Psychology Final Paper On PTSD
Diunggah oleh
api-242593836Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Psychology Final Paper On PTSD
Diunggah oleh
api-242593836Hak Cipta:
Format Tersedia
Post-Traumatic Stress Disorder in
Iraq and Afghanistan War Veterans
Marta Lopez
Salt Lake Community College
Psychology 1010
November 16, 2016
Combat is often highly traumatic with exposure to immediate threats of injury and death. The
most common immediate psychological breakdown on the battlefield is known as combat stress
reaction (CSR; Solomon, 1993). With the end of the war, the debilitating effects of combat stress
may evolve in some cases, while in others they may form into posttraumatic stress disorder
(PTSD). PTSD may develop after the war and is marked by a range of debilitating symptoms,
which are often long lasting and resistant to treatment (American Psychiatric Association [APA],
2000). PTSD may follow increased physical and psychological health risk in combat soldiers and
PTSD was the most common mental health diagnosis in Operation Iraqi Freedom and Operation
Enduring Freedom veterans. Approximately 7.5% of U.S. Operation Iraqi Freedom, Operation
Enduring Freedom, and Operation New Dawn combat veterans develop posttraumatic stress
disorder. Despite psychological treatments and efforts to train providers many service members
do not complete enough treatment sessions for PTSD. Seventy percent of U.S. veterans of Iraq
experienced numerous life-threatening situations and reported higher rates of PTSD, depression,
and overall mental health risk. PTSD or two or mental disorders was highly
predictive of suicide in Iraq and Afghanistan U.S. veterans. Recovery from PTSD is
not returning to a pre-traumatic state but being able to function in life and maintain productive,
healthy relationships. Healthcare providers need to reinforce that seeking psychotherapy is a
normal part of recovery from life threatening combat traumas and explain that treatment makes
transition into civil life easier. Evidence shows that OIF/OEF veterans are less disturbed
psychologically and show higher rates of improvement than veterans from earlier wars can also
be shared to help veterans overcome fear of being stigmatized for seeking help (Fontana &
Rosenheck, 2008). The human cost of war is heavy, but evidence shows that suicide
prevention and PTSD recovery for combat-trauma survivors is increasingly possible with more
aggressive trauma-focused psychological treatments.
Bibliography
Goetter, E. M., Bui, E., Ojserkis, R. A., Zakarian, R. J., Brendel, R. W., & Simon, N. M. (2015).
A Systematic Review of Dropout From Psychotherapy for Posttraumatic Stress Disorder Among
Iraq and Afghanistan Combat Veterans. Journal Of Traumatic Stress, 28(5), 401-409.
Hassija C, Jakupcak M, Maguen S, Shipherd J. The Influence of combat and interpersonal
trauma on PTSD, depression, and alcohol misuse in U.S. Gulf War and OEF/OIF women
veterans. Journal Of Traumatic Stress [serial online]. April 2012;25(2):216-219. Available from:
Psychology and Behavioral Sciences Collection, Ipswich, MA. Accessed November 16, 2016.
Lee E. Complex Contribution of Combat-Related Post-Traumatic Stress Disorder to Veteran
Suicide: Facing an Increasing Challenge. Perspectives In Psychiatric Care [serial online]. April
2012;48(2):108-115. Available from: Psychology and Behavioral Sciences Collection, Ipswich,
MA. Accessed November 16, 2016.
Horesh D, Solomon Z, Ein-Dor T. DELAYED-ONSET PTSD AFTER COMBAT: THE ROLE
OF SOCIAL RESOURCES. Journal Of Community Psychology [serial online]. July
2013;41(5):532-548. Available from: Psychology and Behavioral Sciences Collection, Ipswich,
MA. Accessed November 16, 2016.
