Nejm 1
Diunggah oleh
Tri Anna FitrianiJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Nejm 1
Diunggah oleh
Tri Anna FitrianiHak Cipta:
Format Tersedia
new england
journal of medicine
The
established in 1812
october 2, 2014
vol. 371 no. 14
Withdrawal of Inhaled Glucocorticoids and Exacerbations of COPD
Helgo Magnussen, M.D., Bernd Disse, M.D., Ph.D., Roberto Rodriguez-Roisin, M.D., Anne Kirsten, M.D.,
Henrik Watz, M.D., Kay Tetzlaff, M.D., Lesley Towse, B.Sc., Helen Finnigan, M.Sc., Ronald Dahl, M.D.,
Marc Decramer, M.D., Ph.D., Pascal Chanez, M.D., Ph.D., Emiel F.M. Wouters, M.D., Ph.D.,
and Peter M.A. Calverley, M.D., for the WISDOM Investigators*
A bs t r ac t
Background
Treatment with inhaled glucocorticoids in combination with long-acting bronchodilators is recommended in patients with frequent exacerbations of severe chronic
obstructive pulmonary disease (COPD). However, the benefit of inhaled glucocorticoids in addition to two long-acting bronchodilators has not been fully explored.
Methods
In this 12-month, double-blind, parallel-group study, 2485 patients with a history of
exacerbation of COPD received triple therapy consisting of tiotropium (at a dose of
18 g once daily), salmeterol (50 g twice daily), and the inhaled glucocorticoid
fluticasone propionate (500 g twice daily) during a 6-week run-in period. Patients
were then randomly assigned to continued triple therapy or withdrawal of fluticasone in three steps over a 12-week period. The primary end point was the time to
the first moderate or severe COPD exacerbation. Spirometric findings, health status,
and dyspnea were also monitored.
Results
The authors affiliations are listed in the
Appendix. Address reprint requests to
Dr. Magnussen at the Pulmonary Research
Institute at Lung Clinic Grosshansdorf,
Woehrendamm 80, D-22927 Grosshans
dorf, Germany, or at magnussen@
pulmoresearch.de.
*Investigators in the Withdrawal of Inhaled
Steroids during Optimized Bronchodilator Management (WISDOM) study are
listed in the Supplementary Appendix,
available at NEJM.org.
This article was published on September 8,
2014, and updated on October 2, 2014, at
NEJM.org.
N Engl J Med 2014;371:1285-94.
DOI: 10.1056/NEJMoa1407154
Copyright 2014 Massachusetts Medical Society.
As compared with continued glucocorticoid use, glucocorticoid withdrawal met the
prespecified noninferiority criterion of 1.20 for the upper limit of the 95% confidence
interval (CI) with respect to the first moderate or severe COPD exacerbation (hazard
ratio, 1.06; 95% CI, 0.94 to 1.19). At week 18, when glucocorticoid withdrawal was
complete, the adjusted mean reduction from baseline in the trough forced expiratory volume in 1 second was 38 ml greater in the glucocorticoid-withdrawal group
than in the glucocorticoid-continuation group (P<0.001); a similar between-group
difference (43 ml) was seen at week 52 (P=0.001). No change in dyspnea and minor
changes in health status occurred in the glucocorticoid-withdrawal group.
Conclusions
In patients with severe COPD receiving tiotropium plus salmeterol, the risk of moderate or severe exacerbations was similar among those who discontinued inhaled
glucocorticoids and those who continued glucocorticoid therapy. However, there
was a greater decrease in lung function during the final step of glucocorticoid
withdrawal. (Funded by Boehringer Ingelheim Pharma; WISDOM ClinicalTrials.gov
number, NCT00975195.)
n engl j med 371;14nejm.orgoctober 2, 2014
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2016. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
1285
The
n e w e ng l a n d j o u r na l
xacerbations of chronic obstructive pulmonary disease (COPD) are symptomatically defined, acute events that lead
to a change in treatment1,2 and are associated
with an accelerated decline in lung function and
health status.3 Treatment with inhaled glucocorticoids reduces the exacerbation rate, especially
when the drugs are used in combination with a
long-acting -agonist (LABA).4,5 Consequently,
combination therapy with an inhaled glucocorticoid and a LABA is recommended in patients
with severe COPD or a history of frequent exacerbations.2 Long-acting muscarinic antagonists
(LAMAs) have also been shown to prevent exacerbations.6-8 However, in patients with severe or
very severe COPD and a history of exacerbations,
the benefit of inhaled glucocorticoids in a regimen that includes these two classes of long-acting bronchodilators has not yet been determined
in an adequately powered study.
We hypothesized that with a controlled, stepwise withdrawal of inhaled glucocorticoids, the
risk of exacerbation would be similar to that with
continued use of inhaled glucocorticoids in patients with severe or very severe COPD who were
receiving a combination of a LAMA (tiotropium)
and a LABA (salmeterol). To test this hypothesis,
we conducted the Withdrawal of Inhaled Steroids
during Optimized Bronchodilator Management
(WISDOM) trial, which was designed to determine whether patients with COPD who were receiving both LAMA and LABA therapy with inhaled glucocorticoids would have similar outcomes
regardless of whether the glucocorticoids were
withdrawn or continued.
Me thods
Study Design
From February 2009 through July 2013, we performed this multinational, randomized, doubleblind, parallel-group, active-control study. All patients entered a 6-week run-in period during which
they received 18 g of tiotropium once daily (delivered by a HandiHaler), 50 g of salmeterol xina
foate twice daily (two actuations of 25 g; a dose
of 21 g is designated on the U.S. product label),
and 500 g of fluticasone propionate (an inhaled
glucocorticoid) twice daily (two actuations of 250
g [U.S. designated dose, 230 g] delivered by a
metered-dose inhaler). In this study, we refer to
the European Union designation of doses for
consistency.
