Bookshelf NBK361 PDF
Diunggah oleh
Sri RahayuJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Bookshelf NBK361 PDF
Diunggah oleh
Sri RahayuHak Cipta:
Format Tersedia
4
The Physical Examination
EARL W . CAMPBELL, JR ., and CHRISTOPHER K . LYNN
Definition
The Materials
Physical examination is the process of evaluating objective
anatomic findings through the use of observation, palpation, percussion, and auscultation . The information obtained must be thoughtfully integrated with the patient's
history and pathophysiology . Moreover, it is a unique situation in which both patient and physician understand that
the interaction is intended to be diagnostic and therapeutic .
The physical examination, thoughtfully performed, should
yield 20% of the data necessary for patient diagnosis and
management .
The single most useful device for optimal performance of
the physical examination is an inquisitive and sensitive mind .
Next most useful is mastery of the techniques of observation, palpation, percussion, and auscultation . Less important are the tools required for the examination (Table 4 .1) .
The Examination
As the environment affects the quality of the physical examination, it is wise to arrange for quiet and privacy, darkening the room for parts of the examination, and comfort
for the patient and examiner .
The complete examination should proceed in an orderly
fashion with a minimum of required position shifts by the
patient (Table 4 .2) . On the other hand, the physician must
be able to ascertain the integrity of the various organ systems
from regional examinations . For instance, from examination of the head and neck, the physician must identify the
vascular, neurologic, lymphatic, skeletal, and integumentary components and must relate them to their complements
in other body regions . It would be tedious, by contrast, to
examine the vascular system in its entirety, followed by a
complete neurologic examination and the other organ systems each in turn . When examining an anatomic region,
the observer must be alert to the appearance of any abnormality and question at the time the morphologic aspects
of the abnormality and its clinical significance .
The general physical examination can take many forms
depending upon circumstances . Most often, the examiner
evaluates body regions in a general way, looking for abnormalities . Clues derived from the history signal the need
for a more precise and detailed examination of a given
system . A thorough physical examination often includes the
sequence presented in Table 4 .3 .
The clinically significant physical examination is a flexible entity that should vary with the needs of the patient .
Periodic examinations for health assessment need to be
The Context
Almost without exception, some medical history about the
patient is available at the time of the physical examination .
Rarely, there may be no history, or at best brief recordings
of acute events . Information pertinent to the physical examination can be learned from observation of speech,
gestures, habits, gait, and manipulation of features and extremities . Interactions with relatives and staff are often revealing . Pigmentary changes such as cyanosis, jaundice, and
pallor may be noted . Diaphoresis, blanching, and flushing
may provide clues about vasomotor tone related to mood
or physiologic abnormalities . Aspects of patient habits, interests, and relationships can be ascertained from pictures,
books, magazines, and personal objects at the bedside .
The Physician-Patient Interaction
Aside from the hospital room and office, physical examination may occur in a variety of other settings where it is
difficult to establish privacy and quiet . The best resource
available to the physician to set the stage for the physical
examination is to communicate respect and a genuine interest
in the patient's welfare . The patient should be addressed
politely and asked to perform the required maneuvers of
the examination, a technique far preferable to imperative
language such as, "I want you to Patients should be
prepared for unpleasant portions of the examination .
Aside from explanations and reassurance, it is not necessary to maintain a continuous conversation with the patient
during the examination . Avoid embarrassing the patient .
Be certain that draping material is used appropriately and
that personal areas are not subjected to undue exposure .
An examination that ends abruptly may diminish the value
of the doctor-patient relationship and may destroy its therapeutic content . The patient may benefit from a brief summary of relevant findings and may require reassurance about
what has and has not been found .
Table 4.1
Equipment Required for the Physical Examination
Cotton wisp
Flashlight
Lubricating jelly
Mydriatic solution
Oto-ophthalmoscope
Paper towels
Pocket eye chart
Rectal gloves
Reflex hammer
37
Sphygmomanometer
Stethoscope
Tape measure
Thermometer
Tissues
Tongue depressors
Tuning fork (128 Hz)
Vials of coffee and cinnamon
38
I . INTRODUCTION
Table 4 .2
Positions of Patient and Examiner during the Physical Examination
Anatomical area or activity
Patient
Vital signs, general inspection
Head and neck
Anterior torso
Posterior torso
Anterior chest and abdomen
Male genitalia
Gait, station, coordination
Sitting or reclining
Sitting
Sitting
Sitting
Supine
Standing
Variable positions
Female genitalia
Reclining on examining table, draped, knees
flexed, legs adducted, feet in stirrups
Examiner
Standing before patient or at bedside
Standing before patient
Standing before patient initially, later behind
the patient
At patient's side
Before the patient
Before the patient
Behind the patient
Sitting on stool at times or standing
Table 4.3
Steps of the Physical Examination
1 . Patient's comfort
Be certain that the patient is in a relaxed position, properly gowned or draped .