Anda mungkin juga menyukai
- Powerpoint Presentation-FinalDokumen26 halamanPowerpoint Presentation-Finalapi-242593836Belum ada peringkat
- Marta A. Lopez: ObjectivesDokumen1 halamanMarta A. Lopez: Objectivesapi-242593836Belum ada peringkat
- Homeland Security Emergency Management SLCCDokumen3 halamanHomeland Security Emergency Management SLCCapi-242593836Belum ada peringkat
- Marta Lopez Example of Powerpoint DocumentDokumen7 halamanMarta Lopez Example of Powerpoint Documentapi-242593836Belum ada peringkat
- Marta Lopez Example of Excel DocumentDokumen2 halamanMarta Lopez Example of Excel Documentapi-242593836Belum ada peringkat
- W 04 C 1 AppointmentsDokumen8 halamanW 04 C 1 Appointmentsapi-233253694Belum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Registered Pharmacist Affidavit FormatDokumen1 halamanRegistered Pharmacist Affidavit FormatSyed NawazBelum ada peringkat
- Acquired Brain Injury Early Rehabilitation and Long Term OutcomeDokumen46 halamanAcquired Brain Injury Early Rehabilitation and Long Term OutcomeVeena RaigangarBelum ada peringkat
- Arterial Blood GasDokumen55 halamanArterial Blood GasRathis Dasan100% (1)
- 5 NCLEX NeurologicalDokumen2 halaman5 NCLEX NeurologicalTina Willett-SmithBelum ada peringkat
- Nursing Process For Bipolar DisorderDokumen37 halamanNursing Process For Bipolar DisorderDENVER CABADINBelum ada peringkat
- Product Name:: Alaris™ GS, GH, CC, TIVA, PK, Enteral Syringe PumpDokumen14 halamanProduct Name:: Alaris™ GS, GH, CC, TIVA, PK, Enteral Syringe PumpSalim AloneBelum ada peringkat
- Angie ResumeDokumen2 halamanAngie Resumeapi-270344093Belum ada peringkat
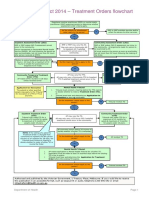
- Flowchart - Mental Health Act Treatment OrderDokumen1 halamanFlowchart - Mental Health Act Treatment OrderEdwin100% (1)
- Cambridge OET AnswersDokumen11 halamanCambridge OET AnswersNimraj Patel100% (3)
- Awesome Review 2018 Internal Medicine ABIM Board Review (PDFDrive)Dokumen592 halamanAwesome Review 2018 Internal Medicine ABIM Board Review (PDFDrive)saideh naghibiBelum ada peringkat
- Endoscopy Neo InfantsDokumen490 halamanEndoscopy Neo InfantsAlexandra NechiforBelum ada peringkat
- My Path to Becoming a Childhood Trauma PsychologistDokumen2 halamanMy Path to Becoming a Childhood Trauma PsychologistThivyana ShrreeBelum ada peringkat
- Format OpnameDokumen21 halamanFormat OpnamerestutiyanaBelum ada peringkat
- Chemotherapy Extravasation: Establishing A National Benchmark For Incidence Among Cancer CentersDokumen9 halamanChemotherapy Extravasation: Establishing A National Benchmark For Incidence Among Cancer CentersRiri AmalinaBelum ada peringkat
- The Comorbidities of Dysmenorrhea: A Clinical Survey Comparing Symptom Profile in Women With and Without EndometriosisDokumen14 halamanThe Comorbidities of Dysmenorrhea: A Clinical Survey Comparing Symptom Profile in Women With and Without EndometriosisSeptian WidiantoBelum ada peringkat
- Advocacy PaperDokumen3 halamanAdvocacy Paperapi-478583234Belum ada peringkat
- Keywords:-URI, Infection, Respiratory System, STP,: Mothers, Under Five ChildrenDokumen9 halamanKeywords:-URI, Infection, Respiratory System, STP,: Mothers, Under Five ChildrenInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- NCP For Acute Gastroenteritis (Pediatric)Dokumen6 halamanNCP For Acute Gastroenteritis (Pediatric)abcel76% (21)
- Bacterial Infection On Upper Respiratory Tract Hemofillus Moraxella Fusobacterium Ed 1Dokumen29 halamanBacterial Infection On Upper Respiratory Tract Hemofillus Moraxella Fusobacterium Ed 1Cintya Risti MawarniBelum ada peringkat
- Newborn Adaptation Assessment 2013 FINALDokumen21 halamanNewborn Adaptation Assessment 2013 FINALJennBelum ada peringkat
- Cipp 2015 AbstractsDokumen88 halamanCipp 2015 AbstractsBuyanaaRise100% (2)
- Jfe Science Abstracts 2019Dokumen31 halamanJfe Science Abstracts 2019api-308218624Belum ada peringkat
- Bertino2022 Book ClinicalEthicsForConsultationPDokumen181 halamanBertino2022 Book ClinicalEthicsForConsultationPJonatán Pérez RochaBelum ada peringkat
- Riza T. Calixtro: ObjectivesDokumen2 halamanRiza T. Calixtro: ObjectivesLorinel MendozaBelum ada peringkat
- Penguins Medicine August-SeptumberDokumen215 halamanPenguins Medicine August-SeptumberKhattabBelum ada peringkat
- The Medical Research Handbook - Clinical Research Centre PDFDokumen96 halamanThe Medical Research Handbook - Clinical Research Centre PDFDaveMartoneBelum ada peringkat
- HaemoparasitesDokumen82 halamanHaemoparasitesAshok WiselinBelum ada peringkat
- Review of Acrylic Removable Partial DenturesDokumen64 halamanReview of Acrylic Removable Partial Denturesasop060% (1)
- Final EthicsDokumen19 halamanFinal EthicsSheel Gautam100% (1)
- NURSING CARE PLAN RealDokumen3 halamanNURSING CARE PLAN RealJorossMabantaMarayanBelum ada peringkat