Keracunan Karbonmonoksida
Diunggah oleh
Cita ChotimahJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Keracunan Karbonmonoksida
Diunggah oleh
Cita ChotimahHak Cipta:
Format Tersedia
Cases Journal
BioMed Central
Open Access
Case Report
Acute carbon monoxide poisoning with severe cardiopulmonary
compromise: a case report
Chang-Teng Wu*, Jing-Long Huang and Shao-Hsuan Hsia
Address: Department of Pediatrics, Children Medical Center, Chang Gung Memorial Hospital, Chang Gung University College of Medicine,
Tauyuan, Taiwan
Email: Chang-Teng Wu* - wct0722@yahoo.com.tw; Jing-Long Huang - long@adm.cgmh.org.tw; Shao-Hsuan Hsia - shsia@adm.cgmh.org.tw
* Corresponding author
Published: 14 January 2009
Cases Journal 2009, 2:52
doi:10.1186/1757-1626-2-52
Received: 25 December 2008
Accepted: 14 January 2009
This article is available from: http://www.casesjournal.com/content/2/1/52
2009 Wu et al; licensee BioMed Central Ltd.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0),
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction: Carbon monoxide (CO) is a colorless, odorless gas produced as a by-product of
incomplete combustion, and a common source is the fuel used for heating water in homes. The
clinical presentation of CO poisoning may be mild, moderate, or severe.
Case presentation: This paper describes carbon monoxide (CO) poisoning in a 15-year-old child
who suffered from severe cardiopulmonary compromise without overt neuropsychiatric sequelae.
This occurred after he was exposed to a home heater producing high levels of carbon monoxide
for an estimated six to eight hours. CO-induced cardiopulmonary compromise is infrequent in
children.
Conclusion: In this case, prolonged exposure to CO resulted in a high carboxyhemoglobin
(COHb) concentration, but the child recovered without overt sequelae, despite severe
cardiopulmonary compromise.
Introduction
Carbon monoxide (CO) is a colorless, odorless gas produced as a by-product of incomplete combustion. The
clinical presentation of CO poisoning may be mild, moderate, or severe. The most frequently documented complications are persistent or delayed neuropsychiatric
sequelae, including dementia, amnestic syndromes, psychosis, and Parkinsonism. These symptoms may be preceded by a lucid period of 240 days after the initial
exposure [1]. The heart is extremely susceptible to COinduced hypoxia, due to its high oxygen demand. Cardiac
involvement manifests mainly as ischemic insult, with
elevated enzyme levels and ECG changes ranging from STsegment depression to transmural infarction. Conduction
abnormalities, atrial fibrillation, prolonged QT interval
[2] and ventricular arrhythmia have been demonstrated.
There have been few studies of CO-induced cardiopulmonary compromise in children. We report a case of severe
cardiopulmonary compromise without overt neuropsychiatric sequelae in a 15-year-old boy. Since such cases are
rare in the pediatric literature, the clinical presentation
and management are discussed here.
Case presentation
This 15-year-old boy was found at home with reduced
consciousness at about 6:30 am on 25 June 2008 According to his parents' statement, he had slept in his room,
which is next to the room containing the home water
heater. His father had taken a bath at 11:00 p.m. He was
first sent to a local hospital, where he was found to be
comatose with urine incontinence and cyanosis. Arterial
blood gases showed pH 7.3, PaCO2 31.8, PaO2 40.9
Page 1 of 3
(page number not for citation purposes)
Cases Journal 2009, 2:52
mmHg, HCO3 16, SaO2 72%, and SBE -8.5. Hypoxemia
was found. His spontaneous breathing was shallow and
weak with O2 mask with oxygen 6 L/min. He was intubated and supplied 100% O2. Hypotension was detected
after intubation. Dopamine 20 g/kg/min was given.
Brain computed tomography revealed brain edema, and
the chest x-ray showed bilateral pulmonary edema. The
arterial carboxyhemoglobin (COHb) level within 1 hour
after discovery was 51.9%. Pertinent laboratory values
included ammonia 103 g/dL, Na 141 mEq/L, K 3.8 mEq/
L, Ca 9.9 mg/dL, glucose 198 mg/dL, WBC 17,490, Hb
16.3 g/dL, and platelets 336,000. Fresh blood and pink
foamy sputum were noted from the endotracheal tube.
