Administration of Tauroursodeoxycholic Acid Enhances Osteogenic Differentiation of Bone Marrow-Derived Mesenchymal Stem Cells and Bone Regeneration
Diunggah oleh
Thanos86Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Administration of Tauroursodeoxycholic Acid Enhances Osteogenic Differentiation of Bone Marrow-Derived Mesenchymal Stem Cells and Bone Regeneration
Diunggah oleh
Thanos86Hak Cipta:
Format Tersedia
Bone 83 (2016) 7381
Contents lists available at ScienceDirect
Bone
journal homepage: www.elsevier.com/locate/bone
Original Full Length Article
Administration of tauroursodeoxycholic acid enhances osteogenic
differentiation of bone marrow-derived mesenchymal stem cells and
bone regeneration
Byung-Hyun Cha a,1, Moon-Joo Jung b,1, Bo-Kyung Moon a, Jin-Su Kim a, Yoonji Ma b, Yoshie Arai a,
Myungkyung Noh b, Jung-Youn Shin b, Byung-Soo Kim b,c,d,, Soo-Hong Lee a,
a
Department of Biomedical Science, College of Life Science, CHA University, Seongnam-si, Republic of Korea
Interdisciplinary Program for Bioengineering, Seoul National University, Seoul 151-744, Republic of Korea
c
School of Chemical and Biological Engineering, Seoul National University, Seoul 151-744, Republic of Korea
d
Bio-MAX Institute, Institute for Chemical Processes, Seoul National University, Seoul 151-744, Republic of Korea
b
a r t i c l e
i n f o
Article history:
Received 27 April 2015
Revised 24 August 2015
Accepted 20 October 2015
Available online 21 October 2015
Keywords:
Tauroursodeoxycholic acid
Mesenchymal stem cells
Apoptosis
Inammatory
Osteogenic differentiation
Bone tissue regeneration
a b s t r a c t
It is known that osteogenic differentiation of mesenchymal stem cells (MSCs) can be promoted by suppression of
adipogenesis of MSCs. We have recently found that the chemical chaperone tauroursodeoxycholic acid (TUDCA)
signicantly reduces adipogenesis of MSCs. In the present study, we examined whether TUDCA can promote
osteogenic differentiation of bone marrow-derived mesenchymal stem cells (BMMSCs) by regulating Integrin
5 (ITGA5) associated with activation of ERK1/2 signal pathway and thereby enhance bone tissue regeneration
by reducing apoptosis and the inammatory response. TUDCA treatment promoted in vitro osteogenic differentiation of BMMSCs and in vivo bone tissue regeneration in a calvarial defect model, as conrmed by microcomputed tomography, histological staining, and immunohistochemistry for osteocalcin. In addition, TUDCA
treatment signicantly decreased apoptosis and the inammatory response in vivo and in vitro, which is important to enhance bone tissue regeneration. These results indicate that TUDCA plays a critical role in enhancing
osteogenesis of BMMSCs, and is therefore a potential alternative drug for bone tissue regeneration.
2015 Elsevier Inc. All rights reserved.
1. Introduction
Tissue engineering to regenerate damaged or defective tissue is a
promising alternative to current clinical treatments [12]. In previous
decades, many clinicians and researchers working in the tissue engineering eld have reported meaningful results regarding the possibility
of inducing tissue regeneration using biomaterials and cells, including
synthetic/natural proteins and growth factors [25]. Although advances
in tissue engineering have improved the clinical treatment of specic
tissue defects, the broad application of tissue engineering is limited by
obstacles such as the functional and morphological maintenance of
newly-formed tissue.
Bone tissue engineering has been developed using various
approaches, such as biodegradable synthetic/natural polymer composites, bone inductive/conductive materials, and genetically modied
Correspondence to: B.S. Kim, Seoul National University, Gwanak-ro 1, Gwanak-gu,
Seoul 151-744, Republic of Korea.
Correspondence to: S.H. Lee, Department of Biomedical Science, CHA University, CHA
Bio Complex, 335 Pangyo-ro, Bundang-gu, Seongnam-si, Gyeonggi-do 463-400, Republic
of Korea.
E-mail addresses: byungskim@snu.ac.kr (B.-S. Kim), soohong@cha.ac.kr (S.-H. Lee).
1
Byung-Hyun Cha and Moon-Joo Jung contributed equally to this work.
http://dx.doi.org/10.1016/j.bone.2015.10.011
8756-3282/ 2015 Elsevier Inc. All rights reserved.
cells, for therapeutic applications [67]. However, the engineered tissues for bone repair often lack vascularity and mechanical strength,
and it is difcult to engineer the complex bone micro-architecture [8].
One major issue is that adipose tissue usually forms along with the
engineered or newly regenerated bone tissue [911]. Likewise, several
studies reported that the decrease in bone volume in age-related osteoporosis is usually accompanied by an increase in bone marrow adipose
tissue [1214]. For successful bone tissue regeneration, adipose tissue
formation at defective bone tissue must be reduced.
Recombinant bone morphogenetic protein (BMP)-2 has a powerful
osteoinductive capacity. Since 2002, BMP-2 has been available for
orthopedic use, particularly anterior lumbar interbody fusion in the
United States [1516], and has been linked with bone tissue regeneration [1718]. However, additional culture and treatment steps requiring
large amounts of expensive growth factors and cytokines, such as
BMP-2 and dexamethasone, which may be cytotoxic and inammatory, are required prior to the implantation of bone grafting materials in order to achieve therapeutic effects [1920]. Due to their
short half-life and high cost, treatment with cytokines cannot solve
the fundamental problems associated with bone tissue regeneration
[3]. Therefore, new drugs need to be discovered to enhance bone tissue
regeneration.
74
B.-H. Cha et al. / Bone 83 (2016) 7381
The chemical chaperone tauroursodeoxycholic acid (TUDCA) has
been approved by the USA Food and Drug Administration and in
Europe. TUDCA is widely used to treat cholelithiasis and cholestatic
liver disease [2122] because it can effectively attenuate endoplasmic reticulum (ER) stress, which is induced by the accumulation of
misfolded proteins in the ER, in liver tissue [2324]. Recent reports
revealed that TUDCA can also decrease the lipid content of adipocytes and reduce the body mass of obese humans [2526]. More
recently, we reported that TUDCA signicantly decreases in vitro
adipogenic differentiation of mesenchymal stem cells (MSCs) and
in vivo adipose tissue formation when injected [27]. It was reported
that osteogenic differentiation of mesenchymal stem cells (MSCs)
can be promoted by suppression of adipogenesis of MSCs [28].
TUDCA can inhibit ER stress-induced apoptosis by modulating the
binding of pro-apoptotic molecules to the mitochondria and the mitochondrial release of cytochrome C [2932]. In addition, TUDCA treatment dramatically decreases inammatory processes such as innate
immunity colitis and acute pancreatitis [3334]. [35]. Indeed, several
studies reported that TUDCA can inhibit or attenuate apoptosis and
inammation in various diseases and traumatic injuries [34,36]. In the
early phases of tissue regeneration, inammatory cells such as monocytes and macrophages, which participate in the inammatory response,
undergo apoptosis resulting in delayed tissue healing and regeneration.
[35]. Thus, it is important to prevent inammation and minimize proinammatory signaling in order to enhance bone tissue regeneration.
In the present study, we hypothesized that TUDCA treatment would
effectively enhance osteogenic differentiation of mesenchymal stem
cells (MSCs) and bone tissue formation by reducing apoptosis and inammation at the implantation site. The effect of TUDCA on bone tissue
regeneration has not been previously studied. We compared TUDCA
with the clinically available BMP-2 recombinant protein in terms of
bone tissue formation.
