Cardiac Assessment
Diunggah oleh
Bryan Mae H. DegorioHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Cardiac Assessment
Diunggah oleh
Bryan Mae H. DegorioHak Cipta:
Format Tersedia
Cardiac Assessment gout, thrombophlebitis, collagen
diseases and bleeding disorders
By: Bryan Mae H. Degorio, RN, MAN
-surgical procedures, OB history
A. Risk Factor Analysis for Cardiovascular (complications of prev. pregnancy
Diseases due to CVD), outpatient interventions
and Dx procedures
Gender and Age
4. Medication- use of herbs, OTC and
Family history of hypertension recreation drug
Family history of heart attack -note for the route, dosage and
frequency of use
Family history of diabetes mellitus
5. Allergies- foods, drugs and note for
Cholesterol level manifestation during acute attack
Serum triglycerides D. Family Health History
Frequency of recreational activity • Provide insight for genetic,
environmental and lifestyle
Frequency of occupational exercise related diseases that contribute
to the occurrence of cardiac
Cigarette smoking problem
Stress at home and at work • Note for history of DM, HPN,
stroke and kidney disorders in
the family
Behavioral pattern
• Modifiable: stress, weight,
Use of oral contraceptives
cholesterol level, smoking and
abuse
Air pollution
• Non-modifiable: heredity, age,
Sleep Pattern
sex and race
B. Biographic and Demographic Data
E. Psychosocial History
- Name, age, sex, place of birth, race,
marital status, occupation and ethnic 1. Occupation- occupation stress, workload,
group job orientation (hard labor or sedentary
work), occupational hazard, jobs that
might not be compatible with existing
• Race- heart disease has twice
CVD
mortality to Native Americans
- Black die twice in stroke 2. Geographical Location- death caused by
compared to white cardiac event where they live (ex: US and
Philippines)
• Age- coronary artery disease are
3. Environment
more fatal to those who have
developed it young
• Home hazard such as area for
repair, presence of stairs, and
- cardiovascular disease are
light condition
common among the elderly
• Transportation (mode and access
-NO such this as congenital
to health care facility)
RHD
C. Past Health History • Neighborhood – noise pollution
• Access to facility- hospital,
1. Childhood Illnesses- previous
church, grocery and pharmacy
streptococcal infection and corrected
congenital heart diseases
• Nurturing environment-conducive
place for recovery
2. Immunization- cardiovascular disorders
needs revaccination of influenza every 6- 4. Exercise
10 years
• Type of exercise (isotonic,
3. Major Illnesses and Hospitalization- pt. isometric, isokinetic, passive,
with DM, obstructive lung diseases, aerobic and anaerobic)
kidney problem, anemia, HPN, stroke,
• Aerobic exercises – lower the • PB, pulses, jugular veins
chance of developing coronary
artery disease • Percuss, palpate and auscultate
the heart
• Note: anaerobic exercises-
increase of 50- 100% 0f the • Evaluation of edema
baseline HR at least 30 min. 3-5
times a week - How it is done?
• Consult physician if to be • Position client in supine position,
performed by 40 y/o and above stand at client’s side and elevate
bed
• Effects of sedentary lifestyle- • From head to toe
increases the lethality of MI
• Prepare the equipment-
5. Nutrition
stethoscope, penlight, ruler and
application stick
• Assess for caloric intake, Na,
cholesterol and saturated fat A. General Appearance
including caffeine intake
- Restlessness, can the client lie or sit
• Assess for economic and cultural upright, signs of pain, cyanosis, pallor
status before recommending for and presence of dyspnea
dietary changes
B. Head, Neck, Nails and Skin
• Foods such as fruits, vegetables,
low fat dairy products and • Head- eyes, earlobe, lips and buccal
saturated fat reduces the BP mucosa
