Intraarticular Injection of Platelet Rich Plasma (PRP) and Hyaluronic Acid (HA) in Early Knee Osteoarthritis
Diunggah oleh
Juniper PublishersHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Intraarticular Injection of Platelet Rich Plasma (PRP) and Hyaluronic Acid (HA) in Early Knee Osteoarthritis
Diunggah oleh
Juniper PublishersHak Cipta:
Format Tersedia
Orthopedics and Rheumatology
Open Access Journal
Research Article
Volume 1 Issue 5 - December 2015
Ortho & Rheum Open Access J
Copyright All rights are reserved by Osama A Seleem
Intraarticular Injection of Platelet Rich Plasma
(PRP) and Hyaluronic Acid (HA) in Early Knee
Osteoarthritis
Osama A Seleem* and Hassam M Gad
Department of Orthopaedic Surgery, Tanta University, Egypt
Submission: December 14, 2015; Published: December 23, 2015
*Corresponding author: Osama A Seleem, Assistant Prof. of Orthopaedic Surgery, Department of Orthopaedic Surgery, Faculty of Medicine,
Tanta University, Tanta, Abo-Bakr El-Sedeek street, Abo- Bakr building, 7th floor, Apartment No. 19, Egypt, Tel: 20401114321200; 20403338880;
Email:
Abstract
Introduction: This is a comparative study between HA and PRP injection in knee osteoarthritis. A total of 224 patients with knee
osteoarthritis (grade I and II) were enrolled in this study. The arthritic changes were graded according to the Kellgren and Lawrence
radiological scale. In the first group, 116 patients were intra-articularly injected with PRP three times with two weeks interval. In the second
group, 108 patients were injected with three intra-articular injections of hyaluronic acid with two weeks interval. The patients age and sex
were comparable in both groups. In the PRP group, the mean of follow up was 30.34 months, while in the hyaluronic injection group, it was
28.886 months.
Results: At the end of follow, in the PRP group, 85 patients (73.3%) had satisfactory results, while 31 patients (26.7%) had unsatisfactory.
The mean International Knee Documentation Committee score (IKDC) before injection was 53.747 5.089 points, while at the end of follow
up, it was 78.336 7.676 points. In the hyaluronic group, 22 patients (20.4%) had fair results and 86 patients (79.6%) had poor results. The
mean IKDC score before the injection was 53.787 5.45 points, while at the end of follow up it was 56.36 6.92 points. No complications
were encountered during this study.
Conclusion: Intraarticular injections of PRP are safe, may be useful with long term effect in the treatment of early osteoarthritis knee.
The patients age and body weight has a significant effect on the final results.
Keywords: Platelet rich plasma; Knee osteoarthritis; Intra-articular injection; Hyaluronic acid
Introduction
Primary osteoarthritis (OA) of the knee can be defined as a
process in which articular degeneration occurs in the absence
of an obvious underlying abnormality [1]. The typical joints
involved with primary osteoarthritis include the large, weightbearing joints such as the hip and knee, as well as selected
smaller joints in the hands, feet, and spine [2].
Primary OA knee is considered one of the most disabling
orthopaedic problems in the middle age group. The problem
is more evident in countries using kneeling in their religious
traditions.
A variety of agents, such as nonsteroidal anti-inflammatory
drugs, glucosamine, chondroitin-sulphate, hyaluronic acid, and
glucocorticoids have been proposed as non invasive solutions
for pain treatment, improvement in function, and disability, and
Ortho & Rheum Open Access J 1(5): OROAJ.MS.ID.55574 (2015)
ultimately modification of severe chondoral degeneration and
osteoarthritis with varying success rates [3].
Hyaluronic acid (HA) produced by synoviocytes, fibroblasts
and chondrocytes, is the major chemical component of synovial
fluid. It is essential for the viscoelastic properties of the fluid
because of high viscosity, and has a protective effect on articular
cartilage and soft tissue surfaces of joints [4].
In OA, the concentration and the molecular weight of HA
are reduced, resulting in synovial fluid of lower elasticity and
viscosity [5]. When the viscoelasticity of synovial fluid is reduced,
the transmission of mechanical force to cartilage may increase
its susceptibility to mechanical damage [6]. Treatment of knee
OA with local injection of hyaluronic acid has been approved by
the FDA, due to its superiority to placebo and other conservative
treatments [7].
001
Orthopedics and Rheumatology Open Access Journal
Platelet-rich plasma (PRP) is a natural concentrate of
autologous growth factors from the blood [8]. The method is
simple, low cost, and minimally invasive [8]. Autologous PRP
is a volume of plasma having a platelet concentration above
normative baseline values [9]. Platelets were thought to act
solely in the clotting process. However, in addition to local
hemostasis at sites of vascular injury, platelets contain an
abundance of growth factors and cytokines that are crucial in
soft tissue healing and bone mineralization [10].
