A Community-Based Intervention To
Diunggah oleh
Abdelßasset ZkrJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
A Community-Based Intervention To
Diunggah oleh
Abdelßasset ZkrHak Cipta:
Format Tersedia
Applied Research and Evaluation
A COMMUNITY-BASED INTERVENTION TO
PROMOTE BREAST CANCER AWARENESS AND
SCREENING AMONG ASIAN AMERICAN WOMEN*
TSU-YIN WU, PH.D., RN
CHIUMAN LIN, MSN, RN
Eastern Michigan University, Ypsilanti
SHU-LING CHEN, PH.D., RN
Hung Kuang University, Taichung, Taiwan
YOOLIM JUNG
University of Michigan, Ann Arbor
ABSTRACT
Cancer is the leading cause of death for Asian Americans, and breast cancer
is the leading cancer diagnosed among Asian American women. Despite
the alarming facts, Asian American women have low breast cancer screening
rates. This study examined the effects of a culturally appropriate communitybased breast intervention program on participants knowledge about breast
cancer and intention for screening among Southeast Asian and South Asian
women in Michigan. Data were collected from 166 women. At baseline,
participants had limited knowledge of breast cancer screening guidelines and
misconceptions about the risk factors of breast cancer. After the educational
*This research was supported by the Susan G. Komen for the Cure (Grant #: POP0503877).
Intl. Quarterly of Community Health Education, Vol. 34(2) 171-185, 2013-2014
2014, Baywood Publishing Co., Inc.
doi: http://dx.doi.org/10.2190/IQ.34.2.e
http://baywood.com
171
172 / WU ET AL.
intervention, participants reported significantly higher knowledge scores
related to breast cancer and screening recommendations and intentions to
obtain follow-up CBE and mammograms. This culturally appropriate intervention provides strategies to overcome personal instructional barriers to
meet the needs of this group for early detection and cancer control.
Cancer is the leading cause of death for female Asian Americans [1]. Although
Asian American women have a lower reported incidence rate of breast cancer
(97 per 100,000) compared with White (141 per 100, 000) and African American
(102 per 100,000) women, the latest statistics available still show breast cancer
as the leading cancer diagnosed in Asian American women [2, 3]. The low breast
cancer incidence rates of Asian Americans perpetuate the belief of Asians as
a healthy minority is no longer true. The epidemiologic study showed that
for Asian women who immigrate to the United States, the incidence rate for
developing breast cancer is six times greater than that of women who remain
in their native countries. In fact, the incidence rate of breast cancer for Asian
American women now has approached that of White American women [4].
A recent study in Britain also revealed the evidence that breast cancer risk for
South Asian women in Britain has increased considerably over the last decade.
During the period 2000-2004, South Asian womens risk of developing breast
cancer was 45% lower than it was for White women. Between 2005-2009,
South Asian women were 8% more likely to develop breast cancer compared to
White women [5].
The literature documented that Asian American women are more likely to
receive a diagnosis in the advanced stages of the disease [6], primarily because
of late detection [7, 8]. In addition, a recent study found the portion of South
Asian women diagnosed at a localized stage was significant lower than proportions in other racial/ethnic groups [9]. Alarmingly, the Surveillance, Epidemiology, and End Results (SEER) data indicated that while the mortality rate
from breast cancer for White and Hispanic women decreased during 1990-1995,
the rates rose for Asian and Pacific Islander women [10]. In addition, a recent
secondary analysis using a national dataset collected by the Agency for Healthcare Research and Quality revealed that among American women with breast
cancer, Asian American (AA) women were the youngest to die (M = 46.2 years,
SD = 10.1) during the hospitalization; in particular, AA women were 17 years
younger at death compared with Caucasian women, 12 years younger compared
with African American women, and almost 19 years younger compared to Latina
women [11]. Therefore, there is an urgent need to promote breast cancer screening
among Asian women, since these screening activities can detect breast cancer
early and prevent thousands of breast cancer deaths each year by diagnosing the
disease when it is easier to treat.
BREAST CANCER AWARENESS AND SCREENING /
173
In various surveillance systems, immigrants from Asian countries in the United
States are classified as Asian Americans and considered as one homogeneous
group; this classification results in generalizations about the population as a
whole [12]. Individuals who are part of this group come from many different
countries and geographic locations, speak different languages, and have a wide
range of religions, lifestyles, and cultures [13]. A generalization that one often
hears about the Asian population is that they are a model minority population
that is successful with few problems or needs [14]. Nevertheless, the Asian
American population is highly diverse with a wide range in socioeconomic
status (SES). For example, whereas Japanese Americans are more acculturated
and have a higher SES, Southeast Asians, who more recently immigrated to
the United States, are less acculturated and have a lower SES. Therefore, the
model minority stereotype could lead to a lack of understanding of the specific
health problems and healthcare needs among different ethnic groups within
Asian Americans. Furthermore, health professionals may underestimate the
developing threat of breast cancer in Asian women due to the lower breast
cancer incidence rate (compared to their Caucasian and African American
counterparts) and cultural barriers (e.g., language, access to care, etc.). As
consequences, Asian women may not receive adequate and culturally appropriate information on mammography and clinical breast examination during
routine care [11]. Therefore, it is critical to increase the awareness of healthcare
providers on Asian womens special needs and cultural barriers toward breast
cancer screening.
