Studies in Rat Liver Perfusion For Optimal Harvest of Hepatocytes
Diunggah oleh
Anonymous wbRUEuDJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Studies in Rat Liver Perfusion For Optimal Harvest of Hepatocytes
Diunggah oleh
Anonymous wbRUEuDHak Cipta:
Format Tersedia
Studies in Rat Liver Ferfusion for Optimal Harvest of Hepatocytes
By J. Aiken, L. Cima, B. Schloo, D. Mooney, L. Johnson, R. Langer, and J.P. Vacanti
Boston, Massachusetts
9 Pediatric liver transplantation is successful but donor
scarcity is a major limitation. W e are studying hepatocyte
transplantation as an alternative to provide functional
hepatic replacement. This report details the study of rat
liver perfusion for optimal harvest of hepatocytes and cell
implantation. W e performed 128 rat liver perfusions using
a technique modified from the two-step enzymatic perfusion described by Seglen. W e examined variations in the
perfusion technique including: in situ versus isolated organ
perfusion, rate, time, antegrade versus retrograde, pulsatile versus continuous flow, temperature, collagenase type,
and variables of buffer composition. W e have found optimal
cell yield and viability under the following conditions: in situ
perfusion, continuous flow at 25 cc/min, retrograde perfusion via the inferior vena cava, w a t e r bath temperature
38~ B o e ~ n g e r - M a n n h e i m collagenase using a nonoxygenated HEPES based perfusion buffer, pH 7.4, for the
initial perfusion and the same buffer with 4.8 mmol/L CaCI 2
for the collagenase perfusion. These conditions consistently generate cell harvests of 500 to 700 10 e cells/g of
liver tissue with cell viability between 8 5 % and 95%.
9 1990 by W.B. Saunders Company.
INDEX WORDS: Liver perfusion; hepatocyte transplantation.
IVER TRANSPLANTATION has become an
L increasingly successful treatment for patients
with generalized liver failure or isolated but critical
hepatic defects. However, the problems of donor organ
scarcity, expense, and complex surgery and postoperative care prevent whole organ transplantation from
reaching the majority of patients with liver failure)
We studied hepatocyte transplantation as an alternative to provide functional hepatic replacement. The
first step in the schema of selective transplantation is to
obtain good primary hepatoeyte cell cultures. In an
effort to optimize rat liver perfusion for cell harvest
and implantation, we performed 128 rat liver perfusions using modifications of the two-step collagenase
perfusion technique introduced by Berry and Friend 2
and adapted by Seglen. 3 The following variables were
investigated: surgical techniques, components of the
perfusion system, rate of flow, time of perfusion,
collagenase type, in situ versus isolated organ perfusion, method of liver dissociation after perfusion, antegrade versus retrograde perfusion, pulsatile versus
continuous flow, temperature, and variables of buffer
composition including base component, oxygenation,
and pH. This report details our studies of rat liver
perfusion for optimal cell isolation and implantation.
MATERIALS AND METHODS
Animals
Experiments were performed on Sprague-Dawley and Fisher 344
rats (Charles River Breeding Laboratories, Wilmington, MA). The
animals were 8 to 16 weeks of age and weighed 125 to 350 g. The
animals were maintained in 12-hour dark/light cycles and had
access to rat chow (Formula b 5008; Purina, St Louis, MO) and tap
water ad libitum.
Collagenase
Collagenase was obtained from Worthington Biochemical (Freehold, N J) and Bod~nger-Mannheim (Indianapolis, IN) and stored
in perfusion buffer (100 mg/mL) at -20~ Sample lots were tested
at predetermined concentrations prepared from the stock solution
immediately before perfusions.
Buffers
All buffers were prepared fresh using sterile technique and filter
sterilized using a Corning 22 /~ filter (Corning NY). Before the
perfusion, the buffers were warmed for 30 to 60 minutes in a water
bath at 38 to 39~ During the perfusion the buffers were contained
in separate glass reservoirs which were aseptically vented to the
atmosphere. Several buffers were studied including a Krebs ringer
buffer (KRB) and the buffers originally used by Seglen. 3 The KRB
buffer consists of the following components per liter of solution:
NaCI 9 g, KC10.42 g, glucose 0.99 g, sodium bicarbonate 2.1 g, and
HEPES 10 mL of a 2 mol/L stock solution.
eerfusion System
The perfusion system consisted of the pump, autcclavable silastic
tubing (Cole Parmer, Chicago, IL), a water bath, and an air trap. A
Cole Parmer Masterflex pump (Cole Parmer, Chicago, IL) was used
with continuous flow at 25 to 30 mL/min. In experiments examining
the effects of oxygenation or the use of KRB (bicarbonate base)
buffer, an in line lung oxygenator was included with either a 95%
02/5% COz or air 5% CO2 gas mixture.
