Overview of Perioperative Nutritional Support
Diunggah oleh
dadupipaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Overview of Perioperative Nutritional Support
Diunggah oleh
dadupipaHak Cipta:
Format Tersedia
7/25/2016
Overviewofperioperativenutritionalsupport
OfficialreprintfromUpToDate
www.uptodate.com2016UpToDate
Overviewofperioperativenutritionalsupport
Authors
KathleenMFairfield,MD,DrPH
RezaAskari,MD,FACS
SectionEditors
TimothyOLipman,MD
HilarySanfey,MD
DeputyEditor
KathrynACollins,MD,PhD,FACS
Alltopicsareupdatedasnewevidencebecomesavailableandourpeerreviewprocessiscomplete.
Literaturereviewcurrentthrough:Jun2016.|Thistopiclastupdated:Apr05,2016.
INTRODUCTIONMalnutritioninhospitalizedpatientsiswelldocumentedwithratesupto50percentincertain
populations[1].Nutritionalsupportmaybeindicatedformalnourishedindividualsrequiringsurgicalintervention,orfor
healthyindividualsundergoingmajorsurgerywithananticipatedlengthyrecoverytimetoreturnofnormal
gastrointestinalfunctionhowever,itcanbeunclearwhenitisappropriatetointervene.Thenotionthatmalnutritioncan
affectoutcomesinsurgicalpatientswasfirstreportedin1936inastudyshowingthatmalnourishedpatients
undergoingulcersurgeryhada33percentmortalityratecomparedwith3.5percentinwellnourishedindividuals[2].A
prospectivestudyof500patients,including200surgicalpatients,admittedtoateachinghospitalinEnglandfoundthat
40percentofpatientswereundernourishedonpresentation,andpatientslostanaverageof5.4percentoftheirbody
weightduringtheirhospitalstay[3].
Thenutritionalassessmentofsurgicalpatients,optionsforandpotentialbenefitsofnutritionalsupportarereviewed
here.Anoverviewofparenteralandenteralnutritionandissuesrelatedtonutritionalsupportincriticallyillpatients,and
otherspecificpopulations(eg,cancer,burns,lungdisease)arediscussedinseparatetopicreviews.
CONSEQUENCESOFMALNUTRITIONINSURGICALPATIENTSReducedfoodintakeresultsinlossoffat,
muscle,skin,andultimatelyboneandviscera,withsubsequentweightloss,andexpansionoftheextracellularfluid
compartment[4].Nutritionalrequirementsfallasanindividual'sbodymassdecreases,probablyreflectingmore
efficientutilizationofingestedfoodandareductioninworkcapacityatthecellularlevel.However,thecombinationof
decreasedtissuemassandreducedworkcapacityimpedesnormalhomeostaticresponsestostressorssuchas
surgeryorcriticalillness[5].
Thestressofsurgeryortraumacreatesahypermetabolicstate,increasingproteinandenergyrequirements.
Macronutrients(fat,protein,andglycogen)fromthelabilereservesoffattissueandskeletalmuscleareredistributedto
moremetabolicallyactivetissuessuchastheliverandvisceralorgans.Thisresponsecanleadtotheonsetofprotein
caloriemalnutrition(definedasanegativebalanceof100gofnitrogenand10,000kcal)withinafewdays[6].Therate
ofdevelopmentofpostoperativemalnutritioninagivenindividualdependsupontheirpreexistingnutritionalstatus,
natureandcomplexityofthesurgicalprocedure,andthedegreeofhypermetabolism.
Malnutritioncausesanumberofnegativeconsequences,including[4,5,7,8]:
Increasedsusceptibilitytoinfection
Poorwoundhealing
Increasedfrequencyofdecubitusulcers
Overgrowthofbacteriainthegastrointestinaltract
Abnormalnutrientlossesthroughthestool
Ofparticularconcernforpatientsundergoingsurgeryaretherisksofpostoperativeinfectionandpoorwoundhealing.
Malnutritionleadstoimmunesystemdysfunctionbyimpairingcomplementactivationandproduction,bacterial
opsonization,andthefunctionofneutrophils,macrophages,andlymphocytes[8].Oneseriesofunderfedpatients
identifiedsubnormalskinreactionstoCandidaandlowlevelsofantibodiestovariousphytomitogens,suggestingthat
humoralandcellmediatedimmunityareaffected[9].(See"Secondaryimmunodeficiencyduetounderlyingdisease
states,environmentalexposures,andmiscellaneouscauses",sectionon'Malnutrition'.)
Patientswithproteinenergymalnutritionalsohaveslowerratesofwoundhealing[10],althoughmostwoundswill
eventuallyhealontheirown[11].Additionaladverseeffectsassociatedwithmalnutritionwereidentifiedinastudyof
2743patientsundergoingcardiothoracicsurgery[12].Patientswithpreoperativehypoalbuminemiaaloneorin
associationwithchronicliverdiseaseorheartfailureweremorelikelytohavepostoperativeorgandysfunction
(cardiac,pulmonary,renal,hepatic,neurologic),gastrointestinalbleeding,nosocomialinfections,increaseddayson
mechanicalventilationandlengthofstayintheintensivecareunit,andinpatientdeath.Abodymassindex(BMI)<20
kg/m2wasassociatedwithlowermorbidityandmortalitycomparedwithahigherBMIhowever,thisfindinginthis
http://www.uptodate.com/contents/overviewofperioperativenutritionalsupport?topicKey=SURG%2F2880&elapsedTimeMs=3&source=search_result&s 1/12
7/25/2016
Overviewofperioperativenutritionalsupport
studycontrastswithotherstudies.BMIisanimperfectmeasureofnutritionalstatusandshouldbeusedinconjunction
withotherclinicalindicators.
NUTRITIONALASSESSMENTINTHESURGICALPATIENTThefirsttaskwhenconsideringperioperative
nutritionalrecommendationsistoassesswhetherornotthepatienthasmalnutrition.Thebasicprincipleofdietaryand
nutritionalassessmentinthegeneralpopulationisdiscussedelsewhere.Importantaspectsofnutritionalassessment
thatpertaintosurgicalpatientsarereviewedbelow.(See"Dietaryassessmentinadults".)
Baseduponexpertconsensus,adiagnosisofmalnutritionrequiresthatthepatientexhibittwoormoreofthefollowing
[13,14]:
Insufficientenergyintake
Weightloss
Lossofmusclemass
Lossofsubcutaneousfat
Localizedorgeneralizedfluidaccumulationthatmaysometimesmaskweightloss
Diminishedfunctionalstatusasmeasuredbyhandgripstrength
HistoryandphysicalSeveralaspectsofthepastmedicalhistoryareofparticularimportance,includingchronic
disease(particularlydiabetes),infection,recenthospitalization,andpriorsurgery(particularlygastrointestinalsurgery).
Onreviewofsystems,ahistoryofweightlossorgainisimportant.Anyrecentlossesorgains(andwhethertheywere
purposefulornot)priortothehospitalstayshouldbeassessed.Thedetailsofthecurrenthospitalizationalsoplaya
centralrole.Newlyadmittedtraumapatientswhoareotherwisewellhavedrasticallydifferentneedsfrompatientswho
havehadsurgeryseveralweeksinthepastbuthaveremainedhospitalizedduetocomplications.
Inadditiontocollectinginformationoncurrentmedications,nonprescriptionmedicinesandothersupplementsshould
benoted.Theuseofdietarysupplements,suchasproteinshakes,shouldalsobedetermined.Lastly,anyallergiesor
foodintolerancesshouldalsobenoted.Adiethistoryshouldbecollectedfromthepatient,family,orcarefacility.
Althoughthereareseveralmethodsofdietaryassessment,themostusefulandstraightforwardmaybetoassessthe
usualintakeonanaveragedaybeforehospitalizationorbeforetheonsetofthecurrentillness[15].
Inadditiontovitalsignsandageneralphysicalexamination,thefollowingshouldbenoted:
Heightandweight(calculatebodymassindex[BMI]usingweightinkgdividedbyheightinmeterssquared
(calculator1),orusinganomogram)(figure1)
General:Lossofsubcutaneousfat,anygeneralizedfluidaccumulation
Headandneckexam:Hairloss,bitemporalwasting,conjunctivalpallor,xerosis,glossitis,bleedingorsoreson
thegumsandoralmucosa,angularcheilosisorstomatitis,dentition
Cardiovascular:Evidenceofheartfailureorhighoutputstate
Neck:Thyromegaly
Extremities:Edema,lossofmusclemass
Neurologic:Evidenceofperipheralneuropathy,reflexes,tetany,mentalstatus,handgripstrength
Skin:Ecchymoses,petechiae,pallor,pressureulcers,assessmentofsurgicalwoundhealingandsignsof
surgicalsiteinfection(ifpostoperative).
