Child - Major Burn PDF
Diunggah oleh
Aldith GrahamJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Child - Major Burn PDF
Diunggah oleh
Aldith GrahamHak Cipta:
Format Tersedia
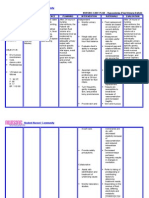
Alterations in Skin Integrity
NURSING CARE PLAN
GOAL
893
The Child with a Major Bur n Injury
INTERVENTION
RATIONALE
EXPECTED OUTCOME
1. Pain related to physical injury agents
NIC Priority Intervention: Pain
Management: Alleviation of pain or a
reduction in pain to a level of comfort
that is acceptable to the patient.
The child will verbalize adequate
relief from pain and will be able to
perform activities of daily living (ADLs).
NOC Suggested Outcome: Comfort
Level: Feelings of physical and
psychological ease.
Assess the level of pain frequently
using pain scales (see Chapter 9).
Pain scale provides objective
measurement. Pain is always
present, but changes location;
intensity may indicate
complications.
Cover burns as much as possible.
Temperature changes or movement
of air causes pain.
Change the childs position
frequently. Perform range-ofmotion exercises.
Reduces joint stiffness and prevents
contractures.
Encourage verbalization about
pain.
Provides outlet for emotions and
helps the child cope.
Provide diversional activities.
Helps lessen focus on pain.
Promote uninterrupted sleep with
use of medications.
Sleep deprivation can increase pain
perception.
Use analgesics before all dressing
changes and burn care.
Helps to reduce pain and decreases
anxiety for subsequent dressing
changes.
The child verbalizes adequate relief
from pain and is able to perform
ADLs.
2. Risk for Infection related to trauma and destruction of skin barrier
NOC Suggested Outcome: Risk
Control: Actions to eliminate or
reduce actual, personal, and
modifiable health threats.
NIC Priority Intervention: Infection
Protection: Prevention and early
detection of infection in a patient at
risk.
The child will be free of infection
during healing process.
Take vital signs frequently.
Increased temperature is an early
sign of infection.
Use standard precautions (gown,
gloves, mask) when wounds of a
major burn are exposed. Limit
visitors (no one with an upper
respiratory infection or other
contagious disease).
Reduces risk of wound
contamination.
Clip hair around burns.
Hair harbors bacteria.
Keep biosynthetic burn dressing
dry.
Helps reduce the number of
bacteria introduced to the burn
site.
Do not place the IV in any burned
area.
Reduces risk of wound
contamination.
Administer oral or IV antibiotics for
diagnosed infections as prescribed.
Antibiotics administered as
prescribed help to clear the
infection quickly.
The child either stays free of
secondary infection, or has infection
diagnosed and treated early.
3. Risk for Fluid Volume Imbalance related to loss of fluids through wounds and to subsequent excess fluid intake
NOC Suggested Outcome: To be
developed.
NIC Priority Intervention: To be
developed.
The child will maintain adequate
urine output.
Monitor vital signs, central venous
pressure, capillary refill time, pulses.
The child is initially at risk for
hypovolemic shock and needs fluid
resuscitation (see Chapter 10).
The child maintains normal urine
output and burn site edema is not
excessive.
(continued)
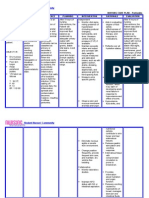
NURSING CARE PLAN
GOAL
The Child with a Major Burn Injury
INTERVENTION
RATIONALE
(continued)
EXPECTED OUTCOME
3. Risk for Fluid Volume Imbalance related to loss of fluids through wounds and to subsequent excess fluid intake (continued)
Administer IV and oral fluids as
ordered.
Careful calculation of fluid needs
and ensuring proper intake help
keep the child properly hydrated.
Estimate insensible fluid losses.
Losses are increased during the first
72 hours after burn injury; may
need replacement. Plasma is lost
through burn site because of
capillary damage.
Monitor intake and output.
