(Articles) Indian Peadiatrics May 1998
Diunggah oleh
Angela Mitchelle NyanganHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
(Articles) Indian Peadiatrics May 1998
Diunggah oleh
Angela Mitchelle NyanganHak Cipta:
Format Tersedia
INDIAN PFDIATRICS
VOLUME 35MAY 1998
Original Articles
AN APGAR SCORE OF THREE OR LESS AT ONE MINUTE IS NOT
DIAGNOSTIC OF BIRTH ASPHYXIA BUT IS A USEFUL
SCREENING TEST FOR NEONATAL ENCEPHALOPATHY
M. Ellis, N. Manandhar*, D.S. Manandhar* and A.M. deL Costello
From the Maternal and Infant Research Activities, Kathmandu, Nepal* and the Institute of Child
Health, London, United Kingdom
Reprint requests: Dr. Anthony Costello Center for International Child Health, Institute of
Child Health, 30 Guilfoord St London WC1N1EH United Kingdom.
Manuscript received: September 23, 1997 Initial review completed October 21, 1997,
Revision accepted December 6, 1997
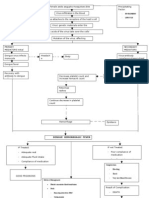
Objective: To evaluate the relationship between an Apgar score of three or less at one minute
of life and the subsequent risk of developing neonatal encephalopathy (NL) Design. Prospective
Setting The principal maternity hospital of Kathmandu, Nepal, a low income country, where
over 50% of the local population deliver Methods All liveborn infants over a 12 month period
with a birthweight of 500 g or more were assessed by the Apgar scoring system at one minute of
age All torn infants with neurological abnormalities presenting in the first day of life were
systematically examined and described according to a conventionally defined encephalopathy
grading system Major congenital malformations and neonatal infections were excluded
Results Over 12 months there were 14,771 total births of a weight of 500g or more of which
14,371 were live births and 400 were stillbirths. Of 734 infants with 1 min Apgar of three or
less, 91 developed NE The positive and negative predictive values of 1 min Apgar of three or less
for NE were 11 4% and 99 9%, respectively The probability of developing NE lose from 0 6%
(amongst all infants born at this hospital) to 11 2% (amongst infants born with a one minute
Apgar of three or less) Conclusions: An Apgar score of 3 or less at one minute is a useful
screening test for clinically significant birth asphyxia (NE) It over estimates by eight fold the
scale of the birth asphyxia problem but identifies a high risk group requiring further observation
of then neurological condition.
Key words: Apgar, Birth asphyxia, Neonatal encephalopathy.
IRTH asphyxia is an important cause
of perinatal mortality and morbidity
in developing countries(l) However, the
definition of birth asphyxia is problematic(2) Most studies from developing
countries report indirect measures of birth
asphyxia, principally Apgar scores, which
have been shown to have poor predictive
power for the key outcomes of death and
serious disability(3,4) The early neurological condition of the newborn is now recognized to be the best available indicator of
significant preceding birth asphyxia(5) and
the best predictor of both death and future
disability(6).
A task force established by the World
Federation of Neurology reviewed the
415
ELLIS ET AL.
clinical definition of birth asphyxia and
concluded that studies should aim to identify neonatal encephalopathy of early onset
(NE), record the clinical signs and investigate the etiology as fully as is feasible and
safe(7). We have done this for the first time
in a developing country hospital setting
and here compare the prevalence of birth
asphyxia using this method as our gold
standard with a conventional low Apgar
score approach. Our aim was to evaluate
the use of an Apgar score of three or less at
one minute as a screening method for the
detection of neonatal encephalopathy.
