Ijpr 12 175
Diunggah oleh
Gaby ValenzuelaJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Ijpr 12 175
Diunggah oleh
Gaby ValenzuelaHak Cipta:
Format Tersedia
Iranian Journal of Pharmaceutical Research (2013), 12 (supplement): 175-182
Received: December 2012
Accepted: February 2013
Copyright 2013 by School of Pharmacy
Shaheed Beheshti University of Medical Sciences and Health Services
Original Article
Potential of Drug Interactions among Hospitalized Cancer Patients in a
Developing Country
Maria Tavakoli-Ardakania,b*, Kaveh Kazemianc,e, Jamshid salamzadehc and Mahshid Mehdizadehd
Department of Clinical Pharmacy, School of Pharmacy, Shahid Beheshti University of
Medical Sciences, Tehran, Iran. bPharmaceutical Sciences Research Center, Shahid Beheshti
University Of Medical Sciences, Tehran, Iran. cDepartment of Clinical Pharmacy, School of
Pharmacy, Mazandaran University of Medical Sciences, Sari, Iran. dBone Marrow Transplantion
Center, Taleghani Hospital,Shahid Beheshti University Of Medical Sciences, Tehran, Iran.
e
Students Research Committee, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
a
Abstract
Cancer patients are more susceptible to adverse drug-drug interactions (DDIs) due to
receiving multiple medications especially chemotherapy medications, hormonal agents and
supportive care drugs. The aim of this study is to describe the prevalence of potential DDIs
and to identify risk factors for these potential interactions in hospitalized cancer patients in a
developing country.
A cross-sectional study conducted by reviewing charts of 224 consecutive in hospitalized
patients in hematology-oncology ward of a teaching hospital in Tehran, during a 12 month
period from July 2009 to July 2010. Drug Interaction Facts 2008, 2009: The Authority on Drug
Interactions was used for screening the potential drug-drug interactions. Potential interactions
were classified by levels of severity and documentation.
The median age of patients was 50 years, the length of hospital stay for patient was 5 days
and the number of drugs per patient was 8 drugs. Two hundred and twenty-eight potential
interactions were detected. Nearly 14% of the interactions were major and 60% were moderate.
Approximately 9% and 10% potential interactions were graded as established and probable.
In multivariate analysis, being older than 61 years old, suffering from hematologic cancer,
source of cancer in different specific organs (esophagus, testis and cervices more than other
sources), and number of ordered drugs for patients were independent predictors of having at
least one potential DDI in hospital order. Suffering from hematologic cancer, source of cancer
in different organs, length of hospital stay and number of ordered drugs for patients were
independent predictors for number of interactions per patients.
Having a DDI seems to be more likely to occur in patients older than 61 years old.
Hematologic cancers, having more medications in physicians order, longer length of hospital
stay, esophageal cancer, testicular cancer and cervical cancer have related to having a DDI and
also having more number of interactions.
Keywords: interactions; Hospitalized cancer patients; Potential.
* Corresponding author:
E-mail: mariatavakoli@yahoo.com
Tavakoli-Ardakani M et al. / IJPR (2013), 12 (supplement): 175-182
Introduction
which a physical or chemical incompatibility
in intravenous injections exists between two
different drugs.
In these years, several studies have
investigated the potential for drug interactions
in cancer patients in developed countries (7-14).
In a Canadian study (2007) between 4 previous
medications of out-patient receiving systemic
cancer therapy for solid tumor, potential drug
interaction associated with increasing number
of medication of patients, type of medications
(medications require for co-morbid conditions)
and presence of brain tumor (10). But the
potential of this action in cancer patients of
developing countries is largely unknown. In
a Brazilian study (2005) potential for drug
interactions unrelated to chemotherapy in
hospitalized cancer patients found to be 63% in
the day half-way through the hospital stay but this
study didnt investigated all patients medication
(15). Propose of this study is to describe the
prevalence of potential DDIs regardless of
whether they actually occurred clinically. Also
we want to correlate the frequency of DDIs
with demographic information of patient and
recognize risk factors for these potential DDIs
in a hematology-oncology ward of hospitalized
patients in a developing country, Iran.
Drug-Drug Interactions (DDIs) cover nearly
20-30% of adverse drug reactions. In elderly
patients, it is increased to 80% and some of these
interactions may become irreversible adverse
reactions and basic health damage. (1) Receiving
multiple medications, cancer patients are more
susceptible to adverse drug-drug interactions.
Beside their cancer pharmacotherapy include
cytotoxic chemotherapy medications, hormonal
agents and supportive care drugs, these patients
are often elderly and use medications require for
co-morbid conditions such as rheumatologic,
gastrointestinal and cardiovascular disease (2).
