Thomas 1995. Orthodontic Camouflage Versus Orthognathic Surgery in The Treatment of Mandibular Deficiency.
Diunggah oleh
Benjamin NgJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Thomas 1995. Orthodontic Camouflage Versus Orthognathic Surgery in The Treatment of Mandibular Deficiency.
Diunggah oleh
Benjamin NgHak Cipta:
Format Tersedia
J Oral Maxillofac Surg
53:579-587, 1995
Orthodontic Camouflage Versus
Orthognathic Surgery in the Treatment of
Mandibular DeficiencY
PAUL M. THOMAS, DMD, MS*
The Class I1 relationship is the most prevalent subclassification of malocclusion.1 Recognizing the limitations of this description, epidemiologists have formulated indices and scales for use in public health studies.
The results of these surveys suggest that 15% to 20%
of the teenage population have an overjet of 6 mm or
greater. Although such studies do not directly address
this issue, it is likely that many of these individuals
have an abnormality in jaw size or position as a contributing factor. ~
Motivations for seeking correction of this imbalance
generally include a mixture of functional and psychosocial concerns, including self-image as influenced
by dental and facial esthetics. It has been suggested
that Class II malocclusion may lead to dental attrition
and periodontal trauma as well as problems with
speech and chewing. Despite conflicting and contradictory evidence, some clinicians still consider Class II
malocclusion a contributing factor in temporomandibular disorders. 3'4 In a psychosocial context, research
has shown that malocclusion affects employability,
interpersonal relationships, and, accordingly, selfimage. 5
of favorable growth and dentoalveolar manipulation
can lead to reasonable results in the appropriate patient. 6
There are two treatment options for postpubertal individuals seeking correction; orthodontic camouflage
and surgical advancement of the mandible in conjunction with orthodontics. Camouflage, or orthodontic
compensation of Class II malocclusion, is one of the
more common treatment strategies used in clinical
practice. The maxillary anterior teeth are retracted and
their counterparts in the lower arch proclined in an
attempt to reduce overjet and establish a Class I canine
relationship. The extraction of teeth, typically first premolars, is necessary in one or both arches to eliminate
crowding and provide room for compensation. Surgical
treatment involves preoperative orthodontics to properly position the teeth in the respective jaw and an
operative procedure to correct mandibular position,
followed by finishing orthodontics for occlusal detailing. The focus of this discussion will be on these two
approaches.
Although there would appear to be ample justification for correcting Class II malocclusions; previous
experience suggests that there are flaws in the process
of selecting treatment options. There is generally little
disagreement when considering patients at the extremes of the classification. Mild Class II problems can
be orthodontically corrected and severe discrepancies
require orthognathic surgery. Problems seem to occur
when the patient falls in a "grey zone" and might be
treated by either option. Needless to say, both orthodontic camouflage and surgery have been used inappropriately in the past. A review of patients seen from
1984 to 1987 in the University of North Carolina Dentofacial Program indicated 20% of those seen had previous orthodontic treatment and were dissatisfied with
the outcome. 7 The majority of these patients had undergone camouflage treatment for Class II malocclusions.
Likewise, mandibular advancements performed to correct moderate overjet have sometimes exposed the individual to greater morbidity, while producing negligible facial change. A primary goal of this article is to
identify factors that influence both the decision-making
Treatment Alternatives
Four options exist for those individuals seeking correction of increased overjet. Patient concerns and clinical findings are key factors in narrowing the choice.
Treatment should not be considered if the outcome is
unlikely to meet patient expectations, or if local factors
such as dental or periodontal health indicate a prosthetic alternative. Growth guidance may be suggested
for the prepubertal patient having a favorable growth
pattern. Although there is mounting evidence that the
skeletal impact is negligible clinically, a combination
* In private practice.
Address correspondence to Dr Thomas: 5501 Fortune's Ridge Dr,
Suite H, Durham, NC 27713-9355.
1995 American Association of Oral and Maxillofacial Surgeons
0278-2391/95/5305-001553.00/0
579
580
ORTHODONTIC CAMOUFLAGE VS ORTHOGNATHIC SURGERY
process and assessment of outcome. Recognition of
these factors should help with the selection of a treatment option that addresses patient concerns while considering a favorable cost (risk) versus benefit ratio.
