Prevalence of Corneal Diseases in The Rural Indian Population The Corneal Opacity Rural Epidemiological CORE Study Ranjith Kumar
Diunggah oleh
angela_karenina_1Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Prevalence of Corneal Diseases in The Rural Indian Population The Corneal Opacity Rural Epidemiological CORE Study Ranjith Kumar
Diunggah oleh
angela_karenina_1Hak Cipta:
Format Tersedia
Downloaded from http://bjo.bmj.com/ on February 2, 2015 - Published by group.bmj.
com
Global issues
Prevalence of corneal diseases in the rural Indian
population: the Corneal Opacity Rural
Epidemiological (CORE) study
Noopur Gupta,1 Praveen Vashist,1 Radhika Tandon,1 Sanjeev K Gupta,2
Sadanand Dwivedi,3 Kalaivani Mani3
1
Dr Rajendra Prasad Centre for
Ophthalmic Sciences, All India
Institute of Medical Sciences,
New Delhi, India
2
Centre for Community
Medicine, All India Institute of
Medical Sciences, New Delhi,
India
3
Department of Biostatistics,
All India Institute of Medical
Sciences, New Delhi, India
Correspondence to
Dr Praveen Vashist,
Dr Rajendra Prasad Centre for
Ophthalmic Sciences, All India
Institute of Medical Sciences,
Room No. 787, 7th oor,
Ansari Nagar, New Delhi
110029, India;
PRAVEENVASHIST@YAHOO.
COM
Received 4 August 2014
Revised 30 September 2014
Accepted 26 October 2014
Published Online First
13 November 2014
ABSTRACT
Objective The present population-based study was
undertaken to estimate the prevalence, determinants and
causes of corneal morbidity and blindness in a rural
North Indian population.
Design Population-based study in India with 12 899
participants of all ages.
Methods Participants were recruited from 25 village
clusters of district Gurgaon, Haryana, India using random
cluster sampling strategy. All individuals were examined
in detail with a portable slit lamp for evidence of any
corneal disease during the door-to-door examination.
Comprehensive ocular examination including logMar
visual acuity, slit lamp biomicroscopy, non-contact
tonometry and dilated retinal evaluation was performed
at a central clinic site in the respective villages.
Results Overall, 12 113 of 12 899 people (93.9%
response rate) were examined during the household
visits. Prevalence of corneal disease was 3.7% (95%
CI 3.4% to 4.1%) and that of corneal blindness was
0.12% (95% CI 0.05% to 0.17%). Multivariable
analysis demonstrated that corneal disease was
signicantly higher in the elderly ( p<0.0001) and
illiterates ( p<0.0001). Common causes of corneal
opacity in the study population were pterygium (34.5%),
ocular trauma (22.3%) and infectious keratitis (14.9%).
Corneal diseases contributing to blindness were postsurgical bullous keratopathy (46.2%) and corneal
degenerations (23.1%).
Conclusions The study ndings demonstrate that
currently ocular trauma, infectious keratitis, post-surgical
bullous keratopathy, and corneal degenerations are
responsible for the major burden of corneal blindness
and morbidity in the Indian population. The prevalence
of corneal morbidity due to vitamin A deciency and
trachoma was low in this rural population.
INTRODUCTION
To cite: Gupta N, Vashist P,
Tandon R, et al. Br J
Ophthalmol 2015;99:147
152.
Corneal blindness, including corneal opacity and
trachoma, contribute to 7% of the blindness
burden globally.1 2 This translates to nearly 2.7
million blind people worldwide due to corneal diseases.2 The global burden of corneal blindness is
concentrated in emerging and developing countries.
The major causes of corneal blindness include
corneal ulceration, ocular trauma, trachoma,
bullous keratopathy, corneal degenerations and
vitamin A deciency. It has been reported that
nearly 90% of the global cases of ocular trauma
and corneal ulceration leading to corneal blindness
occur in developing countries.3 Being a developing
country with a predominantly rural population,
India faces a signicant challenge in eliminating
corneal blindness. A meta-analysis of various
population-based blindness studies conducted in
India demonstrated that the prevalence of corneal
blindness was 0.45% (95% CI 0.27% to 0.64%) in
adults.4
There is an absence of representative communitybased data on the magnitude of corneal diseases in
the general population, especially in North India.
To the best of our knowledge, this study is the rst
of its kind to reect the magnitude of corneal
opacity in a large sample of the Indian population.
Available literature on corneal blindness in India is
either hospital-based5 or extrapolated data from
blindness surveys that were not specically designed
for studying corneal morbidity.612 Hence, this
population-based study provides new insights into
the prevalence, risk factors and causes of corneal
blindness and morbidity across all age groups in a
rural Indian population.
