ARV Adverse
Diunggah oleh
natinlalaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
ARV Adverse
Diunggah oleh
natinlalaHak Cipta:
Format Tersedia
CLINICAL PRACTICE
Behavioral Aspects of HIV Prevention and Care in Indonesia:
A Plea for a Multi-disciplinary, Theory- and Evidencebased Approach
Elmira N Sumintardja*, Lucas WJ Pinxten**, Juke R.L. Siregar*, Harry Suherman***,
Rudy Wisaksana****, Shelly Iskandar*****, Irma A Tasya***, Zahrotur Hinduan*,
Harm J. Hospers**
* Faculty of Psychology, Padjadjaran University. Jl. Pasirkaliki no. 190, Bandung 40151, Indonesia.
** Department of Work and Social Psychology, Faculty of Psychology and Neuroscience, Maastricht University,
Maastricht, The Netherlands. *** Health Research Unit, Faculty of Medicine, Padjadjaran University/Hasan Sadikin
Hospital, Bandung, Indonesia. **** Department of Internal Medicine, Faculty of Medicine, Padjadjaran University/
Hasan Sadikin Hospital, Bandung, Indonesia. ***** Department of Psychiatry, Faculty of Medicine,
Padjajaran University/Hasan Sadikin Hospital, Bandung, Indonesia.
Correspondence mail to: lpinxten@yahoo.com.
ABSTRACT
Projections estimate 1,000,000 HIV infected by 2015 in
Indonesia. Key behaviors to HIV prevention and care are
determined by a complex set of individual/ environmental
factors. This paper presents empirical data, local evidence
and theoretical concepts to determine the role of social
sciences in HIV prevention/care.
Injecting Drug Use (IDU) is a social and very risky
activity: 95% injected in the presence of peers and 49%
reported needles sharing. 82% of IDUs do not use condoms
consistently. Poor adherence to ARV treatment is related to
a complex set of, mostly behavioral, factors beyond effective
influence by standard professional skills of medical staff.
Meta-analysis indicated that about 1/3 of the variance
in behaviour can be explained by the combined effect of
intention and perceived behavioral control, the two
cornerstones of the Theory of Planned Behavior (TPB). It is
advisable to adapt TPB in the light of the Indonesian
context.
Current theories of behavior and behavior change give
professionals of all disciplines, working in HIV prevention
and care, effective tools to change behavior and to improve
HIV prevention and access & quality of HIV care.
Key words: VCT, ARV adherence, injecting drug use, AIDS/
HIV, theory of planned behavior, intervention mapping.
INTRODUCTION
According to UNAIDS and WHO estimates, in Asia
around 5 million people are living with HIV (range: 3.7
million6.7 million). Some Asian countries (Thailand and
Cambodia) managed to halt the HIV epidemic resulting
in an overall declining trend of new infections: from
450,000 in 2001 to 440,000 in 2007.1 Injecting drug use
(IDU) has been identified as a major cause of the
current expansion of the HIV epidemic in Asia.2,3
During the first two decades of the HIV pandemic,
Indonesia was relatively unaffected by the virus.4,5 It
was not until 1999 when a sharp rise in HIV infection in
several subpopulations was recorded. The groups most
affected were intravenous drug users (IDUs) and Sex
Workers (SW) and their clients. An anonymous sentinel
surveillance in Indonesia revealed that in 1999 16% of
IDUs were HIV-infected. This figure rose to 41% in
2000 and to 48% in 2001. In urban areas, HIV-transmission through needle sharing showed an eightfold increase
from 1997 to 2003.6
Current estimates of total HIV infections in
Indonesia range between 190,000 to 400,000 in a nation
of 220 million inhabitants, while prevalence rates of HIV
among different IDU subpopulations in Jakarta range
from 18% to over 90% 7-10 and unsafe injecting
practices are estimated to account for over 75% of all
new HIV infections.9,11 Around the year 2000, approximately one quarter of IDUs in Bandung, Jakarta and
Bali were reported to have engaged in unprotected sex
79
Elmira
with commercially sex workers (SW) in the previous
year.3,10,13 After Jakarta and Papua province (where the
HIV epidemic is primarily heterosexually driven), West
Java is the third worst affected province having an
estimated 22,000 IDUs of which up to 52% are HIVpositive and 21% incarcerated.14,15
Unlike other countries, Indonesia has a quite unique
HIV epidemic: HIV patients mostly (ex-) IDUs and
their spouses are young: 40% of nationally reported
AIDS cases were between 15 and 24 years16 and were
rather well educated: in Jakarta 73% of the IDUs17 had
higher education (high school or beyond) while in
Bandung about 70% had finished senior high school, and
14% of the IDUs had a university degree.18 In the
Bandung RSHS methadone clinic, about 42% of the
patients have a senior high school degree and 31% of
the patients have an academic degree.19
According to the Indonesian National Narcotics
Board, approximately 1% of Indonesias total population
use intravenous drugs, resulting in a concurrent HIV and
IDU epidemic, fuelling through sexual contact between
injectors and non-injectors the Indonesian HIV
epidemic.9,12,20 Unless effective harm reduction targeted
at the most at-risk groups is put in place including clean
needle distribution and adequate condom distribution
scenario studies project at least 1 million HIV infections
by the year 2015.21
On the biomedical front, also in Indonesia, much has
changed in the last decade: multi-drug antiviral (ARV)
regimens have become available, more convenient, less
toxic and, due to generic and off-patent production with
pharmaceutical subsidies and government distribution to
148 designated ARV treatment hospitals, less expensive.
In Bandung, this development is paying off: compared to
the current national mortality figure of 20%22, the
Bandung mortality rate now is 7% one year after
starting ARV.19
Despite this progress, huge challenges still remain in
the field of behavioral aspects of HIV prevention and
care in Indonesia. It is not who a person is but what he
or she does that determines whether one exposes
oneself and/or others to HIV.(after Fishbein, 2000)
Behaviors considered key to HIV prevention and
care are determined by a complex set of individual and
environmental factors. For practical reasons and in
order to gain a better understanding of these individual
and environmental factors, behavioral sciences use
theoretical concepts to model, determine and explain
cognitions, barriers and environmental conditions that
affect behavior of (ex-) IDUs, and other groups at risk,
and their access to and use of services. The
development of HIV prevention and care should be a
80
Acta Med Indones-Indones J Intern Med
well planned evidence and theory-based activity in
order to be effective. 23-25 Especially the use of
behavioral models facilitates all professionals working
in the HIV field to critical analysis of the situation of the
individual, group or the environment in order to develop,
implement and evaluate appropriate and effective
prevention and care interventions.