Signsofspecificnutritionaldeficienciesshouldalsobesought.Someofthesearegiveninthetable(table1).
Appropriatemicronutrientlevelsshouldbeinvestigateddependingonclinicalexamfindings.(See'Otherlaboratory
studies'below.)
Severalclinicaltoolsareavailabletoquicklyassessandscorenutritionstatus.TheSubjectiveGlobalAssessmentof
NutritionalStatusisabrieftoolthatincludeshistoryandphysicalexaminationfindings,andallowsstandardized
assessment[16].TheNutritionalRiskScreeningtool(NRS2002)canbeappliedrapidlyandusedtoscreenforpoor
baselinenutritionalstatus[17].AstudythatassessedtheabilityoftheNRS2002scoretopredicttheincidenceand
severityofpostoperativecomplicationsfoundtheoverallincidenceofnutritionalriskwas14percentamong608
patientsundergoinggastrointestinalsurgery[18].Asignificantlyhigheroverallcomplicationratewasfoundinpatients
atnutritionalriskcomparedwiththosewithanormalNRS2002riskscore(40versus15percent).Severe
complicationswerealsosignificantlyhigherinpatientsatnutritionalrisk(54versus15percent).
http://www.uptodate.com/contents/overviewofperioperativenutritionalsupport?topicKey=SURG%2F2880&elapsedTimeMs=3&source=search_result&s 2/12
7/25/2016
Overviewofperioperativenutritionalsupport
AssessingproteinstatusAssessingproteinstatusisparticularlyimportantinthesurgicalpatientbecauseofthe
closerelationshipbetweenproteinstatusandwoundhealing,andbecauseproteincaloriemalnutritioncanbetreated
withsupplementationasdiscussedbelow[19,20].Proteinstatusisaffectedbypreviousintake,musclemass,duration
ofcurrentillness,bloodloss,woundhealing,infections,andgastrointestinalabsorption.
Threeserummeasuresofproteinstatushavedifferinghalflives.Theseserumcomponentsdonotdirectlyindicate
nutritionalstatus,butratherreflecttheseverityofillnessandmustbeusedinconjunctionwithotherclinicaldatasuch
asthedurationofthecurrentsurgicalillnesstobeusefulindeterminingtherapy.Althoughdecreasedlevelsforthese
proteinmarkerscorrelatewithadverseoutcomes,improvementsinthesemarkerswithnutritionalsupplementationare
notreliablyassociatedwithaclinicalbenefit[21].(See'Outcomesfornutritionalintervention'below.)
Serumalbuminhasthelongesthalflifeat18to20daysandisthemostextensivelyusedparameter.Lowserum
albumin(<2.2g/dL)isamarkerofanegativecatabolicstate,andapredictorofpooroutcome[22].Surgical
stress,otheracutestresses,hepaticdisease,andrenaldiseasedecreaseserumalbuminlevels.
Serumtransferrinhasanintermediatehalflifeofeighttoninedays,reflectingproteinstatusoverthepasttwoto
fourweeks.Transferrinalsoreflectsironstatus,andlowtransferrinshouldbeconsideredanindicatorofprotein
statusonlyinthesettingofnormalserumiron.
Serumprealbumin(transthyretin)hastheshortesthalflifeattwotothreedays.Althoughprealbuminresponds
quicklytotheonsetofmalnutritionandrisesrapidlywithadequateproteinintake,thelevelcanbealteredinthe
acutephaseresponseduetoacuteorchronicinflammation.Ingeneral,inflammatorycytokinesreducethelevel
ofprealbuminsynthesisbytheliver,anditcanalsobereducedwithrenalandhepaticdisease.Therefore,serum
prealbuministheleasthelpfulofthethreeforassessingoverallnutritionalstatus.
OtherlaboratorystudiesInadditiontoassessingproteinstatus,afewotherlaboratorystudiesmaybehelpful.
Electrolytes,glucose,andBUN/creatininehelpassessoverallclinicalandfluidvolumestatusandneedtobeobtained
ifparenteral(intravenous)nutritionwillbeinstituted.Ironlevelsshouldbemeasuredinthesettingofunexplained
anemia,asshouldspecificvitaminlevelsifclinicallyindicated(eg,B12/folateinmacrocyticanemias,othersbased
uponspecificphysicalsigns).Serumcalcium,magnesium,andphosphorousshouldalsobeassessedperiodically,
particularlyinthesettingofpoororalintakeordiarrhea[23].
NUTRITIONALINTERVENTIONSOncethepresenceofmalnutritionisestablished,oritbecomesclearthatthe
patientwillnotbeabletomaintainadequatenutrition,nutritionalinterventionmayincludeoralsupplementation,enteral
(tube)feeding,orparenteral(intravenous)feeding.Enteralsupportisrecommendedoverparenteralsupportbecauseof
itsrelativesimplicity,safety,reducedcomplications,andlowercost,aswellasitsabilitytomaintainmucosalbarrier
function.
EnteralnutritionEnteralnutritionsupportreferstotheprovisionofcalories,protein,electrolytes,vitamins,
minerals,traceelements,andfluidsviaanintestinalroute,eitherorallyorviaafeedingtube.
OralsupplementationThereisawidevarietyofsupplementsavailablefororalsupplementationinawide
rangeofstyles(juice,yogurt,milkshakes),formats(liquid,powder,pudding,prethickened),types(high
protein,fibercontaining,lowvolume),energydensities(1to2.4Kcal/mL),andflavors.Mostoral
supplementsprovide300Kcal,12gprotein,andafullrangeofvitaminsandminerals.Specifictypesoforal
supplementsmaybenefitcertaingroups.Ingeneral,highproteinoralsupplementsaremostsuitablefor
patientswithwounds,andthosewithmalignancy.Prethickenedsupplementsandpuddingsarehelpfulfor
providingnutritionalsupporttoindividualswithdysphagiaandthosewithneurologicalconditions.
TubefeedingEnteralnutritionmaybedeliveredinagastricorpostpyloricfashion.Theavailable
formulations,components,anddeliveryofenteralnutritionarereviewedelsewhere.(See"Nutritionsupport
incriticallyillpatients:Anoverview"and"Nutritionsupportincriticallyillpatients:Enteralnutrition".)
ParenteralnutritionParenteralnutritionisanintravenoussolutionthatcontainsdextrose,aminoacids,
electrolytes,vitamins,minerals,andtraceelements.Theavailableformulations,components,anddeliveryof
parenteralnutritionarereviewedelsewhere.(See"Nutritionsupportincriticallyillpatients:Anoverview"and
"Nutritionsupportincriticallyillpatients:Parenteralnutrition".)
Asthecomplexinteractionsbetweennutrition,mucosalbarrierfunction,immunoregulation,andsevereillnesshave
becomeclearer,tailoredformsofenteralnutritionalsupportforspecificdiseasestateshavebeendeveloped.Many
enteralandparenteralformulascontainnutrientspreviouslyconsiderednonessential,suchasarginine,glutamine,RNA
nucleotides,andomega3fattyacids.Duringanepisodeofcriticalillness,thesenutrientsmaybecome"conditionally
http://www.uptodate.com/contents/overviewofperioperativenutritionalsupport?topicKey=SURG%2F2880&elapsedTimeMs=3&source=search_result&s 3/12
7/25/2016
Overviewofperioperativenutritionalsupport
essential."Formulasthataresupplementedwiththesecomponentsareoftenreferredtoasimmuneenhancing
nutritionalsupplements,orsimplyimmunonutrition.(See"Nutritionsupportincriticallyillpatients:Anoverview"and
'Immuneenhancingnutritionalsupplements'below.)
INDICATIONSThegeneralindicationsfornutritionalsupportincludepreexistingnutritionaldeprivation,anticipated
oractualinadequateenergyintakebymouth,andsignificantmultiorgansystemdisease.Amongpatientsundergoing
surgery,patientswhoundergogastrointestinalsurgerymaybeatagreaternutritionaldisadvantageifthereturnof
intestinalfunctionissignificantlydelayed[2430].