2 . The optimal environment
The examination surface should be at a height appropriate for the examiner . Light sources and curtains should be optimally
arranged . Television sets, radios, and other noisy distractions should be eliminated .
3 . Vital signs and general inspection
Evaluate the radial pulse for rate and rhythm . Measure brachial blood pressure . Inspect nails, skin, and hair. Note the general
appearance, body habitus, hair distribution, muscle mass, movement coordination, odors, and breathing pattern .
4 . Head
a . Eyes : Examine the conjunctiva, sclera, cornea, and iris of each eye . Test pupils for irregularity, accommodation, and reaction .
Evaluate visual fields and visual acuity (cranial nerve II) . Assess extraocular movements (cranial nerves III, IV, VI) . Test the
corneal reflex (cranial nerve V) .
b. Ears : Examine the pinnae and periauricular tissues . Test auditory acuity, perform Weber and Rinne maneuvers (cranial nerve
VIII) .
c . Ophthalmo-otoscopy : The ophthalmoscope can now be used after darkening the room to examine the interior of the eye through
the pupillary aperture . Particular emphasis should be placed on the retina, optic disc, vessels, and macula lutea . Attention must
be given to the media, lens, and cornea . Keeping the room darkened, attach the otoscope head and observe the auditory canals
and tympani .
d. Nose : Connect the nasal speculum to the otoscope and examine the nares, noting the condition of the mucosa, septum and
turbinates .
e. Mouth : Examine the vermilion border, the oral mucosa, the tongue . Identify the salivary duct papillae . Assess the dentition for
decay, repair, condition of bite . View the pharynx . Evaluate the function of cranial nerves IX, X, and XII . If appropriate,
evaluate sensory divisions of cranial nerves V, VII .
f . Face : Evaluation of symmetry, smile, frown, and jaw movement will provide information about motor divisions of cranial nerves
V and VII .
5 . Neck
Palpate the neck with emphasis on the salivary glands, lymph nodes, and thyroid . Look for tracheal deviation . Identify the carotid
arteries and auscultate for bruits . Note jugular venous distention . Reexamine the thyroid from behind the patient . Certain parts of
evaluation of this area, jugular venous filling, may warrant review with the patient reclining . Test shoulder strength of the
sternocleidomastoid and trapezius muscles (cranial nerves XI and XII) .
6 . Anterior torso
With the patient sitting, examine the epitrochlear and axillary nodes . Examine the breasts . Define the PMI and examine the heart,
having the patient lean forward if necessary .
7 . Posterior torso
Observe for spinal curvature or chest deformity . Evaluate the vertebral column and the costovertebral areas . Auscultate the
posterior and lateral lung fields .
8 . Completion of the "sitting" portion of the examination
Evaluate proximal and distal motor strength, deep tendon reflexes, distal pulses and sensation .
9. With the patient supine
a . Thorax : Examine the breasts ; reexamine the heart, turning the patient to the left lateral decubitus position if appropriate .
Auscultate the anterior lung structures.
b. Abdomen : After inspection, auscultate, listening for bowel sounds and bruits . Next inspect, percuss, and palpate the abdomen,
taking special notice of hepatic or splenic enlargements .
c . Proximal lower extremities : Examine the inguinal, femoral, and popliteal regions for adenopathy and pulses . Evaluate range of
motion of hips, knees, and ankles.
10. With the patient standing
Examine external genitalia of the male . In both male and female, evaluate station and gait.
11 . Pelvic and rectal examination
In females, the pelvic examination should be performed on an examining table provided with stirrups . Rectal examination and
occult blood testing should be done simultaneously . In males, the rectal examination is best performed with the patient in the bent
forward position .
4.
THE PHYSICAL EXAMINATION
comprehensive, as do most hospital admission examinations . In contrast, it will not be cost effective to undertake
a complete physical examination in most patients presenting
with symptoms of an upper respiratory tract infection or a
urinary tract infection .