Working with Southeast Asian (SEA) and South Asian (SA) women to promote
their breast health poses additional challenges because these SEA and SA women
often emigrated from countries in political turmoil or where public health efforts
were less advanced and comprehensive. In these countries, a lower priority may
be set for disease prevention because there is a greater need to control more
immediate threats, including infectious diseases and basic survival [15]. It is
hypothesized that culturally sensitive strategies will educate immigrant SEA and
SA women about the importance of early detection for breast cancer; screening
practices will become part of their health consciousness and later transform into
actual screening behavior.
In this article, the project team developed and implemented a culturally
sensitive breast interventional program tailored to the unique cultural needs
of this target population in order to increase the knowledge toward breast
cancer and screening utilization (i.e., breast self-exam (BSE), clinical breast
examination (CBE), and mammography) for SEA and SA women in
Michigan. The current project focused on immigrant women living in those
counties in the state of Michigan who were originally from southeastern and
South Asia, particularly from three larger countriesthe Philippines, Vietnam,
and India.
174 / WU ET AL.
METHODS
Study Design and Procedure
This study used a one-group pre-survey and post-survey design to examine
the impact of a culturally appropriate intervention. The following strategies were
used to recruit eligible women to participate in the current study:
1. collaboration with the local community, ethnic social groups, professional
organizations, and religious associations to distribute information to their
members;
2. collaboration with ethnic student associations to help recruit their mothers
and other relatives into the study;
3. posting flyers at local ethnic grocery stores, restaurants, beauty salons, etc.;
4. making presentations and volunteering in local ethnic celebration events
(e.g., the Mid-Autumn Festival, Asian New Year Celebration, etc.); and
5. providing small monetary incentives for women who refer their friends
and relatives to the project.
In addition, in order to be well connected to each ethnic community, four bilingual
coordinators from the Philippines, Vietnam, and India were hired to facilitate
community networking and participant recruitment. The calculation from the
power analysis indicated that the required sample size for this study was at least
128 participants; with the projected 20% attrition rate, 160 participants were
needed as targeted sample size. Study eligibility criteria included self identify
as SEA and SA women (Philippines, Vietnam, and India) aged 30 or older and
no personal history of breast cancer.
Study protocol was approved by the Institutional Review Board. Informed
consents were obtained at the beginning of educational sessions for completing
the pre- and post-intervention survey. The study intervention was an hour-long
interactive education session delivered in a group format and conducted at community centers, churches, and temples where participants gathered. The Project
Director verbally explained the purpose of the study and its procedures; participants had opportunities to ask any questions they might have.
Conceptual Framework
The study was guided by the Cultural Exploratory Model (CEM), which
provides a comprehensive understanding of the use of breast cancer screening
among minority women. According the CEM, an understanding of minority
womens cultural beliefs and values as well as personal life experiences with
respect to utilization of breast cancer screening is essential. In particular, perceptions about such screening procedures can be considered as increasing
the chance of getting the disease, and the issue of modesty is relevant among
Asian populations. These factors need to be considered in designing strategies to
BREAST CANCER AWARENESS AND SCREENING /
175
promote screening in the minority population. In addition, the CEM stresses that
the needs of minority women within ethnic groups do not only depend on their
cultural background since individuals are shaped by social relationships that
take place within and outside their cultural groups. Therefore, it is important
to consider womens sociodemographic factors, including their socioeconomic
status, educational background, and immigration status. The CEM acknowledges
and respects the individual and cultural explanations in health-seeking behavior
that health professionals can utilize to assess Asian womens needs in cancer
screening. This model has been applied in examining religious and sociocultural
issues relevant to breast cancer screening practices among older immigrant Asian
Islamic women and practices of breast self-examination (BSE) among Middle
Eastern Asian Islamic immigrant women [16, 17]. The current study applied the
CEM to evaluate the cultural beliefs, socioeconomic factors, and barriers to
breast cancer screening in SEA and SA women residing in the United States,
as well as their current practices related to breast cancer screening activities
(e.g., BSE, CBE, and mammography).
Intervention Development and Implementation
The interdisciplinary project team that consisted of professionals from Nursing,
Medicine, and Social Work used findings from earlier qualitative and descriptive
studies to develop linguistically appropriate culturally sensitive content to address
barriers and cultural beliefs toward breast cancer and screening practices.