Cancer patients are particularly more susceptible
to pharmacokinetic parameters alteration since
they often suffer from mucositis, malnutrition,
generalized edema and reduction of serumbinding proteins, hepatic and renal function
which always heightened in elderly patients. This
alteration in absorption, distribution, metabolism
and exertion can also increase the risk of DDIs
and promote them to an important cause of
morbidity and mortality in cancer patients. It is
showed that 4% of mortality in oncology ward is
due to the drug interactions (1).
Pharmacokinetic, pharmacodynamic and
pharmaceutical are three types of drug interactions
(2). Mechanisms of the pharmacokinetic
interactions were related to metabolism and/or
exertion, absorption, elimination and distribution
(3). When Allopurinol and Mercaptopurine are
administered together, a Pharmacokinetic DDI
happens since Allopurinol alters the metabolism
of Mercaptopurine (4). Pharmacokinetic DDI is
a kind of interaction in which one drug changes
the pharmacokinetic factors of another drug
(absorption, distribution, metabolism and/or
exertion). When Fluorouracil and Warfarin are
administered together, a pharmacodynamic
DDI happens as Fluorouracil may significantly
potentiate the hypoprothrombinemic effect of
Warfarin (5). Pharmacodynamic DDI is a kind
of interaction that happens between two drugs
at the site of action. When Penicillins and
Aminoglycosides are administered together,
a pharmacodynamic DDI happens as they
inactivate each other in same IV. solution (6).
Pharmaceutical DDI is a kind of interaction in
Experimental
Methods
A cross-sectional study was conducted on 224
consecutive in-hospital patients in hematologyoncology ward of Taleghani hospital located in
Tehran, during a 12 mounth period from July 2009
to July 2010. Taleghani Hospital is affiliated to
Shahid Beheshti University of Medical Sciences
and is one of the largest referral cancer centers
in Iran.
Our study assessed hospitalized patients
medical chart records on hematology-oncology
ward. All hospitalized patients in hematologyoncology ward with diagnosis of solid tumor
and hematologic malignancy and were currently
receiving standard systemic cancer-directed
treatment were considered to be eligible.
In this ward, patients were visited 2 times
a day by their physicians. After visiting and
ordering registration in chart records, each order
176
Potential of Drug Interactions among Hospitalized Cancer Patients in a
Table 1. Drug-Drug interactions by severity levels (16, 17).
Severity levels
Potential effect of an adverse effect
Major
Life-threatening or permanent damage
Moderate
Minor
including age, gender, type of cancer, source
of cancer, number of ordered drugs and length
of hospital stay based on independent variables
including having at least one potential DDI on
the phamacotherapeutic protocol, and number of
potential DDIs per patients. Odds ratios and their
95% confidence intervals (CI) were estimated
through logistic regression model. Probability
value of less than 0.05 was considered significant.
Deterioration of patients status
Bothersome or little effect
was tabulated in a designed form. These forms
have demographic and medical information of
patients and were filled 2 times a day for each
patient. All ordered drugs in patients chart records
were tabulated in the forms for analyze regardless
of their actual administration. Complementary,
alternative and herbal medication and foods of
patients did not tabulate in designed forms for
future analyze.
Since the original software for drug
interactions was not available, Drug
Interaction Facts 2008, 2009: The Authority
on Drug Interactions was used for screening
the potential DDIs (16, 17). This book has
classified the potential DDIs by severity and
documentation levels. By the level of severity,
potential DDIs have been scored to three level
of major, moderate and minor (Table 1). By the
level of documentation they have been scored
to five level of established, probable, suspect,
possible and unlikely (Table 2).
Descriptive statistics including central
tendency measures and variability measures
were used to describe the data. KolmogorovSmirnov test was used to evaluate the normal
distribution of the variables. Independent sample
t-test, One-way Analysis of Variance, and chisquare test were applied to assess differences
among groups, where appropriate. Pearson
correlation coefficient was used to assess the
relationship between quantitative variables.
Multivariate linear and logistic regression was
applied with to predict dependent variables
Results
For one year period from July 2009 to
July 2010, chart records drugs orders of 224
consecutive eligible cancer hospitalized patients
were studied. Patients characteristics are
shown in Table 3. Median age of patients was
50 years ranging from 14 to 90 years. Females
were 37.5% of patients and approximately 73%
of patients were diagnosed with a solid tumor.
Length of hospital stay for patients varied from
2 to 40 days, with a median of 5 days. Number
of drugs in patients order ranged from 2 to 24
drugs, with a median of 8 drugs.
