Frequently Asked Questions in Composite Restorative Dentistry PDF
Diunggah oleh
David ColonJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Frequently Asked Questions in Composite Restorative Dentistry PDF
Diunggah oleh
David ColonHak Cipta:
Format Tersedia
See
discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/51841324
Frequently asked questions in composite
restorative dentistry
Article in Dental update October 2011
Source: PubMed
CITATIONS
READS
884
5 authors, including:
Robert J Mcconnell
Joseph Sabbagh
Queen's University Belfast
Lebanese University-School of dentistry
48 PUBLICATIONS 799 CITATIONS
14 PUBLICATIONS 253 CITATIONS
SEE PROFILE
SEE PROFILE
Jose C De la Macorra
Complutense University of Madrid
67 PUBLICATIONS 443 CITATIONS
SEE PROFILE
All in-text references underlined in blue are linked to publications on ResearchGate,
letting you access and read them immediately.
Available from: Jose C De la Macorra
Retrieved on: 24 September 2016
RestorativeDentistry
Robert J McConnell
Joseph Sabbagh, Jose C de la Macorra, Arne Lund and Mike Cassidy
Frequently Asked Questions in
Composite Restorative Dentistry
Abstract: With an increasing number of dental practitioners using composite resins as the restorative material of choice, knowledge of
terminology, handling properties and restorative techniques are important.
Clinical Relevance: This paper addresses many of the questions raised by participants at lectures and courses given by the authors across
Europe.
Dent Update 2011; 38: 549556
In a world where success is linked to
aesthetics, there is a growing demand from
our patients for white restorations.
Continuing education
programmes in aesthetic dentistry are in
demand as dental practitioners recognize
that, in order to achieve optimum
aesthetics and long-lasting restorations,
they must have a thorough knowledge of
the materials properties and develop new
clinical skills.
Dental manufacturers regularly
introduce new materials requiring new
techniques and applications, such as selfetch adhesives, self-etch resin cements
and self-etching composites. Practitioners
may find it difficult to stay up-to-date
with these new materials and their
terminology and, as a result, have
difficulties in achieving the best results
from the material for their patients.
Meanwhile, recent graduates are more
competent in using composite resin
materials for the restoration of posterior
teeth.1
This article addresses some
of the questions asked by participants at
continuing education courses presented
by the authors using a question and
answer format.
Bonding
Figure 1. Using suction tip to remove excess
water.
adhesives. If the tooth is over-dried, the
primer in the fourth generation systems can
re-wet it.2,3
Q1. What is wet bonding?
Robert J McConnell, Emeritus Professor
of Restorative Dentistry, University Dental
School and Hospital, Wilton, Cork, Ireland,
Joseph Sabbagh, Assistant Professor,
Department of Conservative and
Aesthetic Dentistry, Lebanese University,
Beirut-Lebanon, Jose C de la Macorra,
Professor of Restorative Dentistry, School
of Dentistry, Complutense University,
of Madrid, Spain, Arne Lund, Private
Practice, Bergen, Norway and Mike
Cassidy, Jersey General Hospital, St
Helier, Jersey Channel Islands, JE1 3QS,
UK.
October 2011
A. Wet bonding is a technique used to
enhance the bond strength of a totaletch adhesive system to dentine. By wet
bonding, the etched dentine surface
is kept moist to prevent the exposed
collagen fibres from collapsing so that
adhesive monomers can easily infiltrate
the network within the demineralized
dentine, forming a well defined hybrid
layer and enhancing bond strength.
Fourth generation adhesive systems are
more forgiving products and require
fewer precautions regarding the wetting
degree compared to self-etching
Q2. How wet should the surface be?
A. The ideal dentine surface for bonding
with a total-etch adhesive system should
be a moist glistening surface with no visible
pooling of water. This can be achieved
by a technique called blot drying. Rinse
the etchant from the tooth surface, then
saturate a cotton pellet with water and
remove any excess water from the pellet by
blotting it on a gauze pad. Use the pellet to
moisten the tooth surface.
Other techniques for obtaining
a moist dentine surface include applying a
brief burst of air (23 seconds) with an air
DentalUpdate 549
RestorativeDentistry
syringe after rinsing the etchant. If using
this technique, ensure that the air syringe
is free from any oil traces or, alternatively,
apply a surgical suction tip on to the cavity
for 2 seconds to remove excess water
(Figure 1).
Wet bonding is not applicable to
self-etch adhesive systems.4
Q3. Explain tooth conditioner, tooth primer
and bonding resin?
A. Tooth conditioner is a name used for
the etchant and was coined in an era
when dentists were worried about using
phosphoric acid on dentine. The most
common etchant is a 37% aqueous solution
of phosphoric acid. The function of an
etchant is to create a clean rough surface
for bonding, removing the smear layer
and demineralized dentine/enamel so
that a primer can effectively hybridize the
dentine/enamel (to form a hybrid layer)
and penetrate collagen fibrils and dentinal
tubules (forming resin tags), resulting in
enhanced bond strength.
Tooth primers are surface
bifunctional active compounds, which
promote adhesion to the hydrophilic
dentine and the hydrophobic monomers.
They can be considered as coupling
agents to link the hydrophilic dentine
surface to hydrophobic bonding resin/
composite resins. They often contain HEMA
(hydroxyethylmethacrylate) and acidic
monomers.
Bonding resins are generally
a blend of methacrylate monomers, to
provide better curing and support for the
primer so that it can more effectively seal
the opened dentinal tubules and therefore
resist the shrinkage of composite resin.
In the more recent adhesive
systems, one or more of the above may be
combined in the same bottle.
Figure 2. Position of light curing unit to obtain
maximum polymerization of the resin.
hybridize the demineralized dentine.
A powerful light-curing
device must be used to ensure complete
polymerization of the resin and thus
avoid leakage towards the pulp (Figure 2).
Microleakage causes pulpal inflammation
and post-operative sensitivity.5,6,7
Q5. What are 7th/8th generation bonding
systems?
A. These are relatively new bonding
systems, often referred to as self-etch
adhesives, where the etchant, the primer
and the bonding agent are incorporated
into the same solution and are applied at
Adhesive
System
Steps
Generation
4th
Etch and Rinse
or Total Etch
the same time or together. The products
may be presented all in a single bottle, or
separately in two bottles, and mixed prior to
their application (Table 1).
The suggested advantage
of these products is that the adhesive
will penetrate and demineralize to the
same depth as the etching, resulting in
a fully supported hybrid layer. Further,
the dentinal tubules are never left
fully opened, so there is less chance of
microleakage and post-operative sensitivity.
This bonding technique tends to be less
technique sensitive, as the challenging
steps of etching, washing and drying are
eliminated.8
Q6. Can the 7th/8th generation bonding
system be used in all clinical techniques?
A. A number of the currently available
systems should not be used with chemically
or dual cured composites. The acidity of the
etching/bonding component will inhibit the
amine effect and thus the polymerization of
the chemically cured composite.
Further, the adhesive should
only be applied to one cavity followed by
the restoration, rather than applying it to a
number of cavities at one time. This is based
Smear Layer
Removal
Complete
2
5th
Q4. Is it safe to etch dentine?
A. It is safe to etch superficial and deep
dentine. It has been shown by many studies
that that the etchant itself does not damage
the pulp or lead to pulp inflammation.
However, this technique is based on a
complete seal of the previously etched
dentine. It is imperative that, following the
etching of dentine and the removal of the
smear layer, a primer and/or an adhesive is
applied on top to seal the open tubules and
550 DentalUpdate
Partial
7th
8th
ClearFil SE Bond (Kuraray)
OptiBond Solo Plus SE (Kerr)
Adper Prompt-LPop (3M ESPE)
AdheSE (Vivadent)
Xenon IV (Dentsply)
Self-etch
1
OptiBond FL (Kerr)
Scotch Bond Multi-Purpose
(3M-ESPE)
Syntac (Vivadent)
AllBond 2 (Bisco)
Optibond Solo (Kerr)
Single Bond 2 (3M ESPE)
Prime & Bond NT (Dentsply)
6th
2
Examples
Partial
Optibond All-in-one (Kerr)
Stae (SDI)
Xenon V (Dentsply)
Table 1. Classification of the different adhesive systems available.
October 2011
RestorativeDentistry
Composite
Company
# Shades
Detail
Amelogen
Charisma
Solitaire II
Filtek Z-250
Esthet-X
Filtek-Supreme XT
Gradia
Point-4
Premise
Vitalessence
Ultradent
Heraeus Kulzer
Heraeus Kulzer
3M ESPE
Dentsply
3M ESPE
GC
KerrHawe
KerrHawe
Ultradent
19
16
10
15
31
30
22
30
32
33
3 Opacities
4 Opacities
3 Opacities
4 Opacities
3 Opacities
3 Opacities
Figure 3. Placement of a flowable composite on
floor of cavity.
Table 2. Examples of previous and recent composites systems.
Point-4
(Kerr)
Premise
(Kerr)
Filtek-Suprem XT
(3M ESPE)
Gradia
(GC)
Opaque = 8
Dentine = 8
Dentine = 10
Opaque = 3
Body = 16
Enamel = 18
Body = 14
Body = 13
Translucent = 3
Translucent = 4
Enamel = 7
Translucent = 6
Extra-Light = 3
Translucent = 4
Table 3. Modern composite systems, with different opacities, used for layering technique.
on the fact that this category of adhesive
contains very hydrophilic monomers, and
may attract water up the tubules which
could compromise the polymerization of
the resin.9
of the polished surfaces compared to
microhybrid composite systems.13,14,15
Q7. What is the best bonding system?
A. No, the modern hybrid composite
resins are suitable for all types of basic
restorations.
A. The 3-step (etching-primingbonding) system or 4th generation (2
Step) adhesive system are still the gold
standards, demonstrating the best clinical
performance and the highest bond strength
to enamel and dentine.3,10,11, 12
Therefore, etch and bond should
be used when retention of the restoration
is poor. Self-etch should be used when
retention is not an issue.
Composite
Q8. What are nano-filled composite resins?
A. These are resin restoratives which have
been manufactured using a percentage
of extremely small particles. At this stage
there is no evidence that they have any
advantages over the traditional hybrid type
resins. Recent studies have shown that
nanocomposites have superior retention
October 2011
Q9. Do I need to purchase different types
of composites for anterior and posterior
restorations?
Q10. Should I get all the available shades of a
composite system?
A. Modern kits of composites contain
different levels of opacity; opaque or
dentine, body or enamel, and translucent or
incisal. The purchase of two opaque shades
(eg OA2, OA3.5), four body shades (eg
A1, A2, A3, A3,5) and a translucent shade
should be adequate for the majority of
clinical cases. (Tables 2 and 3).
Note that for elderly patients
you may need dark shades and for bleached
teeth, very white opaque resins.
flowable composites with differing
percentage of fillers and thus be suitable
for different clinical situations. Ideally, a
flowable composite for use in a cavity
should be easy to apply to the cavity wall
and should not flow beyond the margins
(Figure 3)16,17
Q12. Should a base of flowable composite be
placed prior to the placement of the stiffer
restorative hybrid material?
A. It is more difficult for a packable
composite to wet the adhesive surface,
often resulting in voids or imperfections at
the adhesive-composite interface. Although
evidence is not clear yet, it has been shown
that a flowable composite can improve the
wetting between a stiff composite and the
adhesive. It is also speculated that using a
flowable composite first may also minimize
the damage that a stiff composite, especially
the packable composite, may inflict on
poorly cured adhesive. The adaptation
of the first layer of composite may be
improved if a flowable is used and may
enhance the bond strength and ensure a
void free interface. Polymerization shrinkage
strain can range from 1.7 to 3.1% in modern
packable composite resins and from 3.5 to
6.3% in flowable composites. If a flowable
composite is used, it should be remembered
that it has a lower modulus of elasticity
and that it should be applied in a very thin
layer to avoid the effects of its excessive
polymerization shrinkage.13,18,19,20
Q13. Should composites and bonding systems
be stored in the fridge?
Q11. Are all flowable composites similar?
A. No, there are different viscosities
of flowable composites. The same
manufacturer can produce different
A. No, it is not mandatory to store resins in
the fridge, provided ambient temperatures
are not extreme. It is critical that resins are
not used beyond their shelf life marked on
DentalUpdate 551
RestorativeDentistry
a
the box. Old materials are very useful for
constructing mock-ups and temporaries for
anterior or posterior restorations.
The temperature of the material
will affect its viscosity, thus in a cold state
the material will be stiffer.
Some bonding systems require
refrigeration owing to their more acidic
nature and solvent volatility.
Q14. Do compomers have a role as a
restorative material?
Figure 5. Class II cavity with composite initially
being placed against one wall of the box.
A. Compomers have excellent aesthetics
in Class V restorations and, in theory,
may release some fluoride. The amount
of fluoride released by a compomer is
usually about 1/10 of that released from
a conventional glass ionomer or a resinmodified glass ionomer system.
There would appear to be no
advantage in using a compomer over a
composite resin.
Figure 4. Use of Tofflemire (a) and sectional matrix
systems (b).
Q. 15. Should you line the cavity before the
placement of a resin composite restorative
material?
Otherwise, a circular Tofflemire
matrix system can be used (Figure 4)24,25,26
A. Composite resins are the best materials
we have to seal a cavity. This is based on
bonding to both enamel and dentine.
The presence of a lining compromises this
bond. If a lining is to be used, it should
only be used if there is a direct or indirect
pulp exposure. Calcium hydroxide should
then be placed over the exposure and,
because of its poor initial mechanical
properties, protected by covering it
with a small amount of glass ionomer or
flowable resin.5,21,22,23 MTA (Mineral Trioxide
Aggregate), and Biodentine (bioactive
cement) from Septodont, can also be used
for direct pulp capping.
Q16. What is the best matrix band to use for
posterior composites?
A. A metal or celluloid matrix is suitable.
Choice is based on gaining a close fit in
the cervical area, gaining access through
the contact point and achieving a good
interproximal contact. Ideally, a sectional
matrix is used if the proximal size of the
cavity is not too wide and the matrix is
supported buccally and lingually. A metallic
separator or ring is added to enhance the
contact point and compensate the matrix
thickness.
552 DentalUpdate
Q17. Does a reflective wedge give a better
composite restoration as compared to a
wooden wedge?
A. Some studies have demonstrated
that there is no difference in clinical
performance between celluloid matrix/
reflective wedge technique and metal
matrix/wooden wedge technique. Reflective
wedges were introduced when we thought
composite cured towards the light; this is
not so.
Pre-wedging during preparation
with a wooden wedge will help to achieve
a tight interproximal contact. Pre-wedging
is useful when there is a very tight contact
which might not allow the operator to
insert a matrix band.25,26,27
Q18. What is the best technique for filling
the box of a Class II posterior composite
restoration?
A. It is crucial to fill the cavity in small
increments and to cure each layer
completely. There are many techniques
for incremental filling of the cavity, but
the sequence is important. (a) Fill the
cervical 1mm first and cure. Use a longer
curing time than recommended as light is
Figure 6. Small increments of resin are placed on
each wall and cured to minimize polymerization
shrinkage.
attenuated when we cure from the top.
(b) Next fill one side of the box (buccal or
lingual) and cure. Initially, do not link the
two walls of the cavity with composite
resin (Figure 5). (c) Finally, fill and cure
the other side of the box. This technique
will allow the composite to cure initially
towards the wall and minimize internal
stresses within the box.
Following placement in
the box, the occlusal component of
the cavity is then filled. Remember,
Class I cavities tend to have higher
unfavourable C factors, resulting in
a higher incidence of post-operative
sensitivity. Therefore, they should be
filled in small increments (Figure 6). The
same applies to Class V cavities.27,28
Q19. Are special composite instruments
needed for the placement of resins?
A. Yes, modern composite resin
instruments have a non-stick surface,
which makes the placement of the resin
easier. If a composite continues to stick
to the instrument, it may be appropriate
to change the composite system itself.
October 2011
RestorativeDentistry
Q20. What is the difference between layering
and incremental fill?
A. Incremental filling is a technique where
multiple small increments of composite
are applied and then light cured between
each increment. This technique is used to
minimize the polymerization shrinkage of
the composite that causes stress within the
restoration (C-factor). Ideally, avoid placing
increments attached to both buccal and
lingual walls simultaneously, as this results
in higher stress on the bonded surfaces
and/or within the material.
Layering is the technique where
a dentine shade of composite is applied to
the deeper layers and a shade of enamel is
placed on top. This technique can be used
for anterior and posterior restorations.
Dentine shades are more
opaque, while enamel shades tend to be
more translucent. The surface enamel
layer should be placed in thin sections for
maximum aesthetics.29
Q21. Why do some composites change colour
over time?
A. Chemically cured and dual-cured resins
contain amines, which will result in colour
change over time.
For light-cured resin composites,
the most likely cause of colour change is
insufficient curing. Each increment should
be cured for 30 seconds and cured again
following finishing. The intensity of the
curing light should be checked regularly
with a radiometer to make sure it has
adequate output (minimum intensity 600
mW/cm2). The halogen bulb should be
replaced after 100 hours of use, annually, or
whenever the light intensity is too low. The
end of the light guide should be cleaned
regularly.
Distance from the curing resin
and the shade of composite are important
factors in achieving the maximum cure
of the system, and should be kept to a
minimum. There is no risk in over-curing a
composite.30
Q22. What type of curing light is best?
A. The halogen light is excellent and
continues to be a good choice.