PRP therapy provides delivery of a highly concentrated
cocktail of growth factors to accelerate healing [11]. Plateletderived growth factor, transforming growth factor, vascular
endothelial growth factor, epithelial growth factor and
insulin-like growth factor (IGF) were found in large amounts
[11-13]. Transforming growth factor beta is active during
inflammation, and influences the regulation of cellular migration
and proliferation and stimulates cell replication [11,12].
Transforming growth factor -2 present in PRP has been
associated with chondrogenesis in cartilage repair [13].
The Authors performed this comparative study with the
hypothesis that intraarticular administration of PRP could
improve function and decrease pain in patients suffering from
knee osteoarthritis.
Material and Methods
From August 2010 to August 2013, a comparative
randomized clinical study was performed on two groups of
patients. In the first group, three intra-articular knee injection
of PRP; with two weeks interval; were given to 162 patients
with osteoarthritis knee grade I and grade II according to the
grading system of Kellgren and Lawrence [14]. During the study
46 patients were lost and did not show during follow up. At the
end of follow up period 116 patients included in this study. The
patients age ranged from 45 to 60 years with a mean of 50.93
years. Seventy two patients were females while 44 patients were
males. The right side was affected in 75 patients while the left
side was affected in 41 patients. The follow up period ranged
from 24 to 36 months from the first injection with a mean of
30.026 months (Table 1).
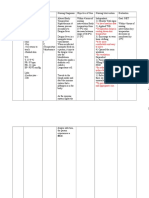
Table 1: Pre-injection clinical data.
Pre-Injection Data
1- Age
2- Sex
3- Side affected
4- Osteoarthritis
grading
002
PRP group
Range 45 y. to 60y.
(Mean 50.93 y.).
72 Females 44
Males.
Hyaluronic Acid
Group
Range 45 y. to 60y.
(Mean 50.87 y.).
75 Females 33
Males.
Right side (75) Left
Right side (68) Left
64 patients Grade II.
58 patients Grade II.
side (41).
52 patients Grade I
side (40).
50 patients Grade I
The second group includes 157 patients with knee
osteoarthritis (grade I and grade II). In these patients three
intra-articular injections of hyaluronic acid; with two weeks
interval; were given in their knees. During the study 49 patients
were lost and did not show during follow up. At the end of follow
up period 108 patients included in this study. The patients age
ranged from 45 to 60 years old with a mean of 50.87 years.
Seventy five were females and 33 were males. The right side
was affected in 68 patients while the left side was affected in
40 patients. The follow up period ranged from 24 to 36 months
from the first injection with a mean of 28.886 months (Table 1).
Selection to perform which procedure was done blindly
without any patients or authors preference. Informed
consent was taken from every participant in this study after
full description of the whole procedures with their benefits
and hazards. All patients signed this consent without any
obligation. The procedures followed were in accordance with
the ethical standards of the responsible committee on human
experimentation.
The inclusion criteria were patients with primary
osteoarthritis knee grade I and grade II after failure of medical
treatment for at least 3 months. The exclusion criteria are
secondary osteoarthritis, grade III or more primary osteoarthritis,
history of previous steroid injection, active infection elsewhere,
patients with blood diseases like thrombocytopenia or patients
receiving any anticoagulant medications.
Secondary OA was excluded after careful evaluation of all
factors that could lead to OA by careful history taking, clinical
examination, as well as laboratory and radiological investigation.
Patients presented with knee effusion were also excluded
temporary till the effusion resolved by rest, medications and
remained as such for one month. The patients in the pre-injection
condition were classified according to the grading system of
Kellgen & Lawrence [14] into: Grade I and Grade II.
In the first group of patients (PRP group)
Under complete aseptic technique; about 30 ml. venous
blood was collected in aseptic tube containing 5 ml of sodium
citrate from every patient treated. Then two centrifugations
(the first at 1,800 rpm. for 15 min. to separate erythrocytes, and
the second at 3,200 rpm. for 10 min. to concentrate platelet)
produced a unit of about 6 ml. of PRP.
One ml. of PRP was sent to the laboratory for analysis of
platelet concentration, bacteriological test and quality test while
the remaining (5 ml.) was used for intra-articular injection
within 2 h. The total number of platelets in the injected PRP has
an average of 5.3 millions (ranged from 4.7 to 6.2 millions).
Before the injection, one ml. of 10% Ca chloride was added to
the 5 ml. PRP (one unit) to activate platelets. The whole procedure
was repeated after two weeks for the second set of injection and
after another two weeks for the third set of injection.
