Diunggah oleh
Juanjo SolanoHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Diunggah oleh
Juanjo SolanoHak Cipta:
Format Tersedia
Home
Search
Collections
Journals
About
Contact us
My IOPscience
Hybrid printing of mechanically and biologically improved constructs for cartilage tissue
engineering applications
This content has been downloaded from IOPscience. Please scroll down to see the full text.
2013 Biofabrication 5 015001
(http://iopscience.iop.org/1758-5090/5/1/015001)
View the table of contents for this issue, or go to the journal homepage for more
Download details:
IP Address: 186.176.90.127
This content was downloaded on 22/10/2015 at 13:59
Please note that terms and conditions apply.
IOP PUBLISHING
BIOFABRICATION
doi:10.1088/1758-5082/5/1/015001
Biofabrication 5 (2013) 015001 (10pp)
Hybrid printing of mechanically and
biologically improved constructs for
cartilage tissue engineering applications
Tao Xu 1 , Kyle W Binder 1 , Mohammad Z Albanna, Dennis Dice,
Weixin Zhao, James J Yoo and Anthony Atala 2
Wake Forest Institute for Regenerative Medicine, Wake Forest University Health Sciences,
Medical Center Blvd, Winston-Salem, NC 27157, USA
E-mail: aatala@wakehealth.edu
Received 27 April 2012
Accepted for publication 18 October 2012
Published 21 November 2012
Online at stacks.iop.org/BF/5/015001
Abstract
Bioprinting is an emerging technique used to fabricate viable, 3D tissue constructs through the
precise deposition of cells and hydrogels in a layer-by-layer fashion. Despite the ability to
mimic the native properties of tissue, printed 3D constructs that are composed of
naturally-derived biomaterials still lack structural integrity and adequate mechanical properties
for use in vivo, thus limiting their development for use in load-bearing tissue engineering
applications, such as cartilage. Fabrication of viable constructs using a novel multi-head
deposition system provides the ability to combine synthetic polymers, which have higher
mechanical strength than natural materials, with the favorable environment for cell growth
provided by traditional naturally-derived hydrogels. However, the complexity and high cost
associated with constructing the required robotic system hamper the widespread application of
this approach. Moreover, the scaffolds fabricated by these robotic systems often lack
flexibility, which further restrict their applications. To address these limitations, advanced
fabrication techniques are necessary to generate complex constructs with controlled
architectures and adequate mechanical properties. In this study, we describe the construction
of a hybrid inkjet printing/electrospinning system that can be used to fabricate viable tissues
for cartilage tissue engineering applications. Electrospinning of polycaprolactone fibers was
alternated with inkjet printing of rabbit elastic chondrocytes suspended in a fibrincollagen
hydrogel in order to fabricate a five-layer tissue construct of 1 mm thickness. The
chondrocytes survived within the printed hybrid construct with more than 80% viability one
week after printing. In addition, the cells proliferated and maintained their basic biological
properties within the printed layered constructs. Furthermore, the fabricated constructs formed
cartilage-like tissues both in vitro and in vivo as evidenced by the deposition of type II collagen
and glycosaminoglycans. Moreover, the printed hybrid scaffolds demonstrated enhanced
mechanical properties compared to printed alginate or fibrincollagen gels alone. This study
demonstrates the feasibility of constructing a hybrid inkjet printing system using off-the-shelf
components to produce cartilage constructs with improved biological and mechanical
properties.
(Some figures may appear in colour only in the online journal)
1
2
These authors contributed equally to this work.
Author to whom any correspondence should be addressed.
1758-5082/13/015001+10$33.00
2013 IOP Publishing Ltd
Printed in the UK & the USA
Biofabrication 5 (2013) 015001
T Xu et al
1. Introduction
transfection of living cells [17]. These experiments support
the use of inkjet bioprinting as a low cost fabrication method
and provide a glimpse of its future potential.
However, like many other bioprinting approaches, inkjet
bioprinting technology utilizes hydrogels as the primary
scaffold materials for printed cells [18]. Although a variety
of tissue constructs can be fabricated with these gel-based
scaffolds, these gels often have limited structural integrity
due to their low mechanical strength [19, 20]. This limitation
hinders development of printed constructs for use in loadbearing tissue engineering applications, such as those designed
to repair or replace cartilage and bone.
We hypothesized that these mechanical limitations
associated with printed hydrogel constructs could be overcome
by using inkjet printing techniques in conjunction with
electrospinning, which is another fabrication technique that
can create nanofibrous scaffolds of synthetic polymer. By
combining flexible mats of electrospun synthetic polymer
with traditional inkjet printing in a layer-by-layer fashion,
functional tissue constructs with enhanced mechanical
properties could be fabricated. In this study, we first
determined whether electrospinning could be employed
in conjunction with inkjet-based cell printing to produce
constructs with enhanced mechanical properties that would
be suitable for cartilage tissue engineering in a proofof-concept design. We then evaluated the functionality of
the resulting constructs in terms of four parameters: cell
survival, maintenance of the layered structure, mechanical
properties, and formation of cartilage-specific extracellular
matrix. Generation of organized layered cartilage constructs
with improved biological and mechanical properties would
have numerous applications clinically. In particular, to meet
the depth-dependent cellular and matrix properties properties
of articular cartilage, biomimetic zonal cartilage repair and
regeneration using modular hydrogel systems has been
envisioned [21]. Our hybrid method allows for control over
construct organization and might have potential to these
applications involving complex zonal properties to tissueengineered constructs for cartilage repair.
Naturally-derived hydrogels such as collagen, fibrin and elastin
have advanced the field of biomaterials in tissue engineering
and regenerative medicine because their composition and
structure resembles that of native tissue [1, 2]. Organ/tissue
printing using inkjet technology is evolving into a practical
method to fabricate viable 3D tissue constructs and has found
widespread applications in the field of tissue engineering and
regenerative medicine [3, 4]. The bioprinting approach often
utilizes naturally-derived hydrogels as cell-printing solutions
to construct tissues in layer-by-layer fashion due to their
superior biocompatibility and low toxicity on the cells [5].
However, the low to moderate mechanical properties of
these hydrogels hinder their utility in load-bearing tissue
engineering applications, such as cartilage, because they are
unable to provide proper 3D structural integrity during surgical
procedures and the regenerative process [6].
