743 Full
Diunggah oleh
Hening Tri UtamiJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
743 Full
Diunggah oleh
Hening Tri UtamiHak Cipta:
Format Tersedia
Antisense Oligonucleotide Directed to Human Apolipoprotein B-100 Reduces
Lipoprotein(a) Levels and Oxidized Phospholipids on Human Apolipoprotein B-100
Particles in Lipoprotein(a) Transgenic Mice
Esther Merki, Mark J. Graham, Adam E. Mullick, Elizabeth R. Miller, Rosanne M. Crooke,
Robert E. Pitas, Joseph L. Witztum and Sotirios Tsimikas
Circulation. 2008;118:743-753; originally published online July 28, 2008;
doi: 10.1161/CIRCULATIONAHA.108.786822
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright 2008 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://circ.ahajournals.org/content/118/7/743
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial
Office. Once the online version of the published article for which permission is being requested is located,
click Request Permissions in the middle column of the Web page under Services. Further information about
this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/
Downloaded from http://circ.ahajournals.org/ by guest on January 7, 2013
Antisense Oligonucleotide Directed to Human
Apolipoprotein B-100 Reduces Lipoprotein(a) Levels and
Oxidized Phospholipids on Human Apolipoprotein B-100
Particles in Lipoprotein(a) Transgenic Mice
Esther Merki, PhD; Mark J. Graham, BS; Adam E. Mullick, PhD; Elizabeth R. Miller, BS;
Rosanne M. Crooke, PhD; Robert E. Pitas, PhD; Joseph L. Witztum, MD; Sotirios Tsimikas, MD
BackgroundLipoprotein (a) [Lp(a)] is a genetic cardiovascular risk factor that preferentially binds oxidized phospholipids (OxPL) in plasma. There is a lack of therapeutic agents that reduce plasma Lp(a) levels.
Methods and ResultsTransgenic mice overexpressing human apolipoprotein B-100 (h-apoB-100 [h-apoB mice]) or
h-apoB-100 plus human apo(a) to generate genuine Lp(a) particles [Lp(a) mice] were treated with the antisense
oligonucleotide mipomersen directed to h-apoB-100 mRNA or control antisense oligonucleotide for 11 weeks by
intraperitoneal injection. Mice were then followed up for an additional 10 weeks off therapy. Lp(a) levels [apo(a) bound
to apoB-100] and apo(a) levels [free apo(a) plus apo(a) bound to apoB-100] were measured by chemiluminescent
enzyme-linked immunoassay and commercial assays, respectively. The content of OxPL on h-apoB-100 particles
(OxPL/h-apoB) was measured by capturing h-apoB-100 in microtiter wells and detecting OxPL by antibody E06. As
expected, mipomersen significantly reduced plasma h-apoB-100 levels in both groups of mice. In Lp(a) mice,
mipomersen significantly reduced Lp(a) levels by 75% compared with baseline (P0.0001) but had no effect on
apo(a) levels or hepatic apo(a) mRNA expression. OxPL/h-apoB levels were much higher at baseline in Lp(a) mice
compared with h-ApoB mice (P0.0001) but decreased in a time-dependent fashion with mipomersen. There was no
effect of the control antisense oligonucleotide on lipoprotein levels or oxidative parameters.
ConclusionsMipomersen significantly reduced Lp(a) and OxPL/apoB levels in Lp(a) mice. The present study
demonstrates that h-apoB-100 is a limiting factor in Lp(a) particle synthesis in this Lp(a) transgenic model. If applicable
to humans, mipomersen may represent a novel therapeutic approach to reducing Lp(a) levels and their associated OxPL.
(Circulation. 2008;118:743-753.)
Key Words: antibodies arteriosclerosis atherosclerosis lipoproteins pharmacology
ipoprotein(a) [Lp(a)] is lipoprotein composed of apolipoprotein(a) [apo(a)], which is covalently bound to
low-density lipoprotein (LDL) via a single disulfide bond on
apoB-100.1,2 Unlike other apolipoproteins, apo(a) is carbohydrate rich and hydrophilic and therefore projects into the
aqueous phase when bound to apoB-100. Apo(a) is composed
of unique loop structures called kringles (K), which are each
stabilized by 3 disulfide bonds. The apo(a) gene encodes for
KIV, KV, and a protease-like domain that is catalytically
inactive. Apo(a) KIV is composed of 10 subtypes, of which
KIV-2 is present in a variable number of copies (from 3 to
40), resulting in markedly different apo(a) sizes among
individuals. Furthermore, most subjects (80%) have 2
distinct apo(a) alleles that also may vary significantly in size.
Apo(a) expression is restricted to humans and Old World
apes and monkeys, but an unrelated version containing only
KIII repeats is present in the European hedgehog. Lp(a) levels
are largely determined genetically, may vary by 1000-fold
(0.1 to 250 mg/dL), and are generally inversely associated with the size of the smaller apo(a) allele.
Clinical Perspective p 753
In clinical studies, Lp(a) is recognized as an independent
risk factor for myocardial infarction, stroke, and peripheral
arterial disease.3 As with most genetic risk factors that initiate
risk at birth, it is a stronger cardiovascular risk factor in
young patients with highly elevated Lp(a) levels and those
with additional atherogenic risk factors, particularly elevated
LDL cholesterol.4 6 Lp(a) has many potential atherogenic
properties resulting from its LDL moiety. Additionally,
Received April 16, 2008; accepted June 11, 2008.
From the University of California San Diego, La Jolla (E.M., E.R.M., J.L.W., S.T.), Gladstone Institute of Cardiovascular Disease, San Francisco
(R.E.P.), and Isis Pharmaceuticals, Inc, Carlsbad (M.J.G., A.E.M., R.M.C.), Calif.
Correspondence to Sotirios Tsimikas, Vascular Medicine Program, University of California San Diego, 9500 Gilman Dr, BSB 1080, La Jolla, CA
92093-0682. E-mail stsimikas@ucsd.edu
2008 American Heart Association, Inc.
Circulation is available at http://circ.ahajournals.org
DOI: 10.1161/CIRCULATIONAHA.108.786822
743
Downloaded from http://circ.ahajournals.org/
by guest on January 7, 2013
744
Circulation
August 12, 2008
apo(a) may confer proinflammatory, proatherogenic, and
prothrombotic properties, although most of these putative
atherogenic attributes have not been conclusively demonstrated in vivo or in humans.1
The pathophysiological role of Lp(a) and the underlying
mechanisms through which it contributes to cardiovascular
disease are unknown. One hypothesis suggests that apo(a)
promotes thrombosis by competitively inhibiting the conversion of plasminogen to plasmin. Although Lp(a) inhibits
thrombolysis in vitro,7 there is little evidence to support such
a role in vivo. We have recently proposed a novel hypothesis
that part of the atherogenicity of Lp(a) may be due to its
unique ability to strongly bind and transport proinflammatory
and proatherogenic oxidized phospholipids (OxPL). OxPL
present on apoB-100 (OxPL/apoB) can be measured by the
murine monoclonal antibody E06, which binds to the phosphocholine head group of OxPL but not native PL. This
observation is supported by experimental studies showing
that Lp(a) is the preferential carrier of PC-containing OxPL in
human plasma8 and by clinical studies showing a strong
correlation between plasma Lp(a) levels and OxPL/
apoB.6,9 16 However, differences exist between Lp(a) mass
and OxPL/apoB within different apo(a) isoform classes (K
repeats), with this correlation being weakest for the largest
isoforms and strongest for the lowest number of KIV repeats
(29 repeats, r0.66; 23 to 29 repeats, r0.88; and 22
repeats, r0.93; P0.001 each).15 In line with these data, a
mouse model overexpressing both human apoB-100 and
apo(a) [Lp(a) mice], to generate authentic Lp(a) particles at
very high plasma levels, was recently described and characterized.17 The Lp(a) particles in these mice carry most of the
E06-detectable OxPL in plasma, similar to Lp(a) particles in
humans.