Earlyenteralfeeding(oral,tubefeeding)canbeinstitutedfollowingmanytypesofsurgery[30,31].ACochranereview
andmetaanalysisupdatedin2011identifiednoobviousadvantagetotheroutinepracticeofmaintainingpatientsnil
peros(ie,NPO)postoperatively[32].Thereviewidentified14trialsthatincluded1224patientsundergoing
predominantlycolorectalsurgery.Nosignificantdifferenceswereidentifiedintheriskofintraabdominalabscess,
anastomoticleak/dehiscence,orpneumoniaforpatientsstartedonearlyoralnutrition(initiatedwithin24hoursof
surgery)comparedwithtraditionalsurgicalcare(ie,nonutritionororalnutritionwhentolerated).Lengthofhospitalstay
andtheincidenceofpostoperativewoundinfectionwerealsosimilar.Ametaanalysisofsixofthetrialsfoundaslightly
increasedriskofvomiting(riskratio1.27,95%CI,1.011.61).Thehigherincidenceofvomitingreportedintheearly
feedinggroupdidnotappeartoberelatedtooralintakecomparedwithtubefeeding.Noadditionalinformationwas
givenregardingthetypeofsurgery(openversuslaparoscopic),orperioperativepainmanagement(eg,opioidor
antiemeticuse).Alatersystematicreviewandmetaanalysisthatfocusedoncolorectalsurgeryfoundsimilarresults
therewasareducedlengthofhospitalstay,butnosignificantdifferenceintherateofvomitingbetweenthosewho
receivedearlyoralfeedingcomparedwiththosewhodidnot[33].
Somepatients,suchasthosewithinflammatoryboweldisease,haveanincreasedriskofbeingmalnourishedwhen
undergoingsurgicalprocedures.Aperiodofbowelrest(nilperos)maybeappropriateforpatientswithdiseasethatis
severeenoughtorequiresurgicalintervention.(See"Nutritionanddietaryinterventionsinadultswithinflammatory
boweldisease".)
Parenteralsupportisindicatedinpostoperativepatientswhoareunabletoreceiveadequateenteralnutritionby
postoperativedays10to14[26,34].Earlierenteralsupportmaybeappropriateinpatientswhoaremalnourishedat
baseline,orwhohaveacomplicatedpostoperativecourse[23,35].Inpatientsundergoingbowelsurgeryfor
gastrointestinalmalignancy,malignancyrelatedmetabolicchangesmayalsosuggesttheneedforearlierintervention.
OUTCOMESFORNUTRITIONALINTERVENTIONThemajorityoftrialsevaluatingthepotentialbenefitsof
perioperativenutritionalsupportaresmall,andcomparisonsaredifficultduetothewidevarietyofsurgeriesstudied,
variabilityinmethodology,andalackofstandarddefinitionsandmeasuresofmalnutritionused.Therisksassociated
witheachrouteofnutritionalsupport,plustheaddedcost,needtobetakenintoaccount,alongwiththepotential
benefits,whenassessingtheneedforperioperativenutritionalsupport.
PreoperativenutritionalsupportPatientswithseveremalnutritionmayderivesomebenefitfromdelayingsurgery
tobefed,butareatanincreasedriskforinfectiouscomplicationsiftreatedwithtotalparenteralnutrition.Patientswill
benefitmorefromenteralfeedingwheneveritispossible.Forpatientswhoareadequatelynourishedorwhohavemild
tomoderatemalnutrition,surgeryneednotbedelayedforpreoperativeparenteralorenteralsupplementation[24,25,35].
(See'Indications'above.)
Amulticentercohortstudyevaluatedtheeffectofpreoperativenutritionalsupportin512patientsundergoingabdominal
surgerywhowereatnutritionalriskasdefinedbytheNutritionalRiskScreeningTool2002(NRS2002)[35].Ofthe120
patientswithanNRSscore5,thecomplicationratewassignificantlylowerinthepreoperativenutritiongroup
comparedwiththecontrolgroup(25.6versus50.6percent).Thelengthofhospitalstaywassignificantlyshorterinthe
preoperativenutritiongroupthaninthecontrolgroup(13.7versus17.911.3days).Nosignificantdifferenceswere
seenforlesserNRSscores.
OralsupplementationAsystematicreviewthatfocusedonpreoperativenutritioninpatientsundergoing
gastrointestinalsurgeryincludedthreestudiescomparingpreoperativeliquidoralsupplementationwithusualcareor
dietaryadvice[36].Nosignificantdifferenceswerefoundintheoverallincidenceofcomplications,infectious
complications,orlengthofstay.Eachofthetrialsevaluatedadifferentoralsupplement.
ParenteralfeedingSeveralmetaanalyseshaveevaluatedpreoperativeparenteralnutrition,buthavereached
inconsistentconclusions[3739].
Onesystematicreviewfoundthatpreoperativeparenteralnutrition(13randomizedtrials)decreasedpostoperative
complicationsby10percent,whilepostoperativeparenteralnutritionalone(8randomizedtrials)resultedina10percent
http://www.uptodate.com/contents/overviewofperioperativenutritionalsupport?topicKey=SURG%2F2880&elapsedTimeMs=3&source=search_result&s 4/12
7/25/2016
Overviewofperioperativenutritionalsupport
increaseincomplicationrates[39].Thesefindingswerenotverifiedbyasubsequentlargermetaanalysisthatincluded
41trialsofparenteralnutritionprovidedbeforeand/oraftersurgery[38].Parenteralnutritionhadnoeffecton
postoperativemortalityandtherewasnosignificanteffectonpostoperativecomplicationrates,althoughtrendsforall
evaluatedoutcomesfavoredparenteralnutritionovernonutrition.
Anothermetaanalysis(26randomizedtrials,although3werenotinsurgicalpatients)foundthatparenteralnutrition
decreasedhospitalcomplicationsinstudieswherelipidfreesolutionswereused,andforpatientswhowere
malnourished(notconsistentlydefined)[37].Thesefindingswerealsonotconfirmedinthelargermetaanalysis,which
foundgreaterbenefitfortotalparenteralnutritionintrialswherelipidswereused,andintrialsevaluatingwellnourished
patients[38].
Studieshavealsofocusedonwhetherparticularsubgroupsmightbenefitfrompreoperativeparenteralfeeding.
Anearlystudysuggestedthatparenteralnutritionwasbeneficialinpatientswithuppergastrointestinal
malignancies[40,41].Mortalityandpostoperativecomplicationsweredecreasedinagroupofpatientswith
gastrointestinalmalignanciesandweightloss(minimum10percent)whoreceived10daysofpreoperative
parenteralnutritionand9daysofpostoperativetotalparenteralnutrition,comparedwithcontrolpatientswhodid
notreceivepreoperativeparenteralnutritionandwereonlypartiallysupplementedpostoperatively[42].
Preoperativetreatmentwithparenteralnutritionalsodecreasedmorbidityinagroupofpatientsundergoing
resectionforhepatocellularcancer[43].(See"Theroleofparenteralandenteral/oralnutritionalsupportinpatients
withcancer".)
TheVACooperativestudyrandomlyassignedpatientstoparenteralnutritionforsevendayspreoperativelyand
threedayspostoperativelyortocontrolgroupswhoeitherreceivednonutritionorwerefedenterally[44].Overall,
patientswhoreceivedparenteralnutritionhadahigherrateofinfectiouscomplications(14.1versus6.4percent),
butmortalityrateswerenotsignificantlydifferent(7.3and4.9percentat30days).However,intheseverely
malnourishedsubgroup,thosetreatedwithparenteralnutritionhadfewermajorpostoperativecomplicationsthan
controls(20to25percentversus40to50percent).
Inalatersystematicreview(discussedabove)thatfocusedonpatientsundergoinggastrointestinalsurgery,
preoperativeparenteralnutritionsignificantlyreducedtheriskformajorcomplications(relativerisk0.64,95%CI
0.46087).However,nodifferencewasobservedforinfectiouscomplications[36].
PostoperativenutritionalsupportFormanypostoperativepatients,earlyenteralnutrition(<24hours)ispossible
andisassociatedwithbeneficialeffects.Enteralnutrition(oralortubefeeds)ratherthanparenteralnutritionshouldbe
institutedwheneverpossible.Forpatientswithadelayedreturnofintestinalfunction,postoperativeparenteralnutrition
isindicatedonlyifreturnofbowelfunctionisnotanticipatedformorethan10days.Earlierinterventionmaybe
appropriateinpatientswhoareseverelymalnourishedatbaseline,orwhohaveacomplicatedpostoperativecourse.
(See'Indications'above.)
EarlyenteralfeedingEarlypostoperativeenteralnutritionalsupportmaydecreasetheincidenceofinfectious
complications,butdoesnotimpactotheroutcomes.Earlynutritionisacomponentofmostenhancedrecoveryafter
surgeryprotocols(ERAS)[4547].
