Acquired Coagulation Disorders
Diunggah oleh
aymenDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Acquired Coagulation Disorders
Diunggah oleh
aymenHak Cipta:
Format Tersedia
Inherited vs Acquired Coagulation Disorders
Study online at quizlet.com/_tx3ks
1.
How do women show
signs of hemophilia?
Symptomatic carrier
Spontaneous mutation in a carrier
What are the percent
activity of factor 8 or 9
associated with severity
of hemophilia?
Mild >5%
Moderate 1-5%
Severe <1%
3.
What bleeding disorder is
associated with joint
problems?
Hemophilia
4.
What disease is
associated with a normal
exam except for bruises
and Petechiae and a
normal CBC except for
low platelets?
Immune thrombocytopenia purpura
5.
What disease is
associated with
consumption of factors
including factors VII, IX,
and VIII?
DIC
6.
What do patients with
Glanzmann
thrombasthenia respond
to, platelet agonist or
ristocetin?
Lack of response to platelet
agonist, response to ristocetin
7.
What factor deficiency is
associated with
amyloidosis in adult
patients?
Factor X deficiency due to
absorption of Factor X
8.
What factor deficiency
may be combined with
Factor 8 deficiency due
to an abnormal
chaperone protein from
ER to Golgi apparatus?
Factor V deficiency
9.
What inheritance type is
associated with
hemophilia?
X linked
10.
What is Glanzmann
thrombasthenia
associated with?
Platelet Deficiency in IIb3
integrin - fibrinogen receptor that
leads to no fibrinogen bridging of
platelets to other platelets can
occur, and the bleeding time is
significantly prolonged
11.
What is necessary for
gamma-carboxylation of
factors II,VII, IX, and X?
Vit K
12.
What is the stabilizer for
Factor 8?
VWF. Deficiency in VWF leads to
deficiency in Factor 8
13.
What is the standard
therapy for Immune
thrombocytopenia
purpura?
Steroids
2.
14.
What percent of hemophilia occurs from
spontaneous mutations?
~20%
15.
What type of VWD has an absence of high
multimer weight of VWD protein?
Type 2
16.
What VWD type is associated with any degree of
reduced levels of VWF (most common and
usually the mildest form)?
Type 1
17.
What VWD type is associated with virtual
absence of VWF (the most severe form, only
occurring in 1 to 3 persons per million)?
Type 3
18.
Which factor deficiency is NOT associated with
bleeding?
Factor XII
19.
Which factor has the shortest half life?
Factor VII
20.
Which syndrome is opposite of Glanzmann
thrombasthenia and can't bind ristocetin?
Bernard
Soulier
Syndrome
Acquired Coagulation Disorders
Study online at quizlet.com/_ogc5l
1.
Acquired
inhibition of XIII
following isoniazid drug therapy for
tuberculosis
2.
Antophosphoipid
Antibody
Syndromes
(APLS)
acquired coag defect associated w
thrombosis
aPL - antophopholipid Ab
aCL - anticardiolipin Ab (false pos w VDRL
test)
LAC - LA
CAPS - catastrophic antiphospholipid
syndrome
3.
Autoimmune
Inhibitors of F
VIII
Acquired VIII:R (vWD)
may be seen with autoimmune disease or
lymphoproliferative disorder
4.
Circulating
Anticoag: Types
Specific inhibitors - specific for particular
factors
Nonspecific - interfere w phospholipid
components of reagents
5.
Circulation
Anticoagulants
develop with underlying disorders or spont
composed of imunoglobulins
allo or auto antibodies
6.
Factor X
deficiencies
occurs rarely in people with amyloidosis
7.
FIX Inhibitors
rare, due to transfusion, classified as
alloAb
VIII:C and IX, Ab do not increase bleeding
frequency, rather hemarthosis, muscle, and
soft tissue hemorrhages are symtpoms
Suspected in hemophiliac if transfused
factor replacement products appear to have
reduced effectiveness, hemostasis is hard
to achieve, or both
8.
FIX Lab Test
11.
FVIII:C
inhibitors
Autoantibodies
most often seen in patients w lupus, RA,
drug reactions, mm, ex
aka aquire hemophilia
Symptoms: lg hematomas, gross hematuria,
bleeding around pharyngeal or peritoneal
cavities, cerebral hemorrhages,
hemarthrosis
Should be suspected in anyone w no prior
history who present w massive bruising or
hematoma
mortality rate 20%
12.
Heparin binds
autoprothrombin
III
greatly enhances ability to bind and
inactivate thrombin
13.
Heparin therapy
fost, potent anticoag
commonly used to treat thrombosis
APTT used to monitor heparin therapy
TT also prolonged bc affected by heparin
and FDPs
Occasionally PT is prolonged if patient has
recived heparin for a long period
PT, APTT, TT greatly prolonged
*confirmed by protamin sulfate (binds to
heparin and removes it)
14.
Inhibitors VIII:C
most result from factor concentrate
transfusions
autoantibodies
IgG antibodies
Do not interfere with function of vWF or BT
Inhibitors in hemophiliacs when VIII has
short half life
15.
LAC Lab Test
PT and TT N
APTT prolonged
mixing study no corection w normal plasma
Extended incubation extends APTT
proportionally to incubation time
Factor Assay N
16.
LAC - Lupus-like
anticoagulant
aka Antiphospholipid Antibody Syndrome
autoantibodies react against phospholipid
portion of APTT reagent
Develops in 31% of patients w SLE, taking
hemothiazine, lymphoproliferative disorders
more frequently associated w venous
thrombosis than arterial
17.
Nonspecific
inhibitors
usually accidentally discovered w prolonged
APTT screening test
Mixing studies = no correction w normal
pool plasma
IgG or IgM interfere w phopholipid
dependent tests
PT N
APTT prolonged
** Mixing study no correction w normal pool
plasma
** Time and Temp Dependency
2Hr incubation at 37 shows prolongation
9.
FIX Treatment
First stabilize hemostasis
Goal - rid body of Ab
low titer inhibitor
- give high conc of VIII:C to overwhelm Ab
and all of binding sites = Bethesda titer
- porcine recombinant FVIII:C concentrates
High titer
- steroids, porcine concentrates,
immunosuppressive, cytotoxic agents,
plasmapheresis
10.
FVIII:C
inhibitors
Alloantibodies
IgG to FVIII/vEF complex
Does not interfere w function of vWF so BT
is normal
frequently encountered
due to transfusion
in vitro - prolongation of tests
in vivo - hypercoagulable state
18.