ApoB-100 and apo(a) are expressed primarily in hepatocytes. Effective therapeutic modalities to reduce Lp(a) levels
in humans are lacking. Lp(a) levels can be lowered by niacin
by 15% to 30%, but niacin is associated with high rate of side
effects (severe flushing and glucose intolerance) that limit its
clinical use. The recent development of antisense oligonucleotides (ASOs) that can target a specific mRNA and suppress
the translation of its protein in the liver has opened up a novel
therapeutic window for reducing levels of atherogenic lipoproteins.18 Mipomersen (ISIS 301012), an antisense inhibitor directed to human apoB-100, was recently documented in
phase 2 clinical trials to lower plasma apoB-100 and LDL
cholesterol levels in humans.19
In the present study, we hypothesized that reducing available apoB-100 particles might also reduce Lp(a) levels in
Lp(a) mice. Furthermore, we also hypothesized that OxPL
levels on apoB-100 particles would be reduced in conjunction
with reductions in Lp(a) levels.
5-GCCTCAGTCTGCTTCGCACC-3, where the italicized bases are
2-MOEmodified ribonucleosides, and all cytosines are methylated at
the C5 position. It does not bind to murine apoB-100 mRNA. ISIS
141923 (5-CCTTCCCTGAAGGTTCCTCC-3), which is the same
chemical class as mipomersen but does not hybridize to either human or
mouse apoB-100 mRNA, was used as a control ASO.
Transgenic Mice
The generation of human apoB-100 transgenic mice (h-apoB mice),
which express only apoB-100 but not apoB-48, and apo(a) mice were
recently described.17 Briefly, wild-type h-apo(a) cDNA encoding
KIV-1, 1 copy of KIV-2, a fusion of KIV-3 and KIV-5, KIV-6 to
KIV-10, KV, and the protease-like domain was inserted into a liver
cDNA expression vector containing the apoE hepatic control region
(LE6). The 8.6-kb apo(a) expression vector [containing the apoE
promoter, ApoE intron 1, the apo(a) cDNA, and LE6] was excised
from pLIVha8 with SacII, purified, and microinjected into C57BL/
6xSJL zygotes.
To generate Lp(a) mice, hemizygous mice expressing apo(a) were
crossed with hemizygous mice expressing h-apoB-100.17 Lp(a) mice
were then mated with wild-type C57BL/6 mice to generate additional
Lp(a) mice. Mice were genotyped by polymerase chain reaction from
tail biopsies. DNA was isolated with the Qiagen DNeasy tissue kit.
Primers for apo(a) were 5 primer GACGGGAGACAGAGTGAAGC and 3 primer TACCTAAACCACGCCAGGAC. Primers
for apoB-100 transgene were 5 primer GAAGAACTTCCGGAGAGTTGCAAT and 3 primer CTCTTAGCCCCATTCAGCTCTGAC.
All mice were weaned at 28 days of age, housed in a barrier
facility with a 12-hour light/12-hour dark cycle, and fed normal
mouse chow containing 4.5% fat (Harlan Teklad, Madison, Wis).
Treatment Protocol
Three studies were performed in this set of experiments. In study 1,
the baseline values of the various lipoprotein and OxPL parameters
were determined in 8 h-apoB mice and 8 Lp(a) mice (Table 1). The
therapeutic experiments were then performed in studies 2 and 3;
study 2 was used to obtain data on the effects of mipomersen on
lipoprotein parameters and apo(a) liver mRNA expression, and study
3 was used to assess the effects of mipomersen on Lp(a) and OxPL
parameters in h-apoB mice and Lp(a) mice.
In study 2, 4 Lp(a) mice were treated for 4 weeks with twiceweekly intraperitoneal injections of mipomersen (25 mg/kg), and 4
Lp(a) mice were treated with control ASO 141923 (25 mg/kg IP).
Blood was collected at baseline and 2 and 4 weeks. After 4 weeks of
treatment, the mice were perfused with ice-cold PBS for 5 minutes,
and liver tissue was harvested. Plasma at each time point was used
for measurement of total cholesterol, triglycerides, Lp(a), and apo(a).
In study 3, h-apoB mice and Lp(a) mice 5 to 7 months of age on
normal mouse chow were administered either mipomersen (25
mg/kg IP) or control ASO 141923 (25 mg/kg IP) twice weekly for a
total of 11 weeks (6 mice in each group, 24 mice total). The
treatment was then stopped, and the mice were followed up for an
additional 10 weeks. Blood samples were collected at baseline, at 1
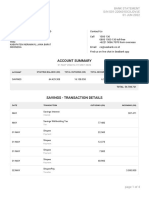
Table 1.
Baseline Levels of Lipid and Oxidation Variables
H-ApoB Mice
Lp(a) Mice
Total cholesterol, mg/dL
148.026.1
180.631.9
0.021
Triglycerides, mg/dL
157.155.3
145.034.7
0.59
Lp(a), mg/dL
NA
95.029.8
H-apoB-100, mg/dL
63.417.3
100.718.2
0.0002
Antisense Oligonucleotides
OxPL/h-apoB
0.060.02
3.280.08
0.0001
The ASOs used in this study were previously described in detail.19,20
Mipomersen is targeted to human apoB-100 and is a 20-nucleotide
phosphorothioate oligonucleotide composed of five 2-O-(2-methoxyethyl)modified ribonucleosides (2-MOE) at the 3 and 5 ends with
ten 2-deoxynucleosides in between. The sequence of mipomersen is
OxPL/m-apoB
0.460.26
0.760.41
0.06
OxPL/apo(a)
NA
1.410.42
NA
Apo(a)/m-apoB
NA
0.650.66
NA
Methods
NA indicates not applicable.
Downloaded from http://circ.ahajournals.org/ by guest on January 7, 2013
NA
Merki et al
Mipomersen Reduces Lp(a) and OxPL/ApoB Levels
week of treatment, and then at 2-week intervals up to 11 weeks of
treatment. After treatment was stopped, blood was also collected at
2, 6, and 10 weeks. Detailed lipoprotein and immunological measurements were then performed as described below.
Determination of Total Cholesterol, Triglycerides,
ApoB-100, Lp(a), and Apo(a) Levels
Total cholesterol and triglycerides were determined by commercial
enzymatic assay using the Roche Cobas Mira Plus Analyzer. Plasma
Lp(a) levels [ie, apoB-100 covalently bound to apo(a)] were measured by a validated sandwich ELISA developed in our laboratory in
which human apoB-100 from plasma (1:400 dilution) is captured on
a plate with monoclonal antibody MB47 (5 g/mL), and apo(a) was
detected with biotinylated murine monoclonal antibody LPA4
(which does not cross-react with plasminogen).13 A standard curve is
generated with human plasma of known Lp(a) mass and was used to
determine Lp(a) levels. We have previously shown that this method
correlates highly (n500, r0.96, P0.0001) with a commercial
assay (Diasorin, Inc, Stillwater, Minn).13 This assay does not
measure free apo(a) levels [ie, apo(a) not bound to apoB-100]. The
Diasorin assay was used to measure total apo(a) [both as Lp(a) and
as free apo(a)] because it was postulated that this mouse model may
have excess apo(a) compared with h-apoB-100. However, because
the calibrators for this assay are based on Lp(a) standards that are of
higher molecular mass than the mini-apo(a) in these mice, the
absolute values of apo(a), but not relative changes, are likely to be
overestimated, as previously suggested.21 H-apoB-100 levels were
determined by a commercial assay (Diasorin, Inc). Mouse apoB
levels were determined with a chemiluminescent ELISA with capture murine monoclonal antibody LF5 and detection antibody LF3.22
These antibodies recognize different epitopes on mouse apoB-100
(m-apoB-100) but do not recognize h-apoB-100.
