Laparoscopic Gastrointestinal Surgery
Diunggah oleh
Roxana BoloagaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Laparoscopic Gastrointestinal Surgery
Diunggah oleh
Roxana BoloagaHak Cipta:
Format Tersedia
Med Clin N Am 86 (2002) 14011422
Laparoscopic gastrointestinal surgery
Carol E.H. Scott-Conner, MD, PhD
Department of Surgery, University of Iowa College of Medicine, 200 Hawkins Drive,
#1516 JCP, Iowa City, IA 52242, USA
Nearly one century ago Kelling [1,2] and Jacobaeus [3] rst inated the
human peritoneal cavity with air and inserted a cystoscope [4]. After numerous small incremental improvements during the next 75 years, Semm [5] was
able to perform a wide spectrum of gynecologic and pelvic procedures,
including incidental appendectomy, with a direct-viewing scope and minimal instrumentation. The introduction of video technology and improvements in hemostatic, stapling, and suturing devices led to the current era
in which minimal-access surgical techniques, including laparoscopy, have
been extended to all areas of surgery. This article briey describes the wide
spectrum of gastrointestinal procedures currently performed laparoscopically. For most of the described procedures, a well-established open surgical
technique has been adapted for minimal-access surgery. The indications for
surgery have remained the same, and the results obtained have often been
comparable with those obtained with the open procedure. Several laparoscopic procedures, such as laparoscopic cholecystectomy (LC), esophagomyotomy for achalasia, and fundoplication for gastroesophageal reux
disease (GERD), have shown clear advantages and superceded the open
procedure. In most procedures, however, advantages are less clear and the
laparoscopic approach is used selectively. The long-term results of laparoscopic cancer surgery are still under investigation.
General considerations in laparoscopic surgery
Virtually all laparoscopic surgery is performed under general anesthesia,
although both local and regional anesthesias are feasible for selected procedures. Initial entry into the abdomen may be made blindly with a special needle, or by direct cutdown. Working space within the abdomen is then created
by abdominal insuation with carbon dioxide. This particular gas is used
E-mail address: carol-scott-conner@uiowa.edu
0025-7125/02/$ - see front matter 2002, Elsevier Science (USA). All rights reserved.
PII: S 0 0 2 5 - 7 1 2 5 ( 0 2 ) 0 0 0 8 1 - 0
1402
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
because it is readily soluble in blood (decreasing the risk of gas embolus);
cheap; and noncombustible. Other gasses, such as room air, nitrous oxide,
or helium, are occasionally used. During laparoscopic surgery, carbon dioxide
is absorbed from peritoneal surfaces and excreted by the lungs. To compensate
for this respiratory excretion, the anesthesiologist increases the minute volume. Alternatively, various mechanical devices can be used to elevate the
anterior abdominal wall to increase the working space within the abdomen
without increasing intra-abdominal pressure or producing hypercarbia.
The laparoscope is inserted and additional trocars are placed under direct
vision. Major vascular injuries (most commonly to the distal aorta or right
common iliac artery) have been reported from the initial blind entry. These
injuries are not always immediately recognized, because either the bleeding
is retroperitoneal and hidden, or the blood pools in the pelvis where it is not
immediately visible. Major vascular injuries carry a reported mortality of
15% [6]. Minor vascular injuries, most frequently involving the inferior epigastric artery, are less life-threatening, but are nonetheless responsible for
reoperation, transfusion, or conversion to open laparotomy. Bowel injuries
have a reported incidence of 0.05 to 0.3%; these are easily managed if recognized during laparoscopy, but result in peritonitis and sepsis if missed. Trocar sites, if not securely closed, may be the site of postoperative hernia
formation and small bowel obstruction. Finally, bladder and other visceral
injuries rarely occur [6].
The carbon dioxide pneumoperitoneum causes signicant cardiopulmonary changes during laparoscopy. The increase in intra-abdominal pressure
decreases venous return to the heart and elevates the diaphragm. These
result in an intraoperative increased peak inspiratory pressure, decreased
pulmonary compliance, acidosis, hypercarbia, and decreased cardiac output
and stroke volume with an increase in mean arterial pressure, systemic vascular resistance, and central venous pressure. The latter hemodynamic
changes are exacerbated if positive end-expiratory pressure is used to compensate for some of the pulmonary diculties. These intraoperative changes
are now fairly well characterized; with proper anesthesiology support, most
patients tolerate laparoscopic surgery [7]. Generally, the laparoscopic is
preferred over the open approach for surgery, even in poor-risk patients,
because postoperative pulmonary problems, such as atelectasis, are less
severe after laparoscopic surgery. With new laparoscopic procedures, new
problems may emerge. For example, extensive mediastinal dissection during
laparoscopic esophageal surgery (myotomy, fundoplication) can result in
increased mediastinal pressure that is poorly tolerated in some patients [7].
LC and other hepatobiliary procedures
In the approximately 15 years since the rst LC in humans, it has become the procedure of choice for the surgical management of symptomatic
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
1403
cholelithiasis [810]. Generally four trocars are used, although methods
using a smaller number have been described. The laparoscope is inserted
by an umbilical or periumbilical portal. Operating trocars are placed in the
epigastrium and right subcostal region at the midclavicular line. A fourth
trocar, placed more laterally, is used for retraction. The subhepatic space
is exposed by elevating the gallbladder. A tense or inamed gallbladder can
be decompressed by suctioning out the bile. Dissection begins in the region
of Calots triangle to identify the cystic artery and cystic duct (Fig. 1). It is
important to keep this dissection close to the gallbladder, rather than to dissect along the cystic duct down to the common bile duct, and to maintain outward traction on the gallbladder to maximally expose the structures in
Calots triangle. Most surgeons create an ample window by dissection behind
the gallbladder and only then clip and divide the cystic duct and cystic artery.
This modied top-down technique allows the surgeon to verify that the
visualized tubular ductal structure is denitely the cystic duct by seeing it funnel into the gallbladder, and that the second visualized tubular structure is
denitely the cystic artery by observing how it terminates on the gallbladder.
Cholangiography is feasible and used liberally to verify the anatomy.
The indications for LC are identical to those for open cholecystectomy,
with the exception of suspected gallbladder carcinoma. Cirrhosis of the liver,
pregnancy, morbid obesity, previous surgery to the right upper quadrant,
and a variety of other conditions may complicate, but rarely preclude, laparoscopy. Acute cholecystitis and biliary colic are the most common indications; the decision-making process for acute cholecystitis is shown in Fig. 2.
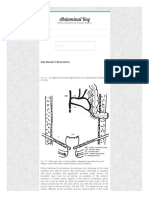
Fig. 1. During laparoscopic cholecystectomy, cephalad traction by one grasper held by an
assistant elevates the liver to expose the subhepatic space. A second grasper is placed lower on
the gallbladder. Outward traction on this second grasper exposes Calots triangle to facilitate
accurate identication of crucial structures. This gure shows an early stage of the dissection:
the peritoneum overlying Calots triangle has been opened and the surgeon is gently dissecting
behind the presumed cystic duct to conrm that this duct terminates in the gallbladder. Note
that the common duct is not visualized clearly, and that no attempt is made to delineate the
cystic-ductcommon-duct junction. (From Scott-Conner CEH. Chassins operative strategy
in general surgery, an expositive atlas. 3rd edition. New York: Springer Verlag; 2002; with
permission.)
1404
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
Fig. 2. Simplied algorithmic approach to the management of patients with acute cholecystitis.
The initial treatment with antibiotics and hydration results in clinical improvement in a
large majority of patients, who may then be considered for early laparoscopic cholecystectomy
(LC), usually during the same hospitalization. If surgery is not performed within that interval,
it should be deferred for 4 to 6 weeks to allow acute inammation to subside. The small
minority of patients who do not improve with antibiotics may undergo either percutaneous
cholecystostomy (PCC) or urgent laparoscopic cholecystectomy. (From Schwesinger WH,
Sirinek KR, Strodel III WE. Laparoscopic cholecystectomy for biliary tract emergencies: state
of the art. World J Surg 1999;23(4):33442; with permission.)
Biliary pancreatitis and common duct stones are discussed briey in the
following section.
