Appendikstomi Vs Antibiotik PDF
Diunggah oleh
dimasJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Appendikstomi Vs Antibiotik PDF
Diunggah oleh
dimasHak Cipta:
Format Tersedia
2006 by the Societe Internationale de Chirurgie
Published Online: 27 April 2006
World J Surg (2006) 30: 10331037
DOI: 10.1007/s00268-005-0304-6
Appendectomy versus Antibiotic Treatment in
Acute Appendicitis. A Prospective Multicenter
Randomized Controlled Trial
Johan Styrud MD, PhD,1 Staffan Eriksson MD, PhD,1* Ingemar Nilsson MD, PhD,2
Gunnar Ahlberg MD, PhD,2 Staffan Haapaniemi MD, PhD,3 Gunnar Neovius MD,4
Lars Rex MD,5 Ibrahim Badume MD,6 Lars Granstrom MD, PhD1
1
Department
Department
3
Department
4
Department
5
Department
6
Department
2
of
of
of
of
of
of
Surgery,
Surgery,
Surgery,
Surgery,
Surgery,
Surgery,
Karolinska Institutet at Danderyd Hospital, S-182 88 Stockholm, Sweden
St Goran Hospital, Karolinska Institutet, S-171 77 Stockholm, Sweden
Norrkoping Hospital, S-60182 Norrkoping, Sweden
Kristianstad Central Hospital, S-29185 Kristianstad, Sweden
Boras Hospital, S-50182 Boras, Sweden
Katrineholm Hospital, S-64122 Katrineholm, Sweden
Abstract
Background: Appendectomy has been the treatment for acute appendicitis for over 120 years.
Antibiotic treatment has occasionally been used in small uncontrolled studies, instead of operation, but this alternative has never before been tried in a multicenter randomized trial.
Patients and Methods: Male patients, 1850 years of age, admitted to six different hospitals in
Sweden between 1996 and 1999 were enrolled in the study. No women were enrolled by decision
of the local ethics committee. If appendectomy was planned, patients were asked to participate,
and those who agreed were randomized either to surgery or to antibiotic therapy. Patients randomized to surgery were operated on with open surgery or laparoscopically. Those randomized to
antibiotic therapy were treated intravenously for 2 days, followed by oral treatment for 10 days. If
symptoms did not resolve within 24 hours, an appendectomy was performed. Participants were
monitored at the end of 1 week, 6 weeks, and 1 year.
Results: During the study period 252 men participated, 124 in the surgery group and 128 in the
antibiotic group. The frequency of appendicitis was 97% in the surgery group and 5% had a
perforated appendix. The complication rate was 14% in the surgery group. In the antibiotic group
86% improved without surgery; 18 patients were operated on within 24 hours, and the diagnosis of
acute appendicitis was confirmed in all but one patient, and he was suffering from terminal ileitis.
There were seven patients (5%) with a perforated appendix in this group. The rate of recurrence of
symptoms of appendicitis among the 111 patients treated with antibiotics was 14% during the 1year follow-up.
Conclusions: Acute nonperforated appendicitis can be treated successfully with antibiotics.
However, there is a risk of recurrence in cases of acute appendicitis, and this risk should be
compared with the risk of complications after appendectomy.
*Present address: Department of Surgery, Vasteras Hospital, S-721
89 Vasteras, Sweden
Correspondence to: Johan Styrud, MD, PhD, Department of Surgery,
Karolinska Institutet at Danderyd Hospital, S-182 88 Stockholm, Sweden, e-mail: johan.styrud@ds.se
1034
Styrud et al.: Appendctomy versus Antibiotic Treatment
ore than 120 years have passed since A. Grooves
performed the first appendectomy in 1883.1 Early
appendectomy has been advocated, especially
since R. Fitz in 1886 published a classic paper on 247
patients with perforated appendicitis.2
There have been occasional reports of conservative
treatment with antibiotics in acute appendicitis. In 1959,
Coldrey reported 471 patients who underwent treatment
with antibiotics alone,3 and a report from China in 1977
described 425 patients who were treated without surgery,
but with antibiotics or traditional Chinese medicine.4 At
follow-up 7% had recurrence. Antibiotic treatment has
also been described in nine U.S, submariners.5
In patients with an appendiceal mass the recommended treatment today is conservatively with antibiotics, and interval appendectomy is under debate.6,7
We have previously shown in a pilot study of 40 patients, that 19/20 (95%) were successfully treated with
antibiotics.8 Treatment with antibiotics resulted in
significantly less pain compared to open appendectomy.