APGAR SCORE & NEONATAL ENCEPHALOPATHY
Subjects and Methods
Kathmandu deliveries(8). There are poor
communications with the hilly regions outside of the Kathmandu Valley. A recent
audit showed less than 3% of the women
delivering at Prasuti Griha were resident
outside of the Kathmandu Valley. There is
no functioning referral system for maternity cases in Nepal. The Hospital budget of
350,000 is supplemented by a modest user
charge. It offers the most competitively
priced institutional delivery service in the
Valley. We therefore consider the population who deliver at Prasuti Griha hospital is
broadly representative of the surrounding
population.
Setting
Clinical Definitions
The study population consisted of all
infants born during a 12 month period
(1995) at Prasuti Griha Maternity Hospital,
Kathmandu. This is the major maternity
hospital for the entire Kathmandu Valley,
delivering over 14,000 women annually
which we estimate to comprise 50% of all
Formal operational criteria to grade the
severity of encephalopathy in term infants
were derived from the descriptions by
Fenichel(9) and Levene et al. (10), modified
in the light of more recent studies and are
presented as Table I. These modifications
incorporate the observations that mild NE
Adapted from Fenichel (9).
The features in bold must be as described to meet the minimum requirements for each grade.
Features not in bold may be present but are not required to make the syndrome assignation.
a/b: Either abnormal tone or abnormal suck should accompany altered conscious level to assign
grade 1.
416
INDIAN PEDIATRICS
cases may have signs of increased as well
as decreased tone(11), that seizures activity
may not be clinically detectable(12) and
that the inclusion of duration in the clinical
definition of a grade renders the scheme
contradictory(13). Inter-observer reliability
of the grading system amongst five nonspecialist assessors on 27 neurologically
abnormal infants was tested. The kappa
value, a measure of agreement where 1 indicates perfect agreement and 0 no agreement better than chance alone, was 0.87 for
the scheme overall. These five assessors
continued to perform the daily neurological grading of NE throughout the study
period. The final assigned grade (1-mild,
2-moderate or 3-severe) as with Fenichel's
scheme corresponded to the most severe
encephalopathic state of the infant
observed during the period of neurological
abnormality.
An Apgar score of less than or equal to
3 at one minute of age was taken as the cut
off for significant birth asphyxia following
the World Health Organization International Classification of Disease (10th revision)(14). This is in line with National
Neontatology Forum guidelines that "gasping and ineffective breathing or lack of
breathing at 1 minute", which it is argued
corresponds to an Apgar at 1 minute of 3 or
less, arid "should be designated as birth
asphyxia"(15).
Case Finding and Investigation
All newborn infants were routinely
assessed and awarded Apgar scores at one
and five minutes of age. This was done by
the attending clinical staff, either a pediatrician or midwife. No special training was
given since it was our intention to compare
the routine measurement of Apgar scores
with subsequent encephalopathy grading.
It is hospital policy to admit to Special
Care Baby Unit (SCBU) all newborns with a
VOLUME 35-MAY 1998
one minute Apgar score less than or equal
to three, those with a birth weight less than
2.0 kg and all sick infants. Over the study
period 2,503 infants were admitted to
SCBU, 17% of all deliveries. At the outset of
the study period 1000 consecutive deliveries were checked on the routine post-natal
wards for clinical signs of encephalopathy.
No cases of NE who had not met the SCBU
admission criteria were identified during
this phase of the study. It was apparent
that the broadly defined admission criteria
for SCBU had already selected those
infants at risk of developing NE and therefore subsequently only SCBU admissions
were prospectively screened by daily neurological assessments.
All neurologically abnormal infants
detected by screening were then formally
examined following a standard examination protocol developed locally following
the principles of neurological evaluation
described by Amiel-Tison(16). The findings
were recorded daily on a standard
proforma. In suspected NE cases blood
sugar was measured by glucose strip testing (BM stix and Reflolux-S meter) to eliminate hypoglycemia (blood glucose less
than 2.6 mmol/L). If hypoglycemia was
detected, corrective measures were taken
and glucose estimation repeated until
normoglycemia was achieved. Blood cultures were performed routinely and Grade
2/3 infants underwent lumbar puncture
provided there was no evidence of raised
intracranial pressure. Infection was defined
by positive culture from either blood or
cerebrospinal fluid. All suspected NE cases
underwent early (first week) and late (six
week) cranial ultrasound.