Conclusion
The physical examination is a key part of a continuum that
extends from the history of the present illness to the therapeutic outcome . If the history and physical examination
are linked properly by the physician's reasoning capabilities,
laboratory tests should in large measure be confirmatory .
The physical examination, however, can be the weak link
in this chain if it is performed in a perfunctory and superficial manner. Understanding the pathophysiologic mechanism of a physical abnormality is essential for correct
diagnosis and management . For instance, the failure to discriminate between and know the origin of carotid bruits
and transmitted sounds of valvular origin can have critical
significance .
As knowledge of disease changes, the techniques of physical examination become augmented . The astute physician
constantly reviews and adds to the repertoire of techniques
for physical examination .
Evaluation of the physical examination in terms of sensitivity and specificity is difficult . Interpretation of isolated
physical findings is often influenced by the presence or
absence of historical information and coexisting physical
findings . For instance, the assessment of whether clubbing
of the fingers is present or absent has significant interobserver variability and has been demonstrated to be influenced by the clinical appearance of the patient.
A number of studies have attempted to look at the validity of the physical exam as a diagnostic tool . The concept
of interobserver and intraobserver variability has been introduced when looking at specific isolated findings . For
example, judging the presence or absence of rales is more
39
likely to be agreed upon by several observers and on repeated exams by a single blinded observer, than is the graded
intensity of breath sounds . The presence or absence of ascites in patients with known liver disease has been shown
to be difficult to determine when using physical exam techniques alone . The bedside measurement of forced expiratory time by auscultation however, has been shown to have
a small interobserver variability in trained observers and to
have clinical value in following the degree of airway obstruction .
Because of the large degree of variability in observing
many physical signs, the following recommendations can be
made when reporting and interpreting physical findings .
1 . Emphasis should be placed on dichotomous variables
(i .e ., presence or absence of rales) rather than on
graded variables (i .e ., intensity of breath sounds) .
2 . Some physical signs (i .e ., clubbing of the fingers) represent a continuum from obviously normal to obviously abnormal. Emphasis should be placed on those
findings which represent the extremes rather than
the "borderline" cases .
3 . Recognition of those physical findings which have a
high degree of interobserver variability is important .
Good examples of this include detection of moderate
or small amounts of ascitic fluid and detection of diaphragmatic movement by percussion . These findings
should be deemphasized in favor of those with better
reproducibility.
4. It is beneficial to use the body's "symmetry" to advantage . Differences auscultated in breath sounds between similar area of the right and left lung are far
more clinically important than an overall decrease in
breath sounds .
If these points are kept in mind, the physical exam will
fill its proper role in the care of the patient. That is as an
adjunct to a thorough history and as a way for the physician
to interact physically with the patient .
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Sistem Persyarafan: Sri Rahayu, S.kep., NersDokumen4 halamanSistem Persyarafan: Sri Rahayu, S.kep., NersSri RahayuBelum ada peringkat
- Saurabh Raj JainDokumen2 halamanSaurabh Raj JainSri RahayuBelum ada peringkat
- Loker Bahasa InggrisDokumen9 halamanLoker Bahasa InggrisSri RahayuBelum ada peringkat
- Bahan 1Dokumen23 halamanBahan 1Sri RahayuBelum ada peringkat
- Jurnal Breast FeedingDokumen1 halamanJurnal Breast FeedingSri RahayuBelum ada peringkat