The child is at risk for fluid overload
during hydration, and for edema in
the tissues at the burn site.
Weigh child daily.
Significant weight loss or gain can
help determine fluid imbalances.
Insert urinary catheter.
Helps maintain accurate output
measurement during critical care
stage.
Monitor for hyponatremia and
hypercalcemia (see Chapter 10).
Sodium is lost with burn fluid and
potassium is lost from damaged
cells, causing electrolyte
imbalances.
4. Altered Peripheral Tissue Perfusion related to mechanical reduction of venous and/or arterial blood flow (edema) of
circumferential burns
NIC Priority Intervention: Circulatory
Care: Promotion of arterial and
venous circulation.
The child will maintain adequate
perfusion in burned extremities.
NOC Suggested Outcome: Tissue
Perfusion (Peripheral): Extent to
which blood flows through the small
vessels of the extremities and
maintains tissue function.
Elevate extremities. Perform hourly
distal pulse checks. Notify the
physician of decreased or absent
pulses.
Elevation helps to reduce
dependent edema by promoting
venous return. Dependent edema
can constrict peripheral circulation.
Check eschar.
Eschar can constrict peripheral
circulation in edematous extremity.
The child has no episodes of poor
perfusion in the burned extremity.
5. Ineffective Breathing Pattern related to respiratory muscle fatigue due to smoke inhalation and airway edema
NIC Priority Intervention: Respiratory
Monitoring: Collection and analysis
of patient data to ensure airway
patency and adequate gas exchange.
The child will maintain or demonstrate
improvement in breathing pattern.
NOC Suggested Outcome: Vital
Signs Status: Temperature, pulse,
respiration, and blood pressure within
expected range for the individual.
Closely monitor quality of
respirations, breath sounds,
mucous secretions, pulse oximetry.
Excess fluid replacement can cause
pulmonary edema; toxins from
burning products can cause airway
inflammation.
Provide thorough pulmonary care.
Pulmonary care assists in removal
of secretions to prevent infection.
Elevate head of bed. Keep
intubation tube at bedside.
Dyspnea, nasal flaring, air hunger
(respiratory distress) may develop.
Administer corticosteroids, as
prescribed.
Reduces airway edema.
The child has regular and unlabored
breathing pattern.
6. Impaired Physical Mobility related to joint stiffness due to burns
NIC Priority Intervention: Exercise
Therapy, Joint Mobility: Use of
active or passive body movement to
maintain or restore joint flexibility.
NOC Suggested Outcome: Joint
Movement (Active): Range of
motion of joints with self-initiated
movement.
NURSING CARE PLAN
GOAL
The child will maintain maximum
range of motion.
in Skin Integrity 895
The Child with a MajorAlterations
Burn Injury
(continued)
INTERVENTION
Arrange physical and occupational
therapy twice daily for stretching
and range-of-motion exercises.
Splint as ordered. Encourage
independent ADLs.
RATIONALE
Good positioning, range-of-motion
exercises, and alignment prevent
contractures.
EXPECTED OUTCOME
The child maintains maximum range
of motion without contractures.
7. Altered Nutrition: Less than Body Requirements related to high metabolic needs
NOC Suggested Outcome:
Nutritional Status: Extent to which
nutrients are available to meet
metabolic needs.
NIC Priority Intervention: Nutrition
Management: Assistance with or
provision of balance dietary intake of
foods and fluids.
The child will maintain weight and
demonstrate adequate serum
albumin and hydration.
Provide an opportunity to choose
meals. Offer a variety of foods.
Provide snacks.
Encourages intake. General malaise
and anorexia lead to poor healing.
Encourage the child to have meals
with other children.
Socialization improves intake.
Provide a multivitamin supplement.
Vitamin C aids zinc absorption; zinc
aids in healing.
Substitute milk and juices for water.
Provide nasogastric feedings as
needed.
A child with a burn greater than
10% of BSA cannot usually meet
nutrition requirements without
assistance.
Weigh the child daily.