Specific Inhibitors
Antibody specific to factor
ABs directly inhibit factor activity or cause inc clearance
Secondary to replacement therapy/transfusion or arise spont wo disorder
19.
Time and Temp Dependency
Initial test: plt + normal pooled plasma
Normal person = correction
Inhibitor = prolonged / no correction
Incubation control: 37 degrees 2 hours
#1 patient
#2 normal pooled plasma
no prolongation indicates inhibitors effect on FVIII:C provided in normal pool plasma
20.
VIII:C Treatment
VIII concentrates (have to give enough to overcome inhibitor
steroids
imunosuppressive therapy
cytotoxic agents
prothrombin-complex concntrates
plasmapheresis in severe cases
21.
Vit K causes
poor diet
biliary obstruction, not absorbing
intestinal malabsorption diseases
gut sterilization
hemorrhagic disease of the newborn
coumadin therapy
22.
Vit K deficiency
Results in impaired synthesis of II, VII, IX, X. Protein C and S
23.
Vit K Lab Test
PT prolonged
APTT possibly prolonged
TT N
Fibrinogen N
Acquired Coagulation Disorders
Study online at quizlet.com/_259q9n
1.
Acute ITP
-children
-self limited
-after immunization or virus
2.
ADAMS TS13
-degrades vWF (breaks up the multimer)
-if deficient: vWF piles up, causes abnormal
platelet adhesion
3.
Alpha 2
Antiplasmin
-shuts down plasmin (inactivates)
4.
Aspirin
(primary, qualitative)
-inactivates cyclooxygenase, lack of TXA2
-impairs platelet aggregation
5.
Bernard Soulier
Syndrome
13.
Disseminated
Intravascular
Coagulation
(DIC)
-depletion of platelets and coag factors >bleeding
-deposition of fibrin -> microvessel
thombosis
14.
Examples of
Fibrinolysis
Disorders
-radical prostatectomy: urokinase
released, activates plasmin
-cirrhosis of liver: reduced alpha 2
antiplasmin
15.
Fibrinolysis
Disorders
-overactive plasmin -> too much
fibrinogen cleavage
-last stage of coagulation, to remove
thrombus
-because they are due to pathology,
theres no thrombus to remove, s plasmin
acts ands destroys coag factors
16.
Glanzmann
thrombasthenia
(primary, qualitative)
-genetic def in gp1b
-mild thrombocytopenia
-LARGE platelets (Big Suckers)
6.
7.
8.
Chronic ITP
Coagulation
Factor Inhibitor
Conditions
Associated
w/DIC
-women
-primary or secondary
-can pass IgG to offspring
(primary, qualitative)
-genetic gp2b/3a def
-platelet aggregation imparied
(secondary hemostatic disorder)
-AQUIRED Ab against coag factor ->
impaired function
-F8 most common
-same symptoms and labs as hemophilia A
17.
Hemophilia A
-sepsis
-trauma: head injury, tissue injury, fat emboli
-obstetrical complications: amniotic fluid
embolus, abruption, retained dead fetus
-Cancer: Trousseau syndrome
-Immune disorders
-toxins
-vascular disorders
(secondary hemostatic disorder)
-xlinked recessive
-factor 8 def
-elevated PTT, low PT
-low factor 8
-normal platelet count
18.
Hemophilia B
(secondary hemostatic disorder)
-factor 9 def
-same symptoms
19.
Heparin Induced
Thrombocytopenia
-heparin therapy destroys platelets
-fragments can activate other platelets,
leading to thrombosis
20.
HIT Mechanism
-heparin forms complex w/PLatelet Factor
4 (on platelets)
-complex causes development of IgG
autoantibodies
21.
How does ITP
happen
-IgG made in spleen
-bind platelets
-pbound platelets eaten by SPLEEN
macrophages
9.
DIC
-pathologic activation of coag cascade
-microthrombi form
10.
DIC Labs
-low platelet
-high PT and PTT: consuming coag factors
-low fibrinogen: linker molecule used up
-microangiopathic hemolytic anemia
-elevated fibrin split products
11.
DIC
Pathophysio
-increased activation of clotting cascafe
-decreased anticoagulants
-impaired fibrinolysis
12.
DIC Treatment
-fix secondary cause
-blood product transfusion
22.
How to differentiate
Coagulation Factor
Inhibitor and
Hemophilia A
-MIXING STUDY
-Coag F Inhibitor does NOT correct
-Hemophilia A does correct
36.
Tests for 2o Disorders
-PT (extrinsic pathway and
common)
-PTT (intrinsic pathway and
common)
23.
HUS
(primary, quantitative)
-hemolytic uremic syndrome
-e.Coli 0517H7 verotoxin damages
endothelial cells, cause
microthrombi formation
-CHILDREN
37.
tPA
plasminogen to plasmin
38.
Treating Fibrinolysis
Disorders
-Aminocaproic Acid: blocks
activation of plasminogen
39.
Treating Hemophilia A
-give Factor 8
40.
Treating TTP and HUS
PLasmaphersis, corticosteroids
41.
Treating vWF Disease
-desmopressin
-increases vWF release from
Weibel-Palade bodies
42.
Treat ITP
-corticosteroids
-IVIG
-Splenectomy: kills source of IgG
and site of destruction
43.
TTP
(primary, quantitative)
-genetic defect OR autoantibody
formed against ADAMSTS13
-caused by low ADAMS TS13
44.
TTP and HUS Symptoms
-skin, mucosal bleeding
-microangiopathic hemolytic
anemia
-fever
-renal insufficiency
-CNS abnormalitues
45.
Types of Platelet
disorders in 1
hemostasis
Quantitative or qualitative
46.
Uremia
(primary, qualitative)
-poor kidney function, build up of
nitrogenous waste products
-disorder of adhesion and
aggregation
47.
Vitamin K Deficiency
(secondary hemostatic disorder)
-2, 7, 9 10 disrupted
-coagulation not happening
48.
Von Willebrand Disease
(secondary hemostatic disorder)
-vWF def (genetic)
-most common, inherited
49.
Von Willebrand Disease
Labs
-long bleeding time
-high PTT, normal PT
-abnormal Ristocetin test
50.
Von Willebrand Disease
Symptoms
-mucosal and skin bleeding (b/c
platelets cant adhere)
51.
Von Willebrand Disease
Types
quantitative or qualitative
-most common: AD
-platelet adhesion cant occur
52.