Number of potential DDIs found for each
patient in the ward ranged from 0-19 interactions
and the mean of potential DDI for each patient
is 1.02. All potential for these 224 patients were
228 interaction in this one year and 84 patients
(37.5%, 95%CI: 31-44%) had at least one
potential interaction on their screening.
Severity and documentation levels of
potential DDIs are shown on Tables 4 and
5. According to the severity level, 14.03%
of interactions were classified as major and
59.65% of them classified as moderate. Based
on the documentation level, 19.29% of the
interactions classified as established and
probable.
A qualitative study was done on the
Table 2. Drug-Drug interactions by documentation level (16, 17).
Documentation level
Type of scientific data for adverse effects
Established
Proven to occur in well-controlled studies
Probable
Very likely, but not proven clinically
Suspected
May occur; some good data, but needs more study
Possible
Could occur, but data are very limited
Unlikely
Doubtful; not good evidence of a clinical effect
177
Tavakoli-Ardakani M et al. / IJPR (2013), 12 (supplement): 175-182
Table 3. Patients characteristics.
Variable
Range Median
Number of patients
14-90
50
Age (years)
Sex
Female
84 (37.5%)
Male
140 (62.5%)
Tumor
Solid
163 (28%)
Hematologic
61 (72%)
Length of hospital stay (days)
2-40
4
Number of drugs per patient
2-24
8
screened potential DDIs. The most frequent
combination with the potential of interaction
in 224 patients was Cisplatin with Furosemide
which encountered 19 times. Next potential
interaction found was Magnesium hydroxide
with Dexamethasone which encountered 7
times. Potential interaction of Magnesium
hydroxide with Ranitidine encountered 6 times.
Potential interactions between Ciprofloxacin
with Doxorubicin and Acetaminophen with
Furosemide had the next frequency by 5 times.
Table 6 demonstrates characteristics of the
two groups of patient: patients with no potential
drug interaction and patients which have at least
one potential interaction on their orders. Patients
with at least one potential interaction are likely
to be older than 61 years old than patients with
no potential drug interaction (p = 0.024). But
no significant association explored between
patients older than 61 years old and number of
interactions and also no correlation was evident
between number of interactions in patients
and age (r = - 0.05, p = 0.938). Gender has no
significant tendency on two groups of patients,
with and without potential interaction, and
also gender did not affect number of potential
DDIs per patients. In patient with hematologic
cancer having potential DDI was significantly
more comparing with patients with a solid
tumor (54.09% versus 31.28%) (p = 0.002)
and also number of interactions in patients
with hematologic cancer is significantly more
than number of interactions in patients with
solid tumor (p = 0.019). Number of ordered
drugs and longer length of hospital stay were
associated with having potential DDI in patients
(p < 0.001, p < 0.001). Also both number of the
ordered drugs and longer length of hospital stay
were correlated with the number of interactions
found for each patients (r = 0.601 and 0.806,
p < 0.001 and p < 0.001). Source of cancer
in different organs have also associated with
having potential DDI in patients (p < 0.001).
All patients with esophageal cancer, testicular
cancer and cervical cancer have at least one
interaction on their medications. So these
patients are more probable to have interactions.
Also number of interactions per patient depends
on the source of cancer. (p = 0.007).
Descriptive statistics including central
Table 4. Drug-drug interactions by severity levels on patients found by screening.
Severity levels
Frequency
Percentile
Major
32
14.03%
Moderate
136
59.65%
Minor
60
26.31%
178
Potential of Drug Interactions among Hospitalized Cancer Patients in a
Table 5. Drug-drug interactions by documentation level.
Documentation level
Frequency
Percentile
Established
21
9.21%
Probable
23
10.09%
Suspect
68
29.82%
Possible
95
41.67%
Unlikely
21
9.21%
tendency measures and variability measures
were used to describe the data. KolmogorovSmirnov test was used to evaluate the normal
distribution of the variables. Independent sample
t-test, One-way Analysis of Variance, and chisquare test were applied to assess differences
among groups, where appropriate. Pearson
correlation coefficient was used to assess the
relationship between quantitative variables.
Multivariate linear and logistic regression was
applied with to predict dependent variables
including age, gender, type of cancer, source
of cancer, number of ordered drugs and length
of hospital stay based on independent variables
including having at least one potential DDI
on the phamacotherapeutic protocol, and
number of potential DDIs per patients. Odds
ratios and their 95% confidence intervals (CI)
were estimated through logistic regression
model. Probability value of less than 0.05 was
considered significant.
(37.5%, 95%CI: 31-44%) had at least one
potential interaction on their screening.
Severity and documentation levels of
potential DDIs are shown on Tables 4 and 5.
