Burchum & Rosenthal: Lehne's Pharmacology For Nursing Care, 9th Edition
Diunggah oleh
hockeyman1584Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Burchum & Rosenthal: Lehne's Pharmacology For Nursing Care, 9th Edition
Diunggah oleh
hockeyman1584Hak Cipta:
Format Tersedia
Burchum & Rosenthal: Lehnes Pharmacology for Nursing Care, 9th Edition
Chapter 94: Antiviral Agents II: Drugs for HIV Infection and Related Opportunistic
Infections
Key Points
This chapter reviews the agents used to treat human immunodeficiency virus (HIV)
infection. The chapter provides a brief overview of the epidemic of acquired
immunodeficiency syndrome (AIDS) while reminding us that HIV and AIDS are not
synonymous. The chapter reviews treatment approaches to HIV infection, including
antiretroviral therapy. The chapter begins with a discussion of the pathophysiology of
AIDS.
It is important to appreciate that HIV infection is not synonymous with AIDS, which
develops years after HIV infection is acquired. AIDS is a syndrome in which the patient
is HIV positive and has either (1) CD4 T-cell counts below 200 cells/mL or (2) an AIDSdefining illness.
Standard antiretroviral therapy (ART) consists of three or four drugs. These
combinations, often referred to as HAART (for highly active antiretroviral therapy), can
decrease plasma HIV to levels that are undetectable with current technology and can
thereby delay or reverse loss of immune function, decrease certain AIDS-related
complications, preserve health, prolong life, and decrease HIV transmission.
However, these benefits do not come without a price: ART is expensive, poses a risk of
long-term side effects and serious drug interactions, and must continue lifelong.
Accordingly, if treatment is to succeed, patients must be highly motivated and well
informed about all aspects of the treatment program. A strong support network is
extremely valuable too.
HIV is a retrovirus. Like all other viruses, retroviruses lack the machinery needed for
self-replication, and hence are obligate intracellular parasites. In contrast to other viruses,
retroviruses have positive-sense, single-stranded RNA as their genetic material.
Accordingly, in order to replicate, retroviruses must first transcribe their RNA into DNA.
The enzyme employed for this process is viral RNA-dependent DNA polymerase,
commonly known as reverse transcriptase.
The principal cells attacked by HIV are CD4 T cells (helper T lymphocytes).
As HIV kills CD4 T cells, the immune system undergoes progressive decline.
HIV replicates rapidly during all stages of the infection.
During the initial phase of infection, replication is massive because (1) the population of
CD4 cells is still large, thereby providing a large viral breeding ground; and (2) the host
has not yet mounted an immune response against HIVhence, replication can proceed
unopposed. During this stage of high viral load, patients often experience an acute
retroviral syndrome.
HIV mutates rapidly because HIV reverse transcriptase is an error-prone enzyme. Hence,
whenever it transcribes HIV RNA into single-stranded DNA and then into doublestranded DNA, there is a high probability of introducing base-pair errors. Because of
these errors, HIV can rapidly mutate from a drug-sensitive form into a drug-resistant
form.
Copyright 2016, 2013, 2010 by Saunders, an imprint of Elsevier Inc.
Key Points
94-2
To minimize the emergence of resistance, patients must be treated with a combination of
antiretroviral drugs.
HIV is transmitted sexually and by other means. The virus is present in all body fluids of
infected individuals. Transmission can be via intimate contact with semen, vaginal
secretions, and blood. The disease can be transmitted by sexual contact, transfusion,
sharing IV needles, and accidental needle sticks.
HIV infection follows a triphasic clinical course. During the initial phase, between 50%
and 90% of patients experience a flu-like acute retroviral syndrome. The middle phase of
HIV infection is characterized by prolonged clinical latency. During the late phase of
HIV infection, CD4 T cells drop below a critical level, rendering the patient highly
vulnerable to opportunistic infections and certain neoplasms. The late phase is when
AIDS occurs.
Many patients with HIV infection experience neurologic complications. Both the
peripheral nervous system and the central nervous system (CNS) may be involved.
Peripheral neuropathies affect 20% to 40% of patients and may develop at any time over
the course of HIV infection. In contrast, CNS complications usually occur late in the
disease.
The chapter then presents the classifications of the antiretroviral drugs.
At this time, we have five types of antiretroviral drugs. Three typesreverse
transcriptase inhibitors, integrase strand transfer inhibitors, and protease inhibitors
inhibit enzymes required for HIV replication. The other two typesfusion inhibitors and
chemokine receptor 5 antagonistsblock viral entry into cells.
The reverse transcriptase inhibitors are subdivided into two groups:
nucleoside/nucleotide reverse transcriptase inhibitors, which are structural analogs of
nucleosides or nucleotides, and (2) non-nucleoside reverse transcriptase inhibitors.
The chapter then discusses the nucleoside/nucleotide reverse transcriptase inhibitors, their
method of action, and their use in HIV treatment.
The nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs) were the first drugs
used against HIV infection and remain mainstays of therapy today.
Antiretroviral effects derive from suppressing synthesis of viral DNA by reverse
transcriptase.
To be effective, all of the NRTIs must first undergo intracellular conversion to their active
(triphosphate) forms.
Rarely, these agents cause a potentially fatal syndrome characterized by lactic acidosis
and hepatomegaly with steatosis.
Zidovudine was the first NRTI available and will serve as the prototype for the group.