What activates VItamin
K
-epoxide reductase
-coumidin blocks^^
24.
ITP Cause
(primary, quantitative)
-IgG attackes platelet antigens (like
gps) -> thrombocytopenia
-common in children and adult
25.
Lab Findings ITP
-low platelet
-normal PT/PTT
-high megakaryocytes
26.
Lab Findings TTP and
HUS
-thrombocytopenia, increased
bleeding time!!
-normal PT/PTT
-anemia + SCHISTOCYTES
-increased megakaryocytes
27.
Large Volume
Transfusions
(secondary hemostatic disorder)
-dilutes coag factors
-results in general deficiency
28.
Mixing Study
-combine normal plasma with
patients plasma
-if CORRECTED: normal plasma
gives back whats deficient, will
reduce PTT (back to normal)
-if NOT CORRECTED: anti-factor Ab
from patient will bind factor in
normal plasma, keeping PTT high
29.
Plasmin
-cleaves fibrin
-cleaves fibrinogen in serum
-destroys coag factors
-blocks platelet aggragtion
30.
PT
-coumidin/warfarin better measured
here
31.
PTT
-measure HEParin effect
32.
Ristocetin test
-give ristocetin to patient platelets,
they will agrregate
-abnormal vWF, no aggregation
33.
34.
35.
Secondary Hemostasis
Disorders
-abnormality in factors
-deep bleeding in muscles or joints
-rebleeding after procedure
Serious Complications
of DIC
microthrombi -> ischemia and
infarcts
bleeding from IV sites and
mucosally because using so much
platelets
Symptoms of 1o
Hemostasis Disorder
-mucosal bleeding
-skin bleeding: easy bruises,
petechiae, ecchymosis (petecheia
is from thrombocytopenia)
53.
What are primary hemostatic disorders characterized by?
Mucosal and Skin Bleeding
-hemoptysis
-**epistaxis**
-menorrhagia
-intracranial bleeding
54.
What causes Vitamin K DEf
-either you have trouble uptaking it, or you lack bacteria that makes it
-newborns, antibiotic therapy, malabsorption, or LIVER FAILURE
-check for liver failure with elevated PT
55.
Whats required to activate factors?
-exposure to activating substance
-phospholipid surface
-Ca+
56.
Where are factors of coag cascade made?
Liver
57.
Why are the factors disrupted in Vitamin K def?
-it gamma carboxylates 2,7, 9 and 10
-promotes coagulation
58.
Why is PTT elevated in VW DIease?
-nee vWF to stabilize factor 8
22- Congenital and Acquired Coagulation Disorders
Study online at quizlet.com/_1zw70f
1.
Acquired deficiency in clotting factors due
to decreased synthesis:
...
2.
Acquired inhibition of coagulation is
sometimes called "____"
acquired
hemophilia
3.
Acquired inhibitors of coagulation are
____ to coagulation factors, usually factor
8
antibodies
4.
Activated factors 2, 7, 9, and 10 are also
called ____
FEIBA
5.
Activation of coagulation system=
secondary
hemostasis
6.
After screening, go to definitive studies
including (2):
Individual factor
levels
Von Willebrand
panel
7.
Ancillary studies can be done to define
more (after general and specific tests) (3):
D-dimers
Thrombin time
Inhibitor titers
8.
aPTT in hemophilia is usually ____
prolonged
9.
____ are the type of RBCs seen in
peripheral blood smear of DIC pt
Schistocytes
10.
Arterial nevi, splenomegaly, palmar
erythema are stigmata of ____
liver disease
11.
Aside from hemarthrosis, 3 S&S of
hemophilia:
Muscle
hemorrhage
Deep soft tissue
hematomas
CNS bleedingwith trauma
Note: secondary hemostasis defects
12.
____ bleeding pattern includes deep
hematomas, muscle bleeding, bleeding
with surgey/trauma
Secondary
hemostatic
13.
Bruising and mucosal bleeding such as
epistaxis and gum bleeding is ____ in
hemophilia
uncommon!!
14.
____ can also be due to excessive
destruction of coagulation factors
Acquired clotting
defects
15.
Carrier testing and ____ diagnosis are
available for hemophilia using RFLP
prenatal
16.
Cirrhosis of liver => splenomegaly =>
combined primary and secondary ____
defects
hemostatic
17.
Cirrhosis of the liver can have what effect
on the spleen and why?
Splenomegaly;
sequestration of
platelets
18.
Clinical circumstance predisposing to DIC
are seen in ____
acute bleeding
19.
Clinical
manifestations of
____:
Easy bruising
Bleeding form
mucous
membranes
(gum bleeding
nosebleeds
(epistaxis)
Menorrhagia)
Bleeding after
surgery or trauma
von Willebrand Disease (VWD)
20.
Coagulation
defects due to
liver disease are
only treated if:
bleeding OR procedure is planned
21.
Coagulation
defects in liver
disease
...
22.
____ contains ALL
factors (a type of
treatment)
FFP (fresh frozen plasma)
23.
Cryoprecipitate
includes:
Fibrinogen
Factor VIII
vWF
Factor XIII
24.
DDAVP MOA:
releases stored vWF from endothelial
cells and platelets
25.
Deep muscle
bleeds can lead to
____ => Volkman's
ischemic
contracture (nerve
damage if
compartment
syndrome is not
corrected)
compartment syndrome
26.
Defective
synthetic function
in liver causes
____
coagulopathy
27.
28.
29.
30.
Degrees of
severity of
hemophilia:
1) Severe: <____%
factor level
2) Moderate ________% factor level
3) Mild ________% factor level
1; 1-5; 5-30
Desmopressin
acetate (DDAVP) is
NOT effective in
____
hemophilia B
DIC especially
uses up which
clotting factor?
Fibrinogen (1)
DIC has what
impact on clotting
factors and
platelets?
Uses up clotting factors and platelets
(Global consumption of coagulation
factors, esp. fibrinogen)
36.
Factors contributing to liver disease
could be indicative of ____
acquired
bleeding/hemophilia
37.
Factor VIII and Factor IX in hemophilia
is ____
ONE or the other is
reduced!
38.
Family history is important to
determine the ____
inheritance pattern
39.
FEIBA= ____
factor eight
inhibitor bypass
activity
40.
FEIBA is used to treat ____
acquired inhibitors
of coagulation
41.
For mild hemophilia A, always consider
administering ____ inhaled or IV
Desmopressin
(DDAVP)
42.
