Colecistitis Aguda Cirurgia
Diunggah oleh
joseaugustorojas9414Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Colecistitis Aguda Cirurgia
Diunggah oleh
joseaugustorojas9414Hak Cipta:
Format Tersedia
J Hepatobiliary Pancreat Surg (2007) 14:9197
DOI 10.1007/s00534-006-1161-x
Surgical treatment of patients with acute cholecystitis:
Tokyo Guidelines
Yuichi Yamashita1, Tadahiro Takada2, Yoshifumi Kawarada3, Yuji Nimura4, Masahiko Hirota5,
Fumihiko Miura2, Toshihiko Mayumi6, Masahiro Yoshida2, Steven Strasberg7, Henry A. Pitt8,
Eduardo de Santibanes9, Jacques Belghiti10, Markus W. Bchler11, Dirk J. Gouma12, Sheung-Tat Fan13,
Serafin C. Hilvano14, Joseph W.Y. Lau15, Sun-Whe Kim16, Giulio Belli17, John A. Windsor18, Kui-Hin Liau19,
and Vibul Sachakul20
1
Department of Surgery, Fukuoka University Hospital, Fukuoka University School of Medicine, 7-45-1 Nanakuma, Jonan-ku,
Fukuoka 814-0180, Japan
2
Department of Surgery, Teikyo University School of Medicine, Tokyo, Japan
3
Mie University School of Medicine, Mie, Japan
4
Division of Surgical Oncology, Department of Surgery, Nagoya University Graduate School of Medicine, Nagoya, Japan
5
Department of Gastroenterological Surgery, Kumamoto University Graduate School of Medical Science, Kumamoto, Japan
6
Department of Emergency Medicine and Critical Care, Nagoya University School of Medicine, Nagoya, Japan
7
Washington University in St Louis and Barnes-Jewish Hospital, St Louis, USA
8
Department of Surgery, Indiana University School of Medicine, Indianapolis, USA
9
Department of Surgery, University of Buenos Aires, Buenos Aires, Argentina
10
Hepatobiliopancreatic Surgery and Liver Transplantation, Hospital Beaujon, Clichy, France
11
Department of Surgery, University of Heidelberg, Heidelberg, Germany
12
G4-116, Academic Medical Center, Amsterdam, The Netherlands
13
Department of Surgery, The University of Hong Kong, Pokfulam, Hong Kong, China
14
Department of Surgery, Philippine General Hospital, University of the Philippines, Manila, Philippines
15
Department of Surgery, The Chinese University of Hong Kong, Hong Kong, China
16
Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
17
General and HPB Surgery, Loreto Nuovo Hospital, Naples, Italy
18
Department of Surgery, The University of Auckland, Auckland, New Zealand
19
Department of Surgery, Tan Tock Seng Hospital / Hepatobiliary Surgery, Medical Centre, Singapore, Singapore
20
Department of Surgery, Phramongkutklao Hospital, Bangkok, Thailand
Abstract
Cholecystectomy has been widely performed in the treatment
of acute cholecystitis, and laparoscopic cholecystectomy has
been increasingly adopted as the method of surgery over the
past 15 years. Despite the success of laparoscopic cholecystectomy as an elective treatment for symptomatic gallstones,
acute cholecystitis was initially considered a contraindication
for laparoscopic cholecystectomy. The reasons for it being
considered a contraindication were the technical difficulty of
performing it in acute cholecystitis and the development of
complications, including bile duct injury, bowel injury, and
hepatic injury. However, laparoscopic cholecystectomy is now
accepted as being safe for acute cholecystitis, when surgeons
who are expert at the laparoscopic technique perform it. Laparoscopic cholecystectomy has been found to be superior to
open cholecystectomy as a treatment for acute cholecystitis
because of a lower incidence of complications, shorter length
of postoperative hospital stay, quicker recuperation, and earlier return to work. However, laparoscopic cholecystectomy
for acute cholecystitis has not become routine, because the
timing and approach to the surgical management in patients
with acute cholecystitis is still a matter of controversy. These
Guidelines describe the timing of and the optimal surgical
Offprint requests to: Y. Yamashita
Received: May 31, 2006 / Accepted: August 6, 2006
treatment of acute cholecystitis in a question-and-answer
format.
Key words Acute cholecystitis Cholecystectomy Laparoscopic cholecystectomy Open surgery Cholecystostomy
Guidelines
Introduction
Cholecystectomy has been widely accepted as an effective treatment for acute cholecystitis. Several studies
conducted during the era of open cholecystectomy
demonstrated the advantages of early cholecystectomy
for patients with acute cholecystitis its safety, costeffectiveness, and the rapid return of the patient to
normal activity (level 1b).13 Although acute cholecystitis had initially been considered a contraindication to
laparoscopic cholecystectomy because of the higher incidence of complications than in non-acute cholecystitis
(level 2b),4 as a result of the mastery of the required
skills by surgeons and the improvements in laparoscopic
instruments, laparoscopic cholecystectomy is now accepted as safe when surgeons who are expert in laparoscopic techniques perform it. Some recent randomized
92
Y. Yamashita et al.: Surgical treatment for acute cholecystitis
clinical trials (level 1b)59 have addressed the timing and
surgical approach to the gallbladder in patients with
acute cholecystitis, and the results have indicated
that laparoscopic cholecystectomy was associated with
a shorter hospital stay, more rapid recovery, and a reduction in the overall cost of treatment, and that early
laparoscopic cholecystectomy was sufficiently safe to be
performed routinely.