How to cite this article: Osama A S, Hassam M G. Intraarticular Injection of Platelet Rich Plasma (PRP) and Hyaluronic Acid (HA) in Early Knee
Osteoarthritis. Ortho & Rheum Open Access J. 2015; 1(5): 555574. DOI: 10.19080/OROAJ.2015.01.555574
Orthopedics and Rheumatology Open Access Journal
The skin was sterilely dressed and the injection was
performed through a classic lateral approach with the help of C
arm Image in obese patients followed by flexion and extension
of the knee few times, to allow the PRP to distribute itself
throughout the joint. After the injection, the patients were sent
home with instructions to limit the use of the leg for at least 24
hours and to use cold ice on the knee for pain. The use of nonsteroidal medication was not allowed.
hyaluronic group, 29 patients (26.9%) had excellent results, 39
patients (36.1%) had good results, 27 patients (25%) had fair
results and 13 patients (12%) had poor results. The mean IKDC
score for the first group was 72.81 9.42 ranged from 45 to 86
points. While the mean IKDC score for the second group was
75.35 9.06 ranged from 53 to 88 points. The difference was
found to be statistically significant in favor of HA injection (P =
0.0407) (Table 2).
Three intra-articular injection of hyaluronic acid
(concentration) with two weeks interval between each injection
was performed in their knees. The injections were performed
under complete aseptic technique with the help of C arm image
intensifier in obese patients.
And according to the IKDC scoring system; 28 patients
(24.1%) had excellent results, 53 patients (45.7%) had good
results, 24 patients (20.7%) had fair results and 11 patients
(9.5%) had poor results in the PRP group. While in the hyaluronic
group, 20 patients (18.5%) had good results, 51 patients (47.2%)
had fair results, and 37 patients (34.3%) had poor results. The
mean IKDC score for the first group was 75.38 8.795 ranged
from 51 to 86 points. While the mean IKDC score for the second
group was 68.14 7.75 ranged from 50 to 79 points. The
difference was found to be statistically highly significant in favor
of PRP injection (P < 0.0001) (Table 2).
In the second group of patients
International Knee Documentation Committee score (IKDC)
[15] was used to evaluate the patients clinically after 3 months,
after one year and at the end of this study. Patients were asked
to make post-injection X-ray after 6, 12, 18, 24 and 30 months.
The changes present on X-rays were recorded and compared
with previous x-rays. The data collected from this study were
statistically analyzed using the mean (average), standard
deviation, and T test.
Results
After 3 months from the first injection
In PRP group, and according to the IKDC scoring system;
24 patients (20.7%) had excellent results, 45 patients (38.8%)
had good results, 34 patients (29.3%) had fair results and 13
patients (11.2%) had poor results in the PRP group. While in the
After one year from the first injection
At the end of follow up
And according to IKDC scoring system; 30 patients (25.9%)
had excellent results, 55 patients (47.4%) had good results, 23
patients (19.8%) had fair results and 8 patients (6.9%) had
poor results in the PRP group. While in the hyaluronic group,
22 patients (20.4%) had fair results and 86 patients (79.6%)
had poor results. The difference was found to be statistically
significant (P < 0.0001) (Table 2).
Table 2: The Functional results after 3 months, after one year and at the end of follow up period.
F o l l o w
p/Group
PRP group
HA group
Total
After 3 months
Sat.
Unsat.
Total
68
40
108
69
137
Sat. means Satisfactory
Unsat. means Unsatisfactory.
47
87
After one year
IKDC
Sat.
Unsat.
Total
75.359.06
20
88
108
116
72.819.42
224
74.089.24
81
101
35
123
116
224
At the end of follow up
IKDC
Sat.
Unsat.
Total
68.147.75
108
108
75.38 .79
71.76 .27
85
85
31
138
IKDC
116
78.347.67
224
67.357.29
56.366.92
After three months, the difference was found to be statistically significant in favor of HA group (P = 0.0407).
After one year, the difference was found to be statistically significant in favor of PRP group (P = 0.0001).
At the end of follow up period, the difference was found to be statistically significant in favor of PRP group (P = 0.0001).
In the PRP group and at the end of follow up period, the
mean IKDC score before injection was 53.715 5.0715 points
ranged from 41 to 64 points. The mean IKDC score at the end of
follow up period was 78.336 points 7.676 ranged from 52 to
88 points. A statistically significant improvement of all clinical
scores was obtained from the basal evaluation (Table 2).
003
In the hyaluronic group the mean IKDC score before the
injection was 53.787 5.45 ranged from 44 to 64 points, while
at the end of follow up period the mean IKDC score after the
injection was 56.36 6.92 ranged from 42 to 68 points. Most of
the patients returned to the pre-injection level of activity or even
got worse functional activity level.
How to cite this article: Osama A S, Hassam M G. Intraarticular Injection of Platelet Rich Plasma (PRP) and Hyaluronic Acid (HA) in Early Knee
Osteoarthritis. Ortho & Rheum Open Access J. 2015; 1(5): 555574. DOI: 10.19080/OROAJ.2015.01.555574
Orthopedics and Rheumatology Open Access Journal
At the end of follow up period, 38 patients (73.07%) out
of 52 patients with grade I knee osteoarthritis had satisfactory
IKDC score after PRP injection with a mean of 79.269 points.
While 47 patients (73.43%) out of 64 patients with grade II knee
osteoarthritis had satisfactory IKDC score after PRP injection
with a mean of 77.89 points. The difference was found to be
statistically insignificant (P = 0.33).