significantly
a. Note for:
6. Habits
1. Arcus senilis – a light gray
• Smoking- nicotine and tar, assess ring around the iris (may
for # of packs/day and the how indicate cholesterol deposit)
long the client has been smoking
2. Xanthelasma – yellow raised
-it increases coronary artery
plaqued around the eyelids
disease and worsen hypertension
( duse to lipid deposits)
• Caffeine
• Skin- assess foe central and
-↑the risk peripheral cyanosis
atherosclerosis
a. Central cyanosis- assess the skin,
- ↑ HR and BP thus buccal mucosa and nasal mucosa
precipitating angina,
palpitation and dysrhythmias May indicate severe
heart and lung
- limit caffeine intake to 8 oz diseases
of coffee/day to those with
known diseases
b. Peripheral cyanosis- check the
nailbed, earlobe and lips
• Alcoholism- an intake of 100 mg
of alcohol (3 beer) may increase Indicates peripheral
heart rate and BP vasocionstriction (ex:
reynauds disease)
-ask for daily and weekly
consumption of alcohol • Nails
- Note: client may lie about the a. Capillary refill
type and amount of alcohol
consumed (denial) Or blunch test
Check capillary refill
before giving pulse
Physical Assessment
oximeter
- Cardiac Physical assessment includes the
Normal- 2 seconds
following:
b. Clubbing of finger
• General appearance
Normal- 160⁰ Hg systolic and more than 10 mm
Hg for diastolic pressure
indicates postural hypotension
180⁰ ↑- associated with
prolong oxygen Hypotension is usually
deprivation accompanied by 10-20% increase
in the heart rate
Can be due to COPD or
chronic anemia 2. Paradoxical Blood Pressure (Pulsus
Paradoxus)
c. Skin Turgor
An abnormal ↓of more than 10
Can be done by lifting a mm Hg of the systolic blood
fold of skin over the pressure during expiration
sternum or lower arm or
abdomen then release Associated with : pericardial
tamponade, constrictive
N⁰- goes back pericarditis and pulmonary
immediately (2-3 seconds hypertension
D. Pulses
Late- indicate
dehydration, malnutrition - Note bilateral pulse
and advancing age
d. Temperature
- Assess for pulse deficit by counting
apical pulse simultaneously with radial
pulse
Warm- associated with
venous disorders and - Note for weakness, thready and if it is
thyrotoxicosis bounding
Cold- arterial occlusive E. Neck
disorders and
hypothyroidism 1. Neck Veins
• Edema Neck vein distention can be used
to estimate CVP (Central Venous
a. Note for the location of edema: Pressure)
Lower extremities- The amount of distention reflects
mobile patients pressure and volume changes in
the Right Side of the Heart
Buttocks or scapular –
bed ridden patients
a. External jugular Vein- easy to
detect but can be altered by
Peripheral edema- RSCHF
little changes in position
Pulmonary edema
(dyspnea and crackles)-
b. Internal Jugular Vein- most
LSCHF reliable indication of CVP
C. Blood Pressure How it is done:
- Measure BP initially in both arm- identify
1. Elevate the head by 15-30⁰
presence of coarctation, aneurysm,
occlusive disorders and errors in reading
2. 45-90⁰ for those with
1. Postural Blood Pressure increase right atrial pressure
Done when extracellular volume 3. Internal jugular vein is just
depletion and decrease vascular located or lies deep in the
tone is suspected sternocleidomastoid
Position client in supine, sitting 4. Place the ruler on the sternal
and standing angle
5. Measure the pulsation
Note the position while taking
the blood pressure
6. N⁰- < 3-4 cm and an ↑
indicates RSCHF and
Abnormal finding: A drop in blood
pericardiac tamponade
pressure of more than 10-15 mm
7. Contralateral distention Pulmonic area- second
indicates onbstructions intercostals space Left of the
sternum
2. Carotid Artery
Erb’s Point- 3rd intercostals
Indicates adequacy of stroke
space Left of the sternum
volume and patency of the
arteries
Tricuspid area- 5th intercostal