Any infant with a gestational age of
more than 37 completed weeks [clinically
assessed by the Parkin method(17)] 'with
neurobehavioural evidence of encephalopathy at examination 6-24 hours after birth
417
ELLIS ET AL.
was defined as a case of NE. Exclusion criteria were: (i) Severely dysmorphic infants
with at least one major congenital abnormality; (ii) Infants with hepatosplenomegaly and cataracts indicative of intrauterine infection; (Hi) Infants with positive
blood/CSF cultures; (iv) Infants whose
neurological condition normalized when
hypoglycemia was corrected; and (v)
Preterm infants (less than 37 weeks). All
mothers of case infants were interviewed
for historical details and to explain the
diagnosis and follow up procedures.
Data Analysis
All data was entered onsite into a computer database using Filemaker Pro v2.0,
double-checked, and subsequently analyzed using Statview v4.1 and Stata 2.1.
Ethical Approval
Ethical approval was sought and given
by both the Nepal Medical Research Council and the Institute of Child Health Ethics
Committee, London.
Results
Study Population
During the study period there were
14,771 total births of a weight of 500 g or
more of which 14,371 were live births and
400 were stillbirths. There were 254 neonatal deaths of a weight of 500 g or more
prior to hospital discharge. This gives a
perinatal mortality rate prior to hospital
discharge of 44.3/1000 total births. Three
infants of probable term gestation (> 2.0 kg
birthweight) died following failed resuscitation efforts prior to admission to SCBU.
These cases all had 1 min Apgar < 3 but did
not survive to satisfy the NE case criteria.
They do not therefore appear in the numerator of NE cases although we consider
it likely that their rapid neonatal death was
due to birth asphyxia.
418
APGAR SCORE & NEONATAL ENCEPHALOPATHY
Birth Prevalence ofLoiv Apgar Score
During the study period a total of 734
infants with a birthweight of 500 g or more
had an Apgar score at 1 minute (Apgar1) of
three or less. Of these 548 (75%) had a
birthweight of 2000 g or more. The data is
presented stratified by birth weight in Table
II.
Prevalence of NE
During the study period 96 infants met
the case definition criteria for NE. Cranial
ultrasound was either normal or diffusely
echobright ('fuzzy' brain(18)) in all cases.
Five of these cases were subsequently
excluded because early neonatal blood
culture was positive and we therefore assume their encephalopathy resulted from
perinatal infection. This leaves a total of 91
cases of early neonatal encephalopathy in
whom no cause other than birth asphyxia
was evident. Table III presents NE grade
data by Apgar1 scores. Seven cases of NE
(8%) had Apgar1 > 3 including two cases
who went on to develop a severe grade 3
NE. All of them had an Apgar1 < 7.
INDIAN PEDIATRICS
Low Apgar Score As A Screening Test For NE
Table IV describes the qualities of the
one minute Apgar score as a test for NE.
For the purposes of evaluation we are here
using NE as the gold standard measure of
birth asphyxia(19).
Discussion
We have demonstrated that in a setting
representative of non-referral hospitals
throughout South Asia, the current definition of severe birth asphyxia used by WHO
identifies a population eight times greater
in magnitude than the population of term
infants manifesting neonatal encephalopathy not attributable to other causes. The
vast majority (92%) of NE cases had an
Apgar1 < 3 and all had an Apgar1 < 7.
Given a high patient to staff ratio and
rapid patient turnover, it is possible that a
VOLUME 35-MAY 1998
few mild cases of NE escaped detection.
However, moderate or severe NE is not
a subtle syndrome and following birth
asphyxia always presents within 24 hours
of birth(9). Therefore the discrepancy is
unlikely to be significantly explained by
under reporting of NE in this population.