Ametaanalysisevaluated44randomizedtrialsofperioperativeenteralnutrition(predominantlypostoperative
support)[48].Trialsweregroupedintothreecomparisons:enteralnutritionversusnoartificialnutrition,enteral
nutritionversusparenteralnutrition,andvolitionalnutritionalsupplements(oralsupplementalfeeding)versusno
artificialnutrition.Therewerenomortalitydifferencesforanyofthecomparatorgroups.Comparedwithno
artificialnutrition,patientsreceivingenteralnutritionhadfewerinfections(absoluterisk11percent,95%CI20to
1percent),buttherewasnosignificantimpactondurationofhospitalizationortheincidenceofwound
complications.Patientswhoreceivedpostoperativeoralnutritionalsupplements,comparedwithnosupplements,
alsohadadecreasedinfectionrate(absoluteriskdifference10percent95%CI19to1),andashorterlengthof
hospitalstaybytwodays(95%CI3.37to0.72).
Anothermetaanalysiscomparingenteralnutritionwithin24hoursofgastrointestinalsurgerywithtraditional
postoperativemanagementshoweda45percentdecreaseintheriskofoverallpostoperativecomplicationsin
thosepatientsreceivingearlypostoperativefeeding.Therewerenodifferencesintheincidenceofanastomotic
dehiscence,lengthofstay,ormortality[49].
TotalparenteralnutritionPatientswhoareunabletotolerateenteralnutritionalsupportwillrequireintravenous
fluidandtotalparenteralnutritionatthediscretionofthetreatingteamuntilsuchtimeastheycanbetransitionedto
enteralnutrition.Theoutcomesoftotalparenteralnutritionincriticallyillpostoperativepatients,andfollowingburnand
http://www.uptodate.com/contents/overviewofperioperativenutritionalsupport?topicKey=SURG%2F2880&elapsedTimeMs=3&source=search_result&s 5/12
7/25/2016
Overviewofperioperativenutritionalsupport
cancersurgery,arediscussedelsewhere.(See"Nutritionsupportincriticallyillpatients:Anoverview"and"Overview
ofnutritionalsupportformoderatetosevereburnpatients"and"Theroleofparenteralandenteral/oralnutritional
supportinpatientswithcancer".)
ImmuneenhancingnutritionalsupplementsTheroleforimmuneenhancingnutritionalsupplements,alsoreferred
toasimmunonutrition,remainsunclear.Thereisinsufficienthighqualityevidencetosuggestanyspecificaminoacid
orothersupplementationforallsurgicalpatients.(See'Nutritionalinterventions'above.)
Severalmetaanalyseshaveevaluatedimmunonutrition(ie,enteralorparenteralsupplementationwitharginine,
glutamine,nonessentialfattyacids,branchedchainfattyacids,orRNA)insurgicalpatients[36,5052].Reductionsin
infectiouscomplicationsandlengthofhospitalstayhavebeenfound,butwithoutaneffectonmortality.A2012
Cochranereviewandmetaanalysisofpreoperativenutritionalsupportfoundthatimmunonutrition(sixtrials)
significantlydecreasedtheriskofcomplications(noninfectiousandinfectious)(relativerisk0.67,95%CI0.530.84)
[36].Thevariousmetaanalyseshavebeeninconsistentintheirresultsandarewithoutsufficientstrengthtomake
clinicalrecommendations[50,51,53,54].Theauthorsofthesemetaanalyseshavenotedmethodologicalflawsinthe
individualstudies.Itisworthnotingthatsurgicalpatientsatthehighestriskforpostoperativecomplicationshavebeen
excludedfromthemajorityofstudiesonimmunonutrition.Thus,untilhigherqualitydatademonstratingunequivocal
benefitareavailable,immunonutritioncannotberecommendedasaroutineadditiontonutritionalsupplementationin
surgicalpatients.
Studiesofindividualandcombinationsofcomponentsofimmunonutritionhavedemonstratedsomebenefitbutno
effectonsurvivalinsurgicalpatients[15,50,51,5465].Separatemetaanalyseshavefoundasignificantlyreduced
incidenceofinfectiouscomplicationsandreducedlengthofhospitalstayforpatientsreceivingsupplementalglutamine
[51],orarginine[50].However,alatermulticentertrialrandomlyassigned150intensivecareunitpatientsrequiring
parenteralnutritionaftergastrointestinal,vascular,orcardiacsurgerytoreceivestandardglutaminefreeparenteral
nutritionoralanylglutaminedipeptideparenteralnutrition[66].Therewerenosignificantdifferencesbetweenthe
groupsforcumulativemortalityatsixmonths,theincidenceofbloodstreaminfection,oranyotheradverseevent.
However,thisstudywaslikelyunderpoweredtofullyassesstheseoutcomes.
SUMMARYANDRECOMMENDATIONS
Malnutritionisaprevalentconditionwithimportantimplicationsforpatientsundergoingsurgery.Whenevaluating
thepatientforpossibleintervention,thepatient'snutritionalstatusshouldbeassessedbyperformingahistory
andphysicalexamination.Judicioususeoflaboratorytestsaimedatassessingproteinstatusisuseful.(See
'Consequencesofmalnutritioninsurgicalpatients'aboveand'Nutritionalassessmentinthesurgicalpatient'
aboveand"Dietaryassessmentinadults".)
Studiesregardingoutcomesofnutritionalinterventionsintheperioperativeperiodarenumerousbutareoftenof
lowquality,andcomparisonsaredifficultgiventhebroadrangeofsurgicalsettingsandinterventions.However,
ourgeneralrecommendationsareasfollows:(see'Nutritionalinterventions'aboveand'Outcomesfornutritional
intervention'above)
Forpatientswhoarenotmalnourishedorwhohavemildtomoderatemalnutrition,surgeryshouldnotbe
delayedforpreoperativeenteralorparenteralfeeding.
Patientswithseveremalnutritionmayderivesomebenefitfromdelayingsurgerytobefed.
Patientsclearlybenefitmorefromenteralfeeding,wheneverpossible,ratherthantotalparenteralnutrition
(TPN),asTPNisassociatedwithanincreasedriskforinfectiouscomplications.
Formanypatientsundergoingsurgery,earlyenteralnutrition(<24hours)ispossibleandisassociatedwith
beneficialeffects.Wheneverpossible,enteralnutrition(oralortubefeeds)shouldbeinstituted,unlessthere
isaspecificcontraindication.
Forpatientswithadelayedreturnofgutfunction,postoperativeparenteralnutritionisnotindicatedunless
bowelfunctionisnotanticipatedtoreturnformorethan10days.Earlierinterventionmaybeappropriatein
patientswhoareseverelymalnourishedatbaseline,orwhohaveacomplicatedpostoperativecourse.
Theroleforimmunonutritionisunclear.Thusfar,thereisinsufficienthighqualityevidencetosuggestany
specificaminoacidorothersupplementationforsurgicalpatients.
UseofUpToDateissubjecttotheSubscriptionandLicenseAgreement.
http://www.uptodate.com/contents/overviewofperioperativenutritionalsupport?topicKey=SURG%2F2880&elapsedTimeMs=3&source=search_result&s 6/12
7/25/2016
Overviewofperioperativenutritionalsupport
REFERENCES
1.BruunLI,BosaeusI,BergstadI,NygaardK.Prevalenceofmalnutritioninsurgicalpatients:evaluationof
nutritionalsupportanddocumentation.ClinNutr199918:141.
2.Studley,HO.Percentageofweightloss:Abasicindicatorofsurgicalriskinpatientswithchronicpepticulcer.
JAMA1936106:458.
3.McWhirterJP,PenningtonCR.Incidenceandrecognitionofmalnutritioninhospital.BMJ1994308:945.
4.ElwynDH,BryanBrownCW,ShoemakerWC.Nutritionalaspectsofbodywaterdislocationsinpostoperative
anddepletedpatients.AnnSurg1975182:76.
5.KinneyJM,WeissmanC.Formsofmalnutritioninstressedandunstressedpatients.ClinChestMed19867:19.
6.BabineauTJ,BorlaseBC,BlackburnGL.AppliedTotalParentalNutritionintheCriticallyIll.In:IntensiveCare
Medicine,RippeJM,IrwinRS,AlpertJS,FinkMP(Eds),Little,BrownandCo,Boston1991.p.1675.
7.SantosJI.Nutrition,infection,andimmunocompetence.InfectDisClinNorthAm19948:243.
8.MainousMR,DeitchEA.Nutritionandinfection.SurgClinNorthAm199474:659.
9.LawDK,DudrickSJ,AbdouNI.Immunocompetenceofpatientswithproteincaloriemalnutrition.Theeffectsof
nutritionalrepletion.AnnInternMed197379:545.