1286
of
m e dic i n e
During the double-blind phase of the trial,
patients underwent randomization in a 1:1 ratio
to the two study groups. The first group continued to receive tiotropium, salmeterol, and flut ic
asone at the same doses as those used during
the run-in period for the duration of the 52-week
study period. The second group continued to receive tiotropium and salmeterol over the 52-week
period but with a stepwise reduction in the flutic
asone dose every 6 weeks, from a total daily dose
of 1000 g to 500 g, then to 200 g, and finally
to 0 g (placebo)9 (Fig. S1 in the Supplementary
Appendix, available with the full text of this article at NEJM.org). Patients who prematurely discontinued therapy were followed for vital status
from the time of discontinuation until the completion of the trial at 52 weeks.
Patients
We recruited patients who were at least 40 years
of age and who were either current smokers (10
pack-years) or former smokers and had received a
diagnosis of severe or very severe COPD, which
was defined as a forced expiratory volume in
1second (FEV1) that was less than 50% of the
predicted volume and less than 70% of the forced
vital capacity after bronchodilation and a history
of at least one documented exacerbation in the
12 months before screening. Full inclusion and
exclusion criteria have been reported previously9
and are provided in the trial protocol, which is
available at NEJM.org. All patients provided written informed consent.
The use of xanthines and mucolytic agents, but
not maintenance oral glucocorticoid treatment,
was allowed throughout the trial. All patients
were provided with open-label salbutamol (also
known as albuterol) for use as needed. At the
investigators discretion, randomized treatment
could be discontinued and open-label fluticasone
could be initiated for the remainder of the trial.
Any exacerbations that were reported after the
discontinuation of randomized treatment were not
included in the primary end point. Included in a
prespecified sensitivity analysis were exacerbations
that were reported in patients who were receiving
open-label fluticasone therapy and in those who
had discontinued treatment.
End Points and Assessments
The primary end point was the time to the first
moderate or severe COPD exacerbation during
the 12-month study period. We used a standard-
n engl j med 371;14nejm.orgoctober 2, 2014
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2016. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
Glucocorticoid Withdr awal and COPD Exacerbations
ized, structured questionnaire to collect data regarding exacerbations, with documentation at
each study visit. In addition, we provided patients
with a simple diary, to be completed on a daily
basis, for noting changes in symptoms and the
use of medications between visits. A moderate
exacerbation was defined as an increase in lower
respiratory tract symptoms related to COPD or
the new onset of two or more such symptoms,
with at least one symptom lasting 3 or more days
and for which the treating physician prescribed
antibiotics, systemic glucocorticoids, or both. A
severe exacerbation was defined as an exacerbation requiring hospitalization in an urgent care
unit. The start date of an exacerbation was defined as the onset date of the first recorded COPD
symptom.
Secondary end points included the time to the
first severe COPD exacerbation, the number of
moderate or severe COPD exacerbations, the
change from baseline in lung function (including
the trough FEV1, forced vital capacity, and peak
expiratory flow rate), health status, and dyspnea.
To assess health status, we used the total score
on the St. Georges Respiratory Questionnaire
(SGRQ), on a scale of 0 to 100, with higher scores
indicating worse function and a minimum clinically important difference of 4 points.10 To assess dyspnea, we used the modified Medical
Research Council (mMRC) scale of 0 to 4, with
higher scores indicating more severe dyspnea; the
absence of breathlessness was given a score of 1.
No minimum clinically important difference has
been identified.11 All secondary end points were
assessed over the 12-month study period.
We performed all spirometric measurements
according to the recommendations of the American
Thoracic Society and the European Respiratory
Society12 at baseline and at weeks 6, 12, 18, and
52. We used values after bronchodilation in qualifying tests of pulmonary function. Before performing spirometric testing, we obtained scores
on the SGRQ at baseline and at weeks 27 and 52
and obtained scores on the mMRC scale at baseline and at weeks 18 and 52. (Additional details
regarding the end points are provided in the
protocol and in Table S1 in the Supplementary
Appendix.)
18, and 52. Chest radiography was requested when
pneumonia was suspected during the trial. Adverse events and serious adverse events, regardless of causality, were recorded throughout the
study, and results are reported descriptively. If patients did not spontaneously report adverse events,
they were asked open-ended questions, such as
How have you felt since the last visit?
Study Oversight
The study protocol was approved by the ethics
review board at each institution. The first draft
of the manuscript and subsequent revisions were
written by the academic authors, and all the authors worked collaboratively to prepare the final
content; all the authors made the decision to submit the manuscript for publication. Editorial assistance was provided by a medical writer employed
by a company that was paid by the study sponsor,
Boehringer Ingelheim Pharma. Statistical analyses
were performed by the sponsor. All study drugs
were supplied by the sponsor. All the authors
vouch for the accuracy and completeness of the
data and the fidelity of the study to the protocol.
Statistical Analysis
We estimated that 2456 patients would need to
undergo randomization at the 200 study centers
to ensure a minimum of 2234 patients who could
be evaluated in order to provide the study with a
power of 90% to determine the noninferiority of
the hazard ratio for exacerbation among patients
in the glucocorticoid-withdrawal group, as compared with the glucocorticoid-continuation group,
with a one-sided alpha level of 0.025 and an expected dropout rate of 15% per year. The assumed median time to the first primary event was
9 months. The prespecified noninferiority margin
of 1.20 was defined as the upper limit of the 95%
confidence interval for the hazard ratio for the
first moderate or severe exacerbation in the glucocorticoid-withdrawal group, as compared with
the glucocorticoid-continuation group. Both efficacy and safety were evaluated in the modified
intention-to-treat population, which was defined
as all patients who received at least one dose of a
study drug.