Although there is significant interobserver variation in Apgar scoring, it
remains a useful indicator of the newborn's
general condition especially at the lower
extremes(20). There are two groups of newborns who may. have a low early Apgar but
do not develop NE. Firstly, there is a large
group of term infants depressed immediately after birth who rapidly improve. This
transient depression in the first minutes of
life is not associated with later neuro-development sequelae(6). Over 75% of the non
encephalopathic cases with low one minute
Apgar in this series had a birthweight of 2.0
Kg or more and are likely to have been of
term gestation.
The second group are preterm infants
who may have a low Apgar score due to
the immaturity of their responses(20). This
does not indicate brain injury due to birth
asphyxia. Less than 25% of this series had a
birthweight less than 2 kgs and are likely to
have been significantly premature.
Perinatal brain injury in premature infants
is generally anatomically different from
that seen in term infants following birth asphyxia and is thought to largely occur after
delivery(21). Interventions to improve outcome for this group of infants are likely to
differ from those aimed at the prevention
of asphyxia in term infants. Therefore a
measure of the prevalence of birth asphyxia should not simply amalgamate all
infants with reduced responses in the first
minutes of life.
Levene and colleagues compared Apgar
scores and what they termed post-
419
ELLIS ET AL.
asphyxial encephalopathy (PAE) in 126
infants in a UK hospital setting(10). They
found that 29 of 126 cases of PAE (23%)
had an Apgar1>3. The comparable proportion from the present study is rather less
(8%); Levene's study gives no data on the
overall prevalence of low Apgar in their
hospital.
Kumari and colleagues report a large
series of Apgar scores from an Indian district hospital in 35,959 infants born in one
of four years between 1981-88. They found
3.4% newborns had Apgar1 <3(22) and
7.6% Apgar1 < 7. Of These 41% had a birth
weight less than 2000 g. A multicenter
study of Apgar scores in Africa reported
that 22.6% of 4268 deliveries in central hospitals had a 5 min Apgar < 7(23). Both these
studies inferred that these large numbers
of infants had suffered significant birth
asphyxia.
We have shown that early Apgar scores
overestimate the scale of the problem of significant birth asphyxia as indicated by NE
but remain a useful screening test in busy
units. Our data suggests that an admission
policy for special care selecting all infants
with a one minute Apgar of three or less
will select approximately 5% of all deliveries and will include almost all cases of NE.
APGAR SCORE & NEONATAL ENCEPHALOPATHY
phyxia? Dev Med Child Neurol 1993; 35:
449-455.
3.
Levene ML, Sands C, Grindulis H, Moore
JR. Comparison of two methods of predicting outcome in perinatal asphyxia.
Lancet 1986; 1:67-69.
4.
Nelson KB, Ellenberg JK. Apgar scores as
predictors of chronic neurological
disability. Pediatrics 1981; 68: 36-44.
5.
Brown JK, Purvis RJ, Forfar JO, Cockburn
F. Neurological aspects of perinatal asphyxia. Dev Med Child Neurol 1974; 16:
567-580.
6.
Ellenberg JH, Nelson KB. Cluster of
perinatal events identifying infants at
high risk for death or disability. J Pediatr
1988; 113: 546-552.
7.
Birth Asphyxia: A statement. Dev Med
Child Neurol 1993; 35:1022-1024.
8.
Bolam AJ, Manadhar DS, Shrestha P,
Manandhar B, Ellis M, Costello AM de L.
Maternity care utilization in the
Kathmandu Valley: A community based
study. J Nepal Med Assoc 1997; 35: 122129.
9.
Fenichel JM. Hypoxic-ischemic encephalopathy in the newborn. Arch Neurol
1983; 40: 261-266.
10.
Levene ML, Kornberg J, Williams THC.
The incidence and severity of postasphyxial encephalopathy in full term infants. Early Hum Dev 1985; 11: 21-26.