Reducing cultural barriers: The results from a previous descriptive study
that examined mammography screening practices and related beliefs in
Chinese, Filipino, and Asian Indian women found that different barriers
related to cultural beliefs were identified by specific ethnic groups; for
example, Afraid that mammogram will find cancer was important for
Filipino women; Dont need mammogram if I feel OK and Waiting time
is too long were mentioned frequently by the Chinese women; and Dont
know where to get a mammogram was a common barrier for the Asian
Indian women [18]. The study intervention was developed utilizing the
results of cultural beliefs and barriers about breast cancer screening that are
specific to each ethnic group and incorporated into the education sessions.
Reducing language barriers: The sessions were conducted separately for
different ethnic groups, and each session was facilitated by bilingual project
staff to assist those women who are not fluent in English. All written materials
were translated into their native languages. All sessions were conducted in
a small group setting (limited to 15 or less) to facilitate interactions.
Reducing structural barriers: Before the education session started, the project
staff (with social work background) performed a needs assessment and identified structural barriers (i.e., access, transportation, child-care issues, etc.)
to screening. A feasible plan to perform the three breast cancer screening
176 / WU ET AL.
modalities (including BSE, CBE, and mammography) was developed. For
those participants who do not have health insurance and cannot have their
screening done via routine healthcare, free state-funded breast and cancer
control program (BCCCP) or low-cost programs were identified and provided
to women participants as resources.
The group presentations were delivered by the principal investigator and facilitated by the bilingual project staff. The presentation content incorporated the
content that addresses cultural, language, and structure barriers encountered by
immigrant SEA and SA women. During the sessions, participants were encouraged to share their personal cancer and screening experiences and points that
highlight the importance of early detection and the necessity of a woman staying
healthy to care for her family were emphasized. The educational program also
included information on following topics:
1. early detection of breast cancer and promotion of breast health;
2. benefits and access to breast cancer screening (i.e., clinical breast exam and
mammogram);
3. effective strategies for reducing barriers and increasing self-efficacy for
adherence;
4. skills for performing breast self-examination; and
5. availability of clinical breast exams and information on MI-BCCCP.
The program lasted approximately one hour and allowed questions and answers
at the end.
Data Collection and Analysis
A self-administered instrument was used to collect demographic data, knowledge of breast cancer risk factors and frequency for recommended screening
tests, beliefs toward susceptibility/risk, self-efficacy, and intentions for future
screening. The study measures were initially developed in English and translated
into Tagalog (for Filipino group), Hindu (for Asian Indian group), and Vietnamese
using standard back translation. The process of back translation can be found in
a previously reported study [19].
The sociodemographic section includes age, ethnicity, education, duration of
residing in the United States, marital status, income, insurance coverage for
mammography, and personal and family histories of breast cancer. Two items
were used to assess participants risk perceptions on getting breast cancer on a
5-point Likert scale (1 = no risk, 2 = low, 3 = moderate, 4 = high, or 5 = extremely
high risk), and another item asked participants to rate their risk compared to
other women with responses ranging from 1 (much lower than average) to 5
(much higher than average). The knowledge sections consisted of: a) knowledge
about breast cancer risks (eight items related to the knowledge of the following
conditions that increases a womans chance of getting breast cancer: (i) hitting,
BREAST CANCER AWARENESS AND SCREENING /
177
bumping, or fondling the breasts; (ii) doing something morally bad; (iii) immigration to the United States; (iv) overweight; (v) air pollution; (vi) large breasts,
(vii) ovarian cancer, and (viii) mammogram helps to detect cancer; and b) knowledge of recommendations for frequency of mammography screening (five items
related to knowledge of the recommended frequency of having a mammogram
for women with the following conditions: (i) does not have any family history
of breast cancer, (ii) does not have any breast symptoms, (iii) had previously
breastfed a child, (iv) older age, and (vi) healthy lifestyles.
Health beliefs (i.e., perceived benefits, perceived barriers, perceived selfefficacy) measures were tested in a previous study, and results demonstrated
excellent internal consistency and provided evidence of construct and predictive
validity [19, 20]. A set of 18 items assessing the womens perceptions about
benefits and barriers of breast cancer screening with six items focusing on the
benefits and 12 items assessing the barriers to regular mammography; each
item used a 4-point Likert scale. The intention to obtain a mammogram and
CBE were assessed using two items in a post-intervention survey asking participants whether they were planning on having a mammogram/CBE in the future
(in 6 months).
The SPSS statistical package, version 18.0, was used to analyze the data.
Descriptive statistics were performed to summarize sample characteristics and
study variables. Paired t-tests were used to determine changes before and after
the educational intervention in knowledge and self-efficacy. McNear Chi-square
tests were used to detect changes in correct responses of individual knowledge
questionnaire items. A p value of < .05 was considered significant.
RESULTS
Social-Demographic Characteristics
Participant characteristics are detailed in Table 1. A total of 166 women
were enrolled to participate in the study and 141 women completed both pre- and
post-surveys. The mean age was 50 years (SD = 12.4; range 30-83); 65% were
married; 75% had received college education (M = 12 years); 37% had annual
income less than $15,000; and 45% had insurance coverage for the mammogram.