10.HaydockDA,HillGL.Impairedwoundhealinginsurgicalpatientswithvaryingdegreesofmalnutrition.JPENJ
ParenterEnteralNutr198610:550.
11.AlbinaJE.Nutritionandwoundhealing.JPENJParenterEnteralNutr199418:367.
12.RadyMY,RyanT,StarrNJ.Clinicalcharacteristicsofpreoperativehypoalbuminemiapredictoutcomeof
cardiovascularsurgery.JPENJParenterEnteralNutr199721:81.
13.WhiteJV,GuenterP,JensenG,etal.Consensusstatement:AcademyofNutritionandDieteticsandAmerican
SocietyforParenteralandEnteralNutrition:characteristicsrecommendedfortheidentificationand
documentationofadultmalnutrition(undernutrition).JPENJParenterEnteralNutr201236:275.
14.MuellerC,CompherC,DruyanMD.AmericanSocietyforParenteralandEnteralNutritionASPENclinical
guidelines:nutritionscreening,assessment,andinterventioninadults.JPEN201135:16.
15.KuppingerD,HartlWH,BertokM,etal.Nutritionalscreeningforriskpredictioninpatientsscheduledfor
abdominaloperations.BrJSurg201299:728.
16.DetskyAS,McLaughlinJR,BakerJP,etal.Whatissubjectiveglobalassessmentofnutritionalstatus?JPENJ
ParenterEnteralNutr198711:8.
17.KondrupJ,RasmussenHH,HambergO,etal.Nutritionalriskscreening(NRS2002):anewmethodbasedon
ananalysisofcontrolledclinicaltrials.ClinNutr200322:321.
18.SchiesserM,MllerS,KirchhoffP,etal.Assessmentofanovelscreeningscorefornutritionalriskinpredicting
complicationsingastrointestinalsurgery.ClinNutr200827:565.
19.ReinhardtGF,MyscofskiJW,WilkensDB,etal.Incidenceandmortalityofhypoalbuminemicpatientsin
hospitalizedveterans.JPENJParenterEnteralNutr19804:357.
20.McClaveSA,SniderHL,SpainDA.Preoperativeissuesinclinicalnutrition.Chest1999115:64S.
21.SeresDS.Surrogatenutritionmarkers,malnutrition,andadequacyofnutritionsupport.NutrClinPract2005
20:308.
22.vanStijnMF,KorkicHalilovicI,BakkerMS,etal.Preoperativenutritionstatusandpostoperativeoutcomein
elderlygeneralsurgerypatients:asystematicreview.JPENJParenterEnteralNutr201337:37.
23.KleinS,KinneyJ,JeejeebhoyK,etal.Nutritionsupportinclinicalpractice:reviewofpublisheddataand
recommendationsforfutureresearchdirections.SummaryofaconferencesponsoredbytheNationalInstitutes
ofHealth,AmericanSocietyforParenteralandEnteralNutrition,andAmericanSocietyforClinicalNutrition.Am
JClinNutr199766:683.
24.BragaM,LjungqvistO,SoetersP,etal.ESPENGuidelinesonParenteralNutrition:surgery.ClinNutr2009
28:378.
25.MartindaleRG,McClaveSA,VanekVW,etal.Guidelinesfortheprovisionandassessmentofnutritionsupport
therapyintheadultcriticallyillpatient:SocietyofCriticalCareMedicineandAmericanSocietyforParenteral
andEnteralNutrition:ExecutiveSummary.CritCareMed200937:1757.
26.SoubaWW.Nutritionalsupport.NEnglJMed1997336:41.
27.MooreFA,FelicianoDV,AndrassyRJ,etal.Earlyenteralfeeding,comparedwithparenteral,reduces
postoperativesepticcomplications.Theresultsofametaanalysis.AnnSurg1992216:172.
28.BowerRH,TalaminiMA,SaxHC,etal.Postoperativeenteralvsparenteralnutrition.Arandomizedcontrolled
trial.ArchSurg1986121:1040.
29.KudskKA,CroceMA,FabianTC,etal.Enteralversusparenteralfeeding.Effectsonsepticmorbidityafterblunt
andpenetratingabdominaltrauma.AnnSurg1992215:503.
http://www.uptodate.com/contents/overviewofperioperativenutritionalsupport?topicKey=SURG%2F2880&elapsedTimeMs=3&source=search_result&s 7/12
7/25/2016
Overviewofperioperativenutritionalsupport
30.ShrikhandeSV,ShettyGS,SinghK,IngleS.Isearlyfeedingaftermajorgastrointestinalsurgeryafashionoran
advance?Evidencebasedreviewofliterature.JCancerResTher20095:232.
31.LewisSJ,AndersenHK,ThomasS.Earlyenteralnutritionwithin24hofintestinalsurgeryversuslater
commencementoffeeding:asystematicreviewandmetaanalysis.JGastrointestSurg200913:569.
32.AndersenHK,LewisSJ,ThomasS.Earlyenteralnutritionwithin24hofcolorectalsurgeryversuslater
commencementoffeedingforpostoperativecomplications.CochraneDatabaseSystRev2006:CD004080.
33.ZhuangCL,YeXZ,ZhangCJ,etal.Earlyversustraditionalpostoperativeoralfeedinginpatientsundergoing
electivecolorectalsurgery:ametaanalysisofrandomizedclinicaltrials.DigSurg201330:225.
34.SandstrmR,DrottC,HyltanderA,etal.Theeffectofpostoperativeintravenousfeeding(TPN)onoutcome
followingmajorsurgeryevaluatedinarandomizedstudy.AnnSurg1993217:185.
35.JieB,JiangZM,NolanMT,etal.Impactofpreoperativenutritionalsupportonclinicaloutcomeinabdominal
surgicalpatientsatnutritionalrisk.Nutrition201228:1022.
36.BurdenS,ToddC,HillJ,LalS.Preoperativenutritionsupportinpatientsundergoinggastrointestinalsurgery.
CochraneDatabaseSystRev201211:CD008879.
37.HeylandDK,MontalvoM,MacDonaldS,etal.Totalparenteralnutritioninthesurgicalpatient:ametaanalysis.
CanJSurg200144:102.
38.KoretzRL,LipmanTO,KleinS,AmericanGastroenterologicalAssociation.AGAtechnicalreviewonparenteral
nutrition.Gastroenterology2001121:970.
39.KleinS,KinneyJ,JeejeebhoyK,etal.Nutritionsupportinclinicalpractice:reviewofpublisheddataand
recommendationsforfutureresearchdirections.ClinNutr199716:193.
40.MllerJM,BrennerU,DienstC,PichlmaierH.Preoperativeparenteralfeedinginpatientswithgastrointestinal
carcinoma.Lancet19821:68.
41.MllerJM,KellerHW,BrennerU,etal.Indicationsandeffectsofpreoperativeparenteralnutrition.WorldJSurg
198610:53.
42.BozzettiF,GavazziC,MiceliR,etal.Perioperativetotalparenteralnutritioninmalnourished,gastrointestinal
cancerpatients:arandomized,clinicaltrial.JPENJParenterEnteralNutr200024:7.
43.FanST,LoCM,LaiEC,etal.Perioperativenutritionalsupportinpatientsundergoinghepatectomyfor
hepatocellularcarcinoma.NEnglJMed1994331:1547.
44.Perioperativetotalparenteralnutritioninsurgicalpatients.TheVeteransAffairsTotalParenteralNutrition
CooperativeStudyGroup.NEnglJMed1991325:525.
45.AartsMA,OkrainecA,GlicksmanA,etal.Adoptionofenhancedrecoveryaftersurgery(ERAS)strategiesfor
colorectalsurgeryatacademicteachinghospitalsandimpactontotallengthofhospitalstay.SurgEndosc2012
26:442.
46.RawlinsonA,KangP,EvansJ,KhannaA.Asystematicreviewofenhancedrecoveryprotocolsincolorectal
surgery.AnnRCollSurgEngl201193:583.
47.VaradhanKK,NealKR,DejongCH,etal.Theenhancedrecoveryaftersurgery(ERAS)pathwayforpatients
undergoingmajorelectiveopencolorectalsurgery:ametaanalysisofrandomizedcontrolledtrials.ClinNutr
201029:434.
48.KoretzRL,AvenellA,LipmanTO,etal.Doesenteralnutritionaffectclinicaloutcome?Asystematicreviewof
therandomizedtrials.AmJGastroenterol2007102:412.
49.OslandE,YunusRM,KhanS,MemonMA.Earlyversustraditionalpostoperativefeedinginpatientsundergoing
resectionalgastrointestinalsurgery:ametaanalysis.JPENJParenterEnteralNutr201135:473.
