Gastrointestinal Bleeding PDF
Diunggah oleh
ArdieJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Gastrointestinal Bleeding PDF
Diunggah oleh
ArdieHak Cipta:
Format Tersedia
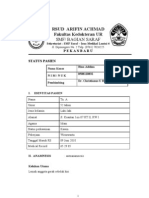
ORIGINAL ARTICLE
Safety and Efficacy of Lansoprazole Injection
in Upper Gastrointestinal Bleeding:
a Postmarketing Surveillance Conducted in Indonesia
Ari F. Syam1, Arini Setiawati2,3
Department of Internal Medicine, Faculty of Medicine, University of Indonesia-Cipto Mangunkusumo Hospital,
Jakarta, Indonesia. 2 Clinical Study Unit, Faculty of Medicine, University of Indonesia, Jakarta, Indonesia.
3
Department of Pharmacology and Therapeutics, Faculty of Medicine, University of Indonesia, Jakarta, Indonesia.
1
Correspondence mail:
Division of Gastroenterology, Department of Internal Medicine, Faculty of Medicine, University of Indonesia-Cipto
Mangunkusumo Hospital. Jl. Diponegoro no. 71, Jakarta 10430, Indonesia. email: arisyam91@yahoo.com.
ABSTRAK
Tujuan: untuk menilai keamanan dan efikasi dari injeksi lansoprazole (Prosogan) pada pasien dengan
perdarahan gastrointestinal atas (UGIB) akibat ulkus peptikum atau gastritis erosiva. Metode: suatu studi
observasional pasca-pemasaran lansoprazol injeksi. Pasien dengan UGIB akibat ulkus peptikum atau gastritis
erosiva diberi lansoprazol injeksi selama maksimal 7 hari atau sampai perdarahan berhenti dan pasien dapat
minum lansoprazol oral. Outcome primer studi ini adalah berhentinya perdarahan. Beberapa parameter
laboratorium juga diukur. Hasil: sejumlah 204 pasien dapat dinilai keamanannya, dan tidak ada kejadian tidak
diinginkan yang dilaporkan selama studi. Sejumlah 200 pasien dapat dinilai efikasinya, 125 pasien di antaranya
adalah pasien laki-laki. UGIB berhenti pada 20 pasien (10%) pada hari pertama, 71 pasien (35,5%) pada hari
ke-2, 75 pasien (37,5%) pada hari ke-3, 24 pasien (12,0%) pada hari ke-4, dan 7 pasien (3,5%) pada hari ke-5,
total 197 pasien (98,5%) pada hari ke-5. Efek hemostatik ini dinilai baik sekali jika perdarahan berhenti dalam
waktu 3 hari dan baik jika perdarahan berhenti dalam waktu 5 hari. Dengan demikian hasilnya baik sekali pada
166 pasien (83,0%) dan baik pada 31 pasien (15,5%). Hasil ini tidak berbeda antara laki-laki dan perempuan,
antara umur di bawah 60 tahun dan 60 tahun ke atas, dan antara Hb awal di bawah 10 g/dL dan 10 g/dL ke atas.
Kesimpulan: hasil studi observasional pasca pemasaran pada 200 pasien dengan UGIB akibat ulkus peptikum
atau gastritis erosiva ini menunjukkan bahwa lansoprazol intravena dua kali sehari aman dan sangat efektif.
Kata kunci: survei pasca-pemasaran, lansoprazole, perdarahan saluran cerna bagian atas.
