The Relation Between Knowledge About Hypertension and Education in Hospitalized Patients With Stroke in Vienna
Diunggah oleh
Gina NdJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
The Relation Between Knowledge About Hypertension and Education in Hospitalized Patients With Stroke in Vienna
Diunggah oleh
Gina NdHak Cipta:
Format Tersedia
The Relation Between Knowledge About Hypertension and
Education in Hospitalized Patients With Stroke in Vienna
Doris Samal, MD; Stefan Greisenegger, MD; Eduard Auff, MD;
Wilfried Lang, MD; Wolfgang Lalouschek, MD
Downloaded from http://stroke.ahajournals.org/ by guest on September 25, 2016
Background and PurposeKnowledge about hypertension and its control influences blood pressure control in patients
with hypertension. We assessed these parameters in a large cohort of patients with ischemic stroke or transient ischemic
attack and analyzed their association with educational attainment.
MethodsFive hundred ninety-one consecutive patients with stroke with a medical history of hypertension were
interviewed about knowledge concerning hypertension within a multicenter hospital-based stroke registry. We analyzed
answers in relation to educational level with multivariate logistic regression adjusted for age and sex.
ResultsSeventy-seven percent of the patients stated to have known about hypertension being a risk factor for stroke, but
only 30% felt at increased risk of stroke. Less than half (47%) could identify 140 mm Hg or less as the maximum
tolerated systolic blood pressure, and 53% had their blood pressure only controlled monthly or less often. Knowledge
of possible consequences of myocardial infarction, nephropathy, peripheral vascular disease, and retinopathy was 64%,
20%, 11%, and 16%, respectively. Approximately half of patients were acquainted with the nonpharmacologic treatment
options of physical activity (49%), reduction of salt intake (54%), and reduction of caloric intake (48%), whereas
relaxation techniques were only known to 17%. Adherence to those treatment options ranged from 42% to 67%.
Educational level was significantly associated with knowledge of increased risk, possible consequences of hypertension,
and knowledge about nonmedication treatment options.
ConclusionKnowledge in our population was insufficient and partly associated with educational level, leaving much
room for improvement by educational campaigns. Furthermore, we found a gap between knowledge of the increased risk
for stroke in patients with hypertension and awareness of their own risk. (Stroke. 2007;38:1304-1308.)
Key Words: education hypertension ischemic socioeconomic status stroke
ypertension is the leading modifiable risk factor for
stroke, being causally involved in nearly 70% of all
stroke cases.1 Sixty percent of all patients with stroke report
a history of arterial hypertension2,3 and up to three fourths of
those with known and treated hypertension are not adequately
controlled.4,5 It has been estimated that nearly half (45%) of
all strokes among subjects with treatment for hypertension
might be attributed to poorly controlled hypertension.6,7
Moreover, a meta-analysis of 17 randomized, controlled trials
demonstrated a 38% reduction of stroke by blood pressure
lowering.8 This leaves plenty of room for population-based
strategies of blood pressure control to produce a substantial
relief in the global burden of stroke.
In hypertensive subjects, awareness about their increased
risk for stroke is connected to higher compliance in stroke
prevention practices.9 However, patients at risk for cerebrovascular disease tend to underestimate their risk, especially if
they are currently without symptoms and lack direct experience with the questioned event. Previous studies showed that
only a minority of individuals at an increased risk for stroke
or already under investigation for possible stroke were aware
of their increased risk.9,10 In these reports, socioeconomic
status was an independent predictor of awareness, a higher
education being linked with increased awareness. We sought
to assess awareness for hypertension and individual knowledge about it in a patient population with transient ischemic
attack (TIA) or ischemic stroke and a history of arterial
hypertension. We also investigated whether socioeconomic
status is associated with knowledge about hypertension.
Methods
Patients
This study was nested in the Vienna Stroke Registry, a prospective
population-based registry of patients admitted to one of the eight
participating neurologic departments in Vienna, Austria, serving a
community of 1.9 million people. Details of the Vienna Stroke
Registry have been published elsewhere.11 In short, all patients with
TIA or ischemic stroke, who were admitted within 72 hours of
symptom onset, were prospectively documented on the basis of
Received June 22, 2006; final revision received October 20, 2006; accepted October 30, 2006.
From the Department of Neurology (D.S., S.G., E.A., W.L.), Medical University of Vienna, Austria; and the Department of Neurology (W.L.), Hospital
Barmherzige Brueder, Vienna, Austria.
Correspondence to Wolfgang Lalouschek, MD, Medical University of Vienna, Department of Neurology, Waehringer Guertel 18-20, 1090 Vienna,
Austria. E-mail wolfgang.lalouschek@meduniwien.ac.at
2007 American Heart Association, Inc.
Stroke is available at http://www.strokeaha.org
DOI: 10.1161/01.STR.0000259733.43470.27
1304
Samal et al
Knowledge About Hypertension in Patients With Stroke
TABLE 1. Questions for Assessment of Knowledge and
Awareness of Hypertension
TABLE 2.
Baseline Characteristics of the Study Population
n591
Did you know about hypertension being a risk factor for stroke?
