Arterioles Summary
Diunggah oleh
Nancy YouDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Arterioles Summary
Diunggah oleh
Nancy YouHak Cipta:
Format Tersedia
ARTERIOLES
When an artery reaches the organ it is supplying, it branches into
numerous arterioles within the organ.
Explain how arteriolar radius can change and what impact this
would have on blood flow
- Arterioles are the major resistance vessel in the vascular tree
because their radius is small enough to offer considerable resistance to
flow.
- Blood flow from the artery to the arterioles (a drop in mean pressure)
helps establish the pressure differential that encourages the flow of
blood from the heart to the various organs downstream.
- The radius can be adjusted independently to accomplish two
functions: 1) to variably distribute the cardiac output among the
systemic organs, depending on the bodys momentary needs; and 2)
help regulate arterial blood pressure
- A smaller radius increases surface area that comes in contact with
blood
- Decreasing radius by results in a 16-fold increase in resistance
Discuss the local chemical and physical influences on arteriolar
radius
- Arteriolar walls contain very little elastic connective tissue; however,
they do have a thick later of smooth muscle that is innervated by
sympathetic nerve fibres
- The smooth muscle is sensitive to many local chemical changes and
to a few circulating hormones
- When the smooth muscle layer contracts, the vessels circumference
becomes smaller, increasing resistance and decreasing flow through
that vessel
Vasoconstriction: the narrowing of a vessel
Increased resistance
Decreased flow through vessel
Can be caused by
o Increased myogenic activity
o Increased oxygen
o Decreased CO2 and other metabolites
o Increased Endothelin
o Increased sympathetic stimulation, vasopressin, cold
Vasodilation: the enlargement in circumference and radius of vessel
Describe the sympathetic and parasympathetic control of
arteriolar radius
Arteriolar smooth muscle normally displays a state of partial
constriction known as vascular tone, which establishes a base line of
arteriolar resistance
- Two factors responsible for vascular tone a
o Arteriolar smooth muscle has considerable myogenic
activity; that is, its membrane potential fluctuates
independent of any neural or hormonal influences, leading
to self-induced contractile activity
o The sympathetic fibres supplying most arterioles
continually release norepinephrine, which further enhance
vascular tone
The ongoing tonic activity makes it possible to either increase or
decrease the level of contractile ability to accomplish vasoconstriction
or vasodilation. Were it not for tone, it would be impossible to reduce
the tension in an arteriolar wall to accomplish vasodilation; only
varying degrees of vasoconstriction would be possible
Discuss the interaction with local chemical control and
hormonal control of arteriolar radius
- Because blood is delivered to all organs at the same mean
arterial pressure, the driving force for flow is identical for each
organ. (total peripheral resistance/TPR is the summation of all
resistance vessels)
- Differences in flow to various organs are completely determined
by differences in the extent of vascularization and by
differences in resistance offered by the arterioles
supplying each organ.
Factors can influence
of contractile activity fall
into two categories:
1) Local (intrinsic) control,
are changes within an
organ that alter the radius
of the vessel and adjust
the blood flow by directly
affecting the smooth
muscles of the organs
arterioles (important in
determining the
distribution of cardiac
output)
levels
Local chemical influences: (are related to metabolic changes within a
given organ)
- Metabolic change (following factors produce relaxation of
arteriolar smooth muscles active hyperaemia)
o Decreased oxygen
o Decreased ATP
o Increase CO2
o Increased acid
o Increased K+
o Increased osmolality
o Adenosine and prostaglandin release
- Vasoactive mediators
o Endothelial cells, a single layer of specialized epithelial
cells that line the lumen of all blood vessel, release
chemical mediators that play a key role in locally
regulating arteriolar caliber
o Endothelial cells release locally acting chemical
messengers in response to chemical changes in their
environment
o Among best studied local vasoactive mediator is nitric
oxide (NO), which causes local arteriolar vasodilation by
inducing relaxation of arteriolar smooth muscle in the
vicinity
Histamine release
o Is synthesized and stores within special connective tissue
cells in many organs and in certain types of circulating
white blood cells
o When organs are injured, histamine is release and acts as a
paracrine in the damaged region
o By promoting relation or arteriolar smooth muscles,
histamine is the major cause of vasodilation in an injured
area.