However, with a recurrence rate of 7/19 (37%), it was
suggested that the treatment should be used when surgery
presented a high risk of complications. The pilot study led to
a larger study to determine whether antibiotic treatment in
acute non-perforated appendicitis could be recommended.
The aim of the present study was to compare antibiotic treatment with surgery in acute appendicitis in a
large series of patients.
PATIENTS AND METHODS
Participants
Six hospitals in Sweden took part in the randomized
study. They were Danderyd Hospital, St Go ran Hospital,
Norrko ping Hospital, Kristianstad Hospital, Bora s Hospital, and Katrineholm Hospital.
A series of 252 men 1850 years of age were randomized to the study between March 1996 and June
1999. No women were enrolled in this multicenter study
by decision of the local ethics committee. All patient data
are presented in Table 1. Excluded were patients with
suspicion of perforation of the appendix, those unwilling
to participate, patients with a C-reactive protein (CRP)
level <10 mg/l, and any who had had an allergic reaction
to the antibiotics to be used in the treatment protocol.
Study Design
All patients admitted for suspected acute appendicitis
with a CRP level >10 mg/l in whom perforation was not
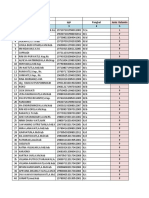
Table 1.
Patient data in the different groups
No of patients
C-reactive protein
Total white cell count
Body temperature
Antibiotics
Surgery
128
55 + 44
12.5 + 3.8
37.5 + 0.7
124
54 + 49
12.4 + 3.5
37.4 + 0.8
Note: Values are mean + S.D.
suspected were asked to participate in the study.811 Each
patient was randomized to surgery or antibiotic therapy at
the time the decision was taken that surgery was needed.
Randomization of each participant was performed by a
telephone call to Danderyd Hospital where a sealed
envelope was opened and revealed the assignment of
surgery or antibiotic therapy. Patients randomized to
surgery were operated open or laparoscopically, at the
surgeons discretion. All removed appendices were sent
for histopathological examination. Patients who underwent appendectomy were discharged when their condition
was deemed satisfactory. The level of pain and sickness
as well as the time off work were recorded.
Patients who received antibiotic treatment were given
the same antibiotics used in the earlier pilot study, but
oral treatment was given for 10 days.8 Treatment was
begun with 2 days of i.v. cefotaxime (Claforan; Aventis
Pharma, Stockholm, Sweden), 2 g 12 hourly, and tinidazole (Fasigyn; Pfizer, Ta by, Sweden), 0.8 g daily. Patients received intravenous fluids during the first 24 hours
and were allowed to eat during the second hospital day. If
their symptoms did not improve within the first 24 hours,
an appendectomy was performed. Participants who received antibiotics alone, were discharged after the 2 days
of i.v therapy and received oral treatment with ofloxacin
(Tarivid; Aventis Pharma, Stockholm; Sweden), 200 mg
twice daily, and tinidazole (Fasigyn; Pfizer, Ta by, Sweden), 500 mg twice daily for 10 days.
Participants were evaluated at follow-up after 1 week, 6
weeks, and 1 year. The number of days of sick leave from
work, the level of pain, and the complications, if any, were
recorded. All conservatively treated patients with a suspected recurrence of appendicitis underwent surgery.
Statistical Methods and Data Management
To evaluate hypotheses of variables in contingency
tables, the chi-square test was used or, in the case of
small expected frequencies, Fishers exact test was
performed. Statistical comparisons to test differences
between the two groups were made with Students t-test
for uncorrelated means. The within-group analysis was
Styrud et al.: Appendctomy versus Antibiotic Treatment
Table 2.