BSE, CBE, and Mammography Use at Baseline
At the baseline, only 36% of the participants had had their last mammogram
within past 2 years, and 27% had never heard about the mammogram. In terms
of CBE use, 51% reported their last visits were up-to-date, and 28% expressed
that they had never received a CBE in the past. Thirty-seven percent of participants reported they performed monthly BSE while 31-33% reported they had
never heard of BSE or had never self-examined.
178 / WU ET AL.
Table 1. Participant Characteristics
Characteristics
na
Ethnicity
India
Philippines
Vietnam
60
17
64
42.6
12.1
45.4
Age (years)
40-49
50-65
> 65
30
62
14
28.3
58.5
13.2
Marital status
Married
Not married
91
50
64.5
35.5
Education
High school or lower
College/university or higher
21
63
25.0
75.0
Length of residency in the United States (years)
< = 10
> 10
60
72
45.5
54.5
Insurance coverage of mammogram
Yes
No
Dont know
57
47
24
44.5
36.7
18.8
aNumbers do not sum to 141 due to missing values.
Knowledge of Risk on Developing Breast Cancer
The effects of the study intervention were examined with participants knowledge of risk of developing breast cancer. Using a paired t-test to determine the
effectiveness of the education intervention, the results showed that the participants
had significantly higher scores in overall knowledge of the risk of developing
breast cancer after educational intervention (t = 11.97, p < 0.05). When individual risk items were examined, the results demonstrated that participants did
not have the correct knowledge on the risks for developing breast cancer. Fewer
than half of the study sample responded to the seven items correctly (Table 2).
Ninety-four percent of participants incorrectly thought that women who have
large breasts have a higher chance of getting breast cancer than women with
BREAST CANCER AWARENESS AND SCREENING /
179
Table 2. Educational Intervention Impact on Knowledge of
Risk of Developing Breast Cancer
Items in knowledge of risk
of developing breast cancer
PrePostintervention intervention
% correct
% correct
c2
Bumping, hitting, or fondling the
breasts increases the risk
41
84
50.70 < 0.05
Doing something morally bad
increases the risk
48
89
497.78 < 0.05
Immigrating to the United States
increases the risk
12
52
36.89 < 0.05
Obesity increases the risk
21
50
21.01 < 0.05
Air pollution increases the risk
24
58
24.54 < 0.05
86
104.42 < 0.05
Ovarian cancer increases the risk
26
45
7.62 < 0.05
Mammogram helps doctors or
nurses find breast cancer before it
can be felt
79
82
0.25
ns
11.97
< 0.05
Large breasts increases the risk
PrePostintervention intervention
Mean
Mean
Overall (eight items)
2.57
5.46
*N = 141; ns = not significant.
larger breasts. Eighty-eight percent of participants did not know that the immigration increases the likelihood of developing breast cancer. The Chi-square
analyses indicated that except for the mammogram item, participants correct
responses for each item significantly increased after the intervention (Table 2).
Knowledge of Mammography Frequency
Under Different Scenarios
In examining the knowledge dimension on recommendations for frequency
of mammography screening with different scenarios, the results from the paired
180 / WU ET AL.
t-test showed that the overall mean score at post-test was not statistically different
from the pre-test score (t = 0.85, p = ns). Nevertheless, participants correct
response rate increased with every item during post-intervention; however, none
of p values reached statistical significance (Table 3).
Knowledge of Recommended Frequency
for Performing BSE and CBE
Participants were also tested on their knowledge of recommended frequency
for performing BSE and CBE before and after the education intervention. The
results showed that participants knowledge of recommended frequency for
performing BSE increased significantly during post-intervention. The correct
response rate increased from 33% to 66% (c2 = 23.60, p < 0.05). The percentage
of participants who correctly knew the recommended frequency of performing CBE also increased after the intervention (pre-intervention: 28%; postintervention: 52%; c2 = 7.81, p < 0.01). For mammography, 23% knew when
to begin regular screening at baseline.
Self-Efficacy, Risk Perception, and Intention
for Future Screening Plans
Participants were asked to rate their self-efficacy for performing BSE (100point scale). During pre-intervention, the mean of participants self-efficacy for
Table 3. Educational Intervention Impact on Knowledge of
Mammography Frequency under Different Scenarios
Preintervention
% correct
Postintervention
% correct
c2
Have no family history
70
72
0.09
ns
No symptom
66
70
0.39
ns
Breast-fed a child
65
69
0.57
ns
Gets older
71
77
1.64
ns
Healthy lifestyles
69.5
70.2
0.00
ns
Items in knowledge of risk
of developing breast cancer
Overall (five items)
*N = 141; ns = not significant.
Preintervention
Mean
Postintervention
Mean
3.57
3.40
0.85
ns
BREAST CANCER AWARENESS AND SCREENING /
181
performing BSE was 46.14 (SD = 31.92), whereas the mean of self-efficacy
for performing BSE upon post-intervention was 73.37 (SD = 26.61). The t-test
analysis showed a significant difference between pre-intervention and postintervention self-efficacy scores (t = 8.43, p = .00). Moreover, at the post-test,
94% of the participants reported their plans for making visits to obtain CBE
and mammograms in the future.