We used a Cox proportional-hazards regression
model with adjustment for the baseline FEV1 in
Safety
the primary analysis, in the prespecified sensiWe performed physical examinations at the time tivity analysis, and in the analysis of the time to
of screening and at week 52 and measured and the first severe COPD exacerbation. In the sensirecorded vital signs at baseline and at weeks 6, 12, tivity analysis, we included exacerbations in pan engl j med 371;14nejm.orgoctober 2, 2014
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2016. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
1287
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
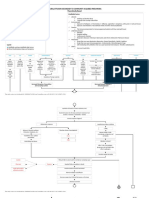
3426 Patients were enrolled
938 Were excluded
72 (7.7%) Had adverse event
679 (72.4%) Did not meet inclusion criteria
or met exclusion criteria
13 (1.4%) Were lost to follow-up
117 (12.5%) Withdrew consent
57 (6.1%) Had other reason
2488 Underwent randomization
1244 Were assigned to glucocorticoid
continuation
1244 Were assigned to glucocorticoid
withdrawal
1243 Were treated
1242 Were treated
231 Discontinued study
101 Had adverse event
6 Had lack of efficacy
23 Did not adhere to study
regimen
7 Were lost to follow-up
61 Declined study
medication
33 Had other reason
227 Discontinued study
108 Had adverse event
6 Had lack of efficacy
27 Did not adhere to study
regimen
9 Were lost to follow-up
48 Declined study
medication
29 Had other reason
1016 (81.7%) Completed study
1011 (81.4%) Completed study
Figure 1. Enrollment and Outcomes.
the patients were men; the mean age was 63.8
years, and the mean FEV1 after bronchodilation
was 0.93 liters, which was 32.8% of the predicted
value. Of the 2485 patients, 2027 completed the
52-week study, including those who received openlabel fluticasone.
Characteristics of the patients at baseline and
dropout rates were similar in the two study groups
(Fig. 1 and Table 1, and Table S2 in the Supple
mentary Appendix). According to the Global Initi
ative for Chronic Obstructive Lung Disease (GOLD)
criteria, 61.2% of the patients had an FEV1 that
was 30 to 49% of the predicted value (GOLD 3),
and 38.1% of the patients had an FEV1 that was
less
than 30% of the predicted value (GOLD 4).
R e sult s
The percentages of patients receiving inhaled gluPatients
cocorticoids, LABAs, or LAMAs at baseline were
A total of 2485 patients underwent randomization 69.9%, 64.6%, and 46.9%, respectively, with 39.0%
at 200 centers in 23 countries. A total of 82.5% of receiving the three treatments in combination.
tients who were switched to open-label fluticasone. In a post hoc sensitivity analysis of the
primary end point, we removed the covariate from
the model in order to include treated patients
with missing data regarding the baseline FEV1.
In addition, we used the KaplanMeier method
to estimate the probability of a moderate or severe COPD exacerbation. This procedure was repeated for determining the probability of a severe
COPD exacerbation. Additional details regarding the statistical analysis are provided in the
protocol and in Section 4 in the Supplementary
Appendix.
1288
n engl j med 371;14nejm.orgoctober 2, 2014
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2016. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
Glucocorticoid Withdr awal and COPD Exacerbations
Table 1. Characteristics of the Patients at Baseline.*
Characteristic
Male sex no. (%)
Glucocorticoid
Continuation
(N=1243)
Glucocorticoid
Withdrawal
(N=1242)
All Patients
(N=2485)
1013 (81.5)
1036 (83.4)
2049 (82.5)
Age yr
63.68.6
64.08.4
Former smoker no. (%)
811 (65.2)
843 (67.9)
1654 (66.6)
63.88.5
Duration of COPD yr
7.755.99
8.006.47
7.876.23
3049%: GOLD 3
760 (61.1)
761 (61.3)
1521 (61.2)
<30%: GOLD 4
473 (38.1)
474 (38.2)
947 (38.1)
Other category
10 (0.8)
7 (0.6)
17 (0.7)
1223
1218
2441
Percentage of predicted FEV1 after
bronchodilation no. (%)
Baseline lung function
Patients with available data no.
FEV1
Value liters
0.970.36
0.980.36
0.980.36
Percentage of predicted value
34.211.2
34.310.8
34.211.0
1238
1237
2475
1.80.9
1.90.9
1.80.9
1136
1126
2262
46.3517.89
45.9118.19
46.1318.04
Score on mMRC scale
Patients with available data no.
Mean score
SGRQ score
Patients with available data no.
Mean score
Medication use no. (%)
LAMA
588 (47.3)
578 (46.5)
1166 (46.9)
LABA
807 (64.9)
798 (64.3)
1605 (64.6)
Inhaled glucocorticoid
876 (70.5)
862 (69.4)
1738 (69.9)
Triple therapy with LAMA, LABA, and inhaled
glucocorticoid, with or without other
pulmonary medication no. (%)**
479 (38.5)
491 (39.5)
970 (39.0)
* Plusminus values are means SD. There were no significant differences between the two groups at baseline on the
basis of t-tests for continuous variables and chi-square tests or Fishers exact test, as appropriate, for categorical variables.
COPD denotes chronic obstructive pulmonary disease, FEV1 forced expiratory volume in 1 second, GOLD Global Initiative
for Chronic Obstructive Lung Disease, LABA long-acting -agonist, and LAMA long-acting muscarinic antagonist.
All patients in the study were either current smokers (10 pack-years) or former smokers.
Of the 17 patients in this category, 3 had mild COPD (FEV1, 80% of predicted value, or GOLD 1), 9 had moderate
COPD (FEV1, 50 to 79% of predicted value, or GOLD 2), and 5 had missing values.
Patients for whom baseline lung-function data were available were evaluated after receiving triple therapy during the
run-in period. Usable data regarding lung function were missing for 44 patients at baseline.
Scores on the modified Medical Research Council (mMRC) scale range from 0 to 4, with higher scores indicating more
severe dyspnea; the absence of breathlessness was given a score of 1. No minimum clinically important difference
has been identified.
Scores on St. Georges Respiratory Questionnaire (SGRQ) range from 0 to 100, with higher scores indicating worse
function and a minimum clinically important difference of 4 points.
** Other respiratory medications included oral -agonists, oral glucocorticoids, leukotriene-receptor antagonists, mucolytic agents, oxygen, and xanthines.