Provides objective evaluation.
The child maintains weight, adequate
hydration, normal serum albumin.
8. Anxiety (Child) related to threat to or change in health status
NOC Suggested Outcome: Coping:
Actions to manage stressors that tax
an individuals resources.
NIC Priority Intervention: Anxiety
Reduction: Minimizing
apprehension, dread, foreboding, or
uneasiness related to an unidentified
source of anticipated danger.
The child will verbalize reduced
anxiety.
Provide continuity of care
providers.
Helps to build a trusting
relationship.
Encourage parents to stay with the
child; calls from home; pictures
from classmates.
Familiar surroundings, people, and
items encourage relaxation.
Group tasks and activities.
Reduces overstimulation and
encourages rest.
The child expresses and shows signs
of reduced anxiety.
9. Anxiety (Parent) related to situational crisis
NOC Suggested Outcome: Anxiety
Control: Ability to eliminate or
reduce feelings of apprehension and
tension from an unidentified source.
NIC Priority Intervention: Anxiety
Reduction: Minimizing
apprehension, dread, foreboding, or
uneasiness related to an unidentified
source of anticipated danger.
Parents will verbalize decreased
anxiety.
Provide educational materials about
healing, grafting, dressing changes,
and course of action.
Knowledge reduces anxiety.
Be flexible when teaching parents
about wound care.
Adults learn in many different ways.
Provide referral to social services or
parent support group
Allows for venting of fears and guilt
feelings, and provides exchange of
ideas on dealing with
hospitalization and long-term care.
Parents state decreased anxiety.
895
Anda mungkin juga menyukai
- NCPsDokumen13 halamanNCPsRocel DevillesBelum ada peringkat
- Imbalanced NutritionDokumen2 halamanImbalanced NutritionRizza 이 동해 Ocampo100% (1)
- Diarrhea Care PlanDokumen2 halamanDiarrhea Care Planzepoli_zepoly6232100% (1)
- Nursing Care Plan: Assessment Diagnosis Inference Goal Intervention Rationale EvaluationDokumen4 halamanNursing Care Plan: Assessment Diagnosis Inference Goal Intervention Rationale EvaluationSugar Capule - ManuelBelum ada peringkat
- NCPDokumen2 halamanNCPNaidin Catherine De Guzman-AlcalaBelum ada peringkat
- NCP FVDDokumen1 halamanNCP FVDsisjing88510Belum ada peringkat
- Nursing Care Plan For Incarcerated Inguinal Hernia RightDokumen2 halamanNursing Care Plan For Incarcerated Inguinal Hernia RightTrisha Lapid MatulaBelum ada peringkat
- COLCHICINE pptx1800128929Dokumen15 halamanCOLCHICINE pptx1800128929April Mergelle LapuzBelum ada peringkat
- Imbalanced Nutrition Less Than Body RequirementsDokumen2 halamanImbalanced Nutrition Less Than Body RequirementsSundaraBharathiBelum ada peringkat
- NCP RiskDokumen2 halamanNCP RiskNorries Jonell CaballarBelum ada peringkat
- Nursing Care PlanDokumen7 halamanNursing Care PlanRhitzle Ann100% (1)
- Health Assessment FHP - Nutrition and MetabolismDokumen25 halamanHealth Assessment FHP - Nutrition and MetabolismKim DajaoBelum ada peringkat
- Deficit)Dokumen2 halamanDeficit)Lee DeeBelum ada peringkat
- Ineffective Peripheral Tissue Perfusion Related To Vasoconstriction Secondary To High Glucose Level.Dokumen6 halamanIneffective Peripheral Tissue Perfusion Related To Vasoconstriction Secondary To High Glucose Level.SAROL, RYAN CHRISTIAN B.Belum ada peringkat
