Artigo Bevacizumab
Diunggah oleh
danielnegraoJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Artigo Bevacizumab
Diunggah oleh
danielnegraoHak Cipta:
Format Tersedia
Systematic review
Bevacizumab for ocular neovascular diseases:
a systematic review
Bevacizumabe para doenas oculares neovasculares: reviso sistemtica
Regis Bruni Andriolo1, Maria Eduarda Puga1, Rubens Belfort Jnior2, lvaro Nagib Atallah3
Universidade Federal de So Paulo Escola Paulista de Medicina (Unifesp-EPM), So Paulo, Brazil
KEY WORDS:
Angiogenesis inhibitors.
Retinal neovascularization.
Corneal angiogenesis.
Macular degeneration.
Review.
ABSTRACT
CONTEXT AND OBJECTIVE: Many eye diseases involve increased local levels of vascular endothelial growth factor (VEGF), and there are several therapeutic
strategies for them. Thus, the aim of this study was to evaluate the effectiveness and safety of bevacizumab for treating eye diseases involving increased
local levels of VEGF, as the assumed pathophysiological mechanism.
DATA SOURCES: The following databases were systematically searched for evidence: PubMed, CENTRAL (Cochrane Library), Literatura Latino-Americana
e do Caribe em Cincias da Sade (Lilacs) and reference lists, without language restrictions. Only randomized controlled trials were included. The primary
outcome of interest was visual acuity, irrespective of the evaluation method.
DATA SYNTHESIS: A total of 667 eyes in nine randomized trials were included. Meta-analysis showed that the proportion of patients with age-related
macular degeneration who presented improvements from baseline regarding best-corrected visual acuity was higher among those treated with bevacizumab
than among those in the photodynamic therapy group (risk ratio, RR, 0.49; 95% confidence interval, CI, 0.31 to 0.78; P = 0.01).
CONCLUSIONS: The evidence available demonstrates that bevacizumab alone or combined with other treatments is more effective than other options,
including photodynamic therapy, focal photocoagulation and triamcinolone. The use of bevacizumab instead of photodynamic therapy could reduce
treatment costs by more than 99% and could significantly increase access to treatment. However, long-term studies are still needed in order to reduce
uncertainty concerning the safety of this medication for all ocular neovascular diseases in which bevacizumab has the potential to improve visual acuity.
RESUMO
PALAVRAS-CHAVE:
Inibidores da angiognese.
Neovascularizao retiniana.
Neovascularizao da crnea.
Degenerao macular.
Reviso.
CONTEXTO E OBJETIVOS: Muitas doenas oculares envolvem o aumento dos nveis locais de fator de crescimento do endotlio vascular (FCEV), uma
diversidade de estratgias teraputicas para tais condies. Assim, o objetivo do presente estudo avaliar a efetividade e a segurana de bevacizumabe
para o tratamento de pacientes com doena ocular que envolva o aumento dos nveis locais de FCEV, como mecanismo patofisiolgico assumido.
FONTE DAS INFORMAES: Foi realizada busca sistemtica pelas evidncias disponveis nas seguintes bases de dados da eletrnicas: PubMed,
CENTRAL (The Cochrane Library), Literatura Latino-Americana e do Caribe em Cincias da Sade (Lilacs), alm de referncias bibliogrficas de estudos
relevantes, sem restries de lngua. Foram includos apenas ensaios controlados e aleatrios. Acuidade visual, independentemente do mtodo de
avaliao, foi considerada o desfecho primrio de interesse.
SNTESE DOS DADOS: Foi includo um total de 667 olhos testados em nove ensaios clnicos aleatrios. A metanlise demonstrou que a proporo de
pacientes com degenerao macular relacionada idade que melhoraram a acuidade visual foi maior entre os tratados com bevacizumabe do que entre
os pacientes em terapia fotodinmica (risco relativo [RR] 0.49, 95% intervalo de confiana [IC] 0,31 a 0,78, P = 0,01).
CONCLUSES: A evidncia disponvel demonstra que bevacizumabe isolado ou combinado com outras terapias mais eficaz que terapia fotodinmica,
fotocoagulao focal e triancinolona. O uso de bevacizumabe em vez da terapia fotodinmica poderia reduzir os custos do tratamento em mais de 99% e
aumentar significativamente o acesso ao tratamento. Entretanto, o aspecto de segurana do frmaco ainda necessita ser avaliado por estudos em longo
prazo com todas as doenas neovasculares em que bevacizumabe tenha o potencial de melhorar acuidade visual.
MSc. Affiliated researcher at Brazilian Cochrane Center and postgraduate student at the Discipline of Emergency Medicine and Evidence-Based Medicine, Department of Medicine,
Universidade Federal de So Paulo Escola Paulista de Medicina (Unifesp-EPM), So Paulo, Brazil.
2
MD, PhD. Full professor of the Discipline of Ophthalmology, Department of Ophthalmology, Universidade Federal de So Paulo Escola Paulista de Medicina (Unifesp-EPM), So
Paulo, Brazil.
3
MD, PhD. Full professor of the Discipline of Emergency Medicine and Evidence-Based Medicine, Department of Medicine, Universidade Federal de So Paulo Escola Paulista de
Medicina (Unifesp-EPM), So Paulo, Brazil.
1
84
Sao Paulo Med J. 2009; 127(2):84-91
Bevacizumab for ocular neovascular diseases: a systematic review
INTRODUCTION
METHODS
Data sources and searches
The following databases were searched: Medical Literature Analysis and Retrieval System Online (Medline) (1966 to June 2008), Controlled Trials Register of the Cochrane Collaboration (2008, issue 2)
and Literatura Latino-Americana e do Caribe em Cincias da Sade
(Lilacs) (1982 to June 2008). A general search strategy was used, with
adaptations to the characteristics of each database, to identify studies on
bevacizumab for ocular diseases that involved increased local levels of
VEGF. Descriptors and synonyms for the intervention of interest (Avastin, bevacizumab) and for the clinical conditions for which this medication potentially could be indicated were used (e.g. age-related macular
disease, corneal neovascularization, retinal angiomatous proliferation or
angiogenic retinal diseases, among others).