Overall, 28.2% of patients had cardiac disorders at Primary End Point
baseline, and 45.8% had vascular disorders (Table The hazard ratio for a first moderate or severe
COPD exacerbation was 1.06 (95% confidence inS3 in the Supplementary Appendix).
n engl j med 371;14nejm.orgoctober 2, 2014
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2016. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
1289
The
n e w e ng l a n d j o u r na l
A Moderate or Severe COPD Exacerbation
1.0
of
m e dic i n e
B Primary End Point and Sensitivity Analyses
Hazard ratio, 1.06 (95% CI, 0.941.19)
P=0.35 by Walds chi-square test
0.9
Hazard Ratio (95% CI)
Estimated Probability
0.8
Primary end point
0.7
0.94
1.06
1.19
0.95
1.06
1.19
0.6
0.5
IGC withdrawal
IGC
continuation
0.4
0.3
Noninferiority
margin
Primary end point
excluding baseline
FEV1 covariate
0.2
0.1
0.0
Primary end point
including exacerbations
on open-label therapy
12
18
24
30
36
42
48
54
0.8
Weeks to Event
No. at Risk
IGC continuation 1243 1059 927 827 763 694 646 615 581
IGC withdrawal 1242 1090 965 825 740 688 646 607 570
1.0
1.0
1.18
1.1
1.2
1.3
1.4
1.5
IGC Continuation
Better
D Change from Baseline in Trough FEV1
Daily Fluticasone Dose in Withdrawal Group
Hazard ratio, 1.20 (95% CI, 0.981.48)
P=0.08 by Walds chi-square test
0.9
0.9
1.05
IGC
Withdrawal
Better
14
19
C Severe COPD Exacerbation
0.93
Reduced to
500 g
Reduced to
200 g
Reduced to
0 g (placebo)
0.7
0.6
0.5
0.4
0.3
0.2
IGC withdrawal
0.1
0.0
IGC continuation
0
12
18
24
30
36
42
48
Adjusted Mean Change
in FEV1 (ml)
Estimated Probability
0.8
20
40
IGC withdrawal
60
80
54
IGC
continuation
P<0.001
P=0.001
0
Weeks to Event
12
18
52
1077
1058
970
935
Week
No. at Risk
No. at Risk
IGC continuation 1243 1180 1117 1066 1026 993 957 928 895
IGC withdrawal 1242 1189 1119 1044 986 941 918 889 863
20
25
IGC continuation 1223
IGC withdrawal 1218
1135
1135
1114
1092
Figure 2. COPD Exacerbations and Lung Function.
Panel A shows KaplanMeier curves for the estimated probability of moderate or severe exacerbations of chronic obstructive pulmonary
disease (COPD) during the study, with no significant difference between the group assigned to withdrawal of inhaled glucocorticoids
(IGC) and the group assigned to continued IGC treatment. Panel B shows a forest plot of hazard ratios for the first COPD exacerbation
(the primary end point), the primary end point including exacerbations during open-label therapy (sensitivity analysis), and the primary
end point excluding the covariate of the baseline forced expiratory volume in 1 second (FEV1) (sensitivity analysis). All three categories
fall within the prespecified noninferiority margin of 1.20 (the upper limit of the 95% confidence interval for the hazard ratio in the glucocorticoid-withdrawal group as compared with the glucocorticoid-continuation group). Horizontal dashed lines indicate 95% confidence
intervals. Panel C shows KaplanMeier curves for the estimated probability of severe COPD exacerbations, with no significant betweengroup difference. Panel D shows the adjusted mean change from baseline in the FEV1, as measured during clinic visits. In the glucocorticoidwithdrawal group, there was a significant decline in lung function at weeks 18 and 52, as compared with the change from baseline in the
glucocorticoid-continuation group. I bars indicate standard errors. In Panels A and C, the study period ends at 54 weeks because some
visits could not be scheduled at 52 weeks.
terval [CI], 0.94 to 1.19) with glucocorticoid withdrawal as compared with glucocorticoid continuation, which indicated noninferiority, since the
upper limit of the confidence interval was below
1290
the predefined noninferiority margin of 1.20
(Fig. 2A and 2B). The results were similar in a
sensitivity analysis that included exacerbations
occurring after patients had discontinued random-
n engl j med 371;14nejm.orgoctober 2, 2014
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2016. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
Glucocorticoid Withdr awal and COPD Exacerbations
ized treatment and in a post hoc analysis that
excluded the FEV1 from the model (Fig. 2B, and
Fig. S2 in the Supplementary Appendix). The time
by which 25% of patients had a first moderate or
severe exacerbation (first quartile) was 110 days
in the glucocorticoid-withdrawal group and 107
days in the glucocorticoid-continuation group.
Secondary End Points
The adjusted event rate for moderate or severe
exacerbations was 0.95 per patient-year (95% CI,
0.87 to 1.04) in the glucocorticoid-withdrawal
group and 0.91 per patient-year (95% CI, 0.83 to
0.99) in the glucocorticoid-continuation group.
Analysis of the time to the first severe COPD exacerbation showed a hazard ratio of 1.20 (95% CI,
0.98 to 1.48) for glucocorticoid withdrawal as compared with glucocorticoid continuation (Fig. 2C).
The majority of patients with one or more exacerbations had one or two moderate or severe exacerbations during the study (Fig. S3 and S4 in the
Supplementary Appendix). There were no significant between-group differences in hazard ratios
in any of the subgroup analyses (Fig. 3).
FEV1
At week 18, when glucocorticoid withdrawal was
complete, the adjusted mean reduction from baseline in the trough FEV1 was 38 ml greater in the
glucocorticoid-withdrawal group than in the glucocorticoid-continuation group (P<0.001). A similar between-group difference (43 ml) was seen at
week 52 (Fig. 2D). No significant between-group
differences were observed at weeks 6 and 12.
Health Status
The change from baseline in the mMRC score
did not differ significantly between the glucocorticoid-withdrawal group and the glucocorticoidcontinuation group at week 18 (0.001 and 0.030
points, respectively; P=0.36) or at week 52 (0.035
and 0.028 points, respectively; P=0.06). The
changes from baseline in the total SGRQ scores
were an increase of 0.55 points in the glucocorticoid-withdrawal group and a reduction of 0.42
points in the glucocorticoid-continuation group
at week 27 (P=0.08) and an increase of 1.15 and
a decrease of 0.07, respectively, at week 52
(P=0.047).