50.DroverJW,DhaliwalR,WeitzelL,etal.Perioperativeuseofargininesupplementeddiets:asystematicreview
oftheevidence.JAmCollSurg2011212:385.
51.ZhengYM,LiF,ZhangMM,WuXT.Glutaminedipeptideforparenteralnutritioninabdominalsurgery:ameta
analysisofrandomizedcontrolledtrials.WorldJGastroenterol200612:7537.
52.MazakiT,IshiiY,MuraiI.Immunoenhancingenteralandparenteralnutritionforgastrointestinalsurgery:a
multipletreatmentsmetaanalysis.AnnSurg2015261:662.
53.MarikPE,ZalogaGP.Immunonutritionincriticallyillpatients:asystematicreviewandanalysisoftheliterature.
IntensiveCareMed200834:1980.
54.MarimuthuK,VaradhanKK,LjungqvistO,LoboDN.Ametaanalysisoftheeffectofcombinationsofimmune
modulatingnutrientsonoutcomeinpatientsundergoingmajoropengastrointestinalsurgery.AnnSurg2012
255:1060.
55.BealeRJ,BrygDJ,BihariDJ.Immunonutritioninthecriticallyill:asystematicreviewofclinicaloutcome.Crit
CareMed199927:2799.
56.HeylandDK,NovakF,DroverJW,etal.Shouldimmunonutritionbecomeroutineincriticallyillpatients?A
systematicreviewoftheevidence.JAMA2001286:944.
57.HegaziRA,HusteadDS,EvansDC.Preoperativestandardoralnutritionsupplementsvsimmunonutrition:
http://www.uptodate.com/contents/overviewofperioperativenutritionalsupport?topicKey=SURG%2F2880&elapsedTimeMs=3&source=search_result&s 8/12
7/25/2016
Overviewofperioperativenutritionalsupport
resultsofasystematicreviewandmetaanalysis.JAmCollSurg2014219:1078.
58.SenkalM,MummeA,EickhoffU,etal.Earlypostoperativeenteralimmunonutrition:clinicaloutcomeandcost
comparisonanalysisinsurgicalpatients.CritCareMed199725:1489.
59.SenkalM,ZumtobelV,BauerKH,etal.Outcomeandcosteffectivenessofperioperativeenteralimmunonutrition
inpatientsundergoingelectiveuppergastrointestinaltractsurgery:aprospectiverandomizedstudy.ArchSurg
1999134:1309.
60.GianottiL,BragaM,NespoliL,etal.Arandomizedcontrolledtrialofpreoperativeoralsupplementationwitha
specializeddietinpatientswithgastrointestinalcancer.Gastroenterology2002122:1763.
61.BragaM,GianottiL,NespoliL,etal.Nutritionalapproachinmalnourishedsurgicalpatients:aprospective
randomizedstudy.ArchSurg2002137:174.
62.Okabayashi,T,Nishimori,I,Sugimoto,T,etal.Thebenefitofthesupplementationofperioperativebranched
chainaminoacidsinpatientswithsurgicalmanagementforhepatocellularcarcinoma:apreliminarystudy.Dig
DisSci2007May18[Epubaheadofprint].
63.MorlionBJ,StehleP,WachtlerP,etal.Totalparenteralnutritionwithglutaminedipeptideaftermajorabdominal
surgery:arandomized,doubleblind,controlledstudy.AnnSurg1998227:302.
64.PowellTuckJ,JamiesonCP,BettanyGE,etal.Adoubleblind,randomised,controlledtrialofglutamine
supplementationinparenteralnutrition.Gut199945:82.
65.FujitaniK,TsujinakaT,FujitaJ,etal.Prospectiverandomizedtrialofpreoperativeenteralimmunonutrition
followedbyelectivetotalgastrectomyforgastriccancer.BrJSurg201299:621.
66.ZieglerTR,MayAK,HebbarG,etal.EfficacyandSafetyofGlutaminesupplementedParenteralNutritionin
SurgicalICUPatients:AnAmericanMulticenterRandomizedControlledTrial.AnnSurg2016263:646.
Topic2880Version12.0
http://www.uptodate.com/contents/overviewofperioperativenutritionalsupport?topicKey=SURG%2F2880&elapsedTimeMs=3&source=search_result&s 9/12
7/25/2016
Overviewofperioperativenutritionalsupport
GRAPHICS
Nomogramfordeterminingbodymassindex
Thenomogramisusedbyplacingarulerorotherstraightedge
betweenthebodyweightinkilogramsorpounds(thelefthandline)
andtheheightincentimetersorinches(therighthandline).Thebody
massindexisreadfromthemiddleofthescale,inmetricunits.
Graphic65305Version1.0
http://www.uptodate.com/contents/overviewofperioperativenutritionalsupport?topicKey=SURG%2F2880&elapsedTimeMs=3&source=search_result& 10/12
7/25/2016
Overviewofperioperativenutritionalsupport
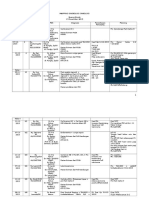
Physicalsignsofselectednutritionaldeficiencystates
Hair
Skin
Signs
Deficiencies
Alopecia
Proteinenergymalnutrition
Brittle
Biotin,Proteinenergymalnutrition
Colorchange
Proteinenergymalnutrition
Dryness
VitaminsEandA
Easypluckability
Proteinenergymalnutrition
Acneiformlesions
VitaminA
Follicularkeratosis
VitaminA
Xerosis(dryskin)
VitaminA
Ecchymosis
VitaminCorK
Intradermalpetechia
VitaminCorK
Erythema(especiallywhereexposedto
Niacin
sunlight)
Hyperpigmentation
Niacin
Seborrheicdermatitis(nose,eyebrows,
VitaminB2,VitaminB6,Niacin
eyes)
Eyes
Mouth
Extremities
Scrotaldermatitis
Niacin,VitaminB2,VitaminB6
Angularpalpebritis
VitaminB2
Cornealrevascularization
VitaminB2
Bitot'sspots
VitaminA
Conjunctivalxerosis,keratomalacia
VitaminA
Angularstomatitis
VitaminB12,VitaminB2,VitaminB6
Atrophicpapillae
Niacin
Bleedinggums
VitaminC
Cheilosis
VitaminB2,VitaminB6
Glossitis
Niacin,folate,vitaminB12,VitaminB2,
VitaminB6
Magentatongue
VitaminB2
Genuvalgumorvarum,metaphyseal
VitaminD
widening
Lossofdeeptendonreflexesofthelower
VitaminsB1andB12
extremities
VitaminB1:thiamineVitaminB2:riboflavinVitaminB3:niacinVitaminB6:pyridoxineVitaminB12:
cyanocobalamin.
Adaptedfrom:BernardMA,JacobsDO,RombeauJL.NutritionandMetabolicSupportofHospitalizedPatients.
WBSaunders,Philadelphia1986.
Graphic78426Version2.0
http://www.uptodate.com/contents/overviewofperioperativenutritionalsupport?topicKey=SURG%2F2880&elapsedTimeMs=3&source=search_result& 11/12
7/25/2016
Overviewofperioperativenutritionalsupport
ContributorDisclosures
KathleenMFairfield,MD,DrPHNothingtodisclose.RezaAskari,MD,FACSNothingtodisclose.TimothyO
Lipman,MDNothingtodisclose.HilarySanfey,MDNothingtodisclose.KathrynACollins,MD,PhD,FACS
Nothingtodisclose.
Contributordisclosuresarereviewedforconflictsofinterestbytheeditorialgroup.Whenfound,theseareaddressed
byvettingthroughamultilevelreviewprocess,andthroughrequirementsforreferencestobeprovidedtosupportthe
content.AppropriatelyreferencedcontentisrequiredofallauthorsandmustconformtoUpToDatestandardsof
evidence.
