ME10!03!003 MMC Pathway2
Diunggah oleh
Indra WijayaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
ME10!03!003 MMC Pathway2
Diunggah oleh
Indra WijayaHak Cipta:
Format Tersedia
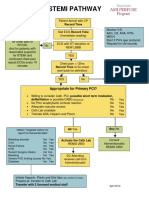
STEMI PATHWAY
ECG shows ST
depression, nonspecific
changes uninterpretible
or is normal - follow
local practice guideline
for chest pain or
R/O MI.
And for patients with
reasonable suspicion
for STEMI and
continued chest pain
repeat ECGs every 10
minutes
Patient Arrival with CP
Record Time
Stat ECG Record Time
(Immediate reading)
ECG with ST elevation or
NEW LBBB
No
Monitor V/S
Adm. O2, ASA, NTG,
MSO4
Start 2 PIVs (per protocol)
Request for old records
YES
Chest pain < 12hrs
Record Time of Sx onset
(see back for definition)
YES
No
Consult
Interventionalist
REMIS 2950
Appropriate for Primary PCI?
Willing to consider Cath, PCI, possible short term intubation,
defibrillation or possible CABG (5%chance)
No
No Prior anaphylactic contrast reaction
No
Adequate vascular access
No
Cath Lab available
No
Tolerate ASA, Heparin and Plavix
No
All Yes
Obtain Targeted history for
report to Interventionalist
Bleeding disorder
CVA
Renal Failure
HTN
Recent Surgery (2wks)
Bleeding
Severe PVD limiting access
Diabetes
No
No
No
No
No
No
No
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Activate the Cath Lab
REMIS 2950
Yes
Yes
Yes
Yes
Yes
Any No
Consult
Interventionalist
REMIS 2950
ED Attending
receives call from
Interventionalist
Initiate Heparin, Plavix and Stat labs (per protocol on back)
Prepare pt. transfer to Cath Lab
Transfer with 2 licensed medical staff
April 2012
Patients Emergently Reperfused by Facilities United for STEMI Excellence
Symptom Onset Definition
For patients reporting symptoms initially intermittent and subsequently constant, the onset time is
defined as the time of change from intermittent to constant symptoms.
Patients reporting symptoms that were initially mild and subsequently changed to severe, the
onset time is defined as the time of change in symptom severity.
For patients with both, the change in symptom severity is given preeminence in determining
symptom onset time.
~AHA/ACC definition
PHYSICIAN ORDER GUIDELINES FOR THE STEMI PATIENT
Ancillary
ECG 12 Lead STAT every 10 min with continuing CP
RN pulse oximetry, adjust oxygen flow to obtain saturation above 95%
Laboratory
CBC STAT
Troponin T STAT
CMP STAT
CK/CKMB STAT
PTT STAT
PRO Time STAT
IV Fluids
Periph Line #1. Start 0.9% N/S 1000 ml @100 ml/hr until D/C. Use 32 extension set
Periph Line #1 Start Nitroglycerin concentration B, (400 mcg/ml D5W)(100mg/250ml)
Titrate to SBP 90 and pain, Cont. until D/C
Medications
Aspirin 325mg STAT
Heparin Inj 60 u/kg IV push Now (maximum dose 4000u)
Metoprolol 5mg IV push every 5 minutes Times 3 as tolerated**
Plavix 600 mg P.O. now
Physician to Nurse
Record estimated height, weight, and allergies
Time permitting
Have patient void before leaving for Cath Lab
Foley catheter at patient request PRN
Mark peripheral pulses
Prepare patient for cath Lab, no clothing, plastic snap gown, portable 02 and monitor
**Consider BB for hypertensive patients
Important occurrences to document and time benchmarks
1. ED Arrival
2. Mode Patient arrived in ED ( PV, EMS w/ECG, EMS w/o ECG)
3. 1st ECG time, subsequent ECG times, 1st ECG time when STEMI is diagnosed
4. Any delays that occur in ED Pt refusal, cardiac arrest, intubation, etc.
5. Time patient departs the ED
Time goals Time is Muscle!
