggested TLRs roles in the development of
atherosclerosis, type 1 diabetes, allergic diseases, systemic lupus
2011 The Authors
Journal of the European Academy of Dermatology and Venereology 2011 European Academy of Dermatology and Venereology
Ermertcan et al.
1000
Figure 1 TLR signalling, the MyD88- and TRIF-dependent pathways.2
erythematosus, rheumatoid arthritis and malignancies, such as
colon cancer, hepatocellular carcinoma, breast cancer, prostate
cancer, lung cancer, ovarian cancer, multiple myeloma, chronic
lymphocytic leukaemia and melanoma.8,9,11,38
Skin diseases related to TLRs reported other than melanoma are
psoriasis, lichen planus, Behcets disease, acne vulgaris, rosacea,
leprosy, syphilis, Lyme disease, atopic dermatitis and allergic contact dermatitis, mycosis fungoides, non-melanoma skin cancers,
bacterial, fungal and viral skin infections and ultraviolet
injury.2,3,12,1416 It has been postulated that TLRs are important
for inducing pruritus,39 wound healing process17 and hypertrophic
scarring.27 In recent years, TLR dysregulation has been approved
in ageing.40 With respect of this idea, TLRs may be important for
dermatologists in anti-ageing strategies in the future. The skin diseases related with TLRs have been summarized in Table 2.
Table 2 Skin diseases related with TLRs
Skin disease
Related TLRs
References
Acne vulgaris
TLR 2, 4
(2,12,13,41,42)
Psoriasis
TLR 14, 5, 9
(12,13,15,4649)
Atopic dermatitis
TLR 2, 9
(15,25,5255)
Basal cell carcinoma
TLR 7, 8, 9
(7276)
Squamous cell
carcinoma
TLR 7, 8
(77,78)
Melanoma
TLR 4, 7, 9
(67,68)
S. aureus
TLR 2, 6
(14,15)
C. albicans
TLR 2, 4
(13,63)
Herpes simplex
Varicella zoster
TLR 2, 3, 9
(15,59,60,62)
Verruca Molluscum
contagiosum
TLR 3, 7, 9
(1,3,12)
Lyme disease
TLR 1 2
(heterodimers), 4, 6
(2,3,12)
Acne vulgaris
Leprosy
TLR 1, 2
(14,15,64,65)
Acne vulgaris is characterized by non-inflammatory and inflammatory lesions. TLR2 expression was detected in biopsy specimens,
particularly in perifollicular regions, and the number of TLR2positive cells increases in long-term disease.2 In addition, it has
been shown that there is a positive correlation between the severity
of acne lesions and the concentration of cells expressing TLR2.13
Kim et al. demonstrated that TLR2 on human monocytes can be
activated by P. acnes in vitro, resulting in increased production of
IL-12 and IL-8. This demonstration of TLR2 expression at the site
of disease suggests that the inflammation triggered by P. acnes
through TLR2 may be an important factor in the pathogenesis of
acne.41,42 Keratinocytes and sebocytes, located near the piloseba-
Syphilis
TLR 2, 4 5
(heterodimer)
(12,13)
Lichen planus
TLR 9
(12)
Sarcoidosis
TLR 2, 4
(1,12)
Behcets disease
TLR 4, 6
(12)
Systemic lupus
erythematosus
TLR 2, 7, 9
(8,9)
Scleroderma
TLR 4
(12)
JEADV 2011, 25, 9971006
ceous unit, may be capable of detecting either pathogens or abnormal lipids. Human SZ95 sebocytes, in particular, express innate
immune molecules such as TLR2, TLR4, IL1b, IL6, IL8, CD1d and
2011 The Authors
Journal of the European Academy of Dermatology and Venereology 2011 European Academy of Dermatology and Venereology
TLRs and skin
1001
CD14. As a result of TLR stimulation due to P. acnes, proinflammatory cytokines, chemokines, antimicrobial lipids, antimicrobial
peptides and human b-defensin-2 are produced by these cells.12
Interestingly, topical retinoids which are used in the treatment of
acne, have been shown to decrease TLR2 expression.43,44 Nicotinamide, through interaction with TLR2 on keratinocytes significantly depresses IL8 production in a dose-dependent manner.45
Psoriasis
Psoriasis is a chronic inflammatory disease mediated by T cells. It
has been associated with Th1 and Th17 cytokine profiles. Keratinocytes from psoriatic plaques express high levels of TLRs 1, 2, 4,
5 and 9 compared with normal skin. Psoriatic lesions are very
resistant to superinfections by pathogens caused by the presence of
high levels of antimicrobial peptides in the psoriatic plaques. Activation of TLRs has been related to resistance to pathogenic microorganisms. TLR activation has also been implicated in the
exacerbation of the disease. In addition, the antimicrobial peptide
cathelicidin has been shown to present self-DNA to activate TLR9
on plasmacytoid dendritic cells leading to the production of
IFN-a, possibly promoting autoimmunity in psoriasis.12,13
Another growth factor important in psoriasis is TGF-a, which
up-regulates TLR5 and 9 expression and function in human
keratinocytes.46 Heat-shock proteins (i.e. HSP60) are suspected
immunogenic proteins that are heavily expressed by epidermal
keratinocytes of psoriasis. HSP60 may subsequently trigger TLR2
and 4 resulting with development and or aggravation of psoriasis.47,48 In psoriasis lesions, the expression of TLR1 and 2 on keratinocytes is further up-regulated. Keratinocytes in psoriatic skin,
activated by TLR 2, 3 and 4 ligands exhibited NFjB nuclear translocation and release of TNF-a and IL-8.49 TLR 7 and 8 signalling
have also been implicated in psoriatic exacerbations.47 It has been
shown that topical application of the TLR7 agonist imiquimod
induced the spreading of psoriatic plaque.15
Atopic dermatitis and allergic contact dermatitis
Atopic dermatitis (AD) is a chronic inflammatory skin disease
which affects up to 20% of the paediatric population.12 Patients
suffering from AD have greater susceptibility to bacterial, viral and
fungal infections; in fact, S. aureus has been associated with its
flares and severity.25,50 In addition to S. aureus, the best characterized infectious agent of AD, strains of Candida species have a
strong ability to colonize atopic skin, and viruses such as herpes
simplex virus can aggravate the infection and exacerbate the disease.51 The pathophysiology of AD involves the presence of Th2
type immune responses in the skin.14
Recent studies have identified the presence of certain polymorphisms in TLRs or TLR signalling molecules in patients with AD.
It has been shown a strong association between TLR2 and the
symptoms of severe AD in some populations.52,53 However, polymorphism C-123T in the TLR9 gene has been attributed as the
cause for impairment of immunity in some cases of AD. These
defects in TLR2 and 9 may be genetic or functional.54 Polymorphism in the Toll interactive protein (TOLLIP), an inhibitory
adapter protein has also been associated with AD.15,25 However,
there has been no significant correlation between TLRs1 and 6
and AD.53,55 Antiga et al. studied effects of tacrolimus ointment
on Toll-like receptors in AD. They suggested that TLR1 expression
is augmented and TLR2 expression is reduced in AD skin and the
down-regulation of TLR1 and the up-regulation of TLR2 induced
by a 3-week treatment with tacrolimus ointment could be two of
the pharmacological effects of the drug in the treatment of AD.