Conversion to open cholecystectomy occurs in a small minority of cases
and is not considered a complication, but rather a sign of a prudent surgeon.
In 1992, Scott et al [10] calculated a conversion rate of 4% among 12,397
cases reported in the surgical literature. The most common reason for conversion is acute or chronic inammatory changes that render dissection difcult [10]. Other reasons include bleeding, uncertain anatomy, or injury to
adjacent structures. All patients should be informed of this possibility before
surgery. Most surgeons attempt to do all cholecystectomies by laparoscopy,
rather than try to predict in advance which patients will have too much
inammation or scarring to perform the procedure successfully. LC is an
alternative salvage maneuver when severe acute inammation precludes safe
dissection.
Complications
The primary complication of LC is injury to the extrahepatic biliary system. Anatomic anomalies are common in this region. The magnied view
during laparoscopy improves visualization of small structures, but can contribute to structure misidentication. Two major injuries can occur: transection of the common bile duct, and injury to a right hepatic or sectoral duct
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
1405
[11]. The Belgian Group for Endoscopic Surgery in a retrospective survey
identied 65 bile duct injuries (0.6% rate) among 9959 LCs. The rate for
individual surgeons ranged from 0.35% to 1.3%. The injury was detected
intraoperatively in only 45% of patients; an additional 29% presented after
surgery with bile leakage and diuse biliary ascites. Five (8%) of the patients
died. Biliary strictures recurred in 20 of 60 surviving patients. The group
concluded that routine operative cholangiography improved intraoperative
detection of biliary injury and stressed the need for a low threshold for conversion to open surgery in dicult cases [12]. Others have reported similar
rates of bile duct injury ranging from 0.3% (which is comparable with the
rate for open cholecystectomy) to 3% [10,13,14]. A learning curve eect has
been postulated in that the incidence of these serious complications
decreases with greater experience. In a large series from multiple hospitals
in Connecticut, the incidence of bile duct injuries rose from the baseline rate
of 0.04% with open cholecystectomy in 1989 to 0.24% in 1991 (early LC
experience) but then fell to 0.11% in 1993 (with greater LC experience [8]).
The common bile duct can be misidentied as the cystic duct when the gallbladder is pulled up too vigorously to enhance visualization of the subhepatic
space. The common bile duct is then mistakenly clipped below and transected
above, and a segment of common bile duct ranging from 1 to 2 cm in length is
completely excised (Fig. 3). This mistake causes obstructive jaundice or, more
commonly, leakage of hepatic bile into the abdomen. The latter produces
abdominal distention, nausea, vomiting, and other nonspecic symptoms
with hyperbilirubinemia. The diagnosis may be made by radionuclide scan
and conrmed by endoscopic retrograde cholangiopancreatography
(ERCP). These injuries are dicult to treat surgically because the common
bile duct is almost invariably minute in caliber (hence the mistaken identication) and is missing a signicant segment, and the surgical eld is contaminated because of delayed diagnosis. Repair (biliary-enteric anastomosis)
should only be undertaken by an experienced surgeon. Right hepatic or sectoral duct injury occurs when part of the right hepatic ductal system empties
directly into the cystic duct (or vice versa), close to the gallbladder. As aforementioned, these injuries are associated with signicant morbidity and mortality. All patients should be counseled preoperatively as to the risk of these
complications, and this counseling should be documented in the chart. Biliary
strictures may also result from injudicious clipping or thermal damage. These
strictures may be amenable to dilatation or stenting.
Gallstones often spill into the peritoneum during laparoscopic cholecystectomy. Retained intraperitoneal gallstones may cause postoperative abscesses
because of bacterial colonization. Modern techniques allow for retrieval of
spilled stones and good peritoneal toilet, so that this spillage no longer mandates conversion to an open procedure.
Ductal injury may cause bile leakage. Most commonly, leakage is from
cystic duct injury, caused by improper clip placement or loss of a clip. Most
of these leaks resolve with adequate drainage. ERCP is an integral part of
1406
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
Fig. 3. In this illustration of a common bile duct injury during laparoscopic cholecystectomy,
the surgeon has mistaken the common bile duct for the cystic duct, clipped the common bile
duct proximally and distally, and excised a segment of it during laparoscopy. This mistake
usually results in a Billroth II with Roux-en-Y hepaticojejunostomy for repair. Note the
typically small caliber of the common duct, which contributes to the misidentication. (From
Scott-Conner CEH. Chassins operative strategy in general surgery, an expositive atlas. 3rd
edition. New York: Springer Verlag; 2002; with permission.)
management: it conrms the integrity of the extrahepatic biliary tree, allows
for management of any retained common duct stone, and with sphincterotomy or biliary stent accelerates sealing of the leak by decreasing intrabiliary
pressure.
Laparoscopic common bile duct exploration
Gallstones can lodge in the common bile duct to produce obstructive
jaundice or cholangitis, or pass through this duct to produce biliary pancreatitis. Laparoscopic common bile duct exploration is complementary to
ERCP with sphincterotomy and stone retrieval. Obstructive jaundice and
cholangitis are appropriately managed by ERCP, with LC done later if the
gallbladder has not been removed previously and the patient can tolerate
surgery. The situation with biliary pancreatitis is more complex because generally the stones already have passed through the ampulla of Vater at diagnosis. A generally accepted algorithm for management of biliary pancreatitis
is shown in Fig. 4 [9].
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
1407
Fig. 4. Simplied algorithmic approach to the management of biliary pancreatitis. Patients who
have severe pancreatitis are best served by endoscopic retrograde cholangiopancreatography
(ERCP) followed by laparoscopic cholecystectomy (LC). Those with mild pancreatitis and a
low probability of common bile duct stones (CBDS) may undergo LC with intraoperative
cholangiography. In a signicant percentage of these patients, the stones have already passed. If
stones are detected by intraoperative cholangiography, then laparoscopic transcystic common
duct exploration (LCTE), laparoscopic choledochotomy (LCDE), open common duct
exploration (OE), or postoperative ERCP may be selected depending on local expertise. (From
Schwesinger WH, Sirinek KR, Strodel III WE. Laparoscopic cholecystectomy for biliary tract
emergencies: state of the art. World J Surg 1999;23(4):33442; with permission.)
There are two ways for the laparoscopic surgeon to clear the common
bile duct of stones under uoroscopic guidance. In transcystic exploration,
stone baskets, lithotriptors, or a small-diameter choledochoscope are passed
through the dilated cystic duct. This method is particularly useful for small
stones in a small-diameter duct. Indeed, some small stones can be ushed
out through the ampulla merely by injecting saline into the ductal system.
This method cannot access stones in the proximal ductal system. This is particularly problematic when the cystic duct enters the common bile duct distally. If the duct cannot be cleared of stones, the surgeon may leave a
catheter in place for subsequent percutaneous access, or pass a guidewire
1408
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
through the ampulla into the duodenum as a guide for subsequent endoscopic retrograde sphincterotomy.
Laparoscopic choledochotomy requires facility with laparoscopic suturing techniques. An incision is made into the common bile duct, allowing
both distal and proximal exploration with baskets, balloon catheters, or the
choledochoscope. The incision must be sutured, generally over a T-tube, as
done during open common duct exploration. This method works well for
large common ducts [15].
Laparoscopic liver surgery
Both needle and wedge liver biopsy are accomplished easily laparoscopically, but are rarely needed unless percutaneous image-guided biopsy fails
[16]. Laparoscopic liver resection has been reported, but is uncommonly performed. In contrast, large symptomatic simple hepatic cysts are easily fenestrated laparoscopically (Fig. 5); this laparoscopic procedure carries a 10%
risk of late cyst recurrence, which compares favorably with the 44% risk
of recurrence reported with radiologic therapy [17].
Laparoscopic esophageal surgery
Techniques for laparoscopic exposure and mobilization of the distal
esophagus are well developed. The visualization is superior to that during
conventional open surgery. Two procedures in particular, laparoscopic
esophagomyotomy and laparoscopic Nissen fundoplication, have become
the surgical procedures of choice for achalasia or GERD, respectively
[1820].