ED arrival to ECG within 10 minutes
Door to Balloon within 90 minutes
Anda mungkin juga menyukai
- Stemi Pathway: Record TimeDokumen2 halamanStemi Pathway: Record TimeOlga Jadha CasmiraBelum ada peringkat
- Induced HPDokumen4 halamanInduced HPmaddythedocBelum ada peringkat
- Iat Sepsis v7 3Dokumen1 halamanIat Sepsis v7 3api-296123515Belum ada peringkat
- Course in The WardDokumen4 halamanCourse in The WardJuan Miguel OliverosBelum ada peringkat
- Case Study Ws I Perki 2019Dokumen70 halamanCase Study Ws I Perki 2019Luh Leni AriniBelum ada peringkat
- CABG PathwayDokumen5 halamanCABG PathwayHardyansyah Harisman100% (1)
- Update in Stroke Management: David Lee Gordon, M.D., FAHADokumen43 halamanUpdate in Stroke Management: David Lee Gordon, M.D., FAHAMuhidin AeBelum ada peringkat
- Hospital Case PneumothoraxDokumen9 halamanHospital Case PneumothoraxJohn Rendel LopezBelum ada peringkat
- 12 Hours: Continue To Monitor: High-Risk NSTEACSDokumen1 halaman12 Hours: Continue To Monitor: High-Risk NSTEACSMeita ReligiaBelum ada peringkat
- AclsDokumen73 halamanAclsKamel Hady50% (2)
- Dka CmeDokumen32 halamanDka CmeAizura Abdul AzizBelum ada peringkat
- Plan - BS: in Active Phase of LabourDokumen5 halamanPlan - BS: in Active Phase of LabourniwasBelum ada peringkat
- Clinical Pathway StrokeDokumen8 halamanClinical Pathway StrokedjizhieeBelum ada peringkat
- Rhythm QRS Duration Atrial Rate QT Interval Ventricular Rate QRS Axis (Compute)Dokumen10 halamanRhythm QRS Duration Atrial Rate QT Interval Ventricular Rate QRS Axis (Compute)Luis PadillaBelum ada peringkat
- Pedia Notes - 112923Dokumen59 halamanPedia Notes - 112923RASHEED ALADDIN N GUIOMALABelum ada peringkat
- Course in The Ward Day 1Dokumen2 halamanCourse in The Ward Day 1PrincessLienMondejarBelum ada peringkat
- Chest Pain Protocol in EDDokumen3 halamanChest Pain Protocol in EDshahidchaudharyBelum ada peringkat
- LDLT V 3.0Dokumen49 halamanLDLT V 3.0anna67890Belum ada peringkat
- Medical Scenario 1Dokumen42 halamanMedical Scenario 1murphy 1087Belum ada peringkat
- Sample Case ScenarioDokumen8 halamanSample Case ScenarioJan Crizza Dale R. FrancoBelum ada peringkat
- Management of Acute Ischemic Stroke (AIS) DR GaneshDokumen69 halamanManagement of Acute Ischemic Stroke (AIS) DR GaneshDr Ganeshgouda MajigoudraBelum ada peringkat
- CORONARY ARTERY BYPASS GRAFT Nurse CareDokumen32 halamanCORONARY ARTERY BYPASS GRAFT Nurse CareCharisma Bailey Doody100% (1)
- Saudi CPR Guidlines in EnglishDokumen16 halamanSaudi CPR Guidlines in EnglishpiyushbamsBelum ada peringkat
- 14 MR Er Krs RDG ZakDokumen15 halaman14 MR Er Krs RDG Zaktriska antonyBelum ada peringkat
- STEMIDokumen34 halamanSTEMIefendiBelum ada peringkat
- ACP PocketbookDokumen91 halamanACP PocketbookjamesbeaudoinBelum ada peringkat
- CTA For IMDokumen46 halamanCTA For IMbsythaymdBelum ada peringkat
- Sample Case Presentation - Occult BacteremiaDokumen51 halamanSample Case Presentation - Occult BacteremiaPrecious Gutierrez BagazinBelum ada peringkat
- Admitting OrdersDokumen10 halamanAdmitting OrdersZinnia Zafra100% (1)
- Internal Medicine Case PresentationDokumen114 halamanInternal Medicine Case PresentationAyen FornollesBelum ada peringkat
- Sample Medical Guidelines: ACLS-BradycardiaDokumen2 halamanSample Medical Guidelines: ACLS-BradycardiaCheewin KhawprapaBelum ada peringkat
- Cerebrovascular Accident Case StudyDokumen5 halamanCerebrovascular Accident Case StudyShainae meriolesBelum ada peringkat
- Massive TransfusionDokumen104 halamanMassive Transfusionbingkydoodle1012Belum ada peringkat
- ACLS Pocket CardDokumen6 halamanACLS Pocket Cardno_spam_mang80% (5)
- AclsalgorithmsrapidratesDokumen8 halamanAclsalgorithmsrapidratesEvy Dwi RahmawatiBelum ada peringkat
- Nyeri DadaDokumen27 halamanNyeri DadaAji Setia UtamaBelum ada peringkat