Sex, %, female/male
Did you feel at increased risk for stroke/myocardial infarction?
Age, median (interquartile range)
Which values should not be exceeded by systolic/diastolic blood pressure?
Education, %
44/56
70 (6078)
How often was your blood pressure controlled?
No basic school education
Do you own a blood pressure meter?
Secondary school graduation
26
Did you know about the following consequences of hypertension:
Apprenticeship
50
Myocardial infarction
Upper secondary graduation
10
Damage of kidney
College
Disturbed blood circulation of the legs
Disturbance of vision
Did you know about the following nonpharmacologic treatment options:
1305
Stroke type, %
TIA/minor stroke
37
Major stroke
63
Physical activity
Reduction of salt intake
Downloaded from http://stroke.ahajournals.org/ by guest on September 25, 2016
Results
Reduction of caloric intake
Relaxation techniques
Did you adhere to the following nonpharmacologic treatment options:
Physical activity
Reduction of salt intake
Reduction of caloric intake
Relaxation techniques
informed consent. We recorded clinical and neurologic parameters
(National Institutes of Health Stroke Scale, Scandinavian Stroke
Scale, modified Rankin Scale, Barthel Index), results of technical
and laboratory investigations, and performed a structured interview
for demographic factors, medical history, socioeconomic circumstances, and knowledge about risk factors. The diagnosis of stroke
was confirmed by cerebral computed tomography or magnetic
resonance imaging scan. Followup was done at 3, 12, and 24 months
after the qualifying event. Recruitment was done between December
1999 and December 2001. The protocol was approved by the local
ethics committee.
Educational Level
We chose education as a marker of socioeconomic status, because it
is reliably recalled, can be easily quantified in terms of numbers of
years, and reverse causation does not confuse interpretation.12 We
divided patients into five categories: no basic school education,
secondary school graduation, apprenticeship, upper secondary
school graduation, and university or college graduation.
Assessment of Awareness and Knowledge
About Hypertension
The questions for assessment of awareness and knowledge about
hypertension are given in Table 1.
Statistical Analysis
Statistical analysis was conducted with SPSS 11.0. Continuous data
are given as means. Categorical data are given as counts and
percentages. Binary and categorical data were analyzed using contingency tables and a 2 statistic. To assess the influence of socioeconomic status on knowledge, we applied multivariate logistic
regression and adjusted for age and sex. Probability values of 0.05
were considered statistically significant. Apprenticeship was used as
the reference category in the logistic regression model. The HosmerLemeshow test was used to assess the model fit; probability values
0.1 indicate an agreeable model fit.
Study Population
Of 1250 patients admitted with ischemic stroke or TIA
between December 1999 and December 2001, 868 (70%)
reported a history of arterial hypertension. One hundred
twenty-one patients were excluded, because their level of
education was unknown. Of the remaining 747 patients, 591
(68% of the population with hypertension) completed the
questionnaire concerning knowledge about hypertension and
were available for further analysis. Compared with the whole
hypertensive population, they did not differ in gender distribution (44% female in either group), but they were significantly younger (median 70 versus 73 years, P0.001).
Characteristics of the study population are summarized in
Table 2. Three hundred thirty-one (44%) were female and
260 (56%) were male. Female sex was associated with a
lower level of education (P0.001). Mean age was 69 years
(SD, 12; median, 70; interquartile range, 60 to 78). There
were no differences in age or severity of the event (TIA or
minor stroke versus major stroke) defined by educational
level. Distribution of cardiovascular risk factors according to
education is given in Table 3. There was no difference in
prevalence of diabetes, current smoking, hypercholesterinemia,
prior stroke, or coronary artery disease between the groups.
Awareness of and Knowledge About
Arterial Hypertension
Results of assessing awareness and knowledge about arterial
hypertension are summarized in Table 4. Seventy-seven
percent of patients claimed to be aware of hypertension as a
risk factor for stroke, but knowledge was highly significantly
correlated with educational level (P0.001). Only 30% had
considered themselves at increased risk for stroke and 34%
felt themselves at increased risk for myocardial infarction.
There was no difference between educational groups. Less
than half of the patients with hypertension (47%) stated a
systolic blood pressure of or below 140 mm Hg as the upper
limit but only 20% of patients stated this without a basic
school education (P0.05 compared with the reference
category). Knowledge of the maximum tolerated diastolic
blood pressure was the same throughout the groups and
comparably high with 81% of patients stating a value of
1306
Stroke
April 2007
TABLE 3.
Vascular Risk Factors According to Level of Education
No Basic
(n31)
Secondary
(n151)
Apprenticeship
(n294)
Upper Secondary
(n60)
University
(n55)
Diabetes, %
39
28
31
18
20
0.11
Current smoking, %
26
20
22
20
0.13
Hypercholesterinemia, %
58
57
54
47
60
0.61
Prior stroke, %
13
21
17
10
15
0.4
Coronary artery disease, %
23
34
25
20
22
0.14
Downloaded from http://stroke.ahajournals.org/ by guest on September 25, 2016
90 mm Hg or below. Fifty-three percent had their blood
pressure controlled at least weekly, whereas the remaining
47% controlled it monthly or less often. Patients without a
basic school education had a significantly lower frequency of
blood pressure measurements than the others (P0.05 compared with the reference category). Three fourths (76%) of
the patients stated they owned a blood pressure meter, but
only 63% used it.
