2013 Radiotherapy For Spermatic Cord Sarcoma
Diunggah oleh
nelsonJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
2013 Radiotherapy For Spermatic Cord Sarcoma
Diunggah oleh
nelsonHak Cipta:
Format Tersedia
ORIGINAL ARTICLE
Radiotherapy for Spermatic Cord Sarcoma
Ronica Hazariwala, BS,* Christopher G. Morris, MS,* Scott Gilbert, MD,w
Chester Algood, MD,w and Robert A. Zlotecki, MD, PhD*w
Objectives: Spermatic cord sarcomas are rare paratesticular tumors
affecting older men. Current management is based on small series, case
reports, and literature reviews, with surgery still the mainstay of
treatment. Local-regional recurrence is common after definitive surgery (B50%), but patients treated with adjuvant radiotherapy may
have improved outcomes.
Methods: We reviewed the outcomes of 15 patients with intermediategrade to high-grade spermatic cord sarcomas treated with radiation at
our institution from 1974 to 2009. Patients were treated to 40 to 60 Gy
using conformal opposed anterior-posterior/posterior-anterior ports to
the scrotum, inguinal canal, and lower pelvic wall with various beam
energies. Some patients were managed with surgical exploration and
resection, followed by radiotherapy and/or definitive surgery. More
recently treated patients had an initial biopsy, followed by preoperative
radiation or planned resection with postoperative radiation therapy.
Results: No patient experienced a local recurrence. Two patients had
regional nodal recurrences and 1 had distant metastases. All recurrences were in patients who had initial exploration with unexpected
findings of sarcoma during surgery versus planned, definitive resection
with planned adjuvant radiotherapy. At 5 years, overall survival was
53%, but cause-specific survival was 80%. Complications were minimal, with only 4 grade 2 or 3 toxicities and no grade 4 toxicities.
Conclusions: Although most patients die from causes other than disease progression, this sarcoma carries grave morbidity. Optimizing the
primary management is of utmost importance. Unplanned treatments
complicate definitive therapy and increase the risk of local-regional
contamination and recurrence. Proactive management is therefore
consistent with sarcomas of other primary sites, ideally with preoperative radiotherapy and definitive resection.
Key Words: spermatic cord, sarcoma, surgical exploration, radiation
(Am J Clin Oncol 2013;36:392394)
permatic cord sarcomas are rare tumors of the paratesticular region affecting primarily older men. Because
these tumors are not well studied, their incidence has not been
quantified. Patients typically present with a nontender mass
within the inguinal region or scrotum, sometimes confused
with either an inguinal hernia or a testicular tumor. Without
complete and appropriate imaging and diagnostic studies, most
of these patients are taken to the operating room for herniorrhaphy or exploratory surgery, with a cancer diagnosis made
intraoperatively. In addition, there is no current well-defined
standard for radiographic evaluation of the inguinal region.
Ultrasonography is indicated for testicular and scrotal masses,1
From the Departments of *Radiation Oncology; and wUrology, University
of Florida College of Medicine, Gainesville, FL.
The authors declare no conflicts of interest.
Reprints: Robert A. Zlotecki, MD, PhD, 2000 SW Archer Rd., PO Box
100385, Gainesville, FL 32610-0385. E-mail: zlotera@ufl.edu.
Copyright r 2012 by Lippincott Williams & Wilkins
ISSN: 0277-3732/13/3604-0392
DOI: 10.1097/COC.0b013e318248dc51
392 | www.amjclinicaloncology.com
but because of variable histologies of these sarcomas, their
respective echogenities are also variable. Computed tomography scans can help exclude a hernia diagnosis, better define
the nature and extent of the mass lesion, indicate pelvic staging, and rule out distant metastasis.1
As an extremely rare malignancy, the recommendations for
management and treatment are based on small retrospective series, case reports, and reviews of the literature. These sarcomas are
typically treated surgically, but because of their location, anatomic
restrictions often preclude achieving the wide, clear resection
margins needed for complete cure. As demonstrated in several
small series,2 even after such definitive surgery, there is an approximately 50% rate of local-regional recurrence. The evidence
to suggest that radiation therapy (RT) before or after surgery
affects outcomes remains equivocal, as rates of nodal failure,
regional and distant metastasis, and overall survival with RT are
largely unknown. Thus, the utility of RT in the management of
sarcomas of the spermatic cord remains controversial even today.