METHODS
Study design and population
The Corneal Opacity Rural Epidemiological
(CORE) study is a cross-sectional study involving
cluster random sampling. It was conducted from
July 2011 to January 2013 to determine the prevalence and determinants of corneal opacity in the
rural regions of Gurgaon district, state of Haryana,
India. A sample size of 9640 was calculated assuming 4% prevalence of corneal opacity,13 design
effect of 2, 0.6% absolute precision, and response
rate of 85%. It was planned to cover a sample of
10 000 people from 25 randomly selected rural
clusters. A computerised simple random sampling
approach was used to select 25 clusters from a sampling frame of 910 clusters generated from the
total rural population of 472 085 from 229 villages
of District Gurgaon.14 The study protocol received
ethical approval from the Institutional Ethics
Committee, All India Institute of Medical Sciences,
New Delhi in April 2010. Written informed
consent for enrolment and examination was
obtained from all adults for their own participation
and from parents or appropriate guardians of all
eligible children before they were included in the
study in accordance with the principles of the
Declaration of Helsinki.
A house-to-house visit was made to each family
in the selected village cluster. All eligible individuals
were examined by an experienced ophthalmologist
for the presence of corneal opacity using a portable
slit-lamp. Individuals detected with corneal
Gupta N, et al. Br J Ophthalmol 2015;99:147152. doi:10.1136/bjophthalmol-2014-305945
147
Downloaded from http://bjo.bmj.com/ on February 2, 2015 - Published by group.bmj.com
Global issues
opacication during the house-to-house examination were
invited for a detailed ocular examination at a temporary makeshift clinic utilising the local infrastructure of the village that
was easily accessible to the enumerated study population of the
concerned village. People who were bedbound or those who
failed to attend the central clinical facility in the village were
examined at home.
The comprehensive ocular examination of patients with
corneal opacity included visual acuity estimation with the
logMAR tumbling E chart for distance and near, noncycloplegic refraction and prescription (cycloplegic refraction
for children), non-contact tonometry, lens examination and cataract assessment by the Lens Opacity Classication System III, slit
lamp biomicroscopy with uorescein staining, and detailed
retinal evaluation. The corneal examination was performed
under high magnication and emphasis was laid on the aetiopathogenesis, morphological characteristics and management of
the corneal disease. In the present study, blindness was dened
as visual acuity <3/60 in the better eye with available
correction.
Quality assurance and standardisation of all study procedures
and equipments was maintained throughout the period of the
study. A single cornea specialist conducted the ophthalmic
examination on the entire study population. The items of ophthalmic equipment were calibrated and standardised at regular
intervals. Any potential observer or measurement bias was thus
reduced.
Statistical analysis
The data were entered into a specially designed Microsoft
Access based platform with inbuilt validation and consistency
checks. Data analysis was carried out using Stata V.12.0 (Stata,
College Station, Texas, USA). Qualitative data has been
described as number (%) and quantitative data has been
described as meanSD and median (range) as appropriate. The
multivariable logistic regression analysis was done to nd the
association between sociodemographic factors and the presence
of corneal opacity and corneal blindness. The results for the
same were reported as OR (95% CI). A value of p<0.05 was
considered statistically signicant.
RESULTS
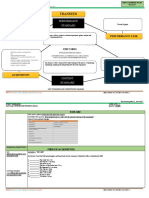
The total enumerated population in the 25 clusters of Rural
Gurgaon was 12 899. Out of these, 12 113 individuals completed all the study procedures, with a coverage of 93.9%. The
synopsis of the study participants recruited at each step has been
summarised in gure 1.
Sociodemographic prole
The age and gender distribution of the enumerated and the
covered population was similar and it matched the national
demographic prole of the Indian population. Although 6.1%
of the sample population could not be covered, the enumerated
population and the covered population had comparable sociodemographic characteristics. Males comprised 51% of the study
population (table 1).
Prevalence of corneal opacity
The prevalence of corneal opacity in this study population was
3.7% (95% CI 3.4% to 4.1%). During house-to-house examination, 452 people were detected with corneal opacity and comprehensive ocular examination was possible for 435 participants
(96.2%). The prevalence increased with age and was highest for
elderly patients (26.1%, 95% CI 23.4% to 28.8%). The prevalence of corneal opacity was higher among females (4.1% 95%
CI 3.6% to 4.6%) compared to males (3.4%, 95% CI 2.9% to
3.8%), the difference being statistically signicant ( p=0.025).
With multivariable analysis, the odds of having corneal
opacity increased with age and decreasing literacy status, and
were higher for females and unemployed participants (table 2).
After adjustment, females were at higher odds of having corneal
opacity, though the difference was not statistically signicant
(p=0.53).
Figure 1 Flow chart summarising
number of participants at various steps
of the study.