When participants were asked about their risk of getting breast cancer on a
scale from no risk to very high risk, more than 70% of the women reported
either no risk or very low risk at baseline. After the educational intervention,
the percentage for reporting on these two categories decreased to 66%. The
women rating their risk as moderate increased from 19% (pre-intervention survey)
to 27% (post-intervention survey) (Table 4). The changes of risk perception from
pre- to post-intervention is statistically significant (t = 2.14, p < .05).
In terms of getting breast cancer screening, 94% of participants indicated
that they were planning to obtain CBEs in the future, and 91% indicated that
they plan to obtain mammograms. Before the education session, more than 90%
of women reported that they were not aware of the state program to obtain
free mammograms; after the study intervention, 60% of them indicated that they
now are aware of MI-BCCCP and know how to contact the program for eligibility
and enrollment information.
DISCUSSION
To our knowledge, this was the first study in the literature to focus on the impact
of educational intervention on Southeast Asian (SEA) and South Asian (SA)
women in Michigan. The results demonstrate that it is feasible and effective in this
study in reaching traditionally under-screened SEA and SA women and providing
culturally appropriate intervention that increases their knowledge on breast cancer
Table 4. Perceptions of Risk of Developing
Breast Cancer
Preintervention
%
Postintervention
%
No risk
37.1
24.8
Low risk
35.6
41.1
Moderate risk
18.9
27.1
High risk
6.8
7.0
Extremely high risk
1.5
(< 1%)
Risk perception
182 / WU ET AL.
and screening practices. SEA and SA women after the education session had
significantly higher knowledge scores related to breast cancer and screening
recommendations. In addition, while the study participants had low levels of
screening practices for CBEs and mammograms (51% and 36% of up-to-date
screening rates respectively) at pre-test, more than 90% of them reported their
intent to obtain follow-up CBE and mammograms at the post-test. While previous
intervention research on Asian Americans focused on current or existing
screening behaviors [21-23], it is important to investigate participants intentions in order to better predict their future screening behaviors. This study intervention bridges the gap and provides strategies to address language, cultural,
and structural barriers so SEA and SA women have skills and knowledge for the
follow-up screening routines. Although the majority of participants heard about
breast cancer screening tests (i.e., mammogram and CBE), they had limited
knowledge of ACS screening guidelines, thus had misconceptions about the
risk factors of breast cancer. In particular, less than one-third of women at baseline
knew obesity and being immigrants can increase the risk, and more than 90%
of participants mistakenly believed that large breasts can increase the risk for
breast cancer. In this immigrant population, with limited health literacy in combination with English language proficiency, immigrant SEA and SA women
presented as one of most vulnerable groups who had limited awareness on early
detection for cancer control and difficulty in accessing health information and
healthcare when they immigrate to the United States. Health education about
the benefits of early detection and recommended screening intervals and tests
is needed on an ongoing basis so the critical breast health information can be
infused to this community. The strength of this study is to incorporate previous
study findings into the study interventions that provide culturally and linguistically appropriate content in their native languages so that women know strategies
and resources for decreasing or minimizing identified barriers, which in turn
increases self-efficacy for participants in this study.
The education was effective in modifying perceived risk perceptions of breast
cancer in this group of SEA and SA women, whereas participants risk perceptions
significantly changed from pre- to post-test. At baseline, a large proportion of
women (73%) indicated they have less or much less risk of developing breast
cancer. Consistent with other studies reporting low perceived risks for breast
cancer among Asian American women [24, 25], the findings from the current
study support the notion that discussing risks is complex and must consider
cultural values and beliefs specific to this group. The findings illustrate the
need for clinicians and health educators to be aware of the way perceived risks
operate within SEA and SA groups and incorporate into an intervention based
on the evaluation of their patients perceived risk of cancer to better deliver the
messages of the importance for screening.
The study is limited by using a convenience sample and did not have a
control group. Therefore, the true intervention effects cannot be estimated. The
BREAST CANCER AWARENESS AND SCREENING /
183
actual risks for developing breast cancer were not measured; therefore, the
changes of risk perception among participants compared with their actual risks
cannot be verified. The participants self select into participation in the study and
were already interested and motivated to learn more about this topic. The study
was conducted in SEA and SA communities in suburban areas in the Midwest
of the United States; the findings of this study may not be generalized to SEA
and SA women in other areas of the United States. A longitudinal study with
longer periods after the study intervention is needed to evaluate the sustaining
effect of educational intervention on knowledge and screening behaviors.