Palpate one side at a time- space on the left side of the
simultaneous palpation sternum
stimulates carotid sinuses
causing bradycardia and sinus Mitral area- 5th intercostals
arrest space MCL left side
Note for Bruits- a blowing sound • Notes:
heard using the diaphragm of the
stethoscope Low pitch- Bell of the
stethoscope
It indicates narrowing of carotid
artery High pitch- diaphragm
F. Chest • Normal Heart Sounds:
1. Pericardium
First Heart Sound (S₁)
• Note for size, symmetry and evidence
a. Closure of the AV valves
of any pulsation – record its location
during ventricular
in relation to MCL and IS
contraction
• PMI (Point of Maximal Impulse)- 5th b. Heard best at mitral and
Intercostal Space MCL tricuspid region
It is associated to left c. It is equivalent to carotid
ventricular contraction artery pulsation or
upstroke of R wave in
Prominent in thin and QRS complex
obscure in fat of have large
breast d. Its intensity varies
according to certain
2 fingerbreadths below the pathologic condition such
nipple or 2 cm as stenosed AV valves
If deviated- can be due to
Right or left Sided Second Heart Sound (S2)
Cardiomegaly
a. The closure of the
• Note for presence of heaves or lifts semilunar valves during
ventricular relaxation
These are visible pulsation
b. It marks the end
associated to pulmonary
ventricular systole and
hypertension
onset of diastole
(ventricular filling)
• Thrills
c. Best heard in aortic and
These are rushing vibration pulmonic area using the
palpated in 5 cardiac diaphragm
auscultatory region that may
indicate murmur
Physiologic Splitting of S₂
Represent turbulent blood
a. Normal
flow through the heart
especially across an
b. Due to delayed closure of
abnormal heart valves
the pulmonic valves
2. Heart Sounds
c. Best heard during
inspiration
• Cardiac Auscultatory Site
- causes negative pressure in the thoracic
Aortic- second intercostals cavity→ pulling of blood on the right
space Right of the sternum
ventricles→ delayed emptying→ delayed a. Occurs in the later stage of diastole
closure of the pulmonic valves as heard during atrial contraction and active filling
as split second heard sound of the ventricles
• Abnormal Heart Sounds b. Heard immediately before S₁ and is
referred as atrial gallop
Pathologic Splitting
c. It is associated with ventricular
a. Wide splitting of S₂ hypertrophy, ischemia and fibrosis
b. Heard best during d. Never heard in the absence of atrial
inspiration and expiration contraction
with an increase during
inspiration
c. Associated with bundle • Quadruple Rhythm
branch block→ delayed
ventricular impulse Is noted when both S₃ and S₄
transmission→ delayed are audible
depolarization→ late
closure of pulmonic Client with this heart sound
valves often have tachycardia which
causes the diastolic filling
d. Associated with atrial sound to fuse forming
septal defects summation gallop that maybe
louder than S₁ and S₂
e. Fixed Splitting- due to
prolong emptying of the
right ventricle It resembles the sound of a
galloping horse
f. Paradoxical Splitting- due
to stenosed aortic valve • Clicks- are extracardiac sound
which is heard best that can be heard anytime
during expiration during the cardiac cycle in client
with aortic stenosis, valve
Gallop prolapsed and prosthetic valves
• Pericardial Friction Rub
a. Diastolic filling sounds
(S₃ and S₄)
Is produced by inflammation
of the pericardial sac
b. Due to sudden changes
of inflow volume causing
It is describe as a scratchy,
vibration of the valves
grating, rasping and much
and the ventricular
like “squeaky leather” sound
supporting structures
producing low pitch
Heard through the
sound either early (S₃) or
respiratory cycle not like
late (S₄) as diastole
pleural friction rub that occur
during inspiration
S₃
a. during passive and rapid filling of the The roughened parietal and