Nevertheless, urgent or early laparoscopic cholecystectomy for acute cholecystits seems to remain unpopular, and the reasons for its unpopularity include a lack
of availability of surgeons who have mastered the necessary skills, as well as the limited availability of operating
room space (level 2c).10,11
Critically ill patients with acute cholecystitis often
present a difficult therapeutic dilemma. Although they
require emergency surgical intervention, many such patients have a serious medical or surgical complication
and may be too ill to undergo open or laparoscopic
cholecystectomy under general anesthesia. By avoiding
the risks of cholecystectomy, drainage by cholecystostomy offers a distinct advantage in such critically ill
patients, but the optimal timing of subsequent surgery
has not been examined. These Guidelines describe the
timing and optimal type of surgical treatment for acute
cholecystitis in a question-and-answer format.
the gallbladder in patients with acute cholecystitis, and
the results have indicated that laparoscopic cholecystectomy performed during the first admission was associated with a shorter hospital stay, quicker recovery, and
reduction in overall cost of treatment compared to open
cholecystectomy. Early laparoscopic cholecystectomy
is now accepted to be sufficiently safe for routine use,
because earlier reports of increased risk of bile duct
injury (level 4)14 have not been substantiated by more
recent experience (level 1b).5,7,8,15
The results of a randomized controlled trial comparing early laparoscopic cholecystectomy after admission
with delayed laparoscopic cholecystectomy showed that
performing the surgery early was superior in terms of a
lower conversion rate to open surgery and shorter total
hospital stay (Table 1). These results indicate that early
laparoscopic cholecystectomy is preferable in patients
with acute cholecystitis.
However, the fact that the above trials excluded patients with pan-peritonitis caused by perforation of the
gallbladder, patients with common bile duct stones, and
those with concomitant severe cardiopulmonary disease
should be borne in mind when evaluating the results.
After evaluation of patients overall condition and
confirmation of the diagnosis by ultrasonography, computed tomography (CT), and/or magnetic resonance
cholargio-parcreatography (MRCP), the timing of the
surgical management of acute cholecystitis patients
should be immediately decided by experienced surgeons (level 5).16
Q1. When is the optimal time for cholecystectomy in
acute cholecystitis?
Cholecystectomy is preferable early after admission (recommendation A).
Randomized controlled trials in the open cholecystectomy era, comparing early surgery with delayed surgery
in the 1970s1980s, found that early surgery had the
advantages of less blood loss, a shorter operation time,
a lower complication rate, and a briefer hospital stay
(level 1b)13,12 (level 3b).13
Some recent randomized clinical trials (level 1b)59
have addressed the timing of and surgical approach to
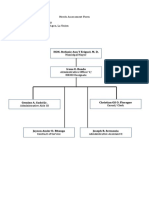
Outcome of the Tokyo Consensus Meeting
The panelists voted on the timing of cholecystectomy in
patients with grade 1 (mild) and 2 (moderate) acute
cholecystitis. The results showed that 72% of doctors
from abroad and 33% of Japanese doctors agreed with
early cholecystectomy, but 28% of the doctors from
abroad and 41% of the Japanese doctors voted that
minor modification of the guideline was needed, and
none of the doctors from abroad and 26% of Japanese
doctors disagreed with early timing (Fig. 1).
Table 1. Comparisons of early and delayed laparoscopic cholecystectomy for acute cholecystitis
Author
Lo et al.5
Lai et al.6
Chandler et al.7
Johansson et al.15
Number
of patients
Conversion
rate of
early LC
Conversion
rate of
delayed LC
Postoperative
complications
of early LC
Length of
Postoperative
complications
of delayed LC
Length of
hospital stay
(days) Early
surgery
hospital stay
(days) Delayed
surgery
86
91
43
143
11%
21%
24%
31%
23%
24%
36%
29%
13%
9%
4%
18%
29%
8%
9%
10%
6
7.6
5.4
5
11
11.6
7.1
8
LC, laparoscopic cholecystectomy; conversion rate, conversion rate to open surgery
Y. Yamashita et al.: Surgical treatment for acute cholecystitis
Panelists from abroad
93
Japanese panelists
26%
28%
33%
72%
41%
Fig. 1. Timing of cholecystectomy for
acute cholecystitis. Votes on the
proposed guideline: cholecystectomy is
preferable early after admission
Yes
Yes, but needs minor modification
No
Panelists from abroad
Japanese panelists
8%
7%
30%
31%
63%
Yes
Yes, but needs minor modification
No
Q2. Which surgical procedure should be adopted,
laparoscopic cholecystectomy or open
cholecystectomy?
Laparoscopic cholecystectomy is preferable to
open cholecystectomy (recommendation A).
Cholecystectomy has been widely performed to treat
acute cholecystitis, with laparoscopic cholecystectomy
having been increasingly adopted over the past 10 years.
Several reports of complications associated with early
laparoscopic cholecystectomy caused a transient wane
in the enthusiasm for early laparoscopic cholecystectomy (level 4),14 (level 2b),17 (level 4),18,19 but such concerns were allayed by evidence indicating that early
laparoscopic cholecystectomy for patients with acute
cholecystitis was safe and effective, and required a
shorter hospitalization time (level 1b)8,9 (level 2b)20,21
(level 3b)22 (level 4).23 Thus, increased experience with
61%
Fig. 2. Surgical procedure for the treatment of acute cholecystitis. Votes on
the proposed guideline: laparoscopic
cholecystectomy is preferable to open
cholecystectomy
laparoscopic surgery has led to laparoscopic cholecystectomy becoming as good as, or safer than, open cholecystectomy for the treatment of acute cholecystitis
(level 1b).8 Although early cholecystectomy for acute
cholecystitis has remained unpopular (level 2c),10,11 if
early cholecystectomy is performed early laparoscopic
cholecystectomy is the preferable procedure.
Because the set of skills required for laparoscopic
cholecystectomy is different from the set required for
conventional open cholecystectomy, only surgeons who
possess that set of skills in laparoscopic cholecystectomy
should perform it. The surgeon should be aware of the
complications (described later in Q4) that have been
associated with the laparoscopic procedure and should
take maximum care to prevent bile duct injury, which
sometimes lead to serious complications. The surgeon
should never hesitate to convert to open cholecystectomy to prevent severe complications, if the anatomy
94
Y. Yamashita et al.: Surgical treatment for acute cholecystitis
of Calots triangle remains unclear despite accurate
dissection.
Decompression of an acutely inflamed gallbladder
may not only allow the patient time to recover from the
acute illness prior to surgery, but may decrease the technical difficulty of cholecystectomy. Open cholecystostomy under local anesthesia is a traditional practice that
provides an alternative to cholecystectomy in critically
ill patients with acute cholecystitis (level 4),24 but percutaneous cholecystostomy has now become a valuable
alternative procedure for decompressing an acutely inflamed gallbladder.
some patients with moderate (grade II) acute cholecystitis, it is difficult to remove the gallbladder surgically,
because of severe inflammation limited to the gallbladder. The severe local inflammation of the gallbladder
is evaluated according to factors such as more than 72 h
from the onset, wall thickness of the gallbladder of
more than 8 mm, and a WBC count of more than 18 000.