They also concluded that expression of TLR4 and TLR9 was not
affected by tacrolimus.56
Table 3 Therapeutic agents using in the treatment of skin diseases related with TLRs
Therapeutic agent
Related TLRs
Targeted skin disease
References
Imidazoquinolinamines
TLR 7
Genital warts, superficial basal cell carcinoma, actinic keratosis
(12,13)
TLR 7
Skin cancer
(12)
Imiquimod
Resiquimod
Immunomodulators
Loxoribine
Bropirimine
Calcineurin inhibitors
Atopic dermatitis
Pimecrolimus
TLR 2 6
Tacrolimus
TLR 1, 2
(87)
(56)
Nicotinamide
TLR 2
Acne vulgaris, bullous pemphigoid,
necrobiosis lipoidica, dermatitis herpetiformis
(45)
All trans retinoic acid
TLR 2, 4
Acne vulgaris
(88)
Adapalene
TLR 2
Acne vulgaris
(13)
Zinc salts
TLR 2
Acne vulgaris
(13)
Sodium tosylchloramide (disifin)
TLR 4
Bacterial skin infections
(10)
CpG-ODN
TLR 9
Melanoma
(89,90)
JEADV 2011, 25, 9971006
2011 The Authors
Journal of the European Academy of Dermatology and Venereology 2011 European Academy of Dermatology and Venereology
Ermertcan et al.
1002
Allergic contact dermatitis, another eczematous process, is a
type IV delayed hypersensitivity reaction seen in the skin. The bacterial infections and haptens binding with self-proteins in the skin
leads to activation of dendritic cells stimulating a specific autoreactive CD8 response against the epidermis in a TLRs 2, 4 and
9-dependent fashion.12 Schmidt et al. showed that nickel induced
an inflammatory response by directly activating human TLR4.
They concluded that site-specific human TLR4 inhibition may be
a potential strategy for therapeutic intervention in contact hypersensitivity reaction.57
Skin infections
Staphylococcus aureus skin infections
Staphylococcus aureus causes infections, such as impetigo, folliculitis and cellulitis upon crossing the skin barrier. More severe infections, such as bacteraemia, sepsis and endocarditis can occur, too.
Several components of the bacteria, such as lipoproteins, peptidoglycans and lipoteichoic acid are agonists to TLR2 6 or TLR2 2.
Signalling pathway through TLR2 adapter molecule MyD88 and
the up-regulation of human b-defensin-3 are major contributors
to the immune response against S. aureus.13 In addition, several
in vivo studies in mice have demonstrated that TLR2-deficient
mice are more susceptible to S. aureus skin infection. This
provides evidence that TLR2 is important in host defence against
S. aureus infections in the skin.14,15 In a recent study performed by
Lai et al., they suggested that potential use of normal commensal
bacterium S. epidermidis may be helpful to activate TLR2 signalling and induce antimicrobial peptide expression, thus enabling
the skin to mount an enhanced response to pathogens.58
Herpes simplex virus and Varicella-Zoster virus
Infections by Herpes simplex virus (HSV) and Varicella-Zoster
virus (VZV) typically result in grouped vesicles that ulcerate and
then heal. Several TLRs have been implicated in the immune
response to HSV and VZV.15 TLR2 has been found to recognize
viral envelope proteins and lipopeptides of specific HSV glycoproteins and is also activated during VZV infection of monocytes.59,60
In addition, TLR9 expressed on plasmacytoid dendritic cells and
myeloid dendritic cells has been shown to recognize and initiate
cytokine production in response to HSV infection and HSV
DNA.61 Furthermore, individuals deficient in TLR3 had increased
spreading of HSV infection from keratinocytes to cranial nerves,
resulting in an increased susceptibility to HSV encephalitis.62
Candidiasis
Clinical infections caused by Candida albicans include mucocutaneous infections as well as invasive and life-threatening infections
usually seen in immunocompromised patients.14 In vitro studies
have demonstrated that TLR2 recognizes the Candida albicans cell
wall surface glycolipid phospholipomannan and TLR4 recognizes
the Candida albicans cell wall polysaccharide manan.63 Activation
JEADV 2011, 25, 9971006
of TLRs by Candida albicans induces the production of proinflammatory cytokines, candidicidal effector molecules and chemoattractant molecules to recruit other inflammatory molecules to
the site of infection.13
Leprosy
Leprosy is characterized by a broad clinical spectrum changing
according to the hosts immunological response to Mycobacterium
leprae. When the hosts immunologic response is strong and driven by cell-mediated Th1 cytokines, tuberculosis form of the disease occur. However, a hosts response with Th2 type cytokines
that promote a humoural immune response causes a more disseminated disease, the lepromatous form of the disease.13 There is
strong evidence implicating TLRs 1 and 2 in the pathophysiology
of leprosy. It has been demonstrated that lepromatous leprosy
patients had a TLR2 polymorphism which was associated with
decreased serum IL-12. TLR2 polymorphism that impair TLR2
function have been shown to have an increased susceptibility to
the development of lepromatous form.64
Krutzik et al. demonstrated that TLRs 1 and 2 are more
strongly expressed in lesions of tuberculoid patients compared
with lepromatous patients.65 It has been shown that TLR2 may
also cause apoptosis of the Schwann cells and increase nerve
damage in leprosy.14,15
Syphilis
In syphilis, the interaction of lipopeptides expressed on the surface
of Treponema pallidum with TLR2 receptors on dendritic cells is
thought to be involved in enhancement of the adaptive immune
system through T-cell activation and Th1 cytokine release. In addition, the polymers of flagellin, key components of the T. pallidum
flagellum, function as another PAMP. Flagellin polymers bind to
TLR5 and leads to production of proinflammatory cytokines, such
as TNF-a.13
Lyme disease
Lyme disease is caused by infection with the spirochete Borrelia
burgdorferi. One of the antigens of B. burgdorferi capable of stimulating an immune response is the outer surface protein A lipoprotein (OspA). It has been shown that TLR2 and 6 are necessary for
OspA induced NFjB activation. Recent studies have demonstrated
that TLR2 1 heterodimers are necessary to recognize OspA.
Patients with erythema migrans were found to have peripheral
monocytes with higher surface expression of TLR1 and 2. Furthermore, monocytoid dendritic cells demonstrated increased levels of
TLR2 and 4 expression.2,3
Ultraviolet injury
UVB radiation stimulates the up-regulation of HSPs from keratinocytes exposed to UVB. These HSPs are capable of binding to
TLRs 2 and 4 and stimulating the Toll IL-1 pathway in dendritic
cells. This signalling induces the downstream production of
2011 The Authors
Journal of the European Academy of Dermatology and Venereology 2011 European Academy of Dermatology and Venereology
TLRs and skin
1003
immunosuppressive cytokines, such as IL-10 and TNF-a. This
may explain the additional role of UVB in cancer development
besides its direct mutagenic effect.66
Melanoma
Melanoma is a malignant tumour of melanocytes which exposure
to UV radiation is the main risk factor for the disease. Melanocytes have the ability to help tumour progression in melanoma
by responding to hyaluronic acid fragments through TLR4 by
inducing MMP and cytokine production. Although melanocytes
have been shown to express other TLRs, TLR9 has been targeted
for modulating immune response.67,68 Many TLR ligands are
considered good adjuvant candidates as they can activate dendritic cells. TLR9 targeting appears to be a viable option in melanoma treatment. Different TLR9 agonists are now included in
vaccine formulations for human trials.69,70 Imiquimod, TLR7
agonist, was used to harness the potential TLR7 based treatment
for melanoma. It has found to be effective in both activating dendritic cells and producing tumour-specific cytotoxic T cells that
arrest disease progression.71
Non-melanoma skin cancers
Non-melanoma skin cancer (NMSC) is the most common form
of cancer worldwide. The two major types of NMSC are basal cell
carcinoma (BCC) and squamous cell carcinoma (SCC). They typically occur in areas of chronic sun exposure. Imiquimod has been
administered successfully as a topical immune modulator which
induces production of IFN-a and IL-2 mediated by TLR7. TLRs 7
and 8 have been manipulated to activate the proinflammatory
machinery against BCC and SCC.7278
Systemic lupus erythematosus
Systemic lupus erythematosus (SLE) is a systemic inflammatory
disorder characterized by small vessel vasculitis affecting multiple
organs and is thought to result from a breakdown of tolerance to
ubiquitous self-antigens, including DNA and RNA. Defects in
apoptosis induction, defective clearance of immunostimulatory
cell debris or a hyperactive B-cell receptor are the driving forces in
the development of SLE.8 Autoantibodies against DNA or chromatin bind DNA released from dying cells, forming complexes
which are most effective in stimulating dendritic cells via TLR9.