Forty four patients (78.57%) out of 56 patients complaining
of knee osteoarthritis less than 3 years had satisfactory IKDC
functional results after PRP injection with a mean of 80.41 points.
While 41 patients (68.33%) out of 60 patients complaining more
than 3 years had satisfactory IKDC score after PRP injection
with a mean of 76.35 points. The difference was found to be
statistically significant (P = 0.004) (Table 3).
Table 3: The relation between the age, body weight, and duration of complaint with the functional outcome at the end of follow up period in the
PRP group.
Age
Body Weight
Duration of Complaint
Group
Sat.
Unsat.
IKDC
Group
Sat.
Unsat.
IKDC
Group
Sat.
Unsat.
IKDC
<50 years
46
81.85.51
<90 Kg.
48
81.925.49
<3 years
44
12
80.416.31
Total
85
116
Total
85
31
116
Total
85
31
116
50 years
39
Sat. means Satisfactory
27
31
75.658.04
90 Kg.
37
26
75.277.99
3 years
41
19
76.358.33
Unsat. means Unsatisfactory
As regard to the age, the difference was found to be statistically significant (P < 0.0001).
As regard to the body weight, the difference was found to be statistically significant (P < 0.0001).
As regard to the duration of complaint, the difference was found to be statistically significant (P = 0.004).
Forty six patients (92%) out of fifty patients below 50 years
old had satisfactory IKDC functional results after PRP injection
with a mean of 81.84. While 39 patients (59.09%) out of 66
patients above 50 years old had satisfactory IKDC score after
PRP injection with a mean of 75.6515 points. The difference was
found to be statistically significant (P < 0.0001) (Table 3).
Forty eight patients (90.56%) out of 53 patients less than 90
kg had satisfactory IKDC functional results after PRP injection
with a mean of 81.924 points, while 37 patients (58.73%) out of
63 patients above 90 kg had satisfactory IKDC functional results
after PRP injection with a mean of 75.269 points. The difference
was found to be statistically significant (P < 0.0001) (Table 3).
There were no complications met with in this study. Most of
the patients (88 patients) complained of mild to moderate knee
pain for 2 to 3 days after the injection. Rest and ice application
were successful in relieving most of that pain. No cases of
intraarticular knee infection happened during this study.
Discussion
Most of the studies on autologous PRP injection have been
focused on the reduction of pain and improvement of function
over time [16,17]. Hyaluronic acid injection trials generally
report positive effects on pain and function scores compared
to placebo [6]. However, the evidence on clinical benefit is
uncertain, due to variable trial quality, potential publication
bias, and unclear clinical significance of the changes reported.
Platelet rich plasma may lead to proliferation of autologous
chondrocytes and mesenchymal stem cells [13,17]. Increased
004
hyaluronic acid secretion has also been noted in the presence
of platelet rich rather than platelet poor preparation [18,19].
Osteoarthritic chondrocytes showed; after Platelet rich plasma
injection; less interleukin-1 -induced inhibition of collagen 2
and aggrecan gene expression and diminished nuclear factor-B
activation, which are the pathways involved in osteoarthritis
pathogenesis [9,19].
Wang-Saegusa et al. [20] reported improvement of Western
Ontario and McMaster Universities score (WOMAC) at the
6-month follow-up in 261 patients with OA symptoms who
had three intraarticular injection of PRP. An improvement was
documented in 192 of 261 patients (73.5%). Filardo et al. [21]
reported improvement in International Knee Documentation
Committee (IKDC) in 72 patients out of 90 patients two years
after three intraarticular injection of PRP. Kon et al. [22]
reported that intra-articular PRP injection in 100 patients with
chronic degenerative condition of the knee had positive effects
on improving pain and quality of life and on the scores of IKDC
at the 1-year follow-up.
In this study, the maximal improvement in the hyaluronic
injection group was after 3 months from the first injection.
However the improvement was dramatically decreased after
that until it became near the base line or even worse at the end
of follow up period.
While in the PRP group; 85 patients (73.4%) had satisfactory
IKDC score while 31 patients (26.6%) had unsatisfactory IKDC
score after three knee intra-articular PRP injection. The mean
IKDC score before injection was 53.747 points 5.089 points
How to cite this article: Osama A S, Hassam M G. Intraarticular Injection of Platelet Rich Plasma (PRP) and Hyaluronic Acid (HA) in Early Knee
Osteoarthritis. Ortho & Rheum Open Access J. 2015; 1(5): 555574. DOI: 10.19080/OROAJ.2015.01.555574
Orthopedics and Rheumatology Open Access Journal
ranged from 41 to 64 points. The mean IKDC score at the end
of follow up period was 78.46 points 5.925 ranged from 52 to
88 points.
In the PRP injection group, the number of unsatisfactory
IKDC score was high (31 patients), but most of them were in the
fair result group and have considerable improvement of their
score with improvement of their activity level. Most of them felt
that they perform better and more activity than before and some
of them stop using NASIDs. Six patients continue using NASIDs at
the end of follow up period.