2. Materials and methods
2.1. Isolation and culture of mouse bone marrow mesenchymal stem
cells (mBMMSCs)
mBMMSCs were isolated from 8 weeks old of male Balb/c mice as
previously described [37]. After 8 h non-adhesive cells were washed
out with Dulbecco's Phosphate Buffered Saline (DPBS, Gibco BRL,
Gaithersburg, MD). The commercial mBMMSCs in immune response
experiments were purchased from Cyagen Biosciences (OriCell,
Guangzhou, China) and approval for their use in this project was obtained from the CHA University of Institutional Review Board.
mBMMSCs were cultured in the proliferation medium, Dulbecco's modied Eagle medium (DMEM, Gibco BRL) supplemented with 10% (v/v)
fetal bovine serum (FBS, Gibco BRL) and 100 units/ml penicillin (Gibco
BRL) in humidied air with 5% (v/v) CO2 at 37 C. The proliferation
medium was changed every two days.
2.2. In vitro osteogenic differentiation of mBMMSCs
Osteogenic differentiation of mBMMSCs was induced at a cell density of 2 104 cells/cm2 in osteogenic medium (DMEM supplemented
with 10%(v/v) FBS, 1% GlutaMAX (Gibco BRL), 0.2 mM ascorbic acid
(Sigma), 10 mM glycerol 2-phosphate (Sigma) and 100 units/ml penicillin (Gibco BRL)) with the presence or absence TUDCA for 21 days
after media change, respectively, and as follows:
Group 1: no TUDCA supplementation during osteogenic medium,
Group 2: 10 nM TUDCA supplementation during osteogenic medium,
Group 3: 100 nM TUDCA supplementation during osteogenic
medium,
Group 4: 300 nM TUDCA supplementation during osteogenic
medium.
Each proliferation and differentiation medium was changed every
two days.
For detection of Calcium deposits, differentiated mBMMSCs were
xed in 10% formalin for 30 min at room temperature (RT). After
xation, 2% (v/v) of Alizarin Red S staining solution was added to
xed mBMMSCs and incubated at RT in the dark for 45 min. The staining
solution was removed and washed three times with deionized water.
The microscopic images were obtained using microscope (IX71 inverted
microscope, Olympus, Tokyo, Japan). Alizarin Red S was extracted using
10% (v/v) of cetylpyridinium chloride (CPC) for the quantication of
calcium deposits and the absorbance was measured at 562 nm using
microplate reader (Molecular devices, CA, USA).
2.3. MEK-1/2 inhibition of mBMMSCs during in vitro
osteogenic differentiation
Osteogenic differentiation of mBMMSCs was induced at a cell density of 2 104 cells/cm2 in osteogenic medium (as previously described)
with the presence or absence TUDCA for 3 days after media change,
respectively, and as follows:
Group 1: no TUDCA supplementation during osteogenic medium,
Group 2: 300 nM TUDCA supplementation during osteogenic
medium,
Group 3: 300 nM TUDCA supplementation during osteogenic medium with 20 M U0126 (MEK-1/2 inhibitor, Abcam).
2.4. Reverse transcription-polymerase chain reaction (RT-PCR) and
quantitative real-time PCR
Total RNA was extracted from transfected cells using TRIzol
(Invitrogen) and 2 g of total RNA was used for cDNA synthesis
with RT-PreMix (Bioneer, Daejeon, Korea). PCR was performed
with PCR-PreMix (Bioneer) under standard PCR conditions: BCL2associated X protein (Bax), B cell leukemia/lymphoma 2 (Bcl-2),
interleukin 1 beta (IL-1), tumor necrosis factor-alpha (TNF), and
glyceraldehyde-3-phosphate dehydrogenase (GAPDH) are shown in
Supplementary Table 1. PCR cycles consisted of an initial denaturation
step at 94 C for 5 min, followed by 32 amplication cycles consisting
of 30 s of denaturation at 94 C, 30 s of annealing at 62 C, and 1 min
of extension at 72 C. Last, a nal extension was performed at 72 C
for 10 min. PCR products were analyzed by UV irradiation on a 1.2%
agarose gel stained with ethidium bromide. For quantitative real-time
PCR analysis, gene-specic primers were designed to amplify runtrelated transcription factor 2 (Runx2), IL-1, TNF and GAPDH. Primer
pairs are as follows: Runx2 (5-TCC ACA AGG ACA GAG TCA GA-3, 5-TGG
CTC AGA TAG GAG GGG TA-3), IL-1 (5-CAA CCA ACA AGT GAT ATT CTC
CAT G-3, 5-GAT CCA CAC TCT CCA GCT GCA-3), TNF (5-GCG GTG CCT
ATG TCT CAG-3, 5-GCC ATT TGG GAA CTT CTC ATC-3) and GAPDH (5ACA TCG CTC AGA CAC CAT G-3, 5-TGT AGT TGA GGT CAA TGA AGG
G-3). All amplications were performed in a nal reaction mixture
(20 l) containing 1 nal concentration of SYBR supermix, 500 nmol/l
of gene-specic primers, and 1 ml of template, using the following conditions: an initial denaturation at 95 C for 1 min, followed by 45 cycles
of 95 C for 15 s, 56 C for 15 s, and 72 C for 15 s, with a nal extension
at 72 C for 5 min. After amplication, the baseline and threshold levels
for each reaction were determined using the company's software package (Exicycler 96; Bioneer). For validation of polymerase chain reaction
(PCR), amplied products were separated on 1% agarose gels and visualized by ethidium bromide staining.
2.5. Western blot analysis
Cells were washed with DPBS, lysed with 200 l of RIPA buffer, and
centrifuged at 13,000 rpm for 20 min. Supernatant was collected in
1.5 ml tube. Protein concentration was determined using BCA assay kit
B.-H. Cha et al. / Bone 83 (2016) 7381
(Life Technologies, IL, USA). 20 g of total protein of samples was separated by SDS-polyacrylamide gel electrophoresis (PAGE) and then these
proteins were transferred to nitrocellulose (NC) membranes. Protein
transferred membranes were blocked with 5% of skim milk in TBS
containing 0.1% Tween-20 (TBS-T) for 30 min. Membranes were
washed three times with TBS-T and incubated with primary antibody
in 5% skim milk in TBS-T at 4 C for overnight. After overnight incubation,
membranes were washed three times with TBS-T and incubated with
secondary antibody in 5% skim milk in TBS-T at RT for 1 h. Immunoreactivity was detected using Amersham ECL Select Western blotting
Detection Reagent (GE Healthcare Life Sciences, UK) and by ChemiDocTM
XRS+ System (Bio-rad, CA, USA). The anti-ERK and anti-pERK antibody
were obtained from cell signaling technology. The anti-integrin 5
(ITGA5) antibody was obtained from Millipore. The horseradish
peroxidase-conjugated anti-mouse IgG secondary antibody and antirabbit IgG were obtained from Santa Cruz.
2.6. Scaffold implantation to mouse calvarial defect model
Type I collagen sponges (CollaCote, Integra LifeSciences Corporation, Plainsboro, NJ, USA) were adjusted to the proper dimension
(5 mm in diameter, 1 mm in thickness). Tauroursodeoxycholic acid
(TUDCA), BMP-2, and ursodeoxycholic acid (UDCA) were purchased
from Calbiochem (Product # 580549, Calbiochem, San Diego, CA,
USA), R&D systems (produced by CHO cells, Minneapolis, MN, USA),
and Sigma-Aldrich (Product # U5127, Sigma-Aldrich, St. Louis, MO,
USA), respectively.