METHODS AND MATERIALS
Under an institutional review board-approved protocol,
we retrospectively reviewed the surgical and RT treatment
plans and outcomes of 15 patients with sarcomas of the spermatic cord managed definitively at the University of Florida
between 1974 and 2009. Patients were contacted when necessary to obtain follow-up. Local and regional primary disease
control, patterns of disease recurrence or progression, and
overall outcomes and patient survival were analyzed.
Radiation treatment in this cohort consisted of both preoperative and postoperative adjuvant therapy. Early in the series,
postoperative adjuvant radiotherapy dominated, and, over the
last decade, planned preoperative radiotherapy was used as is
consistent with standard management of sarcomas of other sites.
Conformal portals, either anterior-posterior and conformal posterior-anterior, or parallel-opposed oblique portals were primarily used, treating the scrotal area, inguinal canal, and
ipsilateral lower pelvic nodes and side walls to irradiation doses
of 40 to 60 Gy. Sequential cone-down ports and surgical scar
coverage with bolus was incorporated into treatment and delivery as appropriate. Exclusion and shielding of the remaining
viable testicle was standard practice. Megavoltage photon energies were used, including Cobalt-60 and 6 MV to 18-20 MV
mixed photons, with the higher energies reserved for the pelvic
nodes. Standardized daily fractionation of 1.8 or 2.0 Gy was
typical, although more recently hyperfractionated RT at 1.2 Gy
has been delivered.
All statistical calculations were accomplished with SAS
and JMP software (SAS Institute, Cary, NC). The KaplanMeier product-limit method provided estimates of local control, overall survival, and cause-specific survival.
RESULTS
The median age of the patients in this analysis was
55-years-old (range, 5- to 79-years-old). The median length
American Journal of Clinical Oncology
Volume 36, Number 4, August 2013
American Journal of Clinical Oncology
Volume 36, Number 4, August 2013
Spermatic Cord Sarcoma
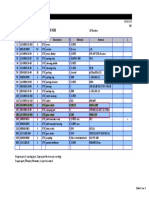
FIGURE 1. Management of patients with exploratory surgery.
of follow-up was approximately 7 years (range, 1.3 to 19.4 y).
All of the cases revealed intermediate-grade to high-grade
histology, with 5 cases of malignant fibrous histiocytoma, 5
cases of leiomyosarcoma, 3 cases of liposarcoma, and 2 cases
involving histologic subtypes. The median tumor size at
maximum dimension was 8 cm (range, 3 to 15 cm).
The 15 patients in this series presented and were managed
in a variety of ways. One group of patients was approached
with exploratory surgery, highlighted in Figure 1, and represents patients mostly treated in earlier decades. Another group
of patients was managed more conservatively, highlighted
in Figure 2, and represents patients treated in later years.
Local-regional Control
There were no local recurrences in this group of 15 patients.
Two patients suffered from regional metastases to the ipsilateral
pelvic nodes. In one case, the patient had exploration and gross
total resection with positive margins before RT. In the other case,
the patient had exploration with gross residual disease, followed
by planned management and was disease-free for 4 years. Unfortunately, he then had 4 regional recurrences, which were
managed surgically before any additional RT was given.
Survival
Only 2 patients died of disease: 1 who experienced
multiple regional recurrences and expired after his sixth attempted surgical resection and the second from a distant
metastasis to the lung, after suffering from delayed diagnosis
for over 1 year before definitive management could be initiated.