Conclusion
At the end of follow up period and in the PRP injection
group, patients with grade I osteoarthritis has better IKDC score
than patients with grade II but with no statistically significant
difference. In the PRP injection group, patients with less than
3 years complaint, patients less than 50 years old and patients
weighing less than 90 kg had better IKDC score than patients
more than 3 years complaint, patients more than 50 years old
and patients weighing more than 90 kg and the difference was
found to be statistically significant.
At the end of follow up period and in both study groups,
there were no or little radiological changes between the first
and last knee x rays. The radiological changes in grade I and
grade II osteoarthritis before the injection were minimal and the
expected radiological changes after the improvement were hard
to detect. MRI study could be included in future authors studies
with special concern about the cost demand in our country.
Cerza et al. [23] found that, treatment with PRP showed a
significantly better clinical outcome than did treatment with
HA, with sustained lower WOMAC scores. Guler et al. [24] in a
comparative study between PRP and Hyaluronic acid injection
concluded that PRP appears to be an appropriate option for
intraarticular treatment in patients with early-stage knee
osteoarthritis.
The results obtained from his short-term are encouraging
and indicate that treatment with autologous PRP intraarticular
injections is safe, and may be useful for the treatment of early
degenerative articular pathology of the knee, aiming to reduce
pain and improve knee function and quality of life. Also a large
number of patients (86.2% of patients) after improvement
stopped using NASIDs with their side effects. Long term
randomized controlled placebo studies are needed for firm
and conclusive evaluation of this method of treatment in
osteoarthritis.
References
1. Mandelbaum B, Waddell D (2005) Etiology and pathophysiology of
osteoarthritis. Orthopedics 28(2 Suppl): s207-s214.
2. Samson DJ, Grant MD, Ratko TA, Bonnell CJ, Ziegler KM, et al. (2007)
Treatment of Primary and Secondary Osteoarthritis of the Knee.
Evid Rep Technol Assess (Full Rep) (157): 1-157.
005
3. Hayami T (2008) Osteoarthritis of the knee joint as a cause of
musculoskeletal ambulation disability symptom complex (MADS).
Clin Calcium 18(11): 1574-1580.
4. Abate M, Pulcini D, Di Iorio A, Schiavone C (2010)
Viscosupplementation with intra-articular hyaluronic acid for
treatment of osteoarthritis in the elderly. Curr Pharm Des 16(6):
631-640.
5. ORegan M, Martini I, Crescenzi F, De Luca C, Lansing M (1994)
Molecular mechanisms and genetics of hyaluronan biosynthesis. Int
J Biol Macromol 16(6): 283-286.
6. Brandt KD, Block JA, Michalski JP, Moreland LW, Caldwell JR, et al.
(2001) Efficacy and safety of intraarticular sodium hyaluronate in
knee osteoarthritis. ORTHOVISC Study Group. Clin Orthop Relat Res
(385): 130-143.
7. Colen S, van den Bekerom MP, Mulier M, Haverkamp D (2012)
Hyaluronic acid in the treatment of knee osteoarthritis: a systematic
review and meta-analysis with emphasis on the efficacy of different
products. BioDrugs 26(4): 257-268.
8. Anitua E, Andia I, Ardanza B, Nurden P,Nurden AT (2004) Autologous
platelets as a source of proteins for healing and tissue regeneration.
Thromb Haemost 91(1): 4-15.
9. Pietrzak WS, Eppley BL (2005) Platelet rich plasma: Biology and
new technology. J Craniofac Surg 16(6): 1043-1054.
10. Anitua E, Sanchez M, Nurden AT, Nurden P, Orive G,et al. (2006) New
insights into and novel applications for platelet-rich fibrin therapies.
Trends Biotechnol 24(5): 227-234.
11. Sampson S, Gerhardt M, Mandelaum B (2008) Platelet rich plasma
injection grafts for musculoskeletal injuries: A review. Curr Rev
Musculoskelet Med 1(3-4): 165-174.
12. Mazzocca AD, McCarthy MB, Chowaniec DM, Cote MP, Romeo AA,
et al. (2012) Platelet rich plasma differs according to preparation
method and human variability. J bone joint Sug 94A(4): 308-316.
13. Burnouf T, Goubran HA, Ou KL, Chen TM, Radosevic M, et al.
(2013) Blood derived biomaterials and platelet growth factors in
regenerative medicine. Blood Rev 27(2): 77-89.
14. Kellgren JH, Lawrence JS (1957) Radiological assessment of
osteoarthritis. Ann Rheum 16(4): 494-501.
15. Higgins LD, Taylor MK, Park D, Ghodadra N, Marchant M, et al. (2007)
Reliability and validity of the International Knee Documentation
Committee (IKDC) Subjective Knee Form. Joint Bone Spine 74(6):
594-599.