A mouse calvarial defect model was fabricated using six-weekold mice from the Institute of Cancer Research (Koatech, Sungnam,
Kyunggi-do, South Korea) as previously described [38]. Mice were
anesthetized with xylazine (20 mg/kg) and ketamine (100 mg/kg),
and their scalp hair was shaved. From the nasal bone to the superior
nuchal line, a 2 cm longitudinal skin incision was made in the middle
of the cranium. The periosteum was elevated, and the surface of the
parietal bone was exposed. Two critical-sized (4 mm in diameter)
calvarial defects were created on the cranium using a surgical trephine burr (Ace Surgical Supply Co., Brockton, MA, USA) and a lowspeed micrometer. The collagen sponge scaffolds were loaded with
25 l of DPBS, 25 l of DPBS containing 6.25 g (500 M) TUDCA,
1 g or 3 g of BMP-2, or 25 l of DPBS containing 4.91 g (500 M)
UDCA, and then implanted to the defect regions. For the TUDCA multiple injection group, 25 l of DPBS containing 6.25 g (500 M)
TUDCA was injected to each of the implanted scaffolds every other
day for 14 days. TUDCA, an osteoinductive candidate, was injected
for 14 days because osteogenic differentiation of MSCs takes a couple
of weeks [39]. In some mice, scaffolds were not implanted (no scaffold group). The scalp was closed with resorbable 60 Vicryl sutures
(Ethicon, Somerville, NJ, USA).
To compare the bone regeneration efcacy of TUDCA and UDCA,
after surgery, 25 l of DPBS containing 6.25 g (500 M) TUDCA or
25 l of DPBS containing 4.91 g (500 M) UDCA was injected to each
of the implanted scaffolds every other day for 14 days. All the animal
experiments were approved by the Institutional Animal Care and Use
Committee of Seoul National University (SNU-120220-3).
2.7. In vivo bone formation analysis
Following implanted at calvarial defect of mouse for 1 week and 8
weeks, the specimens were decalcied using decalcication solution
(Sigma-Aldrich, USA), dehydrated using alcohol and xylene, and
embedded in parafn. The specimens were sectioned transversely to
obtain 4-m-thick sections. The sections were stained with Goldner's
Trichrome staining, and microscopic images were obtained using microscope (IX71 inverted microscope, Olympus). The bone formation
area was determined using Adobe Photoshop software, and showed as
75
the percentage of new bone area in the calvarial defect area [(new
bone area / calvarial defect region area) 100%] [40].
2.8. Micro-CT examination
Eight weeks after implantation, the mice were sacriced. Their skulls
were harvested and xed in 4% (v/v) paraformaldehyde. The degree of
bone formation at the critical-sized calvarial defects was estimated by
micro-computed tomography (micro-CT) scan. Micro-CT images were
obtained by micro-CT scanner (SkyScan-1076, SkyScan, Kontich,
Belgium, voltage of 40 kV, current of 0.2 mA) and CT-analyzer software
program (CT-An, SkyScan). The bone regeneration volume was
determined by analyzing the images using Adobe Photoshop software
(Adobe Systems Inc., San Jose, CA, USA), and expressed as the percentage of new bone volume in the calvarial defect region [(new
bone volume / calvarial defect volume) 100%].
2.9. Terminal deoxynucleotidyl transferase dUTP nick end labeling
(TUNEL) assay
Sections, prepared as described above, were deparafnized and
hydrated by sequential incubations in xylene and ethanol. After being
washed with DPBS for 2 min, the sections were pre-blocked with 3%
H2O2 for 10 min. DNA fragmentation was determined by TUNEL as
described by the manufacturer (Roche Applied Science, Mannheim,
Germany). Fluorescent images were obtained using a Nikon microscope
Eclipse 55i (Nikon, Kanagawa, Japan).
2.10. Immunohistochemical staining
Sections were deparafnized and hydrated by sequential incubations in xylene and ethanol. After being washed with DPBS for 2 min,
the sections were pre-blocked with 3% H2O2 for 10 min. Following
application of the primary antibody against IL-1 (Santa Cruz Biotechnology, CA), TNF (Santa Cruz Biotechnology), the sections were incubated for 1 h at RT, followed subsequently by application of FITC- or
Texas Red-conjugated secondary antibodies (Abcam, Cambridge, MA).
Signals of IL-1 and TNF were quantitatively analyzed using NIH
ImageJ software. For immunohistouorescence analysis of new bone,
the 4-m-thick sections were stained with anti-osteocalcin (OC) antibody (Abcam, Cambridge, UK). Rhodamine-conjugated secondary antibody (Jackson ImmunoResearch Laboratories Inc., West Grove, PA, USA)
was applied to obtain the uorescent signals of OC. Thereafter, the sections were counterstained with 4, 6-diamidino-2-phenylindole (DAPI,
Vector Laboratories Inc., Burlingame, CA, USA), and examined with a
uorescence microscope (IX71 inverted microscope, Olympus).
2.11. Statistical analysis
At least three independent sets of experiments for each condition
were performed in triplicate. Data were pooled and statistically
expressed as mean standard error (S.E). One-way analysis of variance
(ANOVA) was used for analysis of quantitative values, and the Tukey's
honestly signicant difference post hoc test was used for all pair-wise
comparisons among groups. Differences were considered signicant at
p b 0.05. The SPSS software package (version 12.0; SPSS Inc., Chicago,
http://www.spss.com) was used for the statistical tests.
3. Results
3.1. TUDCA promotes osteogenic differentiation of mouse bone marrow
mesenchymal stem cells (mBMMSCs) by Integrin 5 (ITGA5) and activation
of ERK1/2-MAPKs signal pathway
mBMMSCs were seeded at a density of 2 104 cells/cm2 in culture
plates and grown for 3 days. Real-time PCR analysis revealed that
76
B.-H. Cha et al. / Bone 83 (2016) 7381
treatment with 300 nM TUDCA increased expression of the osteogenic marker RUNX2 in comparison to treatment with 10 or 100 nM
TUDCA (Fig. 1A). To conrm that this effect was due to activation of
the osteogenic differentiation signal cascade, cells were co-treated
with a MEK-1/2 inhibitor (U0126) and 300 nM TUDCA. RUNX2 expression was signicantly lower in cells co-treated with a MEK-1/2 inhibitor
and 300 nM TUDCA than in cells treated with 300 nM TUDCA alone
(Fig. 1B). As seen in Fig. 1C, we also analyzed the calcium deposits
from differentiated mBMMSCs, by measuring Alizarin Red S staining.
300 nM TUDCA group distinctly exhibited more Alizarin Red S stained
parts compared with the other group, supported by quantifying Alizarin
Red S. To conrm the mechanism of TUDCA on osteogenic differentiation of mBMMSCs, we tested the expression of ITGA5, p-ERK, and total
ERK at no treatment, 10, 100, and 300 nM TUDCA group. Both protein
expression of ITGA5 and p-ERK were gradually increased in the presence of TUDCA group, especially at 300 nM TUDCA group (Groups 4).
3.2. TUDCA suppresses apoptosis in calvarial defects of mice
To explore the apoptotic effect of TUDCA in calvarial defects, we
injected phosphate-buffered saline (DPBS; TUDCA ()) or 500 mol/l
TUDCA every 2 days for a total of 7 days into the calvarial defects of
mice implanted with a type I collagen sponge scaffold. In tissue sections,
many TUNEL-positive nuclei (green), indicative of apoptotic cells, were
observed in TUDCA (), while only a few were observed in TUDCA (+)
as the TUDCA-treated group (Fig. 2A).
Expression of the pro-apoptotic gene BAX and the anti-apoptotic
gene Bcl-2 was lower and higher, respectively, in the TUDCA (+)
group than in TUDCA () group (Fig. 2B). Real-time PCR analysis revealed that the ratio of BAX to Bcl-2 was signicantly (p b 0.05) lower
in the TUDCA (+) group (0.001 0.001) than in the TUDCA ()
group (1.565 0.145). These results demonstrate that treatment of
the implantation site with TUDCA decreases the number of apoptotic
cells and the level of pro-apoptotic gene expression.