Study selection
We planned to include only randomized or quasi-randomized clinical trials that tested bevacizumab alone or in association with other
strategies available. The clinical condition of interest among the individuals included (of both genders, independent of ethnicity and age) was a
diagnosis of ocular diseases or ocular conditions with the same underlying pathophysiological mechanism of increased local levels of VEGF, according to the criteria established by the authors of the primary studies,
such as age-related macular disease, corneal neovascularization, retinal
angiomatous proliferation or angiogenic retinal diseases, among others.
100
Cumulative Relative Frequency of Papers (%)
Many eye diseases and problems associated with ocular structures
and tissues involve a single pathophysiological mechanism relating to
increased local levels of vascular endothelial growth factor (VEGF) and
consequently to neovascularization.1 Such diseases can include age-related
macular degeneration, affecting 5% to 27% of health-plan beneficiaries,
proliferative diabetic retinopathy, affecting 14.5% to 25.6% of patients
with diabetes mellitus,2 and other less prevalent diseases, such as StevensJohnson syndrome, with 2.2 to 7.1 cases per million inhabitants.3
Bevacizumab, a monoclonal antibody that binds to all VEGF isoforms, was developed to treat colorectal cancer,4 and its use for ocular diseases has not yet been approved by the United States Food and
Drug Administration (FDA).5 Nevertheless, use of bevacizumab has
been supported by Medicare in the United States since July 2006, thus
suggesting that the information available is sufficient to allow bevacizumab to be purchased and included in the management of neovascular macular degeneration.6 A growing number of researchers are making information available regarding the use of bevacizumab for ocular
diseases. Figure 1 demonstrates the number of papers on this subject
that have been published since the first one in 2002.
This scenario clearly indicates the need to conduct a systematic review of randomized clinical trials, in order to reduce the uncertainties
and establish guidelines for future randomized clinical trials that test
hypotheses about bevacizumab for patients diagnosed with ocular neovascular diseases.
237 studies
50
237 studies
0
2 3 3 3 3 3 3 4 4 4 4 4 4 5 5 5 5 5 5 6 6 6 6 6 6 7 7 7 7 7 7 8 8 8
c-0 b-0 pr-0 n-0 g-0 ct-0 c-0 b-0 pr-0 n-0 g-0 ct-0 c-0 b-0 pr-0 n-0 g-0 ct-0 c-0 b-0 pr-0 n-0 g-0 ct-0 c-0 b-0 pr-0 n-0 g-0 ct-0 c-0 b-0 pr-0 n-0
De Fe A Ju Au O De Fe A Ju Au O De Fe A Ju Au O De Fe A Ju Au O De Fe A Ju Au O De Fe A Ju
The chart of cumulative relative frequency demonstrates that 50% of the studies on the application of
bevacizumab for eye diseases were published from December 2002 to September 2007, according to
their indexation in PubMed. The remaining 50% (237 studies) was published over a period of only nine
months, from September 2007 to June 2008.
Figure 1. Papers reporting on bevacizumab for ocular diseases published
per month in the PubMed database.
Studies in which the analysis unit was based on the eyes were not included, since there is evidence demonstrating an adverse event (vitritis)
associated with bevacizumab in the contralateral eye.7
Data extraction and quality assessment
The methodological quality of the studies included was analyzed
independently by two authors (RBA and ANA) according to the risk of
bias (low, moderate or high risk) relating to the following items: selection bias, performance bias, detection bias and attrition bias.8
The outcome of interest for this review was visual acuity, as measured by any validated evaluation instrument (e.g. Snellen acuity charts,
Vernier acuity, Early Treatment Diabetic Retinopathy Study chart and
others). Adverse events, e.g. ocular or systematic hypertension, ocular
toxicity, local inflammation, retinal detachment, vitreous hemorrhage,
corneal abrasions, lens injury and thromboembolic events, were assessed. Surrogate outcomes, such as central foveal thickness, fluorescein angiography and others, were not considered in this analysis. When
the outcome was reported in more than one paper, these results were
combined in meta-analyses using Review Manager 5.0,9 which was developed by the Cochrane Collaboration. Dichotomous data were calculated as risk ratios (RR) with 95% confidence intervals (95% CI).
The estimated effects were combined using the random effect model,10
which considers outliers to be related to heterogeneities of a clinical and
methodological nature, even when they are unknown. Continuous data
were expressed as means and standard deviations, and weighted mean
differences (WMD) were calculated in relation needed to the 95% CI
level. For continuous data, the numerical information needed to perform such analysis was composed of the total number of patients and
the mean and standard deviation, per comparison group. For dichotomous data, the numerical information needed to perform such analysis
was composed of the total number of patients and the number of events,
per comparison group. The reviewers grouped the data as a function of
Sao Paulo Med J. 2009; 127(2):84-91
85
Andriolo RB, Puga ME, Belfort Jnior R, Atallah AN
co-interventions. Statistical heterogeneity between the study results was
evaluated using the inconsistency test (I2), such that inconsistency was
considered present when I2 > 50%.11,12
RESULTS
Description of studies with potential for inclusion
Out of the 474 studies retrieved through the search strategy, only
nine satisfied the preestablished inclusion criteria (Figure 2). A Cochrane systematic review covering all anti-VEGF therapies for age-related macular degeneration was found, but the authors had not included
studies testing bevacizumab by the time the present systematic review
was finished.13 One randomized study was excluded because its outcomes did not align with the purpose of this review and because it allocated the two eyes of each patient to different comparison groups.14
The nine studies included in the present review yielded a total of 667
randomized eyes, as shown in Table 1.15-23
Three studies included patients with diagnoses of diabetic macular edema.17,20,21 One study included patients with diagnoses of clinically significant macular edema who had not responded to earlier subsequent photocoagulation therapy.15 Three studies included patients with
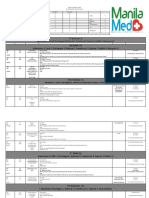