Because this discussion and the companion article have
been written in the context of point/counterpoint, emphasis will be placed on the efficacy of orthodontic
camouflage.
The Decision-Making Process
DIAGNOSIS AND PLANNING
The treatment planning process is well-known to
most contemporary clinicians and generally follows a
method suggested by Ackerman and Proffit more than
20 years ago. Using a scheme of Venn diagrams to
expand on the traditional Angle classification, they
identified five major characteristics of malocclusion
that were descriptive in three dimensions. 8 They also
adapted Lawrence Weed's problem-oriented medical
diagnosis for use in an orthodontic context. 9 Following
this method, data collection includes patient interview,
clinical examination, radiographic studies, standardized photographs or slides, and dental models. This
information is analyzed to produce a list of findings
that may be prioritized in the context of patient concerns according to severity. Treatment alternatives,
orthodontic camouflage, and surgery in this case are
developed with consideration for the ability of each to
address patient concerns with maximum efficiency and
minimum morbidity. This process may include treatment simulation using computer imaging and model
surgery or orthodontic setup. Accepting the limitations
of such simulation, it remains the best means available
to explore options and communicate potential outcome
to the patient and family.
REVIEWING THE OPTIONS
A key part of the preliminary decision-making process involves an unbiased explanation of the alternatives and the associated cost and risk versus benefit
with each. Intellectual honesty is paramount during
both the initial encounter and the subsequent discussion of alternatives. Because it is natural for clinicians
to seek solutions in the context of training and experience, care must be taken to avoid inappropriate influence on patient perceptions and attitudes. This may be
especially difficult for the orthodontist presented with
a patient who is initially expecting limited orthodontic
treatment only to discover there is a significant underlying skeletal imbalance. If there is some uncertainty
regarding alternatives at the initial visit, diagnostic records should be suggested and definitive answers deferred. A sensitive, carefully structured, global discus-
sion can be used to introduce concepts without
committing to a course of action.
If surgery has been discussed at the initial visit and
is a viable option, it is ideal to have the surgeon present
for the subsequent treatment explanation or to arrange
for a timely follow-up consultation. Because treatment
strategies are significantly different for each option,
the individual contemplating treatment must be given
enough information to make an informed decision before starting clinical care. When appropriate, outcome
probabilities should be discussed based on the scientific literature and personal experience. Questions such
as "what would you do?" should be answered carefully by restating the advantages, disadvantages, and
probable outcome with the option in question. Treatment simulations are valuable communication adjuncts, but should be used carefully to avoid creating
unrealistic expectations.
FINANCIAL CONCERNS
The cost of care is frequently a concern, and must
be fully discussed before treatment. This is especially
true given the escalating hospital costs and diminishing
insurance coverage for orthognathic surgery. Poor
communication may result in the orthodontist unilaterally preparing a patient for surgery only to learn thirdparty coverage has changed or is nonexistent. Because
the goals of orthodontic preparation for surgery are
generally the opposite of camouflage, this may leave
the individual with an orthodontic result that has exaggerated the malocclusion.
Factors Affecting Outcome
The evaluation of treatment outcome can be elusive,
but is typically done using a combination of subjective
and objective criteria. Although there are objective
analyses to scrutinize functional change as well as the
accuracy and stability of the outcome, the assessment
of facial attractiveness and body image tends to be less
structured. In addition to feedback from the clinicians
involved, other psychosocial factors such as self-perception and peer reaction shape patient's attitudes.
It is not unusual to see diversity of opinion. A clinician may determine the morphologic and functional
result to be excellent, only to have it perceived as less
than satisfactory by the patient. Likewise an individual
may be thrilled with a result considered only fair by
the treating orthodontist and surgeon. Differences in
perception between surgeons, orthodontists, and laypeople have been shown to exist, and further complicate the issue. In a study of facial improvement, Dunlevy et alm found that surgeons tended to favor more
prominent chins and larger anterior-posterior change
when compared with panels composed of the laypeople
and orthodontists. This bias may affect individual pa-
PAUL M. THOMAS
tient evaluation and is likely to be an influence in
research involving outcome assessment.