- Nursing Care Plan: Histolytica, ADokumen4 halamanNursing Care Plan: Histolytica, AkristennemarieBelum ada peringkat
- Dental Prob NCPDokumen3 halamanDental Prob NCPx483xDBelum ada peringkat
- Assessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationDokumen6 halamanAssessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationimnasBelum ada peringkat
- Infectious Process Secondary To Acute Gastroenteritis Nagtatae Na Talaga Siya", Changed Diaper 3x With Loose and DeformedDokumen1 halamanInfectious Process Secondary To Acute Gastroenteritis Nagtatae Na Talaga Siya", Changed Diaper 3x With Loose and DeformedJoshua MendozaBelum ada peringkat
- Teething:diaper Dermatitis NCPDokumen2 halamanTeething:diaper Dermatitis NCPMARK OLVIER E. MELCHORBelum ada peringkat
- PeritonitisDokumen6 halamanPeritonitisDiane ArgoteBelum ada peringkat
- Revised NCPDokumen8 halamanRevised NCPKryza Dale Bunado BaticanBelum ada peringkat
- NCP DM and HCVDDokumen3 halamanNCP DM and HCVDMAYBELINE OBAOB100% (1)
- Nursing Care Plan For LYING inDokumen4 halamanNursing Care Plan For LYING inKarissa CiprianoBelum ada peringkat
- Compartment Syndrome NCP (PAIN)Dokumen2 halamanCompartment Syndrome NCP (PAIN)eunica16Belum ada peringkat
- Drug StudyDokumen4 halamanDrug StudyJames Lavarias SuñgaBelum ada peringkat
- Nursing Care PlanDokumen4 halamanNursing Care PlanJobelyn TunayBelum ada peringkat
- ncp#2Dokumen2 halamanncp#2khatz91Belum ada peringkat
- Imbalance Nutrition Lass Than Body Requirements Related To Loss of Appetite Due To Aging.Dokumen1 halamanImbalance Nutrition Lass Than Body Requirements Related To Loss of Appetite Due To Aging.Senyorita KHayeBelum ada peringkat
- Assessment Diagnosis Planning Intervention Rationale EvaluationDokumen4 halamanAssessment Diagnosis Planning Intervention Rationale EvaluationJhoizel VenusBelum ada peringkat
- Activity IntoleranceDokumen2 halamanActivity IntoleranceDiane AbanillaBelum ada peringkat
- Impaired Gas Exchange NCPDokumen3 halamanImpaired Gas Exchange NCPRomel BaliliBelum ada peringkat
- Case Study NCPDokumen4 halamanCase Study NCPKelly OstolBelum ada peringkat
- EsophagomyotomyDokumen3 halamanEsophagomyotomySamVelascoBelum ada peringkat
- This Study Resource Was: HypomagnesemiaDokumen1 halamanThis Study Resource Was: HypomagnesemiaMaica LectanaBelum ada peringkat
- NCP2 - DengueDokumen4 halamanNCP2 - DengueSummer SuarezBelum ada peringkat
- Nursing Care Plan Assessment Nursing Diagnosis Planning Implementation Rationale Evaluation Subjective: Objective: STG: at The End of 1 DependentDokumen1 halamanNursing Care Plan Assessment Nursing Diagnosis Planning Implementation Rationale Evaluation Subjective: Objective: STG: at The End of 1 DependentThomas FarrishBelum ada peringkat
- NCP For Dehydration 1Dokumen3 halamanNCP For Dehydration 1Khalid KhanBelum ada peringkat
- G-CFA Instructor Tab 6-2 Handout 2 Sample Adequate Nursing Care Plan-R6Dokumen2 halamanG-CFA Instructor Tab 6-2 Handout 2 Sample Adequate Nursing Care Plan-R6SriMathi Kasi Malini ArmugamBelum ada peringkat
