Endoscopic Cauterization of The Sphenopalatine Artery in
Diunggah oleh
ritno09Deskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Endoscopic Cauterization of The Sphenopalatine Artery in
Diunggah oleh
ritno09Hak Cipta:
Format Tersedia
ORIGINAL ARTICLE
Endoscopic Cauterization of the Sphenopalatine Artery in
Persistent Epistaxis
S Harvinder, MMed (ORL-HNS, S Rosalind, MMed (ORL-HNS, S Gurdeep, MS (HNORL)
Department of ENT, Hospital Ipoh, Jalan Hospital, 30990, Ipoh, Perak, Malaysia
SUMMARY
The management of epistaxis remains to be a challenging
problem for most ENT surgeon especially posterior epistaxis.
Most cases are managed by placement of posterior nasal
packs or balloons and failure leads to more invasive
techniques, involving ligation of the internal maxillary
artery. The above management is associated with significant
patient complication and morbidity. Endoscopic ligation or
cauterization of the sphenopalatine artery has emerged as a
viable and minimally invasive alternative. We have
performed endoscopic cauterization of nine sphenopalatine
arteries in eight patients with no further episodes of
epistaxis and complications, with an average follow-up of 25
months. The mean age of the patients was 52.75 years. Fifty
percent of the patients had a history of hypertension.
KEY WORDS:
Endoscopic, Epistaxis, Sphenopalatine artery
INTRODUCTION
Epistaxis continues to be one of the most common and
intriguing emergencies presenting to the ENT surgeon.
Usually, the posterior epistaxis provides a challenging
management problem as compared to the trivial bleeding
from the Littles area. Placement of posterior nasal packs
and/or balloons has been the first line of management. These
packs often cause considerable discomfort and may cause
mucosal trauma and necrosis. In the elderly, there is
significant increased risk of obstruction of the nasal airway
causing hypoxia, cardiac arrhythmias, or even death1,2.
Patients that continue to bleed despite conservative methods
are then subjected to more invasive techniques3. The internal
maxillary artery is usually ligated through the Caldwell- Luc
approach3. Sometimes ligation of the external carotid artery
in the neck is necessary3. The Caldwell-Luc approach has also
been associated with significant patient morbidity4.
With the advent of the rigid endoscopes for the treatment of
nasal and sinus disease, the expanded role has developed to
encompass cauterization and ligation of the sphenopalatine
artery. Endoscopic cauterization of the sphenopalatine artery
causes interruption of the nasal vasculature at a point distal
enough to prevent direct, retrograde and anastomotic blood
flow from ipsilateral and contralateral carotid systems5.
MATERIALS AND METHODS
Between May 2005 and July 2006, eight consecutive patients
(5 male and 3 females) with posterior epistaxis have
undergone endoscopic cauterization of nine sphenopalatine
arteries (4 right, 3 left and one bilateral) under the care of the
main author. The mean age of patients was 52.75 years (range
26-73). All patients with suspected posterior epistaxis were
initially managed with placement of a 10 mL balloon catheter
in the posterior nasal space and a Merocel pack anteriorly.
The patient is then admitted to the ward for observation. In
the ward, routine blood examination was carried out for
platelet count and coagulation profile. The next day, the
packs were removed and endoscopy performed to confirm the
site of bleeding. Once a posterior bleed is confirmed,
endoscopic cauterization of the sphenopalatine artery is
performed as an emergency procedure.
Surgical Technique
Acute haemorrhage in uncontrolled epistaxis is managed
initially by injecting the pterygopalatine fossa through the
greater palatine foramen in the roof of the hard palate with
1mL of 1:100,000 adrenaline and 2% xylocaine. Once the
patient is under general anaesthesia, the initial 10 mL balloon
catheter which was placed in the posterior nasal space and a
Merocel pack anteriorly is removed. Five neuropathies soaked
in 2 mL 5% cocaine are placed in the affected nasal cavity.
Once the bleeding is controlled and with adequate nasal
decongestion, the area of the sphenopalatine foramen is
inspected. A further 0.5 mL of 1:100,000 adrenaline and 2%
Xylocaine is then injected in these area.
The important landmark to be identified is the junction
between the membranous posterior fontanelle of the
maxillary sinus and the lateral nasal wall. An incision is
made from the under surface of the horizontal portion of the
ground lamella of the middle turbinate to the insertion of the
inferior turbinate on the lateral basal wall. The flap is
elevated with a suction Freers. This flap is elevated
posteriorly, in the lower half of the mucosal incision until the
anterior face of the sphenoid is identified. Once this
landmark is identified the dissection is directed superiorly
until the mucosa tents around the region of the
sphenopalatine foramen. Here the neurovascular bundle will
emerge.