Continuous medical treatment or drainage of the contents of a swollen gallbladder by percutaneous transhepatic gallbladder drainage (PTGBD) or surgical
cholecystostomy is the optimal treatment, with delayed
cholecystectomy indicated after the inflammation of
the gallbladder resolves. Urgent management of severe
(grade III) acute cholecystitis is always necessary, because the patients have organ dysfunction, and drainage of the gallbladder contents and/or cholecystectomy
is required to treat the severe inflammation of the gallbladder. Urgent or early cholecystectomy is required
after improvement of patients general condition.
Out come of the Tokyo Consensus Meeting
Voting for laparoscopic cholecystectomy is preferable
to open cholecystectomy showed that 63% of the doctors from abroad and 61% of the Japanese doctors
agreed with this; 30% of the doctors from abroad and
31% of the Japanese doctors voted that they agreed, but
that minor modification of the guideline was needed;
while 7% of the doctors from abroad and 8% of the
Japanese doctors disagreed (Fig. 2).
Q4. What are the complications of laparoscopic
cholecystectomy to be avoided?
Bile duct injury and injury of other organs.
Q3. What is the optimal surgical treatment for acute
cholecystitis according to grade of severity?
Mild (grade I) acute cholecystitis: early laparoscopic cholecystectomy is the preferred
procedure.
Moderate (grade II) acute cholecystitis: early
cholecystectomy is performed. However, if patients have severe local inflammation, early gallbladder drainage (percutaneous or surgical) is
indicated. Because early cholecystectomy may be
difficult, medical treatment and delayed cholecystectomy are necessary.
Severe (grade III) acute cholecystitis: urgent
management of organ dysfunction and management of severe local inflammation by gallbladder
drainage and/or cholecystectomy should be carried out. Delayed elective cholecystectomy should
be performed later, when cholecystectomy is
indicated.
Treatment of acute cholecystitis essentially consists of
early cholecystectomy, and the optimal surgical treatment for each grade of severity of acute cholecystitis
is required. Early laparoscopic cholecystectomy is indicated for patients with mild (grade I) acute cholecystitis, because laparoscopic cholecystectomy can be
performed in most these patients. Early laparoscopic
or open cholecystectomy (within 72 h of the onset of
acute cholecystitis) is generally required for patients
with moderate (grade II) acute cholecystitis, but in
Complications of laparoscopic cholecystectomy were
reported soon after its introduction, and consist of bile
duct injury, bowel injury, and hepatic injury, as well
as the common complications of conventional open
cholecystectomy, such as wound infection, ileus, intraperitoneal hemorrhage, atelectasis, deep vein thrombosis, and urinary tract infection. Bile duct injury is
considered a serious complication. Bowel and hepatic
injuries should be avoided as they are also serious complications (level 2b).25 These injuries have been attributable to the limitations of laparoscopy, such as the narrow
view and the lack of tactile manipulation. Laparoscopic
cholecystectomy has not always been associated with a
higher incidence of complications than open cholecystectomy, but any serious complication that requires reoperation and prolonged hospitalization may become a
serious problem for patients who firmly believe that
laparoscopic cholecystectomy is less invasive. The incidence of biliary injury has recently decreased in association with the acquisition of greater surgical skills and
the improvements in laparoscopic instruments.
Q5. When is the optimal time for conversion from
laparoscopic to open cholecystectomy?
To prevent injuries, surgeons should never hesitate to convert to open surgery when they
experience difficulty in performing laparoscopic
cholecystectomy.
Y. Yamashita et al.: Surgical treatment for acute cholecystitis
There is a relatively high rate of conversion from laparoscopic cholecystectomy to open cholecystectomy
for acute cholecystitis because of technical difficulties,
and laparoscopic cholecystectomy is associated with a
high complication rate (level 3b).22 Although certain
preoperative factors, such as male sex, previous
abdominal surgery, presence or history of jaundice,
advanced cholecystitis, and infectious complications
are associated with a need for conversion from laparoscopic to open cholecystectomy, they have limited
predictive ability (level 3b).22,26,27 Surgeons find factors
that lead them to decide whether to convert to
open cholecystectomy mostly during the laparoscopic
cholecystectomy. Not only the experience of the surgeon but also the experience of the institution with
laparoscopic cholecystectomy is a prerequisite for successful cholecystectomy for all patients with acute
cholecystitis.
Because conversion to open cholecystectomy is not
disadvantageous for patients, to prevent intraoperative
accidents and postoperative complications, surgeons
should never hesitate to convert when they experience
difficulty in performing laparoscopic cholecystectomy.
A low threshold for conversion to open cholecystectomy is important to minimize the risk of major
complications.
Q6. When is the optimal time for cholecystectomy
following PTGBD?
Early cholecystectomy during the initial hospital
stay is preferable (recommendation B).
There have been no randomized controlled trials of
surgical management in patients with acute cholecystitis
after PTGBD. However, PTGBD is known to be an
effective option in critically ill patients, especially in
elderly patients and patients with complications (level
4).28 Cholecystectomy is often performed at an interval
of several days following PTGBD. Early cholecystectomy following PTGBD is preferable when the patients
condition improves, and if the patient has no complications. Complications of PTGBD, such as intrahepatic
hematoma, pericholecystic abscess, biliary pleural effusion, and biliary peritonitis (which may be caused by
puncture of the liver and migration of the catheter)
sometimes occur (level4)29 and efforts should be made
to prevent such occurrences. More case-series studies
are required.
95
Q7. When is the optimal time for laparoscopic cholecystectomy after endoscopic stone extraction in
patients with cholecysto-choledocholithiasis?
Early cholecystectomy following endoscopic stone
extraction during the same hospital stay is preferable (recommendation B).
Combining endoscopic stone extraction during endoscopic retrograde cholangiography with laparoscopic
cholecystectomy has been found to be a useful means
of treating patients with cholecysto-choledocholithiasis.