The drug is an analog of thymidine, a naturally occurring nucleoside.
When employed in combination with other antiretroviral drugs, zidovudine can decrease
viral load, increase CD4 T-cell counts, delay onset of disease symptoms, and reduce
symptom severity.
The drugs principal dose-limiting toxicities are severe anemia and neutropenia.
Copyright 2016, 2013, 2010 by Saunders, an imprint of Elsevier Inc.
Key Points
94-3
Zidovudine inhibits HIV replication by suppressing synthesis of viral DNA.
Zidovudine penetrates to the CNS better than most other antiretroviral drugs, and hence
can be especially valuable for relieving cognitive symptoms.
The risk of myopathy (damage to muscle fibers) may occur with prolonged use. Myositis
(inflammation of muscle fibers) may also occur.
Drugs that are myelosuppressive, nephrotoxic, or directly toxic to circulating blood cells
can increase the risk of zidovudine-induced hematologic toxicity.
The chapter then discusses the non-nucleoside reverse transcriptase inhibitors, their
method of action, and their use in HIV treatment.
The non-nucleoside reverse transcriptase inhibitors (NNRTIs) differ from the NRTIs in
structure and mechanism of action. The NNRTIs bind to the active center of reverse
transcriptase and thereby cause direct inhibition.
Efavirenz is the only NNRTI deemed a preferred agent for treating HIV. The drug is
effective and, because of its long half-life, can be administered once a day.
Like all other drugs for HIV infection, efavirenz should be used only in combination with
other antiretroviral agents.
CNS symptoms occur in more than 50% of patients.
Rash, which can be severe, occurs often. Very rarely, rash evolves into potentially fatal
Stevens-Johnson syndrome, erythema multiforme, or toxic epidermal necrolysis.
Efavirenz is teratogenic. Women using the drug must avoid getting pregnant.
Efavirenz may pose a risk of liver damage.
Efavirenz can compete with other drugs for metabolism by cytochrome P450, thereby
causing them to accumulate, possibly to dangerous levels.
The chapter then discusses the protease inhibitors.
Protease inhibitors (PIs) are among the most effective antiretroviral drugs available.
When used in combination with NRTIs, they can reduce viral load to a level that is
undetectable with current assays.
PIs cause gastrointestinal disturbances, fat maldistribution, hyperglycemia and diabetes,
reduced bone mineral density, increased bleeding in hemophiliacs, and elevation of
triglyceride and transaminase levels.
All of the PIs can inhibit cytochrome P450 enzymes and can thereby increase levels of
other drugs.
To reduce the risk of resistance, PIs should never be used alone; rather, they should
always be combined with at least one reverse transcriptase inhibitor, and preferably two.
St. Johns wort, an herbal supplement taken for depression, can decrease levels of all PIs.
Garlic supplements can decrease levels of saquinavir, and probably levels of other PIs.
Lopinavir and ritonavir are available in a fixed-dose combination under the trade name
Kaletra. The combination is approved for HIV infection in adults and children older than
6 months. Lopinavir is the active antiretroviral component. Ritonavir is present only to
boost lopinavirs effects: By inhibiting cytochrome P450, ritonavir raises lopinavir levels
Copyright 2016, 2013, 2010 by Saunders, an imprint of Elsevier Inc.
Key Points
94-4
substantially and thereby enhances antiviral actions.
Protease inhibitors bind to the active site of HIV protease and thereby prevent the enzyme
from cleaving HIV polyproteins. As a result, the structural proteins and enzymes of HIV
are unable to function, and hence the virus remains immature and noninfectious.
Lopinavir/ritonavir is generally well tolerated. The most common adverse effects are
diarrhea, nausea, headache, and weakness or tiredness. Like all other PIs,
lopinavir/ritonavir poses a risk of hyperglycemia, new-onset diabetes, exacerbation of
existing diabetes, fat maldistribution, hyperlipidemia, bone loss, elevation of
transaminases, and increased bleeding in patients with hemophilia. Rash may occur in
children.
Lopinavir/ritonavir prolongs both the PR and QT intervals. By prolonging the PR
interval, the drug increases the risk of second- or third-degree atrioventricular (AV)
block. By prolonging the QT interval, lopinavir/ritonavir increases the risk of torsades de
pointes and other severe dysrhythmias.
Lopinavir/ritonavir inhibits two cytochrome P450 drug-metabolizing enzymesCYP3A4
and CYP2D6and can thereby raise levels of drugs that are substrates for these
enzymes. Serious toxicity can result.
Paradoxically, lopinavir/ritonavir can induce metabolism of some drugs, including
methadone and ethinyl estradiol, a component of many oral contraceptives.
Because of its alcohol content, the oral solution of lopinavir/ritonavir should not be
combined with disulfiram or metronidazole.
The taste of ritonavir is unpleasant; dilution of the oral solution in chocolate milk or a
liquid nutritional supplement has no impact on absorption, but does improve its taste.
The chapter then discusses raltegravir, an integrase strand transfer inhibitor.
Raltegravir is the first and only HIV integrase strand transfer inhibitor (INSTI) or,
simply, integrase inhibitor. By inhibiting integrase, raltegravir prevents insertion of HIV
genetic material into the DNA of CD4 cells and thereby stops HIV replication.
Raltegravir is active against HIV strains resistant to other drugs.
Raltegravir (in combination with tenofovir plus either emtricitabine or lamivudine) is
considered a first-choice drug for HIV treatment.
Raltegravir is generally well tolerated. The most common side effects are insomnia and
headache.
Rarely, patients have developed severe hypersensitivity reactions. Skin reactions include
Stevens-Johnson syndrome and toxic epidermal necrolysis, which can be fatal.
The chapter then discusses enfuvirtide, an HIV fusion inhibitor.
Enfuvirtide, widely known as T-20, is the first and only HIV fusion inhibitor.
Unlike most other drugs for HIV, which inhibit essential viral enzymesreverse
transcriptase, integrase, or proteaseenfuvirtide blocks entry of HIV into CD4 T cells.
Enfuvirtide prevents the HIV envelope from fusing with the cell membrane of CD4 cells
and thereby blocks viral entry and replication.
Copyright 2016, 2013, 2010 by Saunders, an imprint of Elsevier Inc.
Key Points
94-5
Enfuvirtide is reserved for HIV infection that is resistant to other antiretroviral drugs.
Injection-site reactions develop in 98% of patients, usually within the first week of
treatment. Principal manifestations are pain and tenderness, erythema and induration,
nodules or cysts, pruritus, and ecchymosis.
Enfuvirtide appears to increase the risk of bacterial pneumonia.
Because enfuvirtide is a foreign peptide, it can trigger hypersensitivity reactions.
Enfuvirtide has also been associated with respiratory distress, glomerulonephritis,
Guillain-Barr syndrome, and primary immune complex reaction, all of which may be
immune mediated.
The chapter next discusses maraviroc, a CCR5 antagonist.
Maraviroc is the first representative of a new class of antiretroviral drugs: the chemokine
receptor 5 (CCR5) antagonists. Maraviroc binds with CCR5 and blocks viral entry.
Maraviroc is indicated for combined use with other antiretroviral agents to treat patients
age 16 years and older who are infected with CCR5-tropic HIV-1 strains.
Use of the drug is likely to remain low because (1) dosing is complex (maraviroc must be
taken twice daily, and dosage must be adjusted on the basis of other drugs being used)
and (2) before maraviroc is used, a relatively expensive test must be performed to
confirm that the infecting HIV strain is indeed CCR5 tropic.
The most common side effects are cough, dizziness, pyrexia, rash, abdominal pain,
musculoskeletal symptoms, and upper respiratory tract infections. Intensity is generally
mild to moderate.
Liver injury has been seen in some patients and may be preceded by signs of an allergic
reaction.
The chapter then presents a discussion of the management of HIV infection.
Thanks to the drugs available today, HIV infection has been transformed from a nearcertain death sentence to a manageable chronic disease. Most patients take several
antiretroviral drugstypically two NRTIs combined with either a PI or an NNRTI.
Patients take a combination of drugs for HIV itself and may take additional drugs to
manage treatment side effects, along with drugs to prevent or treat opportunistic
infections. As a result, the potential for adverse effects and drug interactions is large.
Several tests are used to screen for HIV. They all detect anti-HIV antibodies. If an initial
screen produces a positive result, it must be confirmed by a follow-up test.
The principal laboratory tests employed to monitor HIV infection and guide therapy are
CD4 T-cell counts and plasma HIV RNA (viral load) assays.
Measurement of viral load indicates the magnitude of HIV replication and predicts the
rate of CD4 T-cell destruction. In contrast, CD4 T-cell counts indicate how much damage
the immune system has already suffered.
In addition to these tests, evaluation of HIV drug resistance is now done routinely.
Some patients will also need tests for HLA-B*5701 (a genetic variant linked to abacavir
hypersensitivity) and for HIV CCR5 tropism (a determinant of responsiveness to
Copyright 2016, 2013, 2010 by Saunders, an imprint of Elsevier Inc.
Key Points
94-6
maraviroc).
The term therapeutic drug monitoring (TDM) refers to the measurement of plasma drug
levels to help guide treatment. For antiretroviral therapy, routine TDM is not
recommended.
For patients with symptomatic or acute HIV disease, the benefits of treatment clearly
outweigh the risks; hence, immediate and aggressive treatment is recommended. In
contrast, for patients with asymptomatic HIV disease, the benefits of immediate treatment
may not outweigh the risks; hence, in some cases, it may be appropriate to delay
treatment.
During all phases of HIV disease, treatment has six basic goals:
o Maximal and durable suppression of viral load
o Restoration or preservation of immune function
o Improved quality of life
o Reduction of HIV-related morbidity and mortality
o Reduction of sexual HIV transmission
o Prevention of vertical HIV transmission
All patients with symptomatic (advanced) HIV disease should receive maximally
effective antiretroviral therapy, regardless of CD4 counts.
ART regimens typically contain three drugs. All regimens contain drugs from two
different classes. Preferred regimens consist of either (1) an NNRTI combined with two
NRTIs, (2) a PI combined with two NRTIs, or (3) raltegravir (an INSTI) combined with
two NRTIs. By using drugs from different classes, we can attack HIV in two different
ways, and can thereby enhance antiviral effects and reduce the risk of resistance.
Making the decision to treat during the chronic asymptomatic phase of HIV disease is
more difficult than during the symptomatic phase because we lack strong clinical data to
guide the decision. For most patients in the asymptomatic phase, we do not know if the
benefits will outweigh the risks, and so the optimal time to initiate therapy is uncertain.