Fabrication methods such as solid free form technology,
which is based on computer-aided design/computer-aided
manufacturing, has been employed to fabricate 3D scaffolds
[7]. Despite its ability to control the scaffold porosity, the
scaffold, which often is made of a synthetic polymer, does not
provide the proper affinitive environment to the cells due to the
polymer hydrophobicity properties [8]. Multi-head deposition
systems (MHDS) offer the ability to fabricate hybrid scaffolds
using both synthetic polymers and hydrogel materials. The
hybrid scaffold provides a favorable environment within the
hydrogel for the cells to grow and can possess adequate
mechanical properties that can be altered depending on the
synthetic polymer used during fabrication. Recently, MHDS
was employed to fabricate hybrid scaffolds using synthetic
polymers such as PCL and polyglycolic acid incorporated
within hydrogels such as alginate, gelatin, and hyaluronic
acid as a cell-printing solution [6, 8, 9]. While the ability to
precisely deposit cells and materials has been well-established,
most robotic precision deposition machines are often complex,
expensive to manufacture and require special skills to operate.
By combining synthetic polymers and natural hydrogels, these
systems can offer a hybrid scaffold system, but the main
frame of the scaffold, composed of bulk synthetic polymers,
is very rigid and lack of flexibility, which might not be
suitable for cartilage tissue engineering. Deposition of these
components can also be achieved by inkjet printing system
using off-the-shelf components and provides a platform in
which multiple cell types can be deposited into a construct.
This technique can provide many of the similar functions as
a robotic deposition system but can be effectively utilized
with little specialized equipment [10, 11]. Inkjet technology
has been used in many applications to produce high density
patterns of DNA for microarrays [12], microdepositions of
proteins for enzyme assays [13] and high density arrays of
bacterial colonies [14]. The technique has also been applied
to high-throughput patterning of mammalian cells, including
Chinese hamster ovary cells [15] and hippocampal cells [16].
Even more recently, it has been shown that the environmental
conditions generated during the printing process, such as heat
and shear stress, can be used to perform high-throughput
2. Materials and methods
2.1. Materials
Poly(-caprolactone) (PCL) (704105, average Mn 42,500),
Pluronic F-127 (P2443), fibrinogen from bovine plasma
(F8630) and thrombin from bovine plasma (T4648) were all
purchased from Sigma-Aldrich (St. Louis, MO). Collagen
type I derived from rat tail (354236) was purchased from
BD Biosciences (Billerica, MA). All reagents were chemical
grade.
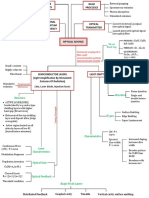
2.2. Construction of the hybrid printing system
To build cartilage constructs, we developed a novel hybrid
printing system by incorporating an electrospinning apparatus
into an inkjet printing platform. Figures 1(A) and (B) show
the schematic drawing of this hybrid printing system and the
actual hybrid printing system after construction, respectively.
2
Biofabrication 5 (2013) 015001
T Xu et al
(A)
(B)
Figure 1. (A) Schematic representation of the hybrid printing system shows the inkjet printhead and the electrospinning printhead. (B) The
actual prototype of the hybrid printing system after construction.
The inkjet printing platform is composed of a customized
XYZ plotter driven by step motors. The printhead was
equipped with a dc solenoid inkjet valve (Offshore Solutions
Inc, Beaverton, OR). Reservoirs for loading the cell suspension
to be printed were connected to the inkjet valve. The cellprinting solution was supplied to the inkjet valve from the
reservoirs using pressurized air. The printhead was mounted
over a XYZ plotter platform to allow deposition of cells
onto the scaffold generated by electrospinning. The XYZ
plotter was positioned under the printhead via a customized
controller. The controller acquires the positioning information
from custom software built on the .NET Framework 2.0
(Microsoft Corp, Redmond, WA). The software converts the
image of the target to a special four byte protocol, which is
used to activate a specific inkjet valve and coordinate XYZ
position.
In this hybrid system, the electrospinning apparatus
is used to generate a polymeric fiber-based scaffold. An
electrospinning head, in tandem with the inkjet head, was
also mounted over the XYZ plotter. The power supply, which
is used to provide a high voltage field for electrospinning,
was modulated by the same customized controller. To prevent
the potential adverse effects of static discharge on the logic
circuitry of the customized controller, the controller was
conductively isolated from the high voltage power supply
through fiber optics.
2.4. Isolation and culture of rabbit articular chondrocytes
Chondrocytes were obtained from rabbit ear cartilage as
described previously [23]. Briefly, the rabbit was sedated
and the ear was shaved, cleaned with povidone-iodine, and
draped. A pocket was resected under sterile conditions at the
subperichondrial level and an approximately 2 2 cm piece
of cartilage was removed. Biopsy specimens were washed
in phosphate-buffered saline (PBS) and finely minced under
sterile conditions. To disassociate chondrocytes from the
cartilage tissue, the minced cartilage was incubated in Hams
F12 medium with glutamine/bicarbonate supplemented with
10% fetal bovine serum (FBS), 100 U ml1 penicillin,
100 g ml1 streptomycin, 2.5 g ml1 amphotericin B
(Gibco-BRL), and 1 mg ml1 collagenase type B (Boehringer
Mannheim GmbH, Germany) at 37 C on an orbital shaker.
After 24 h, the undigested pieces were discarded and the
supernatant was collected and distributed onto fresh tissue
culture dishes. Every dish was filled with 20 ml of fresh
Dulbeccos modified Eagles medium (DMEM) supplemented
with 10% FBS, 1% antibiotic-antimycotic (ABAM) and 1%
L-glutamine. Cell cultures were incubated in a humidified
incubator in 5% CO2 at 37 C. Culture media was changed
every three to four days. To prepare the cell printing solution,
cell pellets at passage 6 were re-suspended in a mixture of
fibrinogen (10 mg ml1) and rat tail collagen type I (1.5 mg
ml1) in PBS at a concentration of 34 106 cells ml1 and
loaded into cell reservoirs.
