Sequential Organ Failure Assessment Score As The Determinant of Outcome For Patients
Diunggah oleh
vidyahamzahJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Sequential Organ Failure Assessment Score As The Determinant of Outcome For Patients
Diunggah oleh
vidyahamzahHak Cipta:
Format Tersedia
45(6):715-720,2004
CLINICAL SCIENCES
Sequential Organ Failure Assessment Score as the Determinant of Outcome for Patients
with Severe Sepsis
Saulius Vosylius, Jurate Sipylaite, Juozas Ivaskevicius
Clinic of Anesthesiology and Intensive Care, Vilnius University, Vilnius, Lithuania
Aim. To evaluate the impact of organ dysfunction in severe sepsis and determine the effectiveness of organ dysfunction
scores to discriminate outcome after admission to the intensive care unit (ICU).
Methods. Patients with a diagnosis of severe sepsis and at least one organ dysfunction on the first day in the ICU
(n=117) were included in the prospective observational study. The presence of organ dysfunction was assessed using
a Sequential Organ Failure Assessment (SOFA). The severity of illness was assessed using a Simplified Acute Physiology Score (SAPS) II during the first 24 hours after the admission to the ICU. The main outcome was survival status on
day 28 after admission to the ICU.
Results. Most common sites of infection were intra-abdominal and respiratory system (77 and 38 cases, respectively).
Median SAPS II score on admission was 47 points (25th-75th quartiles range, 37-57 points). Twenty eight days survival
rate was 41%. The best discrimination results were shown for cumulative scores with the highest for the SOFA score on
day 3 in the ICU. The ability to discriminate outcome on day 1 was weak for the presence of dysfunction in all organ
systems except neurological. The discriminative power of organ dysfunction scores increased during the stay in the
ICU. Neurological and cardiovascular dysfunctions were the independent risk factors for mortality.
Conclusion. The SOFA scores showed high accuracy in describing the course of organ dysfunction for the patients with
severe sepsis. Evolving organ dysfunction following admission to the ICU strongly affected the outcome. Cumulative
SOFA scores were better in discriminating outcome compared to single organ dysfunction scores.
Key words: intensive care units; multiple organ failure; sepsis; treatment outcome; mortality
Severe sepsis became a common condition with
steadily increasing incidence rate (1,2). It is present in
up to 15% of critically ill patients requiring intensive
care, and contributes to the impairments of many organ system functions (3,4). Clinically significant organ dysfunction is the reason for supportive care in
the intensive care unit (ICU) (5). The severity of inflammatory response and impairment of organ function are the major determinants of the outcome in critically ill septic patients. A trend in the outcome improvement was noted over last decade in several
multicenter studies (1,2,6,7).
The severe sepsis is defined as the presence of
sepsis and related organ dysfunction. Clinical trials
and observational studies usually use a scoring system for the assessment of the severity of organ function impairment. Most popular among them are Sequential Organ Failure Assessment (SOFA) score (8),
Logistic Organ Dysfunction System (LODS) (9), and
Multiple Organ Dysfunction Score (MODS) (10). All
of these systems rely on the number and degree of organ dysfunction. Similar feature for all systems is the
measurement of the type and severity of physiologic
function derangement by summing the points of dys-
function from six key organ systems: cardiovascular,
respiratory, neurological, renal, hepatic, and coagulation.
The assessment of the impact of each organ dysfunction to the outcome of the patients admitted to
the ICU with a diagnosis of severe sepsis was undertaken in this study applying a set of reliable statistical
methods. The choice of the SOFA system was made
because it was created to describe a sequence of complications in septic patients (8). Some multicenter and
multinational studies using SOFA system showed different prognostic value of each organ dysfunction and
unequal contribution to outcome in general ICU population (5,8,11). Similar investigations in septic patients are lacking. The objectives of the study were to
evaluate the impact of organ dysfunction in severe
sepsis and to determine the effectiveness of organ
dysfunction scores to discriminate outcome after
admission to the ICU.
Methods
A prospective observational cohort study was performed in
a single medical-surgical ICU of Vilnius University Emergency
Hospital. Data collection took place from February 1, 1998, to
www.cmj.hr 715
Vosylius et al: Organ Dysfunction in Severe Sepsis
Croat Med J 2004;45:715-720
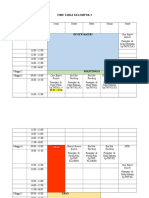
Table 1. Sequential Organ Failure Assessment (SOFA) score (5)
Variables
0
>400
Respiration: PaO2/FiO2
3
Coagulation: platelets, 10 /mL
>150
Liver: bilirubin, mmol/L
<20
Cardiovascular: hypotension no hypotension
Central nervous system:
Glasgow Coma Score
Renal: creatinine, mmol/L
15
<110
1
301-400
101-150
20-32
MAP* <70 mm Hg
13-14
110-170
Score
2
3
4
201-300
101-200
100
51-100
21-50
20
33-101
102-204
>204
Dopamine >5, or
Dopamine >15, or
Dopamine 5, or
dobutamine (any dose) epinephrine 0.1, or epinephrine >0.1, or
norepinephrine 0.1 norepinephrine >0.1
10-12
6-9
<6
171-299
300-440
<440
*MAP mean arterial pressure.