3.3. TUDCA suppresses inammation in mBMMSCs in vitro and in mouse
calvarial defects in vivo
To test whether TUDCA treatment decreases or increases the inammatory response in vitro, mBMMSCs were seeded at a density of 1 103
cells/cm2 in culture plates and grown in osteogenic medium containing
0, 10, 100, or 300 nM TUDCA for 7 days. Thereafter, RT-PCR analysis of
the pro-inammatory markers interleukin (IL)-1 and tumor necrosis
factor (TNF) was performed. mRNA expression of IL-1 was lower
in all the TUDCA (+) group than in TUDCA () as a non-treated
group (0.959 0.150), and was signicantly reduced in cells treated
with 100 nM TUDCA (0.659 0.024) (Fig. 3a, upper panel). In addition,
mRNA expression of TNF was signicantly lower in all the TUDCA (+)
groups (10 nM, 0.238 0.025; 100 nM, 0.494 0.028; 300 nM, 0.157
0.023) than in the TUDCA () group (2.210 0.703) (Fig. 3A). This
demonstrates that TUDCA plays a critical role in reducing the levels of
pro-inammatory factors in MSCs. To explore the effect of TUDCA
treatment on the inammatory response in calvarial defects in vivo,
we implanted a TUDCA-laden type I collagen sponge scaffold into the
calvarial defect site of mice for 7 days as described earlier. Immunohistochemical analysis of tissue sections revealed that levels of the proinammatory proteins IL-1 (green) and TNF (red) were lower in
the TUDCA (+) group than in the TUDCA () group (Fig. 3B). Quantitative expression of IL-1 and TNF was signicantly reduced in the
TUDCA (+) group than TUDCA () group (p b 0.05) (Fig. 3C). Consistent with this, gene expression of IL-1 and TNF was signicantly
reduced in the TUDCA (+) group (p b 0.05) (Fig. 3D). Quantitative
gene expression data showed that IL-1 expression was approximately
2.1-fold lower in the TUDCA-treated group (0.261 0.013) than in the
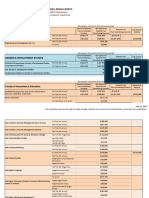
Fig. 1. Effect of TUDCA on osteogenic differentiation of mBMMSCs by Integrin 5 (ITGA5) and activation of ERK1/2-MAPKs signal pathway. (A) Real-time PCR analysis of the adipogenic
marker gene RUNX2 in mBMMSCs treated with various concentrations of TUDCA for 3 days (*, p b 0.05). (B) Real-time PCR analysis of the adipogenic marker gene RUNX2 in mBMMSCs
treated with 300 M TUDCA with or without a MEK-1/2 inhibitor (U0126) for 3 days. Data are the mean standard error of the mean (*, p b 0.05). (C) Histologic examination of calcium
deposit, stained by Alizarin Red S staining and quantied (scale bar = 100 m; *, p b 0.05). (D) The expression of ITGA5, p-ERK and total ERK was determined by Western blotting.
B.-H. Cha et al. / Bone 83 (2016) 7381
77
Fig. 2. Suppression of apoptosis by TUDCA. (A) TUNEL assay of in vivo calvarial defect sites treated with or without TUDCA. (B) RT-PCR analysis of anti-apoptotic (Bcl-2) and pro-apoptotic
(BAX) genes in in vivo calvarial defect sites treated with or without TUDCA. The BAX/Bcl-2 expression ratio was assessed by quantifying band intensities (scale bar = 100 m; *, p b 0.05).
DPBS-treated group (0.546 0.024). In addition, TNF expression was
approximately 1.5-fold lower in the TUDCA (+) group (0.178 0.005)
than in the TUDCA () group (0.271 0.007). Taken together, we
conclude that TUDCA treatment can signicantly decrease the inammatory response in vitro and in vivo by regulating inammatory factors
such as IL-1 and TNF.
3.4. TUDCA promotes bone regeneration in vivo
The in vivo bone formation efcacy of TUDCA was evaluated using
mice with calvarial defects. Mouse calvarial defects were not treated
(no scaffold group) or were treated with a type I collagen sponge scaffold loaded with DPBS (no drug group), BMP-2 (1 or 3 g), or TUDCA.
Fig. 3. Suppression of inammation in vitro and in vivo by TUDCA. (A) RT-PCR analysis of pro-inammatory genes (IL-1 and TNF) in mBMMSCs treated with various concentrations of
TUDCA for 7 days. (B) IL-1 and TNF expression in in vivo calvarial defect sites treated with or without TUDCA was assessed by immunohistochemical staining with an anti-IL-1 antibody
(green) and an anti-TNF antibody (red). DAPI was used to label nuclei (blue). Differential interference contrast (DIC) images show the morphology of calvarial defect sites.
(C) Quantitative data of IL-1 and TNF expression by immunohistochemical staining. (D) RT-PCR analysis of pro-inammatory genes (IL-1 and TNF) in in vivo calvarial defect sites
treated with or without TUDCA. Expression was quantied by measuring band intensities (scale bar = 100 m; *, p b 0.05).
78
B.-H. Cha et al. / Bone 83 (2016) 7381
In some cases, TUDCA was injected into the implanted scaffold every
other day for a total of 14 days. Micro-computed tomography (microCT) analysis revealed that the TUDCA-treated group (multiple
injections) showed notable de novo bone growth in calvarial defects at
8 weeks after implantation (Fig. 4A). A low level of new bone formation
was observed in the no scaffold and no drug groups. Bone formation in
Fig. 4. In vivo bone formation by TUDCA. Mouse calvarial defects were not treated (no scaffold group) or were treated with a type I collagen sponge scaffold loaded with 25 l of DPBS (no
drug group), 1 or 3 g of BMP-2 (BMP-2 groups), or 25 l of DPBS containing 6.25 g (500 M) of TUDCA (TUDCA single injection group). For the TUDCA multiple injection group, 25 l of
DPBS containing 6.25 g (500 M) of TUDCA was injected into the implanted scaffold every other day for a total of 14 days. The BMP-2 groups served as positive controls. Eight weeks after
implantation, bone formation was evaluated by (A) micro-CT analysis (n = 16 per group) and (B) histomorphometric analysis with Goldner's trichrome staining (n = 16 per group). Scale
bars = 4 mm in (A) and 1 mm in (B). Arrows indicate the margins of bone defect sites. *p b 0.05 versus no scaffold, no drug, and TUDCA (single injection) groups. (C) Immunohistochemical
staining of calvarial defect regions for the osteogenic differentiation marker OC (red) at 8 weeks after implantation. Nuclei were stained with DAPI (blue). Arrows indicate the margins of
bone defect sites (scale bars = 500 m).
B.-H. Cha et al. / Bone 83 (2016) 7381
the TUDCA-treated group (single injection) was approximately equal to
that in the no drug group. By contrast, multiple injections of TUDCA over
2 weeks resulted in extensive bone formation. The bone formation efcacy of multiple injections of TUDCA was comparable to that of BMP-2
(1 or 3 g), which served as a positive control. Histomorphometric analysis with Goldner's trichrome staining was also performed to evaluate
new bone formation. Bone regeneration efciency in the TUDCAtreated group (multiple injections) was almost equal to that in the
BMP-2-treated groups (1 or 3 g) (Fig. 4B). Newly-formed bone tissue
had a well-developed structure with lamellae and osteocytes in lacunae
in the TUDCA-treated (multiple injections) and BMP-2-treated (1 or
3 g) groups. By contrast, a single TUDCA injection was not effective
for bone formation. Immunohistouorescence analysis was performed
to examine expression of the osteogenic differentiation marker
osteocalcin (OC) [38,4142] in the calvarial defect region at 8 weeks
after implantation (Fig. 4C). OC expression was considerably higher in
the TUDCA-treated group (multiple injections) than in the no scaffold,
no drug, and TUDCA-treated (single injection) groups.