We also used an additional methodology to assess whether this
Lp(a) mouse model had free circulating apo(a) not bound to
h-apoB-100. It was hypothesized that immunoprecipitation with
MB47 would pellet all h-apoB-100 particles, including Lp(a), but not
free apo(a) or apo(a) noncovalently sticking to other lipoproteins (ie,
mouse apoB-100). Thus, persistence of apo(a) in the supernatant
would represent apo(a) not bound to h-apoB-100. Plasma was
obtained from the 4 Lp(a) mice from study 2 that were treated with
mipomersen at baseline and 4-week time points. Increasing doses of
MB47 (0 to 20-molar excess MB47:apoB-100 based on a molecular
weight of apoB-100 of 515 kDa and MB47 of 165 kDa) were
added to plasma samples and incubated overnight at 4C. The
samples were then centrifuged at 20 000 rpm to pellet MB47:apoB100 complexes, and the supernatant was examined for the presence
of apoB-100, Lp(a), and apo(a). These assays were performed using
a similar ELISA methodology as described above. Briefly, the
capture and detection antibodies for apoB-100 were MB47 (5
g/mL) and a goat anti-human antibody, respectively; for Lp(a),
MB47 (5 g/mL) and LPA4; and for apo(a), LPA4 (5 g/mL) as the
capture antibody and the detection antibody [LPA4 recognizes an
epitope present on apo(a) in 1 copy, so it can be used in this
manner].
Determination of OxPL on H-ApoB-100, Mouse
ApoB-100, or Apo(a)
A chemiluminescence ELISA was used to measure the amount of
OxPLs present on h-apoB-100 particles (OxPL/h-apoB) using E06 as
previously described in detail.14 For this assay, plasma was added
(1:100 dilution) to microtiter plates precoated with MB47; the
presence of OxPL was detected with biotinylated E06; and values
were expressed as relative light units (RLUs). To determine the
amount of h-apoB-100 captured on each well, MB47 was coated on
parallel plates; plasma (1:100 dilution) was added; and then biotinylated goat anti h-apoB-100 was added to determine the amount of
apoB-100 (in RLUs) captured. The E06 RLUs were then divided by
the apoB RLUs, and the OxPL/apoB ratio was derived.
A similar methodology was used to measure the content of OxPL
on apo(a) particles [OxPL/apo(a)], except LPA4 was used as the
745
capture antibody. To determine the amount of apo(a) captured on
each well, LPA4 was coated on parallel plates; plasma (1:100
dilution) was added; and then biotinylated LPA4 was added to
determine the amount of apo(a) (in RLUs) captured. The E06 RLUs
were then divided by the apo(a) RLUs to derive the OxPL/apo(a)
ratio.
To determine OxPL on mouse apoB-100 particles (OxPL/
m-apoB), we used the same methodology as above except that plates
were coated with antibody LF5; plasma (1:100 dilution) was added;
and then OxPL/m-apoB was determined by biotinylated E06. To
determine the amount of m-apoB captured, parallel plates were
coated with LF5; plasma (1:100 dilution) was added; and the amount
of m-apoB captured was determined by LF3. The E06 RLUs were
then divided by the LF3 RLUs to determine the OxPL/m-apoB ratio.
Determination of Autoantibodies to
Malondialdehyde-LDL
Mouse IgG and IgM autoantibodies to malondialdehyde-LDL were
determined as previously described in detail.23
RNA and Reverse-Transcriptase Polymerase
Chain Reaction Analyses
Total RNA was extracted from whole-liver tissue and primary
hepatocytes isolated (Qiagen RNeasy) as previously described.20 The
primers used were as follows: h-apoB-100, 5-TGCTAAAGGCACATATGGCCT-3 and 5-CTCAGGTTGGACTCTCCATTGAG-3
with the fluorescent probe 5-CTTGTCAGAGGGATCCTAACACTGGCCG-3; apo(a), 5-CCACAGTGGCCCCGGT-3 and 5-ACAGGGCTTTTCTCAGGTGGT-3 with the fluorescent probe 5-CCAAGCACAGAGGCTCCTTCTGAACAAG-3; and m-apoB-100, 5-CGTGGGCTCCAGCATTCTA-3 and 5-AGTCATTTCTGCCTTTGCGTC-3
with the fluorescent probe 5-CCAATGGTCGGGCACTGCTCAA-3.
Expression values were normalized to cyclophilin A. DNA was isolated
with the Qiagen DNeasy tissue kit.
HPLC Analysis of Lipoproteins
Serum lipoprotein and cholesterol profiling was performed as
described.20
Western Blots for H-ApoB-100, Lp(a), and Apo(a)
Western blot analyses for h-apoB-100, Lp(a), and apo(a) were
performed on mouse plasma subjected to electrophoresis on 4% to
12% Tris-glycine gels overnight at 4C and transferred to
polyvinylidene-fluoride membranes (Invitrogen, Carlsbad, Calif).
Nondenaturing gels were used for h-apoB and Lp(a); denaturing gels
were used for apo(a). The next day, blots were incubated for 1 hour
with a commercially available horseradish peroxidase conjugated,
human-specific apoB antibody (Untied States Biological, Swampscott, Mass) or LPA4 (1:1,000 dilution), followed by a goat antimouse IgG horseradish peroxidase conjugated antibody (1:15 000,
BD Biosciences, San Diego, Calif). Protein bands were visualized
with the ECL Plus Western blot detection kit (Amersham Biosciences, Inc, Piscataway, NJ). The goat anti-mouse IgG horseradish
peroxidase conjugated antibody also was used to determine the
presence of mouse IgG.
Frozen liver sections 10 m thick were air dried and briefly fixed
with 4% paraformaldehyde, rinsed with 60% isopropanol, stained
with Oil Red O (3 mg/mL) for 15 minutes, rinsed with isopropanol,
and counterstained with Hematoxylin QS (Vector Laboratories,
Burlingame, Calif).
Statistical Analysis
Analysis of quantitative parameters in mice over the time course of
the study was performed with 1-way ANOVA with the posthoc
Bonferroni multiple comparison test as appropriate. Differences
between the groups were assessed by Students t test. Values of
P0.05 were considered significant. The Pearson parametric test
was used to calculate correlations between variables.
Downloaded from http://circ.ahajournals.org/ by guest on January 7, 2013
746
Circulation
August 12, 2008
Table 2. Lipoprotein Variables in Response to Mipomersen or
Control ASO
Baseline Levels of Lipid Variables and OxPLs
The baseline total cholesterol levels (180.631.9 versus
148.026.1 mg/dL; P0.021) and h-apoB-100 levels
(100.718.2 versus 63.417.3 mg/dL; P0.0002) were
significantly higher in the Lp(a) mice compared with the
h-apoB mice (Table 1), as previously described.17
The baseline OxPL/h-apoB ratio was 55-fold higher in the
Lp(a) mice than in the h-apoB mice (3.280.08 versus
0.060.02; P0.0001). There was no significant difference
in the OxPL/m-apoB ratio between groups (0.760.41 versus
0.460.26; P0.06).