148
Gupta N, et al. Br J Ophthalmol 2015;99:147152. doi:10.1136/bjophthalmol-2014-305945
Downloaded from http://bjo.bmj.com/ on February 2, 2015 - Published by group.bmj.com
Global issues
Table 1 Sociodemographic profile of the enumerated and covered
study population in rural Gurgaon
Sociodemographic parameters
Age (years)
015
1639
4059
60
Gender
Male
Female
Occupation
Housework
Agricultural work
Non-agricultural work
Indoor work
Not working
Students and children
Education profile
Illiterate
Primary education*
Schooling (Std. 612)
Graduate and above
Children <7 years
Marital status
Married
Unmarried
Divorced/separated/
widow/widower
Religion
Hindu
Muslim
Total
Enumerated
population
n=12 899
n
Covered
population
n=12 113
n (%)
Uncovered
population
n=786
n (%)
4194
5632
2041
1032
4000 (95.4)
5276 (93.7)
1840 (90.2)
997 (96.6)
194
356
201
35
(4.6)
(6.3)
(9.8)
(3.4)
6745
6154
6173 (91.5)
5940 (96.5)
572 (8.5)
214 (3.5)
3435
709
1337
1263
692
5463
3349 (97.5)
653 (92.1)
1162 (86.9)
1080 (85.5)
668 (96.5)
5201 (95.2)
86
56
175
183
24
262
(2.5)
(7.9)
(13.1)
(14.5)
(3.5)
(4.8)
1949
2267
6292
641
1750
1862 (95.5)
2143 (94.5)
5828 (92.6)
575 (89.7)
1705 (97.4)
87
124
464
66
45
(4.5)
(5.5)
(7.4)
(10.3)
(2.6)
6303
5968
628
5847 (92.8)
5674 (95.1)
592 (94.3)
456 (7.2)
294 (4.9)
36 (5.7)
12 726
173
12 899
11 951 (93.9)
162 (93.6)
12 113 (93.9)
775 (6.1)
11 (6.4)
786 (6.1)
*Includes participants educated up to class 5 of formal schooling and people who
could read and write.
Prevalence of corneal blindness
The overall prevalence of corneal blindness in our study population, including both unilateral and bilateral cases, was 0.55%
(95% CI 0.42% to 0.69%); the prevalence of bilateral cases was
0.12% (95% CI 0.05% to 0.17%) and that of unilateral corneal
blindness was 0.45% (95% CI 0.33% to 0.56%). The majority
of the corneal blind patients were females (61.5%) and were
aged 60 years (84.6%).
Logistic regression analysis was conducted for individuals who
had corneal blindness in any (54) or both eyes (13). In this subgroup, comprising 67 people with either unilateral or bilateral
corneal blindness, the odds of having corneal blindness increased
with age and were higher for females and unemployed participants (table 3). Similar results were obtained after adjustment for
age, gender and other demographic parameters (table 3). The
elderly had 4.7 times more risk of developing corneal blindness
when compared to the younger age group after adjustment for
other demographic factors.
Causes of corneal opacity
Common causes of corneal opacity included pterygium
(34.5%), trauma (22.3%) and infectious keratitis (14.9%). In
the 150 cases with pterygium, 89 (59.3%) had normal vision
and 61 (40.7%) had mild to moderate visual impairment.
Table 4 lists the various corneal diseases prevalent in the study
population. Corneal involvement due to trachomatous infection
and its sequelae was seen in 33 eyes of 21 participants (table 4).
Causes of corneal blindness
Corneal diseases contributing to blindness were aphakic and
pseudophakic bullous keratopathy following cataract surgery,
corneal degenerations, and trauma. Unilateral corneal blindness
was mostly caused by ocular trauma, infectious keratitis, and
post-surgical bullous keratopathy (table 4).
DISCUSSION
The CORE study is the rst detailed, population-based study on
corneal diseases in the Indian population. To the best of our
knowledge, our study is the largest epidemiological study on
corneal opacities worldwide. This study provides reliable epidemiological data on the prevalence and risk factors of corneal
blindness and morbidity across all age groups in a rural North
Indian population.
In the present study, the prevalence of corneal opacity was
3.7% (95% CI 3.4% to 4.1%). There are a few published
studies on ocular morbidity conducted in the Indian population,
which report the prevalence rate of corneal opacity as 4.2% in
people aged 20 years and 3% in people aged 50 years.13 15
These studies involved a very small sample of the population
and hence do not represent accurate estimations of the prevalence of corneal opacity. In a hospital-based study in Haryana,
11.6% of patients with a visual acuity of 6/9 or worse were
found to have corneal disease.16 As these studies did not include
all age groups, they failed to provide comprehensive and representative data on the burden of corneal diseases in the general
population.
The prevalence of corneal blindness in this rural population
was 0.12%, and 0.45% of people were unilaterally blind due to
corneal disease. This amounts to a signicant burden on the
health system in general, and the blindness programme in particular. In another Indian study, the prevalence of corneal blindness (dened as presenting visual acuity <6/60 in the better eye
in this study) was reported to be 0.10% and that of unilateral
corneal blindness was 0.56%.17 A Chinese study also reported a
similar prevalence of corneal blindness of 0.1%.18
The common causes of corneal opacity in this rural population were pterygium (34.5%) followed by trauma (22.3%) and
infectious keratitis (14.9%). The aetiological factors responsible
for corneal disease were reported to be different in the late 19th
century, wherein trachoma was the most common corneal
disease reported (30%) in a hospital-based study.16 The impact
of community trachoma control programmes and nutritional
education together with a measles immunisation programme has
resulted in a reduction of the burden of corneal blindness due
to trachoma and vitamin A deciency.