From the Department of Surgery, The Children's Hospital
Boston, MA.
Funded by grantsfrom Neomorphics, Inc, the Holly Ann Soulard
Research Fund of The Children's Hospital Surgical Foundation,
and the Claude E. Welch Surgical Fellowship, Massachusetts
General Hospital, Boston, MA.
Presented at the 20th Annual Meeting of the American Pediatric
Surgical Association, Baltimore, Maryland, May 28-31, 1989.
Address reprint requests to J.P. Vacanti, Department of Surgery,
The Children's Hospital, 300 Longwood Ave, Boston, MA 02115.
~ 1990 by W.B. Saunders Company.
0022-3468/90/2601-0026503.00/0
Each animal was anesthetized using Metofane (Pitman-Moore
Inc, Washington Crossing, N J) inhalation and given 500 U of
heparin (1,000 U/mL; Elkins-Sinn Inc, Cherry Hill, N J) by intraperitoneal injection. The abdomen was prepped with betadine and
entered through a midline incision. A 16-gauge angiocath (Critikon
140
Journal of Pediatric Surgery, Vol 25, No 1 (January), 1990: pp 140-145
Liver Perfusion Techniques
HEPATOCYTE HARVEST IN LIVER PERFUSlON
Inc, Tampa, FL) was inserted into the inferior vena cava and secured
using silk ties. The perfusate tubing was connected to the cannula
and flowwas initiated at a low rate. The portal vein was cut to allow
efflux and the rate of flow was then increased to 25 mL/min. The
diaphragm was incised and the inferior vena cava damped in the
thorax. The first step of the perfusion was carried out for 5 to 6
minutes with the calcium free buffer, and then via a stopcock, a
switch was made to the collagenaseperfusionwith no interruption of
flow and carried out for 5 to 10 minutes. The endpoint of the
collagenase perfusionwas determined by subjectiveevaluationof the
liverduring the perfusionand varied slightly with the age and weight
of the animal. During the collagenase perfusion the liver was
dissected free, enabling its removal at the completion of the perfusion to a sterile petri dish for dissociation into the primary cell
culture.
Cell Isolation
The liver dissociation was performed in a tissue culture hood with
the liver on ice. A surgical rake was used to peel back the liver
capsule and with gentle shaking the cells were dispersed into
William's E media (GIBCO, Grand Island, NY). The cell suspension was filtered through a 300/~m Nytex mesh bolting cloth (Tetko
Inc, Elmsford, NY) and allowed to settle by gravity. An initial cell
count and viability was performed. A Percoll solution (13% by
volume of 10x phosphate buffered saline [PBS] and 87% sterile
Percoll) (Sigma, St. Louis, MO) was mixed with the cell pellet in
1:1.5 ratio of cells to Percoll solution. 5 The mixture was centrifuged
at 4~ at 1,000 x g for 5 minutes and the dead cells were aspirated
off the top of the gradient. The cell pellet was resuspended in
William's E media (40 mL) and then washed three times in sterile
PBS allowing the cells to pellet by gravity for 15 minutes after each
wash. The cell suspension was counted in a Bflfkerchamber (hemocytometer) and cell viability determined by trypan blue staining.
RESULTS
Our initial series of liver perfusions examined the
surgical technique involved and the components of the
system. Most current techniques for isolation of hepatocytes by enzyme perfusion are based on the two-step
procedure of Seglen and we have also incorporated
adaptations learned from visiting laboratories experienced in liver perfusion (L. Reid, J. McGowan, J.
Jauregui, N. Bucher, and R. Tompkins). O f the first
18 perfusions, 9 failed due to a technical error with the
most common surgical problem, that of perforation of
the back wall of the portal vein during antegrade
cannulation. O f greater than 100 subsequent perfusions less than 5% have been technical failures.