A; P0.29) after 4 weeks of treatment. The 8 Lp(a) mice in
this group had variable baseline apo(a) levels (range, 93 to
163 mg/dL), and interestingly, a strong correlation was noted
between hepatic apo(a) mRNA expression and the final
apo(a) plasma levels (r0.95, P0.0001), but a weaker
correlation was observed with Lp(a) and apo(a) mRNA levels
(r0.75, P0.03). Furthermore, there was no difference
among groups in mouse apoB mRNA expression
(110.113.2% versus 98.112.9%; P0.41). As expected, a
significant reduction in h-apoB-100 mRNA was noted
(26.02.6% versus 87.57.1%; P0.0033) in the
mipomersen-treated group compared with the control ASO
group.
Western blot analysis revealed that h-apoB and Lp(a)
levels were significantly reduced, but there was no effect on
apo(a) levels (Figure 2). There was no evidence of hepatic
steatosis in response to mipomersen, as assessed by Oil Red
O staining of hepatic tissue (data not shown).
To further assess the relative excess of apo(a) and Lp(a) in
the Lp(a) mice, we immunoprecipitated h-apoB-100 from
plasma of Lp(a) mice before treatment with mipomersen with
excess MB47 and assayed the content of apoB-100, apo(a),
and Lp(a) remaining in the supernatant to provide a measure
of the free apo(a). Figure 3 (top) shows changes in these
parameters normalized to pre-MB47 values and demonstrates
that nearly 90% of both h-apoB-100 and Lp(a) but only 25%
of apo(a) was immunoprecipitated [884% of h-apoB-100,
924% of Lp(a), and 2522% of apo(a)]. Thus, at baseline
in these Lp(a) mice, 75% of apo(a) appears to be free, eg, not
bound to h-apoB-100. At the 4-week time point, mipomersen
treatment (Figure 3, bottom) resulted in qualitatively similar
data, except for the presence of higher levels of free apo(a)
after the reduction of h-apoB-100 in response to mipomersen
[apoB, 961.0%; Lp(a), 952.0%; apo(a), 422% of baseline levels].
Study 2 in Lp(a) Mice
Study 3 in H-ApoB Mice and Lp(a) Mice
Effect of Mipomersen on Lipoprotein Levels and
Composition and Hepatic ApoB-100 and Apo(a)
mRNA Expression
Mipomersen reduced total cholesterol levels over the 4-week
treatment period as expected (Table 2). High-performance
liquid chromatography analysis documented that this was due
in large measure to a reduction in LDL, which was decreased
75% in the 2- and 4-week time points in the mipomersen
group (Figure 1). There was no change in high-density
lipoprotein (HDL) cholesterol or in the lipoprotein distribution pattern. No significant changes were noted with the
control ASO 141923 (Figure 1).
Mipomersen also decreased Lp(a) levels over the 4 weeks
(81.324.4 mg/dL at baseline, 33.89.0 mg/dL at 2 weeks,
31.815.6 mg/dL at 4 weeks; P0.0002 for trend; Table 2).
In contrast, apo(a) levels did not change significantly
(98.935.9 mg/dL at baseline, 104.038.72 mg/dL at 3
weeks, 102.136.0 mg/dL at 4 weeks; P0.78 for trend).
This was further supported by evaluating hepatic apo(a)
mRNA expression in mipomersen versus control ASO
141923 (53.837.4% [range, 24% to 108%]; versus
89.236.9% [range, 32% to 138%] normalized to cyclophilin
Effect of Mipomersen on H-ApoB-100 levels and
Lp(a) Levels
After administration of mipomersen, significant reductions
were noted in a time-dependent manner in h-apoB levels in
the h-apoB mice (P0.0001 for trend by ANOVA; Figure
4A). The h-apoB-100 levels reached a nadir by week 3 and
remained low until week 11. After mipomersen treatment was
discontinued, h-apoB-100 levels returned to baseline levels
10 weeks later. The h-apoB-100 levels in Lp(a) mice also
decreased in a similar time-dependent manner when treated
with mipomersen (P0.0001 for trend by ANOVA; Figure
4B). In contrast, there were no significant changes in h-apoB100 levels in either mouse model with the control ASO. No
changes in m-apoB levels were noted with either mipomersen
or control ASO (data not shown).
In the Lp(a) mice, concomitant with the decrease in
h-apoB-100 levels, there was a significant decline in Lp(a)
levels in response to mipomersen (P0.0001 for trend by
ANOVA; Figure 4C). The Lp(a) levels began to decline by 3
weeks and reached a nadir from 5 to 11 weeks. After
discontinuation of therapy, the Lp(a) levels returned to
baseline after 10 weeks.
Total
Cholesterol,
mg/dL
Triglycerides,
mg/dL
Lp(a), mg/dL
Apo(a),
mg/dL
Baseline
156.310.7
121.813.8
81.324.4
70.133.6
2 wk
105.322.6*
33.59.0
92.010.2
4 wk
96.327.3
130.855.6
31.815.6
97.58.4
Mipomersen
82.527.10
ISIS 141923
Baseline
205.026.1
168.334.3
98.324.2
92.019.6
2 wk
215.334.2
151.049.8
95.818.6
94.010.1
4 wk
172.012.5
160.028.6
98.324.0
81.045.1
*P0.05, P0.01, P0.001 vs baseline.
The authors had full access to and take full responsibility for the
integrity of the data. All authors have read and agree to the
manuscript as written.
Results
Study 1 in H-ApoB-100 and Lp(a) Mice
Downloaded from http://circ.ahajournals.org/ by guest on January 7, 2013
Merki et al
Mipomersen Reduces Lp(a) and OxPL/ApoB Levels
747
Figure 1. High-performance liquid chromatography of plasma from Lp(a) mice treated with mipomersen or control ASO. A, Distribution of
cholesterol from 1 mouse in the various fractions. B, Mean levels of LDL cholesterol and HDL cholesterol of all mice at the 3 time points.
To assess the fate of any free apo(a) when Lp(a) levels
decreased, m-apoB-100 was captured on microtiter well
plates, and the content of apo(a) was assessed with antibody
LPA4 [apo(a)/m-apoB]. This analysis revealed a steady
increase in the proportion of apo(a)/m-apoB, which peaked at
11 weeks (P0.014 for trend by ANOVA; Figure 4D),
returning to baseline by 10 weeks after cessation of therapy.
Effect of Mipomersen on OxPL/H-ApoB
and OxPL/M-ApoB
As noted above, the baseline OxPL/h-apoB levels were
55-fold higher in the Lp(a) mice than in the h-apoB mice
(Figure 4A and 4B). Over the study period, there were no
significant changes in OxPL/h-apoB in the h-apoB mice
treated with either ASO 301012 or the ASO control (Figure
Downloaded from http://circ.ahajournals.org/ by guest on January 7, 2013
748
Circulation
August 12, 2008
Figure 2. Western blot analysis of h-apoB-100, Lp(a), apo(a),
and mouse IgG. Shown are the findings from plasma in mice
from study 2 at the baseline and 4-week time points after
administration of mipomersen or control ASO. Lp(a) and h-apoB
immunoblots were performed in nondenaturing conditions,
whereas apo(a) and IgG blots were done under denaturing
conditions.
5A). However, significant decreases were noted in OxPL/hapoB in the Lp(a) mice treated with mipomersen but not in
those treated with control ASO (P0.0001 for trend by
ANOVA; Figure 5B). There were no significant changes in
OxPL/m-apoB levels over time in the h-apoB mice (Figure
5C) or Lp(a) mice (Figure 5D).