Knowledge of other possible consequences of hypertension, namely myocardial infarction, nephropathy, peripheral
TABLE 4.
vascular disease, and retinopathy, were significantly associated with educational attainment. Knowledge about these
consequences ranged from 64% for myocardial infarction to
11% for peripheral vascular disease. Concerning nonpharmacologic options for lowering blood pressure, there were
significant differences defined by educational level as well;
the higher the educational level, the more patients were likely
to know about physical activity, reduction of salt intake,
reduction of caloric intake, and relaxation techniques. Knowledge about these options ranged from 17% (relaxation tech-
Awareness and Knowledge About Hypertension as a Risk Factor for Stroke According to Level of Education
Level of Education
n*
No
Basic
Secondary
Vocational
Upper
Secondary
University
Average
591
55
70
80
85
89
77
0.001
Knowledge about hypertension
Knowledge of hypertension as a risk
factor for stroke
Awareness of increased risk
Myocardial infarction
538
22
42
33
33
31
34
0.14
Stroke
539
26
33
29
22
32
30
0.62
Maximum systolic blood pressure,
140 mm Hg
468
20
48
48
43
52
47
0.17
Maximum diastolic blood pressure,
90 mm Hg
450
67
84
81
77
86
81
0.39
Blood pressure control daily/weekly
580
35
55
56
47
57
53
0.21
Own blood pressure meter
580
62
71
75
85
89
76
0.02
Possible consequences
Myocardial infarction
570
54
49
67
81
83
64
0.001
Nephropathy
563
14
17
32
46
20
0.001
Peripheral vascular disease
562
11
23
23
11
0.003
Retinopathy
564
14
14
25
31
16
0.002
Nonpharmacologic treatment
Physical activity
569
19
33
52
66
69
49
0.001
Reduction of salt intake
569
44
45
56
58
71
54
0.01
Reduction of caloric intake
568
48
38
49
54
67
48
0.007
Relaxation techniques
564
15
14
34
29
17
0.001
Adherence to
Physical activity
270
60
42
41
39
37
41
0.81
Reduction of salt intake
303
58
61
71
59
64
66
0.39
Reduction of caloric intake
269
50
45
53
38
50
49
0.57
94
100
55
41
17
21
37
0.52
Relaxation techniques
*Not all questions were answered by all patients.
Only patients who claimed being aware of the nonpharmacologic treatment option were included in the analysis.
Numbers represent percentages; total number of patients who responded to each of the questions are given on the left.
n1.
Samal et al
Knowledge About Hypertension in Patients With Stroke
niques) to 54% (reduction of salt intake). When asking about
adherence to these lifestyle modifications, 37% to 66%
affirmed to do so.
Discussion
Downloaded from http://stroke.ahajournals.org/ by guest on September 25, 2016
Awareness and knowledge about hypertension in patients
with stroke with a history of hypertension were suboptimal in
our population. Although three fourths (77%) stated they had
known about the increased risk for stroke associated with
hypertension, actually less than one third (30%) felt themselves at increased risk. This implies that more than half of
patients who affirmed the question Do you have a medical
history of hypertension? and had received the information
High blood pressure is a risk factor for stroke neglected
possible consequences for their own risk. The level of
awareness thus was lower than reported previously. Carroll et
al, who interviewed patients with stroke/TIA, found 43% of
the hypertensives were aware of their own risk.13 Samsa et al,
who interviewed 1261 patients with increased stroke risk,
found 41% of them were aware of it.9
Educational level markedly influenced knowledge of hypertension as a risk factor of stroke. It steadily increased from
54% in patients without a basic school education to 89% of
patients with a college degree. Interestingly, missing awareness of being at an increased risk for stroke and myocardial
infarction was the same throughout the groups. Because
patients with higher education were more likely to know
about the connection between stroke and hypertension, this
implies that they also more often denied this fact for themselves. To our knowledge, we are the first to investigate
knowledge and awareness separately, but our results
indicate that these are not necessarily linked to each other.
Notably, only half of the patients were able to state the
maximum tolerated systolic blood pressure (or a value below), which seems surprisingly low but is consistent with a
survey in the United States in 2005, where 49% could name
the target values of blood pressure.14
Questioning about consequences of hypertension revealed
another deficit: myocardial infarction was known by 64% of
the patients followed by nephropathy known by one of
fivewhereas peripheral vascular disease and retinopathy
reached only 11% and 16%, respectively. Compared with
knowledge in older Americans in a recent report, in which
86% could identify heart disease and 49% kidney failure as a
consequence of hypertension, this is clearly lower.15 Again,
there were highly significant differences between the different educational groups.