According to the severity level, 14.03% of
interactions were classified as major and 59.65%
of them classified as moderate. Based on the
documentation level, 19.29% of the interactions
classified as established and probable.
A qualitative study was done on the
screened potential DDIs. The most frequent
combination with the potential of interaction
in 224 patients was Cisplatin with Furosemide
which encountered 19 times. Next potential
interaction found was Magnesium hydroxide
with Dexamethasone which encountered 7
times. Potential interaction of Magnesium
hydroxide with Ranitidine encountered 6 times.
Potential interactions between Ciprofloxacin
with Doxorubicin and Acetaminophen with
Furosemide had the next frequency by 5 times.
Table 6 demonstrates characteristics of the
two groups of patient: patients with no potential
drug interaction and patients which have at least
one potential interaction on their orders. Patients
with at least one potential interaction are likely
to be older than 61 years old than patients with
no potential drug interaction (p = 0.024). But
no significant association explored between
patients older than 61 years old and number of
interactions and also no correlation was evident
between number of interactions in patients
and age (r = - 0.05, p = 0.938). Gender has no
significant tendency on two groups of patients,
with and without potential interaction, and
also gender did not affect number of potential
DDIs per patients. In patient with hematologic
cancer having potential DDI was significantly
more comparing with patients with a solid
tumor (54.09% versus 31.28%) (p = 0.002) and
also number of interactions in patients with
Results
For one year period from July 2009 to
July 2010, chart records drugs orders of 224
consecutive eligible cancer hospitalized patients
were studied. Patients characteristics are
shown in Table 3. Median age of patients was
50 years ranging from 14 to 90 years. Females
were 37.5% of patients and approximately 73%
of patients were diagnosed with a solid tumor.
Length of hospital stay for patients varied from
2 to 40 days, with a median of 5 days. Number
of drugs in patients order ranged from 2 to 24
drugs, with a median of 8 drugs.
Number of potential DDIs found for each
patient in the ward ranged from 0-19 interactions
and the mean of potential DDI for each patient
is 1.02. All potential for these 224 patients were
228 interaction in this one year and 84 patients
179
Tavakoli-Ardakani M et al. / IJPR (2013), 12 (supplement): 175-182
Table 6. Characteristics of the two groups of patients: patients with no potential drug interaction and patients which have at least one
potential interaction on their orders and their univariate analysis.
Variable
Total
With interaction
Without interaction
p-value
48.39 18.39
51.12 19.72
46.75 17.42
0.18
Male
140, 62.5%
54, 64.3%
86, 61.4%
0.66
Female
84, 37.5%
30, 35.7%
54, 38.6%
Solid
163, 72.8%
51, 60.7%
112, 80%
Hematologic
61, 27.2%
33, 39.3%
28, 20%
Length of hospital stay
6.54 5.45
8.55 7.59
5.34 3.06
< 0.001
Ordered drugs per patient
9.37 4.21
12.44 4.24
7.53 3.06
< 0.001
Age (years)
Sex (n, %)
Tumor (n, %)
hematologic cancer is significantly more than
number of interactions in patients with solid
tumor (p = 0.019). Number of ordered drugs and
longer length of hospital stay were associated with
having potential DDI in patients (p < 0.001, p <
0.001). Also both number of the ordered drugs and
longer length of hospital stay were correlated with
the number of interactions found for each patients
(r = 0.601 and 0.806, p < 0.001 and p < 0.001).
Source of cancer in different organs have also
associated with having potential DDI in patients
(p < 0.001). All patients with esophageal cancer,
testicular cancer and cervical cancer have at least
one interaction on their medications. So these
patients are more probable to have interactions.
Also number of interactions per patient depends
on the source of cancer. (p = 0.007).
Multivariate analysis showed that being older
than 61 years old, suffering from hematologic
cancer, source of cancer in different specific
organs (esophagus, testis and cervices more than
other sources), and number of ordered drugs for
patients were independent predictors of having
at least one potential DDI in hospital order.
Multivariate analysis on number of
interactions per patients as an independent factor
shows that suffering from hematologic cancer,
source of cancer in different organs, length of
hospital stay and number of ordered drugs for
patients were independent predictors for this
variable.
Discussion
0.002
pharamacotherapeutical medications. Becoming
hospitalized after a complication increases the
number of medications and raises the risk of
interactions on these people. It has been shown
that 4% mortality in hospitalized oncology
patients is because of their medication DDIs (9).
Frequency of potential DDIs and the risk
factors has widely been investigated in hospital
of modern countries (7-14) but it has not been
considered lot in developing countries. In
a Canadian study (2007), the frequency of
potential drug interactions between outpatients
receiving systemic anticancer therapy for solid
tumors in a 4 weeks period was 27%. (10) In
this study we want to encounter the frequency of
potential DDIs in a hematology-oncology ward
in a developing country.