For prevention of fibrinolysis and
mucous membrane bleeding only,
treatment include ____ and ____
Epsilon-amino
caproic acid;
Tranexamic acid
43.
For surgery/severe loss in VWD,
replacement of vWF with ____ is a
possible treatment
Plasma-derived
products Humate-P
Alphanate
Wilate
44.
General measures for treating VWD
include ____ and topical agents
OCPs (oral
contraceptive pills)
45.
General screening tests used in
diagnosing VWD are ____ and ____
PFA-100; PTT
46.
Hemophilia A and B are identical in
____ and are both defects in the ____
pathway
clinical
presentation;
intrinsic
47.
Hemophilia A- MOST common, is a
defect in ____
Factor VIII
48.
Hemophilia B AKA
Christmas disease
49.
Hemophilia B is a defect in ____
Factor IX
50.
Hemophilia genes have a high rate of
____, leading to 1/3 new cases with a
negative family history
spontaneous
mutation
51.
Hemophilia is a ____ inheritance
disease, but about 30% cases are new
mutations
X-linked recessive
52.
Hemophilia is almost exclusively found
in (males/females)
males
53.
Hospitalized patients with poor oral
intake, often develop ____ deficiency,
especially if on antibiotics! This
impacts production of clotting factors
vitamin K
54.
However, an advantage to using on
demand factor is ____ factor is used
less
DIC leads to
excessive ____
production which
causes fibrin clots
to be deposited in
vessels and block
vital circulation
thrombin
The ____ DIC
usually only
requires treatment
of underlying
condition- retained
dead fetus,
adenocarcinoma
rare chronic
Disadvantage to
using "on demand"
factor treatment is
it is unpredictable
and more likely to
cause ____ over
time
joint damage
34.
Dissolution of the
clot- fibrinolysis=
Tertiary hemostasis
55.
35.
Extensive tissue
damages include:
Get familiar with
acute hemolytic transfusion reaction
tumor lysis syndrome
fat embolism
heat stroke
How to treat DIC?
1) Urgently address ____
2) Replacement of ____
3) Platelet transfusion for bleeding
Underlying cause;
Depleted
coagulation
factors, especially
fibrinogen
56.
Iatrogenic=
caused by doctor
31.
32.
33.
57.
58.
Iatrogenic
complications in
hemophilia can
occur in
circumcision, i.m.
injection, i.j.
stick. Image:
If a forearm
compartment
syndrome is not
corrected, it can
lead to ____
65.
In DIC, fibrin stands can sheer apart ____
causing microangiopathic hemolytic
anemia
RBCs
66.
In DIC patient's peripheral blood smear,
you may also see an absence of ____
because they have been used up
platelets
67.
In DIC:
PT/PTT is ____
Fibrinogen is ____
D-dimers is ____
Thrombin time is ____
Increased
Decreased
Increased
Increased
68.
____ in hemophilia is standard of care
Prophylactic
factor
69.
In neonates, routinely give IM injection of
____ at delivery to prevent acquired
clotting defciency
vitamin K
70.
In progressive hemophilic arthropathy,
usually ____ joints are affected
larger (knees,
hips, elbows,
shoulders,
ankles..)
71.
In Type 2A VWD, there is an absence of
____
large and
intermediate
multimers
72.
In Type 2B VWD, there is an absence of
____
large multimers
73.
In Type 2M, you see a ____ multimer
pattern
NORMAL
74.
In Type 2N VWD, there are ____ multimer
NORMAL
75.
In ____ VWD, there is a decreased affinity
for factor VIII
Type 2N
76.
In ____ VWD, there is an increased
affinity for GpIb (gain of function
mutation)
Type 2B
77.
In ____ VWD, there is decreased plateletdependent function
Type 2M
78.
____ is a medical emergency where
coagulation initiated within the vascular
system
Disemminated
intravascular
coagulation (DIC)
Volkman's ischemic contracture
If it a less
common type of
VWD and the first
three tests do not
clarify diagnosis,
can move on to the
other two tests:
____ and ____
RIPA; VWF multimers + pattern
Important to
consider history of
factors
predisposing to
liver disease such
as ____, ____, and
iron overload
alcohol; chronic hepatitis
61.
In 2014, now have
modified factors
with longer ____
half-life
62.
In acute situation,
the pattern and
clinical scenario
of DIC should be
questioned
...
63.
In addition to
giving factors, you
want to also treat
acquired inhibitors
of coagulation by
____
immunosuppression (reduces Ab
production)
64.
In diagnosing
VWD, only ____,
____, and ____
tests are needed if
the pattern is
autosomal
dominant AND
there is a
proportional
reduction in all
three levels
VWF antigen
VWF activity
Factor VIII level
59.
60.
79.
____ is most
important aspect
of understanding
the patient's
bleeding problem
89.
Mild hemophilia pts have bleeding ____ or
____ only
post-trauma;
surgery
90.
Moderate hemophilia pts have spontaneous
bleeding, or bleeding post-____
spontaneous;
trauma
91.
More commonly factor ____ will be
reduced in hemophilia
92.
Most common type of VWD?
Type I
93.
Most uncommon clotting factor deficiencies
have a ____ inheritance pattern and are
RARE
autosomal
recessive
94.
Most uncommon coagulation factor
deficiencies present with ____ bleeding
pattern
Secondary
hemostatic
defect
95.
Obstetric "catastrophes" include ____ and
____
placental
abruption
placenta
previa
96.
Obstetric catastrophes, trauma, crush
injuries, closed head injuries,
malignancies, and extensive tissue damage
can all cause ____
DIC
97.
One key clinical sign of hemophilia is ____
hemarthrosisjoint bleeding
98.
Other part of the FFP is the ____
cryoprecipitate
99.
Pattern of muscle/deep bleeding suggests
defect in ____ hemostasis- coagulopathy
secondary
100.
Pattern of skin and mucosal bleeding seen
in defect of ____ hemostasis
primary
101.
Patterns seen in defects of primary
hemostasis suggest ____ disease,
thrombocytopenia, and platelet functional
defect
von Willebrand
102.
PFA-100 in hemophilia is ____
normal
103.
PFA-100 replaces ____ (outdated test)
bleeding time
104.
Plasma-derived factors for hemophilia are
purified with ____
monoclonal
antibodies
105.
Plasma-derived products used to treat VWD
include ____, ____, and ____
Humate-P;
Alphanate;
Wilate
106.