Similar to DNA and DNA-containing immune complexes, RNA
and RNA containing immune complexes have been implicated in
the pathogenesis of SLE via activation of TLR7 signalling pathways. Increased levels of IFN-a have long been known to occur in
SLE and have been associated with disease activity. It is feasible to
assume that increased production of IFN-a in SLE is a reaction to
constant activation of TLR pathways.9 In recent years, the roles of
TLR7 and 8 have been supported in the onset of SLE.8 Whereas
expression of mRNA for TLR2, 7 and 9 were found to be elevated
in peripheral blood mononuclear cells of patients with SLE, TLR3,
4, 5 and 8 were not.9
JEADV 2011, 25, 9971006
Role of TLRs in the treatment of skin diseases
As activation of TLRs induce immune responses, there has been a
growing interest in pharmacologic targeting of TLRs in the treatment of several diseases including some skin diseases and skin
cancer.15
Imiquimod, a member of the family of imidazoquinoline compounds, is the first TLR agonist approved for use in humans. Imiquimod and resiquimod are two compounds that are efficient at
activating the immune system. They have potent antiviral and antitumoural properties.12,13 Imidazoquinolines have been identified as
a TLR7 ligand, capable of inducing NFjB through MyD88-dependent pathway in macrophages. They induce the production of
several cytokines including IFN-a, IFN-c, TNF-a and IL-6, IL-8
and IL-12, stimulating the proliferation and maturation of naive
(Th0) lymphocytes, particularly toward Th1 lymphocytes. Furthermore, imiquimod induces langerhans cells to migrate to the lymph
nodes, enhancing antigen presentation to T cells. Imiquimod was
firstly approved for the treatment of genital warts in 1997. Because
of its effective anti-tumoural activity, it was also approved in 2004
for the treatment of superficial basal cell carcinoma and actinic keratosis.13 Current off-label indications for imiquimod include verruca vulgaris, molluscum contagiosum, herpes simplex virus
infections, keloids, Bowens disease, squamous cell carcinoma, lentigo maligna, cutaneous T-cell lymphoma, Kaposis sarcoma, Pagets disease, alopecia areata and vitiligo.7884 Resiquimod is 100
times more potent than imiquimod and it has been used mainly for
the treatment of actinic keratosis and genital HSV2 infections.85,86
Two other immunomodulators which function through TLR7,
loxoribine and bropirimine have also been used. Loxoribine, a
guanosine ribonucleoside, enhances production of IFN and activates NK cells and B cells. Broprimine, an aryl pyrimidinone class
of anti-neoplastic compounds, has a similar effect to loxoribine
and is currently in clinical studies for treatment of carcinomas.12
Calcineurin inhibitors are potent suppressors of the T-cellmediated immune response caused by their ability to inactivate
the serine protease calcineurin. They prevent nuclear translocation
and inhibit the synthesis of proinflammatory cytokines in T cells.
Topical application of pimecrolimus and tacrolimus has primarily
been used in atopic dermatitis. Pimecrolimus has been shown to
enhance the ability of keratinocytes to fight infection when coadministered with TLR2 6 ligands.87 A recent study about the effects
of tacrolimus ointment on Toll-like receptors in atopic dermatitis
revealed that tacrolimus induces the down-regulation of TLR1 and
the up-regulation of TLR2.56
The other topical agents found to have TLR activity are nicotinamide, all trans retinoic acid, adapalene, zinc and sodium tosylchloramide (disifin).13
Nicotinamide, an amide derivative of vitamin B3, inhibits cytokine production and leukocyte chemotaxis. It has been used both
topically and systemically in several diseases including bullous
pemphigoid, necrobiosis lipoidica, dermatitis herpetiformis and
2011 The Authors
Journal of the European Academy of Dermatology and Venereology 2011 European Academy of Dermatology and Venereology
Ermertcan et al.
1004
acne. It down-regulates IL-8 gene expression and IL-8 production
through phosphorylation of the MAPK and TLR2-dependent IjB
degredation, preventing activation of NFjB.45 All trans retinoic
acid directly suppressed TLR-mediated inflammation most likely
by effecting TLR signalling or mRNA stability. It inhibits the
P. acnes dependent activation of TLR 2 and 4.88 It has been shown
that adapalene, a second generation topical retinoid, and zinc salts
also decrease the expression of TLR2 on keratinocytes.13 Disifin is
an efficient disinfectant found to have bactericidal effects on the
skin. It has been mentioned that its effects are related with the
TLR4 activation.10
TLR agonists represent potential adjuvants for vaccines and
cancer immunotherapy. Especially TLR9 agonists are expected to
be safer adjuvants because of their narrow expression profile
among TLRs in humans.13,15 CpG-ODN, a TLR9 agonist, has been
used topically with systemic dacarbazine (DTIC) for cutaneous
melanoma in mice. Combination of the two agents together significantly inhibited tumour growth comparing with the administration of each individual agent.89 In addition, it has been
demonstrated that TLR9 agonists can be used in anti-cancer vaccines against melanoma and other cancers.1,38,90
Therapeutic agents using in the treatment of skin diseases
related with TLRs have been summarized in Table 3.
Conclusions
TLRs play a crucial role in the infectious diseases, inflammatory
diseases and cancer. TLRs have been shown to be important in
cutaneous host defence mechanisms in the skin. Different TLRs
are associated with the pathogenesis of several skin diseases. Development of TLR-based therapies for skin diseases and skin cancer
has gained interest by understanding of the TLR signalling and
discovery of topical TLR agonists, especially imiquimod.
Future research is necessary on the relationship between TLRs
and skin diseases, and TLR-based treatments. The success of these
therapies will require detailed and multidisciplinary trials for optimization of dosage, long-term effects and side effects. As dysregulation of TLR signalling has been shown, we hope that therapeutic
manipulation of TLRs may be used for anti-ageing strategies.
References
1 Ishii KJ, Akira S. Innate immunity. In Rich RR, Fleisher TA, Shearer
WT, Schroeder HW Jr, Frew AJ, Weyand CM, eds. Clinical Immunology
Principles and Practice, 3rd edn. Elsevier Ltd, Philadelphia, 2008: 3951.
2 Chen K, Huang J, Gong W et al. Toll like receptors in inflammation,
infection and cancer. Int Immunopharmacol 2007; 7: 12711285.
3 Mclnturff JE, Modlin RL, Kim J. The role of Toll-like receptors in the
pathogenesis and treatment of dermatological disease. J Invest Dermatol
2005; 125: 18.
4 Janeway CA, Jr, Medzhitov R. Innate immune recognition. Annu Rev
Immunol 2002; 20: 197.
5 Liew FY, Xu D, Brint EK, ONeill LA. Negative regulation of toll-like receptor-mediated immune responses. Nat Rev Immunol 2005; 5: 446458.
6 Visvanathan K, Maclsaac CM, Hall WW, Fischetti VA. Immunological
aspects of infection. In Zabriskie JB, ed. Essential Clinical Immunology.