Local physical influences:
Local
application of
heat or cold
o o
Can
cause localized
arteriolar
vasodilation
Chemical response to shear stress
o Because of friction, blood flowing over the surface of the
vessel lining creates a longitudinal force known as sheer
stress on the endothelial cells. Increase in sheer stress
causes the endothelial cells to release nitric oxide, which
diffuses to the underlying smooth muscle and promotes
vasodilation.
Myogenic response to stretch
o Arteriolar smooth muscle responds to being passively
stretched by myogenically increasing its tone via
vasoconstriction, thereby acting to resist the initial passive
stretch.
o Myogenic responses, coupled with metabolically induced
responses, are important in reactive hyperaemia and auto
regulation.
HYPEREMIA
AUTO-REGULATION
- Local mechanisms that keep tissue blood flow fairly constant
despite rather wide deviations in mean arterial driving pressure
- When mean arterial pressure falls, the driving force is reduced,
so blood flow to organs decrease
- The resultant changes in local metabolites and the reduces
stretch in the arterioles collectively brings about arteriolar
dilation to help restore tissue blood flow to normal despite the
reduced driving pressure
2) Extrinsic control, which are important in blood pressure regulation
Influence of total peripheral resistance
- To find the effect of changes in arteriolar resistance on mean
arterial pressure, the formula F = change in P / R applies to the
entire circulation as well as to a single vessel
Norepinephrines influence on smooth muscle
- The norepinephrine released from sympathetic nerve endings
combines with a-adrenergic receptors on arteriolar smooth
muscle to bring about vasoconstriction.
- Except cerebral arterioles, because brain blood flow must remain
constant to meet the brains continual need for oxygen
- Sympathetic activity contributes in an important way to
maintaining mean arterial pressure, ensuring an adequate
driving force for blood flow to the brain at the expense of organs
that can better withstand reduced blood flow
- Other organs that really need additional blood, such as active
muscles, obtain it thought local controls that override the
sympathetic effect
Local controls override sympathetic vasoconstriction
- Skeletal and cardiac muscles have the most powerful local
control mechanisms with which to override generalized
sympathetic vasoconstriction.
No parasympathetic innervation to arterioles
- There is no significant parasympathetic innervation to arterioles,
with the exception of the abundant parasympathetic vasodilator
supply to the arterioles of the penis and clitoris
- The rapid, profuse vasodilation induced by parasympathetic
stimulation in these organs (by means of promoting release of
NO) is largely responsible for accomplishing erection
- Decreasing sympathetic vasoconstrictor activity below tonic level
elsewhere produces vasodilation. When mean pressure rising
above normal, reflex reduction in sympathetic vasoconstrictor
activity accomplishes generalized arteriolar vasodilation to help
bring the driving pressure down to normal
- The main region of the brain that adjust sympathetic output to the
arterioles is the cardiovascular control center in the medulla of the
brain stem.
- Several hormones also extrinsically influence arteriolar radius
- Epinephrine and norepinephrine, which generally reinforce the
sympathetic nervous system
Vasopressin and angiotensin II, which are important in controlling
fluid balance and are potent vasoconstrictors
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Renal NursinglDokumen36 halamanRenal NursinglgireeshsachinBelum ada peringkat
- Subdivisions of Lung Volumes and Gas ExchangeDokumen4 halamanSubdivisions of Lung Volumes and Gas ExchangeNancy YouBelum ada peringkat
- Blood Pressure SummaryDokumen7 halamanBlood Pressure SummaryNancy You100% (1)
- Arteries SummaryDokumen4 halamanArteries SummaryNancy YouBelum ada peringkat