Fig. 5. Laparoscopic photograph shows a large simple hepatic cyst in which the gallbladder
forms part of the cyst wall. Laparoscopic fenestration and laparoscopic cholecystectomy were
accomplished easily, with cholangiography to delineate the ductal anatomy.
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
1409
Laparoscopic esophagomyotomy
The Heller esophagomyotomy was originally performed by a thoracotomy incision, and so the rst minimal-access esophagomyotomies were
performed thoracoscopically. Access to the distal esophagus and gastroesophageal junction is, however, best obtained with the laparoscope with
extensive mediastinal dissection and mobilization [18]. This has become
the preferred technique when disease is limited to the lower esophageal
sphincter [18,19,21]. Both pneumatic dilatation and laparoscopic esophagomyotomy eectively relieve dysphagia in achalasia. Esophageal dilatation
was associated with a 14.5% rate of esophageal rupture and a similar rate
of failure to relieve symptoms in one series [19]. Myotomy is accompanied
by a higher incidence of postoperative reux, and some surgeons add a partial fundoplication, such as a Dor [21] or Toupet [18], discussed in the following section. The proton pump inhibitors may mitigate this problem.
Careful preoperative work-up and case selection are critical.
Laparoscopic esophagomyotomy is performed under general anesthesia.
The esophagus is accessed by dividing the phrenoesophageal membrane,
and the distal esophagus is mobilized. Belseys fat pad is divided to expose
completely the gastroesophageal junction. A longitudinal incision is made
along the longitudinal muscle bers and the bers are split until the hypertrophied circular muscle bers are exposed. The circular bers are then divided until the epithelial tube pouts out (Fig. 6). Laparoscopic magnication
and visualization allow this to be done with precision. The myotomy is
extended proximally until reaching normal (nonhypertrophied) circular
Fig. 6. In this illustration of laparoscopic esophagomyotomy, the longitudinal muscle of the
esophagus has been incised and is being spread apart by two graspers. A hook electrocautery is
being used to elevate and divide the hypertrophied circular muscle. (From Scott-Conner CEH.
Chassins operative strategy in general surgery, an expositive atlas. 3rd edition. New York:
Springer Verlag; 2002; with permission.)
1410
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
esophageal muscle, and distally approximately 1 cm into the stomach.
Endoscopic guidance is used to conrm that a patulous sphincter is created
by the procedure. The main complications are perforation, gastroesophageal
reux, and recurrence of symptoms [1822]. Perforations are usually managed easily by laparoscopic suture with a buttress of autologous tissue (usually a Dor fundoplication), when recognized intraoperatively [21].
Laparoscopic fundoplication
The 360-degree Nissen fundoplication is an eective open procedure for
GERD that has been adapted and standardized for laparoscopy [11,20,23
28]. The esophagus is rst mobilized thoroughly by extensive dissection in
the lower mediastinum. Unlike the usual practice during open surgery, the
crura of the diaphragmatic hiatus are then closed with several interrupted
sutures to prevent postoperative herniation [29]. The gastric fundus is fully
mobilized by dividing the short gastric vessels. A short loose wrap is then
constructed by pulling the fundus behind the esophagus and suturing it onto
itself (Fig. 7). A calibrated bougie within the esophagus ensures that the
wrap is not too tight.
Esophageal and gastric perforation can occur. Immediate recognition
and repair, buttressed, when possible, with the wrap avoids serious sequelae.
Unrecognized perforations result in severe sepsis and can be fatal. In a study
of 17 perforations, three mechanisms were identied: (1) improper retroesophageal dissection, (2) passage of a bougie or dilator, and (3) sutures cutting
through the bowel wall during the immediate postoperative period. It is
Fig. 7. Laparoscopic Nissen fundoplication creates a 360-degree wrap of the distal esophagus
with the gastric fundus. The wrap is made oppy and short. (From Peters JH. Laparoscopic
treatment of gastroesophageal reux and hiatal hernia. In: Scott-Conner CEH, editor. The
SAGES manual: fundamentals of laparoscopy and GI endoscopy. New York: Springer Verlag;
1999. p. 196212; with permission.)
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
1411
hoped that these complications will become less common now that the
mechanisms are well understood. Diagnosis was delayed in 6 of the 17
patients, of whom one died [11].
Dysphagia is the primary remaining complication. The incidence varies
from 2% to 14% of patients, with many experiencing transient postoperative
dysphagia that resolves with time. Crural closure, type of wrap, length of
wrap, whether or not the short gastric vessels are divided, and unrecognized
preoperative esophageal motility disorders all aect the risk of dysphagia.
The patient must undergo careful evaluation, including esophageal manometry, before surgery and the surgeon must be knowledgeable and experienced in esophageal physiology [30]. Reoperation is ultimately required in
3% to 4% because of recurrence of reux or development of persistent severe
dysphagia from anatomic errors in wrap construction [23,29]. A short
esophagus must be recognized and corrected. This complicates the laparoscopic fundoplication in approximately 10% of patients. In most of these
cases the esophagus can be mobilized into the abdomen with adequate
mediastinal dissection, but in a substantial minority of cases a surgical
lengthening procedure, such as a Collis gastroplasty, must be performed.
If this shortening is not recognized and corrected, the wrap slips with suboptimal results [31].
Alternative partial fundoplications (Dor or Toupet) have a lower incidence of immediate dysphagia, but the long-term results are not well characterized [25]. The Dor fundoplication pulls up and sutures the anterior fundus
over the anterior surface of the distal esophagus. It is used to advantage after
repair of a mucosal injury during esophagomyotomy; in this case the fundus
buttresses the repair. The Toupet fundoplication (Fig. 8) is constructed in a
manner similar to the Nissen, but the fundus is sutured to the esophagus
rather than to itself. This allows approximately 25% of the esophageal surface to remain outside the wrap. Dividing the short gastric vessels usually
is unnecessary for either partial fundoplication. Experienced esophageal surgeons consistently emphasize the need for thorough preoperative evaluation,
including the identication of any associated motility disorders, and the need
to select the most appropriate repair for the individual patient [24,30].
Repair of paraesophageal hernia
In paraesophageal hernia, the stomach slides up into the chest next to the
esophagus. Gastroesophageal reux often coexists. These hernias are quite
amenable to laparoscopic repair. The stomach is reduced fully into the
abdomen and the hernial sac is excised. The crura of the esophageal hiatus
are then sutured closed with pledgeted sutures. Sometimes, a patch of prosthetic material is needed. Many surgeons add a partial or complete fundoplication, selectively suture the stomach to the diaphragm or anterior
abdominal wall, or place a temporary gastrostomy for decompression and
xation [32].
1412
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
Fig. 8. The Toupet fundoplication is a partial wrap in which the gastric fundus is sutured to the
esophagus rather than to itself, producing a 270-degree wrap and less dysphagia. (From Peters
JH. Laparoscopic treatment of gastroesophageal reux and hiatal hernia. In: Scott-Conner
CEH, editor. The SAGES manual: fundamentals of laparoscopy and GI endoscopy. New York:
Springer Verlag; 1999. p. 196212; with permission.)
Esophageal resection
The esophagus can be resected for benign conditions or carefully selected
cases of esophageal cancer by a combined laparoscopic and thoracoscopic
approach. Most of the dissection is accomplished thoracoscopically through
the right chest, with the distal esophagus mobilized laparoscopically as previously described. This approach is ideal for patients with high-grade dysplasia in Barretts esophagus, and has also been used successfully for
tumor in situ, and T1 or 2 N0 lesions [33].
Laparoscopic gastric surgery
At the time that LC was becoming established, vagotomy was still commonly performed for ulcer disease. Better understanding of the pathophysiology and improved medical therapy have rendered vagotomy far less
common than previously. Nonetheless, both truncal and highly selective
vagotomies were adapted to laparoscopic techniques. A hybrid operation,
posterior truncal vagotomy with anterior seromyotomy, was beginning to
emerge as the best laparoscopic vagotomy, when improvements in medical
therapy rendered most of these procedures obsolete [3436].
Surgery for gastric carcinoma
Gastric carcinoma is fortunately rare in Western countries. In the United
States, laparoscopy is occasionally used for preoperative staging before
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
1413
open resection. Extensive experience from countries where gastric cancer is
prevalent indicates that laparoscopic gastric resection technically is feasible.