All patients with primary acute HIV disease should receive maximally effective
antiretroviral therapy. As with symptomatic HIV disease, the preferred regimens consist
of three or four drugs.
There are two basic reasons for changing antiretroviral therapy: treatment failure and
drug toxicity.
When treatment failure occurs, the reason must be determined. Possibilities include
patient nonadherence, poor drug absorption, accelerated drug metabolism (owing to drug
interactions), and viral resistance.
If a patient experiences toxicity typical of a particular drug in the regimen, that drug
should be withdrawn and replaced with a drug that is (1) from the same class and (2) of
equal efficacy.
In young children, the course of HIV infection is accelerated. Whereas adults generally
remain symptom free for a decade or more, many children develop symptoms by their
first birthday. Death usually ensues by age 5 yearseven with ART. Young children
succumb so quickly because their immune systems are immature and less able to fend off
the virus.
Like older patients, young patients should be treated with a combination of antiretroviral
Copyright 2016, 2013, 2010 by Saunders, an imprint of Elsevier Inc.
Key Points
94-7
drugs, with the goals of (1) reducing plasma viral HIV to an undetectable level and (2)
stabilizing or improving immune status.
Unfortunately, therapy in young patients is confounded by limited information on dosing,
pharmacokinetics, and safety, and by the limited availability of pediatric formulations.
In general, management of HIV infection in pregnant women should follow the same
guidelines for managing HIV infection in nonpregnant adults.
ART is recommended for pregnant women who do not yet require therapy for their own
health because, even when ART is not needed for maternal health, it will still reduce the
risk of perinatal HIV transmission.
When treating HIV infection in pregnant women, the goal is to balance the benefits of
treatmentreducing viral load to promote the health of the mother and decrease the risk
of vertical HIV transmissionagainst the risks of drug-induced fetal harm. As a rule, the
benefits of treatment outweigh the risks.
Drug selection is challenging in that information on pharmacokinetics and safety during
pregnancy is limited. The combination of didanosine plus stavudine should be avoided,
owing to a risk of lactic acidosis and maternal/neonatal mortality. Efavirenz should be
avoided during the first trimester, owing to a risk of teratogenesis. All of the protease
inhibitors increase the risk of gestational diabetes, so blood sugar should be monitored
closely.
The chapter then discusses prevention of HIV infection by prophylactic treatment with
antiretroviral drugs.
The term preexposure prophylaxis (PrEP) refers to the use of antiretroviral drugs to
prevent HIV infection, rather than treat it.
One-time exposure to HIV carries a small, but nonetheless real, risk of infection. Sources
of exposure include unprotected vaginal or anal intercourse, receptive oral intercourse,
sharing a contaminated needle, accidental needle sticks, and being splashed with blood
and other body fluids.
The risk of developing HIV disease after a single exposure can be reducedbut not
eliminatedwith prophylactic antiretroviral drugs. Presumably, protection results from
preventing initial cellular infection and local propagation of HIV, thereby allowing host
immune defenses to eliminate the virus before it can become established.
To be effective, postexposure prophylaxis (PEP) should be initiated as soon as possible
after HIV exposurepreferably within 1 or 2 hours, and no later than 72 hoursand
should continue for 28 days. All patients should undergo testing for antibodies against
HIV, preferably at the time of exposure and then 6 weeks, 12 weeks, and 6 months after
exposure.
Most mother-to-child transmission of HIV occurs during the perinatal period, primarily
during delivery.
The risk for vertical transmission can be reduced by giving antiretroviral drugs to the
mother during gestation and labor, and to the infant for 6 weeks postpartum. Delivery by
cesarean section is recommended for patients with a viral load above 1000 copies/mL.
The chapter then reviews the prophylaxis and treatment of opportunistic infections.
Copyright 2016, 2013, 2010 by Saunders, an imprint of Elsevier Inc.
Key Points
94-8
Pneumocystis pneumoniaknown as PCPis a potentially fatal infection caused by
Pneumocystis jiroveci, a fungus.
The treatment of choice for PCP is trimethoprim plus sulfamethoxazole (TMP/SMZ).
TMP/SMZ is effective in 90% of patients. Nothing works better.
Prophylactic therapy of PCP is recommended for all patients with a CD4 T-cell count
below 200 cells/mm3. If ART raises CD4 counts above 200 cells/mm3 for at least 3
months, prophylaxis can be discontinued. The preferred medication for prophylaxis is
TMP/SMZ.
Cytomegalovirus (CMV) retinitis is the leading cause of vision loss in people with AIDS.
Drug therapy of CMV retinitis proceeds in two stages: induction followed by
maintenance. CMV retinitis can be treated with four agents: ganciclovir, valganciclovir,
cidofovir, and foscarnet. Ganciclovir is a drug of choice for CMV retinitis.
Mycobacterium tuberculosis and Mycobacterium avium complex are slow-growing
microbes that require prolonged drug exposure for eradication. To reduce emergence of
resistance, these infections are always treated with multiple drugs.
Toxoplasma gondii is a protozoan of the Sporozoa class. In the immunocompromised
host, infection can be lethal. Among patients with AIDS, toxoplasmosis usually manifests
as encephalitis.
If active T. gondii infection develops, the treatment of choice is pyrimethamine plus
sulfadiazine plus leucovorin. Once toxoplasmosis has been controlled, lifelong
suppressive therapy is needed.