PSYCHOSOCIAL FACTORS AND ESTHETIC CONCERNS
There is considerable research indicating that dental
and facial esthetic concerns are major motivating factors
for those seeking treatment) H2 The type of treatment
selected (surgery or orthodontic camoflage) is related
more to body image or self-perception than morphometric discrepancy. Bell et al ~3 found that patients who opt
for surgery tend to view themselves as being at the
extremes of the profile classification. Paradoxically, objective analysis could not distinguish between their malocclusion and that of patients selecting orthodontic camouflage. These findings were further supported in a
study of facial attractiveness involving females who
have Class II malocclusions. ~4Those selecting a surgical
option tested as having more indicators of global psychologic stress and problems with self-esteem. As in
Bell's study, conventional cephalometric analyses could
not discriminate between patients opting for surgery
versus those selecting orthodontic camouflage. The bottom line would seem to be that the psychosocial factors
of self-perception and body image are of significance
in selecting a course of treatment.
FUNCTIONAL AND MORPHOMETRIC FACTORS
Although morphometric analysis is a poor indicator
of which patient will select surgery versus orthodontic
camouflage, it does provide useful insight into the likelihood of correction with each option. Previous efforts
at establishing numerical guidelines have been directed
primarily at defining the limits for application of a
given treatment option. For example, the "envelope
of discrepany" described by Proffit and Ackerman 15
graphically illustrates their best estimate of the maximum change possible with growth guidance, orthodontic camouflage, and orthognathic surgery. The description is limited to the sagittal and vertical dimension
changes in incisor position, without concern for other
modifying factors. Although this concept is useful to
describe the extremes, it lacks the detail necessary for
decision-making in borderline patients. Additional recommendations have been made for patients with Class
II malocclusions beyond the adolescent growth spurt.
Based on an evaluation of treatment outcome, Proffit
et a116 suggested that orthodontic correction becomes
unlikely in a situation with the following characteristics: an overjet beyond 10 mm; a facial height greater
than 125 nun; a mandibular body length less than 70
ram; and pogonion being located more than 18 mm
behind a nasion perpendicular.
Given these guidelines, a stereotype of the acceptable orthodontic camouflage patient begins to emerge.
The posterior occlusal discrepancy should not be
58"1
greater than the width of a premolar because overjet
correction is usually achieved through retraction of the
upper anterior teeth after premolar extraction. The odds
of successful treatment are further improved if the molar relationship is less than full Class II. This allows for
the loss of some maxillary posterior anchorage without
jeopardizing incisor retraction. A short facial height
with increased overbite is beneficial. Because molar
extrusion is common during mechanotherapy, the accompanying bite opening is less likely to risk loss
of anterior contact and diminish chin projection from
clockwise rotation (Fig 1).
Nonextraction treatment of the lower arch is generally
desirable, when possible. If there is mild to moderate
crowding, with upright incisors and good periodontal
support, the lower arch can be expanded and the incisors
proclined during leveling and alignment. This further reduces the amount of maxillary incisor retraction needed
to correct the overjet. On the other hand, an accentuated
curve of Spee, skeletal asymmetry with midline deviation, pre-existing incisor proclination, and severe crowding all indicate the need for extraction. This increases the
likelihood of lower incisor retraction, which accordingly
reduces the probability of overjet correction.
Facial esthetic outcome is influenced by the proportional relationships of the nose, lips, and chin, as well
as the chin to neck contour. Lip retraction increases
the dominance of the nose and chin as soft tissue facial
features. It follows that the pretreatment facial proportions must be considered in selecting the appropriate
treatment option. The amount of lip support lost with
incisor retraction is a function of tissue tonus, thickness, lip competence, and incisor torque (Figs 2A-2G).
Given the proper soft tissue relationships, incisor
retraction may have a negligible effect on lip support.
If chin prominence is a concern, advancement genioplasty offers a less costly, less risky, alternative to
enhance facial esthetics. Augmentation can be done
under deep sedation on an outpatient basis to further
control expense. The esthetic outcome may be equally
acceptable in the eyes of the patient, while avoiding
the expense and potential morbidity of a more comprehensive operative procedure (Figs 2H and 2I).