Cambridge University Press, New York, 2009: 4560.
JEADV 2011, 25, 9971006
7 Cook DN, Pisestsky DS, Schwartz DA. Toll-like receptors in the pathogenesis of human disease. Nat Immunl 2004; 5: 975.
8 Drexler SK, Foxwell BM. The role of Toll-like receptors in chronic
inflammation. Int J Biochem Cell Biol 2010; 42: 506518.
9 Ospelt C, Gay S. TLRs and chronic inflammation. Int J Biochem Cell
Biol 2010; 42: 495505.
10 Ofodile ON. Disifin (Sodium tosylchloramine) and Toll-like receptors
(TLRs): evolving importance in health and diseases. J Ind Microbiol Biotechnol 2007; 34: 751762.
11 Montero Vega MT, de Andres Martin A. The significance of toll-like
receptors in human diseases. Allergol Immunopathol 2009; 37: 252263.
12 Hari A, Flach TL, Shi Y, Mydlarski PR. Toll-like receptors: role in dermatological disease. Mediators Inflamm 2010; 2010: 437246. Epub 2010
Aug 22.
13 Valins W, Amini S, Berman B. The expression of Toll-like receptors in
dermatological diseases and the therapeutic effect of current and newer
topical Toll-like receptor modulators. J Clin Aesthet Dermatol 2010;
3(9): 2029.
14 Miller LS, Modlin RL. Toll-like receptors in the skin. Semin Immunopathol 2007; 29: 1526.
15 Miller LS. Toll-like receptors in skin. Adv Dermatol 2008; 24: 7187.
16 Kulczycka L, Sysa-Jedrzejowska A, Robak E. Role of Toll-like receptors
in etiology of selected diseases of the skin. Postepy Hig Med Dosw
(online) 2010; 64: 364371.
17 Sato T, Yamamoto M, Shimosato T, Klinman DM. Accelerated wound
healing mediated by activation of Toll-like receptor 9. Wound Repair
Regen 2010; 18(6): 586593. Epub 2010 Oct 13.
18 Kawai T, Akira S. The role of pattern-recognition receptors in innate
immunity: update on Toll-like receptors. Nat Immunol 2010; 11: 373
384.
19 Kaisho T, Akira S. Toll-like receptor function and signaling. J Allergy
Clin Immunol 2006; 117: 979987.
20 Akira S, Takeda K. Toll-like receptor signalling. Nat Rev Immunol 2004;
4: 499511.
21 Palsson-McDermott EM, Doyle SL, McGettrick AF et al. TAG, a splice
variant of the adaptor TRAM, negatively regulates the adaptor MyD88independent TLR4 pathway. Nat Immunol 2009; 10: 579586.
22 Shi M, Deng W, Bi E et al. TRIM30a negatively regulates TLR-mediated NF-jB activation by targetting TAB2 and TAB3 for degradation.
Nat Immunol 2008; 9: 369377.
23 Kayagaki N, Phung Q, Chan S et al. DUBA: a deubiquitinase that regulates type I interferon production. Science 2007; 318: 16281632.
24 Sheedy FJ, Palsson-McDermott E, Hennessy EJ et al. Negative regulation of TLR4 via targeting of the proinflammatory tumor suppressor
PDCD4 by the microRNA miR-21. Nat Immunol 2010; 11: 141147.
25 Lai Y, Gallo RL. Toll-like receptors in skin infections and inflammatory
diseases. Infect Disord Drug Targets 2008; 8: 144155.
26 Lew BL, Sim WY, Kim NI. Expression of Toll-like receptor 2 in cultured human keratinocytes: the effect of bacterial antigens, cytokines
and calcium concentration. Ann Dermatol 2009; 21: 337344.
27 Wang JF, Hori K, Ding J et al. Toll-like receptors expressed by dermal
fibroblasts contribute to hypertrophic scarring. J Cell Physiol 2011; 226:
12651273.
28 ONeill LA, Bryant CE, Doyle SL. Therapeutic targeting of toll-like
receptors for infectious and inflammatory diseases and cancer. Pharmacol Rev 2009; 61: 177197.
29 Olson CK, Miller SD. Microglia initiate central nervous system innate
and adaptive immune responses through multiple TLRs. J Immunol
2004; 173: 39163924.
30 McKimmie CS, Fazakerley JK. In response to pathogens, glial cells
dynamically and differentially regulate Toll-like receptor gene expression. J Neuroimmunol 2005; 169: 116125.
31 Prinz M, Garbe F, Schmidt H et al. Innate immunity mediated by
TLR9 modulates pathogenicity in an animal model of multiple sclerosis.
J Clin Invest 2006; 116: 456464.
2011 The Authors
Journal of the European Academy of Dermatology and Venereology 2011 European Academy of Dermatology and Venereology
TLRs and skin
1005
32 Jack C, Ruffini F, Bar-Or A, Antel JP. Microglia and multiple sclerosis.
J Neurosci Res 2005; 81: 363373.
33 Basu S, Fenton MJ. Toll-like receptors: function and roles in lung
disease. Am J Physiol Lung Cell Mol Physiol 2004; 286: 887892.
34 Torok HP, Glas J, Tonenchi L et al. Polymorphisms of the lipopolysaccharide-signaling complex in inflammatory bowel disease: association of
a mutation in the Toll-like receptor 4 gene with ulcerative colitis. Clin
Immunol 2004; 112: 8591.
35 Singh JC, Cruickshank SM, Newton DJ et al. Toll-like receptormediated responses of primary intestinal epithelial cells during the
development of colitis. Am J Physiol Gastrointest Liver Physiol 2005;
288: 514524.
36 Ishihara S, Rumi MA, Kadowaki Y et al. Essential role of MD-2 in
TLR4-dependent signaling during Helicobacter pylori-associated gastritis.
J Immunol 2004; 173: 14061416.
37 Anders HJ, Banas B, Schlondorff D. Signaling danger: toll receptors and
their potential roles in kidney disease. J Am Soc Nephrol 2004; 15: 854
867.
38 So EY, Ouchi T. The application of Toll like receptors for cancer therapy. Int J Biol Sci 2010; 6: 675681.
39 Liu T, Xu ZZ, Park CK et al. Toll-like receptor 7 mediates pruritus.
Nat Neurosci 2010; 13: 14601462.
40 Shaw AC, Panda A, Joshi SR et al. Dysregulation of human Toll-like
receptor function in aging. Ageing Res Rev 2010, Nov 10. doi: 10.1016/
j.arr.2010.10.007. [Epub ahead of print].
41 Kim J, Ochoa MT, Krutzik SR et al. Activation of toll-like receptor 2 in
acne triggers inflammatory cytokine responses. J Immunol 2002; 169:
15351541.
42 Mclnturff JE, Kim J. The role of Toll-like receptors in the pathophysiology of acne. Semin Cutan Med Surg 2005; 24: 7378.
43 Liu PT, Krutzik SR, Kim J, Modlin RL. Cutting edge: all-trans retinoic
down-regulates TLR2 expression and function. J Immunol 2005; 174(5):
24672470.
44 Tenaud I, Khammari A, Dreno B. In vitro modulation of TLR-2, CD1d
and IL-10 by adapalene on normal human skin and acne inflammatory
lesions. Exp Dermatol 2007; 16: 500506.
45 Grange PA, Raingeud J, Calvez V, Dupin N. Nicotinamide inhibits
Propionibacterium acnes-induced IL-8 production in keratinocytes
through the NF-jB and MAPK pathways. J Dermatol Sci 2009; 56:
106112.