Given his critical condition, he was transferred to our hospital for further management.
One hour after admission, hypotension necessitated the
initiation of a dopamine infusion. The infusion was
http://www.casesjournal.com/content/2/1/52
titrated to effect, with 10 g/kg/min of dopamine.
Echocardiography showed an ejection fraction of 55%.
Four hours after admission, the arterial COHb was 8.4%
and the serum cardiac troponin I was 4.19 ng/mL (normal
< 0.4 ng/mL). Acute pulmonary edema was diagnosed by
chest x-ray (fig 1). The pulmonary edema was treated with
100% oxygen, with increased positive end-expiratory
pressure up to 12 cm H2O. The follow-up chest x-ray
showed worsening pulmonary edema with increasing
bilateral alveolar consolidation. Arterial blood gases
showed severe hypoxemia. Acute respiratory distress syndrome was suspected. High-frequency oscillator ventilation was set to maintain a PaO2 greater than 50 mm Hg
and an oxygen saturation greater than 85%. Beginning
1012 hours after admission, the pulmonary condition
improved progressively. The blood pressure also became
more stable (> 90/50 mmHg).
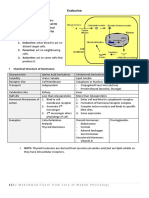
Figurex-ray
Chest
1 showed bilateral acute pulmonary edema
Chest x-ray showed bilateral acute pulmonary edema.
Page 2 of 3
(page number not for citation purposes)
Cases Journal 2009, 2:52
Over the next few days, the patient's cardiovascular and
respiratory status kept improving. The serum cardiac troponin I level declined. The neurological findings
remained a concern. On day four, the dopamine was discontinued. He was extubated successfully on day five. The
neurological findings were normal after extubation. He
was transferred from the pediatric intensive care unit to
the pediatric ward on day 6, and no longer required oxygen.
Discussion
In this report, a 15-year-old boy developed cardiopulmonary compromise following CO poisoning. CO intoxication has been properly named "the great imitator" as a
comment on the various symptoms with which the victim
might present [3]. Common manifestations of acute CO
poisoning in children include gastrointestinal symptoms
and neurological changes [4-6]. The clinical presentation
may mimic a flu-like syndrome or acute gastroenteritis
leading to misdiagnosis [7]. Clarke et al described a possible early sign of CO poisoning, euphoria [8].
http://www.casesjournal.com/content/2/1/52
myocardial damage. Our patient recovered successfully
with aggressive cardiopulmonary management, including
inotropic agents and ventilator support.
This case report is evidence that CO exposure with a high
COHb concentration can cause cardiopulmonary compromise in a child; the child was able to recover smoothly,
without cerebral failure. The COHb concentrations do not
always determine the severity of toxic damage at the level
of selected organs, or serve as a prognostic index [14].
Careful clinical evaluation of the cardiopulmonary and
neurological systems is advisable in children with CO poisoning.
Consent
Written informed consent was obtained from the patient
for publication of this case report and accompanying
images. A copy of the written consent is available for
review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Carbon monoxide binds to hemoglobin reversibly with
an affinity approximately 240 times greater than that of
oxygen, thereby reducing the total oxygen-carrying capacity of the hemoglobin. This competitive binding shifts the
oxygen-hemoglobin dissociation curve to the left, resulting in the impaired release of oxygen at the tissue level
and cellular hypoxia [9]. CO binds to myocardial
myoglobin more slowly than it does to hemoglobin, but
the bond is stronger and the release slower [10].
Authors' contributions
CTW wrote the manuscript and performed the literature
search. JLH and SHH reviewed the manuscript for intellectual content.
References
1.
2.
The arterial blood gases of this patient showed pH 7.3,
PaCO2 31.8, PaO2 40.9 mmHg, HCO3 16, SaO2 72%, and
SBE -8.5. Hypoxemia was found. But Moyle claimed that
the use of pulse oximetry in CO poisoning was negligent.
It must now be considered negligent to use pulse oximetry
on patients who have been at risk of carbon monoxide
inhalation. For every 1% of carboxyhaemoglobin circulating, the pulse oximeter over-reads by approximately 1%
[11].