The perfusion system consists of a pump, autoclavable silastic tubing, a water bath, and an air trap (Fig
1). A series of 12 perfusions was performed to evaluate
the need for oxygenation of the perfusate buffers. A
lung oxygenator was placed in the system and the
buffer and collagenase solutions were gassed with
either a 95% air/5% CO2 or 95% O2/CO2 mix for 30 to
60 minutes before the perfusion. These experiments
demonstrated no significant benefit in cell yield or
viability with oxygenation of the buffers and therefore
to simplify the system and decrease the potential for
141
technical problems (tubing breaks, infection from
tanks) the lung oxygenator was excluded from our
system. We found the air trap, positioned to eliminate
air bubbles in the perfusion buffers, to be a critical
component of the system. Essentially all experiments
in which air bubbles were not eliminated were associated with poor cell yield and viability and represented six of the nine perfusions categorized as technical failures during the initial series of 20 perfusions.
A series of 28 perfusions was performed to examine
in situ versus isolated organ perfusion. Under in situ
conditions, the liver remains in the abdominal cavity,
undisturbed, through both steps of the perfusion and
only following completion of the collagenase perfusion
is surgically removed for dissociation into the primary
cell culture. There is no recirculation of the collagenase perfusate. Isolated organ perfusion differs with
surgical dissection of the liver during the first step
(buffer) of the perfusion enabling removal Of the liver
to a liver platform ( M R A Corp, Clearwater, FL), for
the second step (collagenase) perfusion and thereby
collection and recirculation of the collagenase buffer.
The dissection of the liver and removal to the liver
platform can cause temporary interruption in buffer
flow and also the recirculation of the collagenase
buffer may increase the possibility of infection or
introduction of endotoxin. Although others use isolated
organ perfusion with good success, in our hands we
found in situ perfusion to be superior for cell yield and
viability.
Buffer composition was examined in a series of 20
perfusions using varying salt concentrations and pH
adjustment. We found optimal results using Seglen's
H E P E S base initial buffer, pH 7.4, and the same
buffer with 4.8 m m o l / L CaC12 for the second step
(collagenase) of the perfusion. This buffer contains the
following components per liter of final solution: 8.3 g
NaCI, 500 mg KC1, 2.4 g H E P E S , 5.5 m L N a O H 1
mol/L, and 10 mg soybean trypsin inhibitor (Worthington Biochemical).
Our experiments demonstrated differences in collagenase to be the single most critical variable to optimization of the perfusions. A series of 56 perfusions was
performed to assess variations in collagenase lot, type,
and concentration. We examined Worthington Biochemical types II and IV collagenase and BoerhingerMannheim collagenase type with high collagenase and
low trypsin activity (Fig 2). Worthington collagenase
types are graded according to degree of purification
from contaminating proteases; type I is the least pure
and type V I I I is the most pure; however, because some
proteases are necessary for tissue digestion, liver dissociation cannot be effected using the type V I I I collagenase. 6 Collagenase samples were tested at varying
142
AIKEN ET AL
,.L
38=C
bath
Air trap
8topoocl
Pump
Buffer
Collagenase
solution
PERFUSION
SCHEME
Anesthesia
Into IVC
Fig 1. Diagram of liver perfusion system. Note pump, w a ter bath, air trap, in situ retrograde technique via the inferior
vena csva w i t h efflux via t h e
portal vein.
9P o r t a l V.
drainage
concentrations from 40 I U / m L to 90 I U / m L
(Worthington enzyme) and from .40 mg/mL to .80
mg/mL (Boerhinger enzymei. Small variations within
these test ranges were at times associated with marked
differences in total cell yield and viability. Optimal
concentrations yielded cell harvests in the range of 500
to 700 l0 s cells/g of liver tissue with 85% to 95%
viability, whereas suboptimal conditions could reduce
total cell yield 1,O00-fold and viability to less than
50%.
Length of perfusion and temperature were examined in a series of 22 perfusions. The first step (buffer)
of the perfusion clears blood and calcium from the liver
and we found 5 to 6 minutes to be adequate. The
second step (collagenase) effects architectural break
up and must be long enough to effect good dissociation
of the liver but not excessive leading to damage to the
cells from overexposure to enzyme. We found 5 to 10
minutes to be optimal for the second step with adjustments depending on collagenase variability and the age
and weight of the animal. The optimal temperature of
the water bath was 38 to 39~ corresponding to an
outlet temperature at the cannula of 35 to 36~ (Fig
3). The endpoint of the perfusion is determined subjectively during the perfusion based on liver appearance.
In summary, we performed 128 rat liver perfusions
and found optimal cell yield and viability under the
following conditions: in situ organ perfusions, continu100
100
Z~
80
Zl
[]
80
60
60
m
.o
40
lot 1
lot 2
lot 3
--~r
lot4
0
[]
43
M
"; 40
lot H
lot D-58
lot D,24
o 20
20
S -/
.......O .....