- An Introduction To Obstetrical Emergencies: Charles D Giordano CRNA, MSNDokumen49 halamanAn Introduction To Obstetrical Emergencies: Charles D Giordano CRNA, MSNEffendi ZakriBelum ada peringkat
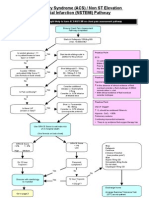
- Acs Nstemi PathwayDokumen3 halamanAcs Nstemi PathwayAliey's SKeplek NgeNersBelum ada peringkat
- Day in The Life 2019Dokumen30 halamanDay in The Life 2019Hoa Cỏ ĐậuBelum ada peringkat
- Management of Post Partum Haemorrhage 2017Dokumen30 halamanManagement of Post Partum Haemorrhage 2017Muhamad IrsyadBelum ada peringkat
- OB NotesDokumen9 halamanOB NotesJohn Christopher Luces100% (1)
- National Stroke Thrombolysis Guideline Template v9 5-12-13 FINAL 2Dokumen15 halamanNational Stroke Thrombolysis Guideline Template v9 5-12-13 FINAL 2Muhammad FauziBelum ada peringkat
- ShockDokumen75 halamanShockaulianmediansyahBelum ada peringkat
- ACS NSTEMI Clinical PathwayDokumen3 halamanACS NSTEMI Clinical PathwayXtiaRBelum ada peringkat
- Doctors OrderDokumen10 halamanDoctors OrderJan Mikhail Frasco100% (4)
- Remon CovidDokumen13 halamanRemon CovidJuli2022 Semnol-SemsaBelum ada peringkat
- ST-Elevation: N N N N N N N NDokumen5 halamanST-Elevation: N N N N N N N NningputBelum ada peringkat
- Cme Acs 2. Stemi (Izzah)Dokumen36 halamanCme Acs 2. Stemi (Izzah)Hakimah K. SuhaimiBelum ada peringkat
- Post-Cardiac Arrest Therapeutic Hypothermia Targeted Temperature Manangement (TTM) Quick SheetDokumen3 halamanPost-Cardiac Arrest Therapeutic Hypothermia Targeted Temperature Manangement (TTM) Quick SheetkimberlyBelum ada peringkat
- Doctor's OrderDokumen5 halamanDoctor's OrderJuan Miguel OliverosBelum ada peringkat
- Kawasaki DiseaseDokumen33 halamanKawasaki Diseasejoshianandk100% (2)
- Fundamental of Nursing Exam For 2nd Year HO StudentsDokumen3 halamanFundamental of Nursing Exam For 2nd Year HO StudentsZe RobelBelum ada peringkat
- Case PresentationDokumen22 halamanCase PresentationManjunath ArunachalamBelum ada peringkat
- Case Report:: Stemi Extensive Anterior OnsetDokumen43 halamanCase Report:: Stemi Extensive Anterior OnsetWardah MuskaBelum ada peringkat
- Weaning Ventilator Protocol For LiberationDokumen3 halamanWeaning Ventilator Protocol For LiberationBonny ChristianBelum ada peringkat
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingDari EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingBelum ada peringkat
- Hari2 4 Cita210413Dokumen45 halamanHari2 4 Cita210413Indra WijayaBelum ada peringkat
- Medication Safety ReconciliationDokumen117 halamanMedication Safety ReconciliationIndra WijayaBelum ada peringkat
- Automatic Stop OrdersDokumen3 halamanAutomatic Stop OrdersindraBelum ada peringkat
- Complication of Enteral Nutrition PDFDokumen3 halamanComplication of Enteral Nutrition PDFIndra WijayaBelum ada peringkat
- Pemateri Paralel SimposiumDokumen8 halamanPemateri Paralel SimposiumIndra WijayaBelum ada peringkat
- Prevention and Management of Procedural Pain in The Neonate An U 2016Dokumen13 halamanPrevention and Management of Procedural Pain in The Neonate An U 2016Indra WijayaBelum ada peringkat
- Accepted Manuscript: 10.1016/j.bpa.2016.12.002Dokumen21 halamanAccepted Manuscript: 10.1016/j.bpa.2016.12.002Indra WijayaBelum ada peringkat
- Afib Flowchart 1-21 SLWDokumen3 halamanAfib Flowchart 1-21 SLWIndra WijayaBelum ada peringkat
- Shock: GeneralDokumen2 halamanShock: GeneralIndra WijayaBelum ada peringkat
- Acute Heart Failure SyndromeDokumen1 halamanAcute Heart Failure SyndromeIndra WijayaBelum ada peringkat
- Posterior Cranial Fossa Anesthetic ManagementDokumen48 halamanPosterior Cranial Fossa Anesthetic ManagementDivya Rekha KolliBelum ada peringkat
- Alterations in Ventricular Pumping in Patients With Atrial Septal Defect at Rest, During Dobutamine Stress and After Defect ClosureDokumen10 halamanAlterations in Ventricular Pumping in Patients With Atrial Septal Defect at Rest, During Dobutamine Stress and After Defect ClosureYusrina Njoes SaragihBelum ada peringkat