The cardiovascular effects of CO include myocardial
ischemia, pulmonary edema, arrhythmia, and stunned
myocardium syndrome [12]. Our case had compromised
cardiac output and pulmonary edema. This clinical presentation is consistent with the known cardiac effects of
carbon monoxide poisoning. Pulmonary edema is
uncommon in children with acute CO poisoning. The
possible causes of pulmonary edema include toxic effects
of CO on the alveolar membranes, myocardial damage
leading to left ventricular failure, the aspiration of gastric
contents after loss of consciousness, and neurogenic pulmonary edema [13]. The cause of pulmonary edema in
our case might have been heart failure resulting from
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
Adir Y, Bentur Y, Melamed Y: Hyperbaric oxygen for neuropsychiatric sequelae of carbon monoxide poisoning. Harefuah
1992, 122:562-3.
Onvlee-Dekker IM, De Vries AC, Ten Harkel AD: Carbon monoxide poisoning mimicking long-QT induced syncope. Arch Dis
Child 2007, 92:244-5.
Grace TW, Platt FW: Subacute carbon monoxide poisoning.
Another great imitator. JAMA 1981, 246:1698-1700.
Binder JW, Roberts RJ: Carbon monoxide intoxication in children. Clin Toxicol 1980, 16:287-95.
Hampson NB, Norkool RN: Carbon monoxide poisoning in children riding in the back of pickup trucks. JAMA 1992,
267:538-40.
Meert KL, Heidemann SM, Sarnaik AP: Outcome of children with
carbon monoxide poisoning with normobaic oxygen. J
Trauma 1980, 44:149-54.
Gemelli P, Cattani R: Carbon monoxide poisoning in childhood.
Br Med J 1985, 291:1197.
Clarke SF, Crosby A, Kumar D: Early carbon monoxide intoxication: happy to be poisoned? Emerg Med J 2005, 22:754-5.
Rhoughton RJW, Darling RC: The effect of carbon monoxide on
oxyhemoglobin dissociation curve. Am J Physiol 1994, 141:17-31.
Jaffe FA: Pathogenicity of carbon monoxide. Am J Forensic Med
Pathol 1997, 18:400-10.
Moyle JT: Uses and abuses of pulse oximetry. Arch Dis Child
1996, 74:77-80.
Tritapepe L, Macchiarelli G, Rocco M: Functional and ultrastructural evidence of myocardial stunning after acute carbon
monoxide poisoning. Crit Care Med 1998, 26:797-801.
Naeije R, Peretz A, Cornil A: Acute pulmonary edema following
carbon monoxide poisoning. Intensive Care Med 1980, 6:189-93.
Sokal JA, Kralkowska E: The relationship between exposure
duration, carboxyhemoglobin, blood glucose, pyruvate and
lactate and the severity of intoxication in 39 cases of acute
carbon monoxide poisoning in man. Arch Toxicol 1985, 57:196-9.
Page 3 of 3
(page number not for citation purposes)
Anda mungkin juga menyukai
- Wu 2009Dokumen3 halamanWu 2009Vivi Evita DewiBelum ada peringkat
- Bilateral Massive Pulmonary Embolism Secondary To Decompression Sickness: A Case ReportDokumen4 halamanBilateral Massive Pulmonary Embolism Secondary To Decompression Sickness: A Case ReportPatricio Toledo FuenzalidaBelum ada peringkat
- Wan 01264Dokumen3 halamanWan 01264Paijo SusenoBelum ada peringkat
- Dengue Perimyocarditis: A Case Report: PL GohDokumen3 halamanDengue Perimyocarditis: A Case Report: PL GohDenny IntanBelum ada peringkat
- Me LZ Hee Nba Cte Witten ReportDokumen10 halamanMe LZ Hee Nba Cte Witten ReportMelzheen Rave PecisionBelum ada peringkat
- Case ReportDokumen5 halamanCase ReportRifqiBelum ada peringkat