Platelet adhesion and aggregation=
primary
hemostasis
107.
Platelet count in hemophilia is ____
normal
108.
Primary or secondary prophylaxis
administeration requires good ____
veins
109.
PT in hemophilia is usually ____
normal
110.
(PT/PTT) will be more marked than
(PT/PTT), since the half-life of factor VII is
shorter
PT; PTT
111.
The PTT in acquired inhibitors of
coagulation is ____
very high
History
____ is the
degradation of
cartilage joint in
hemophilia
patients; it
becomes
destroyed and not
functional
Progressive hemophilic arthropathy
81.
____ is used to
treat VWD Type I
Desmopressin
82.
It takes ____
factor use to treat
hemophilia
prophylactically,
but it does make
for a better
lifestyle
high
Liver synthesizes
all coagulation
factors except
____
factor 8
84.
Low albumin is a
sign of altered
____ function
liver
85.
The lower/later
position of factor
that is deficient is
usually more
____, for example
fibrinogen
severe
86.
MAIN cause of
DIC:
sepsis
87.
Main treatment
goal in acquired
inhibitors of
coagulation is to:
bypass the coagulation factor to which
antibody is directed to (usually factor
VIII)
Medication
history, such as
____, and food
intake, especially
vitamin ____, are
important for
studying bleeding
patients
warfarin (anticoagulant); vitamin K
80.
83.
88.
112.
Recombinant
factor ____
initiates
coagulation via
the extrinsic
pathway and is
used to treat
acquired
inhibitors of
coagulation
VIIa
113.
Recombinant
factors are
available for
hemophilia but
are more ____
expensive
114.
Recombinant
factors available
for what 3
factors?
VIIa
VIII
IX
115.
RIPA=
Ristocetin-induced platelet aggregation
116.
Screening studies
for bleeding
patients (3):
PT, PTT, CBC
Severe
hemophilia pts
have ____
bleeding
spontaneous
Since vitamin K
deficiency affects
all pathways of
coagulation
cascade, both PT
and PTT will be
____
Elevated
Some patients
prefer "on
demand" factor
treatment, where
they wait for ____
to occur before
giving
themselves factor
bleeding
117.
118.
119.
120.
Spontaneous head
bump with severe
hemophilia
(image)
*now totally blood-free
121.
Spontaneous
hemarthrosis
with severe
hemophilia
(image)
122.
Subendothelial
vWF interacts
with the ____
platelet receptor
GpIb
123.
Supernatant of
FFP is used to
make ____
PCC (prothrombin complex concentrate)
124.
Supernatant of
thawed FFP
contains four
factors:
Factor 2, 7, 9, 10 (vit-K dependent)
125.
Tests specific to
VWD (all
available, not all
necessarily
used):
VWF activity
VWF antigen
Factor VIII level
RIPA
VWF multimers and pattern
Get familiar with
list
126.
Three tools for
evaluating patient
you suspect
having a
coagulation
disorder:
1) Medical history
2) Physical exam
3) Lab studies
127.
To replace coag.
factors, esp.
fibrinogen, in DIC
patients,
treatment is
usually admin of
____
cryoprecipitate
128.
Treatment for
hemophilia:
____ factors or
recombinant
factors
plasma-derived
129.
Treatment of
VWD- only on
demand
Desmopressin (DDAVP)
Contraindication: Type 2B!!
130.
Type III is an ____ of vWF
absence
131.
Type III is ____ inheritance pattern
autosomal recessive
very uncommon, very
severe
132.
Type II is ____ inheritance pattern
autosomal dominant
133.
Type II VWD is a ____ deficiency of
vWF
qualitative
134.
Type I VWD is a ____ deficiency of
vWF
quantitative
135.
Type I VWD is an ____ inheritance
pattern
autosomal dominant
136.
Uncommon coagulation factor
deficiencies do not show ____ in
the common clinical
symptoms/signs
joint bleeding
137.
Uncommon S&S of hemophilia:
epistaxis, other ____ bleeding,
prolonged bleeding from cuts,
petechiae
mucosal
138.
Usually factor 8 circulates (halflife) for ____
8-12 hours
*now have better ones
139.
Usually half-life of factor 9 is ____
24 hours
140.
Usually (PT/PTT) >> (PT/PTT) with
coagulation defects in liver disease
PT; PTT
141.
Variable clinical presention
depends on ____ factor level, and
relates to position of ____
baseline; factor in the
pathway
142.
Vitamin K deficiency can occur in a
patient on vitamin K antagonists
such as ____
warfarin
143.
Vitamin K deficiency treated with
vitamin K administration responds
____
rapidly
144.
Vitamin K important for ____ of
factor 2, 7, 9, 10
gamma-carboxylation
145.
Volkman's ischemic contracture is
____ damage when compartment
syndrome not corrected
nerve
146.
Von Willebrand Disease is a ____
coagulation factor deficiency
congenital
147.
____ VWD is impaired secretion or
increased proteolysis
Type 2A
148.
vWF in hemophilia is ____
normal
149.
VWF is very important for two
functions:
1) Carrier for factor
VIII (prevents it from
proteolysis= longer
half-life)
2) Cross-links platelets
to exposed collagen
AND to each other
150.
VWF made in ____
megakaryocytes
151.
Why is rare chronic DIC only
treated with addressing underlying
condition?