ABSTRACT
Aim: to assess the safety and effectiveness of lansoprazole injection (Prosogan) in patients with upper
gastrointestinal bleeding due to peptic ulcers or erosive gastritis. Methods: this study was a multicenter observational
postmarketing study of lansoprazole (Prosogan) injection. Patients with upper gastrointestinal bleeding due
to peptic ulcers or erosive gastritis were given intravenous lansoprazole for a maximum of 7 days or until the
bleeding stopped and the patients were able to take oral doses of lansoprazole. Primary outcome of the study was
cessation of bleeding. Some laboratory parameters were also measured. Results: among a total of 204 patients
evaluable for safety, there was no adverse event reported during the study. A total of 200 patients were eligible
for efficacy evaluation, 125 patients (62.5%) were males. Among these patients, upper GI bleeding stopped in 20
patients (10.0%) on day 1, in 71 patients (35.5%) on day 2, 75 patients (37.5%) on day 3, 24 patients (12.0%)
on day 4, and 7 patients (3.5%) on day 5, making a cumulative of 197 patients (98.5%) on day 5. The hemostatic
Acta Medica Indonesiana - The Indonesian Journal of Internal Medicine
123
Ari F. Syam
Acta Med Indones-Indones J Intern Med
effect was rated as excellent if the bleeding stopped within 3 days, and good if the bleeding stopped within 5
days. Thus, the results were excellent in 166 patients (83.0%) and good in 31 patients (15.5%). These results
were not different between males and females, between age below 60 years and 60 years and above, and between
baseline Hb below 10 g/dL and 10 g/dL and above. Conclusion: the results of this observational postmarketing
study in 200 patients with upper gastrointestinal bleeding due to peptic ulcers or erosive gastritis demonstrated
that intravenous lansoprazole twice a day was well tolerated and highly effective.
Key words: postmarketing surveillance (PMS), lansoprazole, upper gastrointestinal bleeding (UGIB).
INTRODUCTION
Upper gastrointestinal bleeding (UGIB) is a
severe life-threatening disease with a mortality
rate that has remained constant at 5 to 10%,
over the past 50 years.1 Peptic ulcer is the most
common cause of UGIB, accounting for about
50% of cases.2
Medical treatment of ulcer bleeding is
directed to keep the gastric pH above the
proteolytic range for pepsin.3 A rise of the pH
of gastric juice to 4 almost completely abolishes
the fibrinolytic activity in gastric juice. 4 In
keeping the gastric pH above the proteolytic
range for pepsin in bleeders, parenteral proton
pump inhibitors were demonstrated to be
more effective than parenteral histamine H2antagonists.3,5 Lansoprazole injection is the most
recent intravenous PPI available in Indonesia.
Therefore, it requires a postmarketing study to
monitor its safety and effectiveness in clinical
practice.
The general objective was to assess the safety
and effectiveness of lansoprazole injection in
patients with upper gastrointestinal bleeding, due
to peptic ulcers or erosive gastritis. The specific
objectives were: to assess safety based on the
objective and subjective signs and symptoms,
and abnormalities of liver function tests and to
assess effectiveness of its hemostatic effect.
METHODS
Design and Patients
This was an observational, multicenter,
postmarketing study in patients with upper
gastrointestinal bleeding due to peptic ulcers
or erosive gastritis receiving intravenous
lansoprazole for a maximum of 7 days or until
the bleeding stopped and the patients were able
to take oral lansoprazole.
124
Patients recruited were those who came
to the emergency room (ER) of a hospital
with hematemesis and/or melena, and met the
following inclusion and exclusion criteria. A total
of 200 patients were planned to be enrolled from
100 internal medicine specialists in Indonesia.
Patients with upper gastrointestinal bleeding
were considered eligible if they fulfilled the
following inclusion criteria: (i) Men or women
with upper gastrointestinal bleeding (UGIB) due
to peptic ulcers or erosive gastritis, (ii) aged 18
up to 70 years inclusive. Patients were excluded
from the study if they were hemodynamically
unstable (hypotension, tachycardy, or postural
changes in heart rate or blood pressure),
hypersensitive to lansoprazole or other PPIs,
patients with liver cirrhosis, pregnancy or
lactation, patients suffering from gastrointestinal
cancer or receiving atazanavir sulfate.
Study Drug
Eligible patients received lansoprazole
injection 30 mg mixed with 0.9% NaCl or 5%
glucose solution and administered by i.v. drip
twice a day, or lansoprazole injection 30 mg
mixed with 20 mL of 0.9% NaCl or 5% glucose
solution and administered by slow i.v. injection
twice a day, for a maximum of 7 days.
Procedure
Upon arrival at the ER, anamnesis and
physical examination were performed, and also
measurement of blood chemistry (complete
blood count, SGPT, SGOT, creatinine, ureum).
To patients who were hemodynamically stable
with normal blood pressure, intravenous
lansoprazole was given twice a day for a
maximum of 7 days or until the bleeding
stopped and the patients were able to take oral
lansoprazole. Routine upper GI endoscopy was
performed in order to confirm cause of bleeding.