Experienced laparoscopic surgeons can achieve surgical margins, number of
lymph node excised, and short-term survival equivalent to that for open gastric resection. As with most laparoscopic resections for cancer, denitive evidence of ecacy in terms of long-term survival is still lacking. Laparoscopic
resection may have an important role, however, because so many resections
performed in the United States for gastric cancer are palliative. A small incision must be made for specimen removal, and the anastomosis can be created through this incision. Totally intracorporeal anastomotic techniques
have been described, but do not seem to oer any advantage, except for total
gastrectomy [37,38].
Gastrostomy
Percutaneous endoscopic gastrostomy is generally the procedure of
choice to achieve enteral feeding in patients who are chronically unable to
be fed orally because of such conditions as stroke or anoxic encephalopathy.
Percutaneous endoscopic gastrostomy may not be technically feasible or
safe when the esophagus is totally obstructed, when the stomach anatomy
is altered, or when the transverse colon is anterior to the stomach. In such
cases, laparoscopic gastrostomy provides an alternative approach. It can be
performed under local anesthesia.
Plication of perforated ulcers
Graham patch plication with a piece of greater omentum provides excellent short-term management for simple anterior perforated duodenal ulcers
(Fig. 9). This may be the sole surgical therapy when the patient with perforation is clinically unstable or has severe local inammation [39]. This procedure is performed easily laparoscopically and may be combined with
thorough peritoneal lavage under direct vision. Suture xation is not absolutely necessary and alternative techniques have been described [40]. Total
hospital stay is frequently the same for laparoscopic repair as for open
repair, because of the sequelae of the accompanying peritonitis, but overall
convalescence is faster [40]. Medical treatment then generally allows the
ulcer to heal. Perforated gastric ulcers require dierent management because
of the frequent association of adenocarcinoma or lymphoma.
Bariatric surgery
Laparoscopic Roux-en-Y gastric bypass has emerged as a safe and eective surgical treatment for morbid obesity. It is an extremely complex and
technically demanding procedure that should be performed only by surgeons
with considerable experience and expertise [41,42]. As with all bariatric procedures, careful patient selection, counseling, and postoperative follow-up
1414
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
Fig. 9. A laparoscopic Graham patch is being performed by suturing omentum over a simple
anterior perforated duodenal ulcer. The patch seal is tested by pouring and pooling saline over
the repair; air instilled into the nasogastric tube should not bubble out. (From Scott-Conner
CEH. Chassins operative strategy in general surgery, an expositive atlas. 3rd edition. New
York: Springer Verlag; 2002; with permission.)
are essential. A simpler procedure, laparoscopic gastric banding, is popular
in Europe, but has not had such good results in the United States [41].
Small intestinal surgery
Small bowel obstruction
Laparoscopic lysis of adhesions is safe and eective in selected patients
with small bowel obstruction who fail to respond to nonoperative management. The procedure is most eective in patients who are not massively distended, and have not had multiple abdominal operations. A prototype
candidate for this surgery is a woman who developed small bowel obstruction many years after hysterectomy (often caused by one or two band-like
adhesions) because these isolated adhesions are divided easily under laparoscopic guidance.
Small bowel resection
Laparoscopic small bowel resection is occasionally used to treat benign
or malignant tumors, to resect a Meckels diverticulum that cannot be managed by diverticulectomy, or to treat Crohns disease. The diseased loop of
small bowel is identied, elevated with nontraumatic graspers or traction
sutures, and segmentally resected together with a portion of mesentery
(Fig. 10). A small incision is made to retrieve the resected specimen and the
anastomosis generally is completed extracorporeally. Intracorporeal techniques are quite feasible technically, but less commonly performed. Laparoscopy for Crohns disease is being adopted cautiously in some medical
centers. The laparoscopic approach cannot be applied to all Crohns patients
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
1415
Fig. 10. A loop of small bowel containing a small tumor is elevated with traction sutures in
preparation for laparoscopic small bowel resection. A small incision is made to move the
resected specimen. (From Schirmer BD. Small bowel resection, enterolysis, and enteroenterostomy. In: Scott-Conner CEH, editor. The SAGES manual: fundamentals of laparoscopy and
GI endoscopy. New York: Springer Verlag; 1999. p. 25466; with permission.)
because of the predilection for skip lesions, the need carefully to evaluate the
thickness of the bowel to determine the extent of resection, and the tendency
for mesenteric thickening [43,44].
Meckels diverticulum
Asymptomatic Meckels diverticula are left alone when incidentally discovered during laparoscopic procedures just as they are during open surgery. A Meckels diverticulum must be resected when it has caused
bleeding or has perforated. If the inammation is limited to the diverticulum
with a normal-appearing base, the diverticulum is simply excised by ring an
endoscopic linear stapling device across the base. Segmental small bowel
resection, including the diverticulum, may be needed if the inammation
or perforation extends beyond the diverticulum into adjacent small bowel.
Laparoscopic appendectomy
Incidental removal of a normal appendix during a laparoscopic gynecologic procedure was rst described by Semm [5]. Technical renements have
1416
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
now made it possible laparoscopically to remove inamed, even gangrenous,
appendices. Laparoscopic appendectomy is performed under general anesthesia. The abdomen is thoroughly explored to exclude other pathology.
The appendix is identied and elevated. Gentle dissection at the base of the
appendix enables the surgeon to create a window between the mesentery and
the base. The mesentery and appendiceal base are then secured and divided
separately using the endoscopic linear cutting stapler, pretied suture ligatures, clips, or other hemostatic devices (Fig. 11). The base is not inverted.
The appendix is placed in a retrieval bag or withdrawn into a trocar. Antibiotic coverage is essential. A period of postoperative ileus commensurate
with the degree of preoperative inammation is to be expected [45,46].
Many surgeons perform laparoscopic appendectomy selectively (eg, when
the diagnosis is equivocal) and other pathology, particularly gynecologic,
must be excluded. Other surgeons use open appendectomy in young, slender
patients and select the laparoscopic approach for obese or muscular
patients. Benets of laparoscopic appendectomy have been dicult to
prove, and cost-eectiveness has been dicult to demonstrate because most
open appendectomies can be performed through relatively small incisions
in the lower abdomen. For most laparoscopic procedures, higher operating room costs are oset by a shorter postoperative stay. For laparoscopic
appendectomy, the postoperative length of stay is dictated more by the
infectious process than by the length of the incision, and this reduces the
potential savings. At least one study has shown a slight decrease in postoperative hospitalization after laparoscopic appendectomy [46]. The additional
logistical diculties of performing emergently a technically demanding procedure after normal working hours with an operating room sta who may
be unfamiliar with the equipment have proved daunting to some surgeons.
The potential advantages in eliminating wound infection and the attendant
prolonged convalescence are welcome, however, particularly in young active
individuals.
Fig. 11. During laparoscopic appendectomy, the endoscopic cutting linear stapler is positioned
across the base of the appendix and then red. The mesentery is then divided by a second
application of the stapler or by clips or other hemostatic devices. (From Scott-Conner CEH.
Chassins operative strategy in general surgery, an expositive atlas. 3rd edition. New York:
Springer Verlag; 2002; with permission.)
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
1417
Colon resection
The length of incision required for open colonic surgery is dictated by the
need adequately to mobilize the colon. Laparoscopic access has the theoretical appeal of providing mobilization without a long incision. Essentially all
colonic surgery that is performed open can be performed laparoscopically,
but many surgeons are cautious about applying laparoscopy to colon cancer. Clearly equivalent surgical margins and adequate lymphadenectomy
can be performed by laparoscopy and the short-term results seem good.
Carcinoma of the colon, however, is one of relatively few malignancies that
are often cured surgically; long-term survival after laparoscopic resection
remains unknown, pending the results of ongoing prospective trials. This
procedure should continue to be evaluated in the context of clinical trials
[4750]. Proctocolectomy, for ulcerative colitis or familial polyposis, is an
example of a procedure in which laparoscopic mobilization, followed by
construction of a small incision to deliver the specimen and construct the
pouch, makes excellent sense.