Effect of Mipomersen on OxPL on Apo(a) Particles and
Malondialdehyde-LDL Autoantibodies
To assess whether the ratio of OxPL on apo(a) particles
changed during the treatment in Lp(a) mice, apo(a) particles
were captured with antibody LPA4, and the content of OxPL
was assessed with the antibody E06. No changes in OxPL/
apo(a) were noted in Lp(a) mice treated with either mipomersen or ASO control (Figure 6).
There was no effect of mipomersen or control ASO on
malondialdehyde-LDL autoantibody titers (data not shown).
Discussion
This study demonstrates that an ASO directed against
h-apoB-100 significantly reduces plasma Lp(a) levels in
Lp(a) mice. This reduction was related to the reduction in
h-apoB-100 levels in a quantitative and temporal manner,
suggesting that apoB-100 production is a limiting factor in
the generation of Lp(a) particles in this murine model.
Furthermore, because Lp(a) carries OxPL (those detected by
antibody E06) in plasma,6,9 15 there was a reduction in
OxPL/apoB, which reflected a reduction in the mass of Lp(a),
rather than a reduced carrying capacity of Lp(a) for OxPL. If
apoB-100 synthesis is a rate-limiting step in the generation of
human Lp(a) in a similar manner, our findings suggest that
mipomersen may provide a novel therapy to reduce plasma
Lp(a) levels in patients. In preliminary studies in human
subjects treated with mipomersen, Lp(a) levels have been
observed to decrease up to 60% (D. Tribble, Isis, Inc,
personal communication). Prospective studies in humans to
determine the impact of mipomersen on Lp(a) levels seem
warranted.
The mechanisms underlying apo(a) synthesis are relatively
well known. Apo(a) is synthesized in hepatocytes, and the
rate of synthesis is related primarily to apo(a) gene transcription.24 Posttranslational regulation such as formation of the 3
disulfide bonds for each kringle type and N-linked glycation
is important for proper apo(a) folding and transport out of the
endoplasmic reticulum. This process may take up to 120
minutes and depends on apo(a) size. Once apo(a) exits the
endoplasmic reticulum, it travels to the Golgi apparatus,
where it undergoes further posttranslational modification and
is finally transported to the hepatocyte cell surface. Lp(a) is
then thought to be assembled from newly synthesized apoB100, first by low-affinity, noncovalent interactions between
KIV-5 to KIV-8 and then through a disulfide bond between
unpaired cysteine 4057 on KIV-9 on apo(a) and cysteine
4326 on the C-terminal region of apoB-100. Because small
isoform apo(a) particles are more easily synthesized and
secreted, it is postulated that subjects with small apo(a)
isoforms have higher Lp(a) levels. Although apo(a) gene
transcription contributes significantly to plasma Lp(a) levels,25 some variability in those levels may be attributed to
genetic polymorphisms of apo(a).26 It is also quite interesting
that a modest inverse correlation is present between triglyceride levels and Lp(a) levels, suggesting that the rate of
very-low-density lipoprotein synthesis may affect Lp(a) metabolism.27 In fact, up to 4% of apo(a) is present on verylow-density lipoprotein particles, and these complexes may
have a slower catabolism.28,29
In contrast, the clearance of Lp(a) is less well understood.
The preponderance of evidence suggests that the LDL receptor does not play a major role in Lp(a) clearance.24 Approximately 10% to 25% of Lp(a) is converted to LDL when
apo(a) is cleaved off, and LDL is then cleared by the LDL
receptor. There are also some data, although not entirely
consistent,30 that apo(a) may not remain covalently attached
to a single apoB-100 but may in fact associate with 2
apoB-100 molecules over its metabolic lifetime.27 In patients
with renal failure, a small amount (7.5%) of free apo(a),
mainly of large isoforms, may be found in the plasma.31 Some
Lp(a) is cleaved by metalloproteinases and elastases, which
results in apo(a) fragments that are then cleared and/or
secreted in urine by the kidney. Recent data in mice also
suggest the possibility of an as-yet unidentified apo(a) receptor in hepatocytes of mice because intravenously injected free
apo(a) may reduce Lp(a) uptake in hepatocytes.32
ASOs targeting proteins involved in lipoprotein metabolism represent novel therapeutic agents to treat dyslipidemias.18 Proof-of-principle studies initially demonstrated that
Downloaded from http://circ.ahajournals.org/ by guest on January 7, 2013
Merki et al
Mipomersen Reduces Lp(a) and OxPL/ApoB Levels
749
Figure 3. Immunoprecipitation experiment using murine monoclonal antibody MB47 to precipitate out h-apoB from plasma of Lp(a)
mice (n4). A 20:1-molar excess MB47:apoB-100 was used. The supernatant was then assayed for the presence of h-apoB-100 (left),
Lp(a) (middle), and apo(a) (right). Top, Baseline time point; bottom, the 4-week time point after mipomersen administration.
ISIS 147764, an ASO targeted to m-apoB-100, reduced
mouse apoB mRNA levels in the liver and LDL cholesterol
levels in plasma in a dose- and time-dependent manner in
C57BL/6, LDLR/, and apoE/ mice. In a phase 2, doubleblind, randomized, placebo-controlled, 3-month doseescalation study, mipomersen reduced apoB-100 (50% at the
200-mg dose) and LDL cholesterol (35% at the 200-mg dose)
levels in a dose- and time-dependent manner.19
In this study, we hypothesized that reducing hepatic
synthesis of apoB-100 would result in a reduction of plasma
Lp(a) levels in Lp(a) mice. These mice resemble humans in
that they have similar plasma Lp(a) levels and genuine Lp(a)
particles. They differ in that the animals have excess apo(a)
compared with apoB-100, whereas in most humans, there is
an excess of apoB-100 and relatively little free apo(a). After
administration of mipomersen, in conjunction with reduced
hepatic mRNA expression and plasma apoB-100 levels, a
dramatic reduction in plasma Lp(a) levels was evident. This
was not due to reduced apo(a) mRNA expression, suggesting
that apoB-100 availability is a limiting step in the formation
of Lp(a) particles.17,33 Furthermore, in support of this concept, it was shown that the amount of apo(a) on m-apoB-100,
which is known from prior studies to noncovalently associate
with m-apoB-100,17,33 increased in proportion to reduced
h-apoB-100 and Lp(a) levels. Overall, these data suggest a
novel pathway for reducing Lp(a) levels along with apoB-100
levels. Conversely, it is likely that a reduction in Lp(a) may
be mediated by a reduction in apo(a) synthesis using apo(a)-
Downloaded from http://circ.ahajournals.org/ by guest on January 7, 2013
750
Circulation
August 12, 2008
Figure 4. Temporal changes in h-apoB levels in h-apoB mice (A) and Lp(a) mice (B), Lp(a) levels in Lp(a) mice (C), and apo(a) content
on mouse apoB-100 particles [apo(a)/m-apoB] (D) in response to mipomersen or control ASO. *P001, **P0.01 vs baseline values.
specific ASOs, although this hypothesis was not tested in this
study. This approach will be of interest in future studies once
a suitable apo(a) ASO is identified. The fate of free apo(a)
also was not evaluated in this study, and understanding its
kinetics would be important in future experiments.
The relationship between OxPL and Lp(a) has provided
important insights into the potential atherogenicity of Lp(a).
In vitro studies have suggested that Lp(a) is the main carrier
of OxPL, identified by antibody E06, in human plasma.8,9
Additional observations from our laboratory have shown that
the OxPL immunoreactivity may be immunoprecipitated
along with Lp(a), and detailed density gradient ultracentrifugation experiments showed that nearly all OxPLs recognized
by antibody E06 were found in fractions containing apo(a), as
opposed to other apolipoproteins. Furthermore, in vitro transfer studies showed that donor OxPLs from oxidized LDL are
preferentially donated to Lp(a), as opposed to LDL, in a timeand temperature-dependent manner, even in aqueous buffer.