Table 1. Comparison groups and bevacizumab regimen tested in each study
Reference
Intervention
15
a. bevacizumab
b. bevacizumab
triamcinolone
c. sham
16
17
18
19
20
21
22
23
86
Description available in the report
3 1.25 mg at 6-week intervals
3 1.25 mg at 6-week intervals
2 mg (at first session)
syringe without needle pressed
against the conjunctiva and sclera
a. bevacizumab
2.5 mg mean of 2.4 treatments
b. photodynamic therapy
mean of 2.3 treatments with
verteporfin
a. focal photocoagulation
single dose
b. bevacizumab
1.25 mg on entry and after 6 weeks
c bevacizumab
1.25 mg on entry
sham injections
one per week
d. bevacizumab
1.25 mg on entry and after 6 weeks
focal photocoagulation
at week 3
e. bevacizumab
2.5 mg upon entry and after 6 weeks
a. bevacizumab
1.0 mg (single dose)
b. triamcinolone
4.0 mg (single dose)
photodynamic therapy
verteporfin (single dose)
c. triamcinolone
4.0 mg
photodynamic therapy
verteporfin
a. bevacizumab
1.25 mg (single dose)
b. photodynamic therapy
verteporfin (single dose)
c. bevacizumab
1.25 mg within 1 hour after
photodynamic therapy
verteporfin
verteporfin (single dose)
a. triamcinolone
4.0 mg (upon entry)
b. bevacizumab
1.5 mg (upon entry)
a. bevacizumab
1.25 mg (upon entry)
b. bevacizumab
1.25 mg (upon entry)
triamcinolone
2.0 mg (upon entry)
c. macular laser photocoagulation single dose
a. bevacizumab
1.5 mg, week 3
panretinal photocoagulation
weeks 1 and 3
b. panretinal photocoagulation
weeks 1 and 3
a. bevacizumab
1.0 mg (mean of 4.5 treatments)
b. photodynamic therapy
verteporfin (mean of 1.9 treatments)
triamcinolone
4.0 mg (mean of 1.9 treatments)
Sao Paulo Med J. 2009; 127(2):84-91
diagnoses of age-related macular degeneration.18,19,23 One study tested
bevacizumab on patients with subfoveal choroidal neovascularization
associated with age-related macular degeneration.16 Finally, there was
one study that included patients with diagnoses of proliferative diabetic
retinopathy.22
With regard to the origin of the papers, two studies were conducted in Brazil,11,22 two in Iran,15,21 one in Lebanon,16 one in the United
States,17 one in Austria,23 one in Croatia19 and one in Germany.18 None
of these studies mentioned any financial support from pharmaceutical
companies.
Methodological quality of the studies included
Selection bias
Four studies were considered to present low risk of selection bias,
since they were properly conducted with regard to this factor.15,19,21,22
All other studies were considered to present moderate risk because, although their allocations were random, the methods used for generating randomization were not stated. One study allocated the eyes with
the worst visual acuity to receive panretinal photocoagulation in association with bevacizumab (eight eyes), while all other eyes were treated with panretinal photocoagulation alone (eight eyes), among patients
who were at high risk of proliferative diabetic retinopathy in both eyes.
For this reason, this study was considered to present a high risk of systematic error.22 Separate data on the group that was randomly allocated
were not available.
Performance bias
With the exception of three studies15,17,21 that made use of control
groups receiving sham injections or laser, none of the other studies reported any care taken to prevent performance bias.
All studies retrieved using the search
strategy, across all databases (n = 474)
Studies excluded: narrative reviews, in vitro/in situ
studies, animal and diagnostic studies, case reports,
retrospective case series and studies not dealing
with the clinical condition or intervention
of interest (n = 383)
Prospective studies on humans that
dealt with the clinical conditions and
intervention of interest (n = 91)
Prospective case series (n = 77)
Prospective randomized or nonrandomized
controlled trials on humans that dealt with
the clinical conditions and intervention
of interest (n = 14)
Nonrandomized controlled trials (n = 4);
controlled trial with randomization by eyes
instead of by patients and outcomes not
within the scope of this review (n = 1)
Randomized controlled trials on humans
that dealt with the clinical conditions
and intervention of interest (n = 9)
Figure 2. Flow chart of studies, from databases to inclusion in the
systematic review.
Bevacizumab for ocular neovascular diseases: a systematic review
Detection bias
The majority of the studies reported that the evaluators were unaware of the groups to which each patient (eyes) was allocated.15,16,19,21,22
Thus, only these five studies were considered to present a low risk of
detection bias. All the others were considered to present a high risk of
systematic error.
Attrition bias
None of the studies reported any substantial losses from their samples, either overall or among their comparison groups. For this reason,
all the studies were considered to present low risk of attrition bias.
Outcome measurements
Best-corrected visual acuity
Bevacizumab alone was shown to be better than the association of
bevacizumab and with triamcinolone for best-corrected visual acuity
(logMAR, change from baseline), but without a statistically significant
mean difference (MD) (MD, 0.02; 95% CI, - 0.09 to 0.14; P = 0.70].
However, in one study,15 the estimate effect favored the group treated
with bevacizumab in association with triamcinolone (MD, -0.03; 95%
CI, -0.13 to 0.07) (Figure 3, comparison 1; two studies15,21). Comparisons between bevacizumab (both in association with triamcinolone and
alone) and sham injections demonstrated statistically significant MD in
favor of the bevacizumab groups (MD, - 0.18; 95% CI, - 0.28 to -0.08;
P = 0.0003 and MD, - 0.15; 95% CI, - 0.26 to - 0.04; P = 0.008, respectively) (Figure 3, comparisons 2 and 3; one study15).
A statistically nonsignificant MD was observed for best-corrected
visual acuity (logMAR, endpoint), slightly favoring the group treated
with bevacizumab over the group treated with triamcinolone (MD,
0.01; 95% CI, - 0.04 to 0.06; P = 0.68) (Figure 3, comparison 4; one
study20). On the other hand, panretinal photocoagulation alone was
better, but without statistical significance, than when combined with
1.5 mg bevacizumab (MD, 0.02; 95% CI, - 0.12 to 0.16; P = 0.78)
(Figure 3, comparison 5; one study22). Bevacizumab (1.25 mg) in association with triamcinolone was also shown to be better than laser
photocoagulation alone (MD, - 0.11; 95% CI, - 0.30 to 0.08; P =
0.25) (Figure 3, comparison 6; one study21). For these two comparisons, the MD between the groups were not statistically significant.