Laparoscopic pancreatic surgery
Initially, retroperitoneal structures, such as the pancreas, seemed to be
relatively unamenable to laparoscopy. As in other areas, techniques have
evolved that allow the selective application of laparoscopy for surgical management of pancreatic pathology [51,52].
Pancreatic neoplasms
Islet cell tumor enucleation, distal pancreatectomies (both with and without splenectomy), and even pancreaticoduodenectomy have been reported
by laparoscopy [5154]. Laparoscopy is also enthusiastically embraced for
preoperative staging of pancreatic cancer, and for palliative biliary or gastric
bypass when resection is not feasible. Adjunctive use of laparoscopic ultrasound is essential to localize small islet cell tumors for resection. Fig. 12
shows a distal pancreatectomy with splenectomy performed with the endoscopic linear stapling device.
Pancreatitis and pancreatic pseudocysts
Laparoscopic debridement of pancreatic sequestrums associated with
necrotizing pancreatitis has been used and may prove advantageous in
selected cases. Repeat debridement and drainage can be accomplished by
repeat laparoscopy [55]. Both cystgastrostomy and cystjejunostomy are
laparoscopically feasible using the endoscopic cutting linear stapler. Endoscopic or laparoscopic ultrasound assists in cyst localization; an
anastomosis is then constructed in the usual fashion [51].
1418
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
Fig. 12. A 30-mm endoscopic cutting linear stapler is being used to transect the pancreas for
laparoscopic distal pancreatectomy and splenectomy. More than one application of the stapler
is needed. (From Salky BA, Edye M. Laparoscopic pancreatectomy. Surg Clin North Am
1996;76(3):53956; with permission.)
New trends and new procedures
Even when the operating room is set up optimally for laparoscopic surgery, the position of the laparoscopic surgeon remains awkward with
unnatural ergonomics (Fig. 13). To understand the current limitations of
(nonrobotic) laparoscopic surgery, imagine sitting at your desk with your
upper arms clamped rigidly in one position so that all you can do is move
your hands and elbows and that you can rotate, but not bend, your wrists.
Items are frustratingly beyond reach, and many arm movements extremely
dicult or impossible. Then close one eye to correspond with the monocular
view aorded the laparoscopic surgeon, to approximate the limitations of
Fig. 13. Laparoscopic surgery requires the surgeon to operate using long thin instruments that
enter the abdominal cavity through small xed ports. Even with good body mechanics, as
illustrated, fatigue and ergonomic problems are signicant, as well as a lack of binocular vision.
(From Scott-Conner CEH. Chassins operative strategy in general surgery, an expositive atlas.
3rd edition. New York: Springer Verlag; 2002; with permission.)
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
1419
many laparoscopic systems. Minimal-access surgeons anticipate that technologic advances will revolutionize the training of future surgeons to
encourage their performance of complex procedures that are currently performed by only the most experienced laparoscopic surgeons. Whether new
procedures will be invented during this process remains to be determined;
it is hoped that sound physiologic and surgical principles will continue to
govern progress in laparoscopy [5658].
Hand-assisted laparoscopic surgery
Many resective laparoscopies require a small incision at the end of the
procedure to retrieve the resected specimen intact. In hand-assisted laparoscopic surgery, that incision is part of the initial set-up. A special device is
then inserted to enable the surgeon to place the nondominant hand into the
abdomen to retract and facilitate dissection while maintaining pneumoperitoneum. This modication is termed hand-assisted laparoscopy. It improves
control and facilitates retraction during complex procedures. The small incision, typically placed in the lower abdomen, is well-tolerated physiologically
and cosmetically [59].
Endoluminal surgery
Mucosal and submucosal gastric lesions can be resected endoluminally
with laparoscopic techniques under laparoscopic and endoscopic guidance.
An example is a leiomyoma of the posterior gastric wall. Special trocars
are inserted through the abdominal and gastric walls and the stomach is insuated. The laparoscope is passed through a trocar into the stomach
and instruments for the resection are passed through additional trocars
(Fig. 14). At the conclusion of the procedure, the trocars and laparoscope
are withdrawn into the peritoneal cavity and the gastric trocar incisions are
closed under laparoscopic guidance.
Robotic surgery
Robotic surgery provides special challenges and opportunities for the
minimal-access surgeon [60]. The current, commercially available, system
allows the surgeon to operate in a virtual three-dimensional environment,
using fully articulated tools that mimic the motions used during open surgery, allowing full dexterity. The institutional investment is formidable, and
it is currently uncertain how widely such systems will become available.
Summary
In the short time since LC was rst performed in humans, minimal-access
surgical techniques have been applied to the full spectrum of surgical
therapy of gastrointestinal diseases. For many gastrointestinal diseases,
1420
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
Fig. 14. Laparoscopic-guided intraluminal gastric surgery involves placing trocars through the
stomach and the anterior abdominal wall. (From Cuschieri A. Gastric resections. In: ScottConner CEH, editor. The SAGES manual: fundamentals of laparoscopy and GI endoscopy.
New York: Springer Verlag; 1999. p. 23646; with permission.)
laparoscopy seems to oer advantages over traditional open surgery. The
long-term results of laparoscopic surgery for cancer await the results of prospective clinical trials currently underway and caution is urged when laparoscopic curative resection is performed. On the horizon are signicant
improvements in technology that should lead to further applications and
advances in laparoscopic gastrointestinal surgery.
References
[1] Kelling G. Ueber die moglichkeit die zytoskopie bei untersuchungen seroser hohlungen
anzuwenden: Bemerkungzudem artikel von Jacobaeus. Munchen Wochenschr 1910;57:2358.
[2] Kelling G. Ueber oesophagoscopie, gastroskopie, und koelioskopie. Munchen Med
Wochenschr 1902;49:214.
[3] Jacobaeus HC. Ueber die moglichkeit, die zystoskopie bei untersuchung seroser hohlungen
anzuwenden. Munchen Med Wochenschr 1910;57:20902.
[4] Cappell MS, Waye JD, Farrar JT, Sleisenger MH. Fifty landmark discoveries in
gastroenterology during the past 50 years: a brief history of gastroenterology at the
millennium: Part I. Gastrointestinal procedures and upper gastrointestinal disorders.
Gastroenterol Clin North Am 2000;29:22363.
[5] Semm K. Endoscopic appendectomy. Endoscopy 1983;15:5964.
[6] Philips PA, Amaral JF. Abdominal access complications in laparoscopic surgery. J Am
Coll Surg 2001;192:52536.
[7] Hardacre JM, Talamini MA. Pulmonary and hemodynamic changes during laparoscopy
are they important? Surgery 2000;127:2414.
[8] Gadacz TR. Update on laparoscopic cholecystectomy, including a clinical pathway. Surg
Clin North Am 2000;80:112749.
[9] Schwesinger WH, Sirinek KR, Strodel 3rd WE. Laparoscopic cholecystectomy for biliary
tract emergencies: state of the art. World J Surg 1999;23:33442.
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
1421
[10] Scott T, Zucker K, Bailey R. Laparoscopic cholecystectomy: a review of 12,397 patients.
Surg Laparosc Endosc 1992;2:1918.
[11] Schauer PR, Meyer WC, Eubanks S, Norem RF, Franklin M, Pappas TN. Mechanisms of
gastric and esophageal perforations during laparoscopic fundoplication. Ann Surg 1996;223:
4352.
[12] Gigot J-F, Etienne J, Aerts R, et al. The dramatic reality of biliary tract injury during
laparoscopic cholecystectomy. Surg Endosc 1997;11:11718.
[13] McMahon AJ, Fullarton G, Baxter JN, ODwyer PJ. Bile duct injury and bile leakage in
laparoscopic cholecystectomy. Br J Surg 1995;82:30713.
[14] Strasberg S, Hertl M, Soper N. An analysis of the problem of biliary injury during
laparoscopic cholecystectomy. J Am Coll Surg 1995;180:10125.
[15] Memon MA, Hassaballa H, Memon MI. Laparoscopic common bile duct exploration; the
past, the present, and the future. Am J Surg 2000;179:30915.