Hospital stay, sick leave, and time off work in the different
groups treated for acute appendicitis
Hospital stay (days)
Sick leave (days)
Time off work (days)
Antibiotics
Surgery
3.0 + 1.4
5.3 + 4.1
8.0 + 8.0
2.6 + 1.2
6.0 + 4.4
10.1 + 7.6
Values are mean + S.D.
made by use of the pairwise Students t-test for correlated
means. In addition, descriptive statistics and graphical
methods were used to characterize the data. All analyses
were carried out by use of the SAS system, version 8.08
(SAS Institute, Cary; NC, USA), and the 5% level of significance was considered. In the case of a statistically
significant result the probability value (P value) has been
given.
The trial was approved by the local ethical committees,
as well as the Swedish Federal Drug Administration
(lakemedelsverket). All participants were informed orally
and by written information.
RESULTS
Acute appendicitis was found in 97% of the 124 patients
randomized to surgery. Eight patients (6%) underwent
laparoscopic procedures. At operation and normal histopathological examination of the appendix, three patients
had mesenteric adenitis and one patient had no evidence
of pathology. All appendices were sent for histopathological examination, except in one patient with gangrenous appendicitis. Six (5%) patients had perforated
appendices. The complication rate among this surgery
group was 14% (17/124), mainly wound infections. The
time in hospital, sick leave taken and time lost from work
are shown in Table 2.
Of the 128 patients enrolled in the antibiotic group, 15
patients (12%) were operated within the first 24 hours due
to lack of improvement in symptoms and apparent local
peritonitis. The operation showed that seven patients
(5%) had perforation. One patient did not have acute
appendicitis; instead terminal ileitis was found. A total of
113 patients were successfully treated with antibiotics
and were sent home for oral antibiotic therapy for 10
days. The length of the hospital stay and duration of sick
leave were comparable to the surgery group (Table 2).
To learn whether the patients enrolled in this multicenter study differ from those who were unwilling to
participate, we examined the medical records of all men
in the 1850-year age range that underwent appendec-
1035
Table 3.
The histopathological diagnosis in 79 men unwilling to be enrolled in the study compared with 25 men that enrolled and were
included in the surgery group ad Danderyd Hospital 19961997
Percentage (n)
Diagnosis
Appendicitis
Phlegmonous
Gangrenous
Perforated
Normal
Other diagnosis
Unwilling
51
39
1
4
4
(40)
(31)
(1)
(3)
(3)
Surgery enrolled
48
36
12
4
0
(12)
(9)
(3)
(1)
tomy at Danderyd Hospital between 1996 and 1997. A
total of 196 men were operated on, and 67 were excluded
from the study for the following reasons: suspicion
of perforation (41 patients, 61%), CRP <10 mg/l
(25 patients, 37%), and allergy to the antibiotics selected
for the study (1 patient, 2%). Another 79 patients were
unwilling to participate or were not informed about the
study. Of the 50 patients that were enrolled, 25 were
randomized to surgery. There were no significant differences in histopathological findings between those who
participated and those who did not (Table 3).
During the 1-year follow-up period there were 17 (14%)
complications in the surgery group, most of them wound
infections. Four patients had complications after surgery
in the antibiotic-treated group. The recurrence rate within
1 year was 15% (16 patients) in the group treated with
antibiotics. After an average time of 4 months, those
patients underwent operation according to the study
protocol (range: 110 months after antibiotic treatment).
In five of these patients a perforated appendix was found
at operation.
DISCUSSION
The diagnosis of acute appendicitis is often difficult to
make. We have previously shown that with an increasing
interest in acute appendicitis, and by measuring CRP
repeatedly, we have been able to increase diagnostic
accuracy in patients with acute appendicitis.12 A high
diagnostic accuracy was important when patients were
enrolled in our study, because a high probability of acute
appendicitis was mandatory. In the group treated with
antibiotics it can be presumed that 97% had appendicitis.