However, the optimal time for laparoscopic cholecystectomy following endoscopic stone extraction (ESE) is
still a matter of controversy. There have been several
reports of combinations of ESE and laparoscopic cholecystectomy (level 2b),30 (level4),3133 and in most of
them, the interval between the two procedures was a
few days. Actually, the interval between ESE and laparoscopic cholecystectomy was left to the individual surgeon. At present, early laparoscopic cholecystectomy
following ESE during the same hospital stay is regarded
as preferable in most patients without complications
related to ESE.
Acknowledgments. We would like to express our deep
gratitude to the Japanese Society for Abdominal Emergency Medicine, the Japan Biliary Association, and the
Japanese Society of Hepato-Biliary-Pancreatic Surgery,
who provided us with great support and guidance in
the preparation of the Guidelines. This process was
conducted as part of the Project on the Preparation
and Diffusion of Guidelines for the Management of
Acute Cholangitis (H-15-Medicine-30), with a research
subsidy for fiscal 2003 and 2004 (Integrated Research
Project for Assessing Medical Technology) sponsored
by the Japanese Ministry of Health, Labour, and
Welfare.
We also truly appreciate the panelists who cooperated with and contributed significantly to the International Consensus Meeting, held in Tokyo on April 1 and
2, 2006.
References
1. Lahtinen J, Alhava EM, Aukee S. Acute cholecystitits treated by
early and delayed surgery. A controlled clinical trial. Scand J
Gastroenterol 1978;13:6738. (level 1b)
2. Jarvinen HJ, Hastbacka J. Early cholecystectomy for acute cholecystitis: a prospective randomized study. Ann Surg 1980;191:
5015. (level 1b)
3. Norrby S, Herlin P, Holmin T, Sjodahl R, Tagesson C. Early or
delayed cholecystectomy in acute cholecystitis? A clinical trial. Br
J Surg 1983;70:1635. (level 1b)
4. Cushieri A, Dubois F, Mouiel J, Mouiel P, Becker H, Buess G,
et al. The European experience with laparoscopic cholecystectomy. Am J Surg 1991;161:3857. (level 2b)
96
Y. Yamashita et al.: Surgical treatment for acute cholecystitis
5. Lo CM, Liu Cl, Fan ST, Lai EC, Wong J. Prospective randomized
study of early versus delayed laparoscopic cholecystectomy for
acute cholecystitis. Am Surg 1998;227:4617. (level 1b)
6. Lai PB, Kwong KH, Leung KL, Kwok SP, Chan AC, Chung SC.
Randomized trial of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg 1998;85:7647.
(level 1b)
7. Chandler CF, Lane JS, Ferguson P, Thonpson JE. Prospective
evaluation of early versus delayed laparoscopic cholecystectomy
for the treatment of acute cholecystitis. Am Surg 2000;66:896900.
(level 1b)
8. Kiviluoto T, Siren J, Luukkonen P, Kivilaakso E. Randomized
trial of laparoscopic versus open cholecystectomy for acute and
gangrenous cholecystitis. Lancet 1998;351:321325. (level 1b)
9. Berrgren U, Gordh T, Grama D, Haglund U, Rastad J, Arvidsson
D. Laparoscopic versus open cholecystectomy: hospitalization,
sick leave, analgesia and trauma responses. Br J Surg 1994;81:
13625. (level 1b)
10. Senapati PSP, Bhattarcharya D, Harinath G, Ammori BJ. A survey of the timing and approach to the surgical management of
cholelithiasis in patients with acute biliary pancreatitis and acute
cholecystitis in the UK. Ann R Coll Surg Engl 2003;85:30612.
(level 2c)
11. Cameron IC, Chadwick C, Phillips J, Johnson AG. Management
of acute cholecystitis in UK hospitals: time for a charge. Postgrad
Med J 2004;80:2924. (level 2c)
12. van der Linden W, Sunzel H. Early versus delayed operation
for acute cholecystitis. A controlled clinical trial. Am J Surg
1970;120:713. (level 1b)
13. van der Linden W, Edlund G. Early versus delayed cholecystectomy: the effect of a change in management. Br J Surg 1981;68:
7537. (level 3b)
14. Kum CK, Eypasch E, Lefering R, Math D, Paul A, Neugebauer
E, et al. Laparoscopic cholecystectomy for acute cholecystitis: is
it really safe? World J Surg 1996;20:439. (level 4)
15. Johansson M, Tbune A, Blomqvist A, Nelvin L, Lundell L. Management of acute cholecystitis in the laparoscopic era: results of
a prospective, randomized clinical trial. J Gastrointest Surg
2003;7:6425. (level 1b)
16. Mason GR. Acute cholecystitis; surgical aspects. In: Berk JE, editor. 4th ed. Philadelphia: WB Saunders; 1985. p.361618. (level
5)
17. Russell JC, WaIsh SJ, Mattie AS, Lynch JT. Bile duct injuries,
19891993. A statewide experience. Arch Surg 1996;131:3828.
(level 2b)
18. Branum G, Schmtt C, Baillie J. Management of major biliary
complications after laparoscopic cholecystectomy. Ann Surg
1993;217:53240. (level 4)
19. Bender JS, Zenilman ME. Immediate laparoscopic cholecystectomy as definitive therapy for acute cholecystitis. Surg Endosc
1995;9:10818. (level 4)
20. Zacks SL, Sandler RS, Rutledge R, Brown RS. A populationbased cohort study comparing laparoscopic cholecystectomy and
open cholecystectomy. Am J Gastroenterol 2002;97:33440. (level
2b)
21. Flowers JL, Bailey RW, Scovill WA, Zucker KA. The Baltimore
experience with laparoscopic management of acute cholecystitis.