With respiratory support.
Adrenergic agents administered for at least 1 h (dosages are in mg/kg/min).
January 31, 2000. The detailed description of study database and
some definitions of variables (general characteristics, infection)
included in data collection were reported in our previous study
(12). The permission for this study was obtained from the local
Hospital Ethics Committee.
The cohort of 117 patients (5.2% of 2,261 patients in the
database) having a diagnosis of severe sepsis with clinically or
microbiologically confirmed infection on the first day in the ICU
was selected and included to this study. The patients who were
readmitted to the ICU during the same hospitalization or stayed
in the ICU less than 24 hours were not included. Severe sepsis
was defined as sepsis and related dysfunction of at least one organ system. The presence of 6 organ dysfunctions (cardiovascular, neurological, respiratory, renal, hepatic, coagulation) was assessed using a Sequential Organ Failure Assessment (SOFA) score
(Table 1) (5). The presence of each organ dysfunction was defined when degree of dysfunction was equal to 1 and more. The
most abnormal value for each clinical and laboratory parameters
included in the SOFA system was recorded daily and then transformed into the score of dysfunction, graded from 0 to 4. The
SOFA score was calculated daily by summing the worst scores
for each of the six of organ systems on each day. Organ dysfunction on day 1 and maximum score of dysfunction for all the six
organ systems during the whole stay in the ICU were found.
SOFA scores on day 1 and day 3 in the ICU were selected for the
assessment of prognosis.
ICU-acquired infection was defined as an infection occurring more than 48 h after the admission to the ICU. In other cases,
infections were considered as the infections at the ICU admission. The severity of illness was assessed using the Simplified
Acute Physiology Score (SAPS) II during the first 24 hours after
the admission to the ICU (13). The SAPS II score is the sum of the
points assigned to each of the 17 variables (12 physiological variables, age, type of admission, and 3 underlying diseases) with
higher score representing more severe illness. Severe chronic diseases relevant to an infection included: hematological malignancies, metastatic cancer, steroid/immunosuppressive therapy, radio-/chemotherapy, chronic renal failure, diabetes mellitus, and
cirrhosis.
The length of stay in the ICU or hospital was measured as
number of days from admission to the ICU to discharge from the
ICU and hospital, respectively. The main outcome was the survival status on day 28 after the admission to the ICU. The patients
were distributed into two groups according to the 28-day survival
status: alive (n=48) or dead (n=69).
Statistical Analysis
Quantitative normally distributed variables were presented
as means standard deviation (SD) and non-normally distributed
variables (age, length of stay, SAPS II score) as medians and the
25th-75th quartiles range. Univariate comparison was performed
to compare variables between two groups. The organ dysfunction scores were compared using the unpaired t-test. Categorical
variables were expressed as actual numbers and percentages. In
all comparisons, p<0.05 was considered statistically significant.
Multivariate logistic regression analysis was applied to determine the independent contribution of organ dysfunction
scores to the prediction of the mortality as a dependent variable.
The maximum scores for each of the six organ systems were used
716
as independent variables. The regression equation represents
how much dependent variable will change with any given
change of independent variables constructing a regression line
on a scatter diagram. The constant and coefficients () for all variables are used in regression equation. Constant signifies the distance above the baseline at which the regression line cuts the vertical axis. The odds ratios with 95% confidence intervals (CI)
were used to estimate the association between the independent
variables and the dependent variable. The Hosmer-Lemeshow
statistic was used to evaluate the calibration, correspondence between observed and predicted mortality. Lower HosmerLemeshow value and higher p value indicate better fit. Good fit
was defined as p>0.05.
The discriminative power of the SOFA scores for the prediction probability of the ICU mortality was tested by the area under the receiver operating characteristic (ROC) curve. The area
under the ROC curve summarizes the relationship between sensitivity (number of true positives) and 1-specificity (number of
false positives) for all the possible values of the organ dysfunction
scores. The area under the ROC curve estimates the ability of the
model to assign a higher risk of death to patients who die.