- Grass IntroDokumen1 halamanGrass IntroNancy YouBelum ada peringkat
- Chapter 6-10 QuestionsDokumen3 halamanChapter 6-10 QuestionsNancy YouBelum ada peringkat
- Bahasa Inggris Kel.12Dokumen10 halamanBahasa Inggris Kel.12Egi Satya FralazendaBelum ada peringkat
- Rubber Band Ligation: of HaemorrhoidsDokumen1 halamanRubber Band Ligation: of HaemorrhoidsdbedadaBelum ada peringkat
- Khushboo PPT Covid 19Dokumen17 halamanKhushboo PPT Covid 19Birlal SinghBelum ada peringkat
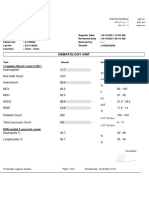
- Hematology Unit: Complete Blood Count (CBC)Dokumen2 halamanHematology Unit: Complete Blood Count (CBC)Rasha ElbannaBelum ada peringkat
- Glass Prescription - SutrishnaDokumen15 halamanGlass Prescription - SutrishnaSutrishna PramanikBelum ada peringkat
- Uts 4Dokumen16 halamanUts 4raine zapantaBelum ada peringkat
- Clinical Manual - Part 2 - Drug Infusion Guidelines Revised - July 2015 - V7.11Dokumen58 halamanClinical Manual - Part 2 - Drug Infusion Guidelines Revised - July 2015 - V7.11Jayaprakash KuppusamyBelum ada peringkat
- Test Bank For Physical Examination and Health Assessment 1st Canadian Edition by JarvisDokumen10 halamanTest Bank For Physical Examination and Health Assessment 1st Canadian Edition by JarvisThomas White100% (22)
- Women S Health MidtermDokumen30 halamanWomen S Health MidtermKatarzyna CiesielskaBelum ada peringkat
- Medical Image Analysis - Overview - NewDokumen11 halamanMedical Image Analysis - Overview - Newedi pBelum ada peringkat
- Checklist - Assisting - Circulating DeliveryDokumen2 halamanChecklist - Assisting - Circulating DeliveryLue Vigiem M. GuiasBelum ada peringkat
- EMS Airflow BrochureDokumen2 halamanEMS Airflow BrochureMELHEM_J8008Belum ada peringkat
- Standard Operating Procedure (Biochemistry - Diasys RESPONS - 910)Dokumen17 halamanStandard Operating Procedure (Biochemistry - Diasys RESPONS - 910)Aniruddha ChatterjeeBelum ada peringkat
- Care of The Ventilated ChildDokumen5 halamanCare of The Ventilated ChildBrahadheeswaran KannanBelum ada peringkat
- Schizophrenia and Other Psychotic DisordersDokumen85 halamanSchizophrenia and Other Psychotic DisordersEsraRamosBelum ada peringkat
- Hema - Guide Notes PDFDokumen21 halamanHema - Guide Notes PDFVanessa Ladra100% (1)
- Therapeutic Management of Clinical Mastitis in Goat: A Case StudyDokumen5 halamanTherapeutic Management of Clinical Mastitis in Goat: A Case StudyIJAR JOURNALBelum ada peringkat
- Daftar Pustaka Refrat Koas HoreDokumen4 halamanDaftar Pustaka Refrat Koas HoreShinta Amalia KartikaBelum ada peringkat
- Perineal Techniques During The Second Stage of Labour For Reducing Perineal Trauma (Review)Dokumen118 halamanPerineal Techniques During The Second Stage of Labour For Reducing Perineal Trauma (Review)Ppds ObgynBelum ada peringkat
- Polio VaccineDokumen10 halamanPolio VaccineLiiaa SiiNouunaa JupheeBelum ada peringkat
- Icd 10Dokumen3 halamanIcd 10ghinaBelum ada peringkat
- ENDO Buku Ekatalog Disposable Fix PDFDokumen12 halamanENDO Buku Ekatalog Disposable Fix PDFHanggar PutraBelum ada peringkat
- A Leading Surgical Gastroenterologist in Hyderabad Dr. Dinesh ReddyDokumen4 halamanA Leading Surgical Gastroenterologist in Hyderabad Dr. Dinesh Reddydrdineshreddy02Belum ada peringkat
- HEPATOMEGALY CaseDokumen5 halamanHEPATOMEGALY CaseKanwaljeet SinghBelum ada peringkat
- Fre Orto 3Dokumen4 halamanFre Orto 3PutriBelum ada peringkat
- Final PPT SiDokumen38 halamanFinal PPT SiSaad IqbalBelum ada peringkat
- Australian and New Zealand College of Veterinary Scientists: Fellowship ExaminationDokumen11 halamanAustralian and New Zealand College of Veterinary Scientists: Fellowship Examinationabazanhasan6705Belum ada peringkat
- 4 - St. Mary's - December 2020 AdmissionDokumen100 halaman4 - St. Mary's - December 2020 AdmissionprashantBelum ada peringkat
- Nursing Care Plan For LEUKEMIASDokumen12 halamanNursing Care Plan For LEUKEMIASMaverick LimBelum ada peringkat