2.3. Preparation of polymer solution
2.5. Fabrication of cartilage constructs
PCL (10% wt/vol) and Pluronic F-127 (5% wt/vol) were
dissolved in acetone under gentle stirring in a warm water bath
(50 C). Acetone was used as a solvent because it is a natural
byproduct of ketone body synthesis in the liver. Pluronic F-127
was added to the polymer solution to reduce the viscosity of
molten PCL and also improve the hydrophilicity properties of
the resulting electrospun PCL scaffold [22]. The final polymer
solution was loaded into the polymer reservoirs of the printing
system.
A layer of PCL was electrospun for 30 min at 3 ml h1 at
20 kilovolts (KV) through an 18.5 gauge blunt needle syringe.
The syringe was placed 8 cm above a sterile 10 cm petri
dish containing sterile PBS. A sheet of aluminum foil was
placed directly under the petri dish and to act as the ground
for the system and force the PCL to spin directly into
the PBS. Wet electrospinning was necessary because dry
PCL/F-127 rapidly absorbs water from printed constructs
and leads to desiccation of the cells. After spinning a
3
Biofabrication 5 (2013) 015001
T Xu et al
layer of PCL, 3 ml of the cell-printing solution containing
chondrocytes/fibrinogen/collagen was printed through the
inkjet valve onto the electrospun PCL fibrous scaffold layer
to form a cell/matrix layer. The cell-printing solution was
allowed to gel through subsequent printing of 1.5 ml thrombin
(20 UI ml1 dissolved in PBS) on the cell/matrix layer to
create a transient clot for structural integrity while spinning.
The thrombin layer was allowed to react with the fibrinogen
for 15 min. Subsequently, PCL was spun again for another
10 min at 3 ml h1 followed by inkjet printing of the cellprinting solution and thrombin. A final layer of PCL was spun
for 30 min at 3 ml h1. The final construct consisted of five
alternating layers of PCL/F-127 (three electrospun layers) and
chondrocytes (two gel layers) with an approximate thickness
of 1 mm. Each of the two gel layers was approximately
150 m, and the central electrospun layer was about 100 um,
and the top and bottom electrospun layers were approximately
300 m thick. The design that central layer of PCL/F-127 was
thinner than the outer electrospun layers was to facilitate more
communication of the cells in the two gel layers and subsequent
integration of the cells upon the degradation of the electrospun
layers. The top and bottom electrospun layers were designed
to provide the mechanical property of the hybrid construct. It
was observed that the thickness of the constructs was reduced
to approximately 0.4 mm as the fibrin degraded and left the
collagen matrix behind. Each construct was square with a
10 cm diagonal. Cartilage constructs were then incubated in
DMEM medium supplemented with 10% FBS, 1% ABAM
and 1% L-glutamine in 5% CO2 at 37 C.
Constructs without cells were fabricated using the same
method of alternating PCL/F-127 and the fibrinogen/collagen
mixture. PCL/F-127 control constructs were fabricated
using the same electrospinning method without the
fibrinogen/collagen mixture. For the purpose of comparing
the printed-electrospun constructs with commonly used
hydrogels, alginate and fibrin/collagen hydrogels were used
as controls. Alginate controls were prepared by mixing 2%
wt/vol sodium alginate (MVG; Pronova Biomedical, Oslo,
Norway) with an overall gluronic acid (G-block) content
of 70% (as recommended by the manufacturer) with PBS.
Solution was gelled by mixing with 0.25 M CaCl2 and
pulled through an even diameter tube before gelling was
complete to ensure a uniform thickness through the construct.
Collagen/fibrin hydrogels were fabricated by plating the
mixture of collagen and fibrin without cells in a petri dish
marked to 0.4 mm to ensure an even thickness and measuring
the resulting gel with digital calipers.
Constructs were then rinsed with PBS and viewed using a
fluorescent microscope at 200 magnification. Cell viability
was assessed by randomly examining five representative fields
per sample with a minimum of 50 cells per field, counting
the number of live cells stained with calcein AM (green) and
comparing this number to the total number of cells.
2.7. Microstructure of cartilage constructs
The microstructure of the cartilage constructs was evaluated
using scanning electron microscopy (SEM). Samples were
lyophilized and sputter coated with gold. Cross-sectional
electron-micrographs were obtained at 200, 500, and
4000 magnification at 20.0 kV and 50 Pa using a
Hitachi S-2600 scanning electron microscope (Hitachi High
Technologies America, Pleasanton, CA).
2.8. Mechanical properties of printed hybrid constructs and
other hydrogel constructs
Mechanical properties of hybrid constructs without cells,
pure PCL/F-127, alginate, and collagen/fibrin gel were
evaluated in fully hydrated conditions using an Instron uniaxial
load frame (Instron Corporation, Issaquah, WA). Rectangular
samples (n = 3) of 6 mm long and 4 mm wide were
prepared from each construct. The thickness of each sample
was measured separately using digital caliper and reported
as average standard deviation (SD). Hybrid samples
had a thickness of 0.38 0.055 mm, alginate samples
0.36 0.05 mm, PCL samples 0.29 0.05 mm and
collagen/fibrin samples 0.4 mm. The samples were allowed to
stretch at 0.2 mm s1 crosshead speed until failure. Ultimate
tensile strength (UTS) was calculated at the maximum load
immediately before breaking. Youngs modulus was calculated
from the slope of the linear segment of the stressstrain curve.
Values were presented as average SD.
2.9. In vitro evaluation of hybrid cartilage constructs
Hybrid printed cartilage constructs were cultured in vitro to
evaluate the cellular organization and proliferation within
each construct. In addition, extracellular matrix deposition and
organization were observed over time. Hybrid constructs were
fabricated as described and cultured in DMEM supplemented
with 10% FBS, 1% ABAM and 1% L-glutamine in 5% CO2 at
37 C for four weeks. Printed hybrid constructed without cells
were used as controls.
2.10. In vivo evaluation of hybrid cartilage constructs
2.6. Evaluation of cell viability
All animal procedures were approved by the Wake Forest
University Health Sciences Animal Care and Use Committee.