-'-'~-'-
3O
O
,
40
50
60
collagenase activity (U/ml)
70
80
0.4
B
0.5
collagenasa concentration (mg/ml)
0.6
Fig 2. (A) Graph of test samples of W o r t h i n g t o n collagenase. Four lots w e r e tested at various concentrations demonstrating
significant differences in cell viability. (B) Graph of performance of Boerhinger-Mannheim collagenase t e s t samples. Three lots w e r e
tested at various concentrations demonstrating significant differences in cell viability.
HEPATOCYTE HARVEST IN LIVER PERFUSION
143
60
50
40
first wash (bath temp. /exit temp.)
.I. ~ 41 (35) C
/ ~
~' 30
"----:==
> 20
Y.
/,,,~1% ~
~
ue lo
o
40
|
60
50
r
Fig 3.
----
44 (38) C
secondwash (bath temp. / exit temp.)
~
41 (35) C
~\
~
44 (38) C
e .
70
80
90
activity (U/ml)
.
100
Graph demonstrating effect of w a t e r bath and exit
(cannula) temperature during liver perfusion on cell viability.
ous flow at 25 mL/min, retrograde perfusions via the
inferior vena cava, water bath temperature 38 to 39~
Boerhinger-Mannheinm collagenase using a nonoxygenated HEPES-based buffer, pH 7.4 for the first step
of the perfusion (5 to 6 minutes), and the same buffer,
with 4.8 mmol/L CaC12 for the collagenase step of the
perfusion (5 to 10 minutes). Collagenase lot and
concentration must be determined in advance by sample testing. These conditions consistently generate cell
harvests of 500 to 700 x 105 cells/g of liver tissue with
cell viability 85% to 95%.
DISCUSSION
The selective transplantation of hepatocytes to provide functional hepatic replacement for generalized
liver failure or isolated hepatic defects has several
potential advantages over whole organ transplantation. 7 As many as 40% of infants with liver failure die
awaiting transplantation and many others become so
critically ill that success of transplantation is diminished. 8 Theoretically, hepatocyte transplantation
would enable a small piece of liver tissue to provide
enough cells for use by multiple recipients, thereby
alleviating the major problem of donor organ scarcity.
Furthermore, there would exist the possibility for using
living related donors. Because a significant amount of
the antigen load associated with liver transplantation
originates from passenger cells, the many serious problems associated with rejection and requirement for
immunosuppression may be decreased, thus decreasing
the incidence of infectious complications.9
Primary hepatocyte cell cultures have been obtained
by various methods including: mechanical methods
such as, forcing the tissue through stainless steel
screens or cheesecloth; chelation primarily using
citrate or EDTA; enzymatic dispersion with collagenase and combinations of these techniques. 1~ Liver
perfusion techniques elaborated by others for obtaining the primary hepatocyte cell culture have incorporated in line oxygenation, alkalinization of the collage-
nase buffer, antegrade perfusion through the portal
vein, and isolated organ perfusion. Our studies indicate
that the system can be simplified and thus more
reliable. Our system is modified from that described by
Jauregui et al. 13 We have found that the variability of
the collagenase is a major determinant of success of
failure in rat liver perfusions. This is consistent with
reports from other investigators. We found no benefit
from oxygenation of the buffers and this is in agreement with studies demonstrating the ability of the
perfused liver to withstand periods of anoxia up to 30
minutes without toxic effects./4 We had best results
using retrograde in situ perfusions via the inferior vena
cava. The retrograde in situ technique is technically
easier and reduces problems related to manipulation of
the liver during the perfusion. Furthermore, since
there is no recirculation of the collagenase buffer, the
tendency toward acidosis during the second stage of
the perfusion is reduced, thus reducing this potential
toxic effect to the cells. When we reduced the HEPES
concentration of the collagenase buffer from 100
mmol/L to 10 mmol/L and the pH from 7.6 to 7.4 we
found subjectively less vacuolization and membrane
damage with equivalent cell yields and viability.