Vol 45 Number 2 April 2013
Safety and efficacy of Lansoprazole injection in upper GI bleeding
If the UGIB was not caused by peptic ulcers or
erosive gastritis, these patients were not included
in the efficacy population, but included in the
safety population. The bleeding stopped if there
was no more hematemesis (the nasal tube fluid
was already clear) and/or melena (the stool was
not black and liquid anymore). Hemoglobin
level was monitored daily depending on the
patient condition. Vital signs and blood chemistry
were measured again on the last day of therapy.
Concomitant medication was recorded, with the
respective indications. Objective and subjective
signs and symptoms which emerged during
intravenous lansoprazole administration were
recorded.
Serious adverse events (AE) were noted:
death, life-threatening, requires/prolongs
hospitalization, results in persistent/significant
disability/incapacity, a congenital anomaly/
birth, requires intervention to prevent one of
the above or may expose the patient to danger.
All serious adverse events had to be reported to
the sponsor within 24 hours (1 working day). A
special form was made available to be filled in by
the investigator, with monitoring doctors help.
Data Analysis
Safety analysis. All adverse events were
listed, and also AEs which were probably and
possibly related to lansoprazole injection.
Efficacy analysis. Efficacy of lansoprazole
injection was evaluated in UGIB patients due
to peptic ulcers or erosive gastritis who did not
require endoscopic hemostasis. In these patients,
the hemostatic effect of lansoprazole injection
was evaluated every day until a maximum of 7
days of treatment and the percentage of patients
whose bleeding stopped was calculated. The
hemostatic effect was determined and rated
as excellent, good, fair or poor as follows.
Excellent: if the bleeding stopped within 3 days.
Good: if the bleeding stopped within 5 days. Fair:
if the bleeding stopped within 7 days. Poor: if
the bleeding did not stop within 7 days, or the
treatment was changed.
RESULTS
During the study from December 2010 until
December 2011, 204 patients were screened, total
patients evaluable for safety were 204, while
total patients evaluable for efficacy were 200
(4 patients did not meet the inclusion criteria:
3 patients aged <18 years, 1 patient was GERD
patient).
Patient demographics and baseline
characteristics are shown in Table 1, vital signs
in Table 2, medical history in Table 3, and blood
chemistry in Table 4.
Table 1. Patient demographics and baseline characteristics
(n=200)
Median
(Range)
Missing
52.1 (13.34)
55.0 (19 70)
Weight (kg)
60.8 (10.39)
60.0 (36 100)
BMI (kg/m2)
23.0 (3.54)
23.0 (14 34)
Variables
Mean (SD)
Male: n (%)
125 (62.5%)
Age (yrs)
Table 2. Vital signs
Mean (SD)
Median
(Range)
Missing
SBP (mm Hg)
123.1 (18.02)
120.0 (90180)
DBP (mm Hg)
77.6 (9.77)
80.0 (50100)
Heart rate
(bpm)
89.5 (10.66)
88.0 (69124)
Respiratory
rate (per min)
20.0 (3.02)
20.0 (1431)
SBP (mm Hg)
121.9 (12.89)
120.0 (90190)
DBP (mm Hg)
78.4 (7.46)
80.0 (60100)
Heart rate
(bpm)
83.7 (8.01)
82.0 (68124)
Respiratory
rate (per min)
19.5 (3.10)
20.0 (1436)
Baseline
End of the
study (day 7)
Patients were mostly males (62.5%), mean
age was 52.1 years, and mean BMI was 23.0.
Systolic as well as diastolic blood pressure
did not change during the study.
Patient medical history consisted of
gastrointestinal diseases such as erosive gastritis
(40.5%), gastric ulcer (26.5%), and duodenal
ulcer (12.0%), and the patients also suffered
from some comorbid diseases such as diabetes
mellitus, hypertension, coronary artery disease,
dyslipidemia, and others.