It is obvious from Table 3 that patients enrolled in the
study didnt differ significantly from the total group of
patients at one of the participating hospitals (Danderyd
Hospital) during the study period.
1036
Although our intention was to exclude patients with
perforations, 5% of the patients in our series had a perforated appendix, fewer than in most studies of patients
with appendicitis.1214 The seven patients with perforated
appendix in the antibiotic group did not have a longer
hospital stay than the six patients with perforation in the
operated group. Nor did their period of sick leave or time
lost from work vary. According to the protocol, patients
with a high suspicion of perforation were operated on
immediately. A perforation rate of 15%25% is often seen
in large groups of patients with acute appendicitis.12,15
This indicates that most patients with suspected acute
appendicitis presenting at the emergency department do
not need an emergency operation. Instead, they can be
treated with antibiotics, and if symptoms progress within
the first 24 hours, they can undergo appendectomy.
Women were excluded from our study by a decision of
the ethics committee, but it is reasonable to believe that
the results we found in men would be relevant for women.
This study shows that antibiotic treatment alone is
sufficient in most patients with acute appendicitis; only 17
patients (12%) from the antiobiotic treatment group went
on to operation within 24 hours. The recurrence rate of
symptoms within 1 year was 15% (16 patients), and many
of those patients ask to be treated conservatively a second time! The incidence of perforation was not higher
among patients with recurrence, and it may be that antibiotic treatment could have been used a second time. If a
fecal stone is lodged in the appendix, there might be a
higher incidence of recurrence.16
There are several different types of antibiotics, and
combinations of antibiotics, that can be used in the
treatment of appendicitis. We used the same combination
we had used in a pilot study with good results.8
There are some potential advantages of antibiotic
treatment versus surgery, one of which is medical cost.
The length of hospital stay could also be shorter with
antibiotic treatment, because parenteral administration of
antibiotics is probably necessary for only 24 hours. Such
patients can be discharged with oral antibiotics for 10 days
and follow-up examination scheduled after the first week.
Another advantage is that risks associated with surgery
and anesthesia are eliminated in patients with acute
appendicitis who receive conservative antibiotic treatment.
Although operative risk is small, complications do exist.
There is also a small morbidity risk at appendectomy, and
that risk is of course increases with age and concomitant
diseases. The rate of intestinal obstruction is known to be
highest after appendectomy of a healthy appendix,17 but
any abdominal operation can result in adhesions, which
may cause intestinal obstruction later in life.
Styrud et al.: Appendctomy versus Antibiotic Treatment
A potential disadvantage of antibiotic treatment is allergy to the drugs employed. As mentioned above, several different types, and combinations, of antibiotics could
be used. Allergy would not be a problem if the surgeon is
aware of the possibility of allergy and prescribes antibiotics suitable for each patient.
Acute appendicitis is a common disease,14 and if antibiotic treatment proves successful in treating the majority
of patients, there will be a large increase in antibiotic use in
the population. That will enhance the risk that patients will
develop susceptibility to bacteria strains that are resistant
to an increasing number of antibiotics, especially if the
criteria for treatment are not correct. Because there is already a large problem with multiresistant bacteria, this is a
major disadvantage of routine antibiotic treatment of acute
appendicitis. Therefore it might not be logical to recommend antibiotic treatment to such a large group of patients.
It is crucial to use antibiotic treatment with the same
high diagnostic accuracy required before considering
surgery; i.e., no patients should be treated with antibiotics
without history and clinical signs indicating appendicitis.
The diagnosis should be confirmed with CT scan and/or
ultrasonography, and no patient without an elevated CRP
level should be treated for suspected appendicitis.13,18
Antibiotic treatment can be recommended in patients
with a high surgical risk, i.e., elderly patients with poor
heart and lung function, and severely obese patients.
In conclusion, this study shows that acute appendicitis
can be treated successfully with antibiotics with a short
hospital stay, minimal sick leave, and limited duration of
pain. There is a risk of recurrence, which should be compared with the rate of complications after appendectomy.
