Biochemical Changes After Trauma and Skeletal Surgery of The Lower Extremity Quantification of The Operative Burden CCM
Diunggah oleh
Diego Cruces OrdoñezJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Biochemical Changes After Trauma and Skeletal Surgery of The Lower Extremity Quantification of The Operative Burden CCM
Diunggah oleh
Diego Cruces OrdoñezHak Cipta:
Format Tersedia
Biochemical changes after trauma and skeletal surgery of the
lower extremity: Quantification of the operative burden
Hans-Christoph Pape, MD; Reinhold E. Schmidt, MD; John Rice, FRCS; Martijn van Griensven, PhD;
Ronjan das Gupta; Christian Krettek, MD; Harald Tscherne, MD
Objective: To quantify changes in variables of inflammation,
coagulation, and fibrinolysis in blunt trauma patients with lower
extremity fractures who underwent different types of surgical
procedures.
Design: Prospective, cohort study.
Setting: Level I university trauma center.
Patients: We allocated 83 blunt trauma patients in stable
condition and 22 patients eligible for elective hip replacement to
four treatment groups.
Interventions: In 34 multiply traumatized patients with femoral
fracture (group PTFF) and in 28 patients with an isolated femoral
fracture (group IFF), primary unreamed intramedullary nailing for
stabilization of the femoral shaft fracture was performed. In 22
patients, an elective uncemented total hip arthroplasty (group
THA) was inserted for osteoarthritis, and in 21 control patients, an
isolated ankle fracture (group AF) was acutely stabilized.
Measurements and Main Results: From serially sampled central venous blood, the perioperative concentrations of interleukin
(IL)-6, of tumor necrosis factor-, of prothrombin fragments 1
2, and of D-dimer cross-linked fibrin degradation products were
evaluated. Intramedullary instrumentation for an isolated femur
fracture caused a significant perioperative increase in the concentrations of IL-6 (preoperative IL-6, 52 12 pg/mL; IL-6 30
mins postinsertion, 78 14 pg/mL; p .02). This increase was
comparable with group THA (preoperative IL-6, 46 16 pg/mL;
IL-6 30 mins postinsertion, 67 11 pg/mL; p .03). A positive
correlation occurred between both groups (r .83, p < .0004).
Multiple trauma patients demonstrated significantly (p .0002)
t is widely accepted that both
blunt trauma and surgery induce
inflammatory changes (1, 2) and
coagulatory and fibrinolytic responses (3, 4). In the multiple trauma
patient, the relative contribution to the
systemic inflammatory response by the
From the Department of Clinical Immunology (Dr.
Schmidt), Hannover Medical School, Hannover, Germany, and the Department of Trauma Surgery at Hannover (Drs. Pape, Rice, van Griensven, and Tscherne
and Mr. das Gupta), Department of Trauma (Dr.
Krettek), Monash University, Melbourne, Australia.
Supported, in part, by the Orthopaedic Trauma Association and the Deutsche Forschungsgemeinschaft,
(Project No. PA 426/21), