8.3 Medicine - Tropical Infectious Diseases Leptospirosis 2014A
Diunggah oleh
Bhi-An BatobalonosJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
8.3 Medicine - Tropical Infectious Diseases Leptospirosis 2014A
Diunggah oleh
Bhi-An BatobalonosHak Cipta:
Format Tersedia
(Missed lecture)
Tropical Infectious
Diseases:
Dra. Rosario
I.
II.
III.
Outline
Introduction: Case 4
Leptospirosis
A. Pathogenesis
B. Transmission
C. Leptospirosis in the Philippines
D. Clinical manifestations
Weils Disease
E. Treatment
F.
Laboratory Diagnosis
G. Prognosis
H. Prevention
Key Concepts
CASE 4
A 28 year-old male, a government employee
consulted the ER because of fever, jaundice, and
oliguria
o Reported abdominal and leg pains
o Wading in floodwater 2 weeks ago
PE: BP=120/90; HR=100/min; RR=26/min; T=39C
With conjunctival suffusion, icteric sclerae
Breath sounds clear
No abnormal heart sounds
Voluntary abdominal guarding; LS: 12 cms; Traube
space obliterated
Calf muscle tenderness
Primary Impression?
1. Dengue fever
2. Enteric fever
3. Malaria
4. Leptospirosis
ISSUES
Early clinical recognition and diagnosis
Management of complications
Prevention and control
LEPTOSPIROSIS
Zoonotic disease caused by spirochetes of the
genus Leptospira
o Thin, flexible, finely coiled, Gram-negative
bacteria
o Obligately aerobic, slow-growing, fastidious
Reservoir: Wild and domestic animals
Human infection acquired through direct contact
with infected animals or by contact with water/soil
contaminated by infected urine
Leptospires are tightly and regularly coiled, with
characteristic hooked ends and are highly motile,
spinning around their longitudinal axis and darting back
and forth [Harrisons]
Leptospira interrogans var. icterohaemorrhagiae
on EM
Question: What is the primary underlying problem in
Leptospirosis?
1. Toxin secretion
2. Invasion of reticulo-endothelial system
3. Hypersensitivity reaction to leptospiral
antigens
4. Systemic vasculitis
Ang, Angulo, Aover; Edited by Aover
PATHOGENESIS
Proliferation in bloodstream and spread to distant
organs
No tissue tropism
Capillary leakage and hemorrhage due to
disruption of endothelial cell membrane (systemic
vasculitis)
o Accounts for broad spectrum of clinical
illness
Leptospires infect humans through the mucosa/abraded
skin. The organism will resist innate immune defenses
and proliferate in the bloodstream or extracellularly
within organs, and then disseminate hematogenously to
all organs. Incubation period averages 5-14 days.
Life cycle will be completed as leptospires traverse the
interstitial space of the kidney, penetrate the basement
membrane of the proximal renal tubules, cross through
proximal renal tubuloepithelial cells, and become
adherent to the proximal renal tubular brush border,
whence they are excreted in the urine. In humans,
colonization can last up to years, with unknown
pathophysiologic consequences[Harrisons]
TRANSMISSION OF LEPTOSPIROSIS
Epidemics common after natural disasters in
endemic areas (flooding, tropical storms,
hurricanes)
Risk factors:
o Walking through streams, creeks, puddles
o Swimming, kayaking, white-water rafting
o Exposure to rodents
Factors that facilitate human infection are those that
bring susceptible persons into indirect contact with
contaminated animal urine through surface waters, moist
soil or other wet environments or into direct contact with
urine and other excreta of infected animals. [Harrisons]
LEPTOSPIROSIS IN THE PHILIPPINES
Average of 680 cases and 40 deaths reported every
year
Prevalence of 10/100,000
Page 1 of 7
Seasonal; peak incidence during the rainy
months of July to October
Urban domestic rats, rural field rats,
water buffalo, cattle, pigs, dogs and
monkeys: tested positive for leptospiral
antibodies
October 2009 Outbreak
Declared by DOH two weeks after widespread
flooding caused by Tropical Storm Ondoy
(Sept. 26, 2009)
Average: 680 cases and 40 deaths per year
As of 13 November 2009: 2,292 suspected
cases (257 confirmed) and 178 deaths (CFR
7.4%) in 15 hospitals in Metro Manila
Figure 2
Classic leptospirosis is usually biphasic. Initial
Leptospiremic phase with acute fever lasting for 310 days, wherein the organism may still be cultured
from blood. Later Immune phase, fever will be
unresponsive to antibiotics, but leptospires can be
isolated from urine. [Harrisons]
Weils Syndrome can be monophasic and
fulminant. [Harrisons]
Severe Leptospirosis: Weils Disease
Rapidity of progression to fulminant illness is
variable
Fatality rate: ranges from 5-40%
Highly dependent on severity of illness caused
by different serovars and quality of supportive
medical care
Weils Disease is characterized by variable
combinations of jaundice, acute kidney injury,
hypotension and hemorrhage, most commonly in the
lungs.[Harrisons]
Question: What is the pathophysiologic
mechanism of hepatic failure in Weils disease?