This paper presents empirical data and theoretical
concepts to determine the role of behavioral sciences in
HIV prevention and care in Indonesia and covers the
following chapters: 1. analysis of the situation/problem;
2. analysis of the behavior at individual and environmental
level (e.g. risky injecting behavior, condom use),
3. analysis of the determinants of the behavior (e.g. group/
peer pressure, self-efficacy), 4. development and pilot
testing of the intervention (e.g. school-based prevention
curriculum, counseling), and 5. implementation of the
intervention (e.g. at schools or at ARV clinics). We will
follow the steps of the Intervention Mapping25 method
to discuss empirical data and theoretical concepts
related to behavioral aspects of HIV prevention and
care, such as: knowledge, attitudes, social norms, risk
perception regarding HIV-related risk behaviors, and
perceived skills related to risk reduction behaviors and
ARV treatment (safer sex; safe injecting, adherence to
ARV treatment).
EVIDENCE ON BEHAVIORAL ASPECTS OF SEXUAL
AND DRUG RELATED RISK BEHAVIORS SUCH AS VCT,
ARV UPTAKE AND ARV ADHERENCE
Next, we will present data of sexual and drugs related risk behaviors among IDUs, leading to health hazards like HIV or HCV infections, as well as local behavioral evidence related to the uptake of VCT, ARV
treatment and adherence.
Sex-related Risk Behavior Among IDU
A 2006 in-depth study of 321 active IDUs in Bandung
revealed that about 15% had a steady partner, that 47%
bought sex in the last year, and that 89% ever had
casual sex partners. Of all respondents, 37% never used
a condom in any sexual contact, 51% did not use a
condom during the last sexual intercourse, 45% reported
to have had unprotected sex with SW the yera before.
Of the 321 surveyed IDUs only 10% of this group had
been tested for HIV.26 According to the 2007 national
bio-behavioral survey, 82% of the Bandung IDUs did
not use condoms consistently and 45% do not use a
condom when having sex with a sex worker.27
Drug-related Risk Behavior Among IDU
The above mentioned 2006 Bandung survey further
showed that the average age of this specific survey
Vol 41 Supplement 1 July 2009
sample was 19 years. The mean age of first illicit drug
use (including alcohol, mushrooms, inhalants, codeine,
ecstasy, marihuana, tranquilizers, cocaine and
amphetamines but excluding tobacco smoking and
injecting drug use) was 16 years and first injection drug
use was at 19 years. Individual risk behavior often is
influenced others: 95% of the IDUs injected in the
presence of peers in 95% of cases and high risk
injecting behavior was common: 49% of IDUs reported
needle sharing in the previous month.18,26,28
Given the high HIV-prevalence and the high
prevalence of risk behaviors among IDU, there is
consensus that this IDU-driven HIV epidemic will
gradually spread to other non-injecting populations, like
partners of IDUs and sex workers.29,30 For example,
we see a steady increase of women in the Bandung
patient group attending the HIV clinic of Rumah Sakit
Hasan Sadikin, most of whom are (ex) spouses of IDU),
who became infected through sexual intercourse.31
Uptake of VCT
Voluntary Counselling and Testing (VCT) is a method
whereby clients or patients with risk behavior (like IDUs
and Sex Workers) are informed about the risks of being
HIV-infected and stimulated to take an HIV test. VCT
is a well proven and cost effective way to increase
knowledge of HIV transmission, to promote behavioral
change, and to stimulate the uptake of health care
services like ARV treatment.32-34 Despite the increase
of VCT testing sites in Indonesia it is estimated that as
many as 70% of the most at risk populations have not
yet found their way to a VCT site.3 Also in Bandung,
VCT is the entry point to HIV services. Ideally VCT
should be accessed before people develop opportunistic
infections or other signs of a diminished immunological
status, but the year before most patients in the Bandung
RSHS decided to go for a VCT test only after being
diagnosed with advanced stage of HIV infection
(median CD4 cell count=193mm2/cell and majority
being advised by health care workers to go for VCT in
the hospital.35
Difficulties with VCT utilization have also been
reported in other countries. Ugandan researchers
evaluating home-based VCT (health workers going door
to door) stated that besides inconvenience of the testing
site, fear of stigmatization and emotional vulnerability and
lack of confidentiality: receiving results in a public
facility (hospital/health centre) were the most common
explanations for the relative popularity of home-based
VCT. 36 Dutch research points out that the main
reason for not taking an HIV test among Men who have
Sex with Men (MSM) was fear of a positive test result
Behavioral Aspects of HIV-prevention and Care in Indonesia
and the perceived psychosocial consequences of this test
result.37 Recent Bandung research points out that IDUs
do not go for VCT because of perceived lack of confidentiality offered at the VCT sites, the costs related to
testing (travel and additional service costs) and perceived
lack of benefits of VCT.38
Access and Adherence to ARV Treatment
As a result, the well education IDUs have a rather
good knowledge on HIV/AIDS.27 But barriers like drug
addiction and/or lack of knowledge about opioid
substitution or ARV treatment probably prevent about
75% of current and former Bandung IDUs having tested
HIV+, to accessed addiction- ARV treatment.39
Access to the Bandung ARV clinic requires, like in
all Indonesian ARV treatment sites, that drug users stop
injecting, abstain from drugs or join a substitution
service. In addition, adherence to ARV treatment is
expected. In the case of ARV for HIV-infection
adherence should be very high (i.e. at least 95% of the
doses taken, and on prescribed times). High adherence
is essential for optimal suppression of the virus load.40,41
Lower adherence is considered as medication failure
which may result in virological failure and ARV drugs
resistance. More recent, research however, indicates that
lower adherence levels (lower than 95%) may achieve
durable viral suppression.42 Poor adherence is common
in short-term treatment regimens like antibiotic courses.43
Reaching and maintaining appropriate adherence levels
to ARV treatment is quite a challenge because ARV
treatment is meant to be life-long. Poor adherence to
ARV treatment is related to a complex set of factors:
regimen related factors like the fit of a complex
regimen to the day to day routines, psychological and
physical adverse/side effects, of the treatment itself44,
socio-economic factors like lack of social support from
family and friends45, patient related factors like: low
self-efficacy and lack of self-control of the requirements
of the ARV treatment, psychological distress,
depression, inadequate confidence in treatment and
providers, knowledge, perceived norms (patients
perception of what others expect him to do) perceived
benefits of treatment related to health outcomes and other
values (being a good parent/partner), forgetfulness,
alcohol and drug use, stigma and fear of discrimination,
poor literacy and cognitive impairment,44,46,47 health
system related factors like lack of clear instruction, inadequate knowledge about relation between adherence
and resistance and poor follow-up and feedback,44 and
condition-related factors like low viral load and
symptoms of HIV like wasting and opportunistic
infections.