Coagulopathy and
thrombocytopenia are
usually mild
Anda mungkin juga menyukai
- Acquired Factor VIII Inhibitors: Pathophysiology and TreatmentDokumen6 halamanAcquired Factor VIII Inhibitors: Pathophysiology and TreatmentSakinah Mar'ie SanadBelum ada peringkat
- Bleeding DisordersDokumen34 halamanBleeding Disordersbpt2Belum ada peringkat
- ThrombocytopeniaDokumen3 halamanThrombocytopeniaSara Abdi OsmanBelum ada peringkat
- PRESENTED:-Dr. Raju NiraulaDokumen29 halamanPRESENTED:-Dr. Raju NiraulaRaju NiraulaBelum ada peringkat
- Hema 2 5th Ed SummaryDokumen9 halamanHema 2 5th Ed Summarymonzon.mika1801Belum ada peringkat
- Understanding Antiphospholipid SyndromeDokumen37 halamanUnderstanding Antiphospholipid SyndromeAhmad Reshad AslamBelum ada peringkat
- BDCB Abnormal Plt Function_230628_205650 (1)Dokumen22 halamanBDCB Abnormal Plt Function_230628_205650 (1)ps.pcpc221Belum ada peringkat
- Antiphospholipid syndrome: Blood clots and pregnancy complicationsDokumen6 halamanAntiphospholipid syndrome: Blood clots and pregnancy complicationshikmat sheraniBelum ada peringkat
- Location Gold Standard Current Practice: Thrombophilia Teaching Points10/19/2005 (JGP)Dokumen2 halamanLocation Gold Standard Current Practice: Thrombophilia Teaching Points10/19/2005 (JGP)aymenBelum ada peringkat
- Disorders Leading To ThrombosisDokumen9 halamanDisorders Leading To ThrombosisGilo IlaganBelum ada peringkat
- Bleeding and Coagulation Disorders: DR Nidhi Chaurasia JR-1 MDS PedodonticsDokumen66 halamanBleeding and Coagulation Disorders: DR Nidhi Chaurasia JR-1 MDS PedodonticsDrNidhi KrishnaBelum ada peringkat
- Coag Unit 6 Notes Coagdisorders Secondary F08Dokumen25 halamanCoag Unit 6 Notes Coagdisorders Secondary F08Nadir A IbrahimBelum ada peringkat
- Antiphospholipid SyndromeDokumen38 halamanAntiphospholipid SyndromeossamafoudaBelum ada peringkat
- Pathology Bleeding DisordersDokumen67 halamanPathology Bleeding DisordersMarcelliaBelum ada peringkat
- Disseminated Intravascular Coagulation: Keith Lewis, MDDokumen37 halamanDisseminated Intravascular Coagulation: Keith Lewis, MDTimea DaniBelum ada peringkat
- Pediatrician's Guide to Evaluating Bleeding DisordersDokumen26 halamanPediatrician's Guide to Evaluating Bleeding DisordersSachidanand ShahBelum ada peringkat
- HEMA - Coagulation Disorders (Dr. Tuy)Dokumen35 halamanHEMA - Coagulation Disorders (Dr. Tuy)Shams JailaniBelum ada peringkat
- Treatment of Hemostasis DisordersDokumen17 halamanTreatment of Hemostasis DisordersDiana HyltonBelum ada peringkat
- Disorders Leading To ThrombosisDokumen27 halamanDisorders Leading To ThrombosisFearless AngelBelum ada peringkat
- Drugs Causing Throm Drugs Causing Thrombocytopenia or Low Platelet CountDokumen4 halamanDrugs Causing Throm Drugs Causing Thrombocytopenia or Low Platelet CountDejan OgnjanovicBelum ada peringkat
- MRCPass Notes For MRCP 1 - HEMATOLOGYDokumen9 halamanMRCPass Notes For MRCP 1 - HEMATOLOGYsabdali100% (1)
- Platelet Storage Pool Disorders PDFDokumen4 halamanPlatelet Storage Pool Disorders PDFMano CempakaBelum ada peringkat
- Case Report: Glanzmann's Thrombasthenia: Report of A Case and Review of The LiteratureDokumen5 halamanCase Report: Glanzmann's Thrombasthenia: Report of A Case and Review of The LiteratureNaifmxBelum ada peringkat
- Dic - MNJDokumen36 halamanDic - MNJmaibejoseBelum ada peringkat
- Antiphospholipid SyndromeDokumen33 halamanAntiphospholipid Syndromeadmin reumatologiBelum ada peringkat
- Platelet Disorders: Autoimmune ThrombocytopeniasDokumen6 halamanPlatelet Disorders: Autoimmune ThrombocytopeniasShī Fu KoBelum ada peringkat
- Antiphospholipid Syndrome: Key PointsDokumen10 halamanAntiphospholipid Syndrome: Key PointsNelson CespedesBelum ada peringkat
- Lecture 3. Bleeding Disorders Part 1Dokumen31 halamanLecture 3. Bleeding Disorders Part 1Kekelwa Mutumwenu Snr100% (1)
- Blood Transfusion AlexDokumen33 halamanBlood Transfusion AlexaymenBelum ada peringkat
- ThrombophiliaDokumen46 halamanThrombophiliaNabelle MarieBelum ada peringkat
- Bleeding and ThrombosisDokumen27 halamanBleeding and Thrombosisswathi bsBelum ada peringkat
- Hematologic Pathology p1-23Dokumen23 halamanHematologic Pathology p1-23zeroun24100% (2)
- Hematology Mccq1Dokumen236 halamanHematology Mccq1javaheri.abdorrazaghBelum ada peringkat
- Guide to Transfusions and CoagulopathiesDokumen10 halamanGuide to Transfusions and Coagulopathieskep1313Belum ada peringkat
- Understanding Coagulation DisordersDokumen23 halamanUnderstanding Coagulation DisordersbrightagbotuiBelum ada peringkat
- 1120314晨會 Miller Ch50. Patient Blood Management CoagulationDokumen56 halaman1120314晨會 Miller Ch50. Patient Blood Management Coagulationw8412358Belum ada peringkat
- G6PDD Deficiency and Hemolytic AnemiaDokumen8 halamanG6PDD Deficiency and Hemolytic AnemiaTrisha ArizalaBelum ada peringkat
- Bleeding Disorders 082508Dokumen46 halamanBleeding Disorders 082508Muhammad ShaikhBelum ada peringkat
- Cushing problem greater than 100 mg/dl cortisol in 24 hour urineDokumen22 halamanCushing problem greater than 100 mg/dl cortisol in 24 hour urinerub100% (4)
- Laboratorial Diagnostics Keypoints RevisionDokumen6 halamanLaboratorial Diagnostics Keypoints RevisionFathimathBelum ada peringkat