4. Discussion
We recently reported that the chemical chaperone TUDCA signicantly decreases adipogenic differentiation of human adipose tissuederived stem cells in vitro and in vivo [27]. Specically, these in vivo
results provide evidence that TUDCA prevents the increase in adipose
tissue formation by decreasing ER stress. In agreement, several
researchers have demonstrated that TUDCA and 4-phenylbutyrate prevent an increase in adipose tissue mass in mice fed a high-fat diet and
promote weight loss [22,25,43]. As mentioned previously, adipose tissue formation in engineered or regenerated bone tissue is a major
issue [911]. Several studies have reported that the decreased bone
volume in osteoporosis is usually accompanied by an increase in bone
marrow adipose tissue, which leads to the weakening and loss of bone
structures [1214]. Our results indicate that TUDCA plays a key role in
enhancing the osteogenic differentiation of mBMMSCs by inhibiting
their adipogenic differentiation (Fig. S1). Therefore, we hypothesize
that decreased lipid accumulation promotes bone tissue regeneration.
In mBMMSCs cultured in osteogenic differentiation media, expression of the osteogenic marker RUNX2 was increased when cells were
treated with 300 nM TUDCA (Fig. 1A). However, expression of RUNX2
was lower in mBMMSCs co-treated with a MEK-1/2 inhibitor (U0126)
and 300 nM TUDCA than in mBMMSCs treated with 300 nM TUDCA
only. These ndings imply that TUDCA is highly associated with MEK1/2 signaling during osteogenic differentiation from mBMMSCs. In addition, we demonstrated that mBMMSCs treated with 300 nM TUDCA
promotes calcium deposits in osteogenic differentiation by stimulating
ITGA5 and ERK1/2-MAPKs (Fig. 1C and D). Previous study reported
that Integrin 5 (ITGA5) was sufcient to enhance ERK1/2-MAPKs
and PI3K signaling and to promote osteoblast differentiation and osteogenic capacity of hMSCs [44]. Interestingly, TUDCA has the unique property to directly interact with a5b1 integrins inside the hepatocyte [45]. A
possible another mechanism underlying the osteogenic effect of TUDCA
is that it suppresses adipogenic differentiation because the osteogenic
and adipogenic differentiation of MSCs are inversely correlated [46].
Taken together with previous reports, it is highly possible that TUDCA
is particular relevance to induce osteogenic differentiation from
mBMMSCs by the expression of ITGA5 and p-ERK.
Apoptosis is a genetically controlled cell suicide program that occurs
naturally to protect the composition of neighboring cells and tissues.
BAX promotes apoptosis by binding to and antagonizing the antiapoptotic protein Bcl-2. Interestingly, Rao et al. reported that TUDCA
prevents an early stage of apoptosis with a concomitant decrease in
ER stress [47]. Recently, other researchers demonstrated that excessive
apoptosis delays skin wound healing [48]. The TUNEL assay and the
ratio of BAX/Bcl-2 expression (Fig. 2) demonstrated that TUDCA
prevented apoptosis at an early stage in calvarial defects. Furthermore,
79
in vitro and in vivo studies revealed that TUDCA treatment signicantly
decreased the mRNA and protein expression of IL-1 and TNF. As a key
pro-inammatory cytokine, IL-1 is generally associated with regulation of the immune and inammatory responses. TNF is a central
regulator of inammation and is an important mediator of the host defense response in various inammatory disorders [4849]. Tavakolidarestani et al. reported that hydroxyapatite loaded with dexamethasone (an anti-inammatory drug) enhances bone regeneration in rat
calvarial defects. Recently, Bury et al. reported that anti-inammatory
peptide amphiphiles are incorporated into self-assembling peptide
nanobers to promote tissue healing in a urinary bladder augmentation
model. Therefore, it is concluded that modulation of apoptosis and inammation is associated with the promotion of repair and regeneration
in defective tissues, even in inammatory disorders.
BMP-2 and BMP-7 are osteoinductive proteins that are clinically
used to regenerate bone in humans [69]. However, Carragee et al.
and Lewandrowski et al. reported that supraphysiological doses of
BMPs incur enormous costs and often have adverse effects such as ectopic bone formation [50], osteolysis [51], and immunogenicity [50].
Therefore, new drugs that do not have these problems and induce effective bone regeneration have been developed and investigated [5254].
Dexamethasone, a small molecule drug, has been extensively used as
an osteopromoter in in vitro cellular studies. Although many studies
have reported the effects of dexamethasone on osteogenic differentiation [55], its clinical use as an osteoinductive drug has limitations
because the efciency with which it induces new bone formation is
low in the absence of concomitant stem cell transplantation [56], and
long-term treatment with this drug can lead to osteoporosis [5758].
The present study demonstrates that the small molecule TUDCA can enhance osteogenic differentiation of BMMSCs in vitro followed by extensive new bone formation at the implanted site. Furthermore, TUDCA has
various advantages: it is more conveniently stored than proteins and
can be mass-produced using high-throughput and quality control procedures. Surprisingly, multiple injections of TUDCA induced much
more bone formation than injection of BMP-2 (Fig. 4). Long-term delivery of TUDCA in vivo is important for effective bone formation because
multiple injections of this drug resulted in signicant bone formation
in comparison with a single injection (Fig. 4). Ursodeoxycholic acid
(UDCA), which has a similar chemical structure to TUDCA, also increased bone formation, although not as effectively as TUDCA (Fig. S2).
Prior to clinical studies of TUDCA for bone regeneration, several additional studies should be performed. The mechanisms underlying the
effects of TUDCA on osteogenic differentiation of MSCs should be elucidated. Delivery systems that allow the sustained release of TUDCA
should be developed for effective bone formation in vivo. The optimal
dosage of TUDCA to maximize bone formation and minimize potential
side effects should be determined using animal studies. Large-animal
studies should be performed to conrm the bone regeneration efcacy
of TUDCA.
5. Conclusions
Multiple injections of TUDCA promoted in vivo bone tissue regeneration much more effectively than injection of BMP-2. TUDCA treatment
signicantly increased osteogenic differentiation of mBMMSCs in vitro
and also decreased levels of apoptosis and inammatory factors at
implantation sites in vivo. Based on our ndings, we conclude that the
chemical chaperone TUDCA is a useful pharmacological substitute for
BMP-2, which is clinically available for bone tissue regeneration.
Supplementary data to this article can be found online at http://dx.
doi.org/10.1016/j.bone.2015.10.011.
Conict of interest
The authors have no conict of interest to disclose.
80
B.-H. Cha et al. / Bone 83 (2016) 7381
Acknowledgments
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare
(HI14C3270) and the National Research Foundation of Korea (NRF)
funded by the Ministry of Science, ICT & Future Planning (NRF2013R1A2A1A09013980), Republic of Korea.
References
[1] R. Langer, J.P. Vacanti, Tissue engineering, Science 260 (1993) 920926.
[2] H. Shin, S. Jo, A.G. Mikos, Biomimetic materials for tissue engineering, Biomaterials
24 (2003) 43534364.
[3] B.H. Cha, J.H. Kim, S.W. Kang, H.J. Do, J.W. Jang, Y.R. Choi, H. Park, B.S. Kim, S.H. Lee,
Cartilage tissue formation from dedifferentiated chondrocytes by codelivery of
BMP-2 and SOX-9 genes encoding bicistronic vector, Cell Transplant. 22 (2013)
15191528.