46 Miller LS, Sorensen OE, Liu PT et al. TGF-a regulates TLR expression
and function on epidermal keratinocytes. J Immunol 2005; 174: 6137
6143.
47 Gaspari AA. Innate and adaptive immunity and the pathophysiology of
psoriasis. J Am Acad Dermatol 2006; 54: S67S80.
48 Seung NR, Park EJ, Kim CW et al. Comparison of expression of heatshock protein 60, Toll-like receptors 2 and 4, T cell receptor cd in
plaque and guttate psoriasis. J Cutan Pathol 2007; 34: 903911.
49 Begon E, Michel L, Flageul B et al. Expression, subcellular localization
and cytokinic modulation of Toll-like receptors (TLRs) in normal
human keratinocytes: TLR2 up-regulation in psoriatic skin. Eur J
Dermatol 2007; 17: 497506.
50 Cho SH, Strickland I, Boguniewicz M, Leung DYM. Fibronectin and
fibrinogen contribute to the enhanced binding of Staphylococcus aureus
to atopic skin. J Allergy Clin Immunol 2001; 108: 269274.
51 McGirt LY, Beck LA. Innate immune defects in atopic dermatitis.
J Allergy Clin Immunol 2006; 118: 202208.
52 Hasannejad H, Takahashi R, Kimishima M et al. Selective impairment
of Toll-like receptor 2 mediated proinflammatory cytokine production
by monocytes from patients with atopic dermatitis. J Allergy Clin
Immunol 2007; 120: 6975.
53 Oh DY, Schumann RR, Hamann L et al. Association of the toll-like
receptor 2 A-16934T promoter polymorphism with severe atopic
dermatitis. Allergy 2009; 64: 16081615.
JEADV 2011, 25, 9971006
54 Novak N, Yu CF, Bussmann C et al. Putative association of a TLR9
promoter polymorphism with atopic eczema. Allergy 2007; 62: 766772.
55 Novak N. New insights into the mechanism and management of allergic
diseases: atopic dermatitis. Allergy 2009; 64: 265275.
56 Antiga E, Volpi W, Torchia D et al. Effects of tacrolimus ointment on
Toll-like receptors in atopic dermatitis. Clin Exp Dermatol 2010, Nov
10. doi: 10. 1111 j.1365-2230.2010.03948.x. [Epub ahead of print]
57 Schmidt M, Raghavan B, Muller V et al. Crucial role for human Tolllike receptor 4 in the development of contact allergy to nickel. Nat
Immunol 2010; 11: 814820.
58 Lai Y, Cogen AL, Radek KA et al. Activation of TLR2 by a small molecule produced by Staphylococcus epidermidis increases antimicrobial
defense against bacterial skin infections. J Invest Dermatol 2010; 130:
22112221.
59 Sato A, Linehan MM, Iwasaki A. Dual recognition of herpes simplex
viruses by TLR2 and TLR9 in dendritic cells. Proc Natl Acad Sci USA
2006; 103: 1734317348.
60 Wang JP, Kurt-Jones EA, Shin OS et al. Varicella-zoster virus activates
inflammatory cytokines in human monocytes and macrophages via
Toll-like receptor 2. J Virol 2005; 79: 1265812666.
61 Lund J, Sato A, Akira S et al. Toll-like receptor 9-mediated recognition
Herpes simplex virus-2 by plasmacytoid dendritic cells. J Exp Med 2003;
198: 513520.
62 Zhang SY, Jouanguy E, Ugolini S et al. TLR3 deficiency in patients with
herpes simplex encephalitis. Science 2007; 317: 15221527.
63 Jouault T, Ibata-Ombetta S, Takeuchi O et al. Candida albicans phospholipomannan is sensed through toll-like receptors. J Infect Dis 2003;
188: 165172.
64 Kang TJ, Lee SB, Chae GT. A polymorphism in the toll-like receptor 2
is associated with IL-12 production from monocyte in lepromatous leprosy. Cytokine 2002; 20: 5662.
65 Krutzik SR, Ochoa MT, Sieling PA et al. Activation and regulation of
Toll-like receptors 2 and 1 in human leprosy. Nat Med 2003; 9: 525
532.
66 Kang SS, Kauls LS, Gaspari AA. Toll-like receptors: applications to
dermatologic disease. J Am Acad Dermatol 2006; 54: 951983.
67 Yu N, Zhang S, Zuo F et al. Cultured human melanocytes express functional Toll-like receptors 2-4, 7 and 9. J Dermatol Sci 2009; 56: 113
120.
68 Fang L, Lonsdorf AS, Hwang ST. Immunotherapy for advanced melanoma. J Invest Dermatol 2008; 128: 25962605.
69 Speiser DE, Lienard D, Rufer N et al. Rapid and strong human CD8+
T cell responses to vaccination with peptide, IFA, and CpG oligodeoxynucleotide 7909. J Clin Invest 2005; 115: 739746.
70 Pashenkov M, Goess G, Wagner C et al. Phase II trial of a toll-like
receptor 9 activating oligonucleotide in patients with metastatic melanoma. J Clin Oncol 2006; 24: 57165724.
71 Steinmann A, Funk JO, Schuler G, Von den Driesch P. Topical imiquimod treatment of a cutaneous melanoma metastasis. J Am Acad Dermatol 2000; 43: 555556.
72 Ruiz-Villaverde R, Sanchez-Cano D, Burkhardt-Perez P. Superficial
basal cell carcinoma treated with imiquimod 5% topical cream for a 4week period: a case series. J Eur Acad Dermatol Venereol 2009; 23: 828
831.
73 Schulze HJ, Cribier B, Requena L et al. Imiquimod 5% cream for the
treatment of superficial basal cell carcinoma: results from a randomized
vehicle-controlled phase III study in Europe. Br J Dermatol 2005; 152:
939947.
74 Vun Y, Siler G. Use of 5% imiquimod cream in the treatment of facial
basal cell carcinoma: a 3-year retrospective follow-up study. Australas J
Dermatol 2006; 47: 169171.
75 van der Geer S, Ostertag JU, Krekels GA. Treatment of basal cell carcinomas in patients with nevoid basal cell carcinoma syndrome. J Eur
Acad Dermatol Venereol 2009; 23: 308313.
2011 The Authors
Journal of the European Academy of Dermatology and Venereology 2011 European Academy of Dermatology and Venereology
Ermertcan et al.
1006
76 Kocabas E, Ermertcan AT, Bilac C et al. Nonsyndromic multiple basal
cell carcinomas successfully treated with imiquimod 5% cream. Cutan
Ocul Toxicol 2010; 29: 300302.
77 Weinberg AS, Ogle CA, Shim EK. Metastatic cutaneous squamous cell
carcinoma: an update. Dermatol Surg 2007; 33: 885899.
78 Micali G, Lacarrubba F, Dinotta F et al. Treating skin cancer with topical cream. Exp Opin Pharmacother 2010; 11: 15151527.
79 Viera MH, Amini S, Huo R et al. Herpes simplex virus and human
papillomavirus genital infections: new and investigational therapeutic
options. Int J Dermatol 2010; 49: 733749.
80 Fenske NA, Spencer J, Adam F. Actinic keratoses: past, present and
future. J Drugs Dermatol 2010; 9: 4549.
81 Love WE, Bernhard JD, Bordeaux JS. Topical imiquimod or fluorouracil therapy for basal and squamous cell carcinoma: a systematic review.
Arch Dermatol 2009; 145: 14311438.
82 Farkas A, Kemeny L, French LE, Dummer R. New and experimental
skin-directed therapies for cutaneous lymphomas. Skin Pharmacol Physiol 2009; 22: 322334.