Cryptococcus neoformans is a fungus that infects 9% to 13% of patients with AIDS. In
80% of these patients, cryptococcosis manifests as meningitis. The treatment of choice
for cryptococcal meningitis is amphotericin B plus flucytosine. After the initial infection
has been controlled, patients should continue maintenance therapy indefinitely. The
treatment of choice is oral fluconazole daily.
Varicella-zoster virus (VZV) can cause chickenpox and herpes zoster, also known as
shingles or simply zoster. Among adults with AIDS, VZV infection usually manifests as
shingles, which results from reactivation of latent VZV infection.
Preferred treatments are oral therapy with acyclovir, valacyclovir, or famciclovir. For
patients with disseminated VZV infection, the preferred treatment is IV acyclovir; IV
foscarnet is an alternative.
Infection with herpes simplex virus (HSV) is common among patients with HIV disease.
Lesions may occur at multiple sites. For infection at all sites, acyclovir is the drug of
choice. For patients with acyclovir-resistant HSV, IV foscarnet can be used.
HIV-infected patients frequently develop infection with Candida species, usually
Candida albicans. Up to 75% of patients experience oral candidiasis, which often
responds to topical therapy, such as swishing and swallowing a nystatin suspension or
sucking clotrimazole troches. Systemic therapy with an oral azolefluconazole,
itraconazole, or posaconazoleis an alternative.
The chapter concludes with a discussion of HIV vaccines and recommendations on how to
keep current regarding HIV therapy.
Copyright 2016, 2013, 2010 by Saunders, an imprint of Elsevier Inc.
Key Points
94-9
Development of an HIV vaccine is critical to controlling the AIDS epidemic worldwide.
Although HIV infection can now be managed with ART, treatment is expensive and
potentially dangerous, and must continue lifelong.
Making a safe and effective vaccine against HIV has proved exceedingly and
unexpectedly difficult.
Drug therapy of HIV infection is continuously evolving. New drugs are being developed,
knowledge of existing drugs is expanding, and new drug combinations are being studied.
These three web sites provide current information:
o AIDSinfo (aidsinfo.nih.gov).
o HIV and AIDS Activities (www.fda.gov/oashi/aids/hiv.html).
o AIDS Education Global Information System (www.aegis.com): perhaps the best
single web site for information on HIV and AIDS.
Copyright 2016, 2013, 2010 by Saunders, an imprint of Elsevier Inc.
Anda mungkin juga menyukai
- Obat Antivirus HIVDokumen16 halamanObat Antivirus HIVRasyidBelum ada peringkat
- M P Aids: Anagement of Atient WithDokumen44 halamanM P Aids: Anagement of Atient WithShubhra PaulBelum ada peringkat
- HivDokumen29 halamanHivSUTHAN100% (2)
- 3 Anti Retroviral Drugs 2012Dokumen29 halaman3 Anti Retroviral Drugs 2012Youths With PurposesBelum ada peringkat
- Hiv-Aids Related DrugsDokumen4 halamanHiv-Aids Related DrugsKitz Irish BelloBelum ada peringkat
- Hiv TreatmentDokumen5 halamanHiv Treatmentkariukijackson469Belum ada peringkat
- Antiretroviral TherapyDokumen41 halamanAntiretroviral TherapySami YGBelum ada peringkat
- Admissao Silvano - CópiaDokumen23 halamanAdmissao Silvano - CópiaOliver QuispeBelum ada peringkat
- HIV Drugs-2019Dokumen23 halamanHIV Drugs-2019salva sambaaBelum ada peringkat
- AntiviralDokumen17 halamanAntiviralDRx Raju ChandranBelum ada peringkat
- HIV Case (Long Case)Dokumen16 halamanHIV Case (Long Case)Max mitchyBelum ada peringkat
- ARVs NotesDokumen9 halamanARVs NotesBwambale AsinanBelum ada peringkat
- Current Perioperative Management of The Patient With Hiv A B, H M, C R, A G, A K e A.M. FDokumen12 halamanCurrent Perioperative Management of The Patient With Hiv A B, H M, C R, A G, A K e A.M. FPrashant SinghBelum ada peringkat
- Immunology AssingmentDokumen10 halamanImmunology AssingmentMedha BanerjeeBelum ada peringkat
- Final HIV Written ReportDokumen19 halamanFinal HIV Written ReportJohara MacasindelBelum ada peringkat
- Study of History and Progress Made in Anti Viral Drugs Used in Hiv/Aids TreatmentDokumen18 halamanStudy of History and Progress Made in Anti Viral Drugs Used in Hiv/Aids TreatmentAYUSH RANJANBelum ada peringkat
- HIV Simple Case StudyDokumen13 halamanHIV Simple Case StudyJanna Pimentel100% (1)