[4] Z. Cheng, S.H. Teoh, Surface modication of ultra thin poly (epsilon-caprolactone)
lms using acrylic acid and collagen, Biomaterials 25 (2004) 19912001.
[5] S.I. Jeong, J.H. Kwon, J.I. Lim, S.W. Cho, Y. Jung, W.J. Sung, S.H. Kim, Y.H. Kim, Y.M. Lee,
B.S. Kim, C.Y. Choi, S.J. Kim, Mechano-active tissue engineering of vascular smooth
muscle using pulsatile perfusion bioreactors and elastic PLCL scaffolds, Biomaterials
26 (2005) 14051411.
[6] M.W. Betz, A.B. Yeatts, W.J. Richbourg, J.F. Caccamese, D.P. Coletti, E.E. Falco, J.P.
Fisher, Macroporous hydrogels upregulate osteogenic signal expression and promote bone regeneration, Biomacromolecules 11 (2010) 11601168.
[7] S.J. Polak, S.K. Levengood, M.B. Wheeler, A.J. Maki, S.G. Clark, A.J. Johnson, Analysis of
the roles of microporosity and BMP-2 on multiple measures of bone regeneration
and healing in calcium phosphate scaffolds, Acta Biomater. 7 (2011) 17601771.
[8] D.L. Butler, S.A. Goldstein, F. Guilak, Functional tissue engineering: the role of
biomechanics, J. Biomech. Eng. 122 (2000) 570575.
[9] J. Justesen, K. Stenderup, E.N. Ebbesen, L. Mosekilde, T. Steiniche, M. Kassem,
Adipocyte tissue volume in bone marrow is increased with aging and in patients
with osteoporosis, Biogerontology 2 (2001) 165171.
[10] M.E. Nuttall, J.M. Gimble, Controlling the balance between osteoblastogenesis and
adipogenesis and the consequent therapeutic implications, Curr. Opin. Pharmacol.
4 (2004) 290294.
[11] E.J. Moerman, K. Teng, D.A. Lipschitz, B. Lecka-Czernik, Aging activates adipogenic
and suppresses osteogenic programs in mesenchymal marrow stroma/stem cells:
the role of PPAR-gamma2 transcription factor and TGF-beta/BMP signaling
pathways, Aging Cell 3 (2004) 379389.
[12] P. Meunier, J. Aaron, C. Edouard, G. Vignon, Osteoporosis and the replacement of cell
populations of the marrow by adipose tissue. A quantitative study of 84 iliac bone
biopsies, Clin. Orthop. Relat. Res. 80 (1971) 147154.
[13] R. Burkhardt, G. Kettner, W. Bohm, M. Schmidmeier, R. Schlag, B. Frisch, B.
Mallmann, W. Eisenmenger, T. Gilg, Changes in trabecular bone, hematopoiesis
and bone marrow vessels in aplastic anemia, primary osteoporosis, and old age: a
comparative histomorphometric study, Bone 8 (1987) 157164.
[14] S. Verma, J.H. Rajaratnam, J. Denton, J.A. Hoyland, R.J. Byers, Adipocytic proportion of
bone marrow is inversely related to bone formation in osteoporosis, J. Clin. Pathol.
55 (2002) 693698.
[15] J.K. Burkus, J.D. Dorchak, D.L. Sanders, Radiographic assessment of interbody fusion
using recombinant human bone morphogenetic protein type 2, Spine (Phila Pa
1976) 28 (2003) 372377.
[16] S.D. Glassman, J.R. Dimar, L.Y. Carreon, M.J. Campbell, R.M. Puno, J.R. Johnson, Initial
fusion rates with recombinant human bone morphogenetic protein-2/compression
resistant matrix and a hydroxyapatite and tricalcium phosphate/collagen carrier in
posterolateral spinal fusion, Spine (Phila Pa 1976) 30 (2005) 16941698.
[17] F.A. Liporace, E.A. Breitbart, R.S. Yoon, E. Doyle, D.N. Paglia, S. Lin, The effect of locally
delivered recombinant human bone morphogenetic protein-2 with hydroxyapatite/
tri-calcium phosphate on the biomechanical properties of bone in diabetes-related
osteoporosis, J. Orthop. Traumatol. (2014).
[18] S.W. Kang, J.S. Kim, K.S. Park, B.H. Cha, J.H. Shim, J.Y. Kim, D.W. Cho, J.W. Rhie, S.H.
Lee, Surface modication with brin/hyaluronic acid hydrogel on solid-free formbased scaffolds followed by BMP-2 loading to enhance bone regeneration, Bone
48 (2011) 298306.
[19] P. Bosch, D. Musgrave, S. Ghivizzani, C. Latterman, C.S. Day, J. Huard, The efciency of
muscle-derived cell-mediated bone formation, Cell Transplant. 9 (2000) 463470.
[20] C. Ito, W.E. Evans, L. McNinch, E. Coustan-Smith, H. Mahmoud, C.H. Pui, D. Campana,
Comparative cytotoxicity of dexamethasone and prednisolone in childhood acute
lymphoblastic leukemia, J. Clin. Oncol. 14 (1996) 23702376.
[21] M. Kars, L. Yang, M.F. Gregor, B.S. Mohammed, T.A. Pietka, B.N. Finck, B.W. Patterson,
J.D. Horton, B. Mittendorfer, G.S. Hotamisligil, S. Klein, Tauroursodeoxycholic acid
may improve liver and muscle but not adipose tissue insulin sensitivity in obese
men and women, Diabetes 59 (2010) 18991905.
[22] U. Ozcan, E. Yilmaz, L. Ozcan, M. Furuhashi, E. Vaillancourt, R.O. Smith, C.Z. Gorgun,
G.S. Hotamisligil, Chemical chaperones reduce ER stress and restore glucose homeostasis in a mouse model of type 2 diabetes, Science 313 (2006) 11371140.
[23] M.F. Gregor, G.S. Hotamisligil, Thematic review series: adipocyte biology. Adipocyte
stress: the endoplasmic reticulum and metabolic disease, J. Lipid Res. 48 (2007)
19051914.
[24] M.F. Gregor, L. Yang, E. Fabbrini, B.S. Mohammed, J.C. Eagon, G.S. Hotamisligil, S.
Klein, Endoplasmic reticulum stress is reduced in tissues of obese subjects after
weight loss, Diabetes 58 (2009) 693700.
[25] S. Basseri, S. Lhotak, A.M. Sharma, R.C. Austin, The chemical chaperone 4phenylbutyrate inhibits adipogenesis by modulating the unfolded protein response,
J. Lipid Res. 50 (2009) 24862501.
[26] L. Ozcan, A.S. Ergin, A. Lu, J. Chung, S. Sarkar, D. Nie, M.G. Myers Jr., U. Ozcan, Endoplasmic reticulum stress plays a central role in development of leptin resistance, Cell
Metab. 9 (2009) 3551.
[27] B.H. Cha, J.S. Kim, J. Chan Ahn, H.C. Kim, B.S. Kim, D.K. Han, S.G. Park, S.H. Lee, The
role of tauroursodeoxycholic acid on adipogenesis of human adipose-derived stem
cells by modulation of ER stress, Biomaterials 35 (2014) 28512858.
[28] M. Kawai, C.J. Rosen, PPARgamma: a circadian transcription factor in adipogenesis
and osteogenesis, Nat. Rev. Endocrinol. 6 (2010) 629636.
[29] Q. Xie, V.I. Khaoustov, C.C. Chung, J. Sohn, B. Krishnan, D.E. Lewis, B. Yoffe, Effect of
tauroursodeoxycholic acid on endoplasmic reticulum stress-induced caspase-12
activation, Hepatology 36 (2002) 592601.