Although all medical orders through hospital
stay have been screened for each patient,
frequency of potential drug interactions was
37.5% of patients. In a study in Brazil (2005),
unrelated to chemotherapy, potential of DDIs for
100 in-hospital cancer patients found to be 63%
in the midpoint of hospital stay but this study
didnt investigated all patients medication.
In this study, on the qualitative analysis,
nearly 28% of all interactions were for cancer
medications interactions with each other or with
a complication pharmacotherapy. Cisplatin and
Furosemide screened as about 30% of these
cancer medication interaction. Cisplatin can
increase the ototoxicity effects of loop diuretics
and hearing tests is necessary when administering
them together (16). Cyclophosphamide founded
to have 9 different interactions which was the
Cancer patients are at the high risk of
drug-drug interactions due to their complex
180
Potential of Drug Interactions among Hospitalized Cancer Patients in a
Table 7. Some important interactions between cancer medications with each other and with other complications medication.
Co-administration
Interaction
Mercaptopurine and Allopurinol
Allopurinol increase pharmacologic and toxic effect of Mercaptopurine when orally administered.
Fluorouracil and Warfarin
Fluorouracil increase the anticoagulant effect of Warfarin
Methotrexate and Vancomycin
Vancomycin can increase the risk of Methotrexate toxicity by elevating its serum concentration and
delaying its clearance
Methotrexate and Cotrimoxazole
(TMP-SMZ)
MTX-induced bone marrow suppression can be increase by using Cotrimoxazole. Methotrexate also
may predispose patients to (TMP-SMZ)-induces megaloblastic anemia
Irinotecan and Phenytoin
Phenytoin can reduce the antitumor activity of Irinotecan
Vincristine and Azole antifungal
Azole antifungals can increase the risk of Vinca alkaloid toxicity
Cyclophosphamide and warfarin
Cyclophosphamide can increase the anticoagulant effect of Warfarin
Etoposide and Warfarin
Etoposide can increase the anticoagulant effect of Warfarin
It must be mentioned that the clinical incidence
of the interactions are not followed in the
ward. Although reviewing hospital records of
patients may include the noting bias which was a
limitation of study.
In conclusion having a DDI seems to be more
likely to occur in patient olders than 61 years old.
Hematologic cancers, having more medications
in physicians order, longer length of hospital
stay, esophageal cancer, testicular cancer and
cervical cancer have related to having a DDI and
also having more number of interactions. In other
studies increasing numbers of drugs, type of
medication (drugs to treat comorbid conditions),
presence of brain tumors found to be risk factors
for patients interaction. (9) In Brazilian study
which was a developing country (2005) being
more than 67 years, hospital stay more than 6
days and having more than 8 drugs in order was
the risk factor for DDI which is consistent with
the results found in this study. It is important to
consider these risk factors to recognize DDIs
occurrence and minimize the dangerous effect of
their incidence. It could be important to highlight
the role of clinical pharmacists in having
collaboration with oncologists on hematology
and oncology wards of developing countries.
most number between cancer medications,
which can be due to the usage of this drug for
different types of malignancy. Nearly 22% of
these interactions were for co-administration for
Ciprofloxacin with Vincristine, Doxorubicin and
cytarabine which must be considered more in
cancer patients, because patients with leukemia
and lymphoma are more susceptible to infection
during and after chemotherapy, so they use
many antibiotics such as ciprofloxacin. Some
important interactions in these cases are shown
in Table 7. On non-chemotherapy medications
co-administration of Magnesium Hydroxide
with Dexamethasone, Ranitidine, Furosemide
and Acetaminophen have the most frequency.
Receiving chemotherapy regimen, cancer
patients are at the risk of gastrointestinal adverse
effects like dyspepsia, diarrhea, constipation and
reflux. Since the more antacid they use for these
adverse effects, the more shown interactions
will happens. So it is recommended to use the
Proton-pump inhibitors such as pantoprazol (not
omeprazole) instead of antacids or use lactulose
as a laxative instead of magnesium hydroxide
which may have less DDIs. Some important
interactions
between
non-chemotherapy
medications in these cases are shown in Table 8.
It must be cleared that these 37.5% interactions
which found from all patients are potential
drug-drug interactions which only screened
through all patients medical orders at the length
of hospital stay on the reference. As it can be
seen nearly 10% of these interactions are just
theoretical mechanisms of action and just about
10% of them confirmed by large clinical trials.
Acknowledgment
This research was supported by Shahid
Beheshti University of Medical Sciences.