125
Ari F. Syam
Acta Med Indones-Indones J Intern Med
Table 3. Medical history
Gastrointestinal diseases:
-- Erosive gastritis
81
40.5
-- Gastric ulcer
53
26.5
-- Duodenal ulcer
24
12.0
-- GERD
19
9.5
-- Hematemesis
13
6.5
-- Dyspepsia
4.5
-- Upper GI bleeding
1.5
-- Others
3.0
-- Diabetes mellitus
11
5.5
-- Hypertension
15
7.5
-- Coronary artery disease
2.5
-- Dyslipidemia
1.0
-- Osteoarthritis
4.0
-- Rheumatoid arthritis
0.5
-- Others:
Other diseases:
-- Obesity
1.0
-- Others
20
10.0
Laboratory findings showed that during
treatment with lansoprazole injection,
hemoglobin level increased. At baseline,
hemoglobin level was 9.9 g/dL and rose to 10.9
g/dL after treatment with lansoprazole injection.
Other laboratory parameters were also examined
in this study. During one week lansoprazole
injection, liver function tests (ALT and AST)
did not change. Kidney function, as shown
by creatinine and BUN, were improved (from
an average of 37.9 to 35.4 mg/dL and from a
mean of 1.2 to 1.1 mg/dL, respectively) during
treatment with lansoprazole injection.
Peptic ulcer was diagnosed endoscopically
in 104 patients (54%) and erosive gastritis in 96
patients (46%).
In this study, 92 patients were given
lansoprazole as intravenous drip and 97 patients
as intravenous slow injection, while 11 patients
were given a combination of both.
Safety Analysis (n=204)
Before
treatment
After
treatment
p value
No adverse events probably or possibly
related to lansoprazole injection was were
reported during the study.
Hb (g/dL)
9.9 (2.68)
10.9 (1.82)
< 0.001
Efficacy Analysis (n=200)
Creatinine
(mg/dL)
1.2 (0.65)
1.1 (0.51)
0.01
BUN (mg/dL)
37.9 (17.22)
35.4 (14.19)
< 0.001
ALT (U/L)
33.5 (19.92)
32.5 (14.49)
0.31 (NS)
AST (U/L)
32.8 (28.64)
30.5 (10.78)
0.17 (NS)
3.5 (0.50)
3.5 (0.49)
0.05
Table 4. Blood chemistry parameter before and after the
study
Variables
Albumin (g/dL)
Number and percentage of patients whose
UGIB stopped during treatment with lansoprazole
injection are shown in Figure 1. Hemostatic
effects of lansoprazole injection and hemostatic
effects based on gender, age groups, and Hb
groups are shown in Table 6.
Figure 1. Percentage of patients whose bleeding stopped during the study
126
Vol 45 Number 2 April 2013
Safety and efficacy of Lansoprazole injection in upper GI bleeding
50% were caused by peptic ulcer and erosive
gastritis.6
The mortality rate associated with UGIB
remained unchanged around 5-10% for the past
50 years, despite continuing improvement in
the diagnostic and therapeutic modalities.1 This
unchanged mortality rate may be accounted by
age and prevalence of concurrent illness, both
are important predictors of death, that continue
to rise among patients with UGIB. Patients with
bleeding usually die not from exsanguination,
but from decompensation due to other diseases.2
Appropriate initial management is one of the
key success to reduce morbidity and mortality. In
general, causes of gastrointestinal bleeding were
variceal or non-variceal. A systematic review and
meta-analysis of 21 randomized controlled trials
comparing 2915 patients (up to February 2003)
showed that proton pump inhibitor treatment
reduced rebleeding (OR=0.46; 95% CI=0.330.64) and the requirement for surgery (OR=0.59;
95% CI=0.46-0.76) after ulcer bleeding but did not
reduce mortality (OR=1.11; 95% CI=0.79-1.57).7
Whittle et al.8 have shown that, unlike in the
skin or vasculature, platelet aggregation plays a
minimal role in the initial hemostatic events in
the gastric mucosa and that the arrest of gastric
hemorrhage is brought about largely by processes
primarily involving the coagulation system.