- ShockDokumen11 halamanShockNatalia WiryantoBelum ada peringkat
- Chronic Cor-Pulmonale in Adults: An Experience From A Tertiary Teaching Hospital in DharwadDokumen4 halamanChronic Cor-Pulmonale in Adults: An Experience From A Tertiary Teaching Hospital in DharwadThariq Mubaraq DrcBelum ada peringkat
- COPD ExacerbationDokumen12 halamanCOPD ExacerbationJeffrey ShermanBelum ada peringkat
- Lesoes Cisticas HIVDokumen5 halamanLesoes Cisticas HIVAndrey Barbosa PimentaBelum ada peringkat
- Copd Exacerbations in EdDokumen23 halamanCopd Exacerbations in EdEzequiel MenesesBelum ada peringkat
- Late Complications of Biliary Atresia: Hepatopulmonary Syndrome and Portopulmonary HypertensionDokumen6 halamanLate Complications of Biliary Atresia: Hepatopulmonary Syndrome and Portopulmonary HypertensionAnisa GayatriBelum ada peringkat
- Fatal Amniotic Fluid Embolism With Typical Pathohistological, HistochemicalDokumen5 halamanFatal Amniotic Fluid Embolism With Typical Pathohistological, HistochemicalAstri Faluna SheylavontiaBelum ada peringkat
- Acute Hypercapnic Respiratory Failure Associated With HemodialysisDokumen3 halamanAcute Hypercapnic Respiratory Failure Associated With HemodialysisMahmoud DiaaBelum ada peringkat
- Critical Care in The Emergency Department: Monitoring The Critically Ill PatientDokumen4 halamanCritical Care in The Emergency Department: Monitoring The Critically Ill PatientNurul Falah KalokoBelum ada peringkat
- A Case of Mushroom Poisoning With Russula Subnigricans: Development of Rhabdomyolysis, Acute Kidney Injury, Cardiogenic Shock, and DeathDokumen4 halamanA Case of Mushroom Poisoning With Russula Subnigricans: Development of Rhabdomyolysis, Acute Kidney Injury, Cardiogenic Shock, and DeathsuserBelum ada peringkat
- A Severe Asphyxiated Newborn: A Case ReportDokumen13 halamanA Severe Asphyxiated Newborn: A Case ReportEeeeeeeeeBelum ada peringkat
- Crim Em2013-948071Dokumen2 halamanCrim Em2013-948071m.fahimsharifiBelum ada peringkat
- Neumonia Anciano 2014Dokumen8 halamanNeumonia Anciano 2014Riyandi MardanaBelum ada peringkat
- 11 - Shock - Current Diagnosis and Treatment Emergency MedicineDokumen18 halaman11 - Shock - Current Diagnosis and Treatment Emergency MedicineRon KBelum ada peringkat
- 121 Anaesthesia For VP Shunt InsertionDokumen8 halaman121 Anaesthesia For VP Shunt InsertionMohammed ElSayedBelum ada peringkat
- PpokDokumen6 halamanPpokSatria UtomoBelum ada peringkat
- COPD and Pulmonary Thromboembolism (For Galley Proof)Dokumen6 halamanCOPD and Pulmonary Thromboembolism (For Galley Proof)Ram AdhikariBelum ada peringkat
- tmp9204 TMPDokumen4 halamantmp9204 TMPFrontiersBelum ada peringkat
- Acute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesDokumen17 halamanAcute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesCandice ChengBelum ada peringkat
- IMCQ 10 - Pulmonary - KEYDokumen13 halamanIMCQ 10 - Pulmonary - KEYReggieBelum ada peringkat
- Metoprolol y El EPOCDokumen10 halamanMetoprolol y El EPOCMadyurit RamírezBelum ada peringkat
- Coagulation Dysfunction in Patients With AECOPD and ItsDokumen6 halamanCoagulation Dysfunction in Patients With AECOPD and ItsAndreea MoalesBelum ada peringkat
- Acute Respiratory Failure 2013 PDFDokumen17 halamanAcute Respiratory Failure 2013 PDFJuan Carlos HuanacheaBelum ada peringkat