The authors of this paper, which is a
production of a Pharm.D. student thesis, would
like to thank all personnel and nursing staff of
181
Tavakoli-Ardakani M et al. / IJPR (2013), 12 (supplement): 175-182
Taback NA and Krzyzanowska MK. Potential drug
interactions and duplicate prescriptions among
cancer patients. J Natl. Cancer. Inst. (2007) 99:
592-600.
(10) Zwart-van Rijkom JE, Uijtendaal EV, ten Berg MJ,
van Solinge WW and Egberts AC. Frequency and
nature of drug-drug interactions in a Dutch university
hospital. Br. J. Clin. Pharmacol. (2009) 68: 187-93.
(11) Sokol KC, Knudsen JF and Li MM. Polypharmacy
in older oncology patients and the need for an
interdisciplinary approach to side-effect management.
J. Clin. Pharm. Ther. (2007) 32: 169-75.
(12) Riechelmann RP, Zimmermann C, Chin SN, Wang
L, OCarroll A, Zarinehbaf S and Krzyzanowska
MK. Potential drug interactions in cancer patients
receiving supportive care exclusively. J Pain
Symptom Manage. (2008) 35: 535-43.
(13) Egger SS, Drewe J and Schlienger RG. Potential
drug-drug interactions in the medication of medical
patients at hospital discharge. Eur. J. Clin. Pharmacol.
(2003) 58: 773-8
(14) Glintborg B, Andersen SE and Dalhoff K. Drug-drug
interactions among recently hospitalised patients-frequent but mostly clinically insignificant. Eur. J.
Clin. Pharmacol. (2005) 61: 675-81.
(15) Riechelmann RP, Moreira F, Smaletz O and Saad
ED. Potential for drug interactions in hospitalized
cancer patients. Cancer. Chemother. Pharmacol.
(2005) 56: 286-90.
(16) Tatro Ds. Drug Interaction Facts 2009: The
Authority on Drug Interactions. Lippincott Williams
& Wilkins, (2008).
(17) Tatro Ds. Drug Interaction Facts 2008: The
Authority on Drug Interactions. Lippincott Williams
& Wilkins, (2007).
the medical records department and oncology/
hematology and BMT ward of Taleghani
hospital, Tehran, Iran.
References
(1) Beijnen JH and Schellens JH. Drug interactions in
oncology. Lancet. Oncol. (2004) 5: 489-96.
(2) Blower P, de Wit R, Goodin S and Aapro M.
Drug-drug interactions in oncology: why are they
important and can they be minimized? Crit. Rev.
Oncol. Hematol. (2005) 55: 117-42.
(3) Nazari AM and Moqhadam K N. Evaluation of
Pharmacokinetic Drug Interactions in Prescriptions
of Intensive Care Unit (ICU) in a Teaching Hospital.
Iran. J. Pharm. Res. (2006) 3: 215-218.
(4) Murrell GA and Rapeport WG. Clinical
pharmacokinetics of allopurinol. Clin. Pharmacokinet.
(1986) 11: 343-53.
(5) Holbrook AM, Pereira JA, Labiris R, McDonald
H, Douketis JD, Crowther M and Wells PS.
Systematic overview of warfarin and its drug and
food interactions. Arch. Intern. Med. (2005) 165:
1095-106.
(6) Farchione LA. Inactivation of aminoglycosides by
penicillins. J. Antimicrob. Chemother. (1981) 8
Suppl A: 27-36.
(7) Van Leeuwen RW, Swart EL, Boom FA,
Schuitenmaker MS, and Hugtenburg JG. Potential
drug interactions and duplicate prescriptions among
ambulatory cancer patients: a prevalence study
using an advanced screening method. BMC. Cancer.
(2010) 10: 679.
(8) Buajordet I, Ebbesen J, Erikssen J, Brrs O and
Hilberg T. Fatal adverse drug events: the paradox of
drug treatment. J. Intern. Med. (2001) 250: 327-41.