Overall, at last follow-up, 8 patients had no evidence of
disease and 5 patients had died from diseases unrelated to their
sarcoma. Thus, at 5 years, local control was 100%, causespecific survival was 80%, and overall survival was 46%, as
shown in Figure 3.
Complications
Few complications were found in our study despite the
sensitive nature of the proximal medial thigh being recognized
for high risks of combined radiotherapy and surgical complications. Complications were scored using the National Cancer
Institutes Common Terminology Criteria for Adverse Events,
version 4.0.3 We had 2 patients with chronic pelvic pain (grade
2), 1 patient with cellulitis requiring incision, drainage, and
antibiotics (grade 3), and 1 patient with bilateral lower-extremity
lymphedema (grade 2).
DISCUSSION
Our results demonstrate that spermatic cord sarcomas are
unlikely to metastasize as compared with soft-tissue sarcomas of
the extremities and other sites and that their growth and development tend to be more indolent. In addition, these tumors are
usually found earlier in the disease process compared with sarcomas of other sites due to their sensitive location, which may
positively affect their outcomes. Ultimately regional control and
survival are exceptional for this group of sarcomas. Recurrences
FIGURE 2. Management of patients with planned resections.
r
2012 Lippincott Williams & Wilkins
www.amjclinicaloncology.com |
393
Hazariwala et al
American Journal of Clinical Oncology
FIGURE 3. Five-year survival outcomes.
were in patients who had undergone unplanned exploration
procedures with unexpected findings of malignant sarcoma, as
opposed to those cases with planned or definitive resection
procedures managed with appropriately coordinated adjuvant
radiotherapy, and they have remained disease-free.
As noted earlier, there is a large disparity between causespecific survival and overall survival, suggesting that these
patients are largely dying from other causes or from old age,
rather than the spermatic cord sarcoma itself. Notably, however, despite its low potential for mortality and death due to
distant or diffuse metastases, this disease carries grave potential for local and regional pelvic morbidity, and thus optimizing local control is of the utmost importance.
The study from Massachusetts General Hospital (Boston,
MA) by Fagundes et al,4 a revision of the first study of spermatic cord sarcomas, similarly found that patients treated with
both radiation and surgery fared significantly better than those
treated with surgery alone. The study by Ballo et al5 from the
MD Anderson Cancer Center (Houston, TX) indicated longterm outcomes comparable with ours in terms of local-regional
control and overall survival, although they followed patients
up to 10 years out. Our series includes 15 patients, representing
significantly more cases treated with adjuvant RT than either
of these studies of 9 and 3 patients, respectively. Catton et al6
published a series of 14 patients treated with postoperative
radiotherapy after repeat wide local excision and found similar
results in terms of local control. Cause-specific survival and
rates of distant metastasis were, however, slightly poorer in
this cohort. Patients in our study did receive irradiation to the
scrotum, inguinal canal, and lower pelvic wall, similar to the
Catton study, but did not routinely have retroperitoneal node
dissection as a proactive measure. Although our outcomes
were better than those in the Catton study, more patients in the
Catton series were managed with surgery followed by postoperative radiation compared with our series. A prospective,
randomized trial would be the ideal approach to devising an
optimal treatment strategy, determining which patients may
benefit from systemic therapy, and confirming the benefits of
coordinated adjuvant preoperative radiotherapy with planned
oncologic surgical resection procedures. In addition, the previously cited MD Anderson report suggests that the risk of
nodal failure is low, as it is for most extremity soft-tissue
sarcoma histologies, and a formal study could help confirm this
394 | www.amjclinicaloncology.com
Volume 36, Number 4, August 2013
question. Thus, if the rates of nodal failure are indeed low, then
the extent of the low pelvic radiation portals can be minimized
as well as the boundaries of the surgical resection, thereby
decreasing potential treatment toxicity. However, such a study
would require a large patient pool in order to adequately power
the endpoints and, given the rarity of these sarcomas, it is
unlikely that such a study will be conducted. Our study looked
at both patients treated preoperatively and postoperatively as
well as patients who did and did not undergo definitive surgery. Given the natural history of this disease, a longer period
of follow-up would be beneficial to determine long-term outcomes of local-regional control, cause-specific survival, and
integrity of the treated tissues.