- COVID-19 Infection Associated With Auto-Immune Hemolytic AnemiaDokumen3 halamanCOVID-19 Infection Associated With Auto-Immune Hemolytic AnemiaAlexandre VizzoniBelum ada peringkat
- Journal Prevalence of Hypokalemia in Covid 19 andDokumen8 halamanJournal Prevalence of Hypokalemia in Covid 19 andAlexa Mae FonteleraBelum ada peringkat
- Cases Journal: Tuberculosis and Venous Thromboembolism: A Case SeriesDokumen4 halamanCases Journal: Tuberculosis and Venous Thromboembolism: A Case SeriesDiana Fadly MatondangBelum ada peringkat
- Organic Phosphorous Compound and Carbamate ToxicityDokumen13 halamanOrganic Phosphorous Compound and Carbamate ToxicityDaniel ChristiantoBelum ada peringkat
- Saddle Embolism in The Pulmonary Artery BifurcationDokumen3 halamanSaddle Embolism in The Pulmonary Artery BifurcationAtiquzzaman RinkuBelum ada peringkat
- Acute Bronchitis Case StudyDokumen6 halamanAcute Bronchitis Case Studyulka0750% (2)
- Clin Perinatol 2012 Mar 39 (1) 149Dokumen16 halamanClin Perinatol 2012 Mar 39 (1) 149Manuel AzabacheBelum ada peringkat
- Pancytopenia Secondary To Bacterial SepsisDokumen16 halamanPancytopenia Secondary To Bacterial Sepsisiamralph89Belum ada peringkat
- Acute Respiratory Failure 2013Dokumen17 halamanAcute Respiratory Failure 20131411731Belum ada peringkat
- Captura de Ecrã 2024-02-07 À(s) 19.30.27Dokumen19 halamanCaptura de Ecrã 2024-02-07 À(s) 19.30.27yurgan7Belum ada peringkat
- 2 Diclihon Ischemic StrokeDokumen5 halaman2 Diclihon Ischemic StrokeAllan CastroBelum ada peringkat
- Routine Blood Results Explained 3/e: A guide for Nurses & Allied Health ProfessionalsDari EverandRoutine Blood Results Explained 3/e: A guide for Nurses & Allied Health ProfessionalsPenilaian: 3 dari 5 bintang3/5 (2)
- en Kerley A Line in An 18 Year Old Female WDokumen7 halamanen Kerley A Line in An 18 Year Old Female WErlina WahyuBelum ada peringkat
- Massive Pulmonary Embolism Presenting As Seizures: December 2008 Vol 10 No 4Dokumen4 halamanMassive Pulmonary Embolism Presenting As Seizures: December 2008 Vol 10 No 4BelladonnaRoxBelum ada peringkat
- Jurnal Bronchitis Dengan AsmaDokumen5 halamanJurnal Bronchitis Dengan AsmaMauLan SaputraBelum ada peringkat
- Therapeutic Hypothermia For Acute Air Embolic Stroke: ASE EportDokumen3 halamanTherapeutic Hypothermia For Acute Air Embolic Stroke: ASE EportTeuku M. FebriansyahBelum ada peringkat
- Copd 2Dokumen26 halamanCopd 2Abid SunhanBelum ada peringkat
- Critical CareDokumen38 halamanCritical CareavisenicBelum ada peringkat
- A Case Report of An Unusual Complication of Amanita Phalloides PoisoningDokumen3 halamanA Case Report of An Unusual Complication of Amanita Phalloides PoisoningArmando BetancourthBelum ada peringkat
- Arterial Blood Gas Analysis - making it easyDari EverandArterial Blood Gas Analysis - making it easyPenilaian: 4.5 dari 5 bintang4.5/5 (4)
- LepsDokumen4 halamanLepslynharee100% (1)
- HipocalemiaDokumen22 halamanHipocalemiaitalofabregaBelum ada peringkat
- Acid Base Disorder - Student HandoutDokumen4 halamanAcid Base Disorder - Student HandoutRabooh AyashiBelum ada peringkat
- COVID-19 Attacks The 1-Beta Chain of Hemoglobin and Captures The Porphyrin To Inhibit Human Heme MetabolismDokumen23 halamanCOVID-19 Attacks The 1-Beta Chain of Hemoglobin and Captures The Porphyrin To Inhibit Human Heme MetabolismEnfermagem IpavaBelum ada peringkat