For the in vivo assessment, printed hybrid constructs were
prepared, cultured in vitro for two weeks and implanted
subcutaneously in immunodeficient mice (nu/nu) (Charles
River Laboratories). An unseeded control hybrid scaffold
also was implanted in each mouse. The constructs were
implanted in the mice for two, four, and eight weeks. Six
animals were used to evaluate the performance of the hybrid
The viability of chondrocytes within the fabricated cartilage
constructs was evaluated at one week after printing by a twocolor fluorescence live/dead assay (Molecular Probes, OR)
following the manufacturers protocol. Briefly, triplicates of
printed cartilage constructs were rinsed with PBS to remove
residual serum and incubated for 30 min in 5% CO2 at
37 C with 2 ml of 2 M calcein AM and 4 M ethidium
homodimer (EthD-1) dissolved in 10 ml PBS solution.
4
Biofabrication 5 (2013) 015001
T Xu et al
cartilage constructs with two at each time point. Each mouse
was anesthetized with isoflurane and two small incisions
were created on the dorsa. Hybrid cartilage constructs were
subcutaneously inserted in the first incision. The control hybrid
constructs without cells were similarly inserted in the second
incision. After two, four, and eight weeks of implantation, the
incisions were closed and mice were examined. At the end of
study, constructs with 6 of the 12 experimental groups were
explanted from the mice and prepared for histological analysis.
polymers to be easily controlled to produce highly organized
porous structures that encourage cellular infiltration and
integration into the surrounding tissue [2426]. Furthermore,
manipulation of the electrospinning technique can produce
highly aligned fibers [27] that can be used to direct the growth
of muscle [28], nerves [29], and cartilage [30]. Like inkjet
printing, electrospinning is a low cost fabrication technique
with immense potential for tissue engineering. By combining
electrospinning with inkjet printing, we were able to obtain a
tissue construct consisting of layers of electrospun PCL and
printed hydrogels containing cells. This layered structure could
have been achieved by alternating electrospinning and inkjet
printing in separate machines. However, the combined hybrid
system allows production of extremely thin patterns in the
electrospun and cellular layers that would not survive repeated
movements between machines. In addition, the hybrid system
maintains the sterility of the printing field by eliminating
transfers between machines. Together, the electrospinning and
printing apparatuses create a system with greater capabilities
than either apparatus alone.
The printed hybrid constructs produced using our system
had adequate mechanical integrity to maintain the structure
of the five printed layers as shown in figures 2(A) and
(B). Microstructural analysis of the printed hybrid constructs
using SEM demonstrated the presence of intact layers of
cell/collagen matrix between the sheets of PCL as shown in
figure 2(C). Measurements of the electrospun fibers showed
an average fiber diameter of 422 62 nm and a pore size
smaller than 5 m. The microstructure of the PCL at high
magnification appeared fibrous, and occasional beads were
present (figure 2(D)). Formation of beads occurs when the
extruded polymer fails to form fibers and instead clusters on
the collection screen. This phenomenon is directly related to
the viscosity and surface tension of the polymer solution and is
inversely related to the charge density of the solution. However,
this can be avoided by increasing the concentration of polymer
in the solution and slowing the flow rate of the solution through
the needle tip. Beading can be controlled to generate structures
with porous membranes and cups [31]. Thus, this technique
may be used to finely tune the scaffold architecture for different
tissue types.
To visualize the attachment of chondrocytes to the
collagen matrix, the top layer of PCL was removed from
the construct and the cells were visualized under SEM.
Chondrocytes appeared to be firmly attached and spread out on
the matrix as shown in figure 2(E). SEM demonstrated that the
layered structure of the construct could be maintained in vitro.
However, we experienced layer separation in two constructs
immediately after printing because the electrospun and printed
layers were not well anchored to each other.
Our approach is very similar to recent work performed
by Yang et al [32], in which skin constructs were produced
by manually seeding fibroblasts and keratinocytes on wet
electrospun layers. Other similar studies have been performed
using electrosprayed cells and fibers, which allow a better
infiltration of cells into the scaffold [33, 34]. In our technique,
direct encapsulation of cells between fiber mats ensures that
cells are evenly distributed through the gel layers within the
2.11. Histological evaluation
Samples from printed hybrid constructs with cells and without
cells from in vitro and in vivo experiments were processed
for histological analyses. Samples were fixed overnight with
10% formalin. Fixed samples were then embedded in paraffin
and cut into 35 m thick sections. Massons Trichrome
(MT) staining for collagen and Safranin O (Saf O) staining
for glycosaminoglycans were performed to evaluate the
deposition and organization of extracellular matrix in the
printed hybrid constructs.
To distinguish collagen that had been deposited by
chondrocytes in the hybrid constructs from the collagen used
to print the constructs, sections were immunostained with antitype II collagen antibodies (Dako, Denmark). Immunostaining
was performed using a DakoAutostainer Universal Staining
System (Dako, Denmark). Slides were rinsed with Dako Wash
Buffer and incubated in 100 l of 3% hydrogen peroxide for
30 min. After rinsing twice in buffer, sections were incubated
with 100 l of 10% Dako ready-to-use protein block serumfree for 30 min and samples were left to air dry. Sections were
then incubated with 100 l of mouse anti-type II collagen
antibody at 1:200 dilution for 90 min, and this was followed
by two washes in buffer. Sections were incubated again
with blocking solution for 30 min and then incubated with
100 l of biotin-labeled rabbit anti-mouse antibody at a 1:200
dilution for 30 min. Sections were rinsed twice with buffer and
biotin was detected using streptavidin-conjugated horseradish
peroxidase (Vector Laboratories, Burlingame, CA).
2.12. Statistical analysis
Statistical analysis was performed using the Student t-test.
Values were represented as average SD where applicable
and p <0.05 was considered to be significant.
3. Results and discussion
3.1. Morphology and microstructure of hybrid
electrospun/inkjet printed constructs
We have developed a novel hybrid fabrication system that
combines both electrospinning and inkjet bioprinting to
achieve simultaneous high throughput cell patterning and
controlled scaffold production, thus overcoming one of the
major limitations of inkjet printing alone. Electrospinning
of PCL was incorporated in this hybrid printing system
because PCL scaffolds have excellent mechanical properties
and because electrospinning allows the composition of the
5
Biofabrication 5 (2013) 015001
T Xu et al
(B)
(A)
(C)
(D)
(E )
Figure 2. (A) Macroscopic view of the printed construct in culture media, scale bar 2 cm. (B) Schematic representation of the five-layer
printed constructs of PCL and chondrocytes. (C) Cross-sectional SEM at 200 magnification shows the layered structure of the scaffold.