LED (Light-Emitting Diode)
lights are now available and will eventually
replace the halogen model. Most are
October 2011
very quickly, revealing any pre-existing
surface defects. You can avoid a sticky
composite resin surface (air inhibited layer)
by placing a water soluble gel on the tooth
and curing the final layer through the gel.
The gel can then be rinsed away.
Figure 7. Presence of white lines.
cordless and they give an excellent level of
light intensity at the desired wavelength
with little heat production.
The depth of cure relates to
the output intensity of the light, not to
the emitting system. Generally, LED units
have a narrow band width (around 470 nm)
and therefore may not cure adequately
some resin composites containing photoinitiators that react at different wavelengths.
This problem may be encountered with
some clear or bleached shades that do not
contain camphoroquinone.
Plasma curing units are usually
high intensity lights, which can cure a
composite in a few seconds. However, this
may have a deleterious effect on the bond
to the tooth as a result of a high rate of
shrinkage stress development.31,32,33,34
Q23. How can you avoid the white lines on the
margin of the restoration that may occur after
finishing procedure?
A. White lines may result from the dust
of the composite that fills the existing
microgaps over the edges of the restoration
if the composite is not well adapted to the
walls of the tooth (Figure 7). Alternatively,
the white lines may result from cracking of
the enamel surrounding the restoration.
This may be caused by unsupported enamel
or too much composite being cured at
any one time. Good bonding technique,
composite application and attention to the
various stages of finishing the restoration
will eliminate these lines. It is important to
run the polishing system (disks, cups) from
the restoration towards the tooth.
Q25. Does preheating the composite filling
material improve its properties?
A. There is evidence that preheating a resin
restorative material improves its ability to
adapt to the cavity margins, with a resultant
reduction in microleakage, and an increase
in surface hardness.35,36
Conclusions
The basis of this article is to
address questions frequently raised by
dentists on continuing education courses.
With the increased use of composite
resin restoratives, it is imperative that
manufacturers and the profession work
closely together to achieve the highest
clinical outcomes.
We have only addressed a
limited number of questions and provided
some answers and recommendations which
may help dentists in their daily practice.
The placement of composite restorations
is more technique-sensitive than amalgam
placement. However, excellent longterm restorations can be achieved when
the operator understands the physical
properties of the material.
References
1.
2.
3.
Q24. Does a layer of unfilled resin help on the
surface of the resin following polishing?
A. A layer of unfilled or slightly filled resin
may help to fill voids on the surface, giving
a shiny finish. However, it does not replace
the finishing process and will be worn away
4.
Lynch CD, McConnell RJ, Wilson NH.
Trends in the placement of posterior
composites in dental schools. J Dent
Educ 2007; 71: 430434.
Manso AP, Marquezini L Jr, Silva SM,
Pashley DH, Tay FR, Carvalho RM.
Stability of wet versus dry bonding
with different solvent-based adhesives.
Dent Mater 2008; 24: 476482.
Peumans M, Kanumilli P, De Munck J,
Van Landuyt K, Lambrechts P, Van
Meerbeek B. Clinical effectiveness of
contemporary adhesives: a systematic
review of current clinical trials. Dent
Mater 2005; 21: 864881.
Nakaoki Y, Nikaido T, Burrow MF,
Tagami J. Effect of residual water on
dentin bond strength and hybridization
DentalUpdate 555
RestorativeDentistry
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
of a one-bottle adhesive system. Oper
Dent 2002; 27: 563568.
Medina VO, Shinkai K, Shirono M,
Tanaka N, Katoh Y. Histopathologic
study of pulp response to singlebottle and self-etching adhesive
systems. Oper Dent 2002; 27: 330
342.
Cox CF, Kim KM, Stevenson RG III,
Hafez AA. Histological evaluation of a
self-priming etchant adhesive system.
Compend Contin Educ Dent 2003; 24(8
Suppl); 1720.
Nayyar S, Tewari S, Arora B.
Comparison of human pulp response
to total-etch and self-etch bonding
agents. Oral Surg Oral Med Oral Pathol
Radiol Endod 2007; 104: 4552.
van Dijken JW, SunnegardhGronberg K, Sorensson E. Clinical
bonding of a single-step self-etching
adhesive in non-carious cervical
lesions. J Adhes Dent 2007; 9: 241
243.
Tay FR, Pashley DH, Suh BI, Hiraishi N,
Yiu CK. Water treeing in simplified
dentine adhesives djvu. Oper
Dent 2005; 30: 561579.
De Munck J, Shirai K, Yoshida Y,
Inoue S, Van Landuyt K, Lambrechts P,
Suzuki K, Shintani H, Van Meerbeek B.
Effect of water storage on the
bonding effectiveness of 6 adhesives
to Class I cavity dentin. Oper Dent
2006; 31: 456465.
Hikita K, Van Meerbeek B,
De Munck J, Ikeda T, Van landuyt K,
Maida T, Lambrechts P, Peumans M.
Bonding effectiveness of adhesive
luting agents to enamel and dentin.
Dent Mater 2006; 23: 7180.
Marques de Melo R, Galhano G,
Barbosa SH, Valandro LF, Pananelli
CA, Bottino MA. Effect of adhesive
system type and tooth region on the
bond strength to dentin. J Adhes Dent
2008; 10: 127133.
Douglas T. Direct applications of a
nanocomposite resin system, part 2.
Pract Periodont Aesthet Dent 2004b;
16(9): 677684.
Beun S, Glorieux T, Devaux J et
al. Characterization of nanofilled
compared to universal and
microfilled composites. Dent Mater
2007; 23: 5159.
Rodrigues SA, Scherrer S, Ferracane J
et al. Microstructural characterization
and fracture behavior of a
556 DentalUpdate
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
microhybrid and a nanofill
composite. Dent Mater 2008; 24:
12811288.
Palaniappan S, Bharadwaj D,
Mattar DL, Peumans M, Van
Meerbeek B, Lambrechts P. Threeyear randomized clinical trial to
evaluate the clinical performance
and wear of a nanocomposite
versus a hybrid composite. Dent
Mater 2009; 25: 13021314.