On the other hand, comparison between bevacizumab alone and triamcinolone in association with photodynamic therapy showed a statistically significant difference in favor of bevacizumab with regard to
the endpoint of best-corrected visual acuity (P < 0.005) in one study.
However, the available estimated effect was not appropriate for inclusion in a forest plot.18
Bevacizumab alone was shown to be better than photodynamic
therapy for best-corrected visual acuity (logMAR, change from baseline), with a statistically significant MD (MD, - 0.09; 95% CI, - 0.13
to - 0.06; P < 0.00001) (Figure 3, comparison 7; one study19). Bevacizumab in association with photodynamic therapy was shown to be
better than both bevacizumab alone and photodynamic therapy alone,
with statistically significant MD (MD, -0.14; 95% CI, - 0.18 to - 0.11;
P < 0.00001 and MD, - 0.24; 95% CI, - 0.27 to - 0.20; P < 0.00001,
respectively) (Figure 3, comparisons 8 and 9; one study19).
Patients whose best-corrected visual acuity decreased
(logMAR, irrespective of authors criteria)
There was a statistically significant greater proportion of patients
whose visual acuity was not reduced by more than three lines in the
group treated with bevacizumab (2/46), compared with the group
treated with photodynamic therapy (15/44), with a risk ratio (RR)
of 0.19 (95% CI, 0.04 to 0.86; P = 0.03). It was necessary to change
three patients (NNT, number needed to treat) from photodynamic
therapy to bevacizumab to avoid an additional patient presenting any
losses in visual acuity (95% CI, 2 to 7) (Figure 4, comparison 1a; two
studies16,23).
Patients who achieved visual acuity > three lines
The proportion of patients who presented visual acuity greater than
three lines was higher and statistically significant in the group treated
with bevacizumab (32/32) than in the group treated with photodynamic therapy (22/30) (RR, 0.74; 95% CI, 0.59 to 0.92; P = 0.007 and
NNT = 4; 95% CI, 2 to 10) (Figure 4, comparison 1b; one study16).
Improvements from baseline in best-corrected visual acuity
A greater proportion of patients presented increased visual acuity (irrespective of authors criteria) in the group treated with bevacizumab (29/100) than in the group treated with photodynamic therapy alone or combined with triamcinolone (12/99) (RR, 0.49; 95%
CI, 0.31 to 0.78; P = 0.003 and NNT = 4; 95% CI, 1 to 4) (Figure
4, comparison 1c; three studies16,19,23). However, bevacizumab combined with photodynamic therapy was shown to benefit more patients
(22/55) than did photodynamic therapy alone (0/55), with RR of
0.02 (95% CI, 0.00 to 0.36; P = 0.007 and NNT = 2; 95% CI, 2 to
4) or bevacizumab alone (1/54), with RR of 0.05 (95% CI, 0.01 to
0.33; P = 0.002 and NNT = 3; 95% CI, 2 to 4) (Figure 4, comparisons 2 and 3, respectively; one study19). There was no statistically significant difference between focal photocoagulation alone (18/19) and
bevacizumab alone or combined with focal photocoagulation (82/90),
with RR of 0.96 (95% CI, 0.85 to 1.09; P = 0.54) (Figure 4, comparison 4; one study17).
Best-corrected visual acuity 20/40
A greater proportion of patients presented visual acuity 20/40 in
the group treated with bevacizumab (6/30) than in the group treated
with photodynamic therapy (0/32), without obtaining statistical significance in estimating this effect (RR, 0.08; 95% CI, 0.00 to 1.39;
P = 0.08 and NNT = 5; 95% CI, 3 to 25) (Figure 4, comparison 1d;
one study16).
Adverse events
Although the adverse events potentially associated with bevacizumab were of diverse types,24 the most common adverse events associated
with bevacizumab, irrespective of whether alone or not, were: moderate
anterior chamber reaction (19%),15 transient anterior chamber reaction
(16%),21 iris neovascularization (11%),15 subconjunctival hemorrhage,22
posterior vitreous detachment (15%)19 and foreign body sensation.22
More details about other adverse events are shown in Table 2.
Sao Paulo Med J. 2009; 127(2):84-91
87
Andriolo RB, Puga ME, Belfort Jnior R, Atallah AN
Comparison
Left Treatment versus Right Treatment
Mean Difference
Study
Mean
SD
Total
Mean
SD
Total Weight IV, Random, 95% CI
1. Bevacizumab + triamcinolone versus bevacizumab alone (change from baseline)
Ahmadieh 2007
-0.21
0.19
37
-0.18
0.26
41 53.7% -0.03 [-0.13, 0.07]
Soheilian 2007
-0.13
0.31
33
-0.22
0.23
37 46.3%
0.09 [-0.04, 0.22]
Subtotal (95% IC)
70
78 100.0%
0.02 [-0.09, 0.14]
Heterogeneity: Tau2 = 0.00; Chi2 = 2.07, df = 1 (P = 0.15); I2 = 52%
Test for effect: Z = 0.38 (P = 0.70)
2. Bevacizumab + triamcinolone versus sham (change from baseline)
Ahmadieh 2007
-0.21
0.19
37
-0.03
0.24
Test for effect: Z = 3.58 (P = 0.0003)
37 100.0% -0.18 [-0.28, -0.08]
3. Bevacizumab isolated versus sham (change from baseline)
Ahmadieh 2007
-0.18
0.26
41
-0.03
0.24
Test for effect: Z = 2.65 (P = 0.008)
37 100.0% -0.15 [-0.26, -0.04]
4. Bevacizumab versus triamcinolone: best-corrected visual acuity (endpoint)
Paccola 2007
0.9125 0.0744
13 0.9233 0.0572
13 100.0%
Test for effect: Z = 0.41 (P = 0.68)
0.01 [-0.04, 0.06]
5. Photocoagulation + bevacizumab versus photocoagulation alone (endpoint)
Tonello 2007
0.29 0.1549
15
0.31 0.1587
7 100.0%
Test for effect: Z = 0.28 (P = 0.78)
0.02 [-0.12, 0.16]
6. Bevacizumab + triamcinolone versus photocoagulation alone (endpoint)
Soheilian 2007
0.67
0.38
33
0.56
0.39
33 100.0%
Test for effect: Z = 1.16 (P = 0.25)
-0.11 [-0.30, 0.08]