83 Ganjian S, Ourian AJ, Shamtoub G et al. Off-label indications for imiquimod. Dermatol Online J 2009; 15: 4.
JEADV 2011, 25, 9971006
84 Novak N, Yu CF, Bieber T, Alam JP. Toll-like receptor 7 agonists and
skin. Drug News Perspect 2008; 21: 158165.
85 Szeimies RM, Bichel J, Ortonne JP et al. A phase II dose-ranging study
of topical resiquimod to treat actinic keratosis. Br J Dermatol 2008; 159:
205210.
86 Fife KH, Meng TC, Ferris DG, Liu P. Effect of resiquimod 0.01%
gel on lesion healing and viral shedding when applied to genital
herpes lesions. Antimicrob Agents Chemother 2008; 52: 477
482.
87 Buchau AS, Schauber J, Hultsch T et al. Pimecrolimus enhances
TLR2 6-induced expression of antimicrobial peptides in keratinocytes.
J Invest Dermatol 2008; 128: 26462654.
88 Liu PT, Krutzik SR, Kim J. Cutting edge: all-trans retinoic acid downregulates TLR2 expression and function. J Immunol 2005; 174:
24672470.
89 Najar HM, Dutz JP. Topical CpG enhances the response of murine
malignant melanoma to dacarbazine. J Invest Dermatol 2008; 128:
22042210.
90 Krieg AM. Development of TLR9 agonists for cancer therapy. J Clin
Invest 2007; 117: 11841194.
2011 The Authors
Journal of the European Academy of Dermatology and Venereology 2011 European Academy of Dermatology and Venereology
Anda mungkin juga menyukai
- Immunology Unveiled: A Comprehensive Journey through the Human Immune System: Guardians of the Body: The Unseen Heroes of ImmunityDari EverandImmunology Unveiled: A Comprehensive Journey through the Human Immune System: Guardians of the Body: The Unseen Heroes of ImmunityBelum ada peringkat
- Toll-Like Receptors As Key Mediators in Innate Antifungal ImmunityDokumen14 halamanToll-Like Receptors As Key Mediators in Innate Antifungal ImmunityKlaus Ramirez SuarezBelum ada peringkat
- TLR DrosophilaDokumen8 halamanTLR DrosophilaSaraTorresBelum ada peringkat
- Toll-Like Receptors: The Swiss Army Knife of Immunity and Vaccine DevelopmentDokumen10 halamanToll-Like Receptors: The Swiss Army Knife of Immunity and Vaccine DevelopmentWilson Barros LuizBelum ada peringkat
- Fimmu 05 00386Dokumen13 halamanFimmu 05 00386Dani PazBelum ada peringkat
- Fimmu 13 812774Dokumen22 halamanFimmu 13 812774nutritionist1234567Belum ada peringkat
- Pathogen Recognition With Toll-Like Receptors: Taro Kawai and Shizuo AkiraDokumen7 halamanPathogen Recognition With Toll-Like Receptors: Taro Kawai and Shizuo Akiraetik ainun rohmahBelum ada peringkat
- Toll-Like Receptors Gene Polymorphisms in Autoimmune DiseaseDokumen11 halamanToll-Like Receptors Gene Polymorphisms in Autoimmune Diseasecheese schedarBelum ada peringkat
- Toll-Like Receptors (TLRS) and Nod-Like Receptors (NLRS) in InflammatoryDokumen12 halamanToll-Like Receptors (TLRS) and Nod-Like Receptors (NLRS) in InflammatoryLarissa SilvaBelum ada peringkat
- Pathologic Basis of Veterinary Disease, 4th Edition: Chapter 5 Diseases of ImmunityDokumen88 halamanPathologic Basis of Veterinary Disease, 4th Edition: Chapter 5 Diseases of ImmunityEdzel Tisado SacloloBelum ada peringkat
- The Role of Pattern-Recognition Receptors in Innate Immunity: Update On Toll-Like ReceptorsDokumen12 halamanThe Role of Pattern-Recognition Receptors in Innate Immunity: Update On Toll-Like ReceptorslilianapradaBelum ada peringkat
- MicrobialDerived Tolllike Receptor Agonism in Cancer Treatment and ProgressionCancersDokumen20 halamanMicrobialDerived Tolllike Receptor Agonism in Cancer Treatment and ProgressionCancersKajelcha FikaduBelum ada peringkat
- Review Article: Holding The Inflammatory System in Check: Tlrs and Their Targeted Therapy in AsthmaDokumen9 halamanReview Article: Holding The Inflammatory System in Check: Tlrs and Their Targeted Therapy in AsthmaArianRizkiAmaliaBelum ada peringkat
- Tollip: A Multitasking Protein in Innate Immunity and Protein TraffickingDokumen8 halamanTollip: A Multitasking Protein in Innate Immunity and Protein TraffickingFadhil AhsanBelum ada peringkat
- Review: Toll-Like Receptors and The Control of ImmunityDokumen23 halamanReview: Toll-Like Receptors and The Control of ImmunityIrma NeyraBelum ada peringkat
- 2019 Article 302Dokumen11 halaman2019 Article 302Noy FaridaBelum ada peringkat
- Allergy - 2019 - MaedaDokumen15 halamanAllergy - 2019 - MaedaLUAN SILVABelum ada peringkat
- Review Article: Viral Modulation of Tlrs and Cytokines and The Related Immunotherapies For Hpv-Associated CancersDokumen17 halamanReview Article: Viral Modulation of Tlrs and Cytokines and The Related Immunotherapies For Hpv-Associated CancersmarconijrrBelum ada peringkat
- Yang 2017Dokumen10 halamanYang 2017wendyBelum ada peringkat
- Gurung 2016Dokumen17 halamanGurung 2016HAVIZ YUADBelum ada peringkat
- Disifin Evolving Importance in Health Okom Nkili F.C OfodileDokumen12 halamanDisifin Evolving Importance in Health Okom Nkili F.C OfodilenassmargBelum ada peringkat
- Beyond Defense: Regulation of Neuronal Morphogenesis and Brain Functions Via Toll-Like ReceptorsDokumen13 halamanBeyond Defense: Regulation of Neuronal Morphogenesis and Brain Functions Via Toll-Like ReceptorsNicole MeloBelum ada peringkat
- Macrophage Subsets Exhibit Distinct E. coli-LPS Tolerisable Cytokines Associated With The Negative Regulators, IRAK-M and TollipDokumen19 halamanMacrophage Subsets Exhibit Distinct E. coli-LPS Tolerisable Cytokines Associated With The Negative Regulators, IRAK-M and TollipFaeGiNBelum ada peringkat
- Toll Like Receptor 4Dokumen10 halamanToll Like Receptor 4NajeebBelum ada peringkat
- Texto Tesis DefinitivoDokumen173 halamanTexto Tesis DefinitivoPEREZ BLAS MAGALI MONSERRATBelum ada peringkat
- A. Immunohematology: I. Basic PrinciplesDokumen15 halamanA. Immunohematology: I. Basic PrinciplesAdi ParamarthaBelum ada peringkat
- Nat Rev Immunol 2011 WestDokumen15 halamanNat Rev Immunol 2011 WestGabriel CamarenaBelum ada peringkat
- Toll-Like Receptor Signaling Pathways: Takumi Kawasaki and Taro KawaiDokumen8 halamanToll-Like Receptor Signaling Pathways: Takumi Kawasaki and Taro Kawainicky_kelly_3Belum ada peringkat
- Review Article The Role of Innate Immunity in Pulmonary InfectionsDokumen14 halamanReview Article The Role of Innate Immunity in Pulmonary InfectionsAbalzBelum ada peringkat
- Immunologyoffungal Infections: Oscar A. Fernández-García,, Jennifer M. Cuellar-RodríguezDokumen16 halamanImmunologyoffungal Infections: Oscar A. Fernández-García,, Jennifer M. Cuellar-RodríguezsilviaBelum ada peringkat
- Dantas 2020Dokumen16 halamanDantas 2020ShreyaBelum ada peringkat
- 1 s2.0 S0021925820870148 MainDokumen11 halaman1 s2.0 S0021925820870148 MainAina SarahBelum ada peringkat
- Molecular Mechanisms in Genetically Defined Autoinflammatory Diseases. Disorders of Amplified Danger SignalingDokumen58 halamanMolecular Mechanisms in Genetically Defined Autoinflammatory Diseases. Disorders of Amplified Danger SignalingAlmudena MeiBelum ada peringkat