PCL can be seen at the left and right with cells and collagen in the middle, scale bar 100 m. (D) 4000 magnification showing the
microstructure of the PCL, scale bar 10 m. (E) 500 magnification shows the chondrocytes attaching to the collagen matrix, scale bar
10 m.
scaffold, but the cell growth, tissue formation, mechanical
properties and functional expression are difficult to control due
to the limitations of this technology. These constructs could
be adequate for use in engineering some tissues, but the cell
placement is not specific enough to build tissues and organs
with complex structural and functional requirements. The
major advantage of our technique over previous work is that we
are using inkjet printing to precisely control deposition of cells
in complex patterns within the layers. This is an ability that no
other system has been able to demonstrate and illustrates the
power of this novel system. The architecture of electrospun
scaffolds could already be controlled by manipulating the
polymer flow rate, needle size, voltage, and electric field
to organize layered tissue constructs in the Z direction. The
current prototype we used for this study needed lengthy time
to fabricate the constructs. This is mostly due to the time
required to electrospin the PCL scaffolds. Further development
is necessary to build a high-throughput system that could
fabricate constructs in a reasonably acceptable time.
The live/dead assay indicated that after one week in culture,
81.58 3.46% of the chondrocytes in the printed hybrid
constructs were viable. This suggests that the combined
electrospinning/printing process did not affect the viability of
the cells, which showed similar viabilities at similar time points
in previous experiments [15]. The electrospinning process did
not significantly affect the printed cells, likely because the
collection plate acted as the ground and prevented the cells
from being directly exposed to the voltage. Furthermore, other
studies have shown that cells can be directly deposited at high
voltage with no apparent detrimental effects [30, 31].
3.3. Mechanical testing
To evaluate the structural and mechanical properties of the
constructs, we examined the Youngs modulus and UTS
of each construct and compared these to the values for
constructs fabricated with PCL alone by electrospinning and
for constructs produced with alginate, the scaffolding material
typically used in bioprinting. Mechanical testing demonstrated
that the printed hybrid constructs were stiffer and were able to
withstand greater tensile stress than alginate, collagen/fibrin or
electrospun PCL/F-127-only constructs (table 1). The Youngs
modulus of the printed hybrid constructs (1.76 MPa) was four
3.2. Cell viability
Printed hybrid constructs with chondrocytes were analyzed
using the Molecular ProbesTM viability/cytotoxicity assay.
6
Biofabrication 5 (2013) 015001
T Xu et al
(hyaluronan, chondroitin sulfate, and keratin sulfate), and
elastin. Of these, type II collagen and the glycosaminoglycans
were expected to be most visible in the fabricated constructs.
Analysis of sections after two weeks in vitro showed the
initiation of cartilage tissue formation, but there was very little
cartilage tissue visible. We hypothesize that the lack of ECM
deposition at two weeks in vitro was due to lack of nutrient
diffusion within the constructs. However, histological analysis
confirmed that the chondrocytes were producing the matrix
components of cartilage tissue after four weeks of in vitro
culture (figure 3). When printed hybrid constructs containing
cells were compared to printed hybrid constructs without
cells at four weeks, H&E staining showed that a significant
population of homogenously organized chondrocytes existed
within the matrix of the printed hybrid constructs with cells
(figure 3(B)) compared to the negative control constructs
(figure 3(A)). MT staining demonstrated the clear presence
of well-dispersed collagen bands accumulated around the
cells (figure 3(D)). Immunohistochemical analysis revealed
formation of type II collagen in the printed hybrid constructs.
This was not present in the print mixture and is a major
component of cartilage (figures 3(G) and (H)). Saf O staining
demonstrated the presence of GAGs only in the printed hybrid
constructs with cells (figures 3(F) and (E)). Interestingly,
glycosaminoglycans and type II collagen, the two important
components of cartilage, seemed to be concentrated at the
edges of the constructs at four weeks in vitro, suggesting that
the cells in the center of the construct were less functionally
active, possibly due to limited diffusion of nutrients and
growth factors from the media to the center of the construct
[32, 38]. The parameters of the electrospinning in this
experiment generated nanofibers with very low porosity,
which may have prevented nutrients in the media from
diffusing through these pores. Altering the parameters of the
electrospinning would change the porosity of the layers, but a
very dense lower layer of PCL should be maintained to prevent
the cells from falling through the construct. Alternatively, a
mixture of nano- and microfibers may be useful to enhance
the diffusion of nutrients and growth factors at the core of the
constructs.
In vivo evaluation of explanted tissues after 8 weeks
showed dense and well organized collagen formation in the
printed hybrid constructs compared to very minimal formation
of collagen in the controls (figures 4(A) and (B)). The structure
of the GAGs appears to resemble typical elastic cartilage with
areas of dense GAGs interspersed with areas of little deposition
(figure 4(D)). Most importantly, constructs recovered from
mice showed rounded chondrocytes with lacunae that are
typical of normal elastic cartilage. Type II collagen was
also visible in the printed constructs (figure 4(F)). Control
constructs showed no presence of collagen type II or GAGs
after eight weeks of implantation (figures 4(C) and (E)).
Constructs retrieved after eight weeks in vivo had large
amounts of collagen and GAGs deposited throughout the entire
construct and appeared histologically similar to normal elastic
cartilage. This demonstrates that the cells were able to maintain
their normal phenotype and produce ECM in vivo despite the
in vitro limitations.
Table 1. Youngs modulus and UTS of pure alginate gel,
electrospun pure PCL, hybrid PCL/collagen/fibrin scaffolds, and
collagen/fibrin matrix. Data were presented as average SD
(n = 3).
Youngs modulus (MPa)
Alginate
PCL
Scaffold
Matrix
0.41 0.06a
0.77 0.22
1.76 0.71a
b
UTS (MPa)
0.26 0.11a
0.92 0.20
1.11 0.12a
b
p < 0.05 versus hybrid scaffold by
two-sample t-test.
b
Mechanical strength of collagen/fibrin
matrix was too low to be distinguished
from random noise.
a
times higher than that of alginate constructs (0.41 MPa) (n
= 4, p = 0.008)). Similarly, the UTS of the printed hybrid
constructs (1.11 MPa) was five times higher than the UTS
of the alginate constructs (0.26 MPa) (n = 4, p = 0.003).