81
Elmira
Acta Med Indones-Indones J Intern Med
International research indicates that patients with an
IDU history on ARV treatment, have a lower treatment
adherence level and resulting in poor response rate.48,49
However, ongoing research in Bandung cannot confirm
this: ex-IDU patients on both methadone substitution and
ARV are doing at least as good (in terms of self
reported adherence, and viral/immunological response)
as patients without an IDU history that are on ARV
treatment only.29 It would be worth while relating the
self-reported adherence to a gold standard like electronic
pill registration devices in order to validate the self
reported adherence.
THEORY OF PLANNED BEHAVIOR: A PRACTICAL
MODEL TO ANALYZE COMPLEX BEHAVIOR
There is a general recognition that behavioral
sciences, theory and research can play an important role
in protecting and maintaining public health.51 However,
a recent review indicated that most of the many
behavioral interventions developed in the HIV field,
neither use an evidence-based approach nor draw
explicitly on theories of health behavior. The review
further showed that the Theory of Planned Behavior
(TPB) had its limitations but was one of the most used
and useful theoretical models to determine factors and
mechanisms influencing various HIV related
behaviors.52 A meta-analysis indicated that about 1/3 of
the variance in behaviour can be explained by the
combined effect of intention and perceived behavioral
control, the two cornerstones of the TPB.53
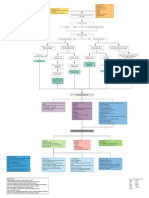
The core of TPB, as illustrated in Figure 1, is the
concept that attitude, subjective (social) norms and
perceived behavioral control (which is similar to
Banduras self-efficacy concept) are the determinants
of motivation, which is usually assessed as the intention
to perform a specific risk or health behavior.54 As an
illustration: the attitude toward learning ones HIV
status is primarily a function of the beliefs about positive
and negative consequences of knowing ones HIV
status. Despite some people knowing about VCT and
the availability of free and easy accessible VCT
centres, they still have certain beliefs (mostly influenced
by others) that influence the balance of perceived
positive and negative consequences of a possible HIV+/
HIV- result of the test. Herewith, the TPB recognizes
that individuals are embedded within interpersonal
relationships, organizations, community and society, and
addresses socio-cultural aspects and incorporates
factors outside the individuals control (like peer
pressure or the opinion of an other important) that may
influence the intention and the actual behavior. As a
result, individuals HIV preventive behaviors, such as
taking up VCT services (in order to know their HIV
status), is a function of individuals cognitions and of the
environment they live in.(24) In Bandung, most people
going for a VCT in RSHS only went for VCT after a
physician or other health care worker told them to check
their status, which suggests negative attitudes towards
testing.35
Subjective or social norms refer to the perceptions
of approval or disapproval of learning of ones HIV
status from significant others (peers, partner, parents).
Ongoing research in Bandung indicates that perceived
lack of confidentiality at the VCT site (individual factor)
and the travel expenses to reach the VCT site
(environmental factor) and perceived fear for
discrimination (individual factor), are the major barriers
to VCT uptake for people at risk. Other Bandung-based
research explains well the distinction between individual
and environmental factor from the research; cost could
Figure 1. Theory of planned behavior (TPB) (Ajzen 1991)
82
Vol 41 Supplement 1 July 2009
be perceived as expensive or cheap to the subjects while
they compare it to the most or less benefit offered by
the services (individual factor) and not by the real
evidence of far or near distance (environmental factor)
they could reach VCT clinic from their residence.38
Self-efficacy/PBC refers to the conviction to be able to
perform the behavior required (coping with bad news or
changing ones life-style or dealing with discrimination)
in learning ones HIV status, whether HIV+ or HIV-.
DEFINING THE BUILDING BLOCKS OF AN EVIDENCE
AND THEORY BASED INTERVENTION: ADHERENCE
TO ARV AS EXAMPLE
Behavioral interventions aiming at changing complex
behavior like sexual risk taking or improving ARV
adherence, are likely to be more effective when based
on evidence of former research and focus on causal
determinants of that specific behavior and when based
on a theoretical concept of behavior and behavior
change. Evidence- and -theory-based interventions also
facilitate evaluation and understanding of the effect of
behavioral interventions, which in their turn feed in the
process of further development of the theoretical
foundations of behavioral interventions. TPB is the most
used and strongest founded theoretical model to predict
a range of behaviors.55,56 Godin and Kok57, reported in
their meta-analysis of 87 TBP studies applied to health
behavior that TPB accounted for 41% of the variance in
behavioral intentions and 34% of the variance in
behavior for a broad range of behaviors. However, TPB
mostly is used as background to understand and explain
the behavior and what to change within the behavior.