[16] Bravo AA, Sheth SG, Chopra S. Liver biopsy. N Engl J Med 2001;344:495500.
[17] Cowles RA, Mulholland MW. Solitary hepatic cysts. J Am Coll Surg 2000;191:31121.
[18] Champion JK, Delisle N, Hunt T. Comparison of thoracoscopic and laparoscopic
esophagomyotomy with fundoplication for primary motility disorders. Eur J Cardiothorac
Surg 1999;16(suppl 1):S346.
[19] Anselmino M, Perdikis G, Hinder RA, Polishuk PV, Wilson P, Terry JD, et al. Heller
myotomy is superior to dilatation for the treatment of early achalasia. Arch Surg 1997;
132:23340.
[20] Soper NJ. Laparoscopic management of hiatal hernia and gastroesophageal reux. Curr
Probl Surg 1999;36:765838.
[21] Rosati R, Fumagalli U, Bona S, Bonavina L, Pagani M, Peracchia A. Evaluating results of
laparoscopic surgery for esophageal achalasia. Surg Endosc 1998;12:2703.
[22] Vogt D, Curet M, Pitcher D, Joslo R, Milne RL, Zucker K. Successful treatment of
esophageal achalasia with laparoscopic Heller myotomy and Toupet fundoplication. Am
J Surg 1997;174:70914.
[23] Carlson MA, Frantzides CT. Complications and results of primary minimally invasive
antireux procedures: a review of 10,735 reported cases. J Am Coll Surg 2001;193:42839.
[24] Hunter JG, Trus TL, Branum GD, Waring JP, Wood WC. A physiologic approach to
laparoscopic fundoplication for gastroesophageal reux disease. Ann Surg 1996;223:
67385.
[25] McKernan JB, Champion JK. Minimally invasive antireux surgery. Am J Surg 1998;175:
2716.
[26] Peters JH, DeMeester TR, Crookes P, Oberg S, Shoop MV, Hagen JA, et al. The treatment
of gastroesophageal reux disease with laparoscopic Nissen fundoplication: prospective
evaluation of 100 patients with typical symptoms. Ann Surg 1998;228:4050.
[27] Spiess AE, Kahrilas PJ. Treating achalasia: from whalebone to laparoscope. JAMA 1998;
280:63842.
[28] Watson DI, Jamieson GG. Antireux surgery in the laparoscopic era. Br J Surg 1998;85:
117384.
[29] Wills VL, Hunt DR. Dysphagia after antireux surgery. Br J Surg 2001;88:48699.
[30] Hogan WJ, Shaker R. Life after antireux surgery. Am J Med 2000;108(suppl 4a):181S91S.
[31] Horvath KD, Swanstrom LL, Jobe BA. The short esophagus: pathophysiology, incidence,
presentation, and treatment in the era of laparoscopic antireux surgery. Ann Surg 2000;232:
63040.
[32] Edye MB, Canin-Endres J, Gattorno F, Salky BA. Durability of laparoscopic repair of
paraesophageal hernia. Ann Surg 1998;228:52835.
[33] Nguyen NT, Schauer PR, Luketich JD. Combined laparoscopic and thoracoscopic
approach to esophagectomy. J Am Coll Surg 1999;188:32832.
[34] Cuschieri A. Laparoscopic vagotomy. Gimmick or reality?. Surg Clin North Am 1992;72:
35767.
1422
C.E.H. Scott-Conner / Med Clin N Am 86 (2002) 14011422
[35] Dallemagne B, Weerts JM, Jehaes C, Markiewicz S, Lombard R. Laparoscopic highly
selective vagotomy. Br J Surg 1994;81:5546.
[36] Poon R, Chow L, Lim B, Gertsch P. Thorascopic vagotomy for recurrent ulcer after
previous gastric operation. Aust N Z J Surg 1997;67:17780.
[37] Goh PM, Khan AZ, So JB, Lomanto D, Cheah WK, Muthiah R, et al. Early experience
with laparoscopic radical gastrectomy for advanced gastric cancer. Surg Laparosc Endosc
Percutan Tech 2001;11:837.
[38] Goh PM, So JB. Role of laparoscopy in the management of stomach cancer. Semin Surg
Oncol 1999;16:3216.
[39] Jordan Jr PH, Morrow C. Perforated peptic ulcer. Surg Clin North Am 1988;68:31529.
[40] Lau W-Y, Leung K-L, Kwong K-H, et al. A randomized study comparing laparoscopic
versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg
1996;224:1318.
[41] DeMaria EJ. Laparoscopic adjustable silicone gastric banding. Surg Clin North Am 2001;
81:112944.
[42] Schauer PR, Ikramuddin S. Laparoscopic surgery for morbid obesity. Surg Clin North Am
2001;81:114579.
[43] Aleali M, Milson JW. Laparoscopic surgery in Crohns disease. Surg Clin North Am
2001;81:21730.
[44] Delaney CP, Fazio VW. Crohns disease of the small bowel. Surg Clin North Am 2001;81:
13758.
[45] Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology 2000;215:33748.
[46] Macarulla E, Vallet J, Abad JM, et al. Laparoscopic versus open appendectomy: a prospective randomized trial. Surg Laparosc Endosc 1997;7:3359.
[47] Greene FL. Laparoscopic management of colorectal cancer. CA Cancer J Clin 1999;49:
199201.
[48] Maxwell-Armstrong CA, Robinson MH, Scholeeld JH. Laparoscopic colorectal cancer
surgery. Am J Surg 2000;179:5007.
[49] Oliver GC. Colorectal surgery. J Am Coll Surg 1999;188:1117.
[50] Stage JG, Schulze P, Overgaard H, et al. Prospective randomized study of laparoscopic
versus open colonic resection for adenocarcinoma. Br J Surg 1997;84:3916.
[51] Park A, Schwartz R, Tandan V, Anvari M. Laparoscopic pancreatic surgery. Am J Surg
1999;177:15863.
[52] Pertsemlidis D, Edye M. Diagnostic and interventional laparoscopy and intraoperative
ultrasonography in the management of pancreatic disease. Surg Clin North Am 2001;
81:36377.
[53] Pisters PW, Lee JE, Vauthey JN, Charnsangavej C, Evans DB. Laparoscopy in the staging
of pancreatic cancer. Br J Surg 2001;88:32537.
[54] Raeburn CD, McIntyre Jr RC. Laparoscopic approach to adrenal and endocrine
pancreatic tumors. Surg Clin North Am 2000;80:142741.
[55] Alverdy J, Vargish T, Desai T, Frawley B, Rosen B. Laparoscopic intracavitary debridement of peripancreatic necrosis: preliminary report and description of the technique.
Surgery 2000;127:1124.
[56] Link RE, Schulam PG, Kavoussi LR. Telesurgery: remote monitoring and assistance
during laparoscopy. Urol Clin North Am 2001;28:17788.
[57] Newman RM, Traverso LW. Cost-eective minimally invasive surgery: what procedures
make sense? World J Surg 1999;23:41521.
[58] Young-Fadok TM, Smith CD, Sarr MG. Laparoscopic minimal-access surgery. Where are
we now? Where are we going?. Gastroenterology 2000;118(2 suppl 1):S14865.
[59] Romanelli JR, Kelly JJ, Litwin DEM. Hand-assisted laparoscopic surgery in the United
States: an overview. Semin Laparosc Surg 2001;8:96103.
[60] Lomanto D, Cheah WK, So JB, Goh PM. Robotically assisted laparoscopic cholecystectomy: a pilot study. Arch Surg 2001;136:11068.