Neither the strength nor the stiffness of the printed hybrid
constructs was significantly different from those measured
for pure PCL/F-127 electrospun fibers (n = 4, p = 0.067).
This observation was expected, as the collagen/fibrin gel
has very low mechanical strength and generally does not
contribute to the combined mechanical properties of the
construct. When tested, collagen/fibrin constructs indeed
displayed such low tensile strength that the stress-strain
profile was indistinguishable from the noise signal generated
by the testing machine. These mechanical testing results
confirmed our hypothesis that the hybrid constructs would
demonstrate increased structural stability over the alginate
or fibrin/collagen hydrogels. Both Youngs modulus and the
UTS of the constructs were significantly greater than alginate
because the constructs took on the structural properties of
the PCL. While the observed beading in the PCL reduced
the tensile strength of woven electrospun fibers by forming
stress defects [35], the hybrid structures still showed better
mechanical properties over the alginate controls. Boland
et al evaluated the Youngs modulus and UTS of printed
alginate constructs to be 89 47 KPa and 56 12 KPa,
respectively and were comparable to our alginate mechanical
values [36]. The mechanical properties of the hybrid cartilage
constructs were lower than those reported for native human
cartilage (Youngs modulus 4.1 MPa) [37]. These properties
are expected to improve during the tissue regeneration process
as cells deposit and align their own ECM. Moreover, the initial
mechanical properties of the printed hybrid constructs can be
easily improved by changing the diameter, porosity and/or
orientation of electrospun PCL fibers.
3.4. Histological analysis
Having demonstrated that cells were able to survive the
printing process and that the printed hybrid constructs were
indeed stronger than standard alginate scaffolds, we examined
ECM production by the printed chondrocytes in order to
determine if the cells retained some or all of their functional
characteristics. The main components of elastic cartilage are
collagen (types II, VI, IX, X, and XI), glycosaminoglycans
7
Biofabrication 5 (2013) 015001
T Xu et al
(A)
(C )
(E)
(G )
(B)
(D)
(F )
(H )
Figure 3. Histological analysis of in vitro printed constructs with cells (printed) and without cells (control) at four weeks. Printed samples
are five layer constructs alternating PCL and cells in a collagen/fibrin gel. Control samples are five layer constructs alternating PCL and
collagen/fibrin gel. (A) Control sample stained with H&E shows no presence of cells. (B) H&E staining of the printed constructs after four
weeks in culture. Dark blue staining indicates cell nuclei. (C) Control sample stained with MT shows no blue collagen. (D) MT staining of
the printed constructs after four weeks in culture. Dark staining shows cell nuclei. Blue staining demonstrates presence of collagen. (E)
Control sample stained with Saf O shows only green counterstain and no red GAGs. (F) Saf O staining of the printed constructs after four
weeks in culture. Dark staining indicates cell nuclei and red shows production of GAGs. (G) Control sample labeled with anti-type II
collagen antibody demonstrating only counterstain. (H) Anti-type II collagen antibody labeling a section after four weeks in culture. Brown
staining indicates production of type II collagen. Magnification: 200 . Scale bars: 100 m.
(A)
(C )
(E )
(B)
(D)
(F )
Figure 4. Histological analysis of in vivo printed constructs with cells (printed) and without cells (controls) at eight weeks after implantation.
Printed samples are five layer constructs alternating PCL and cells in a collagen/fibrin gel. Control samples are five layer constructs
alternating PCL and collagen/fibrin gel. All samples were cultured for two weeks prior to implantation. (A) Control sample stained with MT
shows no blue collagen. (B) MT staining of constructs implanted in vivo for eight weeks demonstrating large bands of collagen. (C) Control
sample stained with Saf O shows no red GAGs. (D) Saf O staining of in vivo constructs shows significant GAG production. (E) Control
sample labeled with anti-type II collagen antibody demonstrating only counterstain. (F) Anti-type II collagen antibody labeling a section
after eight weeks in vivo. Brown staining indicates production of type II collagen. Magnification: 200. Scale bars: 100 m.
Careful selection of scaffold material for each patients
construct would allow the implant to withstand mechanical
forces while encouraging new cartilage to organize and fill
the defect. This technique can also be extended to other tissue
types. Although electrospun scaffolds can direct chondrocytes
3.5. Future direction
Cartilage constructs similar to those created in this experiment
could be applied clinically by using MRI images of a defect in
the knee as a blueprint to bioprint a matching construct.
8
Biofabrication 5 (2013) 015001
T Xu et al
growth [30], they can also direct the formation of myotubes to
enhance strategies for muscle tissue engineering [28]. The use
of hybrid system allows creation of highly aligned electrospun
fibers and targeted application of myotubes. This technique can
then be used to layer patterns of endothelial cells and nerve
cells on the aligned myotubes to create functional muscle.
By overcoming one of the major obstacles associated with
conventional bioprinting, we have expanded the utility of
biofabrication technology.
[9]
[10]
[11]
[12]
Conclusions
This study demonstrates the feasibility of generating layered
cartilage constructs using a combination of electrospinning
and inkjet printing. The hybrid scaffold demonstrated
enhanced mechanical properties compared to conventional
hydrogel constructs generated using inkjet printing alone.
Printed cells maintained their viability and produced cartilagespecific ECM both in vitro and in vivo. Further refinement of
the technique could produce functional cartilage constructs by
using oriented fibers to direct chondrocyte growth. Combining
this tight control of scaffold properties with the precise cell
delivery of the printing process, as well as with advances
in hydrogel technology, will enable production of highly
functional tissue constructs. This work indicates that the hybrid
electrospinning/inkjet printing technique is a promising new
technology that could simplify production of complex tissues.
[13]
[14]
[15]
[16]
[17]
[18]
Acknowledgments
[19]
The authors would like to thank Cathy Mathis for assistance
with histology and Dr Jennifer Olson for editorial assistance
with this manuscript.