Nonpharmacologic treatment options by adoption of
healthy lifestyles have been recommended as an indispensable part of management in patients with hypertension.16
Weight reduction was shown to lower blood pressure with a
5 to 20-mm Hg systolic blood pressure reduction per 10-kg
weight loss,17,18 as does reduction of sodium intake (2 to
8 mm Hg)19 21 and regular physical activity (4 to 9 mm Hg).22,23
All named treatment options were known by approximately
half of our population with exception a fourth option we
askedpracticing relaxing techniqueswhich was only familiar to 17% of patients. Again, there were clear differences
between the educational groups. Consecutively asking about
1307
adherence to these lifestyle modifications showed that better
knowledge is not necessarily related to a better practice; the
only statistical significance according to educational level
concerned reduction of salt intake, whereas the other three
options were adopted by a maximum of nearly 40% of
patients in all educational levels.
In summary, there is much room for improvement in
hypertensive patients awareness of and knowledge about
hypertension, its consequences, and nonpharmacologic ways
to control it. Moreover, it seems to be important to help
patients transfer their knowledge adequately into practice.
Perceived risk is one of the key factors for promoting
behavioral changes; a person perceiving risk for some adverse event as high is more likely to take preventive action to
reduce the risk.10 For our patients, this could, for example,
mean providing individualized risk feedback, which was
shown to be effective in increasing perceived stroke risk
among patients who had underestimated their stroke risk.10
For better adherence to lifestyle modifications, Burke et al
found a structured modification program to be effective.24
Our results do not only point out a strong need for improvement of knowledge in people at increased risk for cerebrovascular disease, but also the need of increasing awareness of
their individual risk. Because the drugs for effective lowering
of blood pressure exist, education of affected patients is an
important target to convert the possible 40% risk reduction
into reality for all patients with hypertension.
Disclosures
None.
References
1. Bronner LL, Kanter DS, Manson JE. Primary prevention of stroke.
N Engl J Med. 1995;333:13921400.
2. Bornstein NM, Aronovich BD, Karepov VG, Gur AY, Treves TA, Oved
M, Korczyn AD. The Tel Aviv Stroke Registry. 3600 consecutive
patients. Stroke. 1996;27:1770 1773.
3. Moulin T, Tatu L, Crepin Leblond T, Chavot D, Berges S, Rumbach T.
The Besancon Stroke Registry: an acute stroke registry of 2500 consecutive patients. Eur Neurol. 1997;38:10 20.
4. Klungel OH, Kaplan RC, Heckbert SR, Smith NL, Lemaitre RN, Longstreth WT Jr, Leufkens HG, de Boer A, Psaty BM. Control of blood
pressure and risk of stroke among pharmacologically treated hypertensive
patients. Stroke. 2000;31:420 424.
5. Luepker RV, Arnett DK, Jacobs DR Jr, Duval SJ, Folsom AR, Armstrong
C, Blackburn H. Trends in blood pressure, hypertension control and
stroke mortality: the Minnesota Heart Survey. Am J Med. 2006;119:
42 49.
6. Li C, Engstroem G, Hedblad B, Berglund G, Janzon L. Blood pressure
control and risk of stroke: a population-based prospective cohort study.
Stroke. 2005;36:725730.
7. Weinehall L, Ohgren B, Persson M, Stegmayr B, Boman K, Hallmans G,
Lindholm LH. High remaining risk in poorly treated hypertension: the
rule of halves still exists. J Hypertens. 2002;20:20812088.
8. Chalmers J. Global burden of stroke. Heart Dis. 2000;2:S13S17.
9. Samsa G, Cohen S, Goldstein L, Bonito A, Duncan P, Enarson C,
DeFriese G, Horner R, Matchar D. Knowledge of risk among patients at
increased risk for stroke. Stroke. 1997;28:916 921.
10. Kreuter MW, Strecher VJ. Changing inaccurate perceptions of health
risk: results from a randomized trial. Health Psychol. 1995;14:56 63.
11. Lang W, Lalouschek W; on behalf of the Vienna Stroke Study Group.
The Vienna Stroke Registry: objectives and methodology. Wien Klin
Wochenschr. 2001;113:141147.
12. Colhoun HM, Hemingway H, Poulter NR. Socio-economic status and
blood pressure: an overview analysis. J Hum Hypertens. 1998;12:91110.
1308
Stroke
April 2007
Downloaded from http://stroke.ahajournals.org/ by guest on September 25, 2016
13. Carroll C, Hobart J, Fox C, Tearne L, Gibson J. Stroke in Devon:
knowledge was good, but action was poor. J Neurol Neurosurg Psychiatry. 2004;75:567571.
14. Cheng S, Lichtman JH, Amatruda JM, Smith GL, Mattera JA, Roumanis
SA, Krumholz HM. Knowledge of blood pressure levels and targets in
patients with coronary heart disease in the USA. J Hum Hypertens.
2005;19:769 774.
15. Egan BM, Lackland DT, Cutler NE. Awareness, knowledge and attitudes
of older Americans about high blood pressure. Arch Intern Med. 2003;
163:681 687.