Anda mungkin juga menyukai
- Safe CholecystectomyDokumen60 halamanSafe CholecystectomyCarlos Reyes100% (1)
- Subtotal Cholecystectomy-''Fenestrating'' Vs ''Reconstituting'' Subtypes and The Prevention of Bile Duct Injury - Definition of The Optimal Procedure In  Difficult Operative ConditionsDokumen8 halamanSubtotal Cholecystectomy-''Fenestrating'' Vs ''Reconstituting'' Subtypes and The Prevention of Bile Duct Injury - Definition of The Optimal Procedure In  Difficult Operative ConditionsBolivar Isea100% (1)
- Percutaneous Surgery of the Upper Urinary Tract: Handbook of EndourologyDari EverandPercutaneous Surgery of the Upper Urinary Tract: Handbook of EndourologyPetrisor Aurelian GeavletePenilaian: 5 dari 5 bintang5/5 (1)
- Diagnostic Laparoscopy in Penetrating Abdominal TraumaDokumen4 halamanDiagnostic Laparoscopy in Penetrating Abdominal TraumaNicolás Joel Peñalosa CupajitaBelum ada peringkat
- Types Sites and Causes of Mechanical Intestinal ObDokumen5 halamanTypes Sites and Causes of Mechanical Intestinal ObPutra FebdianBelum ada peringkat
- Atlas of Surgery Cameron Volume II. 2ndDokumen5 halamanAtlas of Surgery Cameron Volume II. 2ndAlberto Ramírez100% (1)
- Reoperative Antireflux Surgery For Failed Fundoplication: An Analysis of Outcomes in 275 PatientsDokumen8 halamanReoperative Antireflux Surgery For Failed Fundoplication: An Analysis of Outcomes in 275 PatientsDiego Andres VasquezBelum ada peringkat
- Ambulatory Anorectal SurgeryDokumen234 halamanAmbulatory Anorectal SurgeryHermina DicuBelum ada peringkat
- Abdominalkey Com Hartmanns ResectionDokumen5 halamanAbdominalkey Com Hartmanns ResectionAnonymous RFVIG7IaBelum ada peringkat
- Resources For Optimal Care of Emergency SurgeryDokumen155 halamanResources For Optimal Care of Emergency SurgeryKevin QuinterosBelum ada peringkat
- A.Valeri Et Al - Surgery of The Adrenal Gland - 2013Dokumen200 halamanA.Valeri Et Al - Surgery of The Adrenal Gland - 2013Sergiu FedoretBelum ada peringkat
- Atlas of Surgery Cameron Volume II. 2ndDokumen6 halamanAtlas of Surgery Cameron Volume II. 2ndAlberto RamírezBelum ada peringkat
- Atlas of Surgical Techniques For Colon, Rectum and AnusDokumen414 halamanAtlas of Surgical Techniques For Colon, Rectum and AnusjenniferjebamaniBelum ada peringkat
- SurgeryDokumen135 halamanSurgeryAndi AlfianBelum ada peringkat
- Immediate Complications Following Thoracic SurgeryDokumen17 halamanImmediate Complications Following Thoracic SurgeryPopa TiberiuBelum ada peringkat
- Surgery For Recurrent Soft Tissue SarcomaDokumen584 halamanSurgery For Recurrent Soft Tissue SarcomaAr-pardo RogerBelum ada peringkat
- ComponentsDokumen5 halamanComponentsprakashmathewBelum ada peringkat
- Vdoc - Pub Anesthesia and Perioperative Care For Aortic SurgeryDokumen454 halamanVdoc - Pub Anesthesia and Perioperative Care For Aortic SurgerySavoBelum ada peringkat
- All You Need To Know About Vascular SurgeryDokumen33 halamanAll You Need To Know About Vascular SurgeryDr. Vinicius MajdalaniBelum ada peringkat
- Non Cardiac OpDokumen21 halamanNon Cardiac Opc4ri5Belum ada peringkat
- Beck, David E. - Kann, Brian R. - Margolin, David A. - Vargas, H. David - Whitlow, Charles B - Improving Outcomes in Colon and Rectal Surgery (2019, CRC Press - Taylor & Francis Group)Dokumen441 halamanBeck, David E. - Kann, Brian R. - Margolin, David A. - Vargas, H. David - Whitlow, Charles B - Improving Outcomes in Colon and Rectal Surgery (2019, CRC Press - Taylor & Francis Group)Daniel StaniloaieBelum ada peringkat
- Transhiatal EsophagectomyDokumen12 halamanTranshiatal EsophagectomyprofarmahBelum ada peringkat
- Preparing Severely Jaundiced Patient For SurgeryDokumen2 halamanPreparing Severely Jaundiced Patient For Surgerylentini@maltanet.netBelum ada peringkat
- Perioperative Management of Patients Receiving Anticoagulants - UpToDateDokumen65 halamanPerioperative Management of Patients Receiving Anticoagulants - UpToDatejames lxBelum ada peringkat
- Diagnosis, Treatment and Follow-Up in Extracranial Carotid Stenosis, 2020Dokumen16 halamanDiagnosis, Treatment and Follow-Up in Extracranial Carotid Stenosis, 2020CAMILO ARMANDO BENAVIDES BURBANOBelum ada peringkat
- Appendiceal Cancer: - 1% of Appendectomies Contain CancerDokumen28 halamanAppendiceal Cancer: - 1% of Appendectomies Contain CancerRajendra SoniBelum ada peringkat
- ABDOMINOPERINEAL RESECTION SURGERYDokumen19 halamanABDOMINOPERINEAL RESECTION SURGERYJohnson Mallibago100% (2)
- Endoscopic SurgeryDokumen152 halamanEndoscopic SurgeryiciBelum ada peringkat
- Difficult Decisons in CCR 2023Dokumen654 halamanDifficult Decisons in CCR 2023flavia_craBelum ada peringkat
- Practice Guidelines For Juniors 01 June 2016Dokumen3 halamanPractice Guidelines For Juniors 01 June 2016ElaineBelum ada peringkat
- Oral Boards 2Dokumen67 halamanOral Boards 2Steven GodelmanBelum ada peringkat
- Patient Rounding Format in SICU/CTICUDokumen4 halamanPatient Rounding Format in SICU/CTICUseigfried13Belum ada peringkat
- Laparoscopic Hepatectomy Atlas and TechniquesDokumen327 halamanLaparoscopic Hepatectomy Atlas and TechniquesArassika100% (1)
- Neoadjuvant Chemoradiotherapy Followed by Surgery VersusDokumen15 halamanNeoadjuvant Chemoradiotherapy Followed by Surgery VersusRaul Matute MartinBelum ada peringkat
- Principles of Laparoscopic & Robotic Surgery: Aaquila Sherin Bismi J J Blessy OommanDokumen46 halamanPrinciples of Laparoscopic & Robotic Surgery: Aaquila Sherin Bismi J J Blessy OommanAsif AbbasBelum ada peringkat
- Anorectal Surgery PDFDokumen33 halamanAnorectal Surgery PDFLuminitaDumitriuBelum ada peringkat
- Acute Care Surgery in Geriatric Patients.2023Dokumen603 halamanAcute Care Surgery in Geriatric Patients.2023Cirugía General HGRBelum ada peringkat
- New Approaches For The Treatment of Varicose Veins: Theodore H. Teruya, MD, FACS, Jeffrey L. Ballard, MD, FACSDokumen21 halamanNew Approaches For The Treatment of Varicose Veins: Theodore H. Teruya, MD, FACS, Jeffrey L. Ballard, MD, FACSArturo Javier FuentesBelum ada peringkat
- Initial Management of Trauma in Adults - UpToDateDokumen37 halamanInitial Management of Trauma in Adults - UpToDateAlberto Kenyo Riofrio PalaciosBelum ada peringkat
- Flail Chest.Dokumen3 halamanFlail Chest.Irfan ThamrinBelum ada peringkat
- ABSITE CH 25 ThoracicDokumen11 halamanABSITE CH 25 ThoracicJames JosephBelum ada peringkat
- Abdominal Surgery All in OneDokumen50 halamanAbdominal Surgery All in OneAnne ChoyBelum ada peringkat
- Abdominal Organ Transplantation: State of the ArtDari EverandAbdominal Organ Transplantation: State of the ArtNizam MamodeBelum ada peringkat
- A Short Guide To Preparing For The Fellowship Examination: Australian Board in General SurgeryDokumen9 halamanA Short Guide To Preparing For The Fellowship Examination: Australian Board in General SurgeryDronacharya RouthBelum ada peringkat