These observations are supported by several clinical studies
showing that a strong association occurs between OxPL/apoB
and Lp(a)10 14 and that OxPL/apoB and Lp(a) show strikingly
similar risk for angiographically defined coronary artery
disease,6 the presence and progression of carotid and femoral
atherosclerosis,15 and the prediction of death, myocardial
infarction, and stroke in unselected populations.16 Interestingly, the OxPL/apoB measure tends to be numerically
superior in predicting cardiovascular manifestations, and in
some but not all studies, the OxPL/apoB ratio was even
independent of Lp(a) in predicting coronary artery disease in
male subjects 60 years of age.6
In this study, it was demonstrated that Lp(a) mice had
significantly higher baseline levels of OxPL/h-apoB than
h-apoB mice, consistent with prior observations in this model
and with the fact that OxPLs measured by E06 are distributed
mainly on Lp(a).17 This was noted in mice on a chow diet and
without any other stimulus to generate OxPL. These data,
generated even in a weak atherogenic milieu, strongly support
the clinical observations noted above that Lp(a) is a preferential carrier of OxPL. Interestingly, the reduction in OxPL/
h-apoB appeared to be directly related to the lowering of
Lp(a) levels rather than the proportion of OxPL on Lp(a)
particles because the OxPL/apo(a) ratio did not change with
mipomersen, which lowers apoB-100 levels but is not expected to have direct antioxidant properties. This was supported by the immunoprecipitation experiment showing a
reduction in OxPL/h-apoB levels in the supernatant in conjunction with immunoprecipitation of apoB-100 and Lp(a).
We have also previously shown that free apo(a) and recombinant apo(a) peptides bind OxPL.9 However, the relative
proportion bound by Lp(a) versus apo(a) has not been
determined yet and is an area of active investigation. Where
these OxPL are generated and how they are ultimately
Downloaded from http://circ.ahajournals.org/ by guest on January 7, 2013
Merki et al
Mipomersen Reduces Lp(a) and OxPL/ApoB Levels
751
Figure 5. Temporal changes in OxPL/h-apoB levels in h-apoB mice (A), OxPL/h-apoB levels in Lp(a) mice (B), OxPL/m-apoB levels in
h-apoB mice (C), and OxPL/m-apoB levels in h-apoB mice (D) in response to mipomersen or control ASO. *P01, **P0.05 vs baseline values.
transferred onto Lp(a) in vivo are major questions that merit
further exploration.16 They suggest, however, that the ability
of Lp(a) to bind and transport proinflammatory OxPL may be
crucial to understanding its atherogenicity and perhaps its
potential thrombogenicity.
This study is also the first to document that a reduction in
OxPL/apoB levels is achievable with a reduction in Lp(a)
levels. This reduction appeared to be dependent on treatment
duration; the OxPL/apoB levels returned to baseline when
therapy was discontinued. This decrease in OxPL/apoB was
directly related to the reduction in Lp(a) levels because the
OxPL/apo(a) ratio did not change with therapy. In prior
clinical studies with statins and in subjects on low-fat
diets,10,11,14 we actually noted an increase in the OxPL/apoB
ratio and Lp(a) levels and hypothesized that this increase may
reflect an egress of OxPL from the vessel wall, which is then
trapped by Lp(a) in the circulation. Those data also could be
consistent with upregulation of Lp(a) by statins with concomitant binding of OxPL, as well as other undefined mechanisms. In animal studies of dietary regression, the increase in
OxPL/apoB also was noted in rabbits with no Lp(a), along
with concomitant removal of OxPL from the vessel wall as
assessed by immunostaining before plaque regression, suggesting that these 2 processes were linked mechanistically.34
Although further evaluation is needed to understand the
relationship between changes in OxPL/apoB and Lp(a), these
studies suggest that changes in OxPL are linked to changes in
Lp(a). The implications of these observations in clinical risk
prediction await outcomes studies.
Study Limitations
Figure 6. Temporal relationship of OxPL/apo(a) in Lp(a) mice in
response to mipomersen or control ASO.
This study tested the efficacy of mipomersen on 1 specific
mini-apo(a) construct under the control of an apoE promoter;
therefore, translation to humans studies awaits determination.
The role of Lp(a) in atherogenesis in this mouse model, the
Downloaded from http://circ.ahajournals.org/ by guest on January 7, 2013
752
Circulation
August 12, 2008
effect of mipomersen in cholesterol-fed Lp(a) mice, and
whether the reduction in OxPL/apoB will lead to additional
antiatherogenic properties will be addressed in additional
studies.
Conclusion
Administration of mipomersen resulted in a significant reduction in Lp(a) and OxPL/apoB levels in Lp(a) mice and may
represent a novel therapeutic agent in reducing LDL-cholesterol, Lp(a), and OxPL/apoB levels in humans.
Sources of Funding
This study was supported by the Fondation Leducq (Drs Witztum
and Tsimikas) and an unrestricted gift from Isis Pharmaceuticals to
the University of California.
Disclosures
Drs Witztum and Tsimikas are named as inventors in patents and
patent applications for the potential commercial use of antibodies to
oxidized LDL and have served as consultants to Isis Pharmaceuticals, Inc. M.J. Graham and Drs Mullick and Crooke are employees
of ISIS, Inc. The other authors report no conflicts.
References
1. Anuurad E, Boffa MB, Koschinsky ML, Berglund L. Lipoprotein (a): a
unique risk factor for cardiovascular disease. Clin Lab Med. 2006;26:
751772.
2. Marcovina SM, Koschinsky ML. Lipoprotein(a) as a risk factor for
coronary artery disease. Am J Cardiol. 1998;82:57U 66U.
3. Danesh J, Collins R, Peto R. Lipoprotein (a) and coronary artery disease:
metaanalysis of prospective studies. Circulation. 2000;102:10821085.
4. Kiechl S, Willeit J, Mayr M, Viehweider B, Oberhollenzer M,
Kronenberg F, Wiedermann CJ, Oberthaler S, Xu Q, Witztum JL,
Tsimikas S. Oxidized phospholipids, lipoprotein(a), lipoproteinassociated phospholipase A2 activity, and 10-year cardiovascular outcomes: prospective results from the Bruneck Study. Arterioscler Thromb
Vasc Biol. 2007;27:1788 1795.
5. Suk DJ, Rifai N, Buring JE, Ridker PM. Lipoprotein (a), measured with
an assay independent of apolipoprotein (a) isoform size, and risk of future
cardiovascular events among initially healthy women. JAMA. 2006;296:
13631370.
6. Tsimikas S, Brilakis ES, Miller ER, McConnell JP, Lennon RJ, Kornman
KS, Witztum JL, Berger PB. Oxidized phospholipids, Lp(a) lipoprotein,
and coronary artery disease. N Engl J Med. 2005;353:46 57.
7. Caplice NM, Panetta C, Peterson TE, Kleppe LS, Mueske CS, Kostner
GM, Broze GJ Jr, Simari RD. Lipoprotein (a) binds and inactivates tissue
factor pathway inhibitor: a novel link between lipoproteins and
thrombosis. Blood. 2001;98:2980 2987.
8. Bergmark C, Dewan A, Orsoni A, Merki E, Miller ER, Shin MJ, Binder
CJ, Hrkk S, Krauss RM, Chapman MJ, Witzum JL, Tsimikas S. A
novel function of lipoprotein (a) as a preferential carrier of oxidized
phospholipids in human plasma. J Lipid Res. In press.