The main aetiological diseases responsible for corneal blindness in our study population were post-surgical bullous keratopathy (46.2%), corneal degenerations (23.1%) and trachoma
(15.4%). In the South Indian population, corneal blindness was
predominantly due to infectious keratitis (59.5%) and trauma
(23.2%).17 Studies from Thailand and Gambia also report the
common causes of corneal blindness.19 20 In Thailand, these
were infections (35.6%), surgical bullous keratopathy (27.8%),
and trauma (14%).19 In Gambia, vitamin A deciency (7.8%)
was an important cause of corneal blindness in addition to
infectious keratitis (22.7%) and trauma (14.3%).20 Thus,
Gupta N, et al. Br J Ophthalmol 2015;99:147152. doi:10.1136/bjophthalmol-2014-305945
149
Global issues
150
Table 2
Effect of sociodemographic factors on the prevalence of corneal opacity by logistic regression analysis
Corneal opacity
Age group (years)
015
1639
4059
60
Gender
Male
Female
No
n=11 661
Yes
n=452
Prevalence
% (95% CI)
3997
5247
1680
737
3
29
160
260
0.08 (0.01 to 0.16)
0.55 (0.35 to 0.75)
8.70 (7.41 to 9.98)
26.08 (23.35 to 28.81)
5966
5695
207
245
3.35 (2.90 to 3.80)
4.12 (3.62 to 4.63)
No
n=7664
Yes
n=449
Prevalence
% (95% CI)
1554
831
4715
564
271
63
105
10
14.85 (13.22 to 16.48)
7.05 (5.37 to 8.73)
2.18 (1.77 to 2.59)
1.74 (0.67 to 2.82)
3167
616
1118
1041
1722
182
37
44
39
147
5.43
5.67
3.79
3.61
7.87
Unadjusted OR
(95% CI)
p Value
Adjusted OR (95% CI)
p Value
1.0
7.36 (2.24 to 24.19)
126.89 (40.44 to 398.17)
470.02 (150.20 to 1470.83)
0.001
<0.001
<0.001
1.0
7.34 (2.23 to 24.11)
126.23 (40.22 to 396.14)
467.64 (149.42 to 1463.52)
0.001*
<0.001*
<0.001*
0.025*
1.0
1.24 (1.03 to 1.49)
0.025
1.0
1.07 (0.87 to 1.31)
0.533
p Value
Unadjusted OR
(95% CI)
p Value
Adjusted OR (95% CI)
p Value
<0.001*
1.0
0.43 (0.33 to 0.58)
0.13 (0.10 to 0.16)
0.10 (0.05 to 0.19)
<0.001
<0.001
<0.001
1.0
0.80 (0.58 to 1.10)
0.47 (0.34 to 0.64)
0.52 (0.25 to 1.06)
0.168
<0.001*
0.071
1.0
1.04 (0.72 to 1.50)
0.68 (0.49 to 0.96)
0.65 (0.46 to 0.93)
1.5 (1.19 to 1.86)
0.812
0.027
0.017
0.001
1.0
1.02
1.21
1.59
1.48
0.937
0.417
0.056
0.015*
p Value
<0.001*
Corneal opacity
Gupta N, et al. Br J Ophthalmol 2015;99:147152. doi:10.1136/bjophthalmol-2014-305945
Risk Factors
Education
Illiterate
Primary education
Schooling (Std. 612)
Graduate and above
Occupation
Housework
Agricultural work
Non-agricultural work
Indoor work
Not working and students
(4.67
(3.89
(2.69
(2.50
(6.64
to
to
to
to
to
6.20)
7.44)
4.89)
4.73)
9.09)
<0.001*
*Statistically significant difference between groups.
In the multivariable analysis, age and gender were adjusted for each other.
Children aged 05 years were excluded.
Education and occupation were adjusted for all the variables including age and gender and was done excluding children aged 015 years.
Includes participants who could read and write.
(0.63 to
(0.77 to
(0.99 to
(1.08 to
1.64)
1.88)
2.57)
2.03)
Downloaded from http://bjo.bmj.com/ on February 2, 2015 - Published by group.bmj.com
Risk Factors
Downloaded from http://bjo.bmj.com/ on February 2, 2015 - Published by group.bmj.com
Global issues
Table 3 Effect of sociodemographic factors on the prevalence of corneal blindness by logistic regression analysis
Corneal blind
Risk factors
Age (years)
<60
60
Gender
Male
Female
Education
Up to primary
Above primary (>Std. 5)
Occupation
Housework
Agricultural work
Non-agricultural work
Indoor work
Not working/retired
Students and children
No
(n=12 046)
Yes
(n=67)
Prevalence
% (95% CI)
11 093
953
23
44
0.21 (0.12 to 0.29)
4.41 (3.14 to 5.69)
p Value
Unadjusted OR (95% CI)
p Value
Adjusted OR (95% CI)
p Value
1.0
22.27 (13.39 to 37.03)
<0.001*
1.0
4.70 (2.38 to 9.26)
<0.001*
1.0
1.64 (1.00 to 2.69)
0.048*
1.0
1.13 (0.58 to 2.19)
0.720
1.0
0.19 (0.10 to 0.36)
<0.001*
1.0
0.30 (0.15 to 0.62)
0.001*
1.0
0.41
0.69
0.25
6.47
0.03
0.224
0.416
0.057
<0.001*
<0.001*
1.0
0.58
1.38
0.73
2.81
0.04
0.505
0.584
0.679
0.003*
0.002*
<0.001*
0.046*
6147
5899
26
41
0.42 (0.26 to 0.58)
0.69 (0.48 to 0.90)
<0.001*
5655
6391
55
12
0.96 (0.71 to 1.22)
0.19 (0.08 to 0.29)
<0.001*
3324
651
1156
1078
637
5200
25
2
6
2
31
1
0.75
0.31
0.52
0.19
4.64
0.02
(0.45
(0.12
(0.10
(0.07
(3.04
(0.01
to
to
to
to
to
to
1.04)
0.73)
0.93)
0.44)
6.24)
0.06)
(0.10
(0.28
(0.06
(3.79
(0.01
to
to
to
to
to
1.73)
1.69)
1.04)
11.03)
0.19)
(0.12
(0.47
(0.15
(1.41
(0.01
to
to
to
to
to
2.75)
3.99)
3.53)
5.59)
0.32)
*Statistically significant difference between groups.