Am J Surg 1991;161:38892. (level 2b)
22. Eldar S, Sabo E, Nash E, Abrahamson J, Matter I. Laparoscopic
cholecystectomy for acute cholecystitis: prospective trial. World
J Surg 1997;21:5405. (level 3b)
23. Cox MR, Wilson TG, Luck AJ, Leans PL, Padbury RTA, Toouli
J. Laparoscopic cholecystectomy for acute inflammation of the
gallbladder. Ann Surg 1993;218:6304. (level 4)
24. Glenn F. Cholecystostomy in the high risk patient with biliary
tract disease. Ann Surg 1977;185:18591. (level 4)
25. The Southern Surgeons Club. A prospective analysis of 1518
laparoscopic cholecystectomies. N Engl J Med 1991;324:10738.
(level 2b)
26. Brodsky A, Matter I, Sabo E, Cohen A, Abrahamson J, Eldar S.
Laparoscopic cholecystectomy for acute cholecystitis: can the
need for conversion and the probability of complications be
predicted? Surg Endosc 2000;14:75560. (level 3b)
27. Kama NA, Doganay M, Dolapci E, Reis E, Ati M, Kologlu M.
Risk factors resulting in conversion of laparoscopic cholecystectomy to open surgery. Surg Endosc 2001;15:9658. (level 3b)
28. Tseng LJ, Tsai CC, Mo LR, Lin RC, Kuo JY, Chang KK, et al.
Palliative percutaneous transhepatic gallbladder drainage of gallbladder empyema before laparoscopic cholecystectomy. Hepato
gastroenterology 2000;47:9326. (level 4)
29. Kivinen H, Makela JT, Autio R, Tikkakoski T, Leinonen S,
Siniluoto T, et al. Percutaneous cholecystostomy in acute cholecystitis in high-risk patients: an analysis of 69 patients. Int Surg
1998;83:299302. (level 4)
30. Cuschieri A, Crose E, Faggioni A, Jakimowicz J, Lacy A, Lezoche
E, et al. EAES ductal stone study. Preliminary findings of multicenter prospective randomized trial comparing two-stage vs
single-stage management. Surg Endosc 1996;10:11305. (level
2b)
31. Sarli L, Iusco DR, Roncoroni L. Preoperative endoscopic sphincterotomy and laparoscopic cholecystectomy for the management
of cholecystocholedocholithiasis: 10-year experience. World J
Surg 2003;27:1806. (level 4)
32. Basso N, Pizzuto G, Surgo D, Materia A, Silecchia G, Fantini A,
et al. Laparoscopic cholecystectomy and intraoperative endoscopic sphincterotomy in the treatment of cholecysto-choledocholithiasis. Gastrointest Endosc 1999;50:5325. (level 4)
33. Cemachovic I, Letard JC, Begin GF, Rousseau D, Nivet LM.
Intraoperative endoscopic sphincterotomy is a reasonable option
for complete single-stage minimally invasive biliary stone treatment: short-term experience with 57 patients. Endoscopy
2000;32:95662. (level 4)
Discussion at the Tokyo Consensus Meeting
Severity of acute cholecystitis
There has been some high-quality evidences obtained
by randomized controlled trials (RCTs) in the field of
surgical treatment for acute cholecystitis. However, no
RCTs have examined the optimal surgical treatment
for acute cholecystitis according to grade of severity.
The need for surgical treatment according to grade of
severity was suggested by panelists, and surgical treatment strategies were discussed.
Steven Strasberg (USA) proposed grading the
severity of acute cholecystitis as mild (grade I),
moderate (grade II), and severe (grade III).
Early cholecystectomy for acute cholecystitis
There were some important remarks in the discussion
of the concept that early cholecystectomy during the
first admission is preferable. These remarks were that:
(a) it is necessary to know whether the numbers of patients in the RCTs were sufficient to evaluate the incidence of serious complications such as bile duct injury,
(b) it is important to know whether all of the surgeons
who performed cholecystectomy in the RCTs possessed
the skills for laparoscopic surgery, (c) early cholecys-
Y. Yamashita et al.: Surgical treatment for acute cholecystitis
97
tectomy was not defined in any of the RCTs, (d) surgical treatments for acute cholecystitis of each grade
of severity should be stated individually in these
Guidelines.
On the basis of these remarks, the panelists voted
on the timing of cholecystectomy in patients with mild
(grade I) and moderate (grade II) acute cholecystitis.
None of the doctors from abroad disagreed with early
cholecystectomy. In contrast, 26% of the Japanese doctors disagreed with it. Thus, the results of the votes of
the doctors from abroad and the Japanese doctors
differed.
line was needed; only a few percent of both groups of
doctors disagreed. Thus, laparoscopic cholecystectomy
for mild (grade I) and moderate (grade II) acute cholecystitis, except in patients with localized severe inflammation of the gallbladder, was approved of by many
doctors in both groups.
Laparoscopic cholecystectomy for acute cholecystitis
There were some important remarks in the discussion
of the concept that laparoscopic cholecystectomy was
superior to open cholecystectomy. They were: (a) laparoscopic cholecystectomy is associated with a greater
risk of bile duct injury, (b) laparoscopic cholecystectomy should be performed by experienced surgeons, and
(c) the majority of acute cholecystitis patients treated
surgically have mild (grade I) acute cholecystitis.
The vote on the cholecystectomy procedure was performed on the basis of the above remarks. Voting for
laparoscopic cholecystectomy is preferable to open
cholecystectomy showed that approximately 60% of
both Japanese and overseas doctors agreed, and approximately 30% of both groups of doctors voted that
they agreed, but that minor modification of the guide-
Cholecystectomy for acute cholecystitis
The results of the voting on the timing and surgical
procedure for mild (grade I) and moderate (grade II)
acute cholecystitis are described above. There was an
important remark during the discussion, that patients
in whom it is difficult to remove the gallbladder are
frequently encountered among patients with moderate
(grade II) acute cholecystitis, and that removal of the
gallbladder, especially by laparoscopic cholecystectomy, is difficult in such patients. This remark was agreed
with by many panelists at the Meeting, and it was concluded that if patients have severe local inflammation
of the gallbladder, early gallbladder drainage (percutaneous or surgical) is the initial treatment of choice.
Because early cholecystectomy may be difficult,
medical treatment and delayed cholecystectomy are
performed.
The fact that there was a consensus among the doctors from abroad and Japanese doctors concerning the
surgical treatment strategy for moderate (grade II)
acute cholecystitis facilitated the drafting of the
Guideline.