However, other theories are mostly used to explain the
Behavioral Aspects of HIV-prevention and Care in Indonesia
behavior change and how to design behavioral
intervention.58
Adherence to ARV, often, (also in Bandung)
measured through self-report is, when linked to more
objective measures like viral load, sub-optimal in about
half of the patients.50,59,60 Very few rigorous evaluations
of interventions to improve ARV adherence are
available.52,61 From a recent Cochrane review we learn
that interventions aiming at improving and strengthening
medication management skills tend to be the most
effective approach to adherence improvement.62 As
discussed before, adherence is embedded, supported,
facilitated and often frustrated by complex behaviors.63
In defining the determinants of this adherence behavior
TPB can, despite its limitations, be very helpful.52 In
order to develop an intervention to improve adherence
to ARV, De Bruin & Hospers et al adapted the TPB
model into concise behavioral components for a
medication adherence model.63
Based on TPB, De Bruin & Hospers propose the
intention of the patient to adhere as the key
determinant. As illustrated in the above model: intention
is determined by 3 factors: subjective norm: what do
specific others like the nurse, physician or partner
expect the patient to do, attitude: the patients belief, in
terms of perceived costs and benefits outcome his/her
adherence behavior, and the perceived behavioral
control (PBC) consisting of self efficacy: perceived ease
(yes I can!) to perform a certain adherence behavior
and the controllability, how much grip the patient has
on the desired and optimal adherence behavior in
different day to day settings.
Figure 2. Behavioral model for medication adherence (De Bruin & Hospers 2005)
83
Elmira
Ideally, an intervention to optimize adherence, uses
all three factors as building blocks to design a tailor-made
intervention in order to influence the intention and actual
adherence behavior: use peers, partner, or professional
to influence the patients norm, change the attitude of
the patient through effective and/or persuasive
communication. In order to influence PBC and self
efficacy (the last building block) it is advisable to
breakdown desired outcome behavior in sub goals,
facilitate this behavior (using adherence organizers like
pill boxes, electronic reminders), plan together with the
patient the execution of the desired adherence behavior
(fitting ARV treatment into the patients daily life) and
introduce self-monitoring and feedback mechanisms to
improve the awareness, reinforce desired behavior and
develop routine in ARV medication. De Bruin & Hospers
developed a 9 step intervention protocol using all above
mentioned behavioral determinants: knowledge improvement, definition of desired behavioral outcome and HIV
status, joined planning and reinforcement of desired
adherence behavior introducing adherence data and self
monitoring as feedback mechanism, defining causes of
(non-) adherence. This multi-disciplinary intervention
implemented in the Amsterdam Academic Medical
Centre outpatient clinic, resulted in an increase of mean
adherence from 82% to 93%. The Bandung ARV clinic
currently is developing a protocol, based on TPB, to study
and subsequently to design an intervention to improve
adherence to ARV.
According to the medication adherence model,
demographic and social/cultural aspects are minor
variables and are supposed to play an indirect role in
influencing behavior. However, current Bandung research
on access to VCT indicates that HIV patients only seek
VCT only after receiving the advice from a physician to
go for HIV testing.35 This observation confirms Conner
and Armitage64 advise to extend the TPB towards
inclusion of two new variables: self-identity: the way a
person relates his/her behavior to societal goals and moral
norms: the persons feeling to perform or not to perform
a particular behavior. In Indonesia social, cultural,
societal goals and societal influenced (group) norms
strongly determine behavior and it would be advisable to
adapt TPB and redefine these variables in the light of
the Indonesian context. When applied appropriatly and
used in the perspective of the targeted population, TPB
can be cultural specific.
DISCUSSION
Also in Indonesia, professionals face challenges to
change behaviors that are relevant in the field of HIV.
84
Acta Med Indones-Indones J Intern Med
Behaviors considered key to HIV prevention and care
are determined by a complex set of individual and
environmental factors. As pointed out, a well planned,
multi-disciplinary, evidence- and theory based approach
to influencing behavior can contribute a lot to improve
HIV prevention and access and quality of HIV care. In
order to identify determinants of specific risk- or health
behavior, current theories of behavior and behavior
change give all professionals working in prevention and
care effective tools to change behavior. TPB stands out
as particular useful for the HIV field but for practical
and theoretical reasons it needs more and appropriate
conceptualization, definition and explanation. For instance:
Bandungbased research, based on the TPB indicates
that IDUs intention (behavioral intention) is more
affected by the significant others (i.e, parent, peers) when
they ask them to do so (subjective norms) instead of
taking VCT as self-awareness (perceived behavioral
control), despite they have enough relevant knowledge
about the VCT services.38 This result illustrated nicely
that in decision making on what to do or not to do
(behavior intention) Indonesians are strongly influenced
by the value of collective culture, (based on what others
say) to a specific issue. This cultural specific
information,is very important input in the design process
of behavior (change) interventions that work in
Indonesia. As explained before, adherence to ARV as
another example, while description by TPB model is
embedded, supported, and facilitated by complex
behaviors, which can be explained and described through
the intercorrelation of each components in TPB model.
Anyhow, more evidences needed further explaination of
how variance of socio-demographic characteristics and
personality traits, correlated with behavior intention;
which sometimes means as limitation of TPB
explanation or application, so in practice need further
study and research to the approach itself to empower
the utility of the concept. It is advisable to adapt TPB in
the light of the Indonesian context.
CONCLUSION
As mentioned above, high risk behaviors to HIV/
AID (i.e. sharing needles, and sex-related behavior) can
not only be explained by a merely medical conceptual
approach. It needs also explanation based on behavioral
science concepts, as well as medical, and even cultural
concepts to describe the behavior intention, attitude,
perceived belief, or subjective norms, to gain a clear
picture and understanding of the behavior and to make
plan and conduct intervention for behavioral change in
further action. For this purpose researchers can use the
Vol 41 Supplement 1 July 2009
advantages of TPB as a useful overall model to describe
the relation and link of many important components as
reflected by the theory. Therefore, researchers, medical
-and behavioral sciences practitioners and interventionists are challenged to better understand and correctly
utilize existing empirically supported behavioral theories
like TPB, in the process of developing and evaluating
effective behavioral interventions in HIV prevention and
care.
REFERENCES
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
UNAIDS. Redefining AIDS in Asia: crafting an effective
response. Report of the Commission on AIDS in Asia. Bangkok:
UNAIDS; 2008.
UNAIDS. Epidemiological fact sheets on HIV/AIDS and
sexually transmitted infections-Indonesia- 2006. Geneva:
UNAIDS; 2006.
UNAIDS. AIDS epidemic update-2007. Geneva: UNAIDS;
2007.