7. Bevacizumab versus photodynamic therapy (change from baseline)
Lazic 2007
0.079 0.0937
54 -0.012 0.0956
Test for effect: Z = 5.02 (P < 0.00001)
Mean Difference
IV, Random, 95% CI
55 100.0% -0.09 [-0.13, -0.06]
8. Bevacizumab + photodynamic therapy versus bevacizumab (change from baseline)
Lazic 2007
0.223 0.0901
55 0.079 0.0937
54 100.0% -0.14 [-0.18, -0.11]
Test for effect: Z = 8.18 (P < 0.00001)
9. Bevacizumab + photodynamic therapy versus photodynamic therapy (change from baseline)
Lazic 2007
0.223 0.0901
55 -0.012 0.0937
54 100.0% -0.24 [-0.27, -0.20]
Test for effect: Z = 13.34 (P < 0.00001)
-0.2
-0.1
0
-0.1
-0.2
Favours Left Treament Favours Right Treament
95% CI = 95% confidence interval; Change from baseline: means of individual differences between baseline and endpoint; I2 = inconsistency or heterogeneity test, showing statistically significant (or substantial)
heterogeneity between estimated effects from studies included, when I2 > 50%. Tau2 = variance between studies in meta-analysis based on random effects. Intersection between horizontal lines (confidence intervals) and
horizontal line (null hypothesis) means absence of statistical significance between comparison groups. Gray lines illustrate the estimate effects (mean difference between comparison groups). Lozenge illustrates resultant
meta-analysis.
Figure 3. Mean best-corrected visual acuity (logMAR: endpoint and change from baseline).
DISCUSSION
Based on the primary outcome that we planned to analyze in this systematic review, the results showed that intraocular use of bevacizumab
alone was better than photodynamic therapy (alone or combined with
triamcinolone) for patients with subfoveal choroidal neovascularization
associated with age-related macular degeneration, choroidal neovascularization due to age-related macular degeneration and age-related macular
degeneration alone, as reported by the authors of the primary studies. Bevacizumab combined with photodynamic therapy was shown to be better than photodynamic therapy alone and bevacizumab alone for patients
88
Sao Paulo Med J. 2009; 127(2):84-91
diagnosed with choroidal neovascularization due to age-related macular
degeneration. On the other hand, photocoagulation was shown to be better than bevacizumab (alone or combined with photocoagulation) for patients diagnosed with diabetic macular edema, but this finding was not
statistically significant, probably because of the small sample size.
Despite the sensitivity of the search strategy used and the large
number of published papers on this subject (474 studies), only nine
trials satisfied the strict inclusion criteria. These studies presented the
minimum methodological rigor appropriate for this type of question
(i.e. regarding disease treatment) since they were clinical trials with random allocation.25 However, it needs to be noted that the allocation of
Bevacizumab for ocular neovascular diseases: a systematic review
Comparison
Left Treatment versus Right Treament
Outcome
Study
Events
Total
Events
Total
Weight
1. Bevacizumab versus photodynamic therapy (alone or combined with triamcinolone)
a. Patients who lost their visual acuity from baseline (irrespective of authors definition)
Bashushur 2007
0
32
8
30
38.7%
Weigert 2007
2
14
7
14
61.3%
Subtotal (95% CI)
46
44
100.0%
Total events
2
15
Heterogeneity: Tau2 = 0.31; Chi2 = 1.24, df = 1 (P = 0.26); I2 = 20%
Test for overall effect: Z = 2.15 (P = 0.03)
b. Best-corrected visual acuity > 3 lines
Bashshur 2007
32
32
Test for effect: Z = 2.71 (P = 0.007)
22
c. Improved visual acuity (irrespective of authors definition)
Bashshur 2007
16
32
5
Lazic 2007
1
54
0
Weigert 2008
12
14
7
Subtotal (95% CI)
100
Total events
29
12
Heterogeneity: Tau2 = 0.00; Chi2 = 0.61, df = 2 (P = 0.74); I2 = 0%
Test for overall effect: Z = 2.58 (P = 0.010)
d. Best-corrected visual acuity 20/40
Bashshur 2007
6
30
Test for effect: Z = 1.73 (P = 0.008)
30
30
55
14
99
Risk Ratio
Risk Ratio
M-H, Random, 95% CI
M-H, Random, 95% CI
0.06 [0.00, 0.92]
0.29 [0.07, 1.14]
0.19 [0.04, 0.86]
0.74 [0.59, 0.92]
47.0%
13.7%
39.4%
100.0%
32
2. Bavacizumab combined with photodynamic therapy versus photodynamic therapy
a. Improved visual acuity (irrespective of authors definition)
Lazic 2007
22
55
0
55
Test for effect: Z = 2.69 (P = 0.007)
3. Bavacizumab combined with photodynamic therapy versus bevacizumab
a. Improved visual acuity (irrespective of authors definition)
Lazic 2007
22
55
1
54
Test for effect: Z = 3.16 (P = 0.002)
4. Photocoagulation versus bevacizumab alone or combined with photocoagulation
a. Improved visual acuity (irrespective of authors definition)
DRCN 2007
18
19
82
90
Test for effect: Z = 0.62 (P = 0.54)
0.33 [0.14, 0.80]
0.33 [0.01, 7.86]
0.58 [0.33, 1.03]
0.49 [0.31, 0.78]
0.08 [0.00, 1.39]
0.02 [0.00, 0.36]
0.05 [0.01, 0.33]
0.96 [0.85, 1.09]
0.002
0.1
1
10
500
Favours Left Treatment Favours Right Treatment
95% CI = 95% confidence interval; I2 = inconsistency or heterogeneity test, showing statistically significant (or substantial) heterogeneity between estimated effects from studies included, when I2 > 50%. Tau2 = variance
between studies in meta-analysis based on random effects. Intersection between horizontal lines (confidence intervals) and horizontal line (null hypothesis) means absence of statistically significant differences between
comparison groups. Gray lines illustrate the estimate effects (risk ratio between comparison groups). Lozenges illustrate resultant meta-analysis.