Anda mungkin juga menyukai
- Journal ReadingDokumen8 halamanJournal ReadingAnonymous Uh2myPxPHBelum ada peringkat
- Jurnal 3 AppDokumen4 halamanJurnal 3 AppmaulidaangrainiBelum ada peringkat
- Huang2020 Article ComparisonOfEmergencyCholecystDokumen14 halamanHuang2020 Article ComparisonOfEmergencyCholecystLerdsin PlasticBelum ada peringkat
- Guias Tokio 1Dokumen8 halamanGuias Tokio 1Maria Elena VinuezaBelum ada peringkat
- 2015 Laparoscopic Surgery in Abdominal Trauma A Single Center Review of A 7-Year ExperienceDokumen7 halaman2015 Laparoscopic Surgery in Abdominal Trauma A Single Center Review of A 7-Year ExperiencejohnnhekoBelum ada peringkat
- International Journal of Surgery: Original ResearchDokumen9 halamanInternational Journal of Surgery: Original ResearchrejBelum ada peringkat
- 01 HepatogastroDokumen3 halaman01 Hepatogastroyacine26Belum ada peringkat
- 9 Management of Common Bile-Duct Stones and Associated Gallbladder Stones: Surgical AspectsDokumen14 halaman9 Management of Common Bile-Duct Stones and Associated Gallbladder Stones: Surgical AspectsekoBelum ada peringkat
- Ahbps-24-44 Appendicitis After Liver Transplantation JournalDokumen8 halamanAhbps-24-44 Appendicitis After Liver Transplantation JournalIndah JamtaniBelum ada peringkat
- Ileus Obstruksi PDFDokumen20 halamanIleus Obstruksi PDFherfikaBelum ada peringkat
- Versus: Laparoscopic Open Appendectomy: Which Way To Go?Dokumen6 halamanVersus: Laparoscopic Open Appendectomy: Which Way To Go?Claudiu Ungureanu ClauBelum ada peringkat
- Laparoscopic Appendectomy PDFDokumen4 halamanLaparoscopic Appendectomy PDFdydydyBelum ada peringkat
- CHOLESISTITISDokumen6 halamanCHOLESISTITISEka KusumaningatiBelum ada peringkat
- 268 2011 Article 1088 PDFDokumen6 halaman268 2011 Article 1088 PDFIoel Tovar TrovaBelum ada peringkat
- Appendicitis After Liver Transplantation Presentation of JournalDokumen16 halamanAppendicitis After Liver Transplantation Presentation of JournalIndah JamtaniBelum ada peringkat
- Overview of Management of Mechanical Small Bowel Obstruction in Adults - UpToDateDokumen19 halamanOverview of Management of Mechanical Small Bowel Obstruction in Adults - UpToDateDesak PramestiBelum ada peringkat
- Management of Acute Cholecystitis in UK Hospitals: Time For A ChangeDokumen4 halamanManagement of Acute Cholecystitis in UK Hospitals: Time For A ChangeRana BishwoBelum ada peringkat
- Bahasa IndonesiaDokumen4 halamanBahasa IndonesiaNadiah Umniati SyarifahBelum ada peringkat
- Ambulatory Laparoscopic CholecystectomyDokumen6 halamanAmbulatory Laparoscopic CholecystectomyJesús ReyesBelum ada peringkat
- The Incidence and Risk of Early Postoperative Small Bowel Obstruction After Laparoscopic Resection For Colorectal Cancer 2014Dokumen7 halamanThe Incidence and Risk of Early Postoperative Small Bowel Obstruction After Laparoscopic Resection For Colorectal Cancer 2014alemago90Belum ada peringkat
- Sumber Jurnal ReadingDokumen15 halamanSumber Jurnal ReadingagungBelum ada peringkat
- Surgical Management of Acute CholecystitisDokumen17 halamanSurgical Management of Acute Cholecystitisgrayburn_1Belum ada peringkat
- Pattern of Acute Intestinal Obstruction: Is There A Change in The Underlying Etiology?Dokumen4 halamanPattern of Acute Intestinal Obstruction: Is There A Change in The Underlying Etiology?neildamiBelum ada peringkat
- Safe Laparoscopic Cholecystectomy FinaleDokumen5 halamanSafe Laparoscopic Cholecystectomy FinalenipolinBelum ada peringkat
- World Journal of Emergency Surgery: Emergency Laparoscopy - Current Best PracticeDokumen9 halamanWorld Journal of Emergency Surgery: Emergency Laparoscopy - Current Best PracticeHendra JojoBelum ada peringkat
- Art07 PDFDokumen6 halamanArt07 PDFadan2010Belum ada peringkat
- Guidelines For The Clinical Application of Laparoscopic Biliary Tract SurgeryDokumen37 halamanGuidelines For The Clinical Application of Laparoscopic Biliary Tract SurgeryTerence SalazarBelum ada peringkat
- Predictive Factors For Conversion of Laparoscopic CholecystectomyDokumen4 halamanPredictive Factors For Conversion of Laparoscopic CholecystectomyGilang IrwansyahBelum ada peringkat
- Alameldeen 2018Dokumen7 halamanAlameldeen 2018Pallavi SutarBelum ada peringkat
- Periop UrologyKoubaartikelDokumen4 halamanPeriop UrologyKoubaartikeljustin_saneBelum ada peringkat
- HPB2010 791625Dokumen6 halamanHPB2010 791625ocramusBelum ada peringkat
- Original Article Reasons of Conversion of Laparoscopic To Open Cholecystectomy in A Tertiary Care InstitutionDokumen5 halamanOriginal Article Reasons of Conversion of Laparoscopic To Open Cholecystectomy in A Tertiary Care InstitutionLuis Carlos Moncada TorresBelum ada peringkat
- Chole - Protocol - V1-14, Birmingham, UK PDFDokumen23 halamanChole - Protocol - V1-14, Birmingham, UK PDFWorku KifleBelum ada peringkat
- Closure of Loop Ileostomy Potentially ADokumen7 halamanClosure of Loop Ileostomy Potentially Ashah hassaanBelum ada peringkat