1. Hepatocyte degeneration
2. Centrilobular necrosis
3. Periportal necrosis
4. 2 and 3 only
Figure 1. Showing increased incidence of
leptospirosis cases in 2009
CLINICAL MANIFESTATIONS
Subclinical manifestation with subsequent
seroconversion
Two clinical syndromes:
o 90%: self-limited, systemic illness
o 10%: severe, potentially fatal illness
characterized by renal and hepatic
failure and pneumonitis with a
hemorrhagic diathesis (Weils
disease)
Hepatic Failure in Weils Disease
Results from hepatocyte degeneration with
cholestasis and concomitant vascular injury
Hepatosplenomegaly (>25% of icteric
patients)
Bilirubin: normal or slightly increased
(<20mg/dL), peak by day 7 in 85% of patients
o Fulminant disease (>80mg/dL)
AST, ALT rarely >200 U/L, Inc. PT rare
Hepatocellular necrosis is absent
Hepatic histopathology in fatal cases is associated
with disruption of cellular cohesion, plugging of bile
canaliculi, occasional acute inflammatory infiltrates,
and focal periportal cellular necrosis and steatosis.
Widespread hepatocellular necrosis is NOT FOUND.
[Harrisons]
Question: What is the primary pathophysiologic
mechanism of renal failure in Weils disease?
1. Renovascular obstruction
2. Rapidly progressive glomerulonephritis
3. Interstitial nephritis
4. Diffuse acute tubular necrosis
Renal Failure in Weils Disease
Hallmarks: impaired sodium reabsorption,
increased distal sodium delivery, and K+
wasting
Rapid onset of uremia, oliguria (2nd week)
If with thrombocytopenia (even without DIC) or
anuria poor prognosis
BUN: Usually <100, may be >300mg/dL
Ang, Angulo, Aover; Edited by Aover
of 7
Page 2
Creatinine: Usually 2-8, may be >18mg/dL
Biopsy: interstitial nephritis with focal ATN
Leptospirosis and Renal Failure
o Leptospirosis can account for up to
40% of cases of acute renal failure in
Asia (Sitprija et al. 1975)
o Correlates well with prognosis (Marcial
M, Phil J Microbiol Infect Dis 1995)
Oliguria and need for dialysis
Hemorrhage
Duration of jaundice
Acute kidney injury manifests after several days of
illness and can be nonoliguric or oliguric, with serum
electrolyte abnormalities reflecting proximal renal
tubular dysfunction. Hypokalemia and
hypomagnesemia are common in nonoliguric renal
failure. Hypotension is associated with acute tubular
necrosis and oliguria. Renal function typically returns
to normal in survivors of severe disease [Harrisons]
Cardiopulmonary Dysfunction in Weils Disease
Hemorrhagic pneumonitis, ARDS: seen in
severe infection
o CXR: multiple patchy infiltrates =
suggestive of alveolar haemorrhage
Mainly due to widespread vasculitis
Worsened by impaired hepatic production of
coagulation factors
Aggravates existing jaundice and further
compromises renal function
Question: Which patient will need hospital
admission?