Figure 4. Risk ratio for dichotomous outcomes.
participants in the subgroup at high risk of proliferative diabetic retinopathy in both eyes was not random in one study.22 Furthermore, in
one study,23 the nature of the interventions allowed concealment of the
allocation and blinding of patients and therapists regarding the use of
bevacizumab or triamcinolone, but blinding would not be operationally
easy for photodynamic therapy. It was decided to include these studies,
given the lack of high-quality controlled studies on the application of
bevacizumab for treating ocular diseases at the time when this systematic review was implemented.
The fact that Mirshahi et al.14 was not included in this review deserves attention. Today, the internal validity of studies in which the eyes
of a single patient are allocated to different groups is considered to be
unclear. This is illustrated by the existence of contradictory studies. Indeed, there is evidence from studying the pharmacokinetic aspects of
bevacizumab that the possibility of contralateral effects (through systemic absorption of the drug by the contralateral eye) is remote.26 On
the other hand, there is evidence demonstrating the opposite, through
manifestations of adverse events associated with bevacizumab in the
Sao Paulo Med J. 2009; 127(2):84-91
89
Andriolo RB, Puga ME, Belfort Jnior R, Atallah AN
Table 2. Adverse events
Adverse events
Anemia17
Cataract progression19
Congestive heart failure17
Death17
Elevation of blood pressure17
Endophthalmitis17
Foreign Body sensation22
Intraocular pressure rise15,17,20,21,23
Iris neovascularization15
Marked anterior chamber reaction15
Moderate anterior chamber reaction15
Myocardial infarction17
Peripheral vascular disease17
Pigment epithelial tears19
Posterior vitreous detachment19
Progression of fibrous proliferation15
Subconjunctival hemorrhage22
Syncope17
Transient anterior chamber reaction21
Transient intraocular pressure rise17
Vitreous hemorrhage15
Worsened renal function17
Bv
% (n/N)
4 (4/90)
7 (4/54)
1 (1/90)
2 (2/90)*
1 (1/90)
1 (1/90)
4 (1/124)
22 (9/41)
2 (1/41)
19 (8/41)
2 (2/90)
1 (1/90)
3 (3/54)
15 (8/54)
2 (1/41)
1 (1/90)
19 (7/37)
1 (1/90)
0 (0/41)
3 (3/90)
Pg + Bv
% (n/N)
13 (2/15)
47 (7/15)
-
Tr + Bv
% (n/N)
8 (6/70)
0 (0/37)
3 (1/37)
19 (7/37)
0 (0/37)
12 (4/33)
3 (1/37)
-
PDT + Bv
% (n/N)
6 (3/50)
0 (0/50)
8 (4/50)
-
Comparison groups
Sham
Pg
% (n/N)
% (n/N)
5 (1/19)
0 (0/19)
0 (0/19)
0 (1/19)
0 (0/19)
0 (0/7)
0 (0/37)
0 (0/52)
0 (0/37)
0 (0/37)
0 (0/37)
0 (0/19)
10 (2/19)
0 (0/37)
0 (0/7)
0 (0/19)
0 (0/33)
0 (0/19)
0 (0/37)
0 (0/19)
PDT
% (n/N)
0 (0/52)
0 (0/52)
0 (0/52)
-
Tr
% (n/N)
7 (1/13)
-
PDT + Tr
% (n/N)
14 (2/14)
-
The percentages were obtained from all studies reporting at least one event in the bevacizumab group (irrespective of whether combined with other options or alone). Bv = Bevacizumab; Pg = Photocoagulation; Tr = Triamcinolone;
PDT = Photodynamic therapy.
*Reported causes of death were myocardial infarction and pancreatic cancer.
contralateral eye.7 Therefore, it seems sensible for the time being for
researchers to choose types of allocation other than involving different
treatments for each eye of the same individual.
The present scenario is that, taken together, the studies that have
been published are still of an exploratory nature, given the diversity of
comparisons, co-interventions, dosages and variables of interest (outcome measurements), along with the variety of ways of reporting these
variables. Thus, it is recommended that the specialists within this field
should come to a consensus regarding which outcomes are relevant and
how these should be analyzed.
It is possible to estimate the costs associated with bevacizumab.
Bashur et al. found that an average of 2.4 treatments with 2.5 mg bevacizumab per patient was needed to treat persistent subretinal fluid or cystic macular disease, and that 2.3 treatments with photodynamic therapy
were needed when leakage from choroidal neovascularization was present
on fluorescein angiography over a six-month period.16 The gross cost of
bevacizumab is about USD 5.5 per mg (United States dollars).27 The assumed cost of photodynamic therapy with verteporfrin, or Visudyne is
USD 3,000.00.28 The meta-analysis demonstrated that, in order to improve visual acuity in one patient, 3.45 patients (29/100) would have to
be treated with Bevacizumab and 8.25 patients (12/99) with photodynamic therapy (Figure 4, comparison 1c). The estimated expense would
be USD 113.85 for bevacizumab and USD 56,925.00 for photodynamic
therapy. Considering the findings of Brown et al.,29 an average of 11 treatments of 0.5 mg ranibizumab per patient would have to be administered,
at a cost of USD 3,900.00 per mg. 27 To improve visual acuity, defined as
15 letters at 12 months, 2.48 patients (56/139) would have to be treated with ranibizumab. The estimated cost would be USD 53,196.00.
90
Sao Paulo Med J. 2009; 127(2):84-91
Results from future trials may provide more information about
the wide variety of types of outcome measurements (including adverse
events), comparisons and co-interventions, such as photodynamic therapy, laser photocoagulation, triamcinolone and vitrectomy.
REFERENCES
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
Spaide RF. Rationale for combination therapies for choroidal neovascularization. Am J
Ophthalmol. 2006;141(1):149-56.