- Hu Kira Inotrope and Vasopressor Use in CardiogenicDokumen7 halamanHu Kira Inotrope and Vasopressor Use in CardiogenicnhunhuochachBelum ada peringkat
- 35 AnswersDokumen7 halaman35 AnswersJasmine Nicole EnriquezBelum ada peringkat
- Ligasure Retractable Hook Information SheetDokumen2 halamanLigasure Retractable Hook Information SheetCristina PerjuBelum ada peringkat
- What Is Extracorporeal Cardiopulmonary Resuscitation?: Federico Pappalardo, Andrea MontisciDokumen5 halamanWhat Is Extracorporeal Cardiopulmonary Resuscitation?: Federico Pappalardo, Andrea MontisciPrajogo KusumaBelum ada peringkat
- Topic: Recent Advances - Cardiac CT: Journal ClubDokumen130 halamanTopic: Recent Advances - Cardiac CT: Journal Clubjai256Belum ada peringkat
- IGCSE - Bio - Lesson Plan 5 - Blood and CirculationDokumen3 halamanIGCSE - Bio - Lesson Plan 5 - Blood and CirculationHisokagenBelum ada peringkat
- Rhythm Control Versus Rate Control in Atrial Fibrillation - UpToDokumen39 halamanRhythm Control Versus Rate Control in Atrial Fibrillation - UpTohatsune100% (1)
- Iv AdministrationDokumen3 halamanIv AdministrationHBelum ada peringkat
- Thesis On Coronary Artery DiseaseDokumen7 halamanThesis On Coronary Artery Diseasesherielliottbillings100% (1)
- B22123 POCUS Workbook LinkedDokumen39 halamanB22123 POCUS Workbook LinkedDrMarcus KeyboardBelum ada peringkat
- Current Diagnosis and Treatment Cardiology 5Th Edition Michael H Crawford Full ChapterDokumen67 halamanCurrent Diagnosis and Treatment Cardiology 5Th Edition Michael H Crawford Full Chapterkaty.manley552100% (4)
- Diet For Cardiovaskular Disease - ErinetaDokumen8 halamanDiet For Cardiovaskular Disease - ErinetaErin NettaBelum ada peringkat
- Sop Vital SignDokumen5 halamanSop Vital SignKhoylilaBelum ada peringkat
- Bicuspid Aortic Valve and Dilatation of The Ascending Aorta (PDFDrive)Dokumen82 halamanBicuspid Aortic Valve and Dilatation of The Ascending Aorta (PDFDrive)jimurgaBelum ada peringkat
- VITAL SIGNS ReviewDokumen4 halamanVITAL SIGNS ReviewA CBelum ada peringkat
- Hallmark Signs and Symptoms PDFDokumen6 halamanHallmark Signs and Symptoms PDFjjBelum ada peringkat
- AXIOM Innovations: Low Dose - High PrinciplesDokumen32 halamanAXIOM Innovations: Low Dose - High PrinciplesDora Mejia RamirezBelum ada peringkat
- Vascular SurgeryDokumen458 halamanVascular SurgeryZoltan KardosBelum ada peringkat
- Pages From 5090 - w11 - QP - 22Dokumen1 halamanPages From 5090 - w11 - QP - 22Abrar JawadBelum ada peringkat
- Jamacardiology Jain 2021 BR 210009 1630597105.12009Dokumen5 halamanJamacardiology Jain 2021 BR 210009 1630597105.12009Amgad ElhajBelum ada peringkat
- Tani Et Al-2012-EchocardiographyDokumen7 halamanTani Et Al-2012-EchocardiographycesareBelum ada peringkat
- Assess Appropriateness For Clinical Condition. Heart Rate Typically 50/min If BradyarrhythmiaDokumen1 halamanAssess Appropriateness For Clinical Condition. Heart Rate Typically 50/min If BradyarrhythmiaatikaBelum ada peringkat
- Essentials of Diagnosis, Treatment, and Application of Cardiac and Peripheral Vascular DiseasesDokumen295 halamanEssentials of Diagnosis, Treatment, and Application of Cardiac and Peripheral Vascular DiseasesMichael BrunetBelum ada peringkat
- Supraventricular TachycardiaDokumen22 halamanSupraventricular TachycardiaFaza KahfiBelum ada peringkat
- Heart AttackDokumen5 halamanHeart AttackSherilBelum ada peringkat
- Entresto Marketing PlanDokumen1 halamanEntresto Marketing PlanSalmanAhmedBelum ada peringkat
- Incorrect - Right Answer: True: CorrectDokumen10 halamanIncorrect - Right Answer: True: CorrectAhmed - Sawalha100% (2)
- ME Sci 9 Q1 0103 PSDokumen18 halamanME Sci 9 Q1 0103 PScassiopeia bianca sartigaBelum ada peringkat