Safety
The overall proportion of patients who had one
or more adverse events while receiving the study
treatment was 71.2%, and the proportions were
similar in the two groups (Table 2, and Table S4
in the Supplementary Appendix). Serious adverse
events were reported in 24.2% of the patients in
the glucocorticoid-withdrawal group and 23.5%
of the patients in the glucocorticoid-continuation
group. Rates of fatal adverse events were 3.2% in
the glucocorticoid-withdrawal group and 2.7% in
the glucocorticoid-continuation group.
The incidence of pneumonia was 5.5% in the
glucocorticoid-withdrawal group and 5.8% in
the glucocorticoid-continuation group. The incidence of cardiac adverse events of interest was
similarly balanced between the groups, with major
adverse cardiac events reported in 2.2% of the
patients in the glucocorticoid-withdrawal group
and 2.0% of patients in the glucocorticoid-continuation group. Major adverse cardiac events that
were fatal were reported in 1.5% and 1.1% of the
patients, respectively, and stroke was reported
in 0.5% and 0.7% of the patients, respectively
(Table 2).
Discussion
In our study, in which patients with severe or very
severe COPD received triple therapy with a LAMA,
a LABA, and an inhaled glucocorticoid during a
run-in period, followed by withdrawal of the inhaled glucocorticoid over a 3-month period or
continued triple therapy, the upper limit of the
95% confidence interval for an increase in the
risk of a moderate or severe acute exacerbation
was below the prespecified noninferiority margin
of 1.20 in the glucocorticoid-withdrawal group.
Differences in FEV1 and health status emerged in
the 18-week analysis after inhaled glucocorticoid
treatment was completely withdrawn. We did not
identify any subgroup of patients that had an increased likelihood of an exacerbation after glucocorticoid withdrawal. Since a history of exacerbation and substantial impairment in lung function
were entry criteria, our study population was representative of patients for whom inhaled glucocorticoids are recommended on the basis of
GOLD guidance.1
Most clinical trials involving patients with
COPD have established the benefit of treatment
by comparing a new therapy with placebo or a
relevant active control. Few trials have considered
the question of whether such therapy should be
continued after clinical stability has been achieved,
an approach that is commonly adopted for pa-
n engl j med 371;14nejm.orgoctober 2, 2014
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2016. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
1291
The
Subgroup
n e w e ng l a n d j o u r na l
No. of Patients
All patients
Age
<55 yr
55 to <65 yr
65 to <75 yr
75 yr
Sex
Male
Female
Smoking status
Former smoker
Current smoker
Body-mass index
<20
20 to <25
25 to <30
30
IGC at screening
Yes
No
Xanthines at screening
Yes
No
Chronic bronchitis
Yes
No
GOLD stage at screening
3
4
GOLD assessment category at baseline
C
D
Prior antibiotics or systemic glucocorticoids
<2
2
Beta-blockers at screening
Yes
No
of
m e dic i n e
Hazard Ratio (95% CI)
2441
1.06
345
945
883
268
1.04
0.95
1.19
1.06
2010
431
1.08
1.02
1630
811
1.10
0.99
368
912
771
390
0.94
1.17
1.05
0.96
1724
717
1.08
1.00
567
1874
1.15
1.03
1548
891
1.11
0.95
1491
934
1.12
1.00
819
1612
1.15
1.01
1537
903
1.03
1.11
188
2253
0.89
1.07
0.5
1.0
IGC Withdrawal Better
2.0
IGC Continuation Better
Figure 3. Subgroup Analyses of the First Moderate or Severe COPD Exacerbation in All Study Patients.
All categories were evaluated in post hoc analyses except for age, sex, smoking status, and baseline body-mass index. Data with respect to chronic bronchitis were obtained from electronic case-report forms. The size of the diamonds is proportional to the number of patients in the subgroup. The horizontal lines indicate 95% confidence
intervals. Usable data regarding lung function were missing for 44 patients at baseline. GOLD denotes Global
Initiative for Chronic Obstructive Lung Disease.
tients with asthma.13 Initial studies showed that
abrupt withdrawal of inhaled glucocorticoids in
patients with a range of COPD severities led to
more exacerbations and some worsening of lung
function, at least when patients used short-acting
bronchodilators as maintenance treatment.14-17
In our study, we used dual bronchodilation with
salmeterol and tiotropium, which has proved to
1292
be more effective than salmeterol alone in the
prevention of exacerbations.6 Moreover, we withdrew glucocorticoid treatment gradually from a
common baseline of maximized therapy.
In our study, we saw no significant betweengroup difference in the rate of dropout, which
typically occurs more frequently in the placebo
groups in clinical trials.18,19 There was a tran-
n engl j med 371;14nejm.orgoctober 2, 2014
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2016. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
Glucocorticoid Withdr awal and COPD Exacerbations
sient increase in the number of severe exacerbations soon after the complete withdrawal of
glucocorticoids, but this increase was not significant and was not sustained during the study
period. We considered a number of subgroups in
which a greater degree of dependence on glucocorticoids might be expected, but we did not find
notable differences in outcomes between inhaled
glucocorticoid withdrawal and continued triple
therapy in any of these subgroups.
After complete withdrawal of glucocorticoids,
we observed a small but significant and persistent between-group difference in the FEV1, with
a larger reduction from the baseline value in the
glucocorticoid-withdrawal group. This change
was similar to that observed in previous trials of
glucocorticoid withdrawal14-17 and in a study of
roflumilast, an oral nonglucocorticoid antiinflammatory drug, in a patient population that was
similar to the one in our study.20 The change in
the FEV1 may represent the spirometric signal
associated with antiinflammatory therapy but
does not seem to be associated with exacerbations, as reported in recent studies of combination therapy with once-daily inhaled glucocorticoids plus LABAs.21In our study, the between-group
difference in FEV1 became apparent only after the
final step of inhaled glucocorticoid withdrawal
(from 200 g to 0 g of fluticasone per day).
We saw no significant effect of glucocorticoid
withdrawal on the mMRC score, but there was a
difference in the total SGRQ score that was
noted during the study period and that favored
continued glucocorticoid therapy. However, the
importance of this finding is unclear, since the
between-group difference was smaller than the
frequently used minimum clinically important
difference22 and was not related to differences in
the number of exacerbations. We saw no significant between-group difference in the safety
profile, including the number of cases of pneumonia. In contrast, other studies have shown an
increase in cases of pneumonia among patients
with COPD who received fluticasone.5,8,21 On the
basis of our study data, we cannot determine
whether our findings with respect to pneumonia
reflect differences in our patient population or a
sustained effect on pneumonia risk in our glucocorticoid-withdrawal group, since patients in
that group received inhaled glucocorticoids for
4 months (including the run-in period); this
question merits future study.