The stronger drugs suppressing
acid production, the better in stopping the
gastrointestinal bleeding. Proton pump inhibitors
raise the pH to about 6.9 The target therapeutic
goal is to achieve an intragastric pH above 6,
at which the clotting process is optimal and
any formed clot is stabilized. The success of
hemostasis is highly dependent on the intragastric
pH and studies have shown that, when the intragastric pH is low, platelet function is impaired
and pepsinogen is activated to pepsin, which
disaggregates platelet plugs.10-11
Table 5. Hemostatic effects: total and based on gender
Hemostatic
effect
N (%)
Male (%)
Female
(%)
Excellent (bleeding
stopped within 3
days)
166 (83.0)
105 (84.0)
61 (81.3)
Good (bleeding
stopped within 5
days)
31 (15.5)
19 (15.0)
12 (16.0)
Fair (bleeding
stopped within 7
days)
2 (1.0)
1 (1.0)
1 (1.3)
Poor (bleeding
did not stopped
within 7 days)
1 (0.5)
1 (1.3)
125 (100.0)
75 (100.0)
Total
This study showed that lansoprazole injection
could stop bleeding in 10% of cases on day 1,
and on day 3 the cumulative stopped bleeding
rate was 83%, increasing to 99.5% after 7 days
of treatment.
The hemostatic effects of lansoprazole
injection based on gender were not different
(Kolmogorov Smirnov test: Z = 0.183, p = 1.0).
Based on age groups (<60 years and >60
years) the hemostatic effects of lansoprazole
injection were also not different (KolmogorovSmirnov test: Z=0.594, p=0.87), neither the
hemostatic effects of lansoprazole injection
based on Hb groups at baseline (KolmogorovSmirnov test: Z=0.521, p=0.95).
DISCUSSION
In the present study, it was found that 104
cases (52%) of the 200 UGIB cases were due
to peptic ulcer and 96 cases (48%) to erosive
gastritis. Many studies have shown that 50% of
the UGIB cases were caused by peptic ulcer.2
Research conducted at Cipto Mangunkusumo
Hospital that analyzed patients who presented
with upper gastrointestinal bleeding, found that
Table 6. Hemostatic effects based on age group and hemoglobin level at baseline
Hemostatic effect
<60 yrs (%)
>60 yrs (%)
Hb <10 (%)
Hb >10 (%)
Excellent
36 (80.0)
130 (83.9)
76 (79.2)
90 (86.5)
Good
8 (17.8)
23 (14.8)
19 (19.8)
12 (11.5)
Fair
2 (1.3)
1 (1.0)
1 (1.0)
Poor
1 (2.0)
1 (1.0)
Total
45 (100.0)
155 (100.0)
96 (100.0)
104 (100.0)
127
Ari F. Syam
A meta-analysis of 27 randomized trials of
H2-receptor antagonists in over 2500 patients
with acute UIGB suggested that the drugs
reduced the rates of rebleeding, surgery and
mortality, by about 10, 20, and 30%, respectively,
notably among those with gastric ulcers.12 In a
meta-analysis comparing proton pump inhibitors
with H2 antagonists, it was found that persistent
or recurrent bleeding was less frequent with
proton pump inhibitors (6.7) than with H2
antagonists (13.4%) (OR 0.4; 95%CI: 0.270.59). The need for surgery and mortality rates
did not reach statistical significance but showed
a favorable trend towards PPIs.5
Mucosal fibrinolytic activity is enhanced in
patients with bleeding gastrointestinal ulcers.
Acid suppressive therapy reduced this increased
activity and ultimately decreased bleeding in
peptic ulcers.13
This post-marketing survey showed that
lansoprazole injection could stop upper GI
bleeding in 10% of cases on day 1, and 83%
of the upper GI bleeding stopped on day 3,
increasing to 99.7% after 7 days of treatment.
This indicates that lansoprazole injection works
quickly to stop bleeding. The hemostatic effect
was rated as excellent if the bleeding stopped
within 3 days. Accordingly, this drug was
excellent for as much as 83%. These findings
suggest that lansoprazole may be useful in
situations where rapid acid control is required,
such as in emergency care situations.
A preliminary study using intravenous
lansoprazole 30 mg bid in patients with UGIB
for 7 days showed that bleeding was arrested in
16 of 18 patients (89%) within 3 days.14
A previous study using oral omeprazole 40
mg bid vs. placebo in patients with bleeding
peptic ulcers for 5 days showed that omeprazole
therapy was associated with significant reductions
in the rates of further bleeding (10.9% vs. 36.4%)
and surgical intervention (7.2% vs. 23.6%), and
the need for transfusion (29.1% vs. 70.9%).15
Another study with bolus i.v. (80 mg) followed
by infusion (8 mg/h) of omeprazole vs. placebo
for 72 hours in severe ulcer hemorrhage after
endoscopic therapy showed that omeprazole
reduced the number of operations (5.4% vs.