Survival curves were estimated using the Kaplan-Meier
method. The patients admitted to the intensive care unit with a
diagnosis of severe sepsis were stratified into subgroups according to the number of initial organ dysfunctions. Survival times
were measured from the date of the ICU admission until the 28th
day. Statistical analysis was performed using the SPSS 10.0 statistical package (SPSS Inc, Chicago, IL, USA).
Results
Among 117 patients admitted to the ICU with a
diagnosis of severe sepsis, the most common sites of
infection were intra-abdominal and respiratory (77
and 38 cases, respectively). Urinary tract and soft tissue infection (15 and 8 cases, respectively), and other
sites of infections were less common. Forty-two patients had two or more sites of infection on admission.
Bacteremia was confirmed in 20 patients.
Additionally, ICU-acquired infection was diagnosed in 48 patients. Respiratory and urinary tract infections were diagnosed most frequently (30 and 11
cases, respectively). Intra-abdominal, intra-vascular
catheter related, and other sites of infection were less
common. Twenty-one patients acquired bloodstream
infection during the stay in the ICU.
Eighty-eight patients were surgical. Abdominal
surgery was most common among surgical interventions (n=57). The median age of patients was 69
years (25th-75th quartiles range, 57-77 years). Nineteen (16%) patients had at least one severe chronic
disease. The median SAPS II score recorded within 24
hours of the admission was 47 (37-57) points. The
median length of stay in the ICU was 4 (3-7) days, in
Vosylius et al: Organ Dysfunction in Severe Sepsis
Table 2. Sequential Organ Failure Assessment (SOFA) scores
in severe sepsis patients during stay in the intensive care
unit*
alive
Scores
(n=48)
SOFA score 5.22.9
Organ dysfunction:
cardiovascular 1.51.4
neurological 0.81.1
respiratory
0.91.3
coagulation 0.20.5
renal
1.11.2
hepatic
0.70.9
80
60
6
40
4
20
2
0
Number of patients
10
Mean SOFA score
the hospital 8 (4-25) days. Twenty-eight days survival
rate was 41%.
There were 85% of the patients who had two or
more organ dysfunctions on day 1. The incidence of
organ dysfunction on day 1 was noted more frequently for renal, cardiovascular, and neurological
systems (67%, 66%, and 61% of cases, respectively).
The abnormalities in respiratory, hepatic, and coagulation function were less common (42%, 41%, and
25% of cases, respectively). During the whole stay in
the ICU, cardiovascular (80%), renal (78%), and neurological (76%) dysfunction was the most common.
The lowest scores and small contribution of the
coagulation and hepatic systems to the overall SOFA
score was noted. SOFA score on day 1 and day 3 were
significantly higher in non-survivors than those in survivors (Table 2). There were minor differences in the
severity of organ dysfunction on day 1 between two
groups of patients. Significant changes in the course
of organ dysfunction were observed during the stay in
ICU. The non-survivors compared with the survivors
had higher organ dysfunction scores for all organ
systems (p<0.01), except hepatic.
Croat Med J 2004;45:715-720
0
1
Day in the ICU
Figure 1. Sequential organ failure assessment score as the
determinant of outcome for patients with severe sepsis. The
trends in daily Sequential Organ Failure Assessment (SOFA)
scores for the patients with a diagnosis of severe sepsis over
the first seven days in the intensive care unit. The patients
are divided in two groups according to 28-day survival status. The SOFA scores were significantly higher in non-survivors on day 1 (p=0.001), and on each subsequent day
(p<0.001). SOFA scores are expressed as means standard
error. Open bars SOFA score, survivors; closed bars
SOFA score, non-survivors; triangles number of survivors;
squares number of non-survivors.
Day 1
Day 3
dead
alive
dead
(n=69) p (n=48) (n=69)
p
7.43.4 0.001 3.22.0 8.13.9 <0.001
Table 3. Discriminative power of organ dysfunction degree
defined by Sequential Organ Failure Assessment (SOFA)
scores for 117 patients admitted to the intensive care unit
with a diagnosis of severe sepsis*
2.01.5
1.51.4
1.11.3
0.50.7
1.51.3
0.81.0
area
under
Score
ROC
SOFA score 0.68
Organ dysfunction:
cardiovascular 0.60
neurological 0.63
respiratory
0.56
coagulation 0.59
renal
0.59
hepatic
0.51
0.083
0.007
0.269
0.017
0.085
0.687
1.81.5 3.21.4 <0.001
0.91.1 2.41.3 <0.001
1.11.4 2.01.5 0.001
0.60.8 1.11.1 0.005
1.31.2 2.31.4 <0.001
0.91.0 1.01.2 0.294
*The outcome used was 28-day survival status. Data are expressed as
meansstandard deviation.