ventricles visceral layers of the
pericardium against each
other during cardiac motion
b. Early gallop that is heard during early
diastole
• Murmur
c. It follow immediately after S₂ and is dull Is heard as consequence of
and low pitch sound the turbulent blood flow
through the heart and blood
d. N⁰ in children and young adult vessels
e. Older than 30- it is considered a It is caused by:
characteristics of Left ventricular
dysfunction such as CHF, MI and Valvular a. ↑ rate or velocity of the
incompetence blood flow
S₄ b. Abnormal forward and
backward flow in the
stenosed or incompetent f. Grade VI- very loud,
valves heard even without
stethoscope
c. Dilated chamber
3. Lungs
d. Flow through abnormal
passage between heart • Tahcypnea
chambers (VSD, ASD and
TOF) • Crackles
Systolic murmur Adventitious sound heard in
a fluid filled lungs
a. Also called “benign
murmur” Common in LSCHF and heard
well in the base of the lungs
b. Often caused by vigorous
contraction of the • Blood Tinged Sputum
myocardium or strong
blood flow May indicate acute pulmonary
edema accompanied by crackles
c. Common in children and
adults younger than 50 • Cheyne-Stoke Respiration
and pregnant women
Deep breathing with period of
Diaslotic Murmur apnea
a. A pathologic
Common in patients with heart
condition and is produced
failure and anemia
by the mitral and
tricuspid valve stenosis 4. Abdomen
or aortic and pulmonic
insufficiency
• Ascitis
Note the characteristics:
due to fluid accumulation in the
peritoneal cavity
a. Loudness
can be due to chronic right
b. Location
ventricular failure
c. Pitch- high or low,
• Bowel Sounds
musical, harsh, blowing
or buzzing
↓ indicate potassium depletion
d. Place and duration
Loud bruits above the umbilicus
e. Quality- crescendo, may indicate aortic aneurysm or
decrescendo or plateau stenosis
f. Radiation- sounds radiate 5. Do the Following:
to other part of the body
(aortic radiates to carotid • Allen’s Test
artery and mitral murmur
radiates to axilla) Use to assess blood supply to the
upper extremities particularly the
g. Variation- changes occur hand
with movement
As the pt have close fist (tight)→
Grade the Loudness compress the ulnar and radial
artery→ have the client open his
a. Grade I- faint hands (n⁰- pale and mottled-
released the radial pulse- n⁰
b. Grade II- Faint heard hands regain color in about 6
immediately seconds)
c. Grade III- Moderately
loud
d. Grade IV- Loud
e. Grade V- Very loud, heard
only with stethoscope
• Homan’s sign
Pain in the calfs
Done by compressing the
gastrocnemius or quickly
dorsiflexion
Note for pain
Anda mungkin juga menyukai
- Adult III Cardiac Study GuideDokumen15 halamanAdult III Cardiac Study GuideNursingSchoolNotes100% (6)
- Cardiac MedicationsDokumen8 halamanCardiac Medicationsangeline totaram100% (2)
- Ecg Taking and Interpretation.... PowerpointDokumen37 halamanEcg Taking and Interpretation.... PowerpointJara Maris Moreno BudionganBelum ada peringkat
- Chest Tube Explanation by AllnursesDokumen3 halamanChest Tube Explanation by AllnursesYemaya84Belum ada peringkat
- Coumadin Dosing GuideDokumen3 halamanCoumadin Dosing Guidemorale28Belum ada peringkat
- Ecg InterpretationDokumen9 halamanEcg InterpretationEthan Rodriguez100% (3)
- This Study Resource Was Shared Via: Sinus BradycardiaDokumen3 halamanThis Study Resource Was Shared Via: Sinus BradycardiaPascal St Peter NwaorguBelum ada peringkat
- Arterial Lines in PACU: Presented by Autum Jacobs RN, BSNDokumen34 halamanArterial Lines in PACU: Presented by Autum Jacobs RN, BSNinuko1212Belum ada peringkat
- Nursing Care of PlanDokumen16 halamanNursing Care of PlanDbyBelum ada peringkat
- Respiratory DysfunctionDokumen1 halamanRespiratory Dysfunctionoxidalaj100% (3)
- Cardiac Dysrhythmia Chart Med Surg NUR4 PDFDokumen3 halamanCardiac Dysrhythmia Chart Med Surg NUR4 PDFlml100% (1)
- EKG Crash Course NuRsing 390 SMC - 4Dokumen57 halamanEKG Crash Course NuRsing 390 SMC - 4m1k0e100% (2)
- FLASH CardsDokumen3 halamanFLASH Cardsclarheena100% (2)
- Drug Cheat SheetDokumen2 halamanDrug Cheat SheetThomas Hart IIIBelum ada peringkat
- Cardiac Notes NursingDokumen16 halamanCardiac Notes NursingYemaya8494% (17)
- Critical Care Notes Clinical Pocket Guide - (Gastro-Urinary)Dokumen1 halamanCritical Care Notes Clinical Pocket Guide - (Gastro-Urinary)Britanny Nelson100% (1)
- HeartFailure Nursing FIK 2014Dokumen101 halamanHeartFailure Nursing FIK 2014Putri NurlaeliBelum ada peringkat
- DYSRHYTHMIAS (A.k.a. Arrhythmias) Disorders in TheDokumen3 halamanDYSRHYTHMIAS (A.k.a. Arrhythmias) Disorders in TheDarell M. Book100% (1)
- NursesDokumen2 halamanNursesDhingskie100% (5)
- Paeds Handbook Class2021 1568487638Dokumen30 halamanPaeds Handbook Class2021 1568487638kafosidBelum ada peringkat
- Surgical Adult Critical Care Ref SheetDokumen3 halamanSurgical Adult Critical Care Ref Sheetsgod34100% (1)
- CardiacDokumen10 halamanCardiacMarcus Reynolds100% (1)
- Concept Map 1Dokumen5 halamanConcept Map 1api-396919069Belum ada peringkat
- 11 Steps of ECG - Ali Alnahari PDFDokumen16 halaman11 Steps of ECG - Ali Alnahari PDFBìnhBelum ada peringkat
- Cardiac Rhythm Abnormalities GuideDokumen7 halamanCardiac Rhythm Abnormalities GuideAya KamajayaBelum ada peringkat
- EKG Interpretation NursingDokumen14 halamanEKG Interpretation NursingTanya ViarsBelum ada peringkat
- SIrs Sepsis Septic Shock MODSDokumen7 halamanSIrs Sepsis Septic Shock MODSAndrea Norton100% (5)
- Basic EKG Dysrhythmia IdentificationDokumen40 halamanBasic EKG Dysrhythmia IdentificationIlda Dhe Devis Spaho100% (1)
- Fundamentals Note TakingDokumen3 halamanFundamentals Note TakingJero BallesterosBelum ada peringkat
- EKG Quick Reference ChartDokumen4 halamanEKG Quick Reference ChartMildaBelum ada peringkat
- Physical Assessment Charting For NursingDokumen7 halamanPhysical Assessment Charting For NursingChristine Schroeder92% (13)
- Critical Care Calculations Study GuideDokumen6 halamanCritical Care Calculations Study GuideAja Blue100% (2)
- This Study Resource WasDokumen2 halamanThis Study Resource WasKimberly WhitesideBelum ada peringkat
- EKG Study GuideDokumen45 halamanEKG Study GuideBrawner100% (6)
- Cardiac DrugsDokumen5 halamanCardiac Drugseric100% (17)
- Critical Care - Hemodynamic Monitoring TableDokumen7 halamanCritical Care - Hemodynamic Monitoring TableVictoria Romero100% (2)
- Medsurg Cardio Ana&PhysioDokumen6 halamanMedsurg Cardio Ana&Physiorabsibala80% (10)
- Cardiac PacingDokumen4 halamanCardiac PacingmrygnvllBelum ada peringkat
- Latest Priorities in Critical Care Nursing 6th Edition Urden Test BankDokumen11 halamanLatest Priorities in Critical Care Nursing 6th Edition Urden Test BankBaxterBelum ada peringkat
- ABCDE Approach PDFDokumen3 halamanABCDE Approach PDFJohn SmithBelum ada peringkat
- Cardiac Study GuideDokumen11 halamanCardiac Study Guidesurviving nursing school100% (2)
- Dysrhythmia Recognition Pocket Reference Card PDFDokumen14 halamanDysrhythmia Recognition Pocket Reference Card PDFjenn1722100% (2)
- Cardiac Nursing II Study GuideDokumen6 halamanCardiac Nursing II Study GuiderunnermnBelum ada peringkat
- A Simplified ECG GuideDokumen4 halamanA Simplified ECG Guidejalan_z96% (25)
- Sepsis Nursing OutlineDokumen6 halamanSepsis Nursing OutlineSavannah Hayden100% (1)
- Zero Based BudgetDokumen9 halamanZero Based Budgetapi-447860598Belum ada peringkat
- Pharm 1.13 Antidepressant Cheat SheetDokumen1 halamanPharm 1.13 Antidepressant Cheat SheetEunice CortésBelum ada peringkat
- Boot Camp Hemodynamic MonitoringDokumen37 halamanBoot Camp Hemodynamic MonitoringTinaHo100% (7)
- Nursing Care of Cardiovascular DisordersDokumen38 halamanNursing Care of Cardiovascular Disordersprototypeallhell100% (1)