Conflictofinterestpolicy
http://www.uptodate.com/contents/overviewofperioperativenutritionalsupport?topicKey=SURG%2F2880&elapsedTimeMs=3&source=search_result& 12/12
Anda mungkin juga menyukai
- Mind and Emotions: A Universal Treatment For Emotional DisordersDokumen9 halamanMind and Emotions: A Universal Treatment For Emotional DisordersNew Harbinger Publications100% (7)
- CSP and CRSP To Cmiosh Ed New12Dokumen4 halamanCSP and CRSP To Cmiosh Ed New12mokshaq7Belum ada peringkat
- Lesson Plan PEDokumen24 halamanLesson Plan PEJulius Mey Ballecer100% (3)
- Emerging and Re-Emerging Disease in NepalDokumen25 halamanEmerging and Re-Emerging Disease in NepalBinayaBelum ada peringkat
- Form MSDS BambangDokumen2 halamanForm MSDS BambangAzka Nuriel ShiddiqBelum ada peringkat
- TPN Ensuring Safe and Appropriate Use ASHP 2017Dokumen54 halamanTPN Ensuring Safe and Appropriate Use ASHP 2017Michael FreudigerBelum ada peringkat
- 15 Healing Miracles EX735 SCENAR Book StoriesDokumen11 halaman15 Healing Miracles EX735 SCENAR Book StoriesBacean Aurel Ioan100% (5)
- Professional Quality of Life ScaleDokumen2 halamanProfessional Quality of Life ScaleMihaela LauraBelum ada peringkat
- Management of Anastomotic Complications of Colorectal SurgeryDokumen13 halamanManagement of Anastomotic Complications of Colorectal Surgerydadupipa100% (1)
- 4th Quarter Exam Grade 9Dokumen2 halaman4th Quarter Exam Grade 9Noemi Balbido100% (2)
- Pemberian Obat VasconDokumen46 halamanPemberian Obat Vascondadupipa80% (5)
- Nutricion QX Articulo AvancesDokumen56 halamanNutricion QX Articulo AvancesJuan Manuel PadillaBelum ada peringkat
- JCSM 8 437Dokumen10 halamanJCSM 8 437anggi larasatiBelum ada peringkat
- 337.1 s2.0 S0002916522046718 MainDokumen10 halaman337.1 s2.0 S0002916522046718 MaintereBelum ada peringkat
- NIH Public Access: Author ManuscriptDokumen13 halamanNIH Public Access: Author ManuscriptTera LeverenzBelum ada peringkat
- Gastrico Vs TranspiloricaDokumen6 halamanGastrico Vs TranspiloricaMagali FloresBelum ada peringkat
- 231 445 1 SMDokumen4 halaman231 445 1 SMAnonymous zH3OueBelum ada peringkat
- Fast Hug FaithDokumen4 halamanFast Hug FaithHenrique Yuji Watanabe SilvaBelum ada peringkat
- 3 Staging of CancerDokumen7 halaman3 Staging of CancerEdikoup Lakip SediyantoBelum ada peringkat
- TNT - Terapia de Nutricion TotalDokumen6 halamanTNT - Terapia de Nutricion TotalJuana Rosa Martinez BonillaBelum ada peringkat
- Atkins Writ159a Assignment3Dokumen5 halamanAtkins Writ159a Assignment3api-553023922Belum ada peringkat
- Fruit and Vegetable Intakes Are Associated With Lower Risk of Breast Fibroadenomas in Chinese WomenDokumen8 halamanFruit and Vegetable Intakes Are Associated With Lower Risk of Breast Fibroadenomas in Chinese WomenAzedh Az-ZahraBelum ada peringkat
- Meal Frequency and Timing Are Associated With Changes in Body Mass Index in Adventist Health Study 2Dokumen7 halamanMeal Frequency and Timing Are Associated With Changes in Body Mass Index in Adventist Health Study 2Cristi CapetisBelum ada peringkat
- Malnutrition in Acute Care Patients: A Narrative Review: Cathy Kubrak, Louise JensenDokumen19 halamanMalnutrition in Acute Care Patients: A Narrative Review: Cathy Kubrak, Louise JensenchanchandilBelum ada peringkat
- Jurnal JantungDokumen11 halamanJurnal JantungDiah Ayu AdiatiBelum ada peringkat
- Enhanced Recovery After Cesarean DeliveryDokumen20 halamanEnhanced Recovery After Cesarean DeliveryHum FahmiBelum ada peringkat
- A Practical Approach To Nutritional Screening and Assessment in CirrhosisDokumen14 halamanA Practical Approach To Nutritional Screening and Assessment in Cirrhosispamela Urrutia100% (1)
- Enteral Feedings in Hospitalized Patients: Early Versus Delayed Enteral NutritionDokumen7 halamanEnteral Feedings in Hospitalized Patients: Early Versus Delayed Enteral NutritionokipashaBelum ada peringkat
- Nutritional Assessment of Children With Acute Lymphoblastic LeukemiaDokumen9 halamanNutritional Assessment of Children With Acute Lymphoblastic LeukemiaGritoBelum ada peringkat
- ASPEN - Suplemental Parenteral Nutrition - Review of The Literature and Current Nutriton GuidelinesDokumen11 halamanASPEN - Suplemental Parenteral Nutrition - Review of The Literature and Current Nutriton GuidelinesRoberto Cárdenas GarcíaBelum ada peringkat
- NIH Public Access: Author ManuscriptDokumen11 halamanNIH Public Access: Author ManuscriptrizkaBelum ada peringkat
- 2016 June Case StudyDokumen8 halaman2016 June Case StudyMarius Clifford BilledoBelum ada peringkat
- 211 FullDokumen17 halaman211 Fullalfarisi_auliaBelum ada peringkat
- Full Nutrition or Not?Dokumen6 halamanFull Nutrition or Not?Alexandra RodriguesBelum ada peringkat
- Determinants of Malnutrition and Post-Operative Complications in Hospitalized Surgical PatientsDokumen11 halamanDeterminants of Malnutrition and Post-Operative Complications in Hospitalized Surgical PatientsZurezki Yuana YafieBelum ada peringkat
- Lit Reveiw PresentationDokumen18 halamanLit Reveiw Presentationapi-241865788Belum ada peringkat
- Nutritional Support 2004Dokumen20 halamanNutritional Support 2004Amany SalamaBelum ada peringkat
- Nutritional Management of Medical Inpatients: Clinical MedicineDokumen11 halamanNutritional Management of Medical Inpatients: Clinical MedicineLiana LianaBelum ada peringkat
- 10 1001@jamaoncol 2018 1212Dokumen10 halaman10 1001@jamaoncol 2018 1212Gabriel MateusBelum ada peringkat
- Refrat PyelonefritisDokumen12 halamanRefrat PyelonefritisArmando HalauwetBelum ada peringkat
- The ASMBS Textbook of Bariatric Surgery: Volume 2: Integrated HealthDari EverandThe ASMBS Textbook of Bariatric Surgery: Volume 2: Integrated HealthBelum ada peringkat
- 5 Recent Trials in Stress Ulcer ProphylaxisDokumen6 halaman5 Recent Trials in Stress Ulcer ProphylaxisCharan Teja Reddy AvulaBelum ada peringkat
- 15 2820471009 - FTPDokumen7 halaman15 2820471009 - FTPSamuel Kyei-BoatengBelum ada peringkat
- 10 1093@humrep@dex276Dokumen7 halaman10 1093@humrep@dex276Ricky AmeBelum ada peringkat
- International Journal of Gerontology: Thiago J. Avelino-Silva, Omar JaluulDokumen6 halamanInternational Journal of Gerontology: Thiago J. Avelino-Silva, Omar JaluulKaye Antonette AntioquiaBelum ada peringkat
- Burst Abdomen A Post-Operative MorbidityDokumen4 halamanBurst Abdomen A Post-Operative MorbidityDian AdiBelum ada peringkat
- Advances in Surgical NutritionDokumen10 halamanAdvances in Surgical NutritionAndyBelum ada peringkat
- Nutritionalissuesin Cysticfibrosis: Missale Solomon,, Molly Bozic,, Maria R. MascarenhasDokumen11 halamanNutritionalissuesin Cysticfibrosis: Missale Solomon,, Molly Bozic,, Maria R. MascarenhasDea PertiwiBelum ada peringkat
- Vaugh Alimentacio nPancreatitisAguda AnnInternMed 2017-2Dokumen15 halamanVaugh Alimentacio nPancreatitisAguda AnnInternMed 2017-2Paula RodriguezBelum ada peringkat
- Chemotherapy-Induced Nausea and Vomiting in Asian Women With Breast Cancer Receiving Anthracycline-Based Adjuvant ChemotherapyDokumen6 halamanChemotherapy-Induced Nausea and Vomiting in Asian Women With Breast Cancer Receiving Anthracycline-Based Adjuvant ChemotherapyMirza RisqaBelum ada peringkat