The trend of the mean SOFA score for the first
seven days of ICU stay showed a progressive decrease
in the total number of patients and the significant difference of SOFA scores between survivors and
non-survivors in each day over the first week in the
ICU (Fig. 1). Non-survivors had stable higher SOFA
scores daily during the first week in the ICU. In survivors, organ dysfunction declined gradually as reflected by decreasing mean daily SOFA scores over
the first week.
In the evaluation of the discriminative power of
the SOFA scores, the area under the ROC was used
(Table 3). The ability to discriminate outcome on day
1 was weak for the presence of dysfunction in all organ systems except for neurological. However, the
discriminative power of organ dysfunction scores increased over the stay in ICU. The mortality became
significantly related to the severity of dysfunction in
each organ system during stay in the ICU except for
hepatic system with most significant values for cardiovascular and neurological system. The best discrimination results were shown for cumulative scores with
the highest for the SOFA score on day 3, less for the
SOFA score on day 1. The discriminative power of the
Day 1
Day 3
(95%
area
(95%
confidence
under confidence
interval)
p
ROC interval)
p
(0.58-0.78) 0.001 0.86 (0.78-0.93) <0.001
(0.49-0.66)
(0.53-0.74)
(0.46-0.67)
(0.49-0.69)
(0.49-0.69)
(0.41-0.62)
0.092
0.011
0.248
0.097
0.100
0.790
0.80
0.81
0.66
0.62
0.67
0.54
(0.73-0.89) <0.001
(0.73-0.89) <0.001
(0.56-0.76) 0.003
(0.52-0.73) 0.023
(0.60-0.79) <0.001
(0.44-0.65) 0.463
*The outcome used was 28-day survival status.
ROC receiver operating characteristic.
SAPS II score was 0.691 (95% CI 0.594-0.787,
standard error 0.049, p<0.001).
A multivariate logistic regression analysis was
used to evaluate the relative independent contribution to the outcome. Among different organ system
scores on day 1, only neurological dysfunction carried the highest significant correlation with risk of
mortality (odds ratio, 1.490; 95%CI 1.057-2.099;
p=0.023). The contribution of the maximum score of
each organ system dysfunction during stay in the ICU
is shown in Table 4. Neurological and cardiovascular
dysfunction were associated with the highest contribution to the outcome (p<0.001).
Kaplan-Meier survival analysis showed that the
subgroups of patients with three and higher number
of organ systems with dysfunction had a lower survival rate than the subgroups of patients with one or
two organ systems with dysfunction (Fig. 2).
717
Vosylius et al: Organ Dysfunction in Severe Sepsis
Croat Med J 2004;45:715-720
Table 4. Relative contribution of the maximum value of organ dysfunction to the outcome during stay of 117 patients
with a diagnosis of severe sepsis in the intensive care unit for
each of the six components of the Sequential Organ Failure
Assessment (SOFA)
Variable
Nagelkerke R2 Odds ratio (95% confidence intervals)
Neurological
0.561
2.492 (1.621-3.833)
Cardiovascular
2.111 (1.435-3.105)
Respiratory
1.143 (0.798-1.636)
Renal
1.119 (0.744-1.682)
Coagulation
1.269 (0.726-2.217)
Hepatic
1.353 (0.793-2.309)
*The outcome used was 28-day survival status.
1.0
n=1
Probability of survival
0.8
n=2
0.6
0.4
n=3
0.2
n4
0
7
14
21
28
Days
after
to to
intensive
care unit
Days
afteradmisson
admission
the intensive
care unit
Figure 2. Sequential organ failure assessment score as the determinant of outcome for patients with severe sepsis. KaplanMeier estimates of the cumulative probability of survival stratified by the number of initial organ dysfunction for patients admitted to the intensive care unit with a diagnosis of severe sepsis. Comparison of the cumulative survival estimates over the
hospital stay for patients with one (n=1), two (n=2), three
(n=3), or four and more (n4) organ dysfunctions.
Discussion
The results of the present study showed that the
changes in the severity of organ dysfunction were
closely related to the outcome of the patients admitted to ICU with diagnosis of severe sepsis. Initial and
daily scores outlined the baseline and evolution in the
severity of disease. Increasing organ dysfunction
scores and cumulative SOFA scores reflected the
worsening function in organ systems during the
course of severe sepsis mostly in non-surviving patients. The SOFA score on day 3 was better compared
with SOFA score on day 1 as the tool for outcome
prediction.