- Concept MapDokumen22 halamanConcept Mapapi-3017275530% (1)
- MAP, CO, and SV+HRDokumen11 halamanMAP, CO, and SV+HRjenwiley318096% (73)
- Cardiac DisordersDokumen15 halamanCardiac Disordersgold_enriquez100% (3)
- Acls LectureDokumen15 halamanAcls LectureVincent BautistaBelum ada peringkat
- Dimensional Analysis For Nursing StudentsDari EverandDimensional Analysis For Nursing StudentsBelum ada peringkat
- Cardiac Tamponade, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandCardiac Tamponade, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Torsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandTorsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideDari EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideBelum ada peringkat
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsDari EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsBelum ada peringkat
- Drug Cal - Practice TestDokumen2 halamanDrug Cal - Practice TestBryan Mae H. DegorioBelum ada peringkat
- Skeletal SystemDokumen27 halamanSkeletal SystemBryan Mae H. DegorioBelum ada peringkat
- Introduction To Change: Towards Excellence: "PHIC Accredited Health Care Provider"Dokumen3 halamanIntroduction To Change: Towards Excellence: "PHIC Accredited Health Care Provider"Bryan Mae H. DegorioBelum ada peringkat
- Allergies or Food Intolerances.: Therapeutic DietDokumen3 halamanAllergies or Food Intolerances.: Therapeutic DietBryan Mae H. DegorioBelum ada peringkat
- Drugs Affecting The Immune SystemDokumen4 halamanDrugs Affecting The Immune SystemBryan Mae H. DegorioBelum ada peringkat
- NMC Standards To Support Learning AssessmentDokumen85 halamanNMC Standards To Support Learning AssessmentBryan Mae H. DegorioBelum ada peringkat
- Systems of Measurement and Drug CalculationDokumen13 halamanSystems of Measurement and Drug CalculationBryan Mae H. DegorioBelum ada peringkat
- EmbryologyDokumen26 halamanEmbryologyBryan Mae H. Degorio100% (1)
- Worksheet in BloodDokumen12 halamanWorksheet in BloodBryan Mae H. DegorioBelum ada peringkat
- Disaster Nursing and ManagementDokumen39 halamanDisaster Nursing and ManagementBryan Mae H. DegorioBelum ada peringkat
- Sampling Process and Measurement ScaleDokumen18 halamanSampling Process and Measurement ScaleBryan Mae H. DegorioBelum ada peringkat
- APA Referencing 6th Ed Quick GuideDokumen2 halamanAPA Referencing 6th Ed Quick GuidehartymBelum ada peringkat
- Is Mentorship Right for Your Nursing CareerDokumen17 halamanIs Mentorship Right for Your Nursing CareerBryan Mae H. DegorioBelum ada peringkat
- Is Mentorship Right for Your Nursing CareerDokumen17 halamanIs Mentorship Right for Your Nursing CareerBryan Mae H. DegorioBelum ada peringkat
- Documentation and ReportingDokumen32 halamanDocumentation and ReportingBryan Mae H. Degorio100% (1)
- Bowel PreparationDokumen2 halamanBowel PreparationBryan Mae H. DegorioBelum ada peringkat
- Care of Patients with Musculoskeletal IssuesDokumen3 halamanCare of Patients with Musculoskeletal IssuesBryan Mae H. DegorioBelum ada peringkat
- Skeletal SystemDokumen27 halamanSkeletal SystemBryan Mae H. DegorioBelum ada peringkat
- APA Referencing 6th Ed Quick GuideDokumen2 halamanAPA Referencing 6th Ed Quick GuidehartymBelum ada peringkat
- Case Studies in Nursing Fundamentals - Trueman, Margaret Sorrell - Page 170-178Dokumen9 halamanCase Studies in Nursing Fundamentals - Trueman, Margaret Sorrell - Page 170-178Bryan Mae H. Degorio0% (3)
- The Adult LearningDokumen15 halamanThe Adult LearningBryan Mae H. DegorioBelum ada peringkat
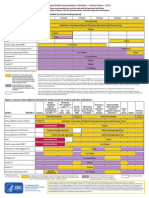
- Adult Immunization ScheduleDokumen3 halamanAdult Immunization ScheduleBryan Mae H. DegorioBelum ada peringkat
- Concept Mapping BMDDokumen4 halamanConcept Mapping BMDBryan Mae H. DegorioBelum ada peringkat