Includes participants educated up to class 5 of formal schooling and people who could read and write.
Includes children <7 years of age.
contrary to popular belief and previous studies,17 19 20 the predominant cause of corneal blindness in the current study was
not infectious keratitis but corneal decompensation following
cataract surgery. Addressing the issue of improving the quality
of cataract surgical services in the country will help reduce the
requirement for corneal transplantation. There is a need for
implementing monitoring mechanisms so that good quality cataract surgery is available at all levels of healthcare delivery,
thereby reducing the load of corneal complications after cataract
surgery.
The study highlights the changing trends in the pattern of
corneal diseases in the rural Indian population. The success of
prevention programmes related to keratomalacia and trachoma
have led to marked reductions in their prevalence, as exemplied in the present study. We need to be cautious about the
Table 4
increasing prevalence and occurrence of corneal complications
due to high-volume cataract surgery, which is shifting the
burden from cataract blindness to corneal blindness in a developing country like India.
It is important to interpret the results of our study keeping in
view the few limitations. Rural data cannot be directly extrapolated to urban populations and further surveys in urban regions
are required to achieve a comprehensive picture. Though the
overall participation rate in the present study was high, the
coverage of individuals aged 4059 years and the male population was comparatively lower than other sub-groups. This could
be attributed to the non-availability of males and people aged
4059 years in their households during daytime, as they constitute the productive population and were out at work when the
house-to-house visits were conducted. Although the present
Causes and age distribution of corneal opacities and corneal blindness in the study population (n=435)
Corneal pathology
Age of participants (years)
Median (range)
People with CO
n=435
n (%)
Bilateral blind*
n=13
n (%)
Unilateral blind
n=54
n (%)
Pterygium associated CO
Traumatic CO
Infectious keratitis
Corneal dystrophy and degenerations
Trachomatous keratopathy
Aphakic/pseudophakic bullous keratopathy
Post-exanthematous CO
Iatrogenic CO
Vitamin A deficiency associated CO
Glaucoma with corneal decompensation
Miscellaneous
Unknown aetiology
55 (1895)
60 (1190)
65 (3094)
72.5 (5192)
68 (3299)
75 (6294)
65 (4282)
68 (6098)
45.5 (1458)
63.5 (6364)
65 (284)
62 (2274)
150 (34.5)
97 (22.3)
65 (14.9)
26 (6.0)
21 (4.8)
17 (3.9)
15 (3.5)
13 (3.0)
4 (0.9)
2 (0.5)
16 (3.8)
9 (2.1)
0
0
1
3
2
6
0
0
1
0
0
0
0 (0.0)
14 (25.9)
12 (22.2)
4 (7.4)
6 (11.1)
8 (14.8)
7 (13.0)
1 (1.9)
1 (1.9)
1 (1.9)
0 (0.0)
0 (0.0)
(0.0)
(0.0)
(7.7)
(23.1)
(15.4)
(46.2)
(0.0)
(0.0)
(7.7)
(0.0)
(0.0)
(0.0)
*Blindness defined as presenting visual acuity <3/60 in better eye.
CO, corneal opacity.
Gupta N, et al. Br J Ophthalmol 2015;99:147152. doi:10.1136/bjophthalmol-2014-305945
151
Downloaded from http://bjo.bmj.com/ on February 2, 2015 - Published by group.bmj.com
Global issues
study involved a large sample population which was larger than
any previously published study on corneal blindness, the sample
size was not adequate for ascertaining the true prevalence of
corneal blindness.17 18 However, the sample size was appropriate for assessing the primary objective of the study which was to
determine the population prevalence of corneal opacity.
The major strengths of this study are the high response rate
(93.9%) in a large sample population covering all age groups,
and that it is the rst reported population-based study, specically designed to study the prevalence of corneal opacity in
India, outlining all determinants and aetiological factors responsible for its occurrence. This study will prove useful in planning
blindness programme initiatives and estimating resources
required to provide comprehensive corneal services for the community, thereby helping to eliminate the causes of avoidable
corneal blindness and visual impairment.