Some degree of organ dysfunction necessitating
active treatment is frequently present in a majority of
critically ill patients. The assessment of organ dysfunction scores are often used to determine the baseline severity of illness and the pattern of changes in organ function over the course of various critical illnesses. In this study we evaluated organ dysfunction
using the SOFA system. This system was developed
as a tool for sepsis-related organ failure assessment
(8). Further, it was validated in general ICU population in subsequent multicenter studies showing the
718
best results (5,8,11). The SOFA system was also applied to many other diagnostic groups of the ICU patients (medical, cardiac, trauma, pancreatitis, acute
renal failure, and hematological malignancy) (14-18).
When comparisons were made among organ dysfunction systems in the predictive ability of outcome,
SOFA system showed highest values (18-20). The results of our study confirmed that the SOFA score is a
good tool for assessing the impact of organ dysfunction in severe sepsis.
An initial wave of dysfunction due to the presence of infection on admission to the ICU is most
commonly observed in main vital organ functions
(cardiovascular, respiratory, and neurological). All
our patients with severe sepsis had at least one organ
dysfunction. A significant proportion of the patients
acquired infection during stay in the ICU. An inflammatory response to new acquired infection episodes
additionally to the initial septic insult or inadequate
resuscitation is the most likely mechanism causing a
second wave of organ dysfunction. The emergence of
more severe organ dysfunction was strongly associated with mortality. So measurements of sepsis-related evolving organ dysfunction are clearly needed
during the course of intensive care (on admission,
daily, maximal scores) to follow organ function over
time (21-23).
The incidence of organ dysfunctions varies according to the definition and the case-mix. For the patients with severe sepsis cardiovascular, respiratory,
neurological, and renal dysfunctions were most common. Hematological and hepatic dysfunction was less
common. Respiratory dysfunction, especially its mild
form, was found less frequently than expected in our
study. It could be related to the existing practice to
take arterial blood samples for blood gas analysis routinely only for most severe cases. In the multicenter
study of working group on sepsis-related problems of
the European Society of Intensive Care Medicine
which involved all ICU patients the incidence rate of
organ dysfunction was highest also for respiratory,
neurological, and renal systems (5). SOFA system was
successfully applied and helped to assess morbidity in
severe sepsis clinical trial managed with and without
recombinant human activated protein C (23).
Discriminatory power in outcome prediction as
estimated by the area under ROC was excellent for
cumulative SOFA scores on day 1, day 3, and for all
organ dysfunctions, except hepatic. However, the initial degree of individual organ dysfunction scores
were less useful for outcome analysis compared with
discriminative capability of increasing severity of acquired organ dysfunction during intensive care. The
measurement of organ dysfunction daily during the
ICU stay provided additional prognostic information
compared to baseline measures. The discriminative
capability of the SOFA score was the highest on day
3. Similarly, Ferreira et al (22) determined that, regardless of the initial score, an increase in SOFA score
during the first 48 hours in the ICU predicts a mortality rate of at least 50%.
The weight of each organ score in cumulative
SOFA scores was not equal. The most severe impair-
Vosylius et al: Organ Dysfunction in Severe Sepsis
ment was noted in cardiovascular system, followed
by renal, neurological, and respiratory systems. Multivariate logistic regression analysis, including maximum values of organ dysfunction, revealed that two
organ systems independently associated with ICU
mortality were the neurological and cardiovascular
ones. The predictive power of other organ dysfunctions was relatively less important which may be due to
a small proportion of more severe dysfunctions.
In the European Sepsis Study, Alberti et al (24)
found that acute organ dysfunction and shock were
among the prognostic factors of hospital mortality.
Jacobs et al (25) described a cohort of critically ill patients who developed septic shock during stay in the
ICU. The development of septic shock was associated
with the progression of organ dysfunction resulting in
higher maximal and delta multiple organ dysfunction
scores, reflecting new organ dysfunction arising following ICU admission. The majority of our patients
underwent abdominal surgery and had intra-abdominal source of infection. Some of them had chronic
liver function impairment. The hepatic dysfunction
was assessed by bilirubin level in serum, which lacks
specificity for acute hepatic dysfunction and has limited ability to reflect the full spectrum of liver dysfunction in sepsis.
This study included only patients admitted to a
single ICU institution. We selected survival status on
day 28 after ICU admission as the main outcome measure and did not take into account the later changes in
clinical course. In original SOFA studies, the ICU
mortality was chosen as the outcome measure (5,8).
The assessment of ICU outcome is readily available
without any additional effort. However, the discrimination power (area under ROC) of SOFA scores was
even slightly higher when using ICU mortality and
lower for hospital mortality as the end point of outcome (our unpublished data). Mortality rate in our
study was high but within reported ranges in recently
conducted multicenter study in the European countries, Canada, and Israel (26).