To summarize, the desireable camouflage candidate
would meet the following criteria: an end-to-end posterior occlusion; an average or short facial height, with
some increase in overbite; mild to moderate mandibular crowding without excessive curve of Spee or incisor
compensation; periodontal support that will allow
expansion and proclination of the lower anterior teeth
without risk of compromise; and soft tissue relationships that are reasonably proportional and likely to
respond favorably to tooth movement.
Advancing the Case for Camouflage
It has been suggested that the actual choice of treatment in borderline cases may be largely a function
582
ORTHODONTIC CAMOUFLAGE VS ORTHOGNATHIC SURGERY
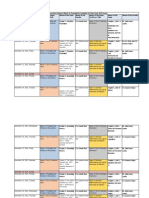
FIGURE 1. A, Normal facial proportions are evident in this frontal view of the patient. The slightly high smile line is a function of the lip
elevating over procumbent incisors during animation. B, In this profile view an acute nasolabial angle suggests that a component of maxillary
protrusion contributes to the Class II malocclusion. C, D, E, The maxillary and mandibular arches are well-formed with no crowding to suggest
the need for extraction. The full Class II malocclusion, with l0 mm of oveljet, will require extraction for camouflage, however, and is at the
limit of orthodontic correction.
o f which specialist the patient happens to contact. 17 Although somewhat tongue-in-cheek, this statement, in reality, m a y be disturbingly accurate. W i l m o t et al analyzed
a series of dentofacial patients' motivations for orthodontic or surgical treatment and examined the association
of these motivations with the severity of the skeletal
malocclusion. Patients in this study, especially those with
Class II relationships, were more motivated for orthodontic treatment than surgery. This is not surprising because
most individuals would prefer the least invasive treatment
that might address their concerns. In keeping with the
findings previously mentioned, there was tittle relationship between the cephalometric variables and motivations
for treatment. These findings, coupled with other research
on psychosocial and morphometric factors, offer some
guidelines that m a y be useful in a clinical setting. Epidemiologic, functional and economic information adds further support for the proposition that camouflage should
be given seriou~ consideration in a majority of postpubertal Class II patients.
PAUL M. THOMAS
583
FIGURE 1 (Cont'd). F, The cephalometric schematic confirms
horizontal maxillary excess and proclined maxillary incisors, in addition to an ample soft tissue chin contour. G, A computer-assisted
treatment simulation suggests that orthodontic camouflage will produce a satisfactory esthetic result. The plan demonstrated involves
extraction of the maxillary first premolars followed by maximum
anchorage retraction of the anterior teeth.
EPIDEMIOLOGY
Proffit et al have suggested that successful orthodontic
camouflage becomes much less likely when the oveqet
is greater than 10 mm. Public health surveys of teenage
malocclusion indicate only 1.6% of those examined
would fall into this category.~ If the criteria for increased
facial height are used, some extrapolation from the public
health data is necessary. Increased facial height (vertical
growth pattern) is often accompanied by diminished
overbite or openbite and clockwise rotation of the mandible. Because no cephalometric data are included in the
public health information, overbite statistics must be substituted. Only 5.2% of the youths surveyed had edge to
edge or openbite relationships of the anterior teeth. The
percentage increases to 16.2 in African American teens.
Because the openbite is frequently combined with bialveolar protrusion in these individuals, correction with
extraction and orthodontics is generally successful. Using
the criteria suggested by Proffit et al, epidemiologic studies indicate the group of patients with Class II malocclusions requiring surgery on a morphologic basis is relatively small.
FUNCTIONAL IMPROVEMENT
The desire for functional improvement is often cited
as the justification for seeking surgical correction) 2
Advocates suggest that improved biomechanics and
masticatory efficiency result from surgical correction.
584
ORTHODONTIC CAMOUFLAGE VS ORTHOGNATHIC SURGERY
FIGURE 2. A, This frontal view suggests relatively normal transverse and vertical facial proportions. B, Mandibular deficiency is
evident on the profile view. Maxillary lip support is within normal
limits. C, D, E, The crowding in the lower dental arch suggests that
extraction may be necessary. Expansion is likely to procline the
incisors beyond the limits of good periodontal support. The occlusal
relationships and overjet are actually less severe than seen in the
patient in Figure 1 due to forward drift of the posterior mandibular
teeth. Correction, however, would require extraction in both arches,
with the likelihood of lower incisor retraction and residual overjet.