- Knowledge DeficitDokumen5 halamanKnowledge DeficitteamstrocaBelum ada peringkat
- Case Pres A1-RhdDokumen11 halamanCase Pres A1-RhdCharm TanyaBelum ada peringkat
- Premenstrual Dysphoric DisorderDokumen11 halamanPremenstrual Dysphoric Disorderapi-3764215Belum ada peringkat
- Ineffective Airway Clearance NCPDokumen1 halamanIneffective Airway Clearance NCPBenz ParCoBelum ada peringkat
- Ineffective Health Management Related To Mrs. Gama: Provide The Client Enough Knowledge About The ProblemDokumen5 halamanIneffective Health Management Related To Mrs. Gama: Provide The Client Enough Knowledge About The ProblemAndrea Albester GarinoBelum ada peringkat
- Ncp. HyperDokumen2 halamanNcp. HyperZmiaBelum ada peringkat
- Emj Cases : Questions For Case 1Dokumen8 halamanEmj Cases : Questions For Case 1Azmyza Azmy100% (1)
- NCP Impaired ComfortDokumen2 halamanNCP Impaired ComfortGia P. de VeyraBelum ada peringkat
- L&D Careplan 1 KarenDokumen4 halamanL&D Careplan 1 KarenSimran SandhuBelum ada peringkat
- Cognitive Disorder QuizDokumen35 halamanCognitive Disorder QuizCamille Joy BaliliBelum ada peringkat
- Medication ThalassemiaDokumen3 halamanMedication ThalassemiaDivya ToppoBelum ada peringkat
- NCP Meningitis Sure NaniDokumen2 halamanNCP Meningitis Sure NaniARISBelum ada peringkat
- NCP BronchopneumoniaDokumen8 halamanNCP BronchopneumoniaCrisantaCasliBelum ada peringkat
- Peritonsillar AbscessDokumen2 halamanPeritonsillar AbscessKevin Leo Lucero AragonesBelum ada peringkat
- Family NCPcorrectDokumen6 halamanFamily NCPcorrectapi-3832358100% (11)
- Nursing Care Plan The Child With A Major Burn InjuryDokumen3 halamanNursing Care Plan The Child With A Major Burn InjuryPamela Soledad Delgado SuárezBelum ada peringkat
- Child Bronchiolitis 1Dokumen2 halamanChild Bronchiolitis 1sarooah1994100% (2)
- Post Assessment PediatricsDokumen4 halamanPost Assessment Pediatricscuicuita100% (4)
- Nursing Care PlanDokumen23 halamanNursing Care PlanLorielle HernandezBelum ada peringkat
- DiagnosisDokumen12 halamanDiagnosisHCX dghhqBelum ada peringkat
- Diagno SIS Planni NG Intervention Rationale Evaluati ONDokumen3 halamanDiagno SIS Planni NG Intervention Rationale Evaluati ONAnn Nicole G. NeriBelum ada peringkat
- Bedmaking PDFDokumen13 halamanBedmaking PDFAldith Graham100% (1)
- Deeper Devotions EbookDokumen32 halamanDeeper Devotions EbookAldith GrahamBelum ada peringkat
- Bed MakingDokumen13 halamanBed MakingAldith GrahamBelum ada peringkat
- Condom UseDokumen1 halamanCondom UseAldith GrahamBelum ada peringkat
- Csec Biology ExcretionDokumen11 halamanCsec Biology ExcretionAldith Graham100% (2)
- 09.Project-Hospital Management SystemDokumen37 halaman09.Project-Hospital Management Systemzahidrafique0% (1)
- A Huge Completely Isolated Duplication CystDokumen6 halamanA Huge Completely Isolated Duplication CystNurlyanti RustamBelum ada peringkat
- Historical and Contemporary Perspectives, Issues of Maternal and Child HealthDokumen96 halamanHistorical and Contemporary Perspectives, Issues of Maternal and Child HealthBindu Philip100% (1)
- Integrated Vector Control ProgramDokumen35 halamanIntegrated Vector Control ProgramKeerthi VasanBelum ada peringkat