Endo T, Finger WL, Kanehira M,
Utterodt A, Masashi Komatsu M.
Surface texture and roughness of
polished nanofill and nanohybrid
resin composites. Dent Mater 2010;
26: 213223.
Sabbagh J, Ryelandt L, Bachrius
L et al. Characterization of
the inorganic fraction of resin
composites. J Oral Rehab 2004; 31:
10901101.
Lee IB, Son HH, Um CM. Rheologic
properties of flowable, conventional
hybrid, and condensable composite
resins. Dent Mater 2003; 19: 298
307.
Versluis A, Douglas WH, Cross M,
Sakaguchi RL. Does an incremental
filling technique reduce
polymerisation shrinkage stresses?
J Dent Res 1996; 75: 871878.
Baroudi K, Saleh AM, Silikas N,
Watts DC. Shrinkage behaviour of
flowable resin-composites related
to conversion and filler-fraction.
J Dent 2007; 35: 651655.
Ruiz JL, Mitra S. Using cavity liners
with direct posterior composite
restorations. Compend Contin Educ
Dent 2006; 27: 347351.
Silva GA, Lanza LD, Lopes-Junior N,
Moreira A, Alves JB. Direct pulp
capping with a dentin bonding
system in human teeth: a clinical
and histological evaluation. Oper
Dent 2006; 31: 297307.
Koliniotou-Koumpia E,
Papadimitriou S, Tziafas D. Pulp
responses after application of
current adhesive systems to deep
cavities. Clin Oral Investig 2007; 11:
313320.
Loomans B. Comparison of proximal
contacts of Class II resin composite
restorations in vitro. Oper Dent 2006;
31: 688693.
Cenci MS, Lund RG, Pereira CL,
de Carvalho RM, Demarco FF. In
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
vivo and in vitro evaluation of Class
II composite resin restorations with
different matrix systems. J Adhes Dent
2006; 8: 127132.
Demarco FF, Cenci MS, Lima FG,
Donassollo TA, Andre Dde A,
Leida FL. Class II composite
restorations with metallic and
translucent matrices: 2-year follow-up
findings. J Dent 2007; 35: 231237.
Davidson CL, de Gee AJ, Feilzer A. The
competition between the compositedentin bond strength and the
polymerization contraction stress.
J Dent Res 1984; 63: 13961399.
Feilzer AJ, de Gee AJ, Davidson CL.
Setting stress in composite resin
in relation to configuration of the
restoration. J Dent Res 1987; 66: 1636
1639.
He Z, Shimada Y, Sadr A, Ikeda M,
Tagami J. The effects of cavity size
and filling method on the bonding to
Class 1 cavities. J Adhes Dent 2008; 10:
447453.
Gaintantzopoulou M, Kakaboura A,
Vougiouklakis G. Colour stability of
tooth-coloured restorative materials.
Eur J Prosthodont Restor Dent 2005; 13:
5156.
Thome T, Steagall W Jr, Tachibano A,
Braga SR, Turbino ML. Influence of the
distance of the curing light source
and composite shade on hardness of
two composites. J Appl Oral Sci 2007;
15: 486491.
OReilly M, Ray NJ, McConnell RJ,
Hannigan A. Surface microhardness
of a nanofilled resin composite: a
comparison of a tungsten halogen
and a light-emitting diode light
curing unit, in vitro. Eur J Prosthodont
Restor Dent 2007; 15: 146152.
Rode KM, Kawano Y, Turbino ML.
Evaluation of curing light distance on
resin composite microhardness and
polymerization. Oper Dent 2007; 32:
571578.
Munoz CA, Bond PR, Sy-Munoz J,
Tan D, Peterson J. Effect of preheating on depth of cure and surface
hardness of light-polymerized resin
composites. Am J Dent 2008; 21: 215
222.
Wagner WC, Aksu MN, Neme AM,
Linger JB, Pink FE, Walker S. Effect
of pre-heating resin composite on
restoration microleakage. Oper Dent
2008; 33: 7278.
October 2011
Anda mungkin juga menyukai
- Frequently Asked Questions on Composite Restorative DentistryDokumen6 halamanFrequently Asked Questions on Composite Restorative DentistryRose Sky100% (1)
- Operative Dentistry: Dental AdhesionDokumen12 halamanOperative Dentistry: Dental AdhesionJohn CenaBelum ada peringkat
- Dentin/enamel Adhesives: Review of The LiteratureDokumen0 halamanDentin/enamel Adhesives: Review of The LiteratureparnedBelum ada peringkat
- FAQs Composite RestorationsDokumen7 halamanFAQs Composite RestorationsMugi100% (1)
- Lec 7 BondingDokumen8 halamanLec 7 BondingAbdur RehmanBelum ada peringkat
- Self Etch or Total EtchDokumen3 halamanSelf Etch or Total EtchKarlina KrishnaBelum ada peringkat
- Universal Adhesives: The Next Evolution in Adhesive Dentistry?Dokumen13 halamanUniversal Adhesives: The Next Evolution in Adhesive Dentistry?kartika tiaraBelum ada peringkat
- Anoverviewofdental Adhesivesystemsandthe Dynamictooth-Adhesive InterfaceDokumen19 halamanAnoverviewofdental Adhesivesystemsandthe Dynamictooth-Adhesive Interfacegerson fabian arangoBelum ada peringkat
- Concepts of Enamel and Dentin AdhesionDokumen12 halamanConcepts of Enamel and Dentin Adhesionizeldien5870Belum ada peringkat
- Dentine Bonding Agents Complete ClassificationDokumen4 halamanDentine Bonding Agents Complete ClassificationRadu LavraniucBelum ada peringkat
- Adhesive Dentsitry Understanding The ScienceDokumen11 halamanAdhesive Dentsitry Understanding The ScienceFatima AliBelum ada peringkat