16. Gobbi A, Karnatzikos G, Mahajan V, Malchira S (2012) Platelet-rich
plasma treatment in symptomatic patients with knee osteoarthritis:
preliminary results in a group of active patients. Sports Health 4(2):
162-172.
17. Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A (2013) Treatment
with platelet-rich plasma is more effective than placebo for knee
osteoarthritis: a prospective, double-blind, randomized trial. Am J
Sports Med 41(2): 356-364.
18. Halpren B, Chaudhury S, Rodeo SA, Hayter C, Bogner E, et al. (2013)
Clinical and MRI outcomes after platelet rich plasma treatment for
knee osteoarthritis. Clin J Sport Med 23(3): 238-239.
19. Andia I, Abate M (2013) Platelet rich plasma: underlying biology and
clinical correlates. Regen Med 8(5): 645-658.
20. Wang-Saegusa A, Cugat R, Ares O, Seijas R, Cusco X, et al. (2011)
Infiltration of plasma rich in growth factors for osteoarthritis of the
knee short-term effects on function and quality of life. Arch Orthop
Trauma Surg 131(3): 311-317.
How to cite this article: Osama A S, Hassam M G. Intraarticular Injection of Platelet Rich Plasma (PRP) and Hyaluronic Acid (HA) in Early Knee
Osteoarthritis. Ortho & Rheum Open Access J. 2015; 1(5): 555574. DOI: 10.19080/OROAJ.2015.01.555574
Orthopedics and Rheumatology Open Access Journal
21. Filardo G, Kon E, Buda R, Timoncini A, Di Martino A, et al. (2011)
Platelet-rich plasma intra-articular knee injections for the treatment
of degenerative cartilage lesions and osteoarthritis. Knee Surg
Sports Traumatol Arthrosc 19(4): 528-535.
22. Kon E, Buda R, Filardo G, Di Martino A, Timoncini A, et al. (2010)
Platelet-rich plasma: intra-articular knee injections produced
favorable results on degenerative cartilage lesions. Knee Surg Sports
Traumatol Arthrosc 18(4): 472-479.
006
23. Cerza F,Carn S, Carcangiu A, Di Vavo I, Schiavilla V, et al. (2012)
Comparison between hyaluronic acid and platelet-rich plasma,
intra-articular infiltration in the treatment of gonarthrosis. Am J
Sports Med 40(12): 2822-2827.
24. Guler O, Mutlu S, Isyar M, Seker A, Kayaalp ME, et al. (2015)
Comparison of short-term results of intraarticular platelet-rich
plasma (PRP) and hyaluronic acid treatments in early-stage
gonarthrosis patients. Eur J Orthop Surg Traumatol 25(3): 509-513.
How to cite this article: Osama A S, Hassam M G. Intraarticular Injection of Platelet Rich Plasma (PRP) and Hyaluronic Acid (HA) in Early Knee
Osteoarthritis. Ortho & Rheum Open Access J. 2015; 1(5): 555574. DOI: 10.19080/OROAJ.2015.01.555574
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- THE PHOENIX PROJECT: Mind ControlDokumen63 halamanTHE PHOENIX PROJECT: Mind Controldaerie1661100% (1)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Dissociative Identity Disorder (Multiple Personality Disorder) - Psychology TodayDokumen3 halamanDissociative Identity Disorder (Multiple Personality Disorder) - Psychology TodayIrzaBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Professional Plaquex InfoDokumen48 halamanProfessional Plaquex Infoamelia rumenta100% (1)
- Blood TransfusionDokumen38 halamanBlood TransfusiontorkBelum ada peringkat
- Bedroom Routine Tip SheetDokumen2 halamanBedroom Routine Tip SheetPatricia BarbosaBelum ada peringkat
- Proliferation Therapy for Tendon and Ligament InjuriesDokumen18 halamanProliferation Therapy for Tendon and Ligament InjuriesJason Tutt GinBelum ada peringkat
- DENGUE CS NCP 1Dokumen8 halamanDENGUE CS NCP 1Karyl SaavedraBelum ada peringkat
- Jung at HeartDokumen8 halamanJung at Heartsorensen1Belum ada peringkat
- Values and PsychotherapyDokumen17 halamanValues and PsychotherapyMariana KaratepeBelum ada peringkat
- 65 Year Old Man with Severe Ear Pain and SwellingDokumen9 halaman65 Year Old Man with Severe Ear Pain and SwellingJoe RealBelum ada peringkat
- Handout 2 Case StudiesDokumen5 halamanHandout 2 Case StudiesKumutha ShiniBelum ada peringkat
- Consent Crown Bridge Pros The TicsDokumen2 halamanConsent Crown Bridge Pros The TicsHussein A.hamadBelum ada peringkat
- DOH NCP - Pulmonary Tuberculosis LectureDokumen19 halamanDOH NCP - Pulmonary Tuberculosis LectureCarlaMonicaRubio0% (1)