[20]
[21]
References
[1] Slaughter B V, Khurshid S S, Fisher O Z, Khademhosseini A
and Peppas N A 2009 Hydrogels in regenerative medicine
Adv. Mater. 21 330729
[2] Mather M L and Tomlins P E 2010 Hydrogels in regenerative
medicine: towards understanding structure-function
relationships Regen. Med. 5 80921
[3] Chung B G, Lee K H, Khademhosseini A and Lee S H 2012
Microfluidic fabrication of microengineered hydrogels and
their application in tissue engineering Lab Chip 12 4559
[4] Huang G Y et al 2011 Microfluidic hydrogels for tissue
engineering Biofabrication 3 012001
[5] Reichert J C, Heymer A, Berner A, Eulert J and Noth U 2009
Fabrication of polycaprolactone collagen hydrogel
constructs seeded with mesenchymal stem cells for bone
regeneration Biomed. Mater. 4 065001
[6] Schuurman W, Khristov V, Pot M W, van Weeren P R,
Dhert W J and Malda J 2011 Bioprinting of hybrid tissue
constructs with tailorable mechanical properties
Biofabrication 3 021001
[7] Hutmacher D W, Sittinger M and Risbud MV 2004
Scaffold-based tissue engineering: rationale for
computer-aided design and solid free-form fabrication
systems Trends Biotechnol. 22 35462
[8] Shim J H, Kim J Y, Park M, Park J and Cho D W 2011
Development of a hybrid scaffold with synthetic
[22]
[23]
[24]
[25]
[26]
[27]
biomaterials and hydrogel using solid freeform fabrication
technology Biofabrication 3 034102
Shim J H, Lee J S, Kim J Y and Cho DW 2012 Bioprinting of
a mechanically enhanced three-dimensional dual cell-laden
construct for osteochondral tissue engineering using a
multi-head tissue/organ building system J. Micromech.
Microeng. 22 085014
Wilson W C Jr and Boland T 2003 Cell and organ printing 1:
protein and cell printers Anat. Rec. 272A 4916
Roth E A, Xu T, Das M, Gregory C, Hickman J J
and Boland T 2004 Inkjet printing for high-throughput cell
patterning Biomaterials 25 370715
Okamoto T, Suzuki T and Yamamoto N 2000 Microarray
fabrication with covalent attachment of DNA using bubble
jet technology Nature Biotechnol. 18 43841
Roda A, Guardigli M, Russo C, Pasini P and Baraldini M 2000
Protein microdeposition using a conventional ink-jet printer
Biotechniques 28 (3) 4926
Xu T et al 2004 Construction of high-density bacterial colony
arrays and patterns by the ink-jet method Biotechnol.
Bioeng. 85 2933
Xu T, Jin J, Gregory C, Hickman J J and Boland T 2005 Inkjet
printing of viable mammalian cells Biomaterials 26 939
Xu T, Gregory C A, Molnar P, Cui X, Jalota S, Bhaduri S B
and Boland T 2006 Viability and electrophysiology of
neural cell structures generated by the inkjet printing
method Biomaterials 27 35808
Xu T, Rohozinski J, Zhao W, Moorefield E C, Atala A
and Yoo J J 2009 Inkjet-mediated gene transfection into
living cells combined with targeted delivery Tissue Eng. A
15 95101
Boland T, Mironov V, Gutowska A, Roth E A
and Markwald R R 2003 Cell and organ printing 2: fusion
of cell aggregates in three-dimensional gels Anat. Rec.
272A 497502
Tanaka Y, Gong J P and Osada Y 2005 Novel hydrogels with
excellent mechanical performance Prog. Polym. Sci. 30 19
Bonn D, Kellay H, Prochnow M, Ben-Djemiaa K
and Meunier J 1998 Delayed fracture of an inhomogeneous
soft solid Science 280 2657
Klein T J, Rizzi S C, Reichert J C, Georgi N, Malda J,
Schuurman W, Crawford R W and Hutmacher D W 2009
Strategies for zonal cartilage repair using hydrogels
Macromol. Biosci 9 104958
Lee S J and Yoo J J 2012 Guidance of cell adhesion,
alignment, infiltration, and differentiation on electrospun
nanofibrous scaffolds Handbook of Intelligent Scaffold for
Tissue Engineering and Regenerative Medicine ed G Khang
(Singapore: Pan Stanford Publishing) pp 20112
Sanz E, Penas L and Lequerica J L 2007 Formation of
cartilage in vivo with immobilized autologous rabbit
auricular cultured chondrocytes in collagen matrices Plast.
Reconstr. Surg. 119 170713
Ekaputra A K, Prestwich G D, Cool S M and Hutmacher D W
2008 Combining electrospun scaffolds with electrosprayed
hydrogels leads to three-dimensional cellularization of
hybrid constructs Biomacromolecules 9 2097103
Lee Y H et al 2005 Electrospun dual-porosity structure and
biodegradation morphology of Montmorillonite reinforced
PLLA nanocomposite scaffolds Biomaterials 26 316572
Kim T G, Chung H J and Park T G 2008 Macroporous and
nanofibrous hyaluronic acid/collagen hybrid scaffold
fabricated by concurrent electrospinning and
deposition/leaching of salt particles Acta Biomater.
4 16119
Li D, Ouyang G, McCann J T and Xia Y 2005 Collecting
electrospun nanofibers with patterned electrodes Nano Lett.
5 9136
Biofabrication 5 (2013) 015001
T Xu et al
[28] Choi J S, Lee S J, Christ G J, Atala A and Yoo J J 2008 The
influence of electrospun aligned poly(epsiloncaprolactone)/collagen nanofiber meshes on the formation
of self-aligned skeletal muscle myotubes Biomaterials
29 2899906
[29] Wang H B et al 2009 Creation of highly aligned electrospun
poly-L-lactic acid fibers for nerve regeneration applications
J. Neural Eng. 6 016001
[30] Wise J K, Yarin A L, Megaridis C M and Cho M 2009
Chondrogenic differentiation of human mesenchymal stem
cells on oriented nanofibrous scaffolds: engineering the
superficial zone of articular cartilage Tissue Eng. A
15 91321
[31] Eda G and Shivkumar S 2006 Bead structure variations
during electrospinning of polystyrene J. Mater. Sci.