In conclusion, the womens decisions for getting breast cancer screening is
influenced by a combination of factors including perceptions of breast cancer
risk, knowledge of risk factors, barriers toward screening, and confidence in
obtaining screening tests. The findings from this study support the notion that
SEA and SA women are no longer considered as low-risk groups for breast
cancer screening since they are less likely to be aware of their risks for breast
cancer. In order to motivate them to obtain the recommended breast cancer
screening tests, SEA and SA women need to increase breast health awareness
and change their misconceptions about risk factors related to breast cancer and
screening procedures. The intervention to promote breast cancer screening can
be effective if the program is appropriately tailored to meet the needs of the
targeted community by providing the relevant health education content and
strategies and skills overcome social, structural, cultural, and linguistic barriers.
In addition, the specific perceptions of SEA and SA women toward such newer
screening practices (for example, mammography) also need to be carefully
assessed during the clinical encounter so health professionals can better provide
culturally competent care. The current study laid the foundation for communitybased culturally appropriate education intervention for promoting breast health
and screening behavior among SEA and SA women.
ACKNOWLEDGMENTS
We thank the Southeast Asian and South Asian community for their support
and those women who participated in our study. We appreciate the work of our
team staff, Angela Shu and Shelly Xiejuan Wu, during earlier stage of manuscript
development and the editorial assistance of Alethea Helbig who helped the
authors to review and improve the manuscript.
REFERENCES
1. www.sp.ohio-state.edu/aancart/ABOUT_AANCART.htm. 2002.
2. A. Jemal, R. Tiwari, T. Murray, A. Ghafoor, A. Samuels, E. Ward, et al., Cancer
Statistics, Cancer Journal for Clinicians, 51, pp. 8-29, 2004.
184 / WU ET AL.
3. B. A. Miller, L. N. Kolonel, L. Bernstein, J. L. Young Jr., G. M. Swanson, and D. West
(eds.), Racial Patterns of Cancer in the United States 1988-1992, National
Cancer Institute, Bethesda, Maryland, National Cancer Institute, NIH Publication,
No. 96-4104, 1996.
4. R. G. Ziegler, R. N. Hoover, M. C. Pike, A. Hildesheim, A. M. Y. Nomura, D. W.
West, et al., Relative Weight, Weight Change, Height and Breast Cancer Risk in
Asian American Women, Journal of the National Cancer Institute, 88, pp. 650-660,
1996.
5. D. Florentin, Breast Cancer Incidence in Leicester 2000-2009, University of
Sheffield, the 2013 National Cancer Intelligence Network Conference, Brighton,
2013.
6. A. N. Hedeen, E. White, and V. Taylor, Ethnicity and Birthplace in Relation to
Tumor Size and Stage in Asian Americans Women with Breast Cancer, American
Journal of Public Health, 89, pp. 1248-1252, 1999.
7. B. Mo, Modesty, Sexuality, and Breast Health in Chinese-American Women, The
Western Journal of Medicine, 157, pp. 260-264, 1992.
8. J. A. Earp, M. Altpeter, L. Mayne, C. I. Viadro, and M. S. OMalley, The North
Carolina Breast Cancer Screening Program: Foundations and Design of a Model for
Reaching Older, Minority, Rural Women, Breast Cancer Research & Treatment, 35,
pp. 7-22, 1995.
9. A. Parikh-Patel, P. K. Mills, and R. V. Jain, Breast Cancer Survival among South Asian
Women in California (United States), Cancer Causes & Control, 17:3, pp. 267-272,
2006.
10. P. A. Wingo, L .A .G. Ries, H. M. Rosenberg, D. S. Miller, and B. K. Edwards, Cancer
incidence and mortality: A report card for the U.S., Cancer, 82, pp. 1197-1207, 1998.
11. C. Polek, P. Klemm, T. Haride, E. Wheeler, M. Birney, and K. Lynch, Asian/Pacific
Islander American Women: Age and Death Rates during Hospitalization for Breast
Cancer, Oncology Nursing Forum, 31, pp. E69-E74, 2004.
12. E. Takada, J. M. Ford, and L. S. Lloyd, Asian Pacific Islander Health, in Handbook
of Immigrant Health, S. Loue (ed.), Plenum Press, New York, 1998.
13. C. Browne and A. Broderick, Asian and Pacific Island Elders: Issues for Social
Work Practice and Education, Social Work, 39, pp. 252-259, 1994.
14. J. S. Lin-Fu, Population Characteristics and Health Care Needs of Asian Pacific
Americans, Public Health Report, 103, pp. 18-27, 1988.
15. M. Meana, T. Bunston, U. George, L. Wells, and W. Rosser, Influences on Breast
Cancer Screening Behaviors in Tamil Immigrant Women 50 Years Old and Over,
Ethnicity and Health, 6, pp. 179-188, 2001.
16. S. S. Rajaram and A. Rashidi, Asian-Islamic Women and Breast Cancer Screening:
A Socio-Cultural Analysis, Women & Health, 28, pp. 45-58, 1999.
17. A. Rashidi and S. S. Rajaram, Middle Eastern Asian Islamic Women and Breast
Self-Examination: Needs Assessment, Cancer Nursing, 23, pp. 64-70, 2000.