Our study has both strengths and limitations.
Table 2. Adverse Events.*
Variable
Glucocorticoid
Continuation
(N=1243)
Glucocorticoid
Withdrawal
(N=1242)
no. of patients (%)
Adverse events
Any
880 (70.8)
890 (71.7)
Leading to discontinuation
of study drug
115 (9.3)
127 (10.2)
292 (23.5)
300 (24.2)
During study period
34 (2.7)
40 (3.2)
Including vital-status follow-up
38 (3.1)
43 (3.5)
273 (22.0)
271 (21.8)
72 (5.8)
68 (5.5)
Any
25 (2.0)
27 (2.2)
Fatal
14 (1.1)
19 (1.5)
9 (0.7)
6 (0.5)
Serious adverse events
Any
Death
Requiring hospitalization
Adverse events of special interest
Pneumonia
Major adverse cardiac event
Stroke
* A more detailed list of adverse events is provided in Table S4 in the Supple
mentary Appendix.
The preferred terms in the Medical Dictionary for Regulatory Activities
(MedDRA) that were included in the category of pneumonia were bronchopneumonia, lobar pneumonia, pneumonia, pneumonia klebsiella, pneumonia
pneumococcal, and pneumonia streptococcal; the system organ classes that
were included in the category of major adverse cardiac events were cardiac disorders (fatal) and vascular disorders (fatal); the preferred terms were sudden
death, cardiac death, and sudden cardiac death; the Standardized MedDRA
query (SMQ) was ischemic heart disease, and the sub-SMQs were myocardial
infarction (broad) and myocardial infarction (fatal); and those that were included in the category of stroke were cerebellar infarction, cerebral infarction,
cerebrovascular accident, embolic cerebral infarction, ischemic cerebral infarction, ischemic stroke, and transient ischemic attack.
We enrolled substantially more patients than were
enrolled in all previous trials of glucocorticoid
withdrawal combined, which allowed for further
examination of the response in various subgroups.
We had 9 months of observation of patients who
were not receiving glucocorticoids, with no suggestion that exacerbations were occurring more
frequently. It is unlikely that a longer follow-up
period would have changed this conclusion. Our
study population consisted mainly of white men;
we believe that the proportionally smaller enrollment of women was the result of a combination of
disease prevalence in the study countries and the
severity of disease within our population. However,
we observed no significant difference in outcome
on the basis of sex (Fig. 3).
n engl j med 371;14nejm.orgoctober 2, 2014
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2016. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
1293
Glucocorticoid Withdr awal and COPD Exacerbations
In conclusion, we found that in patients with needs to be considered when making decisions
severe but stable COPD who were receiving com- regarding maintenance therapy in patients with
bination therapy with tiotropium, salmeterol, severe but stable COPD.
and glucocorticoids, the stepwise withdrawal of
glucocorticoids was noninferior to the continuaSupported by Boehringer Ingelheim Pharma.
Disclosure forms provided by the authors are available with
tion of such therapy, with respect to the risk of
the full text of this article at NEJM.org.
moderate or severe exacerbations. The effect of
We thank Caitlin Watson, Ph.D., of Complete HealthVizion
withdrawal on symptoms and lung function also for medical-writing support.
Appendix
The authors affiliations are as follows: the Pulmonary Research Institute at Lung Clinic Grosshansdorf, Airway Research Center North,
German Center for Lung Research, Grosshansdorf (H.M., A.K., H.W.), Boehringer Ingelheim Pharma, Ingelheim (B.D., K.T.), and the
Department of Sports Medicine, University of Tbingen, Tbingen (K.T.) all in Germany; Servei de Pneumologia, Hospital Clnic
Institut dInvestigacions Biomdiques August Pi i SunyerCIBERES, Universitat de Barcelona, Barcelona (R.R.-R.); the Departments of
Clinical Research UK (L.T.) and Biometry and Data Management (H.F.), Boehringer Ingelheim, Bracknell, and the Institute of Ageing
and Chronic Disease, University Hospital Aintree, Liverpool (P.M.A.C.) both in the United Kingdom; Odense University Hospital,
Odense, Denmark (R.D.); the Department of Respiratory Diseases, University of Leuven, Leuven, Belgium (M.D.); UMR INSERM Unit
1067 CNRS 7733, Aix-Marseille Universit, Department of Respiratory Diseases and CIC Nord, Assistance PubliqueHpitaux de Marseille Hpital Nord, Marseille, France (P.C.); and the Department of Respiratory Medicine, Maastricht University Medical Center, Maastricht, the Netherlands (E.F.M.W.).
References
1. Rabe KF, Hurd S, Anzueto A, et al.
Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med
2007;176:532-55.
2. Vestbo J, Hurd SS, Agust AG, et al.
Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med
2013;187:347-65.
3. Wedzicha JA, Brill SE, Allinson JP,
Donaldson GC. Mechanisms and impact
of the frequent exacerbator phenotype in
chronic obstructive pulmonary disease.
BMC Med 2013;11:181.
4. Burge PS, Calverley PMA, Jones PW,
Spencer S, Anderson JA, Maslen TK. Randomised, double blind, placebo controlled
study of fluticasone propionate in patients
with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trial.
BMJ 2000;320:1297-303.
5. Calverley PMA, Anderson JA, Celli B,
et al. Salmeterol and fluticasone propionate and survival in chronic obstructive
pulmonary disease. N Engl J Med 2007;
356:775-89.
6. Vogelmeier C, Hederer B, Glaab T, et al.
Tiotropium versus salmeterol for the prevention of exacerbations of COPD. N Engl
J Med 2011;364:1093-103.
7. Tashkin DP, Celli B, Senn S, et al.
A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med
2008;359:1543-54.