- Keestra Et Al 2010 tlr21Dokumen9 halamanKeestra Et Al 2010 tlr21misilpiyapiyoBelum ada peringkat
- Torsten, 2008 - Immune Recognition of Streptococcus Pyogenes by Dendritic CellsDokumen8 halamanTorsten, 2008 - Immune Recognition of Streptococcus Pyogenes by Dendritic CellsRima Carolina Bahsas ZakyBelum ada peringkat
- Basic Immunology Functions and Disorders of The Immune System 5th Edition Abbas Test BankDokumen26 halamanBasic Immunology Functions and Disorders of The Immune System 5th Edition Abbas Test BankRussellFischerqxcj98% (55)
- Aspectos InmunologicosDokumen11 halamanAspectos InmunologicosjafralizBelum ada peringkat
- Immune Response Profiles in Human Skin: Epithelial DefenseDokumen7 halamanImmune Response Profiles in Human Skin: Epithelial Defensematrixx15Belum ada peringkat
- 1974 - Journal of Allergy and Clinical ImmunologyDokumen13 halaman1974 - Journal of Allergy and Clinical ImmunologyijposadaaBelum ada peringkat
- Immune Surveillance in The Skin: Mechanisms and Clinical ConsequencesDokumen14 halamanImmune Surveillance in The Skin: Mechanisms and Clinical ConsequencesRhirin Fardianti AtmayasariBelum ada peringkat
- Avian VirusesDokumen10 halamanAvian VirusesMohsan UllahBelum ada peringkat
- Autoimmunity in Atopic Dermatitis: Biomarker or Simply Epiphenomenon?Dokumen8 halamanAutoimmunity in Atopic Dermatitis: Biomarker or Simply Epiphenomenon?Miguel RomeroBelum ada peringkat
- Sha Et Al-2004Dokumen7 halamanSha Et Al-2004Dani PazBelum ada peringkat
- Helminth Infections - Recognition and Modulation of The Immune Response by Innate Immune CellsDokumen12 halamanHelminth Infections - Recognition and Modulation of The Immune Response by Innate Immune CellsponbohacopBelum ada peringkat
- Immunity To Fungi: Tobias M Hohl, Amariliz Rivera and Eric G PamerDokumen8 halamanImmunity To Fungi: Tobias M Hohl, Amariliz Rivera and Eric G PamerPieralessandro LasalviaBelum ada peringkat
- InmunobiologíaDokumen37 halamanInmunobiologíaSoledad Lagunes CastroBelum ada peringkat
- IMS - Intro To Immunology and SerologyDokumen3 halamanIMS - Intro To Immunology and SerologyJeanne RodiñoBelum ada peringkat
- Toll-Like Receptors and Innate ImmunityDokumen14 halamanToll-Like Receptors and Innate ImmunityJUAREZ GONZALEZ EDWARD HASSANBelum ada peringkat
- 13 Enfermedad Inflamatoria IntestinalDokumen54 halaman13 Enfermedad Inflamatoria IntestinalKaren GomezBelum ada peringkat
- TLR y DolorDokumen35 halamanTLR y Doloremanuel santiago camargo parraBelum ada peringkat
- Innate Immune Functions of Astrocytes Are Dependent Upon Tumor Necrosis Factor-AlphaDokumen15 halamanInnate Immune Functions of Astrocytes Are Dependent Upon Tumor Necrosis Factor-AlphaCony GSBelum ada peringkat
- Producing Macrophages T Cells and IL-10 Immunological Priming Requires RegulatoryDokumen15 halamanProducing Macrophages T Cells and IL-10 Immunological Priming Requires RegulatoryLaurenceBelum ada peringkat
- Coatings: Biomedical Nanoparticles: Overview of Their Surface Immune-CompatibilityDokumen21 halamanCoatings: Biomedical Nanoparticles: Overview of Their Surface Immune-CompatibilityDora PopescuBelum ada peringkat
- Basic Immunology 5th Abbas Test BankDokumen9 halamanBasic Immunology 5th Abbas Test BankRamiqqBelum ada peringkat
- Interplay of Strain and Race/ethnicity in The Innate Immune Response To M. TuberculosisDokumen16 halamanInterplay of Strain and Race/ethnicity in The Innate Immune Response To M. TuberculosisGustavo Alejandro CastroBelum ada peringkat
- Self Peptidome Variation Shapes Individual ImmuneDokumen7 halamanSelf Peptidome Variation Shapes Individual ImmuneannavictoriaaltierivanniBelum ada peringkat
- Comprehensive Database On Toll Like Receptors: LiteratureDokumen6 halamanComprehensive Database On Toll Like Receptors: Literaturepatialokkumar4465Belum ada peringkat
- In Silico Leishmania Major in VitroDokumen13 halamanIn Silico Leishmania Major in VitroshahabBelum ada peringkat
- Veterinary Immunology and ImmunopathologyDokumen6 halamanVeterinary Immunology and ImmunopathologyCristhian Felipe Salinas GuerreroBelum ada peringkat
- Associaçao TNF MBL VDR HanseníaseDokumen17 halamanAssociaçao TNF MBL VDR HanseníaseevaldoamaralBelum ada peringkat
- Disseminated Molluscum Contagiosum in A HIV-positive Child. Improvement After Therapy With 5% ImiquimodDokumen5 halamanDisseminated Molluscum Contagiosum in A HIV-positive Child. Improvement After Therapy With 5% ImiquimodBenor Amri MustaqimBelum ada peringkat
- 2015 Pocket Guide CDC ITSDokumen24 halaman2015 Pocket Guide CDC ITSfelix camposBelum ada peringkat
- Forbat 2017 Molluscum Contagiosum Review and UpdateDokumen12 halamanForbat 2017 Molluscum Contagiosum Review and UpdateBenor Amri MustaqimBelum ada peringkat
- Case Controls Studies Lancet PDFDokumen4 halamanCase Controls Studies Lancet PDFAhira Susana Mendoza de RiveraBelum ada peringkat
- 4 Bias and Causal Associations in Observational Research Grimes2002 PDFDokumen5 halaman4 Bias and Causal Associations in Observational Research Grimes2002 PDFBenor Amri MustaqimBelum ada peringkat
- GlossaryDokumen5 halamanGlossaryBenor Amri MustaqimBelum ada peringkat
- Dermatoses of Pregnancy TabulasiDokumen3 halamanDermatoses of Pregnancy TabulasiBenor Amri MustaqimBelum ada peringkat
- New Concepts in Understanding Genital Herpes2Dokumen12 halamanNew Concepts in Understanding Genital Herpes2Benor Amri MustaqimBelum ada peringkat
- Bacterial Skin and Soft Tissue Infections: Review of The Epidemiology, Microbiology, Aetiopathogenesis and TreatmentDokumen11 halamanBacterial Skin and Soft Tissue Infections: Review of The Epidemiology, Microbiology, Aetiopathogenesis and TreatmentBenor Amri Mustaqim100% (1)
- Topical Imiquimod Treatment of Aciclovir-Resistant PDFDokumen5 halamanTopical Imiquimod Treatment of Aciclovir-Resistant PDFBenor Amri MustaqimBelum ada peringkat
- Single-Day, Patient-Initiated Famciclovir PDFDokumen9 halamanSingle-Day, Patient-Initiated Famciclovir PDFBenor Amri MustaqimBelum ada peringkat
- Hansen's Disease (Leprosy) Current and FutureDokumen11 halamanHansen's Disease (Leprosy) Current and FutureBenor Amri MustaqimBelum ada peringkat
- Radiation Physics and Chemistry: Emilie Brun, Cécile Sicard-RoselliDokumen9 halamanRadiation Physics and Chemistry: Emilie Brun, Cécile Sicard-RoselliDavide MessinaBelum ada peringkat
- Family Neisseriaceae: Joy P. Calayo, RMT, MSMT UST Faculty of Pharmacy Dept. of Medical TechnologyDokumen18 halamanFamily Neisseriaceae: Joy P. Calayo, RMT, MSMT UST Faculty of Pharmacy Dept. of Medical Technologypixholic100% (1)
- What Is Muscle Dystrophy?Dokumen4 halamanWhat Is Muscle Dystrophy?Ryan GoldsteinBelum ada peringkat