18. T. Y. Wu, Y. W. Chen, and C. Hergert, Health Beliefs and Practices Related to
Breast Cancer Screening in Filipino, Chinese, and Asian Indian Women, Cancer
Detection & Prevention, 30, pp. 58-66, 2006.
19. T. Y. Wu and M. Y. Yu, Reliability and Validity of the Mammography Screening Beliefs Questionnaire among Chinese American Women, Cancer Nursing, 26,
pp. 131-142, 2003.
BREAST CANCER AWARENESS AND SCREENING /
185
20. T. Y. Wu and W. Brady, Mammography Stage of Adoption and Decision Balance
among Asian Indian and Filipino American Women, Cancer Nursing, 30, pp. 390-398,
2007.
21. A. E. Maxwell, R. Bastani, P. Vida, and U. S. Warda, Results of a Randomized Trial
to Increase Breast and Cervical Cancer Screening among Filipino American Women,
Preventive Medicine, 37:2, pp. 102-109, 2003.
22. T. T. Nguyen, G. Le, T. Nguyen, K. Le, K. Lai, G. Gildengorin, J. Tsoh, N. Bui-Tong,
and S. J. McPhee, Breast Cancer Screening among Vietnamese Americans: A Randomized Controlled Trial of Lay Health Worker Outreach, American Journal of
Preventive Medicine, 37:4, pp. 306-313, 2009.
23. G. R. Sadler, P. R. Beerman, K. Lee, J. Hung, H. Nguyen, J. Cho, and W. Huang,
Promoting Breast Cancer Screening among Asian American Women: The Asian
Grocery Store-Based Cancer Education Program, Journal of Cancer Education, 27:4,
pp. 612-617, 2012.
24. J. S. Haas, C. P. Kaplan, G. Des Jarlais, V. Gildengoin, E. J. Perez-Stable, and
K. Kerlikowske, Perceived Risk of Breast Cancer among Women at Average and
Increased Risk, Journal of Womens Health, 14:9, pp. 845-851, 2005.
25. S. E. Kim, E. J. Prez-Stable, S. Wong, S. Gregorich, G. F. Sawaya, J. M. Walsh, and
C. P. Kaplan, Association between Cancer Risk Perception and Screening Behavior
among Diverse Women, Archives of Internal Medicine, 168:7, pp. 728-734, 2008.
Direct reprint requests to:
Tsu-Yin Wu
Director, Healthy Asian Americans Project
EMU-School of Nursing
Room 328 Marshall Building
Ypsilanti, MI 48197
e-mail: twu@emich.edu
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Helen Hodgson - Couple's Massage Handbook Deepen Your Relationship With The Healing Power of TouchDokumen268 halamanHelen Hodgson - Couple's Massage Handbook Deepen Your Relationship With The Healing Power of TouchLuca DatoBelum ada peringkat
- Emotional Intelligence Assignment 1 PDFDokumen10 halamanEmotional Intelligence Assignment 1 PDFAbdelßasset Zkr100% (2)
- ToonHub - Articles of PartnershipDokumen13 halamanToonHub - Articles of PartnershipKingBelum ada peringkat
- Grade 2 - PAN-ASSESSMENT-TOOLDokumen5 halamanGrade 2 - PAN-ASSESSMENT-TOOLMaestro Varix100% (4)
- ! Sco Global Impex 25.06.20Dokumen7 halaman! Sco Global Impex 25.06.20Houssam Eddine MimouneBelum ada peringkat
- Cookery-10 LAS-Q3 Week5Dokumen7 halamanCookery-10 LAS-Q3 Week5Angeline Cortez100% (1)
- Leadership Style and Employee Turnover IntentionsDokumen21 halamanLeadership Style and Employee Turnover IntentionsAbdelßasset ZkrBelum ada peringkat
- Ijias 15 262 04Dokumen5 halamanIjias 15 262 04Abdelßasset ZkrBelum ada peringkat
- 2Dokumen6 halaman2Abdelßasset ZkrBelum ada peringkat
- Why Management Skills Are A Priority For Nurses 050313Dokumen2 halamanWhy Management Skills Are A Priority For Nurses 050313Rauven Jean Erodias FadriquelaBelum ada peringkat
- Emotional IntelligenceDokumen3 halamanEmotional IntelligenceAbdelßasset ZkrBelum ada peringkat
- Dietery Factor Obesity Microenvironnement and Breast CancerDokumen9 halamanDietery Factor Obesity Microenvironnement and Breast CancerAbdelßasset ZkrBelum ada peringkat
- Knowledge, Attitudes and Practices Toward Breast CancerDokumen9 halamanKnowledge, Attitudes and Practices Toward Breast CancerAbdelßasset ZkrBelum ada peringkat
- A Beautiful MindDokumen6 halamanA Beautiful MindAbdelßasset ZkrBelum ada peringkat