Hepatocyte transplantation has been attempted in
several animal models as a treatment for certain
hepatic defects and induced hepatic failure without
proven clinical efficiency to date? 5 To be clinically
successful, hepatocyte transplantation must be able to
supply a mass of cells capable of performing metabolic
and synthetic function at levels adequate to support an
animal or patient: It has been demonstrated by several
studies that cell-cell and cell-matrix interactions play
an important role in maintenance of liver-specific
transcription and thus differentiated hepatocyte phenotype in cell culture. 1~We believe we have detailed a
simple and reliable system for rat liver perfusion which
consistently generates viable hepatocytes in large numbers. Furthermore, the ability to supply cell mass
seems very important because it has been shown to be
difficult to induce proliferation in cultured hepatocytes
and proliferative activity is associated with a loss of
differentiated function. 17 Consistent with this finding
in cell culture is the demonstration in regenerating
liver of the linkage between hepatocyte proliferation
and loss of differentiated function./8
There are many problems to be solved before hepatocyte transplantation will be a clinically useful methodology. Others have reported adaptation of these
perfusion systems to biopsy specimens of human liver
and obtained satisfactory cell yields of well functioning
human hepatocytes. 19This report details our efforts to
optimize rat liver perfusion for cell isolation and
implantation toward an ultimate goal of clinically
effective human hepatocyte transplantation.
144
AIKEN ET AL
REFERENCES
1. Vacanti JP: Beyond transplantation, Third Annual Samuel
Jason Mixter Lecture. Arch Surg 123:545-549, 1988
2. Berry MN, Friend DS: High yield preparation of isolated rat
parenehymal cells, A biochemical and fine structure study. J Cell
Biol 43:506-520, 1969
3. Seglen PO: Methods in Cell Biology, vol 13. San Diego, CA,
Academic, 1976, pp 29-83
4. McGowan JA: Hepatocyte proliferation in culture, in Guillonzo A, Guguen-Guillonzo C (eds): Research in Isolated and
Cultured Hepatocytes. J. Libbey Urotext Limited/INSERM, 1986,
pp 13-38
5. Kreamer BL, Stuecker JL, Sawada N, et al: Use of low speed,
150-density Percoll centrifugation method to increase the viabilityof
isolated rat hepatocyte preparations. In Vitro Cell Devel Biol
22:201-205, 1986
6. Worthington Biochemical: Personal communication, November 1987
7. Bumgardner GL, Fasola C, Sutherland DER: Prospects for
hepatocyte transplantation. Hepatology 8:1158-1161, 1988
8. Vacanti JP, Lillehei CW, Jenkins RL, et al and The Boston
Center for Liver Transplantation: Liver transplantation in children:
The Boston Center experience in the first 30 months. Transplant
Proc 19:3261-3266, 1987
9. Russell PS: Selective transplantation. Ann Surg 201:255-262,
I985
10. Palade GE, Claude A: The nature of the golgi apparatus, I.
Parallelism between intercellular myelin figures and golgi apparatus
in somatic cells. J Morphol 85:35-69, 1949
1I. Meredith M J: Rat hepatocyte prepared without collagenase:
Prolonged retention of differentiated characteristics in culture. Cell
Biol Toxicol (in press)
12. Schreiber G, Schreiber M: The preparation of single cell
suspensions from liver and their use for the study of protein
synthesis. Sub Cell Biochem 2:321-383, 1973
13. Jauregui HO, McMillan PN, Hevey K, et al: A quantitative
analysis of lectin binding to adult rat hepatocyte cell surfaces. In
Vitro Cell Devel Biol 24:401-412, 1988
14. Younes M, Shubelt O: The involvement of reactive oxygen
species in hypoxic injury to rat liver. Res Commun Chem Pathol
Pharmacol 59:369-381, 1988
15. Demetriou AA, Whiting JF, Feldman D, et al: Replacement
of liver function in rats by transplantation of microearrier attached
hepatocytes. Science 233:1190-1192, 1986
16. Ben-Zeev A, Robinson GS, Bucher NL, et al: Cell-cell and
cell-matrix interactions differentially regulate the expression of
hepatic and cytoskeletal genes in primary cultures of rat hepatocytes. Proc Natl Acad Sci USA 85:1-6, 1988
17. Clayton DF, Harrelson AL, Darnell JE Jr: Dependence of
liver-specific transplantation on tissue organization. Mol Cell Biol
15:2623-2632, 1985
18. Huber BE, Heilman CA, Wirth PJ, et al: Studies of gene
transcription and translation in regenerating rat liver. Hepatology
6:209-219, 1986
19. Hsu TC, Lipsky MM, Cote KE, et al: Isolation and culture of
hepatocytes from human liver of immediate autopsy. In Vitro Cell
Devel Biol 21:154-160, 1985
Discussion
F. Ryckman (Cincinnati, OH): I think we would all
a g r e e that h e p a t i c t r a n s p l a n t a t i o n has b e c o m e a very