Contributors NG: Literature search and compilation, study conception and design,
data collection and acquisition, data analysis and interpretation, drafting and writing
of manuscript. PV: Study conception and design, critical revision of manuscript,
administrative, technical and material support, supervision. RT: Study conception and
design, data interpretation, revision of manuscript for important intellectual content,
supervision. SKG: Study conception and design, data collection and acquisition,
revision of manuscript for important intellectual content, technical support. SD:
Statistical expertise, data analysis and interpretation, revision of manuscript for
important intellectual content. KM: Study design, statistical expertise, data analysis
and interpretation.
Competing interests None.
3
4
5
8
9
10
11
12
13
14
15
Patient consent Obtained.
Ethics approval Institute Ethics Committee, All India Institute of Medical Sciences,
New Delhi, India.
16
Provenance and peer review Not commissioned; externally peer reviewed.
17
18
REFERENCES
1
152
World Health Organization. Prevention of blindness and visual impairment. Priority
eye diseases-corneal opacities. http://www.who.int/blindness/causes/priority/en/
index9.html (accessed Jul 2014).
Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J
Ophthalmol 2012;96:61418.
19
20
Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective.
Bull World Health Organ 2001;79:21421.
Gupta N, Tandon R, Gupta SK, et al. Burden of corneal blindness in India. Indian J
Community Med 2013;38:198206.
Tandon R, Sinha R, Moulick P, et al. Pattern of bilateral blinding corneal disease in
patients waiting for keratoplasty in a tertiary eye care centre in northern India.
Cornea 2010;29:26971.
Murthy GV, Vashist P, John N, et al. Prevalence and causes of visual impairment
and blindness in older adults in an area of India with a high cataract surgical rate.
Ophthalmic Epidemiol 2010;17:18595.
Neena J, Rachel J, Praveen V, et al. Rapid assessment of avoidable blindness India
study group. Rapid assessment of avoidable blindness in India. PLoS One 2008;3:
e2867.
Murthy GV, Gupta SK, Bachani D, et al. Current estimates of blindness in India.
Br J Ophthalmol 2005;89:25760.
Nirmalan PK, Thulasiraj RD, Maneksha V, et al. A population-based eye survey of
older adults in Tirunelveli district of south India: blindness, cataract surgery, and
visual outcomes. Br J Ophthalmol 2002;86:50512.
Thulasiraj RD, Rahamathulla R, Saraswati A, et al. The Sivaganga eye
survey: I. Blindness and cataract surgery. Ophthalmic Epidemiol 2002;9:
299312.
Murthy GV, Gupta S, Ellwein LB, et al. A population-based eye survey of older
adults in a rural district of Rajasthan: I. Central vision impairment, blindness, and
cataract surgery. Ophthalmology 2001;108:67985.
Dandona L, Dandona R, Srinivas M, et al. Blindness in Indian state of Andhra
Pradesh. Invest Ophthalmol Vis Sci 2001;42:90816.
Haq I, Khan Z, Khalique N, et al. Prevalence of common ocular morbidities in adult
population of Aligarh. Indian J Community Med 2009;34:195201.
Area and Population of Haryana: 2011(P). http://esaharyana.gov.in/Data/
StateStatisticalAbstract/2010-11(English)/StateAbst10-11/27-95.pdf (accessed Jul
2014).
Singh MM, Murthy GV, Venkatraman R, et al. A study of ocular morbidity among
elderly population in a rural area of central India. Indian J Ophthalmol
1997;45:615.
Parmar IP, Gupta NC, Garg N, et al. Corneal blindnessa public health problem.
Indian J Public Health 1986;30:1936.
Dandona R, Dandona L. Corneal blindness in a southern Indian population: need
for health promotion strategies. Br J Ophthalmol 2003;87:13341.
Wang H, Zhang Y, Li Z, et al. Prevalence and causes of corneal blindness. Clin
Experiment Ophthalmol 2014;42:24953.
Prabhasawat P, Trethipwanit KO, Prakairungthong N, et al. Causes of
corneal blindness: a multi-center retrospective review. J Med Assoc Thai
2007;90:26517.
Bowman RJ, Faal H, Dolin P, et al. Non-trachomatous corneal opacities in the
Gambiaetiology and visual burden. Eye (Lond) 2002;16:2732.
Gupta N, et al. Br J Ophthalmol 2015;99:147152. doi:10.1136/bjophthalmol-2014-305945
Downloaded from http://bjo.bmj.com/ on February 2, 2015 - Published by group.bmj.com
Prevalence of corneal diseases in the rural
Indian population: the Corneal Opacity Rural
Epidemiological (CORE) study
Noopur Gupta, Praveen Vashist, Radhika Tandon, Sanjeev K Gupta,
Sadanand Dwivedi and Kalaivani Mani
Br J Ophthalmol 2015 99: 147-152 originally published online November
13, 2014
doi: 10.1136/bjophthalmol-2014-305945
Updated information and services can be found at:
http://bjo.bmj.com/content/99/2/147
These include:
References
Email alerting
service
Topic
Collections
This article cites 18 articles, 5 of which you can access for free at:
http://bjo.bmj.com/content/99/2/147#BIBL
Receive free email alerts when new articles cite this article. Sign up in the
box at the top right corner of the online article.