- Adhesive Systems in Restorative DentistryDokumen6 halamanAdhesive Systems in Restorative DentistryStoian SimonaBelum ada peringkat
- An Overview of Dental Adhesive Systems and The Dynamic Tooth-Adhesive InterfaceDokumen19 halamanAn Overview of Dental Adhesive Systems and The Dynamic Tooth-Adhesive InterfaceLynda M. NaranjoBelum ada peringkat
- Artículo 2Dokumen10 halamanArtículo 2jhon valdiviezoBelum ada peringkat
- Nagar Kar 2019Dokumen11 halamanNagar Kar 2019Jessi RecaldeBelum ada peringkat
- Enamel Bonding Has Been Routinely and Successfully Used in Dentistry For About Thirty YearsDokumen17 halamanEnamel Bonding Has Been Routinely and Successfully Used in Dentistry For About Thirty YearsAdina Ioana BordianuBelum ada peringkat
- Dental AdhesivesDokumen8 halamanDental AdhesivesYuttapol Pimpison0% (1)
- New Adhesives and Bonding Techniques. Why and When?: Nicola ScottiDokumen12 halamanNew Adhesives and Bonding Techniques. Why and When?: Nicola ScottiDr. Naji ArandiBelum ada peringkat
- Marginal Microleakage of Composite Resin Restorations Bonded by Desensitizing One Step Self Etch AdhesiveDokumen10 halamanMarginal Microleakage of Composite Resin Restorations Bonded by Desensitizing One Step Self Etch AdhesivenisaBelum ada peringkat
- Old Wine in New Bottle PDFDokumen12 halamanOld Wine in New Bottle PDFMariaBelum ada peringkat
- Pit Fissure REV PDFDokumen9 halamanPit Fissure REV PDFYunita StyaningrumBelum ada peringkat
- DBA DcnaDokumen25 halamanDBA DcnaRuchi ShahBelum ada peringkat
- 1 Adhesives2022 23LectureNotesMaterials HighlightedDokumen12 halaman1 Adhesives2022 23LectureNotesMaterials HighlightedRana hasanaBelum ada peringkat
- Bonding of Universal Adhesives To Dentine - Old Wine in New Bottles?Dokumen13 halamanBonding of Universal Adhesives To Dentine - Old Wine in New Bottles?Learning ClubBelum ada peringkat
- Australian Dental Journal: Current Aspects On Bonding Effectiveness and Stability in Adhesive DentistryDokumen14 halamanAustralian Dental Journal: Current Aspects On Bonding Effectiveness and Stability in Adhesive DentistryGhita HAFFOUBelum ada peringkat
- New Developments in Dental AdhesionDokumen25 halamanNew Developments in Dental AdhesionJoshua ValdezBelum ada peringkat
- Influence of Operator Experience On in Vitro Bond Strength of Dentin AdhesivesDokumen5 halamanInfluence of Operator Experience On in Vitro Bond Strength of Dentin AdhesivesdanielaBelum ada peringkat
- Total Etch Vs Self Etch Adhesives PDFDokumen3 halamanTotal Etch Vs Self Etch Adhesives PDFAfia IzzaBelum ada peringkat
- TMP CE5 CDokumen8 halamanTMP CE5 CFrontiersBelum ada peringkat
- Self-Etch Vs Etch-And - RinseDokumen16 halamanSelf-Etch Vs Etch-And - RinseKarla AlanisBelum ada peringkat
- State of Art Van MeerbeekDokumen12 halamanState of Art Van MeerbeekAkarantayr CurtisBelum ada peringkat
- The Current State of Adhesive DentistryDokumen9 halamanThe Current State of Adhesive DentistrymishBelum ada peringkat
- Dental Economics - Resin-Modified Glass Ionomer vs. Flowable As A Liner or Base EprintDokumen3 halamanDental Economics - Resin-Modified Glass Ionomer vs. Flowable As A Liner or Base EprintNaji Z. ArandiBelum ada peringkat
- Adhesivos UniversalesDokumen9 halamanAdhesivos Universalesmaria posadaBelum ada peringkat
- Effect of Double-Application or The Application of A Hydrophobic Layer For Improved Efficacy of One-Step Self-Etch Systems in Enamel and DentinDokumen7 halamanEffect of Double-Application or The Application of A Hydrophobic Layer For Improved Efficacy of One-Step Self-Etch Systems in Enamel and Dentindr.gonzalezcalvinoBelum ada peringkat
- Effect of Resin Coating and Chlorhexidine On Microleakage of Two Resin Cements After StorageDokumen10 halamanEffect of Resin Coating and Chlorhexidine On Microleakage of Two Resin Cements After StorageHisham HameedBelum ada peringkat
- Adhesion in Restorative Dentistry 2016Dokumen41 halamanAdhesion in Restorative Dentistry 2016mishBelum ada peringkat
- Effects of Dentine Moisture On The Permeability ofDokumen9 halamanEffects of Dentine Moisture On The Permeability ofsarahBelum ada peringkat
- Effect LutingDokumen8 halamanEffect LutingCristina Androne MihăescuBelum ada peringkat
- Muñoz2013 - Immediate Bonding Properties of Universal Adhesives To DentineDokumen9 halamanMuñoz2013 - Immediate Bonding Properties of Universal Adhesives To DentineJosé Ramón CuetoBelum ada peringkat
- Adhesion in Restorative DentistryDokumen16 halamanAdhesion in Restorative DentistryIrene MartinezBelum ada peringkat
- Evolution of Dentin Bonding Agents: AbstractDokumen11 halamanEvolution of Dentin Bonding Agents: AbstractSamuel YeohBelum ada peringkat
- Japanese Dental Science Review: Jorge PerdigãoDokumen8 halamanJapanese Dental Science Review: Jorge PerdigãoJAIR DIEGO VIDAURRE QUISPEBelum ada peringkat
- Total Etch Vs Self EtchDokumen5 halamanTotal Etch Vs Self EtchMaulia Sanaz SeptiariBelum ada peringkat