- Assignment - Anti Viral DrugsDokumen5 halamanAssignment - Anti Viral DrugsmziabdBelum ada peringkat
- 4 HivDokumen33 halaman4 HivAmr KhayyalBelum ada peringkat
- Prepared By: Dr. Brian Gilbert Fernandez, DPCOMDokumen28 halamanPrepared By: Dr. Brian Gilbert Fernandez, DPCOMShivani GauswamiBelum ada peringkat
- Lecture NineDokumen7 halamanLecture NineNyaramba DavidBelum ada peringkat
- Peac Hiv-2Dokumen31 halamanPeac Hiv-2SdBelum ada peringkat
- Antiviral Agents and Infection ControlDokumen94 halamanAntiviral Agents and Infection ControlKimberly GeorgeBelum ada peringkat
- Antiretroviral TherapyDokumen30 halamanAntiretroviral TherapyJon SonBelum ada peringkat
- 3 HIV PresentationDokumen22 halaman3 HIV PresentationMaiCAlmanzorBelum ada peringkat
- Antiretroviral Drugs and The Importance of Adherence To The DrugsDokumen20 halamanAntiretroviral Drugs and The Importance of Adherence To The DrugsSalihu MustaphaBelum ada peringkat
- A Call To Action - A Manual For Homeopaths in The Treatment of Patients With HIVAIDSDokumen44 halamanA Call To Action - A Manual For Homeopaths in The Treatment of Patients With HIVAIDSDR PRABHAT TANDONBelum ada peringkat
- Psychiatric Aspects of HIV Invection and AIDSDokumen28 halamanPsychiatric Aspects of HIV Invection and AIDSKiky SymbiontBelum ada peringkat
- Hiv-Aids SSDokumen22 halamanHiv-Aids SSAIBelum ada peringkat
- Antiviral DrugsDokumen4 halamanAntiviral DrugsD'poetrii Dewi SuryaniBelum ada peringkat
- Presentation - AIDSDokumen14 halamanPresentation - AIDSPuguBelum ada peringkat
- Molecular Virology of HIV-1 and Current Antiviral StrategiesDokumen7 halamanMolecular Virology of HIV-1 and Current Antiviral StrategiesDitha FadhilaBelum ada peringkat
- PALMK-IV - 6 - Obat Antivirus Ganjil 2122Dokumen34 halamanPALMK-IV - 6 - Obat Antivirus Ganjil 2122Oktavia Marintan ManullangBelum ada peringkat
- Medicinal Plant Used in Treatment of The Human Immunode Ciency VirusDokumen6 halamanMedicinal Plant Used in Treatment of The Human Immunode Ciency Virusyogesh ushirBelum ada peringkat
- What Is HIV?Dokumen8 halamanWhat Is HIV?Quan ThieuBelum ada peringkat
- Referat HIV AIDSDokumen13 halamanReferat HIV AIDSoctaviena zakariaBelum ada peringkat
- 2013 Article 325 PDFDokumen14 halaman2013 Article 325 PDFKadek MahariniBelum ada peringkat
- What Is HIV Antiretroviral Drug TreatmentDokumen24 halamanWhat Is HIV Antiretroviral Drug TreatmentDhrishya PadmakumarBelum ada peringkat
- Immune Deficinecy: By: Kirk Odrey O. Jimenez R.NDokumen51 halamanImmune Deficinecy: By: Kirk Odrey O. Jimenez R.NKirk08Belum ada peringkat
- Luo 2019 - Incidence and Types of HIV-1 Drug Resistance Mutation Among Patients Failing First-Line Antiretroviral TherapyDokumen5 halamanLuo 2019 - Incidence and Types of HIV-1 Drug Resistance Mutation Among Patients Failing First-Line Antiretroviral TherapyAndrew BanksBelum ada peringkat
- Hiv Seminar 2019Dokumen49 halamanHiv Seminar 2019clarice_condeno100% (1)
- N.B. HIV-1 and HIV-2 Are The Two Main Types of HIV. Most People With HIV Have HIV-1. HIV in This Document Refers To HIV-1Dokumen4 halamanN.B. HIV-1 and HIV-2 Are The Two Main Types of HIV. Most People With HIV Have HIV-1. HIV in This Document Refers To HIV-1tenqbroBelum ada peringkat
- Hiv/Aids: Mariano Marcos State University College of Health Sciences Department of Nursing Batac City, Ilocos NorteDokumen10 halamanHiv/Aids: Mariano Marcos State University College of Health Sciences Department of Nursing Batac City, Ilocos NorteEyySiEffVee100% (1)
- Journal of Pharmacy and Pharmacology - 2019 - Yap - Antiretroviral Agents in Pre Exposure Prophylaxis Emerging andDokumen14 halamanJournal of Pharmacy and Pharmacology - 2019 - Yap - Antiretroviral Agents in Pre Exposure Prophylaxis Emerging andandi siregarBelum ada peringkat
- Presentation: Anti Viral DrugsDokumen29 halamanPresentation: Anti Viral DrugsUmama WarrichBelum ada peringkat
- Non-Nucleoside Reverse Transcriptase InhibitorsDokumen4 halamanNon-Nucleoside Reverse Transcriptase InhibitorsPhiliplukaBelum ada peringkat
- Gulu Cohes Hiv Nelly MDDokumen68 halamanGulu Cohes Hiv Nelly MDYIKI ISAACBelum ada peringkat
- Biology Ip XiiDokumen8 halamanBiology Ip XiiSugumaran MageshBelum ada peringkat