(9) Riechelmann RP, Tannock IF, Wang L, Saad ED,
This article is available online at http://www.ijpr.ir
182
Anda mungkin juga menyukai
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
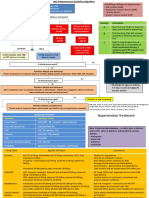
- General Population (No Diabetes or CKD) Diabetes or CKD PresentDokumen2 halamanGeneral Population (No Diabetes or CKD) Diabetes or CKD PresentLalu Ranova100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Evaluation of The Painful EyeDokumen9 halamanEvaluation of The Painful EyeMuthia Farah AshmaBelum ada peringkat
- 0555 - Healthcare Risk Assessment Made Easy PDFDokumen16 halaman0555 - Healthcare Risk Assessment Made Easy PDFCecilia YeniBelum ada peringkat
- Biodiversity of Micro-OrganismsDokumen32 halamanBiodiversity of Micro-Organismsapi-20234922250% (2)
- Risk Assessment: Healthy Working LivesDokumen4 halamanRisk Assessment: Healthy Working LivesGaby ValenzuelaBelum ada peringkat
- Risk Assessment: (Worked Example)Dokumen4 halamanRisk Assessment: (Worked Example)s sanjaiBelum ada peringkat
- Fiscal Health Risk Analysis K 12-4-2015 FinalDokumen7 halamanFiscal Health Risk Analysis K 12-4-2015 FinalGaby ValenzuelaBelum ada peringkat
- Risk Assessment: (Worked Example)Dokumen4 halamanRisk Assessment: (Worked Example)s sanjaiBelum ada peringkat
- MEDDEV 2.7/3 SeriDokumen6 halamanMEDDEV 2.7/3 Serifl_in1Belum ada peringkat
- JRSM 12 0037Dokumen10 halamanJRSM 12 0037Gaby ValenzuelaBelum ada peringkat
- Ni Hms 266357Dokumen15 halamanNi Hms 266357Gaby ValenzuelaBelum ada peringkat
- Review Article: Sex Differences in Drug DispositionDokumen14 halamanReview Article: Sex Differences in Drug DispositionGaby ValenzuelaBelum ada peringkat
- Impact of en ISC-2013 11 6 2013Dokumen4 halamanImpact of en ISC-2013 11 6 2013Gaby ValenzuelaBelum ada peringkat
- Hvi 8 1326Dokumen9 halamanHvi 8 1326Gaby ValenzuelaBelum ada peringkat
- Patient-Centered Communication: Original ArticlesDokumen12 halamanPatient-Centered Communication: Original ArticlesGaby ValenzuelaBelum ada peringkat
- I0003 3006 58 1 31 PDFDokumen11 halamanI0003 3006 58 1 31 PDFGaby ValenzuelaBelum ada peringkat
- Imdrf Proc 151002 Ncar Implementation Material n31Dokumen43 halamanImdrf Proc 151002 Ncar Implementation Material n31Gaby ValenzuelaBelum ada peringkat
- Ni Hms 455527Dokumen13 halamanNi Hms 455527Gaby ValenzuelaBelum ada peringkat
- Study of Drug-Drug Interactions in Prescriptions of General Practitioners and Specialists in Iran 2007-2009Dokumen12 halamanStudy of Drug-Drug Interactions in Prescriptions of General Practitioners and Specialists in Iran 2007-2009Gaby ValenzuelaBelum ada peringkat
- Ni Hms 4256260Dokumen30 halamanNi Hms 4256260Gaby ValenzuelaBelum ada peringkat
- Ni Hms 455524Dokumen14 halamanNi Hms 455524Gaby ValenzuelaBelum ada peringkat
- Drug Interactions: The Clinician S Approach ToDokumen11 halamanDrug Interactions: The Clinician S Approach ToGaby ValenzuelaBelum ada peringkat
- 80 X 2018 Action Plan Final - VermontDokumen1 halaman80 X 2018 Action Plan Final - VermontGaby ValenzuelaBelum ada peringkat
- Ni Hms 449374Dokumen5 halamanNi Hms 449374Gaby ValenzuelaBelum ada peringkat
- ZDD 32Dokumen8 halamanZDD 32Gaby ValenzuelaBelum ada peringkat
- Fphar 03 00069Dokumen19 halamanFphar 03 00069Gaby ValenzuelaBelum ada peringkat
- Ni Hms 513647Dokumen21 halamanNi Hms 513647Gaby ValenzuelaBelum ada peringkat
- Perspective Herb - Drug Interactions: Challenges and Opportunities For Improved PredictionsDokumen17 halamanPerspective Herb - Drug Interactions: Challenges and Opportunities For Improved PredictionsGaby ValenzuelaBelum ada peringkat
- Ajpe 7510199Dokumen4 halamanAjpe 7510199Gaby ValenzuelaBelum ada peringkat
- Clinical Guide SEOM On Venous Thromboembolism in Cancer PatientsDokumen12 halamanClinical Guide SEOM On Venous Thromboembolism in Cancer PatientsGaby ValenzuelaBelum ada peringkat
- Ni Hms 525847Dokumen19 halamanNi Hms 525847Gaby ValenzuelaBelum ada peringkat