F, The cephalometric tracing shows components of both maxillary
protrusion and mandibular deficiency. The maxillary incisors are
already slightly upright and further retraction is best avoided.
PAUL M. THOMAS
585
FIGURE 2 (Cont'd). G, Treatment simulation confirms the undesireable profile changes that would result from orthodontic camouflage.
The nasolabial angle is markedly obtuse and there is inadequate chin projection. H, An advancement genioplasty helps with profile appearance
in the orthodontic camouflage simulation, but the lips are still undersupported. This may be an acceptable alternative, depending on the patient's
concerns and motivation for seeking treatment. L This computer-assisted treatment simulation demonstrates the result from extraction of the
lower first premolars, space closure, and surgical advancement of the mandible. The soft tissue relationships have better balance in the noselip-chin region.
586
ORTHODONTIC CAMOUFLAGE VS ORTHOGNATHICSURGERY
Much of the research in this area has involved bite
force measurement because it is relatively easy to record and analyze. ~8 Unfortunately, bite force does not
correlate with chewing efficiency and has little to do
with improved masticatory function) 9 For all the rhetoric regarding function, there is limited research involving changes in masticatory efficiency after orthognathic surgery. The existing studies deal with
prognathic patients and report no significant improvement in postoperative efficiency.2 In fact, in one report, the number of occlusal contacts decreased with
treatment, as did efficiency when compared with pretreatment and untreated prognathic controls. 2~ Although Class II malocclusion is a much more common
finding, this author is unaware of any research reporting changes in masticatory efficiency after treatment. Suggestions of improvement are subjective at
best or anecdotal in nature.
ECONOMIC FACTORS
Given the rhetoric surrounding the issue of healthcare delivery reform, the cost of treatment is a major
concern for both patient and provider alike. In 1987,
Dolan et a122reported the mean hospital cost (exclusive
of anesthesia professional fees) associated with a mandibular sagittal split osteotomy as being $3,086 with
a range from $1,997 to $4,561. These figures are for
a university hospital in central North Carolina and regional costs are likely to vary widely. Because the
study was conducted with data from patients treated
in 1985, inflation also must be considered for these
figures to be useful. The investigators cited the 1985
escalation of healthcare expenditures as about 9%, but
cautioned that this was the lowest annual increment
since 1965. Based on Consummer Price Index data
from the Bureau of Labor Statistics, hospital-related
charges have increased 150.4% in the 11-year period
from 1982 to 1993. 23 Using this 13.6% per year increment, the 1994 hospital charges for the same institution
could be in excess of $10,000 exclusive of all professional fees.
A recent survey indicated that the charges for a mandibular sagittal split osteotomy ranged from $1,500 to
$11,000, with an average fee of about $4,400. 24 The
assistant surgeon's fee also must be considered and is
usually about 20% to 25% of the surgeon's bill. These
figures are consistent with average fees from this author's locale. Orthodontic fees range from $3,000 to
$5,000 and anesthesiologist's fees from $600 to $900. 25
This brings the potential total expense for mandibular
advancement in a hospital setting to ($21,000). Greater
overhead expense is likely to make this figure considerably higher in selected locations. Using the same
sphere of reference, the surgical option is at least three
to four times the cost of orthodontic camouflage. Certainly this underscores the need for careful consider-
ation of the perceived benefit from orthognathic surg e r y versus the cost and risk.
Summary and Conclusions
Clearly, there are postpubertal patients with Class
II malocclusions for whom orthognathic surgery combined with orthodontics is the " b e s t " option, but epidemiologic information suggests they are a relatively
small percentage of the potential patient pool. The majority of patients fall into either an orthodontic treatment group or a borderline category. Many of these can
be treated successfully with orthodontic camouflage.
Research has shown psychosocial factors play a major
role in determining the patient's selection of a treatment option. This emphasizes the need for careful attention to global psychologic factors, with special emphasis on patient concerns regarding body image.
Morphometric criteria have been offered describing
appropriate candidates for orthodontic camouflage.
These are supported by a combination of research and
clinical experience. Patients who do not fit these criteria should not automatically be considered candidates
for surgery. Psychosocial research suggests a percentage of these individuals place less importance on facial
change and are content to improve dental esthetics and
function to the degree possible.