- 225 - Pengaruh Pijat Oksitosin Terhadap Produksi Asi Ibu Postpartum Di BPM Wilayah Kabupaten KlatenDokumen6 halaman225 - Pengaruh Pijat Oksitosin Terhadap Produksi Asi Ibu Postpartum Di BPM Wilayah Kabupaten KlatenNilza CuemachynxkamoeclmanyaBelum ada peringkat
- Postpartum Care for a 28-Year-Old Woman with Uterine Atony in BPS Yuli, SidoarjoDokumen98 halamanPostpartum Care for a 28-Year-Old Woman with Uterine Atony in BPS Yuli, SidoarjoSri RahayuBelum ada peringkat
- 1 Kuzma Et Al. Food Taboos Pregnant WomenDokumen11 halaman1 Kuzma Et Al. Food Taboos Pregnant WomenSri RahayuBelum ada peringkat
- Postpartum Care for a 28-Year-Old Woman with Uterine Atony in BPS Yuli, SidoarjoDokumen98 halamanPostpartum Care for a 28-Year-Old Woman with Uterine Atony in BPS Yuli, SidoarjoSri RahayuBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- High Voltage - WikipediaDokumen7 halamanHigh Voltage - WikipediaMasudRanaBelum ada peringkat
- Top Sellers Fall Protection Catalogue 2020 ENDokumen44 halamanTop Sellers Fall Protection Catalogue 2020 ENtcBelum ada peringkat
- Clarifying Questions on the CPRDokumen20 halamanClarifying Questions on the CPRmingulBelum ada peringkat
- R02.4 Standard III (A) - AnswersDokumen11 halamanR02.4 Standard III (A) - AnswersShashwat DesaiBelum ada peringkat
- An Interview - ExercisesDokumen3 halamanAn Interview - ExercisesCarmen GloriaBelum ada peringkat
- Practical Visual Inspection of WeldsDokumen40 halamanPractical Visual Inspection of WeldsAmit Sharma100% (1)
- Oral Dislocation Rehabilitation Program - FirstDokumen2 halamanOral Dislocation Rehabilitation Program - FirstPriyaki SebastianBelum ada peringkat
- Stroke RecoveryDokumen20 halamanStroke RecoveryVanessa SnowBelum ada peringkat
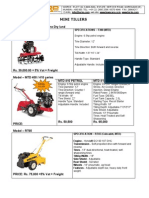
- Optimize soil preparation with a versatile mini tillerDokumen2 halamanOptimize soil preparation with a versatile mini tillerRickson Viahul Rayan C100% (1)
- Strain Gauge Load Cells LPB0005IDokumen2 halamanStrain Gauge Load Cells LPB0005ILordbyron23Belum ada peringkat
- The Payment of Bonus Act 1965 PDFDokumen30 halamanThe Payment of Bonus Act 1965 PDFappu kunda100% (1)
- 1644 CV Europass Daniel MatosDokumen2 halaman1644 CV Europass Daniel MatosDaniel MatosBelum ada peringkat
- 631 500seriesvalves PDFDokumen2 halaman631 500seriesvalves PDFsaiful_tavipBelum ada peringkat
- Anthropometric Measurements Options For Identifying Low Birth Weight Newborns in Kumasi, GhanaDokumen9 halamanAnthropometric Measurements Options For Identifying Low Birth Weight Newborns in Kumasi, GhanaDani KusumaBelum ada peringkat
- Shavuot 5774Dokumen4 halamanShavuot 5774Andrea KingBelum ada peringkat
- Ketamine Drug Study for AnesthesiaDokumen1 halamanKetamine Drug Study for AnesthesiaPRINCESS MARIZHAR OMARBelum ada peringkat
- My Study Plan Guide For AmcDokumen7 halamanMy Study Plan Guide For Amc0d&H 8Belum ada peringkat
- Surface BOP Kill SheetDokumen12 halamanSurface BOP Kill Sheetzouke2002Belum ada peringkat
- Advantest R3131 Spectrum Analyzer Operator ManualDokumen277 halamanAdvantest R3131 Spectrum Analyzer Operator ManualMartin Argay100% (1)
- FAQ For Company Law 2013Dokumen24 halamanFAQ For Company Law 2013Archanat07100% (1)
- Bio Exp 4Dokumen2 halamanBio Exp 4Yi Ling GohBelum ada peringkat
- Cakes Amp Sugarcraft - April-May 2019 EditDokumen45 halamanCakes Amp Sugarcraft - April-May 2019 Editapi-197110397100% (1)
- 22Dokumen22 halaman22vanhau24Belum ada peringkat
- Spiegel Et Al 1999 Psycho OncologyDokumen12 halamanSpiegel Et Al 1999 Psycho Oncologyfatimaramos31Belum ada peringkat
- M Shivkumar PDFDokumen141 halamanM Shivkumar PDFPraveen KumarBelum ada peringkat
- Finding the Right Pharmacy for Your NeedsDokumen4 halamanFinding the Right Pharmacy for Your Needsprabakar VBelum ada peringkat
- ERAS DR - TESAR SP - AnDokumen26 halamanERAS DR - TESAR SP - AnAhmad Rifai R ABelum ada peringkat
- Burns SeminarDokumen66 halamanBurns SeminarPratibha Thakur100% (1)
- Mulching Paper Laying Machine SynopsisDokumen17 halamanMulching Paper Laying Machine SynopsisSiddhesh Zirpe50% (2)
- Register Environmental ImpactsDokumen7 halamanRegister Environmental ImpactsArmand LiviuBelum ada peringkat