9. Edelstein C, Pfaffinger D, Hinman J, Miller E, Lipkind G, Tsimikas S,
Bergmark C, Getz GS, Witztum JL, Scanu AM. Lysinephosphatidylcholine adducts in kringle V impart unique immunological
and potential pro-inflammatory properties to human apolipoprotein (a).
J Biol Chem. 2003;278:5284152847.
10. Rodenburg J, Vissers MN, Wiegman A, Miller ER, Ridker PM, Witztum
JL, Kastelein JJ, Tsimikas S. Oxidized low-density lipoprotein in children
with familial hypercholesterolemia and unaffected siblings: effect of
pravastatin. J Am Coll Cardiol. 2006;47:18031810.
11. Silaste ML, Rantala M, Alfthan G, Aro A, Witztum JL, Kesaniemi YA,
Horkko S. Changes in dietary fat intake alter plasma levels of oxidized
low-density lipoprotein and lipoprotein (a). Arterioscler Thromb Vasc
Biol. 2004;24:498 503.
12. Tsimikas S, Bergmark C, Beyer RW, Patel R, Pattison J, Miller E, Juliano
J, Witztum JL. Temporal increases in plasma markers of oxidized lowdensity lipoprotein strongly reflect the presence of acute coronary syndromes. J Am Coll Cardiol. 2003;41:360 370.
13. Tsimikas S, Lau HK, Han KR, Shortal B, Miller ER, Segev A, Curtiss
LK, Witztum JL, Strauss BH. Percutaneous coronary intervention results
in acute increases in oxidized phospholipids and lipoprotein (a):
short-term and long-term immunologic responses to oxidized low-density
lipoprotein. Circulation 2004;109:3164 3170.
14. Tsimikas S, Witztum JL, Miller ER, Sasiela WJ, Szarek M, Olsson AG,
Schwartz GG. High-dose atorvastatin reduces total plasma levels of
oxidized phospholipids and immune complexes present on apolipoprotein
B-100 in patients with acute coronary syndromes in the MIRACL trial.
Circulation. 2004;110:1406 1412.
15. Tsimikas S, Kiechl S, Willeit J, Mayr M, Miller ER, Kronenberg F, Xu
Q, Bergmark C, Weger S, Oberhollenzer F, Witztum JL. Oxidized phospholipids predict the presence and progression of carotid and femoral
atherosclerosis and symptomatic cardiovascular disease: five-year prospective results from the Bruneck study. J Am Coll Cardiol. 2006;47:
2219 2228.
16. Tsimikas S, Tsironis LD, Tselepis AD. New insights into the role of
lipoprotein(a)-associated lipoprotein-associated phospholipase A2 in atherosclerosis and cardiovascular disease. Arterioscler Thromb Vasc Biol.
2007;27:2094 2099.
17. Schneider M, Witztum JL, Young SG, Ludwig EH, Miller ER, Tsimikas
S, Curtiss LK, Marcovina SM, Taylor JM, Lawn RM, Innerarity TL, Pitas
RE. High-level lipoprotein [a] expression in transgenic mice: evidence for
oxidized phospholipids in lipoprotein [a] but not in low density
lipoproteins. J Lipid Res. 2005;46:769 778.
18. Crooke RM. Antisense oligonucleotides as therapeutics for hyperlipidaemias. Expert Opin Biol Ther. 2005;5:907917.
19. Kastelein JJ, Wedel MK, Baker BF, Su J, Bradley JD, Yu RZ, Chuang E,
Graham MJ, Crooke RM. Potent reduction of apolipoprotein B and
low-density lipoprotein cholesterol by short-term administration of
an antisense inhibitor of apolipoprotein B. Circulation. 2006;114:
1729 1735.
20. Crooke RM, Graham MJ, Lemonidis KM, Whipple CP, Koo S, Perera RJ.
An apolipoprotein B antisense oligonucleotide lowers LDL cholesterol in
hyperlipidemic mice without causing hepatic steatosis. J Lipid Res. 2005;
46:872 884.
21. Marcovina SM, Albers JJ, Scanu AM, Kennedy H, Giaculli F, Berg K,
Couderc R, Dati F, Rifai N, Sakurabayashi I, Tate JR, Steinmetz A. Use
of a reference material proposed by the International Federation of
Clinical Chemistry and Laboratory Medicine to evaluate analytical
methods for the determination of plasma lipoprotein (a). Clin Chem.
2000;46:1956 1967.
22. Zlot CH, Flynn LM, Veniant MM, Kim E, Raabe M, McCormick SP,
Ambroziak P, McEvoy LM, Young SG. Generation of monoclonal antibodies specific for mouse apolipoprotein B-100 in apolipoprotein
B-48-only mice. J Lipid Res. 1999;40:76 84.
23. Tsimikas S, Palinski W, Witztum JL. Circulating autoantibodies to
oxidized LDL correlate with arterial accumulation and depletion of
oxidized LDL in LDL receptor deficient mice. Arterioscler Thromb Vasc
Biol. 2001;21:95100.
24. Hobbs HH, White AL. Lipoprotein(a): intrigues and insights. Curr Opin
Lipidol. 1999;10:225236.
25. Boerwinkle E, Leffert CC, Lin J, Lackner C, Chiesa G, Hobbs HH.
Apolipoprotein (a) gene accounts for greater than 90% of the variation in
plasma lipoprotein (a) concentrations. J Clin Invest. 1992;90:52 60.
26. Luke MM, Kane JP, Liu DM, Rowland CM, Shiffman D, Cassano J,
Catanese JJ, Pullinger CR, Leong DU, Arellano AR, Tong CH,
Movsesyan I, Naya-Vigne J, Noordhof C, Feric NT, Malloy MJ, Topol
EJ, Koschinsky ML, Devlin JJ, Ellis SG. A polymorphism in the
protease-like domain of apolipoprotein(a) is associated with severe
coronary artery disease. Arterioscler Thromb Vasc Biol. 2007;27:
2030 2036.
27. Jenner JL, Ordovas JM, Lamon-Fava S, Schaefer MM, Wilson PW,
Castelli WP, Schaefer EJ. Effects of age, sex, and menopausal status on
plasma lipoprotein (a) levels: the Framingham Offspring Study. Circulation. 1993;87:11351141.
28. Devlin CM, Lee SJ, Kuriakose G, Spencer C, Becker L, Grosskopf I, Ko
C, Huang LS, Koschinsky ML, Cooper AD, Tabas I. An apolipoprotein(a)
peptide delays chylomicron remnant clearance and increases plasma
remnant lipoproteins and atherosclerosis in vivo. Arterioscler Thromb
Vasc Biol. 2005;25:1704 1710.
29. Gaubatz JW, Hoogeveen RC, Hoffman AS, Ghazzaly KG, Pownall HJ,
Guevara J Jr, Koschinsky ML, Morrisett JD. Isolation, quantitation, and
characterization of a stable complex formed by Lp[a] binding to triglyceride-rich lipoproteins. J Lipid Res. 2001;42:2058 2068.
Downloaded from http://circ.ahajournals.org/ by guest on January 7, 2013
Merki et al
Mipomersen Reduces Lp(a) and OxPL/ApoB Levels
30. Su W, Campos H, Judge H, Walsh BW, Sacks FM. Metabolism of
Apo(a) and ApoB100 of lipoprotein(a) in women: effect of postmenopausal estrogen replacement. J Clin Endocrinol Metab. 1998;83:
32673276.
31. Trenkwalder E, Gruber A, Konig P, Dieplinger H, Kronenberg F.
Increased plasma concentrations of LDL-unbound apo (a) in patients with
end-stage renal disease. Kidney Int. 1997;52:16851692.