16. Williams B, Poulter NR, Brown MJ, Davis M, McInnes GT, Potter JF,
Sever PS, Tohm S. Guidelines for management of hypertension: report of
the fourth working party of the British Hypertension Society,
2004 BHS IV. J Hum Hypertens. 2004;18:139 185.
17. The Trials of Hypertension Prevention Collaborative Research Group.
Effects of weight loss and sodium reduction intervention on blood
pressure and hypertension incidence in overweight people with highnormal blood pressure. The Trials of Hypertension Prevention, phase II.
Arch Intern Med. 1997;157:657 667.
18. He J, Whelton PK, Appel LJ, Charleston J, Klag MJ. Long-term effects
of weight loss and dietary sodium reduction on incidence of hypertension.
Hypertension. 2000;35:544 549.
19. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D,
Obarzanek E, Conlin PR, Miller ER 3rd, Simons-Morton DG, Karanja N,
Lin PH; DSH-Sodium Collaborative Research Group. Effects on blood
pressure on reduced dietary sodium and the Dietary Approaches to Stop
Hypertension (DASH) diet. N Engl J Med. 2001;344:310.
20. Vollmer WM, Sacks FM, Ard J, Appel LJ, Bray GA, Simons-Morton DG,
Conlin PR, Svetkey LP, Erlinger TP, Moore TJ, Karanja N; DASHSodium Trial Collaborative Research Group. Effects of diet and sodium
intake on blood pressure: subgroup analysis of the DASH-sodium trial.
Ann Intern Med. 2001;135:1019 1028.
21. Chobanian AV, Hill M. National Heart, Lung and Blood Institute
Workshop on sodium and blood pressure: a critical review of current
scientific evidence. Hypertension. 2000;35:858 863.
22. Kelley GA, Kelley KS. Progressive resistance exercise and resting blood
pressure: a meta-analysis of randomized controlled trials. Hypertension.
2000;35:838 843.
23. Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood
pressure: a meta-analysis of randomized controlled trials. Ann Intern
Med. 2002;38:11121117.
24. Burke V, Beilin LJ, Cutt HE, Mansour J, Wilson A, Mori TA. Effects of
a lifestyle programme on ambulatory blood pressure and drug dosage in
treated hypertensive patients: a randomized controlled trial. J Hypertens.
2005;23:12411249.
The Relation Between Knowledge About Hypertension and Education in Hospitalized
Patients With Stroke in Vienna
Doris Samal, Stefan Greisenegger, Eduard Auff, Wilfried Lang and Wolfgang Lalouschek
Downloaded from http://stroke.ahajournals.org/ by guest on September 25, 2016
Stroke. 2007;38:1304-1308; originally published online February 22, 2007;
doi: 10.1161/01.STR.0000259733.43470.27
Stroke is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright 2007 American Heart Association, Inc. All rights reserved.
Print ISSN: 0039-2499. Online ISSN: 1524-4628
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://stroke.ahajournals.org/content/38/4/1304
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Stroke can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.
Once the online version of the published article for which permission is being requested is located, click
Request Permissions in the middle column of the Web page under Services. Further information about this
process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Stroke is online at:
http://stroke.ahajournals.org//subscriptions/
Anda mungkin juga menyukai
- Cooking - Sauces and Marinade RecipesDokumen96 halamanCooking - Sauces and Marinade Recipesagape_1st7100% (3)
- Practical Visual Inspection of WeldsDokumen40 halamanPractical Visual Inspection of WeldsAmit Sharma100% (1)
- Diagnosis and Management of Subarachnoid HemorrhageDokumen25 halamanDiagnosis and Management of Subarachnoid HemorrhageMisael ClintonBelum ada peringkat
- Mechanic CV TemplateDokumen2 halamanMechanic CV Templateasmaa brkBelum ada peringkat
- FAT Form Winch UnitDokumen7 halamanFAT Form Winch UnitYadi KusmayadiBelum ada peringkat
- JAFZA Construction Regulation - Third Edition 2003Dokumen73 halamanJAFZA Construction Regulation - Third Edition 2003Abdul JabbarBelum ada peringkat
- Wheel Horse by YearDokumen14 halamanWheel Horse by YearNeil SmallwoodBelum ada peringkat
- SuctioningDokumen30 halamanSuctioningbajaoc60% (5)
- Aquatic Therapy ScientificAspects PDFDokumen14 halamanAquatic Therapy ScientificAspects PDFCarlos Ernesto AriasBelum ada peringkat
- Social Learning TheoryDokumen23 halamanSocial Learning TheoryJacqueline Lacuesta100% (2)