In summary, the severity of organ dysfunction
proved to be a good factor in discriminating outcome
for the patients with severe sepsis. The SOFA scores
showed high accuracy describing the course of organ
dysfunction in these patients. Evolving organ dysfunction following admission to the ICU strongly affected
the outcome. Cumulative SOFA scores, particularly
on day 3, were better in predicting outcome compared to single organ dysfunction score. Cardiovascular, neurological, and respiratory dysfunctions were
the independent risk factors for mortality. The assessment of organ dysfunction should be used for risk
stratification in clinical trials including critically ill
patients with severe sepsis.
Acknowledgements
The authors thank Mr A. Bieliauskas for the preparation of
the software for data collection, processing, and statistical analysis. Financial support for the study was received from Open Society Institute, regional program.
Croat Med J 2004;45:715-720
References
1 Angus DC, Wax RS. Epidemiology of sepsis: an update.
Crit Care Med. 2001;29(7 Suppl):S109-16.
2 Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979
through 2000. N Engl J Med. 2003;348:1546-54.
3 Brun-Buisson C, Doyon F, Carlet J, Dellamonica P,
Gouin F, Lepoutre A, et al. Incidence, risk factors, and
outcome of severe sepsis and septic shock in adults. A
multicenter prospective study in intensive care units.
French ICU Group for Severe Sepsis. JAMA. 1995;274:
968-74.
4 Cohen J, Guyatt G, Bernard GR, Calandra T, Cook D,
Elbourne D, et al. New strategies for clinical trials in patients with sepsis and septic shock. Crit Care Med.
2001;29:880-6.
5 Vincent JL, de Mendonca A, Cantraine F, Moreno R,
Takala J, Suter PM, et al. Use of the SOFA score to assess
the incidence of organ dysfunction/failure in intensive
care units: results of a multicenter, prospective study.
Working group on sepsis-related problems of the European Society of Intensive Care Medicine. Crit Care
Med. 1998;26:1793-800.
6 Bernard GR, Vincent JL, Laterre PF, LaRosa SP,
Dhainaut JF, Lopez-Rodriguez A, et al. Efficacy and
safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001;344:699-709.
7 Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A,
Knoblich B, et al. Early goal-directed therapy in the
treatment of severe sepsis and septic shock. N Engl J
Med. 2001;345:1368-77.
8 Vincent JL, Moreno R, Takala J, Willatts S, De
Mendonca A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working
Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med.
1996;22:707-10.
9 Le Gall JR, Klar J, Lemeshow S, Saulnier F, Alberti C,
Artigas A, et al. The logistic organ dysfunction system. A
new way to assess organ dysfunction in the intensive
care unit. ICU Scoring Group. JAMA. 1996;276:802-10.
10 Marshall JC, Cook DJ, Christou NV, Bernard GR,
Sprung CL, Sibbald WJ. Multiple organ dysfunction
score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23:1638-52.
11 Moreno R, Vincent JL, Matos R, Mendonca A, Cantraine
F, Thijs L, et al. The use of maximum SOFA score to
quantify organ dysfunction/failure in intensive care. Results of a prospective, multicenter study. Working
Group on Sepsis related Problems of the ESICM. Intensive Care Med. 1999;25:686-96.
12 Vosylius S, Sipylaite J, Ivaskevicius J. Intensive care unit
acquired infection: a prevalence and impact on morbidity and mortality. Acta Anaesthesiol Scand. 2003;47:
1132-7.
13 Le Gall JR, Lemeshow S, Saulnier F. A new Simplified
Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;
270:2957-63.
14 Janssens U, Graf C, Graf J, Radke PW, Konigs B, Koch
KC, et al. Evaluation of the SOFA score: a single-center
experience of a medical intensive care unit in 303 consecutive patients with predominantly cardiovascular
disorders. Sequential Organ Failure Assessment. Intensive Care Med. 2000;26:1037-45.
719
Vosylius et al: Organ Dysfunction in Severe Sepsis
15 Ceriani R, Mazzoni M, Bortone F, Gandini S, Solinas C,
Susini G, et al. Application of the sequential organ failure assessment score to cardiac surgical patients. Chest.
2003;123:1229-39.
16 Antonelli M, Moreno R, Vincent JL, Sprung CL,
Mendoca A, Passariello M, et al. Application of SOFA
score to trauma patients. Sequential Organ Failure Assessment. Intensive Care Med. 1999;25:389-94.
17 Silfvast T, Pettila V, Ihalainen A, Elonen E. Multiple organ failure and outcome of critically ill patients with hematological malignancy. Acta Anaesthesiol Scand.