[30] C.G. Glabe, R. Kayed, Common structure and toxic function of amyloid oligomers
implies a common mechanism of pathogenesis, Neurology 66 (2006) S74S78.
[31] C.M. Rodrigues, X. Ma, C. Linehan-Stieers, G. Fan, B.T. Kren, C.J. Steer,
Ursodeoxycholic acid prevents cytochrome c release in apoptosis by inhibiting
mitochondrial membrane depolarization and channel formation, Cell Death Differ.
6 (1999) 842854.
[32] C.M. Rodrigues, S. Sola, J.C. Sharpe, J.J. Moura, C.J. Steer, Tauroursodeoxycholic acid
prevents Bax-induced membrane perturbation and cytochrome C release in isolated
mitochondria, Biochemistry 42 (2003) 30703080.
[33] S.S. Cao, E.M. Zimmermann, B.M. Chuang, B. Song, A. Nwokoye, J.E. Wilkinson, K.A.
Eaton, R.J. Kaufman, The unfolded protein response and chemical chaperones
reduce protein misfolding and colitis in mice, Gastroenterology 144 (2013)
9891000 e6.
[34] E. Seyhun, A. Malo, C. Schafer, C.A. Moskaluk, R.T. Hoffmann, B. Goke, C.H. Kubisch,
Tauroursodeoxycholic acid reduces endoplasmic reticulum stress, acinar cell damage, and systemic inammation in acute pancreatitis, Am. J. Physiol. Gastrointest.
Liver Physiol. 301 (2011) G773G782.
[35] D.L. Brown, W.W. Kao, D.G. Greenhalgh, Apoptosis down-regulates inammation
under the advancing epithelial wound edge: delayed patterns in diabetes and
improvement with topical growth factors, Surgery 121 (1997) 372380.
[36] C.M. Rodrigues, S. Sola, Z. Nan, R.E. Castro, P.S. Ribeiro, W.C. Low, C.J. Steer,
Tauroursodeoxycholic acid reduces apoptosis and protects against neurological
injury after acute hemorrhagic stroke in rats, Proc. Natl. Acad. Sci. U. S. A. 100
(2003) 60876092.
[37] M. Soleimani, S. Nadri, A protocol for isolation and culture of mesenchymal stem
cells from mouse bone marrow, Nat. Protoc. 4 (2009) 102106.
[38] W.G. La, S.H. Kwon, T.J. Lee, H.S. Yang, J. Park, B.S. Kim, The effect of the delivery carrier on the quality of bone formed via bone morphogenetic protein-2, Artif. Organs
36 (2012) 642647.
[39] W. Huang, B. Carlsen, I. Wulur, G. Rudkin, K. Ishida, B. Wu, D.T. Yamaguchi, T.A.
Miller, BMP-2 exerts differential effects on differentiation of rabbit bone marrow
stromal cells grown in two-dimensional and three-dimensional systems and is required for in vitro bone formation in a PLGA scaffold, Exp. Cell Res. 299 (2004)
325334.
[40] J.H. Lee, C.S. Kim, K.H. Choi, U.W. Jung, J.H. Yun, S.H. Choi, K.S. Cho, The induction
of bone formation in rat calvarial defects and subcutaneous tissues by recombinant human BMP-2, produced in Escherichia coli, Biomaterials 31 (2010)
35123519.
[41] O. Jeon, J.W. Rhie, I.K. Kwon, J.H. Kim, B.S. Kim, S.H. Lee, In vivo bone formation
following transplantation of human adipose-derived stromal cells that are not
differentiated osteogenically, Tissue Eng. Part A 14 (2008) 12851294.
[42] H.S. Yang, W.G. La, S.H. Bhang, H.J. Kim, G.I. Im, H. Lee, J.H. Park, B.S. Kim, Hyaline
cartilage regeneration by combined therapy of microfracture and long-term bone
morphogenetic protein-2 delivery, Tissue Eng. Part A 17 (2011) 18091818.
[43] Y. Hua, M.R. Kandadi, M. Zhu, J. Ren, N. Sreejayan, Tauroursodeoxycholic acid attenuates lipid accumulation in endoplasmic reticulum-stressed macrophages, J.
Cardiovasc. Pharmacol. 55 (2010) 4955.
[44] Z. Hamidouche, O. Fromigue, J. Ringe, T. Haupl, P. Vaudin, J.C. Pages, S. Srouji, E.
Livne, P.J. Marie, Priming integrin alpha5 promotes human mesenchymal stromal
cell osteoblast differentiation and osteogenesis, Proc. Natl. Acad. Sci. U. S. A. 106
(2009) 1858718591.
[45] H. Gohlke, B. Schmitz, A. Sommerfeld, R. Reinehr, D. Haussinger, alpha5 beta1integrins are sensors for tauroursodeoxycholic acid in hepatocytes, Hepatology 57
(2013) 11171129.
[46] M.F. Pittenger, A.M. Mackay, S.C. Beck, R.K. Jaiswal, R. Douglas, J.D. Mosca, M.A.
Moorman, D.W. Simonetti, S. Craig, D.R. Marshak, Multilineage potential of adult
human mesenchymal stem cells, Science 284 (1999) 143147.
[47] R.V. Rao, E. Hermel, S. Castro-Obregon, G. del Rio, L.M. Ellerby, H.M. Ellerby, D.E.
Bredesen, Coupling endoplasmic reticulum stress to the cell death program.
Mechanism of caspase activation, J. Biol. Chem. 276 (2001) 3386933874.
[48] L. Jiang, Y. Dai, F. Cui, Y. Pan, H. Zhang, J. Xiao, F.U. Xiaobing, Expression of cytokines,
growth factors and apoptosis-related signal molecules in chronic pressure ulcer
wounds healing, Spinal Cord 52 (2014) 145151.
[49] E. Esposito, S. Cuzzocrea, TNF-alpha as a therapeutic target in inammatory
diseases, ischemia-reperfusion injury and trauma, Curr. Med. Chem. 16 (2009)
31523167.
[50] E.J. Carragee, E.L. Hurwitz, B.K. Weiner, A critical review of recombinant human
bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns
and lessons learned, Spine J. 11 (2011) 471491.
B.-H. Cha et al. / Bone 83 (2016) 7381
[51] K.U. Lewandrowski, C. Nanson, R. Calderon, Vertebral osteolysis after posterior
interbody lumbar fusion with recombinant human bone morphogenetic protein
2: a report of ve cases, Spine J. 7 (2007) 609614.
[52] X. Wu, S. Ding, Q. Ding, N.S. Gray, P.G. Schultz, A small molecule with osteogenesisinducing activity in multipotent mesenchymal progenitor cells, J. Am. Chem. Soc.
124 (2002) 1452014521.
[53] K.W. Park, H. Waki, W.K. Kim, B.S. Davies, S.G. Young, F. Parhami, P. Tontonoz, The
small molecule phenamil induces osteoblast differentiation and mineralization,
Mol. Cell. Biol. 29 (2009) 39053914.
[54] D.M. Brey, N.A. Motlekar, S.L. Diamond, R.L. Mauck, J.P. Garino, J.A. Burdick, Highthroughput screening of a small molecule library for promoters and inhibitors of
mesenchymal stem cell osteogenic differentiation, Biotechnol. Bioeng. 108 (2011)
163174.
[55] J.P. Kirton, F.L. Wilkinson, A.E. Caneld, M.Y. Alexander, Dexamethasone
downregulates calcication-inhibitor molecules and accelerates osteogenic
81
differentiation of vascular pericytes: implications for vascular calcication, Circ.
Res. 98 (2006) 12641272.