1. Outpatient (Mild LEPTOSPIROSIS)
Any suspected case of leptospirosis presenting
with acute febrile illness and various
manifestations BUT
o Stable vital signs
o Anicteric sclerae
o With good urine output
o No evidence of
meningismus/meningeal irritation,
sepsis/septic shock, difficulty of
breathing nor jaundice
o Can take oral medications (Grade A)
2. Healthcare/Hospital Setting (Moderate to
Severe)
Any suspected case of leptospirosis presenting
with acute febrile illness associated with
o Unstable vital signs
o Jaundice/icteric sclerae
o Abdominal pain, nausea, vomiting and
diarrhea
o Oliguria and anuria
o Meningismus, meningeal irritation
o Sepsis/septic shock
o Altered mental states
o Difficulty of breathing and hemoptysis
TREATMENT OF LEPTOSPIROSIS
Figure 3. Pulmonary hemorrhage in Leptospirosis
Cardiac arrhythmias in up to 20% of patients;
may progress to cardiovascular collapse with
shock
Histopath: Pulmonary congestion and intraalveolar hemorrhage with severe airspace
disorganization; myocarditis; acute coronary
arteritis and aortitis
Severe pulmonary hemorrhage in leptospirosis is a
clinical problem, manifesting with cough, chest pain,
and hemoptysis but without purulent sputum. Cases
of severe pulmonary hemorrhage syndrome that
come to autopsy are characterized by the absence
of inflammation, the paucity of organisms visible by
silver or immunohistochemical staining, and grossly
obvious frank hemorrhage. Immunoglobulin and
complement deposition have been demonstrated in
lung tissue involved in leptospiral pulmonary
hemorrhage.
Cardiac involvement is commonly reflected on the
electrocardiogram as nonspecific ST and T wave
changes but also as right-bundle-branch block and
right- and/or left-sided ventricular dilation indicating
myocarditis. [Harrisons]
MILD LEPTOSPIROSIS:
Hemorrhagic Diathesis
Ang, Angulo, Aover; Edited by Aover
of 7
Page 3
of this trans included in the
powerpoint)
Mild leptospirosis often is not specifically identified and
typically resolves without antibiotic treatment. If clinical
suspicion is high or the diagnosis is suggested or
confirmed by laboratory findings in an appropriate
context (e.g., clinical presentation, exposure history);
mild disease should be treated with oral antibiotics
particularly, doxycycline. [Harrisons]
When Would You Suspect Pulmonary
Complications of Leptospirosis?
Tachypnea (RR>30/min) is the first sign of
pulmonary involvement
One should consider lung involvement:
o Onset of cough
o Hemoptysis
o Dyspnea
Pulmonary symptoms usually appear on the
4th-6th day of disease
Pulmonary complications in Leptospirosis:
MODERATE TO SEVERE LEPTOSPIROSIS:
Dosage of Antibiotics in ADULTS WITH RENAL
IMPAIRMENT:
What Are the Indications for Acute Renal
Replacement Therapy or Dialysis?
Any one of the following is an indication for
dialysis:
o Uremic symptoms nausea, vomiting,
altered mental status, seizure, coma
o Serum creatinine >3mg/dL
o Serum K >5meq/L in an oliguric
patient
o ARDS, pulmonary hemorrhage
o pH <7.2
o Fluid overload
o Oliguria despite measures following
the algorithm (see figure at the end
Ang, Angulo, Aover; Edited by Aover
of 7
Which Patients Will Need Admission to the
Intensive Care Unit?
A management-oriented approach should be
utilized in the decision to determine the site of
care for patients
ICU admission is needed:
o Tachypnea
o Chest x-ray findings of localized or
multilobar infiltrates or pleural effusion
o Moderate to severe hypoxemia
What is the Role of Steroids in Pulmonary
Complications of Leptospirosis?
Bolus methyl prednisone given within the first
12 hours of onset of respiratory involvement
Methylprednisone should be given at a dose of
1gm IV/day for 3 days followed by oral
prednisolone 1mg/kg/day for 7 days
LABORATORY DIAGNOSIS OF LEPTOSPIROSIS
Direct Detection Method
1. Dark-field
microscopy/immunofluorescence/light
microscopy
Sensitive during the first 7-10 days of the
acute illness
Histopathological stains and
immunohistochemical leptospires in tissues
Direct examination of urine or blood by dark-field
microscopy has the potential to provide a rapid
Page 4
2.