11.1%), endoscopic treatments (4.6% vs. 11.1%),
128
Acta Med Indones-Indones J Intern Med
and the duration and severity of bleeding (18.0%
vs. 31.4% with moderate or severe bleeding).16
Bolus i.v. (80 mg) followed by infusion (8
mg/h) of omeprazole for 3 days in patients
with bleeding peptic ulcers after endoscopic
treatment was also studied by Lau et al.17 and
showed that omeprazole reduced the risk of
recurrent bleeding (6.7% vs. 22.5% within 30
days; HR=3.9).
A recent prospective study conducted by
Liang et al.18 showed that high-dose pantoprazole
infusion therapy following endoscopic hemostasis
treatment is not superior to low-dose PPI therapy
in terms of reducing rebleeding among low risk
patients with a bleeding peptic ulcer (11.1% in
each group). A review by van Rensburg and
Cheer concludes that intravenous pantoprazole is
an effective option in the treatment of UGIB, the
prevention of rebleeding, and for the prophylaxis
of acute bleeding stress ulcers.19
A meta-analysis of 24 randomized controlled
trials (4373 participants) through November
2004 on the efficacy of PPIs for peptic ulcer
bleeding showed that treatment with PPIs did
not reduce mortality (OR=1.01) but significantly
reduced rebleeding (OR=0.49; 95% CI=0.370.65) and the need for surgery (OR=0.61;
95% CI=0.48-0.78). Treatment with PPIs
significantly reduced mortality in Asian trials
(OR=0.35; 95% CI=0.16-0.74) and in patients
with active bleeding or a nonbleeding visible
vessel (OR=0.53; 95% CI=0.31-0.91).20 This
meta-analysis was the extension of the previous
one7, involving 50% more patients, giving the
same results.
In this survey, hemoglobin was also
evaluated. During treatment with lansoprazole
injection, hemoglobin level increased. At
baseline, hemoglobin level was 9.9 g/dL and rose
to 10.9 g/dL after treatment with lansoprazole
injection. These data demonstrated that during
administration of lansoprazole, gastrointestinal
bleeding did not occur, clinically as well as in the
laboratory. In several studies, low hemoglobin
value is one predictor of rebleeding.21
Several laboratory parameters were also
examined in this study. The use of lansoprazole
injection for 1 week did not affect liver function.
Kidney function (creatinine and BUN) was
Vol 45 Number 2 April 2013
Safety and efficacy of Lansoprazole injection in upper GI bleeding
improved during treatment with lansoprazole
injection and these conditions were in line with
the cessation of gastrointestinal bleeding.
CONCLUSION
The results of this observational
postmarketing study in 200 patients with
endoscopically confirmed upper gastrointestinal
bleeding due to peptic ulcers or erosive gastritis
demonstrated that intravenous lansoprazole twice
a day was well tolerated and highly effective.
The authors declare that they have no
conflicts of interest in relation to this manuscript.
ACKNOWLEDGMENTS
We acknowledge PT. Takeda Indonesia for
funding this study. We also thank all physicians
who participated in this postmarketing study.
CONFLICT OF INTEREST
The authors received grant support from
PT. Takeda Indonesia.
REFERENCES
1. Gilbert DA. Epidemiology of upper gastrointestinal
bleeding. Gastrointest Endosc. 1990;36:S8-13.
2. Laine L, Peterson WL. Bleeding peptic ulcer. N Engl
J Med. 1994;331:71727.
3. Lanas A, Aurelio A, Jose B, et al. Effect of parenteral
omeprazole and ranitidine on gastric pH and the
outcome of bleeding peptic ulcer. J Clin Gastroenterol.
1995;21:103-6.
4. Patchett SE, Enright H, Afdhal N, OConnell W,
ODonoghue DP. Clot lysis by gastric juice: an in vitro
study. Gut. 1989;30:1704-7.
5. Gisbert JP, Gonzalez L, Calvet X, et al. Proton pump
inhibitors versus H2 antagonists: a meta-analysis of
their efficacy in treating bleeding peptic ulcer. Aliment
Pharmacol Ther. 2001;15(7):917-26.