- Aplastic Anemia: Definition, Diagnosis, Treatment and Response CriteriaDokumen24 halamanAplastic Anemia: Definition, Diagnosis, Treatment and Response CriteriaAnna Puteri GozaliBelum ada peringkat
- Causes of Thromboctyopenia &Dokumen30 halamanCauses of Thromboctyopenia &Rishabh SinghBelum ada peringkat
- Pharmacology II: Treatments for Blood Disorders and InflammationDokumen61 halamanPharmacology II: Treatments for Blood Disorders and InflammationDiane BanuaBelum ada peringkat
- Thrombocytopenia Thrombocytopenia Thrombocytopenia ThrombocytopeniaDokumen12 halamanThrombocytopenia Thrombocytopenia Thrombocytopenia ThrombocytopeniaRashed ShatnawiBelum ada peringkat
- Thrombocytopenia in The Intensive Care UnitDokumen35 halamanThrombocytopenia in The Intensive Care UnitMarcelliaBelum ada peringkat
- Hemolytic Anemia 9-10-2023Dokumen42 halamanHemolytic Anemia 9-10-2023احمد احمدBelum ada peringkat
- Acquired Thrombophilic Syndromes: Daniela Matei, Benjamin Brenner, Victor J. MarderDokumen18 halamanAcquired Thrombophilic Syndromes: Daniela Matei, Benjamin Brenner, Victor J. MarderRahmat SuhitaBelum ada peringkat
- Aplastic AnaemiaDokumen21 halamanAplastic AnaemiaAbhinav ReddyBelum ada peringkat
- Anemia Hemolítica: Causas, Diagnóstico y TratamientoDokumen52 halamanAnemia Hemolítica: Causas, Diagnóstico y TratamientoJonathan CastillomurilloBelum ada peringkat
- Disseminated Intravascular CoagulationDokumen37 halamanDisseminated Intravascular CoagulationAlfitoHarfahGiffaryBelum ada peringkat
- Qualitative Disorder (1) - 1Dokumen27 halamanQualitative Disorder (1) - 1Christyl JoBelum ada peringkat
- Thrombophilia investigations overviewDokumen61 halamanThrombophilia investigations overviewswaraj sharmaBelum ada peringkat
- Disseminated Intravascular Coagulopathy: D.I.C Specific Learning ObjectivesDokumen15 halamanDisseminated Intravascular Coagulopathy: D.I.C Specific Learning ObjectivesmartinBelum ada peringkat
- Case PresentationDokumen36 halamanCase Presentationalmas khanBelum ada peringkat
- Antiphospholipid Syndrome - StatPearls - NCBI BookshelfDokumen10 halamanAntiphospholipid Syndrome - StatPearls - NCBI BookshelfDika KibasBelum ada peringkat
- Kuliah Blok Bleeding DisordersDokumen39 halamanKuliah Blok Bleeding DisordersmantabsipBelum ada peringkat
- Acquired Hemolytic AnemiaDokumen25 halamanAcquired Hemolytic AnemiaShivBelum ada peringkat
- Disseminated Intravascular Coagulation: Keith Lewis, MDDokumen37 halamanDisseminated Intravascular Coagulation: Keith Lewis, MDPutri UtamiBelum ada peringkat
- AMK Diseases p2Dokumen292 halamanAMK Diseases p2hanif ahmadBelum ada peringkat
- Fast Facts: Thrombotic Thrombocytopenic Purpura: Prompt action saves livesDari EverandFast Facts: Thrombotic Thrombocytopenic Purpura: Prompt action saves livesBelum ada peringkat
- Chronic Myelomonocytic LeukemiaDokumen17 halamanChronic Myelomonocytic LeukemiaaymenBelum ada peringkat
- Cerebrovascular AccidentDokumen5 halamanCerebrovascular AccidentaymenBelum ada peringkat
- Recipient and Donor Gender, Age Matching, and Clinical Outcomes in Allogeneic Hematopoietic Stem Cell TransplantationDokumen10 halamanRecipient and Donor Gender, Age Matching, and Clinical Outcomes in Allogeneic Hematopoietic Stem Cell TransplantationaymenBelum ada peringkat
- Tear Cytokines As Biomarkers For Chronic GVHDDokumen7 halamanTear Cytokines As Biomarkers For Chronic GVHDaymenBelum ada peringkat
- Emergency Meds (Shock, Cardiac Arrest, Anaphylaxis)Dokumen1 halamanEmergency Meds (Shock, Cardiac Arrest, Anaphylaxis)aymenBelum ada peringkat
- Carotid Artery PulseDokumen1 halamanCarotid Artery PulseaymenBelum ada peringkat
- Cardiac Arrest PDFDokumen1 halamanCardiac Arrest PDFaymenBelum ada peringkat
- Clinical Transfusion Practice Guidelines For Medical Interns BangladeshDokumen42 halamanClinical Transfusion Practice Guidelines For Medical Interns Bangladeshratriprimadiati100% (1)
- Follicular LymphomaDokumen12 halamanFollicular LymphomaaymenBelum ada peringkat
- A-Gvhd M.saeedDokumen20 halamanA-Gvhd M.saeedaymenBelum ada peringkat
- General Transfusion Practice Quiz For Rotating Medical StaffDokumen3 halamanGeneral Transfusion Practice Quiz For Rotating Medical StaffaymenBelum ada peringkat
- Future Outlook of Checkpoint Receptor InhibitorsDokumen3 halamanFuture Outlook of Checkpoint Receptor InhibitorsaymenBelum ada peringkat
- Future Outlook of Checkpoint Receptor InhibitorsDokumen3 halamanFuture Outlook of Checkpoint Receptor InhibitorsaymenBelum ada peringkat
- Transfusion Related Immunomodulation (Trim)Dokumen14 halamanTransfusion Related Immunomodulation (Trim)aymenBelum ada peringkat
- AFP 2013 Hemochromatosis Hereditary PDFDokumen8 halamanAFP 2013 Hemochromatosis Hereditary PDFleonelcaolBelum ada peringkat
- Thrombolytics - Hematology - Medbullets Step 1Dokumen5 halamanThrombolytics - Hematology - Medbullets Step 1aymen100% (1)
- TRIM: Transfusion Related Immunomodulation ExplainedDokumen14 halamanTRIM: Transfusion Related Immunomodulation ExplainedaymenBelum ada peringkat
- LymphomasDokumen1 halamanLymphomasaymenBelum ada peringkat
- Genetics Hemophilia Flashcards - QuizletDokumen9 halamanGenetics Hemophilia Flashcards - QuizletaymenBelum ada peringkat
- Naturally Occurring Anticancer DrugsDokumen1 halamanNaturally Occurring Anticancer DrugsaymenBelum ada peringkat