[56] H. Kim, H. Suh, S.A. Jo, H.W. Kim, J.M. Lee, E.H. Kim, Y. Reinwald, S.H. Park, B.H. Min, I.
Jo, In vivo bone formation by human marrow stromal cells in biodegradable scaffolds that release dexamethasone and ascorbate-2-phosphate, Biochem. Biophys.
Res. Commun. 332 (2005) 10531060.
[57] P.D. Sawin, C.A. Dickman, N.R. Crawford, M.S. Melton, W.D. Bichard, V.K. Sonntag,
The effects of dexamethasone on bone fusion in an experimental model of posterolateral lumbar spinal arthrodesis, J. Neurosurg. 94 (2001) 7681.
[58] S. Walsh, G.R. Jordan, C. Jefferiss, K. Stewart, J.N. Beresford, High concentrations of
dexamethasone suppress the proliferation but not the differentiation or further
maturation of human osteoblast precursors in vitro: relevance to glucocorticoidinduced osteoporosis, Rheumatology (Oxford) 40 (2001) 7483.
Anda mungkin juga menyukai
- Dual Luciferase Reporter Assay System Protocol PDFDokumen26 halamanDual Luciferase Reporter Assay System Protocol PDFThanos86Belum ada peringkat
- A Systematic Review of The Efficacy and Pharmacological Profile of Herba Epimedii in Osteoporosis TherapyDokumen10 halamanA Systematic Review of The Efficacy and Pharmacological Profile of Herba Epimedii in Osteoporosis TherapyThanos86Belum ada peringkat
- FASEB J 2013 Shahnazari 3505 13Dokumen10 halamanFASEB J 2013 Shahnazari 3505 13Thanos86Belum ada peringkat
- NCK Influences Preosteoblasticosteoblastic MigrationDokumen6 halamanNCK Influences Preosteoblasticosteoblastic MigrationThanos86Belum ada peringkat
- Activation of STAT3 Is Involved in Malignancy Mediated by CXCL12-CXCR4 Signaling in Human Breast CancerDokumen9 halamanActivation of STAT3 Is Involved in Malignancy Mediated by CXCL12-CXCR4 Signaling in Human Breast CancerThanos86Belum ada peringkat
- Calcium Deposition AssayDokumen1 halamanCalcium Deposition AssayThanos86Belum ada peringkat
- Promotor Region of CXCR4 (1100BP) : I Wish To Have A Promoter Reporter Assay With Detection Via Luciferase MethodDokumen2 halamanPromotor Region of CXCR4 (1100BP) : I Wish To Have A Promoter Reporter Assay With Detection Via Luciferase MethodThanos86Belum ada peringkat
- Biostatistics 101: Data Presentation: YhchanDokumen6 halamanBiostatistics 101: Data Presentation: YhchanThanos86Belum ada peringkat
- Loggerhead Sea Turtle Satoshi KamiyaDokumen13 halamanLoggerhead Sea Turtle Satoshi Kamiyacheeleptaherd100% (2)
- Paper Diamond TemplateDokumen1 halamanPaper Diamond TemplateThanos86Belum ada peringkat
- No - Location Question/Trivia Knowledge/task Answer 1Dokumen3 halamanNo - Location Question/Trivia Knowledge/task Answer 1Thanos86Belum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Penlon Prima 451 MRI Anaesthetic Machine: Anaesthesia SolutionsDokumen4 halamanPenlon Prima 451 MRI Anaesthetic Machine: Anaesthesia SolutionsJuliana Jaramillo LedesBelum ada peringkat
- Statistics: Dr. Ebtisam El - HamalawyDokumen20 halamanStatistics: Dr. Ebtisam El - Hamalawydruzair007Belum ada peringkat
- BICEP GROWTHDokumen3 halamanBICEP GROWTHJee MusaBelum ada peringkat
- My Good Habits - Welcome Booklet 2 - 1Dokumen17 halamanMy Good Habits - Welcome Booklet 2 - 1lisa_ernsbergerBelum ada peringkat
- Health Education Plan-DiarrheaDokumen10 halamanHealth Education Plan-DiarrheaMae Dacer50% (2)
- F&F LetterDokumen3 halamanF&F LetterJaskeerat Singh50% (2)
- Vector and Pest Control in DisastersDokumen10 halamanVector and Pest Control in DisastersTaufik RizkiandiBelum ada peringkat
- Dementia Rating ScaleDokumen2 halamanDementia Rating ScaleIqbal BaryarBelum ada peringkat
- 09022016att ComplaintDokumen25 halaman09022016att Complaintsarah_larimerBelum ada peringkat
- Peace Corps Medical Officer (PCMO) Job AnnouncementDokumen3 halamanPeace Corps Medical Officer (PCMO) Job AnnouncementAccessible Journal Media: Peace Corps DocumentsBelum ada peringkat
- ASHRAE Std 62.1 Ventilation StandardDokumen38 halamanASHRAE Std 62.1 Ventilation Standardcoolth2Belum ada peringkat
- Anti-epileptic drugs: Types, Mechanisms & TreatmentDokumen7 halamanAnti-epileptic drugs: Types, Mechanisms & TreatmentSampada ghodkiBelum ada peringkat
- AFP Hemoptysis - 2022Dokumen9 halamanAFP Hemoptysis - 2022Joshua DiaoBelum ada peringkat
- Safety Signs and SymbolsDokumen5 halamanSafety Signs and Symbolsjon pantz100% (1)
- Hahnemann Advance MethodDokumen2 halamanHahnemann Advance MethodRehan AnisBelum ada peringkat
- Ayurveda Medical Officer 7.10.13Dokumen3 halamanAyurveda Medical Officer 7.10.13Kirankumar MutnaliBelum ada peringkat
- Functional Electrical StimulationDokumen11 halamanFunctional Electrical StimulationMohd Khairul Ikhwan AhmadBelum ada peringkat
- 9 Facebook BmiDokumen29 halaman9 Facebook BmiDin Flores MacawiliBelum ada peringkat
- Appointments Boards and Commissions 09-01-15Dokumen23 halamanAppointments Boards and Commissions 09-01-15L. A. PatersonBelum ada peringkat
- Assessmen Ttool - Student AssessmentDokumen5 halamanAssessmen Ttool - Student AssessmentsachiBelum ada peringkat
- UWI-Mona 2021-2022 Graduate Fee Schedule (July 2021)Dokumen15 halamanUWI-Mona 2021-2022 Graduate Fee Schedule (July 2021)Akinlabi HendricksBelum ada peringkat
- Graphic Health QuestionnaireDokumen5 halamanGraphic Health QuestionnaireVincentBelum ada peringkat
- Work Authorization Permit.Dokumen1 halamanWork Authorization Permit.Gabriel TanBelum ada peringkat
- MediterraneanDokumen39 halamanMediterraneanJeff Lester PiodosBelum ada peringkat
- Testing Antibiotics with Disk Diffusion AssayDokumen3 halamanTesting Antibiotics with Disk Diffusion AssayNguyễn Trung KiênBelum ada peringkat
- Hortatory Exposition Humaira AssahdaDokumen4 halamanHortatory Exposition Humaira Assahdaaleeka auroraBelum ada peringkat
- 116 Draft OilsDokumen233 halaman116 Draft OilsMarcela Paz Gutierrez UrbinaBelum ada peringkat
- School District of Philadelphia's Immigrant & Refugee ToolkitDokumen58 halamanSchool District of Philadelphia's Immigrant & Refugee ToolkitKristina KoppeserBelum ada peringkat
- The Cause of TeenageDokumen18 halamanThe Cause of TeenageApril Flores PobocanBelum ada peringkat
- Improving Healthcare Quality in IndonesiaDokumen34 halamanImproving Healthcare Quality in IndonesiaJuanaBelum ada peringkat