11.
Amiel-Tison C, Ellison P, Birth asphyxia
in the full term newborn: Early assessment and outcome. Dev Med Child
Neurol 1986; 28: 671-682.
12.
Connel J, Oozer R, DeVries L, Dubowitz
LMS, Dubowitz V. Continuous EEG
monitoring of neonatal seizures: Diagnostic and prognostic considerations. Arch
Dis Child 1989; 64: 452-458.
13.
Leviton A, Nelson KB. Problems with
definitions and classifications of newborn
encephalopathy. Pediatr Neurology 1992;
8: 85-90.
Acknowledgements
This work has only been possible with
the support of the Directors and staff of
Prasuti Griha Maternity Hospital. The
MIRA project has enjoyed support from
Overseas Development Administration
and the NE project has been generously
funded by the Wellcome Trust.
REFERENCES
1.
World Health Organization. Essential
Newborn Care. Geneva, World Health
Organization 1996.
2.
Blair E. A research definition for birth as-
420
VOLUME 35-MAY 1998
INDIAN PEDIATRICS
14.
15.
16.
17.
18.
World Health Organization. International
Classification of Diseases and Related
Health Problems, Tenth revision Geneva,
World Health Organization, 1992.
19.
Singh M. Diagnosis and management of
perinatal asphyxia. Indian Pediatr 1994;
31:1169-1174.
Sackett R, Richardson WS, Rosenberg W.
Evidence-Based Medicine. New York,
Churchill Livingstone, 1997.
20.
Marlow N. Do we need an Apgar score?
Arch Dis Child 1992; 67: 765-769.
21.
Volpe JJ. Neurology of the Newborn. 3rd
edn. Boston, W.B. Saunders Co, 1995.
22.
Kumari S, Sharma M, Yadav M, Saraf A,
Kabra M, Mehra R. Trends in neonatal
outcome with low Apgar scores. Indian J
Pediatr 1993; 60: 415-422.
23.
Kinoti SN. Asphyxia of the newborn in
East, Central and Southern Africa. East
Afr Med J 1993; 70: 422-433.
Amiel-Tison C. Clinical assessment of the
infant nervous system. In: Fetal and Neonatal Neurology and Neurosurgery, 2nd
edn. Eds. Levene MI, Lilford RJ, Bennett
MJ, Edinburgh, Churchill Livingstone,
1995; pp 83-104.
Parkin JM, Hey EN, JS C. Rapid assessment of gestational age at birth. Arch Dis
Child 1976; 51: 259-263.
Govaert P, de Vries LS. An Atlas of Neo-
natal
Brain
Sonography.
MacKeith Press, 1997.
London,
421
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Jtptunimus GDL Fikrisanti 6769 2 BabiiDokumen8 halamanJtptunimus GDL Fikrisanti 6769 2 BabiiAngela Mitchelle NyanganBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Management of Breech Presentation: Green-Top Guideline No. 20bDokumen27 halamanManagement of Breech Presentation: Green-Top Guideline No. 20bSastra WijayaBelum ada peringkat
- Management of Status Epilepticus in Children: Clinical MedicineDokumen19 halamanManagement of Status Epilepticus in Children: Clinical MedicineDienda AleashaBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- 01LongChap34 Pneumoniaandcomplications PDFDokumen15 halaman01LongChap34 Pneumoniaandcomplications PDFAngela Mitchelle NyanganBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Management of Prolonged Seizures and Se in ChildhoodDokumen10 halamanManagement of Prolonged Seizures and Se in ChildhoodAngela Mitchelle NyanganBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Inguinal Hernia PDFDokumen6 halamanInguinal Hernia PDFBunmi OGUNGBEBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- 4600223Dokumen6 halaman4600223Angela