- Arterial Blood Gases (ABG) : Shaza AlyDokumen56 halamanArterial Blood Gases (ABG) : Shaza AlyaymenBelum ada peringkat
- Causes of Anemia - Autoimmune Hemolytic AnemiaDokumen2 halamanCauses of Anemia - Autoimmune Hemolytic AnemiaaymenBelum ada peringkat
- Hematological Manifestations of Connective Tissue Disorders: Aymen OmerDokumen69 halamanHematological Manifestations of Connective Tissue Disorders: Aymen OmeraymenBelum ada peringkat
- Protein C - S Deficiency - Hematology - Medbullets Step 1Dokumen4 halamanProtein C - S Deficiency - Hematology - Medbullets Step 1aymenBelum ada peringkat
- Lymphadenopathy and MalignancyDokumen8 halamanLymphadenopathy and MalignancymolenBelum ada peringkat
- Lecture Hemophilia and Thrombocytopenic PurpuraDokumen55 halamanLecture Hemophilia and Thrombocytopenic PurpuraaymenBelum ada peringkat
- Highferritin Web ServerDokumen6 halamanHighferritin Web ServeraymenBelum ada peringkat
- Acute Lymphoblastic Leukemia Prof.S.Tito'S Unit M5 Dr.M.ArivumaniDokumen47 halamanAcute Lymphoblastic Leukemia Prof.S.Tito'S Unit M5 Dr.M.ArivumaniaymenBelum ada peringkat
- Mnemonics M2Dokumen22 halamanMnemonics M2aymenBelum ada peringkat
- Blood Coagulation Overview and Inherited Hemorrhagic Disorders Questions 2Dokumen25 halamanBlood Coagulation Overview and Inherited Hemorrhagic Disorders Questions 2John M. Hemsworth50% (2)
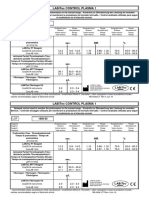
- LABiTec Control 1 Insert 1956 35 Revision 2.0Dokumen1 halamanLABiTec Control 1 Insert 1956 35 Revision 2.0Carla YcoBelum ada peringkat
- Management of Bleeding in Dentistry NewDokumen59 halamanManagement of Bleeding in Dentistry NewAnushriya DuttaBelum ada peringkat
- Drugs Used in Disorders of CoagulationDokumen6 halamanDrugs Used in Disorders of CoagulationAimee Redor100% (1)
- Blood Coagulation SeminarDokumen115 halamanBlood Coagulation SeminarmeghaBelum ada peringkat
- Physiology of Hemostasis - Dr. Rahmat Dani Satria PH.D., SP - PK (K)Dokumen27 halamanPhysiology of Hemostasis - Dr. Rahmat Dani Satria PH.D., SP - PK (K)Viand NugrohoBelum ada peringkat
- HomeostasisDokumen8 halamanHomeostasisLely SharmaBelum ada peringkat
- Review Article: The Role of Thrombophilia in PregnancyDokumen14 halamanReview Article: The Role of Thrombophilia in PregnancyTina GrosuBelum ada peringkat
- TEG® Analysis: Sample Data: Normal Values: CPT/Billing Codes: UnitsDokumen1 halamanTEG® Analysis: Sample Data: Normal Values: CPT/Billing Codes: UnitsDendyBelum ada peringkat
- Interpreting Thromboelastography (TEG) - RK - MDDokumen1 halamanInterpreting Thromboelastography (TEG) - RK - MDNicolas HortonBelum ada peringkat
- Hemodynamic Disorders Thrombosis and Shock MCQS2Dokumen4 halamanHemodynamic Disorders Thrombosis and Shock MCQS2Tahir AzizBelum ada peringkat
- Bloody Easy - Coagulation ExplainedDokumen25 halamanBloody Easy - Coagulation ExplainedDaniela GreereBelum ada peringkat
- Experiment 11: Bleeding Disorder Excessive Clotting Disorder AnticoagulantDokumen3 halamanExperiment 11: Bleeding Disorder Excessive Clotting Disorder AnticoagulantDhyu FernaBelum ada peringkat
- Disseminated Intravascular Coagulation Concept MapDokumen3 halamanDisseminated Intravascular Coagulation Concept MapphoebjaetanBelum ada peringkat
- How I Treat Disseminated Intravascular CoagulationDokumen10 halamanHow I Treat Disseminated Intravascular CoagulationSergio Alberto Sulub NavarreteBelum ada peringkat
- Bleeding NeonateDokumen38 halamanBleeding NeonateAchyut KanungoBelum ada peringkat
- LABORATORY EVALUATION OF PLATELETSDokumen4 halamanLABORATORY EVALUATION OF PLATELETScherry nokiaBelum ada peringkat
- Coagulation Guidelines For Unexplained Bleeding DisordersDokumen2 halamanCoagulation Guidelines For Unexplained Bleeding DisordersPieter Du Toit-EnslinBelum ada peringkat
- Secondary HemostasisDokumen9 halamanSecondary HemostasisMedicah Simon PeligrinoBelum ada peringkat
- HDB 20303 BASIC HEMATOLOGY TOPICS ON HEMOSTASIS AND LAB EVALUATIONDokumen3 halamanHDB 20303 BASIC HEMATOLOGY TOPICS ON HEMOSTASIS AND LAB EVALUATIONNida RidzuanBelum ada peringkat
- Lupus AnticoagulantDokumen27 halamanLupus AnticoagulantAndrew Arnold David Villanueva100% (1)
- Hema2 Lec PrefinalDokumen9 halamanHema2 Lec Prefinallai cruzBelum ada peringkat
- Perioperative Thrombocytopenia.98643Dokumen10 halamanPerioperative Thrombocytopenia.98643Andreea MitranBelum ada peringkat
- Bleeding TimeDokumen47 halamanBleeding Timechickenbacon34Belum ada peringkat
- Hemostasis - Hematology BlockDokumen40 halamanHemostasis - Hematology BlockamandaBelum ada peringkat
- When a Child's Nosebleeds Could Be a Blood DisorderDokumen29 halamanWhen a Child's Nosebleeds Could Be a Blood Disordergalihmd07Belum ada peringkat
- Bleeding and ThrombosisDokumen27 halamanBleeding and Thrombosisswathi bsBelum ada peringkat
- Tutorial Module 4 "Scenario 2": By: Group 5ADokumen18 halamanTutorial Module 4 "Scenario 2": By: Group 5ASalman MuhammadBelum ada peringkat
- PBL 5 Coagulation PathwaysDokumen7 halamanPBL 5 Coagulation PathwaysHugh JacobsBelum ada peringkat
- CTH D Dimers May 2 2013 PDFDokumen42 halamanCTH D Dimers May 2 2013 PDFRaghu NadhBelum ada peringkat
- MLS 014 - Sas 4Dokumen5 halamanMLS 014 - Sas 4Ylia MastarsBelum ada peringkat