NAC. HIV/AIDS in Indonesia: challenges and opportunities
for action. Jakarta: National AIDS Control Commission; 2001.
Republic of Indonesia, MOH tables contained in January 1997.
World Bank report no. 32572. Project performance assessment
report, Indonesia. HIV/AIDS and STDs prevention and
management project (LOAN NO. 3981). Jakarta: Ministry of
Health; 2005.
Pisani E, Garnett GP, Brown T, Stover J, Grassly NC, Hankins
C. et al. Back to basics in HIV-prevention: focus on exposure.
BMJ. 2003;326:1384-7.
UNAIDS. Epidemiological fact sheets on HIV and AIDS,
epidemiological core data on epidemiology and response.
Indonesia-Update 2008. Geneva: UNAIDS; 2008.
Indonesia Review: evidence to action. Available from: URL:
h t t p : / / w w w. a i d s d a t a h u b . o r g / f i l e s / d o c u m e n t s /
Indonesia_review_(FINAL_revision_2_08).pdf. Cited: April
04 2009.
Family Health International. AIDS in Asia; face the facts.
Bangkok: FHI; 2004.
Pisani E, Dadun, Sucahya PK, Kamil O, Jazan S. Sexual
behavior among injecting drug users in 3 Indonesian cities
carries a high potential for HIV spread to non-injectors. J Acquir
Immune Defic Syndr. 2003;34(4):403-6.
Pisani E, Lazzari S, Walker N, Schwartlander B. HIV
surveillance: a global perspective. J Acquir Immune Defic Syndr.
2003;32(Suppl.1):S3-11.
Saidel TJ, Des Jarlais DC, Peerapatanapokin W, Dorabjee J,
Sing S, Brown T. Potential impact of HIV among IDU on
heterosexual transmission in Asian settings: scenarios from the
Asian Epidemic Mode. Intern J Drug Policy. 2003;14:63-74.
Setiawan M, Patten J, Triadi A, Yulianto S, Adnyana T, Arif
M. Report on injecting drug use in Bali (Denpasar and Kuta):
results of an interview survey. Intern J Drug Policy. 1999;
10:109-16.
NAC. Country report on the following up to the declaration of
commitment on HIV/AIDS. UNGASS reporting period 20062007. Jakarta: National Aids Committee; 2008.
UNAIDS. Epidemiological fact sheets on HIV/AIDS and
sexually transmitted infections. Jakarta: UNAIDS; 2006.
Behavioral Aspects of HIV-prevention and Care in Indonesia
16. Anasrul SR, Fonny S. HIV/Young people among injecting drug
users cited from WHO/Searo fact sheet. Available from: URL:
http://www.searo.who.int/LinkFiles/Fact_Sheets_IndonesiaAHD-07.pdf, cited on April 16, 2009.
17. Kort de GL, Batra S, Nassirimanesh B, Pasaribu R, Ul-Hassan
S. Through the eye of the needle. International Conference on
AIDS. 15th ed. Bangkok, Thailand: 2004.
18. Boom J, Ven van der A , Iskander S, Hidayat T, Basar D, Zain T,
Crevel van R, Jong de C, Pinxten WJL. Needle exchange and
injection related risk behavior among intravenous drug users in
Bandung/ West Java. Poster presentation for the 2007 Open
Science Meeting Bali, November 15-18.
19. Unpublished data from routine reporting of Project IMPACT
and Dr. Hasan Sadikin Hospital. Bandung: Indonesia; 2009.
20. Indonesian office of the coordinating minister for peoples health/
national AIDS commission. National HIV/AIDS strategy.
Jakarta: National Aids Commission; 2007.
21. Impacts of HIV/AIDS 2005-2025 in Papua New Guinea,
Indonesia and East Timor. Final report of HIV epidemiological
modeling and impact study. Government of Australia: AUSAID,
Canberra: February 2006.
22. Ministry of Health Indonesia. Results ART in Indonesia:
Treatment situation until December 2008 (report in Indonesian language). Jakarta: Sub-Directorate HIV/AIDS/Ministry
of Health Indonesia; 2008.
23. Bartholomew KL, Parcel GS, Kok G. Intervention mapping: a
process for designing theory- and evidence-based health
education programs. Hlth Educ Behav. 1998;25:545-63.
24. Kok G. Targeted prevention for people with HIV/AIDS:
Feasible and desirable? Patient Education and Counseling. 1999;
36:239-46.
25. Bartholomew LK, Parcel GS, Kok G, Gottlieb NH. Planning
health promotion programs: an intervention mapping approach.
2nd ed. San Francisco (CA): Jossey-Bass; 2006.
26. Pinxten WJL, Boom J, Basar D, Iskander S, Hidayat T, Kamil
V, Zain T, Ven van der A, Hospers HJ. Sexual risk behavior and
low condom use among intravenous drug users in Bandung/
West Java. Poster presentation for the 2007 Open Science
Meeting Bali, November 15-18.
27. Ministry of Health, Statistics Indonesia, and National AIDS
Commission, Integrated biological-behavioral surveillance among
most-at-risk-groups (MARG) in Indonesia 2007. Surveillance
highlights: injecting drug users. 2008: Jakarta.
28. Santoso RR. The overt aggression pathway of male
adolescence in Bandung: The influence of personality trait,
parents discipline styles, and peers. Unpublished dissertation, Post Graduate Program University of Padjadjaran,
Bandung, 2009, 231-233, 262-267, 271
29. Monitoring the AIDS Pandemic (MAP) Network. Available
from: URL: http:// www.mapnetwork.org/reports.shtml. Cited
5 march 2009.
30. Jones GW, et al. Prostitution in Indonesia. In: Lim LL, editor.
The sex sector: the economic and social bases of prostitution in
South-east Asia. Geneva: ILO; 1998. p. 52-7.
31. Wisaksana R, Indrati A, Rogayah E, Sudjana P, Djajakusumah
TS, Ven van der A, Crevel van R. Response to highly active
antiretroviral therapy among HIV-infected patients with and
without a history of injecting drug use in Indonesia. Bandung:
IMPACT unpublished publication; 2009.
32. Bateganya MH, Abdulwadud OA, Kiene SM. Home-based HIV
voluntary counseling and testing in developing countries.