- Deyo 1992Dokumen6 halamanDeyo 1992Wwwanand111Belum ada peringkat
- Approach To Peritoneal Fluid AnalysisDokumen10 halamanApproach To Peritoneal Fluid AnalysisLady BugBelum ada peringkat
- Science Grade 7 Second QuarterDokumen12 halamanScience Grade 7 Second QuarterAnneKARYLE67% (3)
- Preventing Hip Dysplasia BrochureDokumen2 halamanPreventing Hip Dysplasia Brochurepcr_22Belum ada peringkat
- Necrotizing Ulcerative GingivitisDokumen8 halamanNecrotizing Ulcerative GingivitisryanfransBelum ada peringkat
- Meconium-Stained Amniotic Fluid MSAFDokumen54 halamanMeconium-Stained Amniotic Fluid MSAFJhansi PeddiBelum ada peringkat
- CH 32 Gallbladder and Extrahepatic Biliary SystemDokumen33 halamanCH 32 Gallbladder and Extrahepatic Biliary SystemElisha BernabeBelum ada peringkat
- Management of C Shaped Canals: 3 Case ReportsDokumen3 halamanManagement of C Shaped Canals: 3 Case ReportsTaufiqurrahman Abdul Djabbar100% (1)
- Ramatu Kamara ResumeDokumen1 halamanRamatu Kamara Resumeapi-707616686Belum ada peringkat
- Osce Notes - Rac - Safina AdatiaDokumen35 halamanOsce Notes - Rac - Safina AdatiaTraventure 2000Belum ada peringkat
- MR - Kuldeep Pandya PDFDokumen1 halamanMR - Kuldeep Pandya PDFabhishek mayekarBelum ada peringkat
- Antibiotic Skin TestingDokumen8 halamanAntibiotic Skin TestingFitz JaminitBelum ada peringkat
- Dysbiosis of The Human Oral Microbiome During The Menstrual Cycle and Vulnerability To The External Exposures of Smoking and Dietary SugarDokumen14 halamanDysbiosis of The Human Oral Microbiome During The Menstrual Cycle and Vulnerability To The External Exposures of Smoking and Dietary SugarPaloma C. PeñaBelum ada peringkat
- Primer On Nephrology 2022Dokumen1.713 halamanPrimer On Nephrology 2022Maievp53100% (1)
- Psychiatry 101Dokumen17 halamanPsychiatry 101Vaso Talakvadze0% (1)
- MEAL (Psychiatric Nursing 2)Dokumen4 halamanMEAL (Psychiatric Nursing 2)Yucef Bahian-AbangBelum ada peringkat
- Kurva LubchencoDokumen3 halamanKurva LubchencoDanil Armand67% (3)
- Health Is WealthDokumen1 halamanHealth Is Wealthriana safrianiBelum ada peringkat
- Ultrasound GuidanceDokumen111 halamanUltrasound GuidanceRahmanandhikaBelum ada peringkat
- Breast Sarcoidosis An Extremely Rare Case of Idiopathic Granulomatous MastitisDokumen3 halamanBreast Sarcoidosis An Extremely Rare Case of Idiopathic Granulomatous MastitisInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Ventilation Cheat SheetDokumen1 halamanVentilation Cheat Sheetlizzy59683% (6)
- U.S. Patent 9,301,519, Entitled, Systems and Methods For Ex Vivo Organ Care, To Hassanein Et Al., Issued Apr. 5, 2016.Dokumen106 halamanU.S. Patent 9,301,519, Entitled, Systems and Methods For Ex Vivo Organ Care, To Hassanein Et Al., Issued Apr. 5, 2016.Anonymous a7S1qyXBelum ada peringkat
- Interstitial PXDokumen56 halamanInterstitial PXmenkir tegegneBelum ada peringkat
- Case Study Colorectal CancerDokumen23 halamanCase Study Colorectal CancerLeogalvez BedanoBelum ada peringkat
- Head TraumaDokumen4 halamanHead TraumaDaniel GeduquioBelum ada peringkat
- Lab Values: Interpreting Chemistry and Hematology For Adult PatientsDokumen36 halamanLab Values: Interpreting Chemistry and Hematology For Adult PatientsBrian Johnson100% (1)