- Basic Surgical Techniques PDFDokumen111 halamanBasic Surgical Techniques PDFBoţu AlexandruBelum ada peringkat
- Notes, 1/e: Surgical Incisions, Needle and Suture MaterialsDokumen7 halamanNotes, 1/e: Surgical Incisions, Needle and Suture MaterialsvkBelum ada peringkat
- Radiofrequency AblationDokumen6 halamanRadiofrequency Ablationraviks34Belum ada peringkat
- Management of Anastomotic Complications of Colorectal SurgeryDokumen13 halamanManagement of Anastomotic Complications of Colorectal Surgerydadupipa100% (1)
- Hand Sewn GI AnastomosisDokumen7 halamanHand Sewn GI AnastomosisAmmoResearchBelum ada peringkat
- CME - An Algorithmic Approach to Reconstructing Acquired Scalp DefectsDokumen19 halamanCME - An Algorithmic Approach to Reconstructing Acquired Scalp DefectsGleny SumBelum ada peringkat
- Conservative Management of Perforated Peptic UlcerDokumen4 halamanConservative Management of Perforated Peptic UlcerAfiani JannahBelum ada peringkat
- Cardiothoracic Surgery Pocket MentorDokumen34 halamanCardiothoracic Surgery Pocket MentorGaetano Di Giovanni100% (1)
- Dokumen - Pub - Operative Techniques in Thoracic and Esophageal Surgery 1st Edition 9781496318954Dokumen557 halamanDokumen - Pub - Operative Techniques in Thoracic and Esophageal Surgery 1st Edition 9781496318954adel husseinBelum ada peringkat
- Oxford Surgery 2018Dokumen14 halamanOxford Surgery 2018Debby rahmadiniBelum ada peringkat
- C 1+ 2 Surgicl Pathology of OesophagusDokumen91 halamanC 1+ 2 Surgicl Pathology of OesophagusSayuridark5Belum ada peringkat
- Walter Siquini (Eds.) - Total, Subtotal and Proximal Gastrectomy in Cancer - A Color Atlas-Springer-Verlag Mailand (2015)Dokumen222 halamanWalter Siquini (Eds.) - Total, Subtotal and Proximal Gastrectomy in Cancer - A Color Atlas-Springer-Verlag Mailand (2015)Andrea PicoBelum ada peringkat
- Penetrating TraumaDokumen606 halamanPenetrating TraumaMajdEddeinAlmustafaBelum ada peringkat
- Ashcraft - Pediatric SurgeryDokumen1.092 halamanAshcraft - Pediatric SurgeryRoxana Boloaga100% (1)
- Gillenwater - Adult and Pediatric Urology 4th EdDokumen1.564 halamanGillenwater - Adult and Pediatric Urology 4th EdRoxana Boloaga100% (1)
- Pablo Neruda - The Captain's VersesDokumen158 halamanPablo Neruda - The Captain's VersesDaniel Mestiz100% (1)
- Pablo Neruda 2000Dokumen71 halamanPablo Neruda 2000Aganooru Venkateswarulu100% (1)
- Arensman - Pediatric SurgeryDokumen486 halamanArensman - Pediatric Surgeryedrons0% (1)
- Lobe - Pediatric Laparoscopy (Landes Bioscience Vademecum)Dokumen276 halamanLobe - Pediatric Laparoscopy (Landes Bioscience Vademecum)Roxana BoloagaBelum ada peringkat
- Perioperative Nursing Care PhasesDokumen5 halamanPerioperative Nursing Care PhasesanjieBelum ada peringkat
- KNH 413 Case Study 4Dokumen12 halamanKNH 413 Case Study 4api-272540385100% (1)
- PT of The Shoulder PDFDokumen573 halamanPT of The Shoulder PDFMuhammad Salman AzimBelum ada peringkat
- Impaired Gas ExchangeDokumen10 halamanImpaired Gas ExchangeWardinatul ImanBelum ada peringkat
- Psychology Presentation Chapter 10 - Life Span DevelopmentDokumen15 halamanPsychology Presentation Chapter 10 - Life Span DevelopmentEduardo VillanuevaBelum ada peringkat
- Canine Parvovirus ExplainedDokumen2 halamanCanine Parvovirus ExplainedReading_EagleBelum ada peringkat
- The Benefits of ExerciseDokumen3 halamanThe Benefits of ExerciseAtet KurniadiBelum ada peringkat
- Family Nursing Care Plan: (A Case Study of Paglingayen Family)Dokumen9 halamanFamily Nursing Care Plan: (A Case Study of Paglingayen Family)Adrian MallarBelum ada peringkat
- Intro To Pharmacology Study GuideDokumen93 halamanIntro To Pharmacology Study GuideMichelle Morgan LongstrethBelum ada peringkat
- Case #2: Group CDokumen27 halamanCase #2: Group CKartik SharmaBelum ada peringkat
- ParacetamolDokumen1 halamanParacetamolcen janber cabrillos100% (1)
- Plumbing Questionnaire 2Dokumen51 halamanPlumbing Questionnaire 2mcpayod100% (1)
- Antioxidant Micronutrient Impact On Hearing Disorders: Concept, Rationale, and EvidenceDokumen7 halamanAntioxidant Micronutrient Impact On Hearing Disorders: Concept, Rationale, and EvidenceFongmeicha Elizabeth MargarethaBelum ada peringkat
- Anesthesia and Myasthenia Gravis2012Dokumen22 halamanAnesthesia and Myasthenia Gravis2012Alisher AgzamovBelum ada peringkat
- Diet With Beans - Lose 5-7 Kilograms in 5 Days! - Shakahari TipsDokumen7 halamanDiet With Beans - Lose 5-7 Kilograms in 5 Days! - Shakahari TipsHemant VinayakBelum ada peringkat
- Twin Force® Bite Corrector Device Comparison With ForsusDokumen2 halamanTwin Force® Bite Corrector Device Comparison With ForsusOrtho OrganizersBelum ada peringkat
- How To Boost Your Immune System - Harvard HealthDokumen6 halamanHow To Boost Your Immune System - Harvard HealthAnonymous 0qsjVfQtLBelum ada peringkat
- 1 A Randomized Clinical Trial of Manual Therapy For Cervico Brachial Pain Syndrome A Pilot StudyDokumen8 halaman1 A Randomized Clinical Trial of Manual Therapy For Cervico Brachial Pain Syndrome A Pilot StudyCassie RodriguezBelum ada peringkat
- Social Stories™ For Children With Autism: A Review of The LiteratureDokumen27 halamanSocial Stories™ For Children With Autism: A Review of The LiteratureHusna YussofBelum ada peringkat
- Colonic InertiaDokumen20 halamanColonic InertiaAndina Destiyani PutriBelum ada peringkat
- MMPI-2 Validity ScalesDokumen7 halamanMMPI-2 Validity ScalesEspíritu Ciudadano50% (2)
- Family Systems Theory ExplainedDokumen10 halamanFamily Systems Theory ExplainedHoney Bitas OriasBelum ada peringkat
- Journal Article Explains Scope of Self-Efficacy TheoryDokumen15 halamanJournal Article Explains Scope of Self-Efficacy TheoryBangtan HearteuBelum ada peringkat
- What's The Childbearing Age?: Woman's Reproductive Years Are Between Ages andDokumen4 halamanWhat's The Childbearing Age?: Woman's Reproductive Years Are Between Ages andJeffrey MagadaBelum ada peringkat
- Ocular Trauma: State of Illinois Trauma Nurse Specialist ProgramDokumen38 halamanOcular Trauma: State of Illinois Trauma Nurse Specialist ProgramMayuha SaidBelum ada peringkat
- Peritoneal Dialysis Sao PauloDokumen8 halamanPeritoneal Dialysis Sao PauloRemberto RamosBelum ada peringkat
- Ohi Graphic OrganizerDokumen1 halamanOhi Graphic Organizerapi-278298083Belum ada peringkat
- Casestudy Pott's DiseaseDokumen36 halamanCasestudy Pott's DiseaseyasiraBelum ada peringkat
- FAQ Updated Must Read For Apple Therapy-9Dokumen23 halamanFAQ Updated Must Read For Apple Therapy-9dpparkheBelum ada peringkat
- Health & Nutrition Classification of FoodDokumen10 halamanHealth & Nutrition Classification of Foodg20kpBelum ada peringkat