- 1924426Dokumen4 halaman1924426Langat IsaacBelum ada peringkat
- Abb IonsDokumen26 halamanAbb Ionssaxebe7427Belum ada peringkat
- Endocrinopathies in The ICU Patient Case FileDokumen2 halamanEndocrinopathies in The ICU Patient Case Filehttps://medical-phd.blogspot.comBelum ada peringkat
- Respiratory Case StudiesDokumen6 halamanRespiratory Case Studiesadom09Belum ada peringkat
- InnisDokumen6 halamanInnisapi-289577018Belum ada peringkat
- WSPH 2019Dokumen15 halamanWSPH 2019Faisol SiddiqBelum ada peringkat
- Likert ScaleDokumen4 halamanLikert Scaleapi-305319592Belum ada peringkat
- Ipi 341446Dokumen6 halamanIpi 341446Cita ChotimahBelum ada peringkat
- 1483 2752 1 SMDokumen10 halaman1483 2752 1 SMMirna WidyanaBelum ada peringkat
- Xerostomia: Faktor Etiologi. Etiologi Dan PenanggulanganDokumen8 halamanXerostomia: Faktor Etiologi. Etiologi Dan PenanggulanganJonathan JojoBelum ada peringkat
- Naocl Risk and ManagementDokumen5 halamanNaocl Risk and ManagementCita ChotimahBelum ada peringkat
- Accidental Injection With Sodium HypochlDokumen8 halamanAccidental Injection With Sodium HypochlCita ChotimahBelum ada peringkat
- Jurnal Ikga Kelompok 1 PDFDokumen7 halamanJurnal Ikga Kelompok 1 PDFCita ChotimahBelum ada peringkat
- Jurnal Perio PDFDokumen3 halamanJurnal Perio PDFCita ChotimahBelum ada peringkat
- Naocl JurnalDokumen9 halamanNaocl JurnalCita ChotimahBelum ada peringkat
- Cronicon: Dental ScienceDokumen5 halamanCronicon: Dental ScienceCita ChotimahBelum ada peringkat
- 1483 2752 1 SMDokumen10 halaman1483 2752 1 SMMirna WidyanaBelum ada peringkat
- April2005 Nicotinic - Kurzbaum 1Dokumen2 halamanApril2005 Nicotinic - Kurzbaum 1Cita ChotimahBelum ada peringkat
- Chap 004Dokumen42 halamanChap 004NguyênBelum ada peringkat
- Jurnal RADIO PDFDokumen4 halamanJurnal RADIO PDFCita ChotimahBelum ada peringkat
- KERACUNAN JamurDokumen4 halamanKERACUNAN JamurCita ChotimahBelum ada peringkat
- Ini Jurnal Readingnya PDFDokumen3 halamanIni Jurnal Readingnya PDFAmanda AndikaBelum ada peringkat
- Case Report: Combined Treatment With Laser Sintering and Zirconium: A Case Report of Dentinogenesis ImperfectaDokumen7 halamanCase Report: Combined Treatment With Laser Sintering and Zirconium: A Case Report of Dentinogenesis ImperfectaCita ChotimahBelum ada peringkat
- Relasi Overjet Overbite Terhadap TMJDokumen8 halamanRelasi Overjet Overbite Terhadap TMJCita ChotimahBelum ada peringkat
- Kehamilan Dan Periodontal PDFDokumen7 halamanKehamilan Dan Periodontal PDFBellia MarsyaBelum ada peringkat
- Jurnal RADIO PDFDokumen4 halamanJurnal RADIO PDFCita ChotimahBelum ada peringkat
- KERACUNAN JamurDokumen4 halamanKERACUNAN JamurCita ChotimahBelum ada peringkat
- Meatball PoisoningDokumen3 halamanMeatball PoisoningCita ChotimahBelum ada peringkat
- Keracunan StaphylococcusDokumen3 halamanKeracunan StaphylococcusCita ChotimahBelum ada peringkat
- 16 53 1 PBDokumen7 halaman16 53 1 PBArmitha HapsariBelum ada peringkat
- Traumatik GranulomaDokumen1 halamanTraumatik GranulomaCita ChotimahBelum ada peringkat
- Ardiologi Yang Berhubungan Dengan DRGDokumen19 halamanArdiologi Yang Berhubungan Dengan DRGCita ChotimahBelum ada peringkat
- Rhythm ECG Characteristics Strip Example: ECG Rhythms and Other Helpful ToolsDokumen6 halamanRhythm ECG Characteristics Strip Example: ECG Rhythms and Other Helpful ToolsJohnildy MatiasBelum ada peringkat