- Diabetik Keto AsDokumen162 halamanDiabetik Keto AsayudilaBelum ada peringkat
- Multiple AllelesDokumen31 halamanMultiple AllelesJENNIFER DAVIDBelum ada peringkat
- Hormones: Target CellsDokumen2 halamanHormones: Target CellsLarasBelum ada peringkat
- Rsemue Video IsiDokumen5 halamanRsemue Video IsiPuvaan RaajBelum ada peringkat
- Recurrent Aphthous Stomatitis e Etiology, Serum Autoantibodies, Anemia, Hematinic Deficiencies, and ManagementDokumen11 halamanRecurrent Aphthous Stomatitis e Etiology, Serum Autoantibodies, Anemia, Hematinic Deficiencies, and ManagementorizaBelum ada peringkat
- DocumentDokumen15 halamanDocumentJennifer BanteBelum ada peringkat
- 2011 Diagnosis and Treatment in ProsthodonticsDokumen353 halaman2011 Diagnosis and Treatment in ProsthodonticsAnonymous 0pg1qSpO100% (1)
- Mutations in SLC26A1 Cause Nephrolithiasis: Table S1Dokumen7 halamanMutations in SLC26A1 Cause Nephrolithiasis: Table S1Johnny GoteBelum ada peringkat
- Tongue Diseases NDokumen46 halamanTongue Diseases NhazeemmegahedBelum ada peringkat
- Antiviral DrugsDokumen56 halamanAntiviral DrugsciccianoBelum ada peringkat
- Premature Rupture of MembranesDokumen3 halamanPremature Rupture of MembranesSheena Kunkel100% (2)
- Using Knockout and Transgenic Mice To Study Physiology and BehaviorDokumen34 halamanUsing Knockout and Transgenic Mice To Study Physiology and Behaviorgülsüm önalBelum ada peringkat
- Burnout Among NursesDokumen6 halamanBurnout Among NursesYousef KhalifaBelum ada peringkat
- Concept of Health Disease and PreventionDokumen33 halamanConcept of Health Disease and PreventionitdocBelum ada peringkat
- Benign Diseases of Cervix, Uterus & OvaryDokumen58 halamanBenign Diseases of Cervix, Uterus & OvaryFaheem HassanBelum ada peringkat
- GS2011Dokumen29 halamanGS2011Priya MehtaBelum ada peringkat
- An Effective Solution To Optimise Health Status and Nutrient Utilisation - GUSTOR AQUADokumen5 halamanAn Effective Solution To Optimise Health Status and Nutrient Utilisation - GUSTOR AQUAInternational Aquafeed magazineBelum ada peringkat
- ICMR Ethical Guidelines (India)Dokumen77 halamanICMR Ethical Guidelines (India)api-3836189100% (2)
- The Kidneys The Functions of The KidneyDokumen5 halamanThe Kidneys The Functions of The KidneylaraBelum ada peringkat
- Clinical Manifestation in Sickle Cell Anemia: A Study in Chhattisgarh Institute of Medical Sciences (CIMS) Bilaspur, Chhattisgarh, India.Dokumen4 halamanClinical Manifestation in Sickle Cell Anemia: A Study in Chhattisgarh Institute of Medical Sciences (CIMS) Bilaspur, Chhattisgarh, India.IOSRjournalBelum ada peringkat
- Thyroid Gland Review of SystemsDokumen3 halamanThyroid Gland Review of Systemssyderman999Belum ada peringkat
- A Review of Lung Cancer Research in MalaysiaDokumen9 halamanA Review of Lung Cancer Research in MalaysiaCahrun CarterBelum ada peringkat
- Seminar On Protein and Peptides Drug DeliveryDokumen37 halamanSeminar On Protein and Peptides Drug DeliverykeyurBelum ada peringkat
- Leukemia Thesis PDFDokumen5 halamanLeukemia Thesis PDFjpwvbhiig100% (2)
- Bone TissueDokumen66 halamanBone TissueFunikawati Baldiyah100% (1)
- ISBB Wall Notes PDFDokumen8 halamanISBB Wall Notes PDFLynx EemanBelum ada peringkat
- The Age of Magical Overthinking: Notes on Modern IrrationalityDari EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityPenilaian: 4 dari 5 bintang4/5 (29)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDari EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDPenilaian: 5 dari 5 bintang5/5 (2)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDari EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsBelum ada peringkat
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDari EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionPenilaian: 4 dari 5 bintang4/5 (404)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDari EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedPenilaian: 5 dari 5 bintang5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDari EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsPenilaian: 3.5 dari 5 bintang3.5/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDari EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsPenilaian: 4.5 dari 5 bintang4.5/5 (170)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Dari EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Belum ada peringkat
- The Obesity Code: Unlocking the Secrets of Weight LossDari EverandThe Obesity Code: Unlocking the Secrets of Weight LossPenilaian: 4 dari 5 bintang4/5 (6)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDari EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsPenilaian: 5 dari 5 bintang5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDari EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BePenilaian: 2 dari 5 bintang2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDari EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisPenilaian: 4.5 dari 5 bintang4.5/5 (42)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDari EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessPenilaian: 4.5 dari 5 bintang4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDari EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisPenilaian: 4 dari 5 bintang4/5 (1)
- The Comfort of Crows: A Backyard YearDari EverandThe Comfort of Crows: A Backyard YearPenilaian: 4.5 dari 5 bintang4.5/5 (23)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDari EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityPenilaian: 4 dari 5 bintang4/5 (5)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Dari EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Penilaian: 4.5 dari 5 bintang4.5/5 (110)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDari EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisPenilaian: 5 dari 5 bintang5/5 (8)
- To Explain the World: The Discovery of Modern ScienceDari EverandTo Explain the World: The Discovery of Modern SciencePenilaian: 3.5 dari 5 bintang3.5/5 (51)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDari EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisPenilaian: 3.5 dari 5 bintang3.5/5 (2)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDari EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Marshmallow Test: Mastering Self-ControlDari EverandThe Marshmallow Test: Mastering Self-ControlPenilaian: 4.5 dari 5 bintang4.5/5 (58)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDari EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryPenilaian: 4 dari 5 bintang4/5 (45)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDari EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifePenilaian: 4.5 dari 5 bintang4.5/5 (253)