To assist in the decision-making process, patients
should be given the best information available regarding potential outcome. Currently this may involve
treatment simulation using a combination of computer
images and dental models. Caution has been suggested,
given the variability associated with predicting soft
tissue change. 26 There are additional legal concerns
regarding the implied guarantee of treatment outcome. 22'27 Correspondingly, the influence of this technology must be kept in perspective. Recent research
on the decision-making process found computer imaging to be an important factor in only 24% of the
patients studied. 28 However, the value of this technology for communication was underscored when these
same individuals ranked computer simulation as the
best information source when considering all diagnostic records.
The future of orthognathic surgery is uncertain,
given the current climate surrounding health care in
general. Coverage is being specifically excluded as
many patients change to low option policies or managed care plans. For those still having coverage, the
process of gaining prior approval has become increasingly stringent and slow. For those without coverage,
there is a trend toward developing "package deals"
to make care more affordable. It would appear that
although the demand for treatment will continue, the
orthognathic surgery option may become less feasible
and orthodontic camouflage more frequent. It continues to be imperative that we discuss treatment options
PAUL M. THOMAS
with our patients in an honest and forthright manner
to t h e b e s t o f o u r a b i l i t y . T h e i n f o r m a t i o n s h o u l d b e
free from personal bias and should incorporate the advantages and disadvantages of various options, including risk and economic information. Only then will our
patients be able to make a truly informed decision.
References
1. Kelly JE: An assessment of the occlusion of the teeth of youths
12-17 years, United States. Vital and Health Statistics, Data
from the National Health Survey, Series l l-Number 162,
February 1977, p 3
2. Profit WR, Field HW: Malocclusion and dentofacial deformity
in contemporary society, in Contemporary Orthodontics. St
Louis, MO, Mosby, 1993, pp 7-8
3. Witzig TW, Yerkes I: Functional jaw orthopedics; Mastering
more than technique, in Gelb H (ed): Clinical Management
of Head Neck and TMJ Pain and Dysfunction (ed 2) Philadelphia, PA, Saunders, 1985
4. Owen AH: Orthodontic/orthopedic treatment of craniomandibular dysfunction. Part 2. Posterior condylar displacement. J
Craniomandibular Prac 2:344, 1984
5. Kiyak HA, Bell R: Psychosocial considerations in surgery and
orthodontics, in Proffit WR, White RP Jr (eds): Surgical Orthodontic Treatment. St Louis, MO, Mosby, 1991, pp 71-96
6. Nelson C, Harkness M, Herbison P: Mandibular changes during
functional appliance treatment. Am J Orthod Dentofac Orthod
104:153, 1993
7. Thomas PM: Unpublished data, University of North Carolina
Dentofacial Program
8. Ackerman JL, Profit WR: The characteristics of malocclusion:
A modern approach to classification and diagnosis. Am J
Orthod 75:282, 1969
9. Weed LL: Medical records, medical education and patient care:
The problem-oriented record as a basic tool. Cleveland, OH,
1969, Case-Western Reserve Press
10. Dunlevy HA, White RP, Profit WR, OH, et al: Professional
and lay judgement of facial esthetic changes following orthognathic surgery. J Adult Orthod Orthognath Surg 2:151, 1987
11. Mayo KH, Dryland-Vig KWL, Vig PS, et al: Attitude variables
of dentofacial deformity patients: Demographic characteristics and associations. J Oral Maxillofac Surg 49:594, 1991
58"/
12. Flanary CM, Barnwell GM, Alexander JM: Patient perceptions
of orthognathic surgery. Am J Orthod 88:137, 1985
13. Bell R, Kiyak HA, Joondeph DR, et al: Perceptions of facial
profile and their influence on the decision to undergo orthognathic surgery. Am J Orthod 88:232, 1985
14. Griffin TJ: Perception of facial attractiveness and esthetic treatment goal preferences by patients, peer group, and professionals. Master's Thesis, University of North Carolina, 1994
15. Profit WR, Ackerman JL: Diagnosis and treatment planning,
in Graber TM, Vanarsdall RL Jr (eds): Orthodontics: Current
Principals and Treatment. St Louis, MO, Mosby, 1994
16. Profit WR, Phillips C, Tulloch JFC, et al: Surgical versus orthodontic correction of skeletal class II malocclusion in adolescents: Affects and indications. Int J Adult Orthod Orthog
Surg 7:209, 1992
17. Cassidy DW Jr, Herbosa EG, Rotskoff KS, et al: A comparison
of surgery and orthodontics in borderline adults with class
II, division I malocclusions. Am J Orthod Dentofac Orthop
104:455, 1993
18. Profit WR: Masticatory performance, muscle activity, and occlusal force in preorthognathic surgery patients: Discussion.