- Journal 4Dokumen7 halamanJournal 4Denys PutraBelum ada peringkat
- Journal StrokeDokumen5 halamanJournal StrokeRika Sartyca IlhamBelum ada peringkat
- Seminar: EpidemiologyDokumen13 halamanSeminar: EpidemiologySol LakosBelum ada peringkat
- Knowledge, Awareness and Self-Care Practices of Hypertension Among Cardiac Hypertensive PatientsDokumen11 halamanKnowledge, Awareness and Self-Care Practices of Hypertension Among Cardiac Hypertensive PatientsWaqas ShahnawazBelum ada peringkat
- Low Systemic Vascular ResistanceDokumen7 halamanLow Systemic Vascular ResistanceMuhammad BadrushshalihBelum ada peringkat
- Article For Journal - CETDokumen9 halamanArticle For Journal - CETawuahbohBelum ada peringkat
- DNB Vol25 No2 142Dokumen7 halamanDNB Vol25 No2 142Apsopela SandiveraBelum ada peringkat
- International Journal of Scientific Research: General MedicineDokumen4 halamanInternational Journal of Scientific Research: General MedicineTriple ABelum ada peringkat
- Abstracs Neuroepidemiology 2021Dokumen106 halamanAbstracs Neuroepidemiology 2021NICOLAS PEREZBelum ada peringkat
- Tgs Jurnal 1Dokumen7 halamanTgs Jurnal 1suciBelum ada peringkat
- Risk of OSA in patients with type 2 diabetesDokumen9 halamanRisk of OSA in patients with type 2 diabetesadityakurniantoBelum ada peringkat
- Risk Factors For Hypertension and Its Complications Case Control StudyDokumen4 halamanRisk Factors For Hypertension and Its Complications Case Control StudyutarinuBelum ada peringkat
- Missed Ischemic Stroke Diagnosis in The Emergency Department by Emergency Medicine and Neurology ServicesDokumen7 halamanMissed Ischemic Stroke Diagnosis in The Emergency Department by Emergency Medicine and Neurology ServicesReyhansyah RachmadhyanBelum ada peringkat
- Toast CriteriaDokumen4 halamanToast CriteriaKanagavalli VijayakumarBelum ada peringkat
- Levy2012 PDFDokumen9 halamanLevy2012 PDFDianBelum ada peringkat
- Subclinical Hypertensive Heart Disease in Black Patients With Elevated Blood Pressure in An Inner-City Emergency DepartmentDokumen9 halamanSubclinical Hypertensive Heart Disease in Black Patients With Elevated Blood Pressure in An Inner-City Emergency DepartmentDianBelum ada peringkat
- Arterial HypertensionDokumen13 halamanArterial HypertensionZedodurex100% (1)
- The Dynamics of Haemostatic Parameters in Acute Psychotic Patients: A One-Year Prospective StudyDokumen8 halamanThe Dynamics of Haemostatic Parameters in Acute Psychotic Patients: A One-Year Prospective StudyApsopela SandiveraBelum ada peringkat
- The Prevalence of ArterialDokumen8 halamanThe Prevalence of ArterialInternational Medical PublisherBelum ada peringkat
- Thirty-Day Readmission Is Higher in Patients With Brainstem vs. Non-Brainstem Lacunar StrokeDokumen5 halamanThirty-Day Readmission Is Higher in Patients With Brainstem vs. Non-Brainstem Lacunar StrokeijasrjournalBelum ada peringkat
- Captura de Pantalla 2021-08-02 A La(s) 1.24.53 P. M.Dokumen6 halamanCaptura de Pantalla 2021-08-02 A La(s) 1.24.53 P. M.Andres Felipe Quimbayo CifuentesBelum ada peringkat
- Prehypertensive and Mildly Hypertensive Young Adults at Higher Cardiovascular RiskDokumen8 halamanPrehypertensive and Mildly Hypertensive Young Adults at Higher Cardiovascular RiskIndah SundariBelum ada peringkat
- 1-s2.0-S1525505013004186 TUGAS INDAH-mainDokumen5 halaman1-s2.0-S1525505013004186 TUGAS INDAH-mainRendi Er PratamaBelum ada peringkat
- Exercise Stress Test As An Antidote For Anxiety Ne PDFDokumen2 halamanExercise Stress Test As An Antidote For Anxiety Ne PDFmehrshad Farahpour Gp5Belum ada peringkat
- Development and Validation of A Risk Score For Predicting Death in Chagas' Heart DiseaseDokumen8 halamanDevelopment and Validation of A Risk Score For Predicting Death in Chagas' Heart Diseaserandom guyBelum ada peringkat
- Population-Based Study of Incidence, Risk Factors, Outcome, and Prognosis of Ischemic Peripheral Arterial EventsDokumen11 halamanPopulation-Based Study of Incidence, Risk Factors, Outcome, and Prognosis of Ischemic Peripheral Arterial EventsIrina NeamtuBelum ada peringkat
- Relation Between Vascular Risk Factors and Cognition at Age 75Dokumen7 halamanRelation Between Vascular Risk Factors and Cognition at Age 75Fajar Rudy QimindraBelum ada peringkat
- Pattern of Stroke in Type 2 Diabetic Subjects Versus Non Diabetic SubjectsDokumen4 halamanPattern of Stroke in Type 2 Diabetic Subjects Versus Non Diabetic SubjectsRobbi OcktadinataBelum ada peringkat