8. Wedzicha JA, Calverley PMA, Seemungal TA, Hagan G, Ansari Z, Stockley RA.
The prevention of chronic obstructive pul-
1294
monary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med
2008;177:19-26.
9. Magnussen H, Watz H, Kirsten A, et al.
Stepwise withdrawal of inhaled corticosteroids in COPD patients receiving dual
bronchodilation: WISDOM study design
and rationale. Respir Med 2014;108:593-9.
10. Jones PW, Quirk FH, Baveystock CM,
Littlejohns P. A self-complete measure of
health status for chronic airflow limitation: the St. Georges Respiratory Questionnaire. Am Rev Respir Dis 1992;145:
1321-7.
11. de Torres JP, Pinto-Plata V, Ingenito E,
et al. Power of outcome measurements to
detect clinically significant changes in
pulmonary rehabilitation of patients with
COPD. Chest 2002;121:1092-8.
12. Miller MR, Hankinson J, Brusasco V,
et al. Standardisation of spirometry. Eur
Respir J 2005;26:319-38.
13. Global Initiative for Asthma. Global
strategy for asthma management and
prevention, revised 2014 (http://www
.ginasthma.org/local/uploads/files/
GINA_Report_2014_Jun11.pdf).
14. Jarad NA, Wedzicha JA, Burge PS, Calverley PMA. An observational study of inhaled corticosteroid withdrawal in stable
chronic obstructive pulmonary disease.
Respir Med 1999;93:161-6.
15. van der Valk P, Monninkhof E, van der
Palen J, Zielhuis G, van Herwaarden C. Effect of discontinuation of inhaled corticosteroids in patients with chronic obstructive pulmonary disease: the COPE study.
Am J Respir Crit Care Med 2002;166:135863.
16. Choudhury AB, Dawson CM, Kilving-
ton HE, et al. Withdrawal of inhaled corticosteroids in people with COPD in primary care: a randomised controlled trial.
Respir Res 2007;8:93.
17. Wouters EFM, Postma DS, Fokkens B,
et al. Withdrawal of fluticasone propionate from combined salmeterol/fluticasone treatment in patients with COPD
causes immediate and sustained disease
deterioration: a randomised controlled
trial. Thorax 2005;60:480-7.
18. Vestbo J, Anderson JA, Calverley PM,
et al. Bias due to withdrawal in long-term
randomised trials in COPD: evidence
from the TORCH study. Clin Respir J
2011;5:44-9.
19. Calverley PMA, Spencer S, Willits L,
Burge PS, Jones PW. Withdrawal from
treatment as an outcome in the ISOLDE
study of COPD. Chest 2003;124:1350-6.
20. Calverley PMA, Rabe KF, Goehring
U-M, Kristiansen S, Fabbri LM, Martinez FJ.
Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trials. Lancet 2009;374:68594. [Erratum, Lancet 2010;376:1146.]
21. Dransfield MT, Bourbeau J, Jones PW,
et al. Once-daily inhaled fluticasone furoate and vilanterol versus vilanterol only
for prevention of exacerbations of COPD:
two replicate double-blind, parallelgroup, randomised controlled trials. Lancet Respir Med 2013;1:210-23.
22. Jones PW. Estimation and application
of the minimum clinically important difference in COPD. Lancet Respir Med
2014;2:167-9.
Copyright 2014 Massachusetts Medical Society.
n engl j med 371;14nejm.orgoctober 2, 2014
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2016. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- UWorld NCLEX-RN QBank 2018 PDFDokumen103 halamanUWorld NCLEX-RN QBank 2018 PDFIlluminatis99% (90)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Part IIDokumen64 halamanPart IIhussainBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- SOAP NoteDokumen3 halamanSOAP NoteAuliya J'ga BontzBelum ada peringkat
- Obstructive JaundiceDokumen18 halamanObstructive JaundiceBellinda PaterasariBelum ada peringkat
- Key signs and symptoms of respiratory diseasesDokumen35 halamanKey signs and symptoms of respiratory diseasesEmereole FrancesBelum ada peringkat
- Human Respiratory SystemDokumen32 halamanHuman Respiratory SystemOyrik Mukhopadhyay100% (1)
- Berman Ch29 CrsDokumen24 halamanBerman Ch29 CrsKwena100% (1)
- Energy Medicine and DiabetesDokumen66 halamanEnergy Medicine and DiabetesSatinder Bhalla83% (6)
- 12 MRCP PACES Station 5 CasesDokumen23 halaman12 MRCP PACES Station 5 CasesTahir Ali100% (1)
- HAAD ExamDokumen17 halamanHAAD ExamDaniel Alvarez95% (22)
- Krok 2 2012-2019Dokumen59 halamanKrok 2 2012-2019Donya GholamiBelum ada peringkat
- 2Dokumen3 halaman2Tri Anna FitrianiBelum ada peringkat
- Mata 1Dokumen9 halamanMata 1Tri Anna FitrianiBelum ada peringkat
- NepalDokumen4 halamanNepalTri Anna FitrianiBelum ada peringkat
- QwertyDokumen1 halamanQwertyTri Anna FitrianiBelum ada peringkat
- Tension PneumothoraxDokumen18 halamanTension PneumothoraxTri Anna FitrianiBelum ada peringkat
- Nejmn 5Dokumen13 halamanNejmn 5Tri Anna FitrianiBelum ada peringkat
- A Case of Infant Accidental Hanging Caused by A Toy Strap: Ase ReportDokumen3 halamanA Case of Infant Accidental Hanging Caused by A Toy Strap: Ase ReportTri Anna FitrianiBelum ada peringkat
- Tension PneumothoraxDokumen18 halamanTension PneumothoraxTri Anna FitrianiBelum ada peringkat
- QwertyDokumen1 halamanQwertyTri Anna FitrianiBelum ada peringkat
- JP2012 630519 PDFDokumen10 halamanJP2012 630519 PDFFitriatun NisaBelum ada peringkat
- Nejm 4Dokumen19 halamanNejm 4Tri Anna FitrianiBelum ada peringkat