6. Syam AF, Abdullah M, Makmun D, et al. The causes
of upper gastrointestinal bleeding in the National
Referral Hospital : Evaluation on upper gastrointestinal
tract endoscopic result in five years period. Indones J
Gastroenterol Hepatol Digest Endosc. 2005;6:71-4.
7. Leontiadis GI, Sharma VK, Howden CW. Systematic
review and meta-analysis of proton pump inhibitor
therapy in peptic ulcer bleeding. BMJ. 2005;330:568-75.
8. Whittle BJ, Kaufman GL Jr, Moncada S. Hemostatic
mechanisms independent of platelet aggregation: arrest
gastric mucosal bleeding. Proc Natl Acad Sci USA.
1986;83(15):5683-7.
9. van Rensburg CJ, Hartmann M, Thorpe A, et al.
Intragastric pH during continuous infusion with
pantoprazole in patients with bleeding peptic ulcer.
Am J Gastroenterol. 2003;98:2635-41.
10. Green FW Jr, Kaplan MM, Curtis LE, Levine PH.
Effect of acid and pepsin on blood coagulation
and platelet aggregation: a possible contributor to
prolonged gastroduodenal mucosal hemorrhage.
Gastroenterol. 1978;74(1):38-43.
11. Berstadt A. Does profound acid inhibition improve
hemostasis in peptic ulcer bleeding. Scand J
Gastroenterol. 1997;32(4):396-8.
12. Collins R, Langman M. Treatment with histamine H2
antagonists in acute upper gastrointestinal hemorrhage:
implications of randomized trials. N Engl J Med.
1985;313:660-6.
13. Vreeburg EM, Levi M, Rauws EAJ, et al. Enhanced
mucosal fibrinolytic activity in gastroduodenal
ulcer haemorrhage and the beneficial effect of acid
suppression. Aliment Pharmacol Ther. 2002;16:113742.
14. Aoki T. Intravenous administration of lansoprazole:
a preliminary study of dose ranging and efficacy in
UGIB. Aliment Pharmacol Ther. 1995;9(Suppl.1):51-7.
15. Khuroo MS, Yattoo GN, Javid G, et al. A comparison
of omeprazole and placebo for bleeding peptic ulcer.
N Engl J Med. 1997;336:1054-8.
16. de Muchadell DBS, Havelund T, Harling H, et al.
Effect of omeprazole on the outcome of endoscopically
treated bleeding peptic ulcers. Second J Gastroenterol.
1997;32:320-7.
17. Lau JYW, Sung JJY, Lee KKC, et al. Effect of
intravenous omeprazole on recurrent bleeding after
endoscopic treatment of bleeding peptic ulcers. NEJM.
2000;343:310-6.
18. Liang CM, Lee JH, Kuo YH, et al. Intravenous nonhigh-dose pantoprazole is equally effective as highdose pantoprazole in preventing rebleeding among
low risk patients with a bleeding peptic ulcer after
initial endoscopic hemostasis. BMC Gastroenterol.
2012;12:28-35.
19. van Rensburg CJ, Cheer S. Pantoprazole for the
treatment of peptic ulcer bleeding and prevention of
rebleeding. Gastroenterol. 2012;5:51-60.
20. Leontiadis GI, Sharma VK, Howden CW. Proton pump
inhibitor therapy for peptic ulcer bleeding. Cochrane
collaboration meta-analysis of randomized controlled
trials. Mayo Clin Proc. 2007;82(3):286-96.
21. Suk KT, Kim HS, Lee CS, et al. Clinical outcomes and
risk factors of rebleeding following endoscopic therapy
for nonvariceal upper gastrointestinal hemorrhage. Clin
Endosc. 2011;44(2):93-100.