- Dapus 2-Feigin2005Dokumen9 halamanDapus 2-Feigin2005sri noviyanty yusufBelum ada peringkat
- 302 Cardiovascular Risk: AssessmentDokumen1 halaman302 Cardiovascular Risk: AssessmentLêHữuHoàiBelum ada peringkat
- Blood Pressure Control and Primary Prevention of Stroke: Summary of The Recent Clinical Trial Data and Meta-AnalysesDokumen16 halamanBlood Pressure Control and Primary Prevention of Stroke: Summary of The Recent Clinical Trial Data and Meta-AnalysesAngelika AHuiBelum ada peringkat
- Early Prediction of Severity StrokeDokumen11 halamanEarly Prediction of Severity StrokeainihanifiahBelum ada peringkat
- Research: The Burden of Rheumatic Heart Disease Among Children in Lagos: How Are We Fairing?Dokumen10 halamanResearch: The Burden of Rheumatic Heart Disease Among Children in Lagos: How Are We Fairing?hazer sanoyBelum ada peringkat
- MGvol81.2011 25Dokumen8 halamanMGvol81.2011 25eminacengic5851Belum ada peringkat
- Diabetes Mellitus and Heart Failure 2017 The American Journal of MedicineDokumen11 halamanDiabetes Mellitus and Heart Failure 2017 The American Journal of MedicineAlina PopaBelum ada peringkat
- Ni Hms 643292Dokumen12 halamanNi Hms 643292LeksmanaHidayatullahBelum ada peringkat
- Ni Hms 366201Dokumen17 halamanNi Hms 366201Habiburrahman EffendyBelum ada peringkat
- Resistant HypertensionDokumen12 halamanResistant Hypertensionsury listinBelum ada peringkat
- Gupea 2077 35191 1Dokumen81 halamanGupea 2077 35191 1pearl ikebuakuBelum ada peringkat
- Blood Pressure and Clinical Outcomes in The International Stroke TrialDokumen7 halamanBlood Pressure and Clinical Outcomes in The International Stroke TrialMif Al-HudaBelum ada peringkat
- Hipertrofia VD en HTADokumen8 halamanHipertrofia VD en HTAgustavo reyesBelum ada peringkat
- Original Article: Hyponatremia in Stroke Patients and Its Association With Early MortalityDokumen7 halamanOriginal Article: Hyponatremia in Stroke Patients and Its Association With Early Mortalitykholis rizqullahBelum ada peringkat
- Arteritis TakayasuDokumen7 halamanArteritis TakayasuGina ButronBelum ada peringkat
- Stroke 1998 Davis 1333 40Dokumen9 halamanStroke 1998 Davis 1333 40ari_julian94Belum ada peringkat
- Literature Review of Rheumatic Heart DiseaseDokumen5 halamanLiterature Review of Rheumatic Heart Diseaseafdtakoea100% (1)
- Discharge Medications Among Ischemic Stroke SurvivorsDokumen6 halamanDischarge Medications Among Ischemic Stroke SurvivorsAnonymous EAPbx6Belum ada peringkat
- Heart Rate Variability and Myocardial Infarction Systematic Literature Review and Meta AnalysisDokumen7 halamanHeart Rate Variability and Myocardial Infarction Systematic Literature Review and Meta Analysisea68afjeBelum ada peringkat
- Hipertensi Infark Lacunar 1Dokumen6 halamanHipertensi Infark Lacunar 1anankastikBelum ada peringkat
- BallDokumen8 halamanBallAllan Alejandro SevillaBelum ada peringkat
- Pharm D (PB) 2 YEAR 2020-2021: Under The Guidance of GuideDokumen41 halamanPharm D (PB) 2 YEAR 2020-2021: Under The Guidance of Guidesufiya fatimaBelum ada peringkat
- Nota 2Dokumen8 halamanNota 2Hector GuzmanBelum ada peringkat
- Relationship between anxiety, stress, depression and hypertensionDokumen5 halamanRelationship between anxiety, stress, depression and hypertensionkamel abdiBelum ada peringkat
- Martini2012 PDFDokumen10 halamanMartini2012 PDFSofia ImaculataBelum ada peringkat
- Estudo CompletoDokumen16 halamanEstudo CompletoRitaIvoBelum ada peringkat
- Jurnal Kedokteran Dan Kesehatan Indonesia: Association Between Malnutrition and StrokeDokumen7 halamanJurnal Kedokteran Dan Kesehatan Indonesia: Association Between Malnutrition and StrokeAditya BatlajeryBelum ada peringkat
- Intraoperative Hypotension and Myocardial.3Dokumen10 halamanIntraoperative Hypotension and Myocardial.3novita ChristinaBelum ada peringkat
- Initiation of Antihypertensive Therapy Based On.480Dokumen2 halamanInitiation of Antihypertensive Therapy Based On.480jackie funtanillaBelum ada peringkat
- Anemia in Young Patients With Ischaemic Stroke2015Dokumen6 halamanAnemia in Young Patients With Ischaemic Stroke2015Nicolas RodriguezBelum ada peringkat
- Secondary HypertensionDari EverandSecondary HypertensionAlberto MorgantiBelum ada peringkat