J Oral Maxillofac Surg 52:482, 1994
19. Tate GS, Throckmorton GS, Ellis E III, et al: Masticatory performance, muscle activity and occlusal force in preorthognathic
surgery patients. J Oral Maxillofac Surg 52:476, 1994
20. Shiratsuchi Y, Kouno K, Tashiro H: Evaluation of masticatory
function following orthognathic surgical correction of mandibular prognathism. J Cranio Max Fac Surg 19:299, 1991
21. Kobayashi T, Honma K, Nakajima T, et al: Masticatory function
in patients with mandibular prognathism before and after
orthognathic surgery. J Oral Maxillofac Surg 51:997, 1993
22. Dolan P, White RP Jr, Tnlloch JFC: An analysis of hospital
charges for orthognathic surgery. Int J Adult Orthod Orthog
Surg 1:9, 1987
23. Williams KR, Bentley JE: Survey findings on dental fees: A
comparison from 1982-93. J Am Dent Assoc 125:1260, 1994
24. Networker feedback: Survey of selected fees. American College
of Oral and Maxillofacial Surgeons Newsletter, October 1993
25. Personal Communication: Durham Anesthesia Associates, Durham, NC
26. Turpin DL: Computers coming on line for diagnosis and treatment planning. Angle Orthod 60:163, 1990 (editorial)
27. Sarver DM: Video imaging: The pros and cons. Angle Orthod
63:167, 1993
28. Hill B: Influence of video imaging on patients' expectations.
Master's Thesis, University of North Carolina, 1993
Anda mungkin juga menyukai
- K Schleich Pharmacotherapy of Osteoporosis 2017 AUDIENCEDokumen32 halamanK Schleich Pharmacotherapy of Osteoporosis 2017 AUDIENCEBenjamin NgBelum ada peringkat
- NCCS Understanding Radiation Therapy (Eng)Dokumen20 halamanNCCS Understanding Radiation Therapy (Eng)Benjamin NgBelum ada peringkat
- Osteoporosis UpdateDokumen57 halamanOsteoporosis UpdatepuskesbinangunBelum ada peringkat
- Osteoporosis UpdateDokumen57 halamanOsteoporosis UpdatepuskesbinangunBelum ada peringkat
- Trauma ATACC Manual 2014 PDFDokumen460 halamanTrauma ATACC Manual 2014 PDFBenjamin Ng100% (1)
- BCA - Home GuidelineDokumen54 halamanBCA - Home GuidelineJan Kristoffer Aguilar UmaliBelum ada peringkat
- 4 Listgarten M. Electron Microscopic Study of The Gingivodental Junction of Man. Am J Anat 1966 119-147 (HWN)Dokumen31 halaman4 Listgarten M. Electron Microscopic Study of The Gingivodental Junction of Man. Am J Anat 1966 119-147 (HWN)Benjamin NgBelum ada peringkat
- Facial Trauma Clinical ExaminationDokumen10 halamanFacial Trauma Clinical ExaminationBenjamin NgBelum ada peringkat
- Travelshield DBSDokumen12 halamanTravelshield DBSBenjamin NgBelum ada peringkat
- Life Expectancy of Patients With Malignant Pleural Effusion Treated With Video-Assisted Thoracoscopic Talc PleurodesisDokumen6 halamanLife Expectancy of Patients With Malignant Pleural Effusion Treated With Video-Assisted Thoracoscopic Talc PleurodesisBenjamin NgBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Viscosity IA - CHEMDokumen4 halamanViscosity IA - CHEMMatthew Cole50% (2)
- Range of Muscle Work.Dokumen54 halamanRange of Muscle Work.Salman KhanBelum ada peringkat
- Thick Seam Mining Methods and Problems Associated With It: Submitted By: SAURABH SINGHDokumen13 halamanThick Seam Mining Methods and Problems Associated With It: Submitted By: SAURABH SINGHPrabhu PrasadBelum ada peringkat