- Key Principles of Catholic Social TeachingDokumen1 halamanKey Principles of Catholic Social TeachingBryan Mae H. DegorioBelum ada peringkat
- Preceptor Handbook For Nursing EducationDokumen41 halamanPreceptor Handbook For Nursing EducationBryan Mae H. Degorio0% (1)
- 04 Tissue, Glands and MembranesDokumen52 halaman04 Tissue, Glands and MembranesBryan Mae H. Degorio100% (1)
- Human Immunodeficiency Virus /AIDSDokumen7 halamanHuman Immunodeficiency Virus /AIDSBryan Mae H. DegorioBelum ada peringkat
- Disaster Nursing and ManagementDokumen39 halamanDisaster Nursing and ManagementBryan Mae H. DegorioBelum ada peringkat
- Case Studies For Bowel EliminationDokumen2 halamanCase Studies For Bowel EliminationBryan Mae H. Degorio100% (2)
- Kidney Disease: Underwriter FocusDokumen3 halamanKidney Disease: Underwriter FocusBryan Mae H. DegorioBelum ada peringkat
- AIDA3 Pool Manual - EnglishDokumen97 halamanAIDA3 Pool Manual - EnglishHimar Mendoza MárquezBelum ada peringkat
- Etiology of Angina Pectoris With Special Reference To Coronary SPDokumen52 halamanEtiology of Angina Pectoris With Special Reference To Coronary SPNicholas MachadoBelum ada peringkat
- 10 Common EKG Heart RhythmsDokumen204 halaman10 Common EKG Heart RhythmsJames BrooksherBelum ada peringkat
- Anatomy NotebookDokumen39 halamanAnatomy Notebookrhowme100% (1)
- CardiologyDokumen7 halamanCardiologyEmanuela SîrbuBelum ada peringkat
- Simman 2024Dokumen54 halamanSimman 2024Doshi SahilBelum ada peringkat
- Natural Remedies Encyclopedia (PDFDrive) - 3Dokumen30 halamanNatural Remedies Encyclopedia (PDFDrive) - 3angelobuffaloBelum ada peringkat
- MCQ IM DepDokumen183 halamanMCQ IM DepHesham A100% (2)
- Self-propelled cono weeder evaluatedDokumen7 halamanSelf-propelled cono weeder evaluatedSapuniiBelum ada peringkat
- Brugada SyndromeDokumen13 halamanBrugada SyndromeBelajar100% (1)
- 466 Concept MapDokumen6 halaman466 Concept Mapapi-284107243Belum ada peringkat
- Can "Daniel's Diabetic Miracle" Naturally Heal Diabetes in As Little As 3 DaysDokumen33 halamanCan "Daniel's Diabetic Miracle" Naturally Heal Diabetes in As Little As 3 Daysaz75% (4)
- ECG ExaminationDokumen70 halamanECG ExaminationPercy Caceres OlivaresBelum ada peringkat
- Mitral Valve ReplacementDokumen44 halamanMitral Valve ReplacementYusardi R Pradana100% (1)
- TAVR CostsDokumen11 halamanTAVR CostsTom BiusoBelum ada peringkat
- Acute Coronary SyndromeDokumen24 halamanAcute Coronary SyndromeMuhammad Alauddin Sarwar100% (8)
- StemiDokumen35 halamanStemiIndra ChristiantoBelum ada peringkat
- 3 Rituals OF: Sex MagicDokumen14 halaman3 Rituals OF: Sex Magicjoel100% (1)
- IGCSE Biology Transport in Animals NotesDokumen62 halamanIGCSE Biology Transport in Animals NotesSir AhmedBelum ada peringkat
- Case Study On Neonatal SepsisDokumen19 halamanCase Study On Neonatal SepsisMary Menu100% (2)
- Answer Key CicDokumen3 halamanAnswer Key Cictiburshoc16Belum ada peringkat
- CHF Case StudyDokumen38 halamanCHF Case StudyMelissa David100% (1)
- The Human Heart: Presentation By: Zuhaib FayyazDokumen22 halamanThe Human Heart: Presentation By: Zuhaib Fayyazfdrz200887Belum ada peringkat
- Cardiac Catheterization: Why It's DoneDokumen3 halamanCardiac Catheterization: Why It's DoneRania S. HamdanBelum ada peringkat
- History Taking Complete KrishnaDokumen7 halamanHistory Taking Complete KrishnaMuhammad AfiqBelum ada peringkat
- CARDIAC MUSCLE STRUCTUREDokumen16 halamanCARDIAC MUSCLE STRUCTUREsentilbalan@gmail.comBelum ada peringkat
- Case Study RleDokumen25 halamanCase Study Rlelea jumawanBelum ada peringkat
- KatukiDokumen21 halamanKatukiShantu ShirurmathBelum ada peringkat
- Syllabus 112Dokumen9 halamanSyllabus 112Hassen Zabala100% (2)
- 12th Biology EngMed QueBank MSCERTDokumen48 halaman12th Biology EngMed QueBank MSCERTPratik PandeyBelum ada peringkat