- WomensSupportGroupArticle1993PrepublicationFinal PDFDokumen34 halamanWomensSupportGroupArticle1993PrepublicationFinal PDFGina NdBelum ada peringkat
- Quality Clinical Governance Framework Distributed Final 9 April 2015Dokumen24 halamanQuality Clinical Governance Framework Distributed Final 9 April 2015Gina NdBelum ada peringkat
- The History of Knowledge Development in Nursing - Feb15Dokumen6 halamanThe History of Knowledge Development in Nursing - Feb15Gina NdBelum ada peringkat
- Jurnal Rokok Vs InsomniaDokumen7 halamanJurnal Rokok Vs InsomniaAgung Ihsan WibowoBelum ada peringkat
- JurnalDokumen13 halamanJurnalGina NdBelum ada peringkat
- 2761 9274 1 PBDokumen16 halaman2761 9274 1 PBGina NdBelum ada peringkat
- Higher Algebra - Hall & KnightDokumen593 halamanHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- RC14001® & RCMS®: Your Guide To Implementing A Responsible Care® Management SystemDokumen4 halamanRC14001® & RCMS®: Your Guide To Implementing A Responsible Care® Management SystemMohammed MehranBelum ada peringkat
- "Residential Childcare Facilities: Better Services For Namibia's Vulnerable Children" - Pact End-Of-Project ReportDokumen7 halaman"Residential Childcare Facilities: Better Services For Namibia's Vulnerable Children" - Pact End-Of-Project ReportNathan Wilkinson100% (1)
- Cottonhill - Red Collection PDFDokumen33 halamanCottonhill - Red Collection PDFVioricaBelum ada peringkat
- The Baking and Frozen Dough MarketDokumen4 halamanThe Baking and Frozen Dough MarketMilling and Grain magazineBelum ada peringkat
- Effective Determinantsof Consumer Buying Decisionon OTCDokumen13 halamanEffective Determinantsof Consumer Buying Decisionon OTCThinh PhamBelum ada peringkat
- Magnum 3416 SC: Product InformationDokumen2 halamanMagnum 3416 SC: Product InformationDridi BadredineBelum ada peringkat
- Palm Avenue ApartmentsDokumen6 halamanPalm Avenue Apartmentsassistant_sccBelum ada peringkat
- Entrenamiento de Fuerza y Salud Pediátrica Ingles PDFDokumen9 halamanEntrenamiento de Fuerza y Salud Pediátrica Ingles PDFGiiovanny PardoBelum ada peringkat
- Mini City Direct Heating SubstationDokumen4 halamanMini City Direct Heating SubstationPaul ButucBelum ada peringkat
- SEAS Scoliosis Course NYC Feb 2018Dokumen4 halamanSEAS Scoliosis Course NYC Feb 2018BorislavBelum ada peringkat
- Forensic Science Project Group B5518Dokumen5 halamanForensic Science Project Group B5518Anchit JassalBelum ada peringkat
- HVDC Vs HVAC TransmissionDokumen2 halamanHVDC Vs HVAC TransmissionBilal SahiBelum ada peringkat
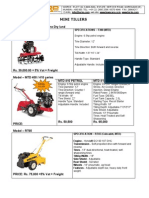
- Optimize soil preparation with a versatile mini tillerDokumen2 halamanOptimize soil preparation with a versatile mini tillerRickson Viahul Rayan C100% (1)
- King Khalid University College of Engineering Department of Chemical EngineeringDokumen9 halamanKing Khalid University College of Engineering Department of Chemical EngineeringbaderBelum ada peringkat
- RL Procedure Hard Natural Rubber PT - SURYA SAKTI SUKSESDokumen7 halamanRL Procedure Hard Natural Rubber PT - SURYA SAKTI SUKSESMuhammad ZakiBelum ada peringkat
- Form-Ii (See Regulation 4) Postal Bill of Export - II (To Be Submitted in Duplicate)Dokumen1 halamanForm-Ii (See Regulation 4) Postal Bill of Export - II (To Be Submitted in Duplicate)mrthilagamBelum ada peringkat
- Solution Manual For Safety Health and Environmental Concepts For The Process Industry 2nd EditionDokumen8 halamanSolution Manual For Safety Health and Environmental Concepts For The Process Industry 2nd EditionRobert Hornback100% (34)
- Solutions To Exercises, Chapter 19: Okuyama & Maskill: Organic ChemistryDokumen6 halamanSolutions To Exercises, Chapter 19: Okuyama & Maskill: Organic ChemistryM Irfan KhanBelum ada peringkat
- Developmental Psychology - Socioemotional Development in Middle & Late ChildhoodDokumen56 halamanDevelopmental Psychology - Socioemotional Development in Middle & Late ChildhoodAlyBelum ada peringkat
- Spez KR QUANTEC Prime enDokumen155 halamanSpez KR QUANTEC Prime enDave FansolatoBelum ada peringkat
- Guillermo Waco v. People Homicide RulingDokumen1 halamanGuillermo Waco v. People Homicide RulingCandelaria QuezonBelum ada peringkat
- Idioma Extranjero I R5Dokumen4 halamanIdioma Extranjero I R5EDWARD ASAEL SANTIAGO BENITEZBelum ada peringkat
- Vodafone Idea Limited: PrintDokumen2 halamanVodafone Idea Limited: PrintPrakhar KapoorBelum ada peringkat