diagnosis but is not recommended because of
complicating artifacts [Harrisons]
Culture and isolation
Remains the GOLD standard
Requires 6 to 8 weeks for the result
Can identify the serovar but is insensitive
Requires biosafety level II facility
Leptospires can be cultured from blood and CSF
during the first 710 days of illness and from urine
beginning in the second week. Cultures usually
become positive after 24 weeks (range, 1 week to 6
months). Urine cultures can remain positive for
months or years despite antibiotic therapy
[Harrisons]
3. Polymerase Chain Reaction (PCR)
Has the advantage of early confirmation of the
acute leptospiremic phase
Currently not generally available because of
the cost-limiting nature of the test and the
need for trained personnel
Indirect Detection Method
1. Microagglutination Test (MAT)
A four-fold rise of the titer from acute to
convalescent sera is confirmatory of the
diagnosis
Highly sensitive and specific BUT timeconsuming
Cross-reactions may occur with syphilis, viral
hepatitis, HIV, relapsing fever, Lyme disease,
legionellosis and autoimmune diseases
A single titer of at least 1:1600 in
symptomatic patients is indicative of
leptospirosis
A positive MAT result reflects the presence only of
Leptospira-specific antibodies and cannot be used to
precisely identify the infecting serovar because one
serovar may induce antibodies that cross-react with
other serovars. When patients have a high pretest
probability of leptospirosis, a single antibody titer
>1:200 is considered strong evidence of infection;
however, in regions where leptospirosis transmission
and subclinical disease are common, higher titers
are generally required for a confident diagnosis
because of long-lasting antibodies after a previous
infection. Because the MAT is generally negative in
the first 710 days after the onset of infection,
paired acute- and convalescent-phase serum
samples are preferred to document seroconversion
or a fourfold rise in titer. [Harrisons]
2. Specific IgM Rapid Diagnostic Tests
(LeptoDipstick, Leptospira IgM ELISA
(PanBio), MCAT and Dridot)
Serologic tests in a single test format
Quick detection of Leptospira genus-specific
IgM antibodies
Sensitivity improves if taken beyond 7 days
(>90%)
3. Nonspecific Rapid Diagnostic Tests like
LAATS (Leptospira Antigen-Antibody
Agglutination Test (Leptospira Serology BioRad)
Ang, Angulo, Aover; Edited by Aover
of 7
Detects Leptospira antibody in human serum
through agglutination reaction
Used as a screening test and should be
confirmed with MAT
PROGNOSIS
Case fatality rate of about 10% in severe cases
Dependent on several factors
o Timely administration of effective
chemotherapeutic agents
o Quality of supportive care provided
o Virulence of infecting serovar
o Severity of the disease on admission
o Presence of co-morbidities
Adverse Prognostic Factors
Strongest predictor of death: Altered mental
status
Other poor prognostic signs:
o Acute renal failure (oliguria,
hyperkalemia, serum creatinine
>3.0mg/dL)
o Respiratory insufficiency (dyspnea,
pulmonary rales, CXR infiltrates)
o Hypotension
o Arrhythmias
**Hepatic failure alone (without renal failure)
rarely leads to a fatal outcome
The severity of illness in terms of pulmonary and
renal dysfunction is the most important determinant
of prognosis. Advanced age, clinically evident
pulmonary involvement, elevated serum creatinine
level, oliguria, and thrombocytopenia are associated
with a poor prognosis. [Harrisons]
PREVENTION
Avoid exposure
Chemoprophylaxis?
Antibiotic Prophylaxis for Leptospirosis
The most effective preventive measure is
avoidance of high-risk exposure