- Effects of Timing of Appendectomy On The Risks of Perforation and Postoperative Complications of Acute AppendicitisDokumen9 halamanEffects of Timing of Appendectomy On The Risks of Perforation and Postoperative Complications of Acute AppendicitisLydia EniithBelum ada peringkat
- 1 Bjs 10662Dokumen8 halaman1 Bjs 10662Vu Duy KienBelum ada peringkat
- Laparoscopy in The Acute AbdomenDokumen15 halamanLaparoscopy in The Acute AbdomenDragoiu AlexandraBelum ada peringkat
- Appendiceal Mass: Is Interval Appendicectomy "Something of The Past"?Dokumen4 halamanAppendiceal Mass: Is Interval Appendicectomy "Something of The Past"?galihmuchlishermawanBelum ada peringkat
- Laparoscopic Appendectomy PostoperativeDokumen6 halamanLaparoscopic Appendectomy PostoperativeDamal An NasherBelum ada peringkat
- Assessing Clinical Outcomes of Patients With AcuteDokumen7 halamanAssessing Clinical Outcomes of Patients With AcuteAdrian BăloiBelum ada peringkat
- 3Dokumen8 halaman3polomska.kmBelum ada peringkat
- Randomized Comparison of SubcuDokumen11 halamanRandomized Comparison of SubcuRafael MarvinBelum ada peringkat
- Corto y Largo PlazoDokumen6 halamanCorto y Largo PlazoElard Paredes MacedoBelum ada peringkat
- Violation of Water-Electric Exchange in Patients With Nospecific Ulcerative Colitis Before Total ColectomyDokumen5 halamanViolation of Water-Electric Exchange in Patients With Nospecific Ulcerative Colitis Before Total ColectomyIJRASETPublicationsBelum ada peringkat
- A Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisDokumen5 halamanA Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisBenjamin PaulinBelum ada peringkat
- Cholecystitis Treatment & ManagementDokumen8 halamanCholecystitis Treatment & ManagementTruly Dian AnggrainiBelum ada peringkat
- Apendisitis MRM 3Dokumen8 halamanApendisitis MRM 3siti solikhaBelum ada peringkat
- Could Laparoscopic Colon and Rectal Surgery Become The Standard of Care? A Review and Experience With 750 ProceduresDokumen9 halamanCould Laparoscopic Colon and Rectal Surgery Become The Standard of Care? A Review and Experience With 750 ProcedurespingusBelum ada peringkat
- Laparoscopic Cholecystectomy:An Experience of 200 Cases: Original ArticleDokumen4 halamanLaparoscopic Cholecystectomy:An Experience of 200 Cases: Original ArticleAndrei GheorghitaBelum ada peringkat
- Management of Pyogenic Liver Abscesses - Percutaneous or Open Drainage?Dokumen8 halamanManagement of Pyogenic Liver Abscesses - Percutaneous or Open Drainage?Muhammad FadillahBelum ada peringkat
- Evaluation of Early Cholecystectomy For Acute Cholecystitis Within 10 Days of 7780Dokumen5 halamanEvaluation of Early Cholecystectomy For Acute Cholecystitis Within 10 Days of 7780Jemimah BureresBelum ada peringkat
- Open CholecystectomyDokumen35 halamanOpen CholecystectomywqBelum ada peringkat
- 10.1007@s11605 018 04090 ZDokumen11 halaman10.1007@s11605 018 04090 ZGabriel RangelBelum ada peringkat
- Role of Laparoscopic Cholecystectomy in The Early Management of Acute Gallbladder DiseaseDokumen6 halamanRole of Laparoscopic Cholecystectomy in The Early Management of Acute Gallbladder DiseaseHoracio ChaconBelum ada peringkat
- Laparoscopic Versus Open Cystogastrostomy For Pancreatic Pseudocysts A Comparative StudyDokumen4 halamanLaparoscopic Versus Open Cystogastrostomy For Pancreatic Pseudocysts A Comparative StudyInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Analysis of Risk Factors For Postoperative Morbidity in Perforated Peptic UlcerDokumen10 halamanAnalysis of Risk Factors For Postoperative Morbidity in Perforated Peptic UlcerNurul Fitrawati RidwanBelum ada peringkat
- Impact of Postoperative Morbidity On Long-Term Survival After OesophagectomyDokumen10 halamanImpact of Postoperative Morbidity On Long-Term Survival After OesophagectomyPutri PadmosuwarnoBelum ada peringkat
- Post-Cholecystectomy Acute Injury: What Can Go Wrong?Dokumen7 halamanPost-Cholecystectomy Acute Injury: What Can Go Wrong?Ramyasree BadeBelum ada peringkat
- Repair of Common Bile Duct InjuriesDokumen12 halamanRepair of Common Bile Duct InjuriesDragoș PopaBelum ada peringkat
- The Liver Graft Before Transplantation: Defining Outcome After Liver TransplantationDari EverandThe Liver Graft Before Transplantation: Defining Outcome After Liver TransplantationXavier VerhelstBelum ada peringkat
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in AdultsDokumen17 halamanDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adultsjoseaugustorojas9414Belum ada peringkat
- Surgical Approaches To Groin Hernia RepairDokumen1 halamanSurgical Approaches To Groin Hernia Repairjoseaugustorojas9414Belum ada peringkat
- Fracturas TraumaDokumen8 halamanFracturas Traumajoseaugustorojas9414Belum ada peringkat
- REBOA in Hemorrhagic Shock: A Unique Non-Responder?Dokumen3 halamanREBOA in Hemorrhagic Shock: A Unique Non-Responder?joseaugustorojas9414Belum ada peringkat
- Sleisenger and Fordtrans Gastrointestinal and Liver Disease Review and AssessmentDokumen325 halamanSleisenger and Fordtrans Gastrointestinal and Liver Disease Review and AssessmentJimmy Alberto González Castillo100% (2)
- Silverbook2011 PDFDokumen57 halamanSilverbook2011 PDFjoseaugustorojas9414Belum ada peringkat