- Cardiac Imaging CasesDokumen278 halamanCardiac Imaging Casesandrew100% (1)
- CHF FC III Ec Mitral StenosisDokumen36 halamanCHF FC III Ec Mitral Stenosisbroken18bear100% (1)
- Contrast Agents, Cath Lab & Anaphylatic Shock-ParamedDokumen29 halamanContrast Agents, Cath Lab & Anaphylatic Shock-ParamedManikanta GupthaBelum ada peringkat
- 418RLE M2 SL1 Basic ECGDokumen8 halaman418RLE M2 SL1 Basic ECGCamille Neypes CarreraBelum ada peringkat
- Post TestDokumen11 halamanPost TestDemuel Dee L. BertoBelum ada peringkat
- Neuro Sample QuestionsDokumen14 halamanNeuro Sample Questionsanonymousah777Belum ada peringkat
- Study of Illness Condition: Assessment Organ Involved Normal Function Pathophysiology AnalysisDokumen3 halamanStudy of Illness Condition: Assessment Organ Involved Normal Function Pathophysiology AnalysisCHRISTINE JOY. MOLINABelum ada peringkat
- Reading ComprehensionDokumen13 halamanReading ComprehensiontarsyBelum ada peringkat
- Moraj 3 ADokumen12 halamanMoraj 3 AMohammed EljackBelum ada peringkat
- Angiology: (Circulatory System)Dokumen40 halamanAngiology: (Circulatory System)api-19641337100% (1)
- Pastel Watercolor Painted PowerPoint TemplateDokumen44 halamanPastel Watercolor Painted PowerPoint TemplateFatimah AlzahraBelum ada peringkat
- Ob2 Sas 26Dokumen9 halamanOb2 Sas 26????Belum ada peringkat
- Assignment (Diabetes)Dokumen9 halamanAssignment (Diabetes)Wynne EnglatieraBelum ada peringkat
- Aspire NotesDokumen561 halamanAspire NoteskirtanyaBelum ada peringkat
- Nicotine: How Does Nicotine Deliver Its Effect?Dokumen6 halamanNicotine: How Does Nicotine Deliver Its Effect?jmolaecheaBelum ada peringkat
- Adrenergic DrugsDokumen14 halamanAdrenergic DrugsMarian YuqueBelum ada peringkat
- CoffeeDokumen3 halamanCoffeejejosefBelum ada peringkat
- Case History: Year 8 SemesterDokumen26 halamanCase History: Year 8 SemesterNarmada PemathilakaBelum ada peringkat
- Acute Diseases and Life-Threatening Conditions: Assistant Professor Kenan KaravdićDokumen33 halamanAcute Diseases and Life-Threatening Conditions: Assistant Professor Kenan KaravdićGoran MaliBelum ada peringkat
- Class Presentation CVADokumen23 halamanClass Presentation CVAAmbika Ghosh SenBelum ada peringkat
- Maria Obra V SSSDokumen2 halamanMaria Obra V SSSAnonymous i19DbbQTBelum ada peringkat
- Hydrocephalus by MacDokumen44 halamanHydrocephalus by MacMacktevin FraterinBelum ada peringkat
- EFNS Congress Vienna Semax AbstractDokumen60 halamanEFNS Congress Vienna Semax AbstractnontjeBelum ada peringkat
- QDokumen541 halamanQAmeer Youseff MarotoBelum ada peringkat
- Dr. MD - Serajul Islam ChowdhuryDokumen64 halamanDr. MD - Serajul Islam ChowdhuryPyronBelum ada peringkat
- DR R.V.S.N. Sarma., Consultant Physician and Chest SpecialistDokumen58 halamanDR R.V.S.N. Sarma., Consultant Physician and Chest SpecialistVaibhav BharatBelum ada peringkat
- Sepsis Quick Reference GuideDokumen1 halamanSepsis Quick Reference GuideRavin DebieBelum ada peringkat
- De La Cruz, A - BSN 3b - Case Study For RM 219 - 1st Week of DutyDokumen13 halamanDe La Cruz, A - BSN 3b - Case Study For RM 219 - 1st Week of DutyAlia De La CruzBelum ada peringkat
- Body Fluids Analysis LectureDokumen17 halamanBody Fluids Analysis LectureAsd Asd100% (1)