Pre-exposure antibiotic prophylaxis is NOT
ROUTINELY RECOMMENDED
Recommended regimen for pre-exposure
prophylaxis for non-pregnant, non-lactating
adults:
o Doxycycline 200mg once weekly (to
begin 1 to 2 days before exposure and
continued throughout the period of
exposure [Grade B])
Recommended Post-Exposure Prophylaxis for
Leptospirosis
Page 5
KEY CONCEPTS
Tropical infectious diseases usually occur,
but not exclusively, in developing countries
with warmer climates
Formulate a diagnosis of microbial infection
based on clinical and epidemiologic evidence,
supported by laboratory examinations
Inexpensive and effective medications are
available to treat most tropical infectious
diseases
Cost, as well as antimicrobial resistance, can
become a barrier to effective treatment
Adequate supportive measures are necessary,
to prevent complications and mortality
o Host factors, including the severity of
the illness and co-morbid conditions,
as well as the intervention-related
factors, are important to consider in
the overall management
Many tropical infections are preventable by
means of simple, inexpensive, and currently
available methods
Algorithm for the MANAGEMENT OF
OLIGURIA IN LEPTOSPIROSIS
Ang, Angulo, Aover; Edited by Aover
of 7
Page 6
(Missed lecture)
Getting Sick in the
Tropics
Dra. Rosario
Ang, Angulo, Aover; Edited by Aover
Page 7 of 7
Anda mungkin juga menyukai
- Urinary Tract Infection in Children - Classification, Diagnosis and TreatmentDari EverandUrinary Tract Infection in Children - Classification, Diagnosis and TreatmentBelum ada peringkat
- Leptospirosis: Dr. Doni Priambodo Wijisaksono, Sppd-KptiDokumen33 halamanLeptospirosis: Dr. Doni Priambodo Wijisaksono, Sppd-KptialbaazaBelum ada peringkat
- Leptospirosis (Weil's Disease) : EpidemiologyDokumen4 halamanLeptospirosis (Weil's Disease) : EpidemiologyaudyodyBelum ada peringkat
- LeptospirosisDokumen10 halamanLeptospirosisrommel f irabagonBelum ada peringkat
- Leptospirosis (Weil's Disease) : EpidemiologyDokumen4 halamanLeptospirosis (Weil's Disease) : EpidemiologyTio Prima SBelum ada peringkat
- Leptospirosis: Nurul Hidayu - Nashriq Aiman - Audi AdibahDokumen28 halamanLeptospirosis: Nurul Hidayu - Nashriq Aiman - Audi AdibahAkshay D'souzaBelum ada peringkat
- 012 LeptospirosisDokumen8 halaman012 LeptospirosisSkshah1974Belum ada peringkat
- Lepto SpirosDokumen6 halamanLepto SpirosMar OrdanzaBelum ada peringkat
- Pemicu 3Dokumen15 halamanPemicu 3iche_lovemeBelum ada peringkat
- Case Study Leptospirosis PowerpointDokumen17 halamanCase Study Leptospirosis Powerpointbeancent100% (2)
- Leptospirosis in ChildrenDokumen5 halamanLeptospirosis in ChildrenPramod KumarBelum ada peringkat
- Leptospirosis FinalDokumen5 halamanLeptospirosis FinalufrieBelum ada peringkat
- Fever With Jaundice and A Purpuric RashDokumen4 halamanFever With Jaundice and A Purpuric RashRaida Uceda GarniqueBelum ada peringkat
- Acute Febrile IllnessesDokumen54 halamanAcute Febrile IllnessesfraolBelum ada peringkat
- Medscape LeptospirosisDokumen26 halamanMedscape LeptospirosisEBNY MOBA & PUBG Mobile GamingBelum ada peringkat
- Acute Fulminent Leptospirosis With Multi-Organ Failure: Weil's DiseaseDokumen4 halamanAcute Fulminent Leptospirosis With Multi-Organ Failure: Weil's DiseaseMuhFarizaAudiBelum ada peringkat
- Case 1Dokumen4 halamanCase 1Irsanti SasmitaBelum ada peringkat
- Causes of Drowsiness in This PatientDokumen12 halamanCauses of Drowsiness in This PatientNu JoeBelum ada peringkat
- Leptospirosis - Clinical Aspects - PMCDokumen9 halamanLeptospirosis - Clinical Aspects - PMCJhimy Eraldo Alfaro LopezBelum ada peringkat
- Liver AbscessDokumen6 halamanLiver AbscessKenneth SunicoBelum ada peringkat