- Ni Hms 562777Dokumen17 halamanNi Hms 562777Gaby ValenzuelaBelum ada peringkat
- A Pre Experimental Study To Assess The Effectiveness of Planned Teaching Programme On Knowledge Towards Safe Handling of Chemotherapeutics Drugs Among Staff Nurses in C.H.R.I Gwalior M.PDokumen6 halamanA Pre Experimental Study To Assess The Effectiveness of Planned Teaching Programme On Knowledge Towards Safe Handling of Chemotherapeutics Drugs Among Staff Nurses in C.H.R.I Gwalior M.PEditor IJTSRDBelum ada peringkat
- Effects of The Treatment Method of Reproductive Performance in Cows With Retention of Fetal MembranesDokumen10 halamanEffects of The Treatment Method of Reproductive Performance in Cows With Retention of Fetal MembranesAlberto BrahmBelum ada peringkat
- Discuss Ethical and Cultural Consideration in DiagnosisDokumen2 halamanDiscuss Ethical and Cultural Consideration in DiagnosisJames Harlow0% (1)
- Quality Form Oplan Kalusugan Sa Deped Accomplishment Report FormDokumen11 halamanQuality Form Oplan Kalusugan Sa Deped Accomplishment Report Formchris orlanBelum ada peringkat
- ELISIO Clinical StudiesDokumen12 halamanELISIO Clinical StudiesIndra NugrohoBelum ada peringkat
- Diarrhea: On This PageDokumen6 halamanDiarrhea: On This PageKristine AlejandroBelum ada peringkat
- Toxicology-Handbook PDFDokumen2 halamanToxicology-Handbook PDFssb channelBelum ada peringkat
- SymbicortDokumen18 halamanSymbicortkaditasookdeoBelum ada peringkat
- Full Download Book Medical Epigenetics PDFDokumen41 halamanFull Download Book Medical Epigenetics PDFandrew.lindsey981100% (14)
- Implementasi Program Antenatal Terpadu Di Puskesmas Tanjung Agung Kabupaten Ogan Komering Ulu Dengan Pendekatan Balance ScorecardDokumen9 halamanImplementasi Program Antenatal Terpadu Di Puskesmas Tanjung Agung Kabupaten Ogan Komering Ulu Dengan Pendekatan Balance ScorecardRosinta Dwi OktaviaBelum ada peringkat
- HLTENN045 - HO - Physiological Changes and Affect Nursing CareDokumen3 halamanHLTENN045 - HO - Physiological Changes and Affect Nursing CareChepwogen TowettBelum ada peringkat
- Leung 2019Dokumen10 halamanLeung 2019Ari KurniawanBelum ada peringkat
- NeedlestickDokumen14 halamanNeedlestickluis_chubeeBelum ada peringkat
- Ok Urologi Maret 2021 Minggu IDokumen25 halamanOk Urologi Maret 2021 Minggu ILittle DevBelum ada peringkat
- Centrilobular Fibrosis in Fibrotic (Chronic)Dokumen8 halamanCentrilobular Fibrosis in Fibrotic (Chronic)yuriescaidaBelum ada peringkat
- ASTHMADokumen48 halamanASTHMAifcrstarsBelum ada peringkat
- Emergency DrugsDokumen10 halamanEmergency DrugsnieacatleyaBelum ada peringkat
- Coronary Artery Bypass SurgeryDokumen3 halamanCoronary Artery Bypass Surgeryapi-355048975Belum ada peringkat
- UrosepsaDokumen2 halamanUrosepsaHazir AziriBelum ada peringkat
- Bio Investigatory ProjectDokumen24 halamanBio Investigatory ProjectTIBIN DANIEL BijuBelum ada peringkat
- Fynadine 20mgDokumen2 halamanFynadine 20mgNgo Van TruongBelum ada peringkat
- Viva GuideDokumen27 halamanViva GuideCHIMA ONWUKA MONGBelum ada peringkat
- Instrument Cleaning ProgramDokumen6 halamanInstrument Cleaning ProgramGood M ArifinBelum ada peringkat
- La Union Arrival Card - V1 PDFDokumen2 halamanLa Union Arrival Card - V1 PDFLorei LeeBelum ada peringkat
- Ambulance App - Book An Ambulance in A ClickDokumen4 halamanAmbulance App - Book An Ambulance in A ClickbloodforsureBelum ada peringkat
- Discontinuing β-lactam treatment after 3 days for patients with community-acquired pneumonia in non-critical care wards (PTC) : a double-blind, randomised, placebo-controlled, non-inferiority trialDokumen9 halamanDiscontinuing β-lactam treatment after 3 days for patients with community-acquired pneumonia in non-critical care wards (PTC) : a double-blind, randomised, placebo-controlled, non-inferiority trialSil BalarezoBelum ada peringkat
- Midterms Psyc LecDokumen14 halamanMidterms Psyc LecMiden AlbanoBelum ada peringkat