Mitchelle NyanganBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- 01 Editorial DyspepsiaDokumen15 halaman01 Editorial DyspepsiaAngela Mitchelle NyanganBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- 10.hipernatremia AncianoDokumen6 halaman10.hipernatremia AncianoAngela Mitchelle NyanganBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- 10.hipernatremia AncianoDokumen6 halaman10.hipernatremia AncianoAngela Mitchelle NyanganBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- 01 Editorial DyspepsiaDokumen1 halaman01 Editorial DyspepsiaDiva Augusti DirgahayuBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Contact DermatitisDokumen70 halamanContact DermatitisThariq Mubaraq DrcBelum ada peringkat
- 01 GDL Puspawijay 205 1 Puspawi 7Dokumen10 halaman01 GDL Puspawijay 205 1 Puspawi 7Angela Mitchelle NyanganBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Eustachian Tube DysfunctionDokumen2 halamanEustachian Tube DysfunctionAngela Mitchelle NyanganBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Radiologic: Notes in Cardiology InterstitialDokumen9 halamanRadiologic: Notes in Cardiology InterstitialAngela Mitchelle NyanganBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- 01 Editorial DyspepsiaDokumen1 halaman01 Editorial DyspepsiaDiva Augusti DirgahayuBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Rapid Sequence InductionDokumen8 halamanRapid Sequence InductionAngela Mitchelle NyanganBelum ada peringkat
- Rapid Sequence InductionDokumen8 halamanRapid Sequence InductionAngela Mitchelle NyanganBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- 01 Editorial DyspepsiaDokumen1 halaman01 Editorial DyspepsiaDiva Augusti DirgahayuBelum ada peringkat
- Rapid Sequence InductionDokumen8 halamanRapid Sequence InductionAngela Mitchelle NyanganBelum ada peringkat
- Rapid Sequence InductionDokumen8 halamanRapid Sequence InductionAngela Mitchelle NyanganBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rapid Sequence InductionDokumen8 halamanRapid Sequence InductionAngela Mitchelle NyanganBelum ada peringkat
- TCP 23 15Dokumen6 halamanTCP 23 15Angela Mitchelle NyanganBelum ada peringkat
- Birth Injuries: Auwal M. Abubakar Johanna R. Askegard-Giesmann Brian D. KenneyDokumen4 halamanBirth Injuries: Auwal M. Abubakar Johanna R. Askegard-Giesmann Brian D. KenneyAngela Mitchelle NyanganBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Infantile Periocular Capillary Hemangioma An Unusual PresentationDokumen2 halamanInfantile Periocular Capillary Hemangioma An Unusual PresentationAngela Mitchelle NyanganBelum ada peringkat
- J Oftalmologi Vol 7 No 1 (Heni Riyanto)Dokumen4 halamanJ Oftalmologi Vol 7 No 1 (Heni Riyanto)Mahanani SubagioBelum ada peringkat
- Deep NeckSpaces 2002 04 Slides PDFDokumen61 halamanDeep NeckSpaces 2002 04 Slides PDFAngela Mitchelle NyanganBelum ada peringkat
- Millie Jones Case Study - Dysplipidemia and CKDDokumen7 halamanMillie Jones Case Study - Dysplipidemia and CKDAngela Mitchelle NyanganBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- (Case Report) CRF and Costal MassDokumen5 halaman(Case Report) CRF and Costal MassAngela Mitchelle NyanganBelum ada peringkat
- SIGN NHS Diagnosis Dan Management of CKD PDFDokumen57 halamanSIGN NHS Diagnosis Dan Management of CKD PDFAngela Mitchelle NyanganBelum ada peringkat