- AidsDokumen11 halamanAidsroseannurakBelum ada peringkat
- Antibiotics Antiviral 10Dokumen30 halamanAntibiotics Antiviral 10Mylene MendozaBelum ada peringkat
- PM - Materi 1 HIV AIDS RevDokumen72 halamanPM - Materi 1 HIV AIDS RevSaly AlatasBelum ada peringkat
- Sup Ped 121401Dokumen28 halamanSup Ped 121401PRINCESASLUKBelum ada peringkat
- Adiel Joy P. Calsa (HIV AIDS Output)Dokumen6 halamanAdiel Joy P. Calsa (HIV AIDS Output)Adiel CalsaBelum ada peringkat
- Tagalog Na Tula Tungkol Sa WowoweeDokumen4 halamanTagalog Na Tula Tungkol Sa WowoweeStaff House50% (2)
- 0002YDokumen26 halaman0002YYogesh RathiBelum ada peringkat
- AidsDokumen10 halamanAidsDaniela OxaniBelum ada peringkat
- Therapeutic Drug Monitoring in Human Immunodeficiency Virus/Acquired Immunodeficiency SyndromeDokumen3 halamanTherapeutic Drug Monitoring in Human Immunodeficiency Virus/Acquired Immunodeficiency SyndromeFransiskus Samuel RenaldiBelum ada peringkat
- Zepatier As An Improved Drug Treatment For Hepatitis C Genotypes 1 and 4Dokumen10 halamanZepatier As An Improved Drug Treatment For Hepatitis C Genotypes 1 and 4api-317047226Belum ada peringkat
- Details On HIV/AIDSDokumen4 halamanDetails On HIV/AIDSTheSubhas ChandraBelum ada peringkat
- Society Is in The Middle of A Technological Transformation,' Andreessen Says - BloombergDokumen8 halamanSociety Is in The Middle of A Technological Transformation,' Andreessen Says - Bloomberghockeyman1584Belum ada peringkat
- SSRN Id1907904Dokumen127 halamanSSRN Id1907904hockeyman1584Belum ada peringkat
- Smart Beta: Too Good To Be True?: Bruce I. Jacobs and Kenneth N. LevyDokumen12 halamanSmart Beta: Too Good To Be True?: Bruce I. Jacobs and Kenneth N. Levyhockeyman1584Belum ada peringkat
- 3Dokumen31 halaman3hockeyman1584Belum ada peringkat
- Madrid (1775-1789) : Tapestry Cartoons El Escorial Palacio Real Del Pardo RococoDokumen2 halamanMadrid (1775-1789) : Tapestry Cartoons El Escorial Palacio Real Del Pardo Rococohockeyman1584Belum ada peringkat
- José Luzán Anton Raphael Mengs Spanish Real Academia de Bellas Artes de San FernandoDokumen2 halamanJosé Luzán Anton Raphael Mengs Spanish Real Academia de Bellas Artes de San Fernandohockeyman1584Belum ada peringkat
- Fuendetodos Aragón Zaragoza Notary Basque Zerain Gilder Basilica of Our Lady of The PillarDokumen1 halamanFuendetodos Aragón Zaragoza Notary Basque Zerain Gilder Basilica of Our Lady of The Pillarhockeyman1584Belum ada peringkat
- Hello 5Dokumen1 halamanHello 5hockeyman1584Belum ada peringkat
- Eastern Green Mamba: Venomous East Africa Scottish Zoologist Andrew Smith MambaDokumen1 halamanEastern Green Mamba: Venomous East Africa Scottish Zoologist Andrew Smith Mambahockeyman1584Belum ada peringkat
- Jessie Bonstelle: Disasters of War The Second of May 1808 The Third of May 1808 Caprichos Los DisparatesDokumen1 halamanJessie Bonstelle: Disasters of War The Second of May 1808 The Third of May 1808 Caprichos Los Disparateshockeyman1584Belum ada peringkat
- Paoli / Thorndale Line: Saturdays Sundays and Major HolidaysDokumen5 halamanPaoli / Thorndale Line: Saturdays Sundays and Major Holidayshockeyman1584Belum ada peringkat
- Francisco José de Goya y Lucientes (: La Maja Desnuda Charles IV of Spain and His FamilyDokumen1 halamanFrancisco José de Goya y Lucientes (: La Maja Desnuda Charles IV of Spain and His Familyhockeyman1584Belum ada peringkat
- Did You Know ... : Mosses Turkey Women's National FootballerDokumen1 halamanDid You Know ... : Mosses Turkey Women's National Footballerhockeyman1584Belum ada peringkat
- Harsh 5-4 Downshift On Deceleration: T-SB-0033-08 April 15, 2008Dokumen3 halamanHarsh 5-4 Downshift On Deceleration: T-SB-0033-08 April 15, 2008hockeyman1584Belum ada peringkat
- Hello 2Dokumen1 halamanHello 2hockeyman1584Belum ada peringkat
- Crosstrek MSA5P001SS9 24 12Dokumen18 halamanCrosstrek MSA5P001SS9 24 12hockeyman1584Belum ada peringkat
- Brake - Brake - Front Brake Pad - InspectionDokumen1 halamanBrake - Brake - Front Brake Pad - Inspectionhockeyman1584Belum ada peringkat
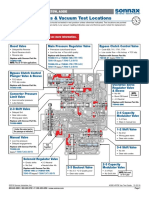
- AODE-4R75E VacTestDokumen2 halamanAODE-4R75E VacTesthockeyman1584Belum ada peringkat
- Course Outline 306 - Fall16Dokumen2 halamanCourse Outline 306 - Fall16hockeyman1584Belum ada peringkat