2003;47:301-6.
18 Halonen KI, Pettila V, Leppaniemi AK, Kemppainen EA,
Puolakkainen PA, Haapiainen RK. Multiple organ dysfunction associated with severe acute pancreatitis. Crit
Care Med. 2002;30:1274-9.
19 Peres Bota D, Melot C, Lopes Ferreira F, Nguyen Ba V,
Vincent JL. The Multiple Organ Dysfunction Score
(MODS) versus the Sequential Organ Failure Assessment (SOFA) score in outcome prediction. Intensive
Care Med. 2002;28:1619-24.
20 Pettila V, Pettila M, Sarna S, Voutilainen P, Takkunen
O. Comparison of multiple organ dysfunction scores in
the prediction of hospital mortality in the critically ill.
Crit Care Med. 2002;30:1705-11.
21 Russell JA, Singer J, Bernard GR, Wheeler A, Fulkerson
W, Hudson L, et al. Changing pattern of organ dysfunction in early human sepsis is related to mortality. Crit
Care Med. 2000;28:3405-11.
22 Ferreira FL, Bota DP, Bross A, Melot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in
critically ill patients. JAMA. 2001;286:1754-8.
720
Croat Med J 2004;45:715-720
23 Vincent JL, Angus DC, Artigas A, Kalil A, Basson BR,
Jamal HH, et al. Effects of drotrecogin alfa (activated) on
organ dysfunction in the PROWESS trial. Crit Care Med.
2003;31:834-40.
24 Alberti C, Brun-Buisson C, Goodman SV, Guidici D,
Granton J, Moreno R, et al. Influence of systemic inflammatory response syndrome and sepsis on outcome
of critically ill infected patients. Am J Respir Crit Care
Med. 2003;168:77-84.
25 Jacobs S, Zuleika M, Mphansa T. The multiple organ
dysfunction score as a descriptor of patient outcome in
septic shock compared with two other scoring systems.
Crit Care Med. 1999;27:741-4.
26 Alberti C, Brun-Buisson C, Burchardi H, Martin C,
Goodman S, Artigas A, et al. Epidemiology of sepsis and
infection in ICU patients from an international multicenter cohort study. Intensive Care Med. 2002;28:
108-21.
Received: March 12, 2004
Accepted: September 29, 2004
Correspondence to:
Juozas Ivaskevicius
Clinic of Anesthesiology and Intensive Care
Vilnius University Emergency Hospital
Siltnamiu 29
04130 Vilnius-43, Lithuania
juozas.ivaskevicius@mf.vu.lt
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Career Opportunities in NursingDokumen16 halamanCareer Opportunities in NursingRani100% (5)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- CCN (Critical Care Nursing)Dokumen4 halamanCCN (Critical Care Nursing)Laurence ZernaBelum ada peringkat
- Log Book IdccmDokumen38 halamanLog Book IdccmAnish H Dave50% (2)
- International Case StudyDokumen36 halamanInternational Case Studymamona zaheerBelum ada peringkat
- New Assessment Tool Level 2 Hospital PDFDokumen18 halamanNew Assessment Tool Level 2 Hospital PDFMaridel JuenBelum ada peringkat
- Ijmr Tetanus in 2 Yo PDFDokumen4 halamanIjmr Tetanus in 2 Yo PDFvidyahamzahBelum ada peringkat
- CHF (Diagnosis, Patophysiology, Therapy, and Implication For Respiratory Care)Dokumen10 halamanCHF (Diagnosis, Patophysiology, Therapy, and Implication For Respiratory Care)blobfish_danboBelum ada peringkat
- 4398 8451 1 SM PDFDokumen9 halaman4398 8451 1 SM PDFKavita FairuzBelum ada peringkat
- Time Table Kelompok 2Dokumen3 halamanTime Table Kelompok 2vidyahamzahBelum ada peringkat
- CataractDokumen26 halamanCataractHasnan HabibBelum ada peringkat
- LGBT or GLBT Is AnDokumen2 halamanLGBT or GLBT Is AnvidyahamzahBelum ada peringkat
- 2049 9752 5 2Dokumen7 halaman2049 9752 5 2BillGhoes'toBelum ada peringkat
- Unusual Airway Situation, Esophageal Stethoscope Knotted AroundDokumen2 halamanUnusual Airway Situation, Esophageal Stethoscope Knotted AroundvidyahamzahBelum ada peringkat
- 2049 9752 2 25Dokumen5 halaman2049 9752 2 25dewi_s_3Belum ada peringkat