a c c e p t a b l e p r o c e d u r e for patients who have irreversible h e p a t i c failure. However, t h e concept of hepatocyte t r a n s p l a n t a t i o n is even m o r e a p p e a l i n g , as you
pointed out, especially for several disease processes
including: h e r e d i t a r y e n z y m e a b n o r m a l i t i e s ; a c u t e
hepatic failure, where the ability of the liver to regenerate m a y still exist; and also as a b r i d g e to h e p a t i c
t r a n s p l a n t a t i o n in patients who develop sudden h e p a t i c
failure, either because of m e d i c a l progression or
b e c a u s e of r e j e c t i o n - r e l a t e d problems. H e p a t o c y t e
t r a n s p l a n t s have obvious a d v a n t a g e s in t h a t they
require m i n i m a l surgical intervention to i m p l a n t the
hepatocytes and a very small a m o u n t of h e p a t o c y t e s
a r e necessary to e x a c t some i m p r o v e m e n t in h e p a t i c
function. Obviously, living related donors could be
used. W i t h the new cryopreservation techniques t h a t
have been described by Dickset a n d his associates at
U C L A , you could a c t u a l l y set up a h e p a t o c e l l u l a r
b a n k and then r e i m p l a n t patients when necessary. I
think Dr V a c a n t i and his associates have m a d e g r e a t
strides in the p r e p a r a t i o n of successful cell c u l t u r e lines
and also perfecting the i m p l a n t a t i o n techniques. T h e
P e d i a t r i c Liver C a r e C e n t e r in C i n c i n n a t i has used a
very similar t e c h n i q u e with in situ perfusion, a n d our
only exceptions a r e we do use pulsatile perfusion, we do
bubble o x y g e n a t e our p e r f u s a t e buffers, and we like to
control for perfusion volume r a t h e r t h a n t h e a m o u n t o f
time t h a t we perfuse the liver. O t h e r w i s e , our techniques a r e identical to yours a n d I a p p l a u d you for
presenting these techniques for o t h e r l a b o r a t o r i e s to
begin to use. I t h i n k you have very good cell harvest
volumes and viabilities and the p o l y m e r scaffolding to
s u p p o r t the cells really offers an excellent initial
e n g r a f t m e n t procedure. I think s i m i l a r work by D e m e triou and his associates at V a n d e r b i l t would c e r t a i n l y
support the scaffolding technique. O t h e r h e p a t o c y t e
p r e p a r a t i o n s , including m i c r o e n c a p s u l a t i o n d e s c r i b e d
by D i c k s e t t a n d t h e new e x t r a c o r p o r e a l liver s u p p o r t
system, which is a c t u a l l y fixed h e p a t o c y t e s onto a
hollow fiber system s i m i l a r to the hemofiltration system, are also intriguing. Clearly, the best system for
e n g r a f t m e n t , prevention o f rejection, a n d m a i n t e n a n c e
of the c o m p l e x b i o c h e m i c a l function of t h e liver
i m p l a n t is still to be proven. M y real questions to you
revolve a r o u n d t h r e e different issues. Do the microc a r r i e r s t h a t you use e n h a n c e the effectiveness o f the
h e p a t o c y t e t r a n s p l a n t ? Do you believe b e c a u s e t h e y
provide a d e q u a t e s u r f a c e a r e a for h e p a t o c y t e a t t a c h -
HEPATOCYTE HARVEST IN LIVER PERFUSION
ment, they have improved vascularization of the graft
or are they in fact functionally blocking the RES
allowing implantation of your cells. Second, is the
model that you used a syngeneic model? Have you
used this at all in an allogeneic model and does this
affect the inflammation that you have recognized on
your cut sections? Is this related to the hepatocytes
themselves or do you believe it is related to the scaffold
carrier? My final question revolves around your site of
implantation. These were muscle pockets. Have you
thought about alternative sites of implantation within
the portal system where you could take advantage of
the hepatotrophic factors that are present in portal
circulation to enhance both your survival and your
proliferation of cells. All of those who get up in the
middle of the night to transplant would be delighted to
see this work progress because we could have someone
come and put in some hepatocytes and we could all
stay in bed.
W. Andrews (Dallas, TX): Unfortunately, I have
little to add to the comments of Dr Ryckman. This is
extremely important work that gives us the opportunity, especially in patients with metabolic disease, to
replace function when only enzyme replacement is
necessary. I have a rather simplistic question. One of
the things that we have discovered in looking at
different perfusion systems, such as rat liver or small
bowel is that often the collagenase system that is used
can alter liver cell viability as well as their function.