- Critical Limb Ischemia Treatment Strategies in Diabetics: Present Deeds and Future ChallengesDokumen5 halamanCritical Limb Ischemia Treatment Strategies in Diabetics: Present Deeds and Future ChallengesJuniper PublishersBelum ada peringkat
- In The Era of Budgetary Constraints, Cost-Effective Management of Metabolic Syndrome, Type 2 Diabetes, and Obesity Is EssentialDokumen6 halamanIn The Era of Budgetary Constraints, Cost-Effective Management of Metabolic Syndrome, Type 2 Diabetes, and Obesity Is EssentialJuniper PublishersBelum ada peringkat
- Lifestyle and DiabesityDokumen1 halamanLifestyle and DiabesityJuniper PublishersBelum ada peringkat
- DiabesityDokumen1 halamanDiabesityJuniper PublishersBelum ada peringkat
- Value of Urocortin As A Marker For Preterm LaborDokumen7 halamanValue of Urocortin As A Marker For Preterm LaborJuniper Publishers100% (1)
- Experience and Knowledge of Female Genital Mutilation Amongst London Obstetrics and Gynaecology TraineesDokumen4 halamanExperience and Knowledge of Female Genital Mutilation Amongst London Obstetrics and Gynaecology TraineesJuniper PublishersBelum ada peringkat
- The Hidden EctopicDokumen2 halamanThe Hidden EctopicJuniper PublishersBelum ada peringkat
- Safety and Efficacy of Yoga and Naturopathy Based Lifestyle in Patients Suffering From Rheumatoid ArthritisDokumen5 halamanSafety and Efficacy of Yoga and Naturopathy Based Lifestyle in Patients Suffering From Rheumatoid ArthritisJuniper PublishersBelum ada peringkat
- Type 2 Diabetic Patients On Insulin Can Reduce or Eliminate Insulin With Lifestyle Change and Carbohydrate RestrictionDokumen5 halamanType 2 Diabetic Patients On Insulin Can Reduce or Eliminate Insulin With Lifestyle Change and Carbohydrate RestrictionJuniper PublishersBelum ada peringkat
- Use of Semen Quality To Predict Pregnancy in Couples Undergoing ICSIDokumen4 halamanUse of Semen Quality To Predict Pregnancy in Couples Undergoing ICSIJuniper PublishersBelum ada peringkat
- Infertility Awareness Among UK University StudentsDokumen9 halamanInfertility Awareness Among UK University StudentsJuniper PublishersBelum ada peringkat
- Endometrial Cancer Treatment: New Insights Into The Role of Erbb ReceptorsDokumen3 halamanEndometrial Cancer Treatment: New Insights Into The Role of Erbb ReceptorsJuniper PublishersBelum ada peringkat
- Energy Balance in Modern Agroecosystems Why and How?Dokumen4 halamanEnergy Balance in Modern Agroecosystems Why and How?Juniper PublishersBelum ada peringkat
- Arsenic Pollution in Agriculture: Its Uptake and Metabolism in Plant SystemDokumen5 halamanArsenic Pollution in Agriculture: Its Uptake and Metabolism in Plant SystemJuniper PublishersBelum ada peringkat
- Rural Composting For Improvement of Soil Health and Sustainable AgricultureDokumen8 halamanRural Composting For Improvement of Soil Health and Sustainable AgricultureJuniper PublishersBelum ada peringkat
- Portal Venous Gas in A Patient With End-Stage Renal DiseaseDokumen4 halamanPortal Venous Gas in A Patient With End-Stage Renal DiseaseJuniper PublishersBelum ada peringkat
- Diagnostic Performance of Magnetic Resonance Imaging in The Pretreatment Evaluation of Invasive Cervical CarcinomaDokumen7 halamanDiagnostic Performance of Magnetic Resonance Imaging in The Pretreatment Evaluation of Invasive Cervical CarcinomaJuniper PublishersBelum ada peringkat
- Unusual Clinical Presentation of Congenital Malaria: Cholestasis in NewbornDokumen3 halamanUnusual Clinical Presentation of Congenital Malaria: Cholestasis in NewbornJuniper PublishersBelum ada peringkat
- Six Million Ways of Science CommunicationDokumen2 halamanSix Million Ways of Science CommunicationJuniper PublishersBelum ada peringkat
- Quantifying The Trade Effects of Sanitary and Phytosanitary Regulations of The Eu On Sudan's Groundnuts ExportsDokumen9 halamanQuantifying The Trade Effects of Sanitary and Phytosanitary Regulations of The Eu On Sudan's Groundnuts ExportsJuniper PublishersBelum ada peringkat
- Evaluation of Human Epidermal Growth Factor As A Tumor Marker in Patients With Hepatocellular Carcinoma Related To Hepatitis C VirusDokumen5 halamanEvaluation of Human Epidermal Growth Factor As A Tumor Marker in Patients With Hepatocellular Carcinoma Related To Hepatitis C VirusJuniper PublishersBelum ada peringkat