- Lepto Spiros IsDokumen7 halamanLepto Spiros IslansoprazoleBelum ada peringkat
- Fever Synonym:: Modes of TransmissionDokumen6 halamanFever Synonym:: Modes of TransmissionEjie Boy IsagaBelum ada peringkat
- And-Asses-At-Spring-Break-Pt-1-3/?from VBWN: LeptospirosisDokumen8 halamanAnd-Asses-At-Spring-Break-Pt-1-3/?from VBWN: LeptospirosisEjie Boy IsagaBelum ada peringkat
- Salmonella InfectionsDokumen3 halamanSalmonella InfectionsYolanda Dwi OktaviyaniBelum ada peringkat
- Lapkas Dalam Nefro AyuhatiDokumen13 halamanLapkas Dalam Nefro Ayuhatix22xBelum ada peringkat
- LepsDokumen4 halamanLepslynharee100% (1)
- LeptospirosisDokumen7 halamanLeptospirosisFarah Nadia MoksinBelum ada peringkat
- Leptospirosis: A Case Study: Mathew SullivanDokumen3 halamanLeptospirosis: A Case Study: Mathew SullivanSagara MaheshBelum ada peringkat
- Anak 1Dokumen4 halamanAnak 1Vega HapsariBelum ada peringkat
- 7 - LeptospirosisDokumen18 halaman7 - LeptospirosisCAÑADA, JOHANNELYN M.Belum ada peringkat
- Leptospirosis, Typhoid and Other FeversDokumen37 halamanLeptospirosis, Typhoid and Other FeverskarageeBelum ada peringkat
- Leptospirosis by MedlineDokumen4 halamanLeptospirosis by MedlineniabustamBelum ada peringkat
- 伤寒英文教案 Typhoid Fever-应若素Dokumen36 halaman伤寒英文教案 Typhoid Fever-应若素Wai Kwong ChiuBelum ada peringkat
- Leptospirosis: Where Is Leptospirosis Found?Dokumen4 halamanLeptospirosis: Where Is Leptospirosis Found?Ariffe Ad-dinBelum ada peringkat
- Acute GlomerulonephritisDokumen4 halamanAcute GlomerulonephritisJulliza Joy PandiBelum ada peringkat
- Leptospirosis: Interrogans, Pomona, Icterohaemorrhagiae, Canicola, and AutumnalisDokumen5 halamanLeptospirosis: Interrogans, Pomona, Icterohaemorrhagiae, Canicola, and AutumnalisAlina CebanBelum ada peringkat
- What Is LeptospirosisDokumen18 halamanWhat Is LeptospirosisLuphly TaluvtaBelum ada peringkat
- Leptospirosis ReadDokumen26 halamanLeptospirosis ReadAngeline SoepartoBelum ada peringkat
- LeptospirosisDokumen9 halamanLeptospirosisDeepu VijayaBhanuBelum ada peringkat
- Leptospirosis: Causes, Incidence, and Risk FactorsDokumen6 halamanLeptospirosis: Causes, Incidence, and Risk FactorsJackii DoronilaBelum ada peringkat
- Henoch - Schonlein Purpura (HSP) : - It Is The Most Common Cause of Non-Thrombocytopenic Purpura in ChildrenDokumen23 halamanHenoch - Schonlein Purpura (HSP) : - It Is The Most Common Cause of Non-Thrombocytopenic Purpura in ChildrenLaith DmourBelum ada peringkat
- Thypoid - RPUDokumen22 halamanThypoid - RPUERONADIAULFAH SUGITOBelum ada peringkat
- 68 JMSCRDokumen3 halaman68 JMSCRVani Junior LoverzBelum ada peringkat
- 4th Grand CPC ScriptDokumen3 halaman4th Grand CPC ScriptEunice RiveraBelum ada peringkat
- CholangitisDokumen15 halamanCholangitisFaye TanBelum ada peringkat
- P 04-LeptospirosisDokumen2 halamanP 04-LeptospirosisRaymund AldabaBelum ada peringkat
- HepatitisDokumen24 halamanHepatitisEric PeprahBelum ada peringkat
- LeptospirosisDokumen10 halamanLeptospirosisjramos11067920Belum ada peringkat
- Amoebic Liver Abscess: Clinical MedicineDokumen5 halamanAmoebic Liver Abscess: Clinical MedicineAizat KamalBelum ada peringkat
- Leptospirosis - Policy Guide by PhilhealthDokumen6 halamanLeptospirosis - Policy Guide by PhilhealthKathrina AbastarBelum ada peringkat
- Physiology of HyperbilirubinemiaDokumen6 halamanPhysiology of HyperbilirubinemiaAdiel OjedaBelum ada peringkat
- 2 Renal Tubular, Interstitial Disease 2Dokumen94 halaman2 Renal Tubular, Interstitial Disease 2Coy NuñezBelum ada peringkat
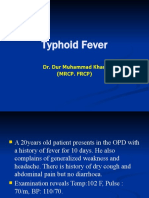