32. Cain WJ, Millar JS, Himebauch AS, Tietge UJF, Maugeais C, Usher D,
Rader DJ. Lipoprotein [a] is cleared from the plasma primarily by the liver in a
process mediated by apolipoprotein [a]. J Lipid Res. 2005;46:26812691.
753
33. Chiesa G, Hobbs HH, Koschinsky ML, Lawn RM, Maika SD, Hammer
RE. Reconstitution of lipoprotein (a) by infusion of human low density
lipoprotein into transgenic mice expressing human apolipoprotein (a).
J Biol Chem. 1992;267:24369 24374.
34. Tsimikas S, Aikawa M, Miller FJ Jr, Miller ER, Torzewski M, Lentz SR,
Bergmark C, Heistad DD, Libby P, Witztum JL. Increased plasma
oxidized phospholipid:apolipoprotein B-100 ratio with concomitant
depletion of oxidized phospholipids from atherosclerotic lesions after
dietary lipid-lowering: a potential biomarker of early atherosclerosis
regression. Arterioscler Thromb Vasc Biol. 2007;27:175181.
CLINICAL PERSPECTIVE
Lipoprotein(a) [Lp(a)] is composed of apolipoprotein(a) [apo(a)], which is covalently bound to a low-density lipoprotein
by a single disulfide bond on apoB-100. Lp(a) levels are genetically determined and vary widely (0.1 to 250 mg/dL)
among individuals. Lp(a) is an independent risk factor for myocardial infarction, stroke, and peripheral arterial disease,
particularly in younger patients. However, its pathophysiological role and the underlying mechanisms through which it
contributes to cardiovascular disease are unknown. It also has not been determined yet whether lowering Lp(a) levels is
clinically beneficial, largely because of the lack of specific agents to lower Lp(a). We have recently discovered that Lp(a)
preferentially binds oxidized phospholipids in plasma. In this study, we demonstrate that the antisense oligonucleotide
mipomersen, directed to human apoB-100, significantly reduced human apoB-100 levels in Lp(a) transgenic mice
[expressing human apoB-100 and apo(a) to make authentic Lp(a) particles], as expected. However, over the 11-week
treatment period, compared with baseline, it also reduced Lp(a) levels by 75% (P0.0001) in a time-dependent fashion.
This was due primarily to limiting the availability of apoB-100 to bind to apo(a). Furthermore, it significantly reduced
plasma levels of oxidized phospholipids on apoB and apo(a) particles. This study demonstrates that apoB-100 is a limiting
factor in Lp(a) particle synthesis in this Lp(a) transgenic model. If applicable to humans, mipomersen may represent a novel
therapeutic approach in not only reducing apoB-100 and low-density lipoprotein cholesterol but also in reducing Lp(a) and
associated oxidized phospholipids.
Downloaded from http://circ.ahajournals.org/ by guest on January 7, 2013
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Low Budget Music Promotion and PublicityDokumen41 halamanLow Budget Music Promotion and PublicityFola Folayan100% (3)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Top Activist Stories - 5 - A Review of Financial Activism by Geneva PartnersDokumen8 halamanTop Activist Stories - 5 - A Review of Financial Activism by Geneva PartnersBassignotBelum ada peringkat
- Aliping PDFDokumen54 halamanAliping PDFDirect LukeBelum ada peringkat
- Draft JV Agreement (La Mesa Gardens Condominiums - Amparo Property)Dokumen13 halamanDraft JV Agreement (La Mesa Gardens Condominiums - Amparo Property)Patrick PenachosBelum ada peringkat
- Toh MFS8B 98B 003-11114-3AG1 PDFDokumen92 halamanToh MFS8B 98B 003-11114-3AG1 PDFDmitry NemtsoffBelum ada peringkat
- Account Statement 250820 240920 PDFDokumen2 halamanAccount Statement 250820 240920 PDFUnknown100% (1)
- Data StructuresDokumen4 halamanData StructuresBenjB1983Belum ada peringkat
- NIQS BESMM 4 BillDokumen85 halamanNIQS BESMM 4 BillAliBelum ada peringkat
- Seabank Statement 20220726Dokumen4 halamanSeabank Statement 20220726Alesa WahabappBelum ada peringkat
- Logiq v12 SM PDFDokumen267 halamanLogiq v12 SM PDFpriyaBelum ada peringkat
- DFo 2 1Dokumen15 halamanDFo 2 1Donna HernandezBelum ada peringkat
- Standard Test Methods For Rheological Properties of Non-Newtonian Materials by Rotational (Brookfield Type) ViscometerDokumen8 halamanStandard Test Methods For Rheological Properties of Non-Newtonian Materials by Rotational (Brookfield Type) ViscometerRodrigo LopezBelum ada peringkat
- Design and Analysis of Modified Front Double Wishbone Suspension For A Three Wheel Hybrid VehicleDokumen4 halamanDesign and Analysis of Modified Front Double Wishbone Suspension For A Three Wheel Hybrid VehicleRima AroraBelum ada peringkat
- Project Document EiDokumen66 halamanProject Document EiPrathap ReddyBelum ada peringkat
- ThorpeDokumen267 halamanThorpezaeem73Belum ada peringkat
- Building and Structural Construction N6 T1 2024 T2Dokumen9 halamanBuilding and Structural Construction N6 T1 2024 T2FranceBelum ada peringkat
- Odisha State Museum-1Dokumen26 halamanOdisha State Museum-1ajitkpatnaikBelum ada peringkat
- Math 9 Quiz 4Dokumen3 halamanMath 9 Quiz 4Lin SisombounBelum ada peringkat
- Wwii TictactoeDokumen2 halamanWwii Tictactoeapi-557780348Belum ada peringkat
- Introduction To Atomistic Simulation Through Density Functional TheoryDokumen21 halamanIntroduction To Atomistic Simulation Through Density Functional TheoryTarang AgrawalBelum ada peringkat
- Haier in India Building Presence in A Mass Market Beyond ChinaDokumen14 halamanHaier in India Building Presence in A Mass Market Beyond ChinaGaurav Sharma100% (1)
- Back Propagation Neural NetworkDokumen10 halamanBack Propagation Neural NetworkAhmad Bisyrul HafiBelum ada peringkat
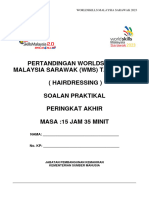
- Final WMS2023 HairdressingDokumen15 halamanFinal WMS2023 HairdressingMIRAWATI SAHIBBelum ada peringkat
- Guardcam InstructionsDokumen12 halamanGuardcam InstructionsCompuFix RepairsBelum ada peringkat
- Assignment 4Dokumen5 halamanAssignment 4Hafiz AhmadBelum ada peringkat
- COURTESY Reception Good MannersDokumen1 halamanCOURTESY Reception Good MannersGulzina ZhumashevaBelum ada peringkat
- Numerical Modelling and Design of Electrical DevicesDokumen69 halamanNumerical Modelling and Design of Electrical Devicesfabrice mellantBelum ada peringkat
- Ci Thai RiceDokumen4 halamanCi Thai RiceMakkah Madina riceBelum ada peringkat
- Power Curbers, Inc. v. E. D. Etnyre & Co. and A. E. Finley & Associates, Inc., 298 F.2d 484, 4th Cir. (1962)Dokumen18 halamanPower Curbers, Inc. v. E. D. Etnyre & Co. and A. E. Finley & Associates, Inc., 298 F.2d 484, 4th Cir. (1962)Scribd Government DocsBelum ada peringkat
- BS 7974 2019Dokumen68 halamanBS 7974 2019bcyt00Belum ada peringkat