Cochrane Database. 2007;4:CD006493.
85
Elmira
33. Sweat M, Gregorich S, Sangiwa G, Furlonge C, Balmer D,
Kamenga C, Grinstead O, Coates T. Cost-effectiveness of
voluntary HIV-1 counseling and testing in reducing sexual
transmission of HIV-1 in Kenya and Tanzania. The Lancet.
2000;356(9224):113-21.
34. De Zoysa I, Phillips KA, Kamenga MC, OReilly KR, Sweat
MD, White RA, Grinstead OA, Coates TJ. Role of HIV
counseling and testing in changing risk behavior in developing
countries. AIDS. 1995;9(Suppl A):S95-101.
35. Hinduan ZR, Kesumah N, Crevel van R, Hospers HJ. Factors
associated with up taking voluntary counseling and testing
(VCT): a review of literature and empirical evidence from Dr.
Hasan Sadikin Hopital in Bandung, West Java, Indonesia.
Bandung: IMPACT unpublished publication; 2009.
36. Wolff B, Nyanzi B, Katongole G, Ssesanga D, Ruberantwari A,
Whitworth J. Evaluation of a home-based voluntary counseling
and testing intervention in rural Uganda. Health Policy Plan.
2005;20(2):109-16.
37. Mikolajczak J, Hospers HJ, Kok G. Reasons for not taking a
HIV-test among untested men who have sex with men: an
internet study. AIDS and Behavior. 2006;4(10):431-5.
38. Suherman H, Sodjakusumah TI, Fitriana E, Puspitasari TS,
Sumintardja EN, Pinxten WJL, Tasya IA, Hospers HJ.
Perceived barriers of taking HIV test (VCT) among IDUs in
Bandung. Bandung: IMPACT unpublished publication; 2009.
39. Iskander S, Basar D, Hidayat T, Siregar IM, Pinxten WJL,
Crevel van R, Ven van der A, Jong de C. The risk behavior
among current and former Injection Drug Users (IDUs) in
Bandung, West Java, Indonesia. Bandung: IMPACT
unpublished publication; 2009.
40. Paterson DL, Swidells S, Mohr J, Bresters M, Vergis EN, Squier
C, et al. Adherence to protease inhibitors, HIV-1 viral load, and
outcomes in patients with HIV infection. Ann Intern Med.
2000;133:21-30.
41. McNabb J, Ross JW, Abriola K, Turley C, Nightingale CH,
Nicolau DP. Adherence to highly active antiretroviral therapy
predicts virological outcome at an inner-city human immunodeficiency virus clinic. Clin Infect Dis. 2000;133:700-5.
42. Bangsberg DR, Weiser S, Guzman D, Riley E. 95% Adherence
is not necessary for viral suppression to less than 400 copies/
ml in the majority of individuals on NNRTI regimens. Twelfth
Conference on retroviruses and opportunistic infections. 2005;
poster 616.
43. Hawkins NJ, Butler CC, Wood F. Antibiotics in the
community: a typology of user behaviors. Patient Educ Couns.
2008;73(1):146-52.
44. Ammassari A, Trotta MP, Murri R, Castelli, F, Narciso P,
Noto P, et al. Correlates and predictors of adherence to highly
active antiretroviral therapy: overview of published research.
J Acquir Immune Defic Syndr. 2002;31(Suppl. 3):S123-S7.
45. World Health Organization. Adherence to long-term therapy:
evidence for action. Geneva: WHO; 2003.
46. Pence BW, Thielman NM, Whetten K, Ostermann J, Kumar V,
Mugavero MJ. Coping strategies and patterns of alcohol and
drug use among HIV-infected patients in the United StatesSoutheast. AIDS Patient Care STDS. 2008;11:869-77.
47. Talam NC, Gatongi P, Rotich J, Kimaiyo S. Factors affecting
antiretroviral drug adherence among HIV/AIDS adult patients
attending HIV/AIDS clinic at Moi teaching and referral
hospital, Eldoret, Kenya. East Afr J Public Health. 2008;5(2):
74-8.
86
Acta Med Indones-Indones J Intern Med
48. Waldrop-Valverde D, Jones DL, Weiss S, Kumar M, Metsch L.
The effects of low literacy and cognitive impairment on
medication adherence in HIV-positive injecting drug users. AIDS
Care. 2008;20(10):1202-10.
49. Braitsten P, Brinkhof MW, Dabis F, Schechter M, Boulle A,
Moitti P, et al. Mortality of HIV-1 infected patients in the first
year of antiviral therapy; comparison between low-income and
high-income countries. Lancet. 2006;356(6513):817-24.
50. Nieuwkerk PT, Oort FJ. Self-reported adherence to
antiretroviral therapy for HIV-1 infection and virological
treatment response; a meta analysis. J Acquir Immune Defic
Syndr. 2001;38(4):445-8.
51. Fishbein M. The role of theory in HIV prevention. AIDS Care.
2000;12(3):273-8.
52. Munro S, Lewin L, Swart T, Volmink J. A review of health
behavior theories: how useful are these for developing
interventions to promote long term medication adherence for
TB and HIV/AIDS? BMC Public Health. 2007;7:104.
Available from:URL: http://www.biomedcentral.com/14712458/7/104. cited January 26, 2009.
53. Glanz K, Rimer BK, Lewis FM. Health behavior and health
education. In: Theory Research and Practice. 3rd ed. San
Francisco: Jossey-Bass; 2002. p. 74-81.
54. Ajzen I. The theory of planned behavior. Organizational
Behavior and Human Decision Process. 1991;50:179-211.
55. Armitage CJ, Conner M. Social cognition models and health
behavior: a structured review. Psychology and Health. 2000;
15:173-89.
56. Armitage CJ, Conner M. Efficacy of the theory of planned
behavior: a meta-analytic view. British J Soc Psychol. 2001;
40:471-99.
57. Godin G, Kok G. The theory of planned behavior: a review of
its applications to health-related behaviors. American J Health
Promotion.1996;1:87-98.
58. Michie S, Johnston M, Francis J, Hardeman W, Eccles M.
From theory to intervention: mapping theoretical derived
behavioral determinants to behavior change techniques.