Further gentle dissection in this area is done until the artery
is identified. This artery is then diathermied with a bipolar
cautery. The flap is then returned and a small piece of
This article was accepted: 18 January 2008
Corresponding Author: Harvinder Singh, Consultant ENT Surgeon, Ipoh Hospital, 30990, Ipoh, Perak
Email: harvindersran@hotmail.com
Med J Malaysia Vol 63 No 5 December 2008
377
Original Article
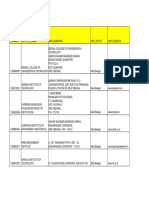
Table I: Indications, Medical History and Follow-up
1
Age
52
Sex
F
45
27
69
73
58
62
26
Cause
Recurrent
Epistaxis
Spontaneous
Epistaxis
Recurrent
Epistaxis
Spontaneous
Epistaxis
Spontaneous
Epistaxis
Spontaneous
Epistaxis
Spontaneous
Epistaxis
Spontaneous
Epistaxis
Medical History
NPC
HPT
HPT
Follow-up (months)
33
Recurrence
None
30
None
Nil
28
None
Nil
25
None
HPT/DM
24
None
Nil
21
None
HPT/DM
20
None
Nil
19
None
HPT, hypertension; DM, diabetes mellitus; NPC, nasopharyngeal carcinoma.
surgicel is placed overlying this area. No intranasal packing is
inserted. Patients are discharged the next day with antibiotics
and oxymethazoline nasal sprays. Further review is done in
the out-patient clinics.
popular approach to deal with posterior refractory epistaxis.
The transnasal approach is more direct and feasible as
compared to the trans-antral approach. It allows direct entry
into the sphenopalatine fossa where the sphenopalatine
artery can be easily identified.
RESULTS
The results are summarized in Table I. In all patients, their
platelet counts and coagulation profile was normal. The
average length of the procedure was 54.44 minutes. All
patients were discharged the next day. In every case, no intra
or post-operative complications were recorded in particular
intracranial or intraorbital sequelae. Minor complications
like numbness of the teeth, palate and upper lip was also
absent. All patients have subsequently been followed up on
average of 25 months with no further episodes of epistaxis.
Four patients (50%) were hypertensives with associated NPC
(one) and diabetes (two). The rest of the patients had
unremarkable medical history.
Sharp et al5 reported a series of ten consecutive patients that
had undergone endoscopic ligation of 11 sphenopalatine
arteries over a 26 month period. No patient has had further
epistaxis requiring medical attention. Wormald et al7 has also
reported a high success rate of 92% in patients with refractory
posterior epistaxis treated with endoscopic ligation of the
sphenopalatine arteries using Ligar clips.
DISCUSSION
Traditional methods of arterial ligation like the trans-antral
approach causes significant morbidity. The trans-antral
approach to the internal maxillary artery (IMA) via the
posterior wall of the maxillary sinus is also known by the
Caldwell-Luc approach. Reported morbidity includes dental
injury, infraorbital nerve damage, oro-antral fistula, blindness
and ophthalmoplegia6. This procedure is also associated with
a failure rate of as high as 40%4,5. The most common cause for
the failure to ligate or cauterize the IMA was due to the
surgeons inability to identify the IMA or its terminal
branches in the pterygomaxillary fossa. Additionally, surgical
clips were not correctly placed in 13% of cases4.
The endoscopic approach is a non-invasive technique, with
easy access transnasally to the sphenopalatine foramen. It
also offers considerable reduction in surgical and anaesthetic
time as compared with the more traditional approaches
hence reducing surgical morbidity and failure rates. This also
avoids the necessity to pack the nose for several days. This
improves patients comfort and need for prolonged
hospitalization. As a conclusion, endoscopic cauterization of
the sphenopalatine artery is a safe and cost effective
technique in the management of posterior epistaxis.
REFERENCES
1.
2.
3.
4.
5.
The sphenopalatine artery is the terminal branch of the
internal maxillary artery. Endoscopic cauterization of the
sphenopalatine artery causes interruption of the nasal
vasculature at a point distal enough to prevent direct,
retrograde and anastomotic blood flow from ipsilateral and
contralateral carotid systems5. It is due to this fact that
endoscopic cauterization of this artery has become a more
378
6.
7.
Elwany S, Kamel T, Mekhamer A. Pneumatic nasal catheters: advantages
and drawbacks. J Laryngol Otol. 1986; 100: 641-47.
Jacobs JR, Dickson CB. Effects of nasal and laryngeal stimulation upon
peripheral lung function. Otol Head Neck Surg. 1986; 95: 298-303.
Pritikin JB, Caldarelli DD, Panke WR. Endoscopic ligation of the internal
maxillary artery for treatment of intractable posterior epistaxis. Ann Otol
Rhinol Laryngol. 1998; 107: 85-91.
Metson R, Lane R. Internal maxillary artery ligation for epistaxis: an
analysis of failures. Laryngoscope. 1988; 98: 760-64.
Sharp HR, Rowe-Jones JM, Biring GS, Mackay IS. Endoscopic ligation or
diathermy of the sphenopalatine artery in persistent epistaxis. J Laryngol
Otol. 1997; 111: 1047-50.
Strong EB, Bell DA, Johnson LP, Jacobs JM. Intractable epistaxis:
Transantral ligation vs. embolization: efficacy review and cost analysis.