- Smear Layer-Deproteinization: Improving The Adhesion of Self-Etch Adhesive Systems To Caries-Affected DentinDokumen9 halamanSmear Layer-Deproteinization: Improving The Adhesion of Self-Etch Adhesive Systems To Caries-Affected DentinlucianoBelum ada peringkat
- Enamel Acid Etching - A ReviewDokumen8 halamanEnamel Acid Etching - A ReviewSiddharth NairBelum ada peringkat
- Provisional RestorationsDokumen9 halamanProvisional RestorationsMukhtar AndrabiBelum ada peringkat
- Articulo 5Dokumen9 halamanArticulo 5SofiaBelum ada peringkat
- 1 s2.0 S0109564122001968 MainDokumen13 halaman1 s2.0 S0109564122001968 Maindr.camelia.marisBelum ada peringkat
- Bond Strength of Newer Dentin Bonding Agents in Different Clinical SituationsDokumen8 halamanBond Strength of Newer Dentin Bonding Agents in Different Clinical Situationsmuhammadalfian8Belum ada peringkat
- Enamel DamageDokumen11 halamanEnamel DamagenomanBelum ada peringkat
- Denture AdhesiveDokumen11 halamanDenture AdhesiveAmniAzmiBelum ada peringkat
- Journal 1Dokumen3 halamanJournal 1JeevithaBelum ada peringkat
- Effect of Double-Layer Application On Dentin Bond Durability of One-Step Self-Etch AdhesivesDokumen11 halamanEffect of Double-Layer Application On Dentin Bond Durability of One-Step Self-Etch Adhesivesmarli meridaBelum ada peringkat
- Five-Year Clinical Evaluation of 300 Teeth Restored With Porcelain Laminate Veneers Using Total-Etch and A Modified Self-Etch Adhesive SystemDokumen8 halamanFive-Year Clinical Evaluation of 300 Teeth Restored With Porcelain Laminate Veneers Using Total-Etch and A Modified Self-Etch Adhesive SystemEric Arnold dos Santos BritoBelum ada peringkat
- Dentsplay AdhesivesDokumen16 halamanDentsplay AdhesivesAdina Ioana BordianuBelum ada peringkat
- Outline 9, Principles of AdhesionDokumen9 halamanOutline 9, Principles of AdhesionJustDen09Belum ada peringkat
- Enamel Acid Etching - A ReviewDokumen8 halamanEnamel Acid Etching - A ReviewAmee PatelBelum ada peringkat
- Changing Concepts in Cariology: Forty Years OnDokumen7 halamanChanging Concepts in Cariology: Forty Years OnDavid ColonBelum ada peringkat
- Bio EmulationDokumen13 halamanBio EmulationFabio WenoBelum ada peringkat
- Protective Effect of Chicken Egg Shell Powder Solution (CESP) On Artificially Induced Dental Erosion: An in Vitro Atomic Force Microscope StudyDokumen7 halamanProtective Effect of Chicken Egg Shell Powder Solution (CESP) On Artificially Induced Dental Erosion: An in Vitro Atomic Force Microscope StudyDavid ColonBelum ada peringkat
- Rubber Dam Isolation Techniques for Difficult Clinical Situations in Endodontic TreatmentDokumen8 halamanRubber Dam Isolation Techniques for Difficult Clinical Situations in Endodontic TreatmentDavid ColonBelum ada peringkat
- When Does A Patient Need A "Functional Analysis" of Their Dental Occlusion?Dokumen3 halamanWhen Does A Patient Need A "Functional Analysis" of Their Dental Occlusion?David ColonBelum ada peringkat
- Occlusion TextbookDokumen45 halamanOcclusion Textbookوا إسلاماه100% (1)
- Restoration of The Worn DentitionDokumen11 halamanRestoration of The Worn DentitionDavid ColonBelum ada peringkat
- Occlusion: 2. Occlusal Splints, Analysis and Adjustment: Dental Update November 2003Dokumen7 halamanOcclusion: 2. Occlusal Splints, Analysis and Adjustment: Dental Update November 2003Mostafa HassanBelum ada peringkat
- Clinical Approach To Anterior Adhesive RestorationDokumen25 halamanClinical Approach To Anterior Adhesive RestorationDavid ColonBelum ada peringkat
- Chapter 11 Occlusal Adjustment PDFDokumen8 halamanChapter 11 Occlusal Adjustment PDFDavid ColonBelum ada peringkat
- JIndianSocPedodPrevDent353229-4602923 124709Dokumen9 halamanJIndianSocPedodPrevDent353229-4602923 124709David ColonBelum ada peringkat
- Diagnostic Wax Up Instructions BWDokumen5 halamanDiagnostic Wax Up Instructions BWKatalin RungBelum ada peringkat
- Altering Occlusal Vertical Dimension in FunctionalDokumen8 halamanAltering Occlusal Vertical Dimension in FunctionalDavid ColonBelum ada peringkat
- Tscan Clinical EbookDokumen46 halamanTscan Clinical EbookRotariu Ana MariaBelum ada peringkat
- A OcclusionDokumen112 halamanA OcclusionSaowalak Koosriteppratan100% (1)
- JIntOralHealth104176-8185891 224418Dokumen4 halamanJIntOralHealth104176-8185891 224418David ColonBelum ada peringkat
- Cario I EnglezaDokumen8 halamanCario I EnglezaRazvanAngheleBelum ada peringkat
- Protective Effect of Chicken Egg Shell Powder SoluDokumen8 halamanProtective Effect of Chicken Egg Shell Powder SoluDavid ColonBelum ada peringkat
- A Novel Dentin Bonding System Containing Poly Methacrylic Acid Grafted Nanoclay Synthesis, Characterization and PropertiesDokumen10 halamanA Novel Dentin Bonding System Containing Poly Methacrylic Acid Grafted Nanoclay Synthesis, Characterization and PropertiesDavid ColonBelum ada peringkat