Articles on similar topics can be found in the following collections
Cornea (467)
Ocular surface (557)
Neurology (1229)
Vision (579)
Epidemiology (928)
Conjunctiva (203)
Eye (globe) (635)
Public health (437)
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Customer satisfaction at Zara storesDokumen11 halamanCustomer satisfaction at Zara storesIrina BalanBelum ada peringkat
- Research MethodologyDokumen4 halamanResearch MethodologyBharat Ahuja100% (1)
- CH 01Dokumen3 halamanCH 01Tibet Boğazköy AkyürekBelum ada peringkat
- Eastern Mediterranean University Department of Industrial EngineeringDokumen3 halamanEastern Mediterranean University Department of Industrial EngineeringAngela NatashaBelum ada peringkat
- Translational Research in Anatomy: James P. Nott, Elizabeth A. Bonney, James D. Pickering, Nigel A.B. SimpsonDokumen7 halamanTranslational Research in Anatomy: James P. Nott, Elizabeth A. Bonney, James D. Pickering, Nigel A.B. Simpsonangela_karenina_1Belum ada peringkat
- UMEM Educational Pearls - University of Maryland School of Medicine, Department of Emergency MedicineDokumen2 halamanUMEM Educational Pearls - University of Maryland School of Medicine, Department of Emergency Medicineangela_karenina_1Belum ada peringkat
- S - An Outcome Audit of Three Day Antimicrobial Prescribing For The Acute Dentoalveolar AbscessDokumen4 halamanS - An Outcome Audit of Three Day Antimicrobial Prescribing For The Acute Dentoalveolar Abscessangela_karenina_1Belum ada peringkat
- Traumasystems: Origins, Evolution, and Current ChallengesDokumen13 halamanTraumasystems: Origins, Evolution, and Current Challengesangela_karenina_1Belum ada peringkat
- Morgan 2016Dokumen3 halamanMorgan 2016angela_karenina_1Belum ada peringkat
- Patofisiologi Preeklamsi1Dokumen4 halamanPatofisiologi Preeklamsi1Andini RizkyBelum ada peringkat
- Ditorial What's in A Word?: Stewart. Michael@mayo - EduDokumen2 halamanDitorial What's in A Word?: Stewart. Michael@mayo - Eduangela_karenina_1Belum ada peringkat
- Kapoor 2018Dokumen8 halamanKapoor 2018angela_karenina_1Belum ada peringkat
- Tide Man 2016Dokumen9 halamanTide Man 2016angela_karenina_1Belum ada peringkat
- Park 2015Dokumen7 halamanPark 2015angela_karenina_1Belum ada peringkat
- Ong 2017Dokumen5 halamanOng 2017angela_karenina_1Belum ada peringkat
- S - Histology of Ancient Soft Tissue Tumors A ReviewDokumen13 halamanS - Histology of Ancient Soft Tissue Tumors A Reviewangela_karenina_1Belum ada peringkat
- Neonatal Side Effects of Maternal Labetalol Treatment in Severe PreeclampsiDokumen5 halamanNeonatal Side Effects of Maternal Labetalol Treatment in Severe Preeclampsiangela_karenina_1Belum ada peringkat
- Peran GNRHDokumen7 halamanPeran GNRHMerliana DebyantiBelum ada peringkat
- Clin Infect Dis.-2011-Lawn-1384-7 PDFDokumen4 halamanClin Infect Dis.-2011-Lawn-1384-7 PDFangela_karenina_1Belum ada peringkat
- Distance Visual Acuity Measurement StudyDokumen1 halamanDistance Visual Acuity Measurement Studyangela_karenina_1Belum ada peringkat
- Prognostic Impact of HIF-1α Expression in PatientsDokumen6 halamanPrognostic Impact of HIF-1α Expression in Patientsangela_karenina_1Belum ada peringkat
- Vaughan and Asbury's General Ophthalmology, 17th Edition: System For Ophthalmic Dispensing WasDokumen2 halamanVaughan and Asbury's General Ophthalmology, 17th Edition: System For Ophthalmic Dispensing Wasangela_karenina_1Belum ada peringkat
- Jia 2016Dokumen12 halamanJia 2016angela_karenina_1Belum ada peringkat
- Carica papaya seed extract reduces steroidogenesis and spermatogenesis in ratsDokumen5 halamanCarica papaya seed extract reduces steroidogenesis and spermatogenesis in ratsangela_karenina_1Belum ada peringkat
- HIV in ChildrenDokumen28 halamanHIV in Childrenangela_karenina_1Belum ada peringkat
- Asymptomatic Bacteriuria During Pregnancy: Eyal Sheiner, Efrat Mazor-Drey, & Amalia LevyDokumen5 halamanAsymptomatic Bacteriuria During Pregnancy: Eyal Sheiner, Efrat Mazor-Drey, & Amalia Levyangela_karenina_1Belum ada peringkat
- Padegimas2015 PDFDokumen12 halamanPadegimas2015 PDFangela_karenina_1Belum ada peringkat
- Maconochie2015 PDFDokumen22 halamanMaconochie2015 PDFangela_karenina_1Belum ada peringkat