129
Anda mungkin juga menyukai
- SOP Pemberian Anastesi Lokal Dan Sedasi Di Puskesmas BU HeniDokumen4 halamanSOP Pemberian Anastesi Lokal Dan Sedasi Di Puskesmas BU HeniRachindi Qory TrysiaBelum ada peringkat
- Kata PengantarDokumen2 halamanKata PengantarRachindi Qory TrysiaBelum ada peringkat
- Stroke InfarkDokumen27 halamanStroke InfarkRachindi Qory TrysiaBelum ada peringkat
- Referat Luka BakarDokumen43 halamanReferat Luka BakarRachindi Qory TrysiaBelum ada peringkat
- CoverDokumen1 halamanCoverRachindi Qory TrysiaBelum ada peringkat
- Lapsus 1Dokumen18 halamanLapsus 1Rachindi Qory TrysiaBelum ada peringkat
- Daftar IsiDokumen2 halamanDaftar IsiRachindi Qory TrysiaBelum ada peringkat
- Kata Pengantar 1Dokumen4 halamanKata Pengantar 1Rahmi Dwi AzkiahBelum ada peringkat
- Kata Pengantar 1Dokumen4 halamanKata Pengantar 1Rahmi Dwi AzkiahBelum ada peringkat
- GAMBAR SkizofreniaDokumen10 halamanGAMBAR SkizofreniaRachindi Qory TrysiaBelum ada peringkat
- Daftar Pustaka SkizofreniaDokumen2 halamanDaftar Pustaka SkizofreniaRachindi Qory TrysiaBelum ada peringkat
- Lembar Awal REFERATDokumen3 halamanLembar Awal REFERATRachindi Qory TrysiaBelum ada peringkat
- Cover Laporan Kasus RuanganDokumen1 halamanCover Laporan Kasus RuanganRachindi Qory TrysiaBelum ada peringkat
- AbstrakDokumen4 halamanAbstrakRachindi Qory TrysiaBelum ada peringkat
- Bab I, Ii, IiiDokumen35 halamanBab I, Ii, IiiRachindi Qory TrysiaBelum ada peringkat
- Daftar PustakaDokumen1 halamanDaftar PustakaRachindi Qory TrysiaBelum ada peringkat
- Laporan Kasus Stroke Infark RinaDokumen16 halamanLaporan Kasus Stroke Infark RinaRina Addina100% (1)
- Presentation 1Dokumen3 halamanPresentation 1Rachindi Qory TrysiaBelum ada peringkat
- Kata PengantarDokumen5 halamanKata PengantarRachindi Qory TrysiaBelum ada peringkat
- Anestesi PediatrikDokumen1 halamanAnestesi PediatrikRachindi Qory TrysiaBelum ada peringkat
- Kata Pengantar 1Dokumen4 halamanKata Pengantar 1Rahmi Dwi AzkiahBelum ada peringkat
- Laporan Kasus RuanganDokumen22 halamanLaporan Kasus RuanganRachindi Qory TrysiaBelum ada peringkat
- Bab I, Ii, IiiDokumen36 halamanBab I, Ii, IiiSari RezekiBelum ada peringkat
- Daftar IsiDokumen1 halamanDaftar IsiRachindi Qory TrysiaBelum ada peringkat
- ReferatDokumen21 halamanReferatRachindi Qory TrysiaBelum ada peringkat
- Warna Cover ReferatDokumen1 halamanWarna Cover ReferatRachindi Qory TrysiaBelum ada peringkat
- Daftar IsiDokumen1 halamanDaftar IsiRachindi Qory TrysiaBelum ada peringkat
- Tugas Fisiologi Pernapasan Dan Gagal NapasDokumen27 halamanTugas Fisiologi Pernapasan Dan Gagal NapasRachindi Qory TrysiaBelum ada peringkat
- Cover SkripsiDokumen1 halamanCover SkripsiRachindi Qory TrysiaBelum ada peringkat
- Cover ReferatDokumen1 halamanCover ReferatRachindi Qory TrysiaBelum ada peringkat
- Anatomi GI Tract, 2012Dokumen55 halamanAnatomi GI Tract, 2012wisnu_23Belum ada peringkat
- Acuan Tarif Jasa Medik ICD 9Dokumen549 halamanAcuan Tarif Jasa Medik ICD 9Dadang Sudirman96% (23)
- Kuliah PA Gastrointestinal DR RestiDokumen124 halamanKuliah PA Gastrointestinal DR RestiSatrio Adhy WibowoBelum ada peringkat
- Diagnosa Icd XDokumen5 halamanDiagnosa Icd XUmah NurmahBelum ada peringkat