- Acute Oncology Handbook R8 PDFDokumen46 halamanAcute Oncology Handbook R8 PDFjoseaugustorojas9414Belum ada peringkat
- Introduction To Acute OncologyDokumen34 halamanIntroduction To Acute Oncologyjoseaugustorojas9414Belum ada peringkat
- Surgery Critical View - StrasbergDokumen7 halamanSurgery Critical View - Strasbergjoseaugustorojas9414Belum ada peringkat
- Acute Oncology Clinical Guidelines September 2013Dokumen59 halamanAcute Oncology Clinical Guidelines September 2013joseaugustorojas9414Belum ada peringkat
- Esofago SurgeryDokumen19 halamanEsofago Surgeryjoseaugustorojas9414Belum ada peringkat
- Attia General Surgery Review ManualDokumen158 halamanAttia General Surgery Review Manualbphage100% (2)
- Group 5 Transforming Banana Stem Waste To Eco Tote Bag.Dokumen4 halamanGroup 5 Transforming Banana Stem Waste To Eco Tote Bag.Gabriel Abram JopiaBelum ada peringkat
- Repair of Small Household Appliances and Power ToolsDokumen315 halamanRepair of Small Household Appliances and Power ToolsahmadnawazjaswalBelum ada peringkat
- CHAPTER 2 Principles of MarketingDokumen41 halamanCHAPTER 2 Principles of MarketingASHIMA THAPABelum ada peringkat
- US Navy Course NAVEDTRA 14342 - Air Traffic ControllerDokumen594 halamanUS Navy Course NAVEDTRA 14342 - Air Traffic ControllerGeorges100% (4)
- A Thermoelectric Scanning Facility For The Study of Elemental Thermocouples Robin E Bentley - Meas. Sci. Technol. 11 (2000) 538-546Dokumen10 halamanA Thermoelectric Scanning Facility For The Study of Elemental Thermocouples Robin E Bentley - Meas. Sci. Technol. 11 (2000) 538-546Ver OnischBelum ada peringkat
- BBBB - View ReservationDokumen2 halamanBBBB - View ReservationBashir Ahmad BashirBelum ada peringkat
- Industrial Training HandbookDokumen26 halamanIndustrial Training HandbookChung tong Betty wongBelum ada peringkat
- Box MCB Hager BrochureDokumen5 halamanBox MCB Hager BrochureTOLLAUT DESIGNBelum ada peringkat
- Guidelines in Research Proposal WritingDokumen19 halamanGuidelines in Research Proposal WritingMark RelloresBelum ada peringkat
- Assignment 2Dokumen4 halamanAssignment 2LaDonna WhiteBelum ada peringkat
- Needs Assessment Form Company Name: HRMO Address: Sta. Barbara Agoo, La UnionDokumen2 halamanNeeds Assessment Form Company Name: HRMO Address: Sta. Barbara Agoo, La UnionAlvin LaroyaBelum ada peringkat
- How To Post Bail For Your Temporary Liberty?Dokumen5 halamanHow To Post Bail For Your Temporary Liberty?Ruel Benjamin Bernaldez100% (1)
- Web Development Company in BhubaneswarDokumen4 halamanWeb Development Company in BhubaneswarsatyajitBelum ada peringkat
- The Properties of Chopped Basalt Fibre Reinforced Self-CompactingDokumen8 halamanThe Properties of Chopped Basalt Fibre Reinforced Self-CompactingEjaz RahimiBelum ada peringkat
- Calculation of Work IndexDokumen5 halamanCalculation of Work IndexEnryan Oreski RiyadiBelum ada peringkat
- Scope and Sequence Plan Stage4 Year7 Visual ArtsDokumen5 halamanScope and Sequence Plan Stage4 Year7 Visual Artsapi-254422131Belum ada peringkat
- Sample Resume FinalDokumen2 halamanSample Resume FinalSyed Asad HussainBelum ada peringkat
- Merenstein Gardners Handbook of Neonatal Intensive Care 8Th Edition Sandra Lee Gardner Brian S Carter Mary I Enzman Hines Jacinto A Hernandez Download PDF ChapterDokumen52 halamanMerenstein Gardners Handbook of Neonatal Intensive Care 8Th Edition Sandra Lee Gardner Brian S Carter Mary I Enzman Hines Jacinto A Hernandez Download PDF Chapterrichard.martin380100% (16)
- Case 2:09-cv-02445-WBS-AC Document 625-1 Filed 01/21/15 Page 1 of 144Dokumen144 halamanCase 2:09-cv-02445-WBS-AC Document 625-1 Filed 01/21/15 Page 1 of 144California Judicial Branch News Service - Investigative Reporting Source Material & Story Ideas100% (2)
- LC1D40008B7: Product Data SheetDokumen4 halamanLC1D40008B7: Product Data SheetLê Duy MinhBelum ada peringkat
- Surface Treatments & Coatings Ref: S. KalpakjianDokumen22 halamanSurface Treatments & Coatings Ref: S. KalpakjianjojoBelum ada peringkat
- Azhar Marketing Final PPRDokumen9 halamanAzhar Marketing Final PPRafnain rafiBelum ada peringkat
- 147380-1 Motoman XRC Controller Fieldbus (XFB01) Instruction ManualDokumen102 halaman147380-1 Motoman XRC Controller Fieldbus (XFB01) Instruction Manualrubi monBelum ada peringkat
- Urban Jungle 8Dokumen3 halamanUrban Jungle 8Angel Medez GonzalezBelum ada peringkat
- Business PlanDokumen20 halamanBusiness PlanRona BautistaBelum ada peringkat
- Đo Nhiệt Độ LI-24ALW-SelectDokumen4 halamanĐo Nhiệt Độ LI-24ALW-SelectThang NguyenBelum ada peringkat
- Labour and Human Resource Issues in Industry 4.0: A Case Study Report OnDokumen20 halamanLabour and Human Resource Issues in Industry 4.0: A Case Study Report OnNPMYS23100% (1)
- Dorp Handbook and Plan EBCESDokumen30 halamanDorp Handbook and Plan EBCESJenelou delapenaBelum ada peringkat
- 3-Module 3-23-Feb-2021Material I 23-Feb-2021 Error Detection and CorrectionDokumen39 halaman3-Module 3-23-Feb-2021Material I 23-Feb-2021 Error Detection and CorrectionPIYUSH RAJ GUPTA 19BCE2087Belum ada peringkat