- The Relationship of Turnover Intention With Job Satisfaction, Job Performance, Leader Member Exchange, Emotional Intelligence and Organizational CommitmentDokumen15 halamanThe Relationship of Turnover Intention With Job Satisfaction, Job Performance, Leader Member Exchange, Emotional Intelligence and Organizational CommitmentgaluhfitriBelum ada peringkat
- Emotional IntelligenceDokumen3 halamanEmotional IntelligenceAbdelßasset ZkrBelum ada peringkat
- EQ Interview Assignment - Evaluate Candidate's Empathy SkillsDokumen1 halamanEQ Interview Assignment - Evaluate Candidate's Empathy SkillsAbdelßasset ZkrBelum ada peringkat
- Why Management Skills Are A Priority For Nurses 050313Dokumen2 halamanWhy Management Skills Are A Priority For Nurses 050313Rauven Jean Erodias FadriquelaBelum ada peringkat
- FIITJEE Talent Reward Exam 2020: Proctored Online Test - Guidelines For StudentsDokumen3 halamanFIITJEE Talent Reward Exam 2020: Proctored Online Test - Guidelines For StudentsShivesh PANDEYBelum ada peringkat
- Unofficial Transcript - Printer FriendlyDokumen4 halamanUnofficial Transcript - Printer Friendlyapi-251794642Belum ada peringkat
- Research Methods LessonDokumen26 halamanResearch Methods LessonCarole Janne EndoyBelum ada peringkat
- Specification Table - Stocks and ETF CFDsDokumen53 halamanSpecification Table - Stocks and ETF CFDsHouse GardenBelum ada peringkat
- Other Project Content-1 To 8Dokumen8 halamanOther Project Content-1 To 8Amit PasiBelum ada peringkat
- Bhikkhuni Patimokkha Fourth Edition - Pali and English - UTBSI Ordination Bodhgaya Nov 2022 (E-Book Version)Dokumen154 halamanBhikkhuni Patimokkha Fourth Edition - Pali and English - UTBSI Ordination Bodhgaya Nov 2022 (E-Book Version)Ven. Tathālokā TherīBelum ada peringkat
- Simptww S-1105Dokumen3 halamanSimptww S-1105Vijay RajaindranBelum ada peringkat
- Dealer DirectoryDokumen83 halamanDealer DirectorySportivoBelum ada peringkat
- Term2 WS7 Revision2 PDFDokumen5 halamanTerm2 WS7 Revision2 PDFrekhaBelum ada peringkat
- Robots Template 16x9Dokumen13 halamanRobots Template 16x9Danika Kaye GornesBelum ada peringkat
- CV Finance GraduateDokumen3 halamanCV Finance GraduateKhalid SalimBelum ada peringkat
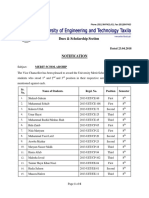
- Dues & Scholarship Section: NotificationDokumen6 halamanDues & Scholarship Section: NotificationMUNEEB WAHEEDBelum ada peringkat
- MES - Project Orientation For Night Study - V4Dokumen41 halamanMES - Project Orientation For Night Study - V4Andi YusmarBelum ada peringkat
- License Key Windows 8Dokumen7 halamanLicense Key Windows 8Juned FahriBelum ada peringkat
- Das MarterkapitalDokumen22 halamanDas MarterkapitalMatthew Shen GoodmanBelum ada peringkat
- Diabetic Foot InfectionDokumen26 halamanDiabetic Foot InfectionAmanda Abdat100% (1)
- Sustainable Marketing and Consumers Preferences in Tourism 2167Dokumen5 halamanSustainable Marketing and Consumers Preferences in Tourism 2167DanielBelum ada peringkat
- FOL Predicate LogicDokumen23 halamanFOL Predicate LogicDaniel Bido RasaBelum ada peringkat
- Lucid Motors Stock Prediction 2022, 2023, 2024, 2025, 2030Dokumen8 halamanLucid Motors Stock Prediction 2022, 2023, 2024, 2025, 2030Sahil DadashovBelum ada peringkat
- 100 Bedded Hospital at Jadcherla: Load CalculationsDokumen3 halaman100 Bedded Hospital at Jadcherla: Load Calculationskiran raghukiranBelum ada peringkat
- Statement of Purpose EitDokumen3 halamanStatement of Purpose EitSajith KvBelum ada peringkat
- TOPIC - 1 - Intro To Tourism PDFDokumen16 halamanTOPIC - 1 - Intro To Tourism PDFdevvy anneBelum ada peringkat
- PAASCU Lesson PlanDokumen2 halamanPAASCU Lesson PlanAnonymous On831wJKlsBelum ada peringkat
- Ten Lessons (Not?) Learnt: Asset AllocationDokumen30 halamanTen Lessons (Not?) Learnt: Asset AllocationkollingmBelum ada peringkat
- MAS-06 WORKING CAPITAL OPTIMIZATIONDokumen9 halamanMAS-06 WORKING CAPITAL OPTIMIZATIONEinstein Salcedo100% (1)