- Typhoid Fever: Dr. Dur Muhammad Khan (Mrcp. FRCP)Dokumen52 halamanTyphoid Fever: Dr. Dur Muhammad Khan (Mrcp. FRCP)Osama HassanBelum ada peringkat
- A Case HistoryDokumen43 halamanA Case Historymel_pusagBelum ada peringkat
- Intern TicklerDokumen10 halamanIntern TicklerRem AlfelorBelum ada peringkat
- Lower Respiratory Tract InfectionDokumen21 halamanLower Respiratory Tract InfectionJohn Vincent Dy OcampoBelum ada peringkat
- Karnik Indian Journal Critical Care Medecine 2021 Leptospirosis in ICUDokumen4 halamanKarnik Indian Journal Critical Care Medecine 2021 Leptospirosis in ICUBCR ABLBelum ada peringkat
- Salmonella Typhi and Salmonella Paratyphi Are The Causative Agents of Typhoid FeverDokumen15 halamanSalmonella Typhi and Salmonella Paratyphi Are The Causative Agents of Typhoid FeverfitrianugrahBelum ada peringkat
- Referat SepsisDokumen18 halamanReferat SepsisImelva GirsangBelum ada peringkat
- Pedia Census: Ruby Anne D. BatobalonosDokumen57 halamanPedia Census: Ruby Anne D. BatobalonosBhi-An BatobalonosBelum ada peringkat
- Pre-Operative Conference Anesthetic Considerations For Laryngectomy and Total Thyroidectomy in GeriatricsDokumen4 halamanPre-Operative Conference Anesthetic Considerations For Laryngectomy and Total Thyroidectomy in GeriatricsBhi-An BatobalonosBelum ada peringkat
- Sepsis M&MDokumen20 halamanSepsis M&MBhi-An BatobalonosBelum ada peringkat
- Anesthetic Implications of Guillain-Barre Syndrome in PregnancyDokumen34 halamanAnesthetic Implications of Guillain-Barre Syndrome in PregnancyBhi-An BatobalonosBelum ada peringkat
- Pedia Census 5Dokumen62 halamanPedia Census 5Bhi-An BatobalonosBelum ada peringkat
- Preop Conference AnesthesiaDokumen33 halamanPreop Conference AnesthesiaBhi-An BatobalonosBelum ada peringkat
- Pedia Census ArrythmiaDokumen48 halamanPedia Census ArrythmiaBhi-An BatobalonosBelum ada peringkat
- ResearchDokumen21 halamanResearchBhi-An BatobalonosBelum ada peringkat
- Blunt Trauma Abdomen: (Operative V/S Conservative Management)Dokumen41 halamanBlunt Trauma Abdomen: (Operative V/S Conservative Management)Bhi-An BatobalonosBelum ada peringkat
- Census - High SpinalDokumen30 halamanCensus - High SpinalBhi-An BatobalonosBelum ada peringkat
- Diificult AirwayDokumen13 halamanDiificult AirwayBhi-An BatobalonosBelum ada peringkat
- Anesthetic Management of Non-Fasted Patients Requiring Emergency SurgeryDokumen17 halamanAnesthetic Management of Non-Fasted Patients Requiring Emergency SurgeryBhi-An BatobalonosBelum ada peringkat
- Ancient Dental PracticesDokumen1 halamanAncient Dental PracticesBhi-An BatobalonosBelum ada peringkat
- Anes Reporting - Chronic PainDokumen60 halamanAnes Reporting - Chronic PainBhi-An BatobalonosBelum ada peringkat
- Gynecology Abnormal Bleeding 2014aDokumen8 halamanGynecology Abnormal Bleeding 2014aBhi-An BatobalonosBelum ada peringkat
- Annex B. School Level Report On The 3rd Quarter NSEDDokumen3 halamanAnnex B. School Level Report On The 3rd Quarter NSEDMaria Claret alcazarBelum ada peringkat
- Establishing The Legal Framework of Telehealth in The PhilippinesDokumen10 halamanEstablishing The Legal Framework of Telehealth in The Philippineshazell_aseronBelum ada peringkat
- Immunization HandbookDokumen200 halamanImmunization Handbooktakumikuroda100% (1)
- Paired Facial Treatment With 755nm Picosecond Laser With Diffractive Lens Array and 1060nm Laser Lipolysis of The Submentum - An Open-Label Prospective TriaDokumen7 halamanPaired Facial Treatment With 755nm Picosecond Laser With Diffractive Lens Array and 1060nm Laser Lipolysis of The Submentum - An Open-Label Prospective TriaErik BrooksBelum ada peringkat