- Robotic by Pass Made SimpleDokumen1 halamanRobotic by Pass Made SimpleJuniper PublishersBelum ada peringkat
- Effect of Quercus Cortex Extract With Alum For Bacterial Metritis and Vaginitis Treatment in Different Ages in CowsDokumen5 halamanEffect of Quercus Cortex Extract With Alum For Bacterial Metritis and Vaginitis Treatment in Different Ages in CowsJuniper PublishersBelum ada peringkat
- Ogilvie's Syndrome Complicating A Hemorrhagic Stroke of BrainstemDokumen3 halamanOgilvie's Syndrome Complicating A Hemorrhagic Stroke of BrainstemJuniper PublishersBelum ada peringkat
- Transient Elastography is superior to the FIB 4 Index, Aspartate Platelet Ratio Index, Aspartate Alanine Aminotransferase Ratio, Age Platelet Index and Fibrosis Index in Diagnosing Fibrosis in Chronic Hepatitis B PatientsDokumen17 halamanTransient Elastography is superior to the FIB 4 Index, Aspartate Platelet Ratio Index, Aspartate Alanine Aminotransferase Ratio, Age Platelet Index and Fibrosis Index in Diagnosing Fibrosis in Chronic Hepatitis B PatientsJuniper PublishersBelum ada peringkat
- Serum Serotonin As A Novel Marker For Hepatocellular CarcinomaDokumen7 halamanSerum Serotonin As A Novel Marker For Hepatocellular CarcinomaJuniper PublishersBelum ada peringkat
- Hepatic Artery Thrombosis After Orthotopic Liver TransplantationDokumen4 halamanHepatic Artery Thrombosis After Orthotopic Liver TransplantationJuniper PublishersBelum ada peringkat
- A Randomized Comparative Study of Efficacy of Lamivudine and Adefovir Combination Versus Tenofovir Versus Entecavir in Decompensated Cirrhotic Patients of Hepatitis BDokumen5 halamanA Randomized Comparative Study of Efficacy of Lamivudine and Adefovir Combination Versus Tenofovir Versus Entecavir in Decompensated Cirrhotic Patients of Hepatitis BJuniper PublishersBelum ada peringkat
- Quality and Complications of Colonoscopy in Ahvaz Jundishapur UniversityDokumen4 halamanQuality and Complications of Colonoscopy in Ahvaz Jundishapur UniversityJuniper PublishersBelum ada peringkat
- DysfagiaDokumen4 halamanDysfagiaVarvara MarkoulakiBelum ada peringkat
- Hildegard PeplauDokumen8 halamanHildegard PeplauNeven BuhinBelum ada peringkat
- Tube Thoracostomy GuideDokumen47 halamanTube Thoracostomy GuideleizelgalvezBelum ada peringkat
- InglesDokumen34 halamanInglesGabriel Peguero100% (1)
- Peritonsillar Abscess DrainageDokumen4 halamanPeritonsillar Abscess Drainagesyibz100% (1)
- Nurse's Study Guide To BurnsDokumen14 halamanNurse's Study Guide To BurnsCassie GonzalezBelum ada peringkat
- Gastritis DDDokumen78 halamanGastritis DDsotoshaBelum ada peringkat
- CBT Feminist TheoryDokumen7 halamanCBT Feminist TheoryAvalon LearningBelum ada peringkat
- Crisis Intervention HMWK 1Dokumen3 halamanCrisis Intervention HMWK 1Janeth GmBelum ada peringkat
- revision 復健科Dokumen4 halamanrevision 復健科屏頂大Belum ada peringkat
- A Logical Framework For Functional Analytic Group TherapyDokumen9 halamanA Logical Framework For Functional Analytic Group TherapyMaría Emilia Schultz100% (1)
- Emilio Aguinaldo College City of Dasmariñas, Cavite: Senior High SchoolDokumen7 halamanEmilio Aguinaldo College City of Dasmariñas, Cavite: Senior High SchoolNicole De AsisBelum ada peringkat
- Dr.P.Udhaya Kumar MD - PM&R 1st Year PG Department of PM&R Moderator Dr.S.Chidambaranathan Department of PaediatricsDokumen45 halamanDr.P.Udhaya Kumar MD - PM&R 1st Year PG Department of PM&R Moderator Dr.S.Chidambaranathan Department of PaediatricsUdhaya KumarBelum ada peringkat
- PT - PR 9996666 OccupiedDokumen107 halamanPT - PR 9996666 OccupiedBelal AhmedBelum ada peringkat
- TCCC Guidelines August 2011Dokumen12 halamanTCCC Guidelines August 2011OnTheXBelum ada peringkat
- PulmonaryUpdate: New Definitions and Diagnoses in Interstitial PneumoniaDokumen8 halamanPulmonaryUpdate: New Definitions and Diagnoses in Interstitial Pneumoniaade hajizah br ritongaBelum ada peringkat
- 35 Drugs Used DyslipidemiaDokumen58 halaman35 Drugs Used DyslipidemiaNibshian Dela RosaBelum ada peringkat