- Are We Jumping The Gun With Pharmaconutrition (Immunonutrition) in Gastrointestinal Onoclogical Surgery?Dokumen3 halamanAre We Jumping The Gun With Pharmaconutrition (Immunonutrition) in Gastrointestinal Onoclogical Surgery?HebaHanyOmarBelum ada peringkat
- ALL GizburDokumen3 halamanALL GizburPratita Jati PermatasariBelum ada peringkat
- Iefing The Value of Quality Malnutrition CareDokumen5 halamanIefing The Value of Quality Malnutrition CareVelasquez LuisBelum ada peringkat
- Peptic Ulcer Case Study 1Dokumen9 halamanPeptic Ulcer Case Study 1Alejandro Daniel Landa MoralesBelum ada peringkat
- Parturition Events and Risk of Urinary Incontinence in Later LifeDokumen16 halamanParturition Events and Risk of Urinary Incontinence in Later LifeMutia LailaniBelum ada peringkat
- Update On Cancer CachexiaDokumen4 halamanUpdate On Cancer CachexiaIyanBelum ada peringkat
- Endoscopic Intervention and Cholecystectomy in Pregnant Women With Acute Biliary Pancreatitis Decreases Early ReadmissionsDokumen19 halamanEndoscopic Intervention and Cholecystectomy in Pregnant Women With Acute Biliary Pancreatitis Decreases Early ReadmissionsCarlos Altez FernandezBelum ada peringkat
- The ASMBS Textbook of Bariatric Surgery: Volume 1: Bariatric SurgeryDari EverandThe ASMBS Textbook of Bariatric Surgery: Volume 1: Bariatric SurgeryBelum ada peringkat
- A Prospective Randomized Controlled Trial On The Value of Prophylactic Supplementation Pral NutritionDokumen7 halamanA Prospective Randomized Controlled Trial On The Value of Prophylactic Supplementation Pral NutritionOkky IrawanBelum ada peringkat
- Mal Nutri SiDokumen7 halamanMal Nutri SiNurul Kamilah SadliBelum ada peringkat
- FolatosDokumen6 halamanFolatosBlackbeetleBelum ada peringkat
- J Appet 2015 08 039Dokumen23 halamanJ Appet 2015 08 039Y NguyenBelum ada peringkat
- Current Practice in Nutritional Support and Its Association With Mortality in Septic Patients-Results From A National, Prospective, Multicenter StudyDokumen6 halamanCurrent Practice in Nutritional Support and Its Association With Mortality in Septic Patients-Results From A National, Prospective, Multicenter StudyLuis Miguel Díaz VegaBelum ada peringkat
- Assessment of Dietary Intakes of Filipino-Americans: Implications For Food Frequency Questionnaire DesignDokumen10 halamanAssessment of Dietary Intakes of Filipino-Americans: Implications For Food Frequency Questionnaire DesignClaude Geoffrey L. EscanillaBelum ada peringkat
- Colon Cancer ResearchDokumen4 halamanColon Cancer Researchapi-296922357Belum ada peringkat
- JOURNAL Where Is The Nurse in Nutritional CareDokumen5 halamanJOURNAL Where Is The Nurse in Nutritional Carevia macarioBelum ada peringkat
- Imc y FertilidadDokumen9 halamanImc y FertilidadRichard PrascaBelum ada peringkat
- High Folate Intake Is Associated With Lower Breast Cancer Incidence in Postmenopausal Women in The Malmö Diet and Cancer Cohort1,2,3Dokumen13 halamanHigh Folate Intake Is Associated With Lower Breast Cancer Incidence in Postmenopausal Women in The Malmö Diet and Cancer Cohort1,2,3Airi IsDjarieBelum ada peringkat
- J Parenter Enteral Nutr - 2022 - Gressies - Nutrition Issues in The General Medical Ward Patient From General Screening ToDokumen8 halamanJ Parenter Enteral Nutr - 2022 - Gressies - Nutrition Issues in The General Medical Ward Patient From General Screening ToRaiden EiBelum ada peringkat
- Nutrients 08 00342 With CoverDokumen6 halamanNutrients 08 00342 With Coverredactor 1Belum ada peringkat
- Ncbi - Nlm.nih - Gov-Post-Op Urinary RetentionDokumen9 halamanNcbi - Nlm.nih - Gov-Post-Op Urinary RetentiondadupipaBelum ada peringkat
- Tamoxifen Comittee OpinionDokumen4 halamanTamoxifen Comittee OpiniondadupipaBelum ada peringkat
- HB-0353-004 HB Qa Dna Ffpe 0220 WWDokumen28 halamanHB-0353-004 HB Qa Dna Ffpe 0220 WWdadupipaBelum ada peringkat
- Cardiac TumorsDokumen37 halamanCardiac TumorsdadupipaBelum ada peringkat
- Pamflet - Cervical CancerDokumen8 halamanPamflet - Cervical CancerdadupipaBelum ada peringkat
- Wound Infection Following Repair of Abdominal Wall HerniaDokumen13 halamanWound Infection Following Repair of Abdominal Wall HerniadadupipaBelum ada peringkat
- Mapping Ginekologi Onkologi Ruang Merak 13 Desember 2015Dokumen11 halamanMapping Ginekologi Onkologi Ruang Merak 13 Desember 2015dadupipaBelum ada peringkat
- Overview of Management of Mechanical Small Bowel Obstruction in AdultsDokumen16 halamanOverview of Management of Mechanical Small Bowel Obstruction in AdultsdadupipaBelum ada peringkat
- Maternal Medical Complications: NeurologyDokumen2 halamanMaternal Medical Complications: NeurologydadupipaBelum ada peringkat
- Weekly PH2 24-30 Juni 2013Dokumen1 halamanWeekly PH2 24-30 Juni 2013dadupipaBelum ada peringkat
- Obstetric Emergency and Anesthetic ManagementDokumen11 halamanObstetric Emergency and Anesthetic ManagementmichaelBelum ada peringkat
- Psychosocial AssessmentDokumen10 halamanPsychosocial AssessmentAlthea TuguinayBelum ada peringkat
- Model of Heavy Work InvestmentDokumen12 halamanModel of Heavy Work InvestmentaBelum ada peringkat
- Cambridge 17 Listening Test 1Dokumen6 halamanCambridge 17 Listening Test 1Ngọc Hân Trần0% (1)
- Staphylococcus Aure SalmonellaDokumen6 halamanStaphylococcus Aure Salmonellaمحمد السعديBelum ada peringkat
- Rle For Wednesday and Thursday: Time ActivityDokumen2 halamanRle For Wednesday and Thursday: Time ActivityJay VillasotoBelum ada peringkat
- Physical EducationDokumen8 halamanPhysical EducationLESLIE MARTINEZBelum ada peringkat
- Vince Sisneros Project 2Dokumen8 halamanVince Sisneros Project 2api-279313843Belum ada peringkat
- 1-2 - Final Activity-Covid19 Updates and Pva - HernandezDokumen3 halaman1-2 - Final Activity-Covid19 Updates and Pva - HernandezJosephine FranciscoBelum ada peringkat
- Breastfeeding and Travel: Be Culturally SensitiveDokumen3 halamanBreastfeeding and Travel: Be Culturally Sensitivesina bayat shahbaziBelum ada peringkat
- Pananaliksik References'Dokumen14 halamanPananaliksik References'Perf LasquiteBelum ada peringkat
- Personality and Social Psychology: Cyberbullying Status and Mental Health in Norwegian AdolescentsDokumen7 halamanPersonality and Social Psychology: Cyberbullying Status and Mental Health in Norwegian AdolescentsElena ElenaBelum ada peringkat
- Issue 3 Michael Deren Man With 2 Hearts ArticleDokumen1 halamanIssue 3 Michael Deren Man With 2 Hearts Articleapi-400507461Belum ada peringkat
- Calculation of DosesDokumen31 halamanCalculation of DosesCresencia Fidela TominesBelum ada peringkat
- Oral Diagnosis: The Physical ExamDokumen40 halamanOral Diagnosis: The Physical ExamDivyanshBansalBelum ada peringkat
- Endometrial CarcinomaDokumen6 halamanEndometrial CarcinomaĶHwola ƏľsHokryBelum ada peringkat
- Illegal Drugs FlyersDokumen2 halamanIllegal Drugs FlyersPCR OPERATIONBelum ada peringkat
- The Power of Protein - How Much Should You Really Be Eating? - Fitbit BlogDokumen12 halamanThe Power of Protein - How Much Should You Really Be Eating? - Fitbit BlogDele Jnr EriboBelum ada peringkat
- PDF 6Dokumen5 halamanPDF 6k.asif911Belum ada peringkat
- CHN PPT PrelimDokumen101 halamanCHN PPT PrelimgmatbdotsBelum ada peringkat
- Study About Herbal MedicineDokumen47 halamanStudy About Herbal MedicineEli EstrellaBelum ada peringkat
- Cold InjuryDokumen34 halamanCold Injurydassdeepak69100% (1)