Lee PP, Feldman ZW, Ostermann J, Brown DS, Sloan FA. Longitudinal prevalence of major eye
diseases. Arch Ophthalmol. 2003;121(9):1303-10.
Strom BL, Carson JL, Halpern AC, et al. A population-based study of Stevens-Johnson syndrome. Incidence and antecedent drug exposures. Arch Dermatol. 1991;127(6):831-8.
Ferrara N, Hillan KJ, Gerber HP, Novotny W. Discovery and development of bevacizumab, an
anti-VEGF antibody for treating cancer. Nat Rev Drug Discov. 2004;3(5):391-400.
Grisanti S, Ziemssen F. Bevacizumab: off-label use in ophthalmology. Indian J Ophthalmol.
2007;55(6):417-20.
Bevacizumab (Avastin) Coverage for neovascular (Wet) macular degeneration. Cahaba
GBA Medicare B Newsline. 2008. p. 11. Available from: https://www.cahabagba.com/
part_b/education_and_outreach/newsletters/2008/2008_03NL.pdf. Accessed in 2009
(Apr 15).
Neri P, Mariotti C, Mercanti L, Salvolini S, Giovannini A. Vitritis in the contralateral uninjected
eye following intravitreal bevacizumab (Avastin). Int Ophthalmol. 2008;28(6):425-7.
Feinstein AR. An outline from cause-effect evaluations. In: Clinical Epidemiology: The Architecture of Clinical Research. Philadelphia: WB Saunders; 1985. p. 39-52.
Review Manager (RevMan) [Computer program]. Version 5.0. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2007.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):17788.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med.
2002;21(11):1539-58.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses.
BMJ. 2003;327(7414):557-60.
Vedula SS, Krzystolik MG. Antiangiogenic therapy with anti-vascular endothelial growth factor
Bevacizumab for ocular neovascular diseases: a systematic review
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
modalities for neovascular age-related macular degeneration. Cochrane Database Syst Rev.
2008;(2):CD005139.
Mirshahi A, Roohipoor R, Lashay A, Mohammadi SF, Abdoallahi A, Faghihi H. Bevacizumabaugmented retinal laser photocoagulation in proliferative diabetic retinopathy: a randomized double-masked clinical trial. Eur J Ophthalmol. 2008;18(2):263-9.
Ahmadieh H, Ramezani A, Shoeibi N, et al. Intravitreal bevacizumab with or without triamcinolone for refractory diabetic macular edema; a placebo-controlled, randomized clinical
trial. Graefes Arch Clin Exp Ophthalmol. 2008;246(4):483-9.
Bashshur ZF, Schakal A, Hamam RN, El Haibi CP, Jaafar RF, Noureddin BN. Intravitreal bevacizumab vs verteporfin photodynamic therapy for neovascular age-related macular degeneration. Arch Ophthalmol. 2007;125(10):1357-61.
Diabetic Retinopathy Clinical Research Network, Scott IU, Edwards AR, et al. A phase II
randomized clinical trial of intravitreal bevacizumab for diabetic macular edema. Ophthalmology. 2007;114(10):1860-7.
Hahn R, Sacu S, Michels S, et al. Intravitreales Bevacizumab vs. Verteporfin und intravitreales Triamcinolon Acetonid bei Patienten mit neovaskulrer AMD [Intravitreal bevacizumab
versus verteporfin and intravitreal triamcinolone acetonide in patients with neovascular agerelated macula degeneration]. Ophthalmologe. 2007;104(7):588-93.
Lazic R, Gabric N. Verteporfin therapy and intravitreal bevacizumab combined and alone
in choroidal neovascularization due to age-related macular degeneration. Ophthalmology.
2007;114(6):1179-85.
Paccola L, Costa RA, Folgosa MS, Barbosa JC, Scott IU, Jorge R. Intravitreal triamcinolone
versus bevacizumab for treatment of refractory diabetic macular oedema (IBEME study). Br
J Ophthalmol. 2008;92(1):76-80.
Soheilian M, Ramezani A, Bijanzadeh B, et al. Intravitreal bevacizumab (avastin) injection
alone or combined with triamcinolone versus macular photocoagulation as primary treatment of diabetic macular edema. Retina. 2007;27(9):1187-95.
Tonello M, Costa RA, Almeida FP, Barbosa JC, Scott IU, Jorge R. Panretinal photocoagulation versus PRP plus intravitreal bevacizumab for high-risk proliferative diabetic retinopathy
(IBeHi study). Acta Ophthalmol. 2008;86(4):385-9.
Weigert G, Michels S, Sacu S, et al. Intravitreal bevacizumab (Avastin) therapy versus photodynamic therapy plus intravitreal triamcinolone for neovascular age-related macular degeneration: 6-month results of a prospective, randomised, controlled clinical study. Br J
Ophthalmol. 2008;92(3):356-60.
24. Fung AE, Rosenfeld PJ, Reichel E. The International Intravitreal Bevacizumab Safety Survey: using the internet to assess drug safety worldwide. Br J Ophthalmol. 2006;90(11):
1344-9.
25. Moher D, Pham B, Jones A, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet. 1998;352(9128):
609-13.
26. Bakri SJ, Snyder MR, Reid JM, Pulido JS, Singh RJ. Pharmacokinetics of intravitreal bevacizumab (Avastin). Ophthalmology. 2007;114(5):855-9.
27. Steinbrook R. The price of sight--ranibizumab, bevacizumab, and the treatment of macular
degeneration. N Engl J Med. 2006;355(14):1409-12.
28. Photodynamic therapy. Available from: http://www.mdsupport.org/library/photther.html.
Accessed in 2009 (Apr 15).
29. Brown DM, Kaiser PK, Michels M, et al. Ranibizumab versus verteporfin for neovascular agerelated macular degeneration. N Engl J Med. 2006;355(14):1432-44.