- Artikel Tri Anna Fitriani - H1a012060Dokumen8 halamanArtikel Tri Anna Fitriani - H1a012060Tri Anna FitrianiBelum ada peringkat
- Table 2 Preoperative Characteristics and Treatment of Patients Presenting With Complex Anal FistulaDokumen4 halamanTable 2 Preoperative Characteristics and Treatment of Patients Presenting With Complex Anal FistulaTri Anna FitrianiBelum ada peringkat
- Anthocyanins Induce Cholesterol Efflux From Mouse Peritoneal MacrophagesDokumen10 halamanAnthocyanins Induce Cholesterol Efflux From Mouse Peritoneal MacrophagesTri Anna FitrianiBelum ada peringkat
- 4Dokumen4 halaman4Tri Anna FitrianiBelum ada peringkat
- Anal Fistula: Results of Surgical Treatment in A Consecutive Series of PatientsDokumen5 halamanAnal Fistula: Results of Surgical Treatment in A Consecutive Series of PatientsTri Anna FitrianiBelum ada peringkat
- Jurnal 1 PDFDokumen7 halamanJurnal 1 PDFTri Anna FitrianiBelum ada peringkat
- Anthocyanin Prevents CD40-Activated Proinflammatory Signaling in Endothelial Cells by Regulating Cholesterol DistributionDokumen15 halamanAnthocyanin Prevents CD40-Activated Proinflammatory Signaling in Endothelial Cells by Regulating Cholesterol DistributionTri Anna FitrianiBelum ada peringkat
- Anthocyanin Prevents CD40-Activated Proinflammatory Signaling in Endothelial Cells by Regulating Cholesterol DistributionDokumen15 halamanAnthocyanin Prevents CD40-Activated Proinflammatory Signaling in Endothelial Cells by Regulating Cholesterol DistributionTri Anna FitrianiBelum ada peringkat
- Clinical Study: Nitroglycerin For Management of Retained Placenta: A Multicenter StudyDokumen7 halamanClinical Study: Nitroglycerin For Management of Retained Placenta: A Multicenter StudyTri Anna FitrianiBelum ada peringkat
- JurnalDokumen7 halamanJurnalTri Anna FitrianiBelum ada peringkat
- Burkitt's Lymphoma: Causing Obstructive Jaundice in An AdultDokumen3 halamanBurkitt's Lymphoma: Causing Obstructive Jaundice in An AdultTri Anna FitrianiBelum ada peringkat
- What Are The Markers of Aggressiveness in Prolactinomas? Changes in Cell Biology, Extracellular Matrix Components, Angiogenesis and GeneticsDokumen11 halamanWhat Are The Markers of Aggressiveness in Prolactinomas? Changes in Cell Biology, Extracellular Matrix Components, Angiogenesis and GeneticsTri Anna FitrianiBelum ada peringkat
- AnggurDokumen8 halamanAnggurTri Anna FitrianiBelum ada peringkat
- Gastrointestinal Motility Disorders: An Update: Brian E. Lacy Kirsten WeiserDokumen15 halamanGastrointestinal Motility Disorders: An Update: Brian E. Lacy Kirsten WeiserTri Anna FitrianiBelum ada peringkat
- TyrDokumen7 halamanTyrTri Anna FitrianiBelum ada peringkat
- 3 MAIN B February 23Dokumen13 halaman3 MAIN B February 23Student Access SLMC-IMBelum ada peringkat
- 06章(224 271)Dokumen48 halaman06章(224 271)zhangpengBelum ada peringkat
- Medicine All DIagnosis by AVI SeriesDokumen8 halamanMedicine All DIagnosis by AVI SeriesMuhammad Awais Hassan AwaanBelum ada peringkat
- Medical Terminology For Health Professions 7th Edition Ehrlich Test BankDokumen10 halamanMedical Terminology For Health Professions 7th Edition Ehrlich Test Bankphoebedavid2hqjgm100% (32)
- Pediarespi QuizDokumen1 halamanPediarespi QuizAlessa Mikkah BaltazarBelum ada peringkat
- Ards Case StudyDokumen1 halamanArds Case StudyLyons MacBelum ada peringkat
- Sir ClanDokumen109 halamanSir ClanJames AbendanBelum ada peringkat
- Cardiovascular Examination 1Dokumen43 halamanCardiovascular Examination 1ערין גבאריןBelum ada peringkat
- COPD Guide for GPsDokumen28 halamanCOPD Guide for GPseimearBelum ada peringkat
- Pleural Effusion Secondary To Community Acquired Pneumonia PathophysiologyDokumen5 halamanPleural Effusion Secondary To Community Acquired Pneumonia PathophysiologySteffiBelum ada peringkat
- AEBA QUESTIONS-WPS OfficeDokumen2 halamanAEBA QUESTIONS-WPS OfficeMarj Castor LisondraBelum ada peringkat
- Atypical Manifestations of Acute Coronary Syndrome - Throat Discomfort: A Multi-Center Observational StudyDokumen8 halamanAtypical Manifestations of Acute Coronary Syndrome - Throat Discomfort: A Multi-Center Observational StudyYo MeBelum ada peringkat
- Postoperative Care: Nursing ManagementDokumen25 halamanPostoperative Care: Nursing ManagementHarjotBrarBelum ada peringkat
- Abnormal Breathing PatternsDokumen5 halamanAbnormal Breathing PatternsJonalyn EtongBelum ada peringkat
- CCJM Symptom Management An Important Part of Cancer CareDokumen10 halamanCCJM Symptom Management An Important Part of Cancer CareBrian HarrisBelum ada peringkat
- COPD AsthmaDokumen16 halamanCOPD Asthma09172216507Belum ada peringkat
- BloatDokumen57 halamanBloatHari Krishnaa AthotaBelum ada peringkat
- Nursing Assessment of Patient with Acute Heart FailureDokumen5 halamanNursing Assessment of Patient with Acute Heart FailureShereen AlobinayBelum ada peringkat
- Acute Respiratory FailureDokumen28 halamanAcute Respiratory FailureMohamed Na3eemBelum ada peringkat
- Snakebite Severity Score Flowsheet Algorithm PDFDokumen2 halamanSnakebite Severity Score Flowsheet Algorithm PDFUmbu WindiBelum ada peringkat