When you examined your various collagenase systems
for cell viability, did you in fact alter the functional
capabilities of the hepatocytes?
M. Schwartz (Sacramento, CA)." I have two brief
questions. You did not elude to the pressure that you
were perfusing the liver before the cell harvest and I
think it is at least empirically known that high pressure
perfusion in whole organ transplantation has a negative impact. Second, it was not clear to me how you
define cell viability? What was the time frame? Did
you use a histologic or other criteria?
J.P. Vacanti (closing): First, in answer to Dr Ryckman's questions, we feel that the biodegradable
scaffolds do greatly enhance the effectiveness of transplantation. Hepatocytes in culture are termed "anchorage-dependent," meaning that they cannot survive
in suspension. Therefore, a simple injection into a
noninjured animal would result in the cells not finding
sites of attachment. We feel that this would be a very
inefficient way of delivering cells. By having them
preanchored on their own scaffolding, we feel that the
145
delivery is much more efficient. Our scaffold systems
are also designed so that structural cues can be
provided to the implanted cells to help them remodel
the tissue. By using systems such as fiber systems, we
greatly increase the surface area available for attachment as well as for diffusion of nutrients, gas exchange,
and waste exchange. Since the biodegradable matrix is
a foreign body, it does produce an inflammatory
response. We feel that the inflammatory response is a
combination of surgical wounding, implanted foreign
body material, and a reaction to the cells. This inflammatory response probably enhances the neovascularization that we routinely see in our grafts. Virtually all
of our studies have been carried out in the syngeneic
model described and we really have not yet performed
a systematic study using an aliogeneic model. We do
know, however, that if outbred rats are transplanted
the implants become inflamed and eventually resorb,
indicating rejection. Finally, Dr Ryckman, we have
implanted these polymer cell constructs at multiple
sites including subcutaneous tissue, intermuscular
pockets, retroperitoneum, omentum, and mesentery.
We have seen engraftment in all of these tissues, which
suggests to us that the more important variable is the
adherence to the biophysical constraints of cell viability until vascularization occurs. We do feel that some
sites will be better than others. For example, fatty
tissue is much more highly vascularized and may be a
more optimal site for hepatocyte implantation, which
requires a very high degree of vascularization. Dr
Andrews, we have found that small changes in the
collagenase perfusion produce large changes in our
ability to produce good yields of viable functioning
hepatocytes. The differences can be caused by the
coilagenase type and lot, the type of perfusion system,
the concentration of collagenase, and the duration of
infusion. This great variability is a weakness of hepatocyte harvest as currently practiced today. In answer to
Dr Schwartz, we have not directly measured the
pressures in our circuit. However, because of the flow
rates and the fact that the perfusion is in an open
system, we feel that the pressures are low. We have
measured cell viability using the trypan blue exclusion
test, which is a standard test. We measure it at several
steps in the process. We do a cell count and cell
viability right after the cells have been dispersed, after
they have been washed and separated. This gives us a
good idea of what happens to the cells while they are
being processed before implantation.
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- InDesign Mac PC Keyboard ShortcutDokumen2 halamanInDesign Mac PC Keyboard ShortcutAnonymous wbRUEuDBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Regulation of LipolysisDokumen32 halamanRegulation of LipolysisAnonymous wbRUEuDBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Lipases in LipolysisDokumen13 halamanLipases in LipolysisAnonymous wbRUEuDBelum ada peringkat