- Bacterial VaginosisDokumen9 halamanBacterial Vaginosisangela_karenina_1100% (1)
- Obermair 2003Dokumen7 halamanObermair 2003angela_karenina_1Belum ada peringkat
- Morley 2004Dokumen6 halamanMorley 2004angela_karenina_1Belum ada peringkat
- Autophagy and Autophagy-Related Proteins in The Immune SystemDokumen12 halamanAutophagy and Autophagy-Related Proteins in The Immune Systemangela_karenina_1Belum ada peringkat
- S - Factors That Affect The Decision To Undergo Amniocentesis in Women With Normal Down Syndrome Screening Results It Is All About The Age PDFDokumen12 halamanS - Factors That Affect The Decision To Undergo Amniocentesis in Women With Normal Down Syndrome Screening Results It Is All About The Age PDFangela_karenina_1Belum ada peringkat
- Who Should We Cool After Perinatal AsphyxiaDokumen6 halamanWho Should We Cool After Perinatal Asphyxiaangela_karenina_1Belum ada peringkat
- The Public Image of The PoliceDokumen122 halamanThe Public Image of The PoliceAnuar Abdul FattahBelum ada peringkat
- Kear 2004 - Mine Project Life CycleDokumen4 halamanKear 2004 - Mine Project Life CycleedatgkaBelum ada peringkat
- Statistics For BCADokumen6 halamanStatistics For BCAsebastian cyriac100% (1)
- Research LP (3RD Quarter)Dokumen7 halamanResearch LP (3RD Quarter)Jaidee BiluganBelum ada peringkat
- Variance and Standard DeviationDokumen16 halamanVariance and Standard Deviationmehtab sanaBelum ada peringkat
- Simpson's Diversity Index ExplainedDokumen5 halamanSimpson's Diversity Index ExplainedGISSABelum ada peringkat
- Microsoft Word 20. SES 2151 RESEARCH METHODOLOGYDokumen2 halamanMicrosoft Word 20. SES 2151 RESEARCH METHODOLOGYKelvin MagiriBelum ada peringkat
- Case Analysis on Performance Management at Vitality Health EnterprisesDokumen10 halamanCase Analysis on Performance Management at Vitality Health Enterprisescinthiya aliBelum ada peringkat
- Columbia Case Analysis - Group 3Dokumen16 halamanColumbia Case Analysis - Group 3Abhishek Singhvi100% (1)
- Chap 13: Turning Customer Knowledge Into Sales KnowledgeDokumen3 halamanChap 13: Turning Customer Knowledge Into Sales KnowledgeHEM BANSALBelum ada peringkat
- Almanac, 2001) - Use The Median Age of The Preceding Data To Comment OnDokumen2 halamanAlmanac, 2001) - Use The Median Age of The Preceding Data To Comment Ontushar jainBelum ada peringkat
- Using Composition To Assess and Enhance Visual Values in LandscapesDokumen31 halamanUsing Composition To Assess and Enhance Visual Values in LandscapesTosia PlotaBelum ada peringkat
- 04 11yohannanDokumen8 halaman04 11yohannanRaja RajanBelum ada peringkat
- Distribution of Vertical Loads in a Machinery Support SystemDokumen4 halamanDistribution of Vertical Loads in a Machinery Support SystemnavinzhereBelum ada peringkat
- Desalegn Kassaye FinalDokumen93 halamanDesalegn Kassaye FinalTedros BelaynehBelum ada peringkat
- Simple Research Paper Outline TemplateDokumen5 halamanSimple Research Paper Outline Templatemkcewzbnd100% (1)
- Department of Education: Lesson Plan in MathematicsDokumen2 halamanDepartment of Education: Lesson Plan in MathematicsShiera SaletreroBelum ada peringkat
- Exercise 1.4Dokumen2 halamanExercise 1.4Almavilla BantayanBelum ada peringkat
- Evaluating Employee Performance PDFDokumen2 halamanEvaluating Employee Performance PDFJonathan0% (1)
- CRISC Review QAE 2015 Correction Page 65 XPR Eng 0615Dokumen1 halamanCRISC Review QAE 2015 Correction Page 65 XPR Eng 0615Sakil MahmudBelum ada peringkat
- Problems and Prospects of Cashew Workers in KanyakumariDokumen14 halamanProblems and Prospects of Cashew Workers in KanyakumariDrGArumugasamyBelum ada peringkat
- Sparks and The 40 Developmental AssetsDokumen2 halamanSparks and The 40 Developmental AssetsMartin GonzalezBelum ada peringkat
- First Year Critical Appraisal Randomize Control TrialDokumen4 halamanFirst Year Critical Appraisal Randomize Control Trialapi-615708784Belum ada peringkat
- COPARDokumen12 halamanCOPARGlenn Asuncion PagaduanBelum ada peringkat
- Analysis of Sarcasm in "SnatchDokumen14 halamanAnalysis of Sarcasm in "SnatchFauzan RodhiBelum ada peringkat
- Research - G12 HUMSS 1Dokumen56 halamanResearch - G12 HUMSS 1Neil Marjunn TorresBelum ada peringkat