- Burchum & Rosenthal: Lehne's Pharmacology For Nursing Care, 9th EditionDokumen7 halamanBurchum & Rosenthal: Lehne's Pharmacology For Nursing Care, 9th Editionhockeyman1584Belum ada peringkat
- Burchum & Rosenthal: Lehne's Pharmacology For Nursing Care, 9th EditionDokumen2 halamanBurchum & Rosenthal: Lehne's Pharmacology For Nursing Care, 9th Editionhockeyman1584Belum ada peringkat
- Aac 02167-19Dokumen17 halamanAac 02167-19leokadiobarroso.rjBelum ada peringkat
- Bipolar DisorderDokumen83 halamanBipolar DisorderEko PriyantoBelum ada peringkat
- Digoxin (Lanoxin) : Routes of Administration Methods For Iv Administration and DosageDokumen2 halamanDigoxin (Lanoxin) : Routes of Administration Methods For Iv Administration and Dosageiamlx2Belum ada peringkat
- Ncmb317 Lecture: Psychiatric Mental Health Nursing: Bachelor of Science in Nursing 3YBDokumen5 halamanNcmb317 Lecture: Psychiatric Mental Health Nursing: Bachelor of Science in Nursing 3YB2 - GUEVARRA, KYLE JOSHUA M.Belum ada peringkat
- Cough and Common Cold Case PresentationDokumen5 halamanCough and Common Cold Case Presentationismael al karkosh100% (1)
- Unit-2 Drug InteractionsDokumen29 halamanUnit-2 Drug InteractionsMohammad Kaif50% (2)
- Case Study TBDokumen4 halamanCase Study TBMichael Baylon DueñasBelum ada peringkat
- Pharma - 2020 General Principles of Drug ActionDokumen163 halamanPharma - 2020 General Principles of Drug Actiongelean payodBelum ada peringkat
- "Speed-Balling": Mixing Stimulants and Opioids: MicromoduleDokumen40 halaman"Speed-Balling": Mixing Stimulants and Opioids: MicromoduleHigor ChamaneBelum ada peringkat
- 2005 Pleiotropic Effects of StatinsDokumen9 halaman2005 Pleiotropic Effects of StatinsK KBelum ada peringkat
- Acetylsalicylic AcidDokumen5 halamanAcetylsalicylic Acidarfa shemnaBelum ada peringkat
- The Medicalization of Mental Disorder Authors Peter Conrad, Caitlin SloddenDokumen13 halamanThe Medicalization of Mental Disorder Authors Peter Conrad, Caitlin SloddenBrett Lyszak100% (1)
- Assignment of Pharmacology Submitted by Laiba Shah To DR MaryumDokumen5 halamanAssignment of Pharmacology Submitted by Laiba Shah To DR MaryumLaiba ShahBelum ada peringkat
- Escitalopram in Post Traumatic Stress DisorderDokumen11 halamanEscitalopram in Post Traumatic Stress DisorderVivekBelum ada peringkat
- Jurnal Epo 1Dokumen7 halamanJurnal Epo 1Evelin VelinnBelum ada peringkat
- Research KajalDokumen5 halamanResearch KajalNutan Desai RaoBelum ada peringkat
- 4 Tribulus 1Dokumen15 halaman4 Tribulus 1ZozoBelum ada peringkat
- Aspartame Studies Correlation Outcome Funding Sources PDFDokumen18 halamanAspartame Studies Correlation Outcome Funding Sources PDFportosinBelum ada peringkat
- Terbutaline BricanylDokumen1 halamanTerbutaline BricanylB PBelum ada peringkat
- Conscious Sedation Lecture PDFDokumen18 halamanConscious Sedation Lecture PDFKhalid AhmedBelum ada peringkat
- Lower Back Pain Diagnostic AlgorithmDokumen1 halamanLower Back Pain Diagnostic AlgorithmZia HaywoodBelum ada peringkat
- Patient Education and Counseling HeadingsDokumen3 halamanPatient Education and Counseling HeadingsAnamta AshfaqBelum ada peringkat
- 2023 CC Full WorkbookDokumen988 halaman2023 CC Full WorkbookZahra Ahmed AlzaherBelum ada peringkat
- Gujarat Technological University: W.E.F. AY 2017-18Dokumen3 halamanGujarat Technological University: W.E.F. AY 2017-18raj royelBelum ada peringkat
- Urge Incontinence: +nocturnal Symptoms, Gets Urges All The Time DX: Cystometry: It Will Show Random Peaks RX: Anticholinergics: Oxybutynin, Tolteridine, Frequent VoidingsDokumen44 halamanUrge Incontinence: +nocturnal Symptoms, Gets Urges All The Time DX: Cystometry: It Will Show Random Peaks RX: Anticholinergics: Oxybutynin, Tolteridine, Frequent VoidingsAppu ayyalaBelum ada peringkat
- Research Essay 2Dokumen14 halamanResearch Essay 2api-549293108Belum ada peringkat
- ANESTHESIADokumen5 halamanANESTHESIALei DulayBelum ada peringkat
- Papich Handbook of Veterinary Drugs 5Th Edition Mark G Papich Full ChapterDokumen67 halamanPapich Handbook of Veterinary Drugs 5Th Edition Mark G Papich Full Chapterfrank.storm860100% (3)
- Aac 37 2 178Dokumen5 halamanAac 37 2 178Marcelo salvador silva MacotoraBelum ada peringkat