ACKNOWLEDGMENTS
This work was supported by research funds of the
Swedish Society of Medicine, Karolinska Institutet; the
Wallenius Corporation; Aventis Pharma (former Hoecht
Marion Roussel). We are indebted to G. Orrebrink and
O. Sta hlebrandt for their contributions to this study.
REFERENCES
1. Harris CW. The first elective appendectomy? Can J Surg
1961;4:405410.
2. Fitz RH. Perforating inflammation of the vermiform appendix. Am J Med Sci 1886;92:321346.
3. Coldrey E. Five years of conservative treatment of acute
appendicitis. J Int Coll Surg 1959;32:255261.
Styrud et al.: Appendctomy versus Antibiotic Treatment
4. Anonymous. Combined traditional Chinese and Western
medicine for acute appendicitis. Chinese Med J 1977;3:
266269.
5. Adams ML. The medical management of acute appendicitis
in a nonsurgical environment: a retrospective case review.
Milit Med 1990;155:345347.
6. Nitecki S, Assalia A, Schein M. Contemporary management
of appendeceal mass. Br J Surg 1993;80:820.
7. Eriksson S, Styrud J. Interval appendicectomy: a retrospective study. Eur J Surg 1998;164:771774.
8. Eriksson S, Granstro m L. Randomized controlled trial of
appendicectomy versus antibiotic treatment therapy for
acute appendicitis. Br J Surg 1995;82:166169.
9. Eriksson S, Granstro m L, Bark S. Laboratory tests in patients with suspected acute appendicitis. Acta Chir Scand
1989;155:117120.
10. Eriksson S, Granstro m L, Carlstro m A. The diagnostic value
of repetitive preoperative analysis of C-reactive protein and
total leukocyte count in patients with suspected acute
appendicitis. Scand J Gastroenterol 1994;29:11451149.
sberg A. The accuracy of C-reactive protein in
11. Hallan S, A
the diagnosing acute appendicitisa meta analysis. Scand
J Clin Lab Invest 1997;57:373380.
1037
12. Styrud J, Eriksson S, Segelman J, et al. Diagnostic accuracy in 2351 patients undergoing appendicectomy for suspected acute appendicitis. Dig Surg 1999;16:3944.
13. Styrud J, Josephson T, Eriksson S. Reducing negative
appendectomy evaluation of ultrasonography and computer
tomography in acute appendicitis. Int J Qual Health Care
2000;12:6568.
14. Andersson RE, Hugander A, Thulin AJG. Diagnostic accuracy and perforation rate in appendicitis: association with
age and sex of the patient and with appendectomy rate. Eur
J Surg 1992;158:3741.
15. Andersson R, Hugander A, Thulin A, et al. Indications for
operation in suspected appendicitis and incidence of perforation. Br Med J 1994;308:107110.
, Granstro m L. Ultrasonographic
16. Eriksson S, Tisell A
findings after conservative treatment of acute appendicitis and open appendicectomy. Acta Radiol 1995;36:173
177.
17. Arnbjo rnsson E. Small intestinal obstruction after appendectomy: an avoidable complication. 1984;41:354357.
18. Andersson R, Hugander A, Ghazi S, et al. Why does the
clinical diagnosis fail in suspected appendicitis. Eur J Surg
2000;166:796802.