Applied Psychology: an international review. 2008;574:66080.
59. Shah B, Walshe L, Saple DG, Mehta,S, Ramnani JP, Kharkar
RC, Gupta B, Gupta A. Adherence to antiretroviral therapy
and virological suppression among HIV-infected persons
receiving care in private clinics in Mumbai, India. Clin
Infect Dis. 2007;44:1235-44.
60. Guarinieri M. Highly active antiretroviral therapy adherence:
the patients point of view. JAIDS. 2002;31:167-9.
61. Simoni JM, Frick PA, Pantalone DW, Turner BJ. Antiretroviral
adherence interventions: a review of current literature and
ongoing studies. Top HIV Med. 2003;11:185-98.
62. Rueda S, Park-Wyllie LY, Bayoumi A, Tynan AM, Antoniou,
Rourke S, Glazier R. Patient support and education for
promoting adherence to highly active antiretroviral therapy.
Cochrane collaboration 2009: http://www.thecochranelibrary.
com cited on January 26, 2009.
63. De Bruin M, Hospers HJ, Borne van de HW, Kok G, Prins JM.
Theory and evidence-based intervention to improve adherence
to antiretroviral theory in The Netherlands: a pilot study. AIDS
Patient Care and STDs. 2005;19(6):384-94.
64. Conner M, Armitage CJ. Extending the theory of planned
behavior: a review and avenues for further research. J Applied
Soc Psychol. 1998;28:146-9.
Anda mungkin juga menyukai
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Roles of MicroRNAs On Tuberculosis InfectionDokumen23 halamanThe Roles of MicroRNAs On Tuberculosis InfectionnatinlalaBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- MicroRNA-17 Untuk BCGDokumen12 halamanMicroRNA-17 Untuk BCGnatinlalaBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- microRNA 146aDokumen11 halamanmicroRNA 146anatinlalaBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Host-Directed Therapy of Tuberculosis - What Is in It For MicroRNADokumen4 halamanHost-Directed Therapy of Tuberculosis - What Is in It For MicroRNAnatinlalaBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Mir 155Dokumen7 halamanMir 155natinlalaBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Mirna - MDR MTBDokumen7 halamanMirna - MDR MTBnatinlalaBelum ada peringkat
- Tinjauan miRNA PDFDokumen11 halamanTinjauan miRNA PDFnatinlalaBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Perseption HivDokumen6 halamanPerseption HivnatinlalaBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- microRNA 146aDokumen11 halamanmicroRNA 146anatinlalaBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Mirna - MDR MTBDokumen7 halamanMirna - MDR MTBnatinlalaBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hiv/aids ..Dokumen22 halamanHiv/aids ..natinlalaBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Boateng2013 PDFDokumen8 halamanBoateng2013 PDFnatinlalaBelum ada peringkat
- Amfoterisin B - HPLCDokumen6 halamanAmfoterisin B - HPLCnatinlalaBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Formulasi Tablet VaginalDokumen9 halamanFormulasi Tablet VaginalnatinlalaBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Amfoterisin BDokumen4 halamanAmfoterisin BnatinlalaBelum ada peringkat
- Sativa: Blood Glucose Lowering Effect of Nigella in Alloxan Induced Diabetic RatsDokumen4 halamanSativa: Blood Glucose Lowering Effect of Nigella in Alloxan Induced Diabetic RatsnatinlalaBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- What Is Conjunctivitis and Pink Eye?Dokumen2 halamanWhat Is Conjunctivitis and Pink Eye?natinlalaBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- AntimikrobaaDokumen6 halamanAntimikrobaanatinlalaBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- PWDT YeeeyDokumen5 halamanPWDT YeeeynatinlalaBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Polimorfisme TransporterDokumen7 halamanPolimorfisme TransporternatinlalaBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Sativa: Blood Glucose Lowering Effect of Nigella in Alloxan Induced Diabetic RatsDokumen4 halamanSativa: Blood Glucose Lowering Effect of Nigella in Alloxan Induced Diabetic RatsnatinlalaBelum ada peringkat
- FarmakogenomiikDokumen5 halamanFarmakogenomiiknatinlalaBelum ada peringkat
- Susceptibility - of - Common - Bacterial Respiratory Pathogens To Antimicrobial Agents in Outpatients From South Backa DistrictDokumen7 halamanSusceptibility - of - Common - Bacterial Respiratory Pathogens To Antimicrobial Agents in Outpatients From South Backa DistrictnatinlalaBelum ada peringkat
- Goossens tcm18-198315Dokumen83 halamanGoossens tcm18-198315Just MahasiswaBelum ada peringkat
- On Being The Right Size - The Impact of Population Size and Stochastic Effects On The Evolution of Drug Resistance in Hospitals and The Community PDFDokumen11 halamanOn Being The Right Size - The Impact of Population Size and Stochastic Effects On The Evolution of Drug Resistance in Hospitals and The Community PDFnatinlalaBelum ada peringkat
- Antimicrobial Use and Indication-Based Prescribing Among General Practitioners in Eastern Croatia - Comparison With Data From The European Surveillance of Antimicrobial Consumption ProjectDokumen10 halamanAntimicrobial Use and Indication-Based Prescribing Among General Practitioners in Eastern Croatia - Comparison With Data From The European Surveillance of Antimicrobial Consumption ProjectnatinlalaBelum ada peringkat