- 750-59 Nanohybrid vs. Fine PDFDokumen10 halaman750-59 Nanohybrid vs. Fine PDFDavid ColonBelum ada peringkat
- Comparative Evaluation of Remineralizing Potential of Three Pediatric DentifricesDokumen6 halamanComparative Evaluation of Remineralizing Potential of Three Pediatric DentifricesDavid ColonBelum ada peringkat
- Kerstein Speaker PacketDokumen8 halamanKerstein Speaker PacketDavid ColonBelum ada peringkat
- 24 - Nanovative Dentistry PDFDokumen3 halaman24 - Nanovative Dentistry PDFDavid ColonBelum ada peringkat
- 2013 Nanorobots PDFDokumen5 halaman2013 Nanorobots PDFDavid ColonBelum ada peringkat
- Dentinal HypersensitivityDokumen11 halamanDentinal HypersensitivityAmira KaddouBelum ada peringkat
- Occurrence and Causing Stimuli of Postoperative Sensitivity in Composite Restorations PDFDokumen8 halamanOccurrence and Causing Stimuli of Postoperative Sensitivity in Composite Restorations PDFDavid ColonBelum ada peringkat
- Barodontalgia As A Differential Diagnosis PDFDokumen4 halamanBarodontalgia As A Differential Diagnosis PDFDavid ColonBelum ada peringkat
- Book CritiqueDokumen4 halamanBook CritiqueDavid ColonBelum ada peringkat
- Case StudyDokumen57 halamanCase StudyShivanand Pegu100% (6)
- Phimosis and ParaphimosisDokumen3 halamanPhimosis and ParaphimosisJoshua PowersBelum ada peringkat
- Strong Letter of Recommendation for Radiology ResidencyDokumen1 halamanStrong Letter of Recommendation for Radiology Residencydrsanjeev15Belum ada peringkat
- "Combining Medical Excellence With Luxury Travel": Marketing Strategies of Medical TourismDokumen18 halaman"Combining Medical Excellence With Luxury Travel": Marketing Strategies of Medical TourismRajesh SainiBelum ada peringkat
- FrenectomiaDokumen8 halamanFrenectomiaRafa LopezBelum ada peringkat
- E W C O F: Arly Ound ARE IN PEN RacturesDokumen3 halamanE W C O F: Arly Ound ARE IN PEN RacturesMatheis Laskar PelangiBelum ada peringkat
- NMAT Perceptual Acuity Module 3 WojrkehjDokumen4 halamanNMAT Perceptual Acuity Module 3 Wojrkehjlorrainebarandon100% (2)
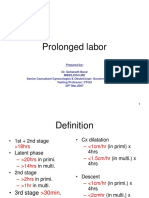
- Prolonged Labor Diagnosis and ManagementDokumen8 halamanProlonged Labor Diagnosis and ManagementMadhu Sudhan PandeyaBelum ada peringkat
- Guide To Skilled Migration To Australia ++ Phil - Uplaw - BookDokumen7 halamanGuide To Skilled Migration To Australia ++ Phil - Uplaw - BookShierwin ManabatBelum ada peringkat
- SterilizationDokumen6 halamanSterilizationMaria Ella Joanne DapitonBelum ada peringkat
- Excerpt: "Birth Matters" by Ina May GaskinDokumen16 halamanExcerpt: "Birth Matters" by Ina May Gaskinwamu885100% (1)
- External Review of London Emergency Dept.Dokumen11 halamanExternal Review of London Emergency Dept.The London Free PressBelum ada peringkat
- Cancer 2019 PDFDokumen652 halamanCancer 2019 PDFWahyu Maulana100% (1)
- Apollo Hospital ReportDokumen16 halamanApollo Hospital ReportTarun AroraBelum ada peringkat
- Compound Palmar Ganglion Cross FluctuationDokumen19 halamanCompound Palmar Ganglion Cross Fluctuationchinmayghaisas100% (3)
- Schedule of Charges-Holy Family - Sep 08Dokumen64 halamanSchedule of Charges-Holy Family - Sep 08Quirinevv100% (1)
- Patelpriya InterventionalresumeuncDokumen2 halamanPatelpriya Interventionalresumeuncapi-356366193Belum ada peringkat
- Specific Adaptations for Premature NewbornsDokumen16 halamanSpecific Adaptations for Premature NewbornsIntekhabAtaharBelum ada peringkat
- Role of PharmacistDokumen9 halamanRole of PharmacistAbid Ali Khan0% (1)
- Bilateral Hypoplastic or Aplastic Posterior Tibial ArteryDokumen2 halamanBilateral Hypoplastic or Aplastic Posterior Tibial ArteryPaul HartingBelum ada peringkat
- Percakapan Dwi, Vina, Voni, FenyDokumen3 halamanPercakapan Dwi, Vina, Voni, Fenyvina tri utamiBelum ada peringkat
- Nursing Care of Client With Cataract SurgeryDokumen11 halamanNursing Care of Client With Cataract SurgeryFatin Fatihah AzizanBelum ada peringkat
- Total Experience 12 Years: Academic QualificationsDokumen3 halamanTotal Experience 12 Years: Academic QualificationsNHNBelum ada peringkat
- Medicinos Anglu KnygaDokumen76 halamanMedicinos Anglu KnygaJigglypuff166Belum ada peringkat
- Medscape Hypovolemic ShockDokumen14 halamanMedscape Hypovolemic ShockSarah Ovinitha100% (1)
- UntitledDokumen8 halamanUntitledPrakash SinghBelum ada peringkat
- Rekapan Instrumen Bedah Ok RSDMDokumen25 halamanRekapan Instrumen Bedah Ok RSDMnuningBelum ada peringkat
- SDL 4 MCN PDFDokumen3 halamanSDL 4 MCN PDFella retizaBelum ada peringkat
- Enciclopedia della Nutrizione clinica del caneDokumen3 halamanEnciclopedia della Nutrizione clinica del caneFrancesco NaniaBelum ada peringkat
- Graber and Wilbur's Family Medicine Examination and Board Review 4th Edition PDF (October 2016 Release) PDFDokumen801 halamanGraber and Wilbur's Family Medicine Examination and Board Review 4th Edition PDF (October 2016 Release) PDFYan Hoai100% (2)