- Press Release - No Ebola in UgandaDokumen2 halamanPress Release - No Ebola in UgandaThe Independent MagazineBelum ada peringkat
- Arthritis Case Presentation - Dr. KlaesDokumen27 halamanArthritis Case Presentation - Dr. KlaesShanti VennamBelum ada peringkat
- Acute Gastritis CiciDokumen43 halamanAcute Gastritis CiciDwi Rezky AmaliaBelum ada peringkat
- Genital Ulcer DiseaseDokumen29 halamanGenital Ulcer DiseaseFu' BudhyBelum ada peringkat
- Pertusis 2Dokumen21 halamanPertusis 2AbhishekBelum ada peringkat
- New Lifebuoy Soap Ad AnalysisDokumen18 halamanNew Lifebuoy Soap Ad AnalysisAmit Pathak0% (1)
- 03 4502US Prospect SONOCA 185 - x2xDokumen7 halaman03 4502US Prospect SONOCA 185 - x2xJorge FerreiraBelum ada peringkat
- Glaucoma Pathophysiology and DetectionDokumen77 halamanGlaucoma Pathophysiology and DetectionSuleman MuhammadBelum ada peringkat
- Pedro Zuniga LawsuitDokumen28 halamanPedro Zuniga LawsuitJoshua DanzigBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Pnle Exam 2Dokumen39 halamanPnle Exam 2Anonymous hDcvppt100% (1)
- IV Oral Table PDFDokumen2 halamanIV Oral Table PDFRosyadi AkbarriBelum ada peringkat
- Brain InfectionsDokumen45 halamanBrain InfectionsjyothiBelum ada peringkat
- EPI To SendDokumen13 halamanEPI To SendMarylle Joy SullanoBelum ada peringkat
- Case StudyDokumen19 halamanCase StudySkyerexBelum ada peringkat
- Mers-Cov: Frequently Asked Questions and AnswersDokumen2 halamanMers-Cov: Frequently Asked Questions and AnswersKath ViteBelum ada peringkat
- HDFC Ie Pune 06 04 2020 PDFDokumen15 halamanHDFC Ie Pune 06 04 2020 PDFadvait_etcBelum ada peringkat
- Health DeclarationDokumen5 halamanHealth Declarationust dol100% (1)
- Thyroid CrisisDokumen20 halamanThyroid CrisisJeffrey DyerBelum ada peringkat
- Myanmar Translation Blog, Vol-1, Issue-14Dokumen24 halamanMyanmar Translation Blog, Vol-1, Issue-14ane lwanBelum ada peringkat
- Abnormal ECG Findings in Athletes: Seattle CriteriaDokumen1 halamanAbnormal ECG Findings in Athletes: Seattle CriteriaCésar Morales GarcíaBelum ada peringkat
- Diseases of Hard Tissues of Teeth PDFDokumen152 halamanDiseases of Hard Tissues of Teeth PDFAPARNA AARATHI SREEKUMARBelum ada peringkat
- Staphylococcus AureusDokumen3 halamanStaphylococcus AureusDenisse Watt CuarterosBelum ada peringkat
- MudrasDokumen4 halamanMudrasBabou ParassouramanBelum ada peringkat
- Molecular Diagnostics of Infectious Diseases, 2010, PGDokumen207 halamanMolecular Diagnostics of Infectious Diseases, 2010, PGrieza_husein100% (2)
- EpilepsyDokumen38 halamanEpilepsyJareena BegumBelum ada peringkat
- 1siras 1Dokumen16 halaman1siras 1Venkatesan VidhyaBelum ada peringkat
- Pathophysio DHF EDITEDDokumen3 halamanPathophysio DHF EDITEDricmichael100% (1)
- Health: Quarter 1 - Module 1: Community and Environmental HealthDokumen24 halamanHealth: Quarter 1 - Module 1: Community and Environmental Healthma kathrine cecille macapagal100% (1)
- Principles of Epidemiology - Lesson 1 - Section 7Dokumen3 halamanPrinciples of Epidemiology - Lesson 1 - Section 7Faria bukhariBelum ada peringkat
- Ayliffes Control of Healthcare-Associated Infection A Practical Handbook PDFDokumen521 halamanAyliffes Control of Healthcare-Associated Infection A Practical Handbook PDFAbidi Hichem100% (1)