- Impact of First-Line Antifungal Agents On The Outcomes and Costs of CandidemiaDokumen7 halamanImpact of First-Line Antifungal Agents On The Outcomes and Costs of CandidemianatinlalaBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- Hypoglycemic and Hepatoprotective Effects of Processed Aloe Vera Gel 2155 6156.1000303Dokumen6 halamanHypoglycemic and Hepatoprotective Effects of Processed Aloe Vera Gel 2155 6156.1000303Eric GibsonBelum ada peringkat
- 56 e F 05 PDFDokumen5 halaman56 e F 05 PDFnatinlalaBelum ada peringkat
- Standard of Care in DentistryDokumen8 halamanStandard of Care in DentistryKavitha P. DasBelum ada peringkat
- Child Health Problems GlobalDokumen86 halamanChild Health Problems GlobalBagus P Agen SuplierBelum ada peringkat
- Design NICUDokumen74 halamanDesign NICUMonica SurduBelum ada peringkat
- Final Exam of Dental Material: by Samir AlbahranyDokumen72 halamanFinal Exam of Dental Material: by Samir AlbahranyMustafa H. KadhimBelum ada peringkat
- Cleansing and Moist Greg Goodman 2009Dokumen1 halamanCleansing and Moist Greg Goodman 2009Prajnamita Manindhya El FarahBelum ada peringkat
- NP1 Nursing Board Exam June 2008 Answer KeyDokumen15 halamanNP1 Nursing Board Exam June 2008 Answer KeyBettina SanchezBelum ada peringkat
- Introduction To PainDokumen21 halamanIntroduction To Painayanle Abdi AliBelum ada peringkat
- HIQA Residential Care Standards 2008Dokumen86 halamanHIQA Residential Care Standards 2008Debora Tolentino Grossi0% (1)
- 9 1 EndosDokumen6 halaman9 1 EndosmghBelum ada peringkat
- PASSMED MRCP MCQs-INFECTIOUS DISEASES CompleteDokumen131 halamanPASSMED MRCP MCQs-INFECTIOUS DISEASES CompleteStarlight100% (1)
- Chemicals, Pharmaceuticals, Oil, Dairy, Food, Beverages, Paint & Others Industry DetailsDokumen12 halamanChemicals, Pharmaceuticals, Oil, Dairy, Food, Beverages, Paint & Others Industry DetailsSuzikline Engineering100% (1)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- How Can The Game End You?Dokumen1 halamanHow Can The Game End You?leikastarry NightBelum ada peringkat
- Evaluasi Penatalaksanaan Prolanis Di Puskesmas Kota BengkuluDokumen11 halamanEvaluasi Penatalaksanaan Prolanis Di Puskesmas Kota Bengkulunanasila02Belum ada peringkat
- 2021.10.27 Letter To NIHDokumen14 halaman2021.10.27 Letter To NIHZerohedge Janitor100% (1)
- Alginate ImpressionDokumen60 halamanAlginate ImpressionNugraha AnggaBelum ada peringkat
- Myocardial Infarction With CABG Concept MapDokumen1 halamanMyocardial Infarction With CABG Concept MapMaria Therese100% (1)
- Psychiatrist in Pune - Dr. Niket KasarDokumen8 halamanPsychiatrist in Pune - Dr. Niket KasarDr. Niket KasarBelum ada peringkat
- Patients ' Views of Wearable Devices and Ai in Healthcare: Findings From The Compare E-CohortDokumen8 halamanPatients ' Views of Wearable Devices and Ai in Healthcare: Findings From The Compare E-CohortPratush RajpurohitBelum ada peringkat
- Otago 1 PDFDokumen3 halamanOtago 1 PDFAde Maghvira PutriBelum ada peringkat
- Reflex Anal Dilatation An Observational Study On Non-Abused ChildrenDokumen5 halamanReflex Anal Dilatation An Observational Study On Non-Abused Childrenaniendyawijaya0% (1)
- Pathophysiology (Cervical Cancer) Case StudyDokumen7 halamanPathophysiology (Cervical Cancer) Case StudyRosalie Valdez Espiritu100% (2)
- Vehling Annika ResumeDokumen1 halamanVehling Annika Resumeapi-733364471Belum ada peringkat
- Burning Mouth SyndromeDokumen40 halamanBurning Mouth SyndromeSuci Sylvana HrpBelum ada peringkat
- Case Study 2Dokumen3 halamanCase Study 2XilcaBelum ada peringkat
- CystoclysisDokumen29 halamanCystoclysisKate PedzBelum ada peringkat
- Unit 11 FormatDokumen15 halamanUnit 11 Formatapi-26148150Belum ada peringkat
- Gambaran Kebutuhan Keluarga Pasien Diruang Intensif: Literature Review Nurhidayatul Nadya Gamya Tri Utami, Riri NovayelindaDokumen10 halamanGambaran Kebutuhan Keluarga Pasien Diruang Intensif: Literature Review Nurhidayatul Nadya Gamya Tri Utami, Riri Novayelindagamma kurnia mahananiBelum ada peringkat
- Palmer - Final CoachingDokumen9 halamanPalmer - Final CoachingDonald SebidanBelum ada peringkat
- Depression and Heart Disease - Johns Hopkins Women's Cardiovascular Health CenterDokumen3 halamanDepression and Heart Disease - Johns Hopkins Women's Cardiovascular Health CenterSanjay KumarBelum ada peringkat
- PrediabetesDokumen8 halamanPrediabetesVimal NishadBelum ada peringkat
- Healing Your Aloneness: Finding Love and Wholeness Through Your Inner ChildDari EverandHealing Your Aloneness: Finding Love and Wholeness Through Your Inner ChildPenilaian: 3.5 dari 5 bintang3.5/5 (9)
- Breaking Addiction: A 7-Step Handbook for Ending Any AddictionDari EverandBreaking Addiction: A 7-Step Handbook for Ending Any AddictionPenilaian: 4.5 dari 5 bintang4.5/5 (2)
- Save Me from Myself: How I Found God, Quit Korn, Kicked Drugs, and Lived to Tell My StoryDari EverandSave Me from Myself: How I Found God, Quit Korn, Kicked Drugs, and Lived to Tell My StoryBelum ada peringkat
- Allen Carr's Easy Way to Quit Vaping: Get Free from JUUL, IQOS, Disposables, Tanks or any other Nicotine ProductDari EverandAllen Carr's Easy Way to Quit Vaping: Get Free from JUUL, IQOS, Disposables, Tanks or any other Nicotine ProductPenilaian: 5 dari 5 bintang5/5 (31)
- Allen Carr's Easy Way to Quit Smoking Without Willpower: The best-selling quit smoking method updated for the 21st centuryDari EverandAllen Carr's Easy Way to Quit Smoking Without Willpower: The best-selling quit smoking method updated for the 21st centuryPenilaian: 5 dari 5 bintang5/5 (47)
- Stop Drinking Now: The original Easyway methodDari EverandStop Drinking Now: The original Easyway methodPenilaian: 5 dari 5 bintang5/5 (28)