- 2015 AHA Guidelines Highlights EnglishDokumen36 halaman2015 AHA Guidelines Highlights EnglishshiloinBelum ada peringkat
- SOFA (Sequential Organ Failure Assessment) and PELOD (Pediatric LogisticDokumen5 halamanSOFA (Sequential Organ Failure Assessment) and PELOD (Pediatric LogisticvidyahamzahBelum ada peringkat
- Fss-Icu An Outcome Worth MeasuringDokumen15 halamanFss-Icu An Outcome Worth Measuringapi-703723590Belum ada peringkat
- Pediatric Medical DevicesDokumen25 halamanPediatric Medical DevicesDuck Mann-ConsulBelum ada peringkat
- Fluid Response Evaluation in Sepsis Hypotension and Shock A Randomized Clinical TrialDokumen15 halamanFluid Response Evaluation in Sepsis Hypotension and Shock A Randomized Clinical TrialntnquynhproBelum ada peringkat
- Tell The World Project WC EditDokumen3 halamanTell The World Project WC Editapi-473913057Belum ada peringkat
- J Parenter Enteral Nutr - 2021 - Compher - Guidelines For The Provision of Nutrition Support Therapy in The AdultDokumen30 halamanJ Parenter Enteral Nutr - 2021 - Compher - Guidelines For The Provision of Nutrition Support Therapy in The Adultsulemi castañonBelum ada peringkat
- American Journal of Respiratory and Critical Care MedicineDokumen12 halamanAmerican Journal of Respiratory and Critical Care MedicineChanya ChomchoeyBelum ada peringkat
- Weaning ProtocolDokumen6 halamanWeaning ProtocolerwanBelum ada peringkat
- Accelerating System Thinking in Health SystemsDokumen23 halamanAccelerating System Thinking in Health SystemsFadhila Nurfajrina100% (1)
- ALVO Mobile HospitalDokumen8 halamanALVO Mobile HospitalGUSTAVO el canal de youtubeBelum ada peringkat
- Australasian Emergency Care: Happy I. Kusumawati, Judy Magarey, Philippa RasmussenDokumen6 halamanAustralasian Emergency Care: Happy I. Kusumawati, Judy Magarey, Philippa Rasmussenrida rahmayantiBelum ada peringkat
- ANP CASE PRESENTATION OF ICU 101 ShilpaDokumen23 halamanANP CASE PRESENTATION OF ICU 101 ShilpaShilpa JoshiBelum ada peringkat
- Emily Morgan - ResumeDokumen2 halamanEmily Morgan - Resumeapi-283578734Belum ada peringkat
- Hospital Assessment ToolDokumen68 halamanHospital Assessment ToolXylia TocaoBelum ada peringkat
- Materi B. InggrisDokumen9 halamanMateri B. Inggrisdita novia maharaniBelum ada peringkat
- The Guitar in MTDokumen20 halamanThe Guitar in MTDorcas WongBelum ada peringkat
- The Organization of Internal Management ConsultancyDokumen8 halamanThe Organization of Internal Management ConsultancyBenjamin C. OkoroaforBelum ada peringkat
- Alex Hardin Resume 2015Dokumen3 halamanAlex Hardin Resume 2015api-306883462Belum ada peringkat
- Bicar IcuDokumen10 halamanBicar Icuhemodiálise NIRBelum ada peringkat
- Adnan - Abdi 2Dokumen65 halamanAdnan - Abdi 2Shükrî ÆbBelum ada peringkat
- Indianbank Policy WordingsDokumen32 halamanIndianbank Policy WordingsRaja KatareBelum ada peringkat
- Flannery 2016Dokumen10 halamanFlannery 2016mohamad safiiBelum ada peringkat
- Uoi Affidavit 9052021 Final With Annexures 1 91 393168Dokumen91 halamanUoi Affidavit 9052021 Final With Annexures 1 91 393168RUDRAA HIRANWARBelum ada peringkat
- Tutorials / Workshops: 9th Annual Critical Care SymposiumDokumen2 halamanTutorials / Workshops: 9th Annual Critical Care SymposiumredmondptBelum ada peringkat
- Inferior Vena Cava Diameter and Collapsibility IndexDokumen9 halamanInferior Vena Cava Diameter and Collapsibility IndexmalisalukmanBelum ada peringkat
- Achmad R. Muttaqien Cost Effectiveness of Intensive Care in A Low Resource Setting A Prospective Cohort of Medical Critically Ill PatientsDokumen17 halamanAchmad R. Muttaqien Cost Effectiveness of Intensive Care in A Low Resource Setting A Prospective Cohort of Medical Critically Ill PatientsAchmad R. MuttaqienBelum ada peringkat