41 57048
[32] Yang X, Shah J D and Wang H 2009 Nanofiber enabled
layer-by-layer approach toward three-dimensional tissue
formation Tissue Eng. A 15 94556
[33] Stella J A, Liao J, Hong Y, David Merryman W, Wagner W R
and Sacks M S 2008 Tissue-to-cellular level deformation
[34]
[35]
[36]
[37]
[38]
10
coupling in cell micro-integrated elastomeric scaffolds
Biomaterials 29 322836
Townsend-Nicholson A and Jayasinghe S N 2006 Cell
electrospinning: a unique biotechnique for encapsulating
living organisms for generating active biological
microthreads/scaffolds Biomacromolecules 7 33649
Cha D I, Kim H Y, Lee K H, Jung Y C, Cho J W
and Chun B C 2005 Electrospun nonwovens of
shape-memory polyurethane block copolymers J. Appl.
Polym. Sci. 96 4605
Boland T, Xu T, Damon B and Cui X 2006 Application of
inkjet printing to tissue engineering Biotechnol. J. 1 9107
Woodfield T B, Malda J, de Wijn J, Peters F, Riesle J and van
Blitterswijk C A 2004 Design of porous scaffolds for
cartilage tissue engineering using a three-dimensional
fiber-deposition technique Biomaterials 25 414961
Wang H J, Bertrand-De Haas M, Riesle J, Lamme E and Van
Blitterswijk C A 2003 Tissue engineering of dermal
substitutes based on porous PEGT/PBT copolymer
scaffolds: comparison of culture conditions J. Mater. Sci.
Mater. Med. 14 23540
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Maths Question of The DayDokumen162 halamanMaths Question of The DayGaurav YadavBelum ada peringkat
- The Neurohistological TechniquesDokumen4 halamanThe Neurohistological Techniquesapi-3846255100% (2)
- DST 60 IFT MeasurementDokumen12 halamanDST 60 IFT Measurement김동완Belum ada peringkat
- C12HDokumen129 halamanC12Hkhudhayer1970Belum ada peringkat
- Task 3 - New Research Proposal, C Vides o ZamudioDokumen3 halamanTask 3 - New Research Proposal, C Vides o ZamudioOctavio LópezBelum ada peringkat
- Pages From SAES-H-001-19Dokumen1 halamanPages From SAES-H-001-19mohammed s fawabBelum ada peringkat
- Bm101: Biology For Engineers: Instructor: Yashveer Singh, PHDDokumen15 halamanBm101: Biology For Engineers: Instructor: Yashveer Singh, PHDhimanshu singhBelum ada peringkat
- Chemistry Final Cheat SheetDokumen1 halamanChemistry Final Cheat SheetScott Allred100% (2)
- Pamphlet TG-X SeriesDokumen2 halamanPamphlet TG-X SeriesrajeshBelum ada peringkat
- Dna Repair MechanismsDokumen49 halamanDna Repair MechanismsayeshaBelum ada peringkat
- Marine Science Semester 1 ReviewDokumen18 halamanMarine Science Semester 1 ReviewJoe Xavier ReidyBelum ada peringkat
- Din 50942-96Dokumen13 halamanDin 50942-96RONALD100% (2)
- Redox ExerciseDokumen4 halamanRedox ExerciseHau Hei, Matthew LinBelum ada peringkat
- In-Line Pulsation Dampeners For Bredel 25-100, APEX 28 and APEX 35 PumpsDokumen2 halamanIn-Line Pulsation Dampeners For Bredel 25-100, APEX 28 and APEX 35 PumpsVruno Velasquez LBelum ada peringkat
- CBSE Class 11 and 12 Chemistry Notes The P-Block ElementsDokumen45 halamanCBSE Class 11 and 12 Chemistry Notes The P-Block ElementsPrabhuPalanichamy50% (2)
- Ultimate Cheatcode CematconDokumen82 halamanUltimate Cheatcode CematconJulian Deleon100% (1)
- Copper Filling of Blind Micro Vias and Through Holes Using Reverse Pulse PlatingDokumen4 halamanCopper Filling of Blind Micro Vias and Through Holes Using Reverse Pulse PlatingteehoweBelum ada peringkat
- Sika®-1: Product Data SheetDokumen2 halamanSika®-1: Product Data SheetKhin Sandi KoBelum ada peringkat
- An Overview of Traditional Fish Smoking in Africa PDFDokumen20 halamanAn Overview of Traditional Fish Smoking in Africa PDFBzmania SlimnzieBelum ada peringkat
- Duplex and Superduplex Stainless Steel Fittings (Amendments/Supplements To Astm A 815)Dokumen11 halamanDuplex and Superduplex Stainless Steel Fittings (Amendments/Supplements To Astm A 815)Mathew CherianBelum ada peringkat
- Suitable dimensions, performance requirements, and processes for optical transmittersDokumen1 halamanSuitable dimensions, performance requirements, and processes for optical transmittersshruti soniBelum ada peringkat
- Assignment 5: Unit 7 - Week 5Dokumen1 halamanAssignment 5: Unit 7 - Week 5atulBelum ada peringkat
- Efficient H2S Scavenger Glyoxal Outperforms TriazineDokumen8 halamanEfficient H2S Scavenger Glyoxal Outperforms TriazineMo OsBelum ada peringkat
- Udel PSU Design Guide - EN v5.0 - 0 - 0 PDFDokumen84 halamanUdel PSU Design Guide - EN v5.0 - 0 - 0 PDFReza Pencinta AL HadadBelum ada peringkat
- Carbonate Acidizing Design PDFDokumen15 halamanCarbonate Acidizing Design PDFNelson PuentsBelum ada peringkat
- GraniteDokumen4 halamanGranitequsaiBelum ada peringkat
- OzonolysisDokumen1 halamanOzonolysisThu NguyenBelum ada peringkat
- Metabolisme ImmunometabolismDokumen25 halamanMetabolisme ImmunometabolismOKE channelBelum ada peringkat
- Reinforcing Low-Grade Glulam Beams with GFRP RodsDokumen12 halamanReinforcing Low-Grade Glulam Beams with GFRP RodsCălin MartonBelum ada peringkat
- Important Aspect of Viscosity in Gravure Printing ProcessDokumen18 halamanImportant Aspect of Viscosity in Gravure Printing ProcessMakarand Dole100% (1)