Anda mungkin juga menyukai
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Print - 1 - Foundations of High-Performing Healthcare Organizations PDFDokumen5 halamanPrint - 1 - Foundations of High-Performing Healthcare Organizations PDFIntan Dwi LestariBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Oxford: ReferenceDokumen846 halamanOxford: ReferenceNMC NEPHROLOGY100% (1)
- 3 Analytic StudyDokumen49 halaman3 Analytic Studyyoyo90% (10)
- List of Hospitals in UAEDokumen7 halamanList of Hospitals in UAEaneebqualitasBelum ada peringkat
- The Theory of Preventive Stress ManagementDokumen13 halamanThe Theory of Preventive Stress ManagementOsama JamranBelum ada peringkat
- 1 - Top Cyber Security Risks in HealthcareDokumen5 halaman1 - Top Cyber Security Risks in HealthcarevelangniBelum ada peringkat
- BibliotherapyDokumen4 halamanBibliotherapyMonirul Islam100% (2)
- Atlas of Head & Neck Surgery-Vol 2 Lore & Medina PDFDokumen848 halamanAtlas of Head & Neck Surgery-Vol 2 Lore & Medina PDFroata cristian100% (3)
- CLSI M39-A5E AntibiogramsDokumen192 halamanCLSI M39-A5E AntibiogramsdianBelum ada peringkat
- Docs in PuneDokumen238 halamanDocs in Punemenolove100% (1)
- PART 1 Coran Pediatric Surgery, 7th Ed PDFDokumen402 halamanPART 1 Coran Pediatric Surgery, 7th Ed PDFCarmen Chivu100% (17)
- Fractured Wrist: Information For PatientsDokumen4 halamanFractured Wrist: Information For Patientsviv stewBelum ada peringkat
- Corrected Index: FIVE DAYS AT MEMORIAL First EditionDokumen11 halamanCorrected Index: FIVE DAYS AT MEMORIAL First EditionSheri Fink0% (1)
- NICE DRAFT - Drug Allergy Diagnosis and Management of Drug Allergy in Adults, Children and Young PeopleDokumen29 halamanNICE DRAFT - Drug Allergy Diagnosis and Management of Drug Allergy in Adults, Children and Young Peopletian download doangBelum ada peringkat
- Form Pip - Dinkes (3) Puskesmas Purwodadi IIDokumen9 halamanForm Pip - Dinkes (3) Puskesmas Purwodadi IIUptd Puskesmas Purwodadi IIBelum ada peringkat
- Removable Orthodontic Appliances and Patient Percieved ProblemsDokumen5 halamanRemovable Orthodontic Appliances and Patient Percieved ProblemsRati Ramayani AbidinBelum ada peringkat
- Case Study - ExDokumen5 halamanCase Study - ExSarah W.Belum ada peringkat
- Ob GynotDokumen4 halamanOb Gynotapi-463220004Belum ada peringkat
- Assignment in EFTP-Reading and Note-TakingDokumen1 halamanAssignment in EFTP-Reading and Note-TakingMarc FresBelum ada peringkat
- Cci 2022 Eng FinalDokumen2.761 halamanCci 2022 Eng FinalNguyễn Xuân LộcBelum ada peringkat
- Project Seminar Hospice FedoraDokumen3 halamanProject Seminar Hospice FedoralalithaBelum ada peringkat
- DR Geeta Pangi HypertensionDokumen6 halamanDR Geeta Pangi HypertensionSheera EiyraaBelum ada peringkat
- Napro Pamphlet Shelly KellyDokumen2 halamanNapro Pamphlet Shelly Kellyapi-290098737Belum ada peringkat
- Healy World Flyer Wellbeing en USDokumen1 halamanHealy World Flyer Wellbeing en USAllan Emmanuel Lopez MarquezBelum ada peringkat
- BCBS LA 2020IndividualSolutions PDFDokumen28 halamanBCBS LA 2020IndividualSolutions PDFger80Belum ada peringkat
- On My Honor, I Have Neither Given Nor Received Aid On This Assignment or Test, and I Pledge That I Am in Compliance With The BSMCON Honor System.Dokumen6 halamanOn My Honor, I Have Neither Given Nor Received Aid On This Assignment or Test, and I Pledge That I Am in Compliance With The BSMCON Honor System.api-273018832Belum ada peringkat
- Health PresentationDokumen16 halamanHealth PresentationSCS-Abarquez, Christel Jade D.Belum ada peringkat
- Journal of Applied Health Management and TechnologyDokumen12 halamanJournal of Applied Health Management and Technologysalsabil vaniBelum ada peringkat
- r1 InstwiseadmDokumen187 halamanr1 InstwiseadmMadhavBelum ada peringkat
- List of Specialist Accredited Hospitals (Metro Manila)Dokumen20 halamanList of Specialist Accredited Hospitals (Metro Manila)Jimbo OctagonBelum ada peringkat