As a retrospective case series, this study has several
limitations, despite the potential value of such a study design.
First, one must depend on the accuracy of the medical record
and its availability. The data in the chart are also subject to
patient recall bias. In addition, the study is prone to selection
bias, as the investigator is the one to choose the cases. Finally,
there are no control cases in this study. Further studies comparing patients treated solely with surgery versus those treated
with neoadjuvant radiation and surgery may be of value. Alternatively, additional studies examining various radiation
fields may help to determine if some toxicities can be limited
or if outcomes can be further improved.
CONCLUSIONS
Proper evaluation and diagnostic staging before initiating
planned treatment is critical, which can allow proactive management comparable with that of sarcomas of other primary
sites. Unplanned management, as we have seen, greatly complicates appropriate therapy and increases the risk of contamination around the tumor site and thus local-regional
recurrence. Compared with other sarcomas, most patients
survive their disease and die of unrelated causes, likely due to
early detection secondary to its location and readily apparent
symptoms. However, improper management can severely
compromise quality of life for these patients, and delayed
treatment carries a grave prognosis. To avoid such adverse
outcomes and morbidity, we strongly recommended planned,
preoperative radiotherapy followed by definitive resection
procedures as the optimal management strategy.
REFERENCES
1. Cardenosa G, Papanicolaou N, Fung Cy, et al. Spermatic cord sarcomas:
sonographic and CT features. Urol Radiol. 1990;12:163167.
2. Enoch S, Wharton SM, Murray DS. Management of leiomyosarcomas of the spermatic cord: the role of reconstructive surgery. World
J Surg Oncol. 2005;3:23. (Article no.).
3. Cancer Therapy Evaluation Program. Common Terminology
Criteria for Adverse Events v4.0, DCTD, NCI, NIH, DHHS.
http://ctep.cancer.gov/protocolDevelopment/electronic_applications/
docs/ctcae_index.pdf#search = "common terminology". Updated
April 15, 2010. Accessed June 4, 2010.
4. Fagundes MA, Zietman AL, Althausen AF, et al. The management
of spermatic cord sarcoma. Cancer. 1996;77:18731876.
5. Ballo MT, Zagars GK, Pisters PW, et al. Spermatic cord sarcoma:
outcome, patterns of failure and management. J Urol. 2001;
166:13061310.
6. Catton C, Jewett M, OSullivan B, et al. Paratesticular sarcoma:
failure patterns after definitive local therapy. J Urol. 1999;
161:18441847.
2012 Lippincott Williams & Wilkins
Anda mungkin juga menyukai
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Fe jkj101Dokumen5 halamanFe jkj101ApezAnuarBelum ada peringkat
- Ora Laboratory Manual: Section 1 Section 1Dokumen36 halamanOra Laboratory Manual: Section 1 Section 1Ahmed IsmailBelum ada peringkat
- ZW250-7 BROCHURE LowresDokumen12 halamanZW250-7 BROCHURE Lowresbjrock123Belum ada peringkat
- Chapter 4 Occupational Safety Hazards in Food Service OperationsDokumen14 halamanChapter 4 Occupational Safety Hazards in Food Service OperationsStraichea Mae TabanaoBelum ada peringkat
- Sample Dewa Inspection CommentsDokumen2 halamanSample Dewa Inspection Commentsrmtaqui100% (1)
- Marxism and The Oppression of Women Lise VogelDokumen259 halamanMarxism and The Oppression of Women Lise VogelMoises SaavedraBelum ada peringkat