Otol Head Neck Surg. 1995; 113: 674-78.
Wormald PJ, Wee DT, van Hasselt CA. Endoscopic ligation of the
sphenopalatine artery for refractory posterior epistaxis. Am J Rhinol. 2000;
14: 261-64.
Med J Malaysia Vol 63 No 5 December 2008
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Evolution Army 3 R DadDokumen341 halamanEvolution Army 3 R DadStanisław DisęBelum ada peringkat
- Aluminum PorterDokumen2 halamanAluminum PorterAmir ShameemBelum ada peringkat
- 2016 Closing The Gap ReportDokumen64 halaman2016 Closing The Gap ReportAllan ClarkeBelum ada peringkat
- Continue Practice Exam Test Questions Part 1 of The SeriesDokumen7 halamanContinue Practice Exam Test Questions Part 1 of The SeriesKenn Earl Bringino VillanuevaBelum ada peringkat
- Presentation About GyroscopesDokumen24 halamanPresentation About GyroscopesgeenjunkmailBelum ada peringkat
- Aleutia Solar Container ClassroomDokumen67 halamanAleutia Solar Container ClassroomaleutiaBelum ada peringkat
- EqualLogic Release and Support Policy v25Dokumen7 halamanEqualLogic Release and Support Policy v25du2efsBelum ada peringkat
- IEC TC 56 Dependability PDFDokumen8 halamanIEC TC 56 Dependability PDFsaospieBelum ada peringkat
- Performance Task 1Dokumen3 halamanPerformance Task 1Jellie May RomeroBelum ada peringkat
- WBDokumen59 halamanWBsahil.singhBelum ada peringkat
- Cummin C1100 Fuel System Flow DiagramDokumen8 halamanCummin C1100 Fuel System Flow DiagramDaniel KrismantoroBelum ada peringkat
- ELEVATOR DOOR - pdf1Dokumen10 halamanELEVATOR DOOR - pdf1vigneshBelum ada peringkat
- WAQF Podium Design Presentation 16 April 2018Dokumen23 halamanWAQF Podium Design Presentation 16 April 2018hoodqy99Belum ada peringkat
- Implementation of E-Governance To Improve The Civil Administration Service Quality in Public SectorDokumen11 halamanImplementation of E-Governance To Improve The Civil Administration Service Quality in Public SectorChristie YohanaBelum ada peringkat
- 2011-2012 - Medical - DirectoryDokumen112 halaman2011-2012 - Medical - DirectoryЈелена КошевићBelum ada peringkat
- Peer PressureDokumen13 halamanPeer PressuremightymarcBelum ada peringkat
- Eggermont 2019 ABRDokumen15 halamanEggermont 2019 ABRSujeet PathakBelum ada peringkat
- Fundamentals of Public Health ManagementDokumen3 halamanFundamentals of Public Health ManagementHPMA globalBelum ada peringkat
- Illustrating An Experiment, Outcome, Sample Space and EventDokumen9 halamanIllustrating An Experiment, Outcome, Sample Space and EventMarielle MunarBelum ada peringkat
- Teaching Profession - Educational PhilosophyDokumen23 halamanTeaching Profession - Educational PhilosophyRon louise PereyraBelum ada peringkat
- 16783Dokumen51 halaman16783uddinnadeemBelum ada peringkat
- CV Augusto Brasil Ocampo MedinaDokumen4 halamanCV Augusto Brasil Ocampo MedinaAugusto Brasil Ocampo MedinaBelum ada peringkat
- Disassembly Procedures: 1 DELL U2422HB - U2422HXBDokumen6 halamanDisassembly Procedures: 1 DELL U2422HB - U2422HXBIonela CristinaBelum ada peringkat
- NCP - Major Depressive DisorderDokumen7 halamanNCP - Major Depressive DisorderJaylord Verazon100% (1)
- Iguana Joe's Lawsuit - September 11, 2014Dokumen14 halamanIguana Joe's Lawsuit - September 11, 2014cindy_georgeBelum ada peringkat
- Catedral de SevillaDokumen28 halamanCatedral de SevillaAnonymous LkgNmKeBelum ada peringkat
- Drive LinesDokumen30 halamanDrive LinesRITESH ROHILLABelum ada peringkat
- UT Dallas Syllabus For Govt4396.002.08s Taught by Gregory Thielemann (Gregt)Dokumen2 halamanUT Dallas Syllabus For Govt4396.002.08s Taught by Gregory Thielemann (Gregt)UT Dallas Provost's Technology GroupBelum ada peringkat
- Bullshit System v0.5Dokumen40 halamanBullshit System v0.5ZolaniusBelum ada peringkat
- Where We Are in Place and Time "We Are Part of The Universe and Feel Compelled To Explore It."Dokumen1 halamanWhere We Are in Place and Time "We Are Part of The Universe and Feel Compelled To Explore It."Safia-umm Suhaim- FareedBelum ada peringkat