Sources of funding: Science and Technology Department of the Science Secretariat, Brazilian Ministry of Health. The sponsor had no role in the design and conduct of the study or
in collection, management, analysis and interpretation of the data or in preparation, review
or approval of the manuscript
Conflict of interest: None known
Date of first submission: October 24, 2008
Last received: March 31, 2009
Accepted: April 23, 2009
Address for correspondence:
lvaro Nagib Atallah
Rua Borges Lagoa, 564 Conjunto 63
Edifcio Espao So Paulo
So Paulo (SP) Brasil CEP 04038-000
Tel. (+55 11) 5571-4721
E-mail: atallahmbe@uol.com.br
Sao Paulo Med J. 2009; 127(2):84-91
91
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Grant L Et Al 2018 Integratign Palliative Care Into National Health Systems in AfricaDokumen12 halamanGrant L Et Al 2018 Integratign Palliative Care Into National Health Systems in AfricadanielnegraoBelum ada peringkat
- English Translation of Radbruch's ThesisDokumen21 halamanEnglish Translation of Radbruch's ThesisclapyourcarpalsBelum ada peringkat
- Murray SA Et Al Illness Trajectories and Palliative Care PDFDokumen5 halamanMurray SA Et Al Illness Trajectories and Palliative Care PDFdanielnegraoBelum ada peringkat
- 1.3 The Special Case ThesisDokumen11 halaman1.3 The Special Case ThesisdanielnegraoBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Secrets of Psychic HealingDokumen140 halamanSecrets of Psychic Healingkonoha G100% (39)
- Biological Control 178 (2023) 105145 M. Yousefvand Et AlDokumen5 halamanBiological Control 178 (2023) 105145 M. Yousefvand Et AlGenaina CristofoliBelum ada peringkat
- Book of Vile DarknessDokumen25 halamanBook of Vile Darknessv0idless100% (2)
- Couser Signifying Bodies - ExtractDokumen79 halamanCouser Signifying Bodies - ExtractMarceloBelum ada peringkat
- Ms. Michelle Lau Sook Yee (First Speaker)Dokumen5 halamanMs. Michelle Lau Sook Yee (First Speaker)Nurhidayah MuhamadBelum ada peringkat
- Boaz Gobera (NsambyaHospitalReport2021)Dokumen62 halamanBoaz Gobera (NsambyaHospitalReport2021)GOBERA BOAZBelum ada peringkat
- Pom Maker The Ultimate Yarn Guide For Pompom MakingDokumen20 halamanPom Maker The Ultimate Yarn Guide For Pompom MakingMaciek PikułaBelum ada peringkat
- Single Best Answer Question-Writing Tips For Clinicians: J L Walsh, B H L Harris, P E SmithDokumen6 halamanSingle Best Answer Question-Writing Tips For Clinicians: J L Walsh, B H L Harris, P E SmithSandro ToninBelum ada peringkat
- Air Traffic Controllers Warned on Sleeping on the JobDokumen108 halamanAir Traffic Controllers Warned on Sleeping on the Jobeduardo juniorBelum ada peringkat
- The Impact of Life Cycles on Family HealthDokumen27 halamanThe Impact of Life Cycles on Family Healthmarcial_745578124Belum ada peringkat
- Course On Lamellar Corneal SurgeryDokumen3 halamanCourse On Lamellar Corneal SurgerydrfoglaBelum ada peringkat
- Budwig Cancer GuideDokumen116 halamanBudwig Cancer GuideStanley ChanBelum ada peringkat
- Elderly Hip FractureDokumen9 halamanElderly Hip FractureIlyes FerenczBelum ada peringkat
- IMCI child health strategyDokumen11 halamanIMCI child health strategyIvy100% (2)
- The Vanuatu Cooking Project ProposalDokumen6 halamanThe Vanuatu Cooking Project ProposalBunga Melur MewangiBelum ada peringkat
- Col, Major Among 5 Martyred While Rescuing Hostages in J&KDokumen14 halamanCol, Major Among 5 Martyred While Rescuing Hostages in J&KAshisBelum ada peringkat
- Clinical For PracticalDokumen72 halamanClinical For PracticalYogendra SinghBelum ada peringkat
- Managing Fatigue During PregnancyDokumen2 halamanManaging Fatigue During PregnancyBlanz Irybelle KindomBelum ada peringkat
- Census August 8 - August 9, 2020Dokumen6 halamanCensus August 8 - August 9, 2020Patrick JohnBelum ada peringkat
- NAIOMT C-516 Cervical Spine I (v2014)Dokumen4 halamanNAIOMT C-516 Cervical Spine I (v2014)bmj123Belum ada peringkat
- Allele-specific expression of variant-specific surface proteins in Giardia lambliaDokumen7 halamanAllele-specific expression of variant-specific surface proteins in Giardia lambliawiwienBelum ada peringkat
- ShaylaDokumen3 halamanShaylaapi-530728661Belum ada peringkat
- Basics of Microvascular SurgeryDokumen33 halamanBasics of Microvascular SurgeryPratikshya KothiaBelum ada peringkat
- Nursing Care of Clients Undergoing Eye SurgeryDokumen1 halamanNursing Care of Clients Undergoing Eye SurgerySewyel GarburiBelum ada peringkat
- Ingrown Nail RemovalDokumen28 halamanIngrown Nail RemovaljaphetnwapiBelum ada peringkat
- Izatizon, As An Izatin-Thiosemicarbazone Derivative, Has Antiviral, Anti-Tumor Actions and No Side EffectsDokumen3 halamanIzatizon, As An Izatin-Thiosemicarbazone Derivative, Has Antiviral, Anti-Tumor Actions and No Side EffectsinventionjournalsBelum ada peringkat
- Nucleotides, Nucleic Acids, and Heredity: Bettelheim / Brown / Campbell / Farrell / TorresDokumen55 halamanNucleotides, Nucleic Acids, and Heredity: Bettelheim / Brown / Campbell / Farrell / TorresMica BernardoBelum ada peringkat
- Oman New Health Application FormDokumen3 halamanOman New Health Application FormAravind AlavantharBelum ada peringkat
- Management of The Medically Compromised Dental PatientDokumen40 halamanManagement of The Medically Compromised Dental PatientabodyzizoBelum ada peringkat
- Anticoagulation Options For Intermittent HDDokumen10 halamanAnticoagulation Options For Intermittent HDNarinder SharmaBelum ada peringkat