- Notice - Appeal Process List of Appeal Panel (Final 12.1.24)Dokumen13 halamanNotice - Appeal Process List of Appeal Panel (Final 12.1.24)FyBerri InkBelum ada peringkat
- The Western and Eastern Concepts of SelfDokumen3 halamanThe Western and Eastern Concepts of SelfTakumi Shawn Hinata100% (3)
- Pantalla Anterior Bienvenido: Cr080vbesDokumen3 halamanPantalla Anterior Bienvenido: Cr080vbesJuan Pablo Virreyra TriguerosBelum ada peringkat
- Strange Christmas TraditionsDokumen2 halamanStrange Christmas TraditionsZsofia ZsofiaBelum ada peringkat
- Chapter 1 - Part 1 Introduction To Organic ChemistryDokumen43 halamanChapter 1 - Part 1 Introduction To Organic ChemistryqilahmazlanBelum ada peringkat
- 4 Pure BendingDokumen42 halaman4 Pure BendingOmarfirozBelum ada peringkat
- Battery Installation ProcedureDokumen5 halamanBattery Installation ProceduresantoshkumarBelum ada peringkat
- IDRW MagazineDokumen10 halamanIDRW MagazineVirarya100% (1)
- What A Wonderful WorldDokumen3 halamanWhat A Wonderful Worldapi-333684519Belum ada peringkat
- Need For Advanced Suspension SystemsDokumen10 halamanNeed For Advanced Suspension SystemsIQPC GmbHBelum ada peringkat
- Rezhna Hassan FarajDokumen2 halamanRezhna Hassan FarajchristoptBelum ada peringkat
- Solids Separation Study Guide: Wisconsin Department of Natural Resources Wastewater Operator CertificationDokumen44 halamanSolids Separation Study Guide: Wisconsin Department of Natural Resources Wastewater Operator CertificationkharismaaakBelum ada peringkat
- (ARTICLE) Misguided in Understanding The Term Open MindedDokumen8 halaman(ARTICLE) Misguided in Understanding The Term Open MindedMuhammad Rafeli FakhlipiBelum ada peringkat
- Feasibility Study On The Seaweed Kappaphycus Alvarezii Cultivation Site in Indari Waters ofDokumen9 halamanFeasibility Study On The Seaweed Kappaphycus Alvarezii Cultivation Site in Indari Waters ofUsman MadubunBelum ada peringkat
- Etl 213-1208.10 enDokumen1 halamanEtl 213-1208.10 enhossamBelum ada peringkat
- QIAGEN Price List 2017Dokumen62 halamanQIAGEN Price List 2017Dayakar Padmavathi Boddupally80% (5)
- 1.1 Introduction To KennametalDokumen40 halaman1.1 Introduction To KennametalVig PankajBelum ada peringkat
- EU - Guidance On GMP For Food Contact Plastic Materials and Articles (60p)Dokumen60 halamanEU - Guidance On GMP For Food Contact Plastic Materials and Articles (60p)Kram NawkBelum ada peringkat
- Plaquette - PRECASEM - CIMEC 2019 English VersionDokumen18 halamanPlaquette - PRECASEM - CIMEC 2019 English VersionFranck BertrandBelum ada peringkat
- Syllabi: The Institution of Engineers, Sri LankaDokumen107 halamanSyllabi: The Institution of Engineers, Sri LankaAmal Priyashantha Perera100% (2)
- Brainedema 160314142234Dokumen39 halamanBrainedema 160314142234Lulu LuwiiBelum ada peringkat
- Charles Haanel - The Master Key System Cd2 Id1919810777 Size878Dokumen214 halamanCharles Haanel - The Master Key System Cd2 Id1919810777 Size878Hmt Nmsl100% (2)
- T 1246784488 17108574 Street Lighting Control Based On LonWorks Power Line CommunicationDokumen3 halamanT 1246784488 17108574 Street Lighting Control Based On LonWorks Power Line CommunicationsryogaaBelum ada peringkat
- Bsi MD Ivdr Conformity Assessment Routes Booklet Uk enDokumen15 halamanBsi MD Ivdr Conformity Assessment Routes Booklet Uk enGuillaumeBelum ada peringkat