- Activity 26 Assessment and Care of Antenatal Woman Ante Natal Case Record - 2Dokumen5 halamanActivity 26 Assessment and Care of Antenatal Woman Ante Natal Case Record - 2A J FathimaBelum ada peringkat
- Pretibial LacsDokumen8 halamanPretibial LacsMiguel JohnsonBelum ada peringkat
- Free Online Courses WebsitesDokumen27 halamanFree Online Courses Websitespervez4356Belum ada peringkat
- Aap MCQ 2007Dokumen537 halamanAap MCQ 2007Kriti Gupta100% (4)
- Assignment On-: "Pharmacokinetics of Drug Molecules in Different Disease Condition"Dokumen19 halamanAssignment On-: "Pharmacokinetics of Drug Molecules in Different Disease Condition"Susmoy SinhaBelum ada peringkat
- Evidence Based Physical Therapy, 2nd EditionDokumen240 halamanEvidence Based Physical Therapy, 2nd EditionJason100% (1)
- Cultural Competence or Cultural Humility Moving Beyond The DebateDokumen4 halamanCultural Competence or Cultural Humility Moving Beyond The DebateEstela MedinaBelum ada peringkat
- Caesarean Section at Full Dilatation: Incidence, Impact and Current ManagementDokumen20 halamanCaesarean Section at Full Dilatation: Incidence, Impact and Current ManagementAbdur RaheemBelum ada peringkat
- Acute PancreatitisDokumen40 halamanAcute PancreatitisAbdulsalam DostBelum ada peringkat
- Verify Category B2 Report V6.35 Rev 1.0Dokumen39 halamanVerify Category B2 Report V6.35 Rev 1.0Roger SchulpBelum ada peringkat
- Lect 3 Trauma CounsellingDokumen28 halamanLect 3 Trauma Counsellingumibrahim75% (8)
- 7 Habits of Highly Effective PeopleDokumen15 halaman7 Habits of Highly Effective Peopleshanocampo30Belum ada peringkat
- Vasculitis When To Consider This DiagnosisDokumen15 halamanVasculitis When To Consider This DiagnosisAndres PortesBelum ada peringkat
- Jaa 178927 Approaches To The Assessment of Severe Asthma Barriers and PDFDokumen17 halamanJaa 178927 Approaches To The Assessment of Severe Asthma Barriers and PDFNikki LangatoBelum ada peringkat
- Preparation For Child BirthDokumen41 halamanPreparation For Child BirthAngelica ErguizaBelum ada peringkat
- Intradermal Delivery Vaccines Report 2009 SeptDokumen94 halamanIntradermal Delivery Vaccines Report 2009 SeptSantoso CokroBelum ada peringkat
- Spinal Cord Injury Rehabilitation Webinar 2020 PDFDokumen2 halamanSpinal Cord Injury Rehabilitation Webinar 2020 PDFGirijashankar KhuntiaBelum ada peringkat
- Thesis About Quack DoctorsDokumen22 halamanThesis About Quack DoctorsJervyn Guianan100% (3)
- CORAD 101, Health and Welfare ProgramsDokumen5 halamanCORAD 101, Health and Welfare ProgramsdaybudsvaldezBelum ada peringkat
- Major Haemorrhage ProtocolDokumen2 halamanMajor Haemorrhage ProtocollaurenBelum ada peringkat
- Research ProposalDokumen6 halamanResearch ProposalAhmad NajjarBelum ada peringkat
- Constructing A Nursing Budget Using A Pateint Classification SystemDokumen3 halamanConstructing A Nursing Budget Using A Pateint Classification SystemRhey March100% (1)
- TP Integrador Inglés Técnico IDokumen5 halamanTP Integrador Inglés Técnico ITaborga Pereira WillansBelum ada peringkat
- Systemic Review On The Use of Diclofenacb Complex As An Antiinflammatorytreatment With Pain Relief Effect For Patients With Acute Lower Back Pain 2167 0846 1000216Dokumen5 halamanSystemic Review On The Use of Diclofenacb Complex As An Antiinflammatorytreatment With Pain Relief Effect For Patients With Acute Lower Back Pain 2167 0846 1000216Dhea Yulia LubisBelum ada peringkat
- An Overview of The Role of Nurses and Midwives in Leadership and Management in EuropeDokumen44 halamanAn Overview of The Role of Nurses and Midwives in Leadership and Management in EuropeTCBelum ada peringkat
- Vasopressors For ShockDokumen21 halamanVasopressors For ShocknugrahaBelum ada peringkat