- BCNU - An Antimalarial DugDokumen6 halamanBCNU - An Antimalarial DugAnonymous wbRUEuDBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Quercetin Inhibits Hydrogen Peroxide (H O) - Induced Nf-Binding Activity and Dna Damage in Hepg2 CellsDokumen7 halamanQuercetin Inhibits Hydrogen Peroxide (H O) - Induced Nf-Binding Activity and Dna Damage in Hepg2 CellsAnonymous wbRUEuDBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Refactoring SoftwareDokumen54 halamanRefactoring SoftwareAnonymous wbRUEuDBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Swish Max 3 HelpDokumen788 halamanSwish Max 3 HelpAnonymous wbRUEuDBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- ROS Technical DetailsDokumen5 halamanROS Technical DetailsAnonymous wbRUEuDBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Chikungunya Brief DCO 29jul2014Dokumen19 halamanChikungunya Brief DCO 29jul2014Anonymous wbRUEuDBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- AIDS in The Workplace LawDokumen30 halamanAIDS in The Workplace LawPacific SpectrumBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Approved Moh Guidelines On Submission of Documentation For Registration of Human Pharmaceutical Products RwandaDokumen436 halamanApproved Moh Guidelines On Submission of Documentation For Registration of Human Pharmaceutical Products RwandaAry Bima WinardoBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Supine PositionDokumen29 halamanThe Supine PositionKlaue Neiv CallaBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Basic Principles of Radiology: Bachtiar MurtalaDokumen75 halamanBasic Principles of Radiology: Bachtiar MurtalaMargaretha SonoBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Jurnal Ria Suak 091511195Dokumen6 halamanJurnal Ria Suak 091511195resyaBelum ada peringkat
- MCQs 1Dokumen10 halamanMCQs 1Mostafa MahmoudBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- SCREEMDokumen2 halamanSCREEMDranreb Berylle MasangkayBelum ada peringkat
- DMDS MSDSDokumen11 halamanDMDS MSDSamirhosseine00Belum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Case Study - DR EldaDokumen3 halamanCase Study - DR EldaShashi KumarBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Acquired Peripheral NeuropathiesDokumen20 halamanAcquired Peripheral Neuropathiesfire_n_iceBelum ada peringkat
- Daftar Obat Kapal REKOMENDASI WHO 3RD Rev KKP SemarangDokumen1 halamanDaftar Obat Kapal REKOMENDASI WHO 3RD Rev KKP Semaranganon_914901469Belum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Pathophysiology of TetanusDokumen2 halamanPathophysiology of TetanusAnitha SuprionoBelum ada peringkat
- Nabh Entry LevelDokumen64 halamanNabh Entry LevelRenuka MuruganBelum ada peringkat
- B.pharmacy AyurvedaDokumen55 halamanB.pharmacy Ayurvedapokeman693Belum ada peringkat
- Project Report On Pharmaceutical Unit (Tablet, Capsules, Syrups, Lotion Etc.)Dokumen6 halamanProject Report On Pharmaceutical Unit (Tablet, Capsules, Syrups, Lotion Etc.)EIRI Board of Consultants and Publishers100% (3)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Borax PDFDokumen4 halamanBorax PDFZi LaBelum ada peringkat
- Anaesthesia For Medical Students-Review QuestionsDokumen20 halamanAnaesthesia For Medical Students-Review QuestionsJohnny Lee100% (6)
- Laporan Obat Sesuai Formularium Maret 2019Dokumen22 halamanLaporan Obat Sesuai Formularium Maret 2019Maria AmabiBelum ada peringkat
- Update Stock PT KMD 14-6Dokumen46 halamanUpdate Stock PT KMD 14-6rio1995Belum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- History Taking and MSE AIIMS PatnaDokumen34 halamanHistory Taking and MSE AIIMS PatnaShivendra Kumar100% (1)
- Benign Prostatic HyperplasiaDokumen9 halamanBenign Prostatic HyperplasiaElizabeth Mapa100% (1)
- Una Coales-Get Through Medical School - 1000 Sbas Bofs and Emqs (Get Through Series) (2003) PDFDokumen151 halamanUna Coales-Get Through Medical School - 1000 Sbas Bofs and Emqs (Get Through Series) (2003) PDFCathy QianBelum ada peringkat
- Chief Complaints: Sl. Medicine Name Dosage Freq. Duration InstructionsDokumen4 halamanChief Complaints: Sl. Medicine Name Dosage Freq. Duration InstructionsBanshi Lal MaanBelum ada peringkat
- #Spirochaetes & Mycoplasma#Dokumen28 halaman#Spirochaetes & Mycoplasma#Sarah PavuBelum ada peringkat
- Management of Infective EndocarditisDokumen14 halamanManagement of Infective Endocarditismhafzam2020Belum ada peringkat
- UNIVERSITY OF DELHI - Student Hand BookDokumen75 halamanUNIVERSITY OF DELHI - Student Hand Bookvfxindia100% (1)
- Funny StoriesDokumen5 halamanFunny Storiesamin jamalBelum ada peringkat
- CeftriaxoneDokumen2 halamanCeftriaxoneFlora Angeli PastoresBelum ada peringkat
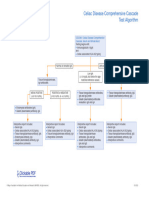
- Celiac Disease Comprehensive Cascade Test AlgorithmDokumen1 halamanCeliac Disease Comprehensive Cascade Test Algorithmayub7walkerBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- NCP 2Dokumen2 halamanNCP 2hsiria100% (1)