- Genigraphics Poster Template 36x48aDokumen1 halamanGenigraphics Poster Template 36x48aMenrie Elle ArabosBelum ada peringkat
- Rustia V Cfi BatangasDokumen2 halamanRustia V Cfi BatangasAllen GrajoBelum ada peringkat
- Format For Handout - Comparative Models of EducationDokumen5 halamanFormat For Handout - Comparative Models of EducationAdrian AsiBelum ada peringkat
- Feyzin Oil Refinery DisasterDokumen8 halamanFeyzin Oil Refinery DisasterDavid Alonso Cedano EchevarriaBelum ada peringkat
- Geomatics Lab 6 (GPS)Dokumen24 halamanGeomatics Lab 6 (GPS)nana100% (1)
- Chapter 1-The Indian Contract Act, 1872, Unit 1-Nature of ContractsDokumen10 halamanChapter 1-The Indian Contract Act, 1872, Unit 1-Nature of ContractsALANKRIT TRIPATHIBelum ada peringkat
- CVR College of Engineering: UGC Autonomous InstitutionDokumen2 halamanCVR College of Engineering: UGC Autonomous Institutionshankar1577Belum ada peringkat
- Demo TeachingDokumen22 halamanDemo TeachingCrissy Alison NonBelum ada peringkat
- Volume 4-6Dokumen757 halamanVolume 4-6AKBelum ada peringkat
- New Wordpad DocumentDokumen6 halamanNew Wordpad DocumentJonelle D'melloBelum ada peringkat
- American Literature TimelineDokumen2 halamanAmerican Literature TimelineJoanna Dandasan100% (1)
- Latihan Soal Recount Text HotsDokumen3 halamanLatihan Soal Recount Text HotsDevinta ArdyBelum ada peringkat
- Infineum Ilsa Gf-6 API SP e JasoDokumen28 halamanInfineum Ilsa Gf-6 API SP e JasoDanielBelum ada peringkat
- Single-phase half-bridge inverter modes and componentsDokumen18 halamanSingle-phase half-bridge inverter modes and components03 Anton P JacksonBelum ada peringkat
- Biology 11th Edition Mader Test BankDokumen25 halamanBiology 11th Edition Mader Test BankAnthonyWeaveracey100% (44)
- G10 - Math - Q1 - Module 7 Grade 10Dokumen12 halamanG10 - Math - Q1 - Module 7 Grade 10Shua HongBelum ada peringkat
- Rigor Mortis and Lividity in Estimating Time of DeathDokumen2 halamanRigor Mortis and Lividity in Estimating Time of DeathfunnyrokstarBelum ada peringkat
- HDL Coder™ ReferenceDokumen487 halamanHDL Coder™ ReferenceVictor Colpo NavarreteBelum ada peringkat
- Gender and Other Cross Cutting Issues Mental HealthDokumen6 halamanGender and Other Cross Cutting Issues Mental HealthJamira Inoc SoboBelum ada peringkat
- Inbound 8511313797200267098Dokumen10 halamanInbound 8511313797200267098phan42Belum ada peringkat
- Captive Screws - Cap Head: Hex. SocketDokumen5 halamanCaptive Screws - Cap Head: Hex. SocketvikeshmBelum ada peringkat
- Pyrolysis ProjectDokumen122 halamanPyrolysis ProjectSohel Bangi100% (1)
- EMA Guideline on Calculating Cleaning LimitsDokumen4 halamanEMA Guideline on Calculating Cleaning LimitsshivanagiriBelum ada peringkat
- Participatory Assessment of Ragay Gulf Resources and SocioeconomicsDokumen167 halamanParticipatory Assessment of Ragay Gulf Resources and SocioeconomicsCres Dan Jr. BangoyBelum ada peringkat
- ATM ReportDokumen16 halamanATM Reportsoftware8832100% (1)
- Harajuku: Rebels On The BridgeDokumen31 halamanHarajuku: Rebels On The BridgeChristian Perry100% (41)
- IT Technician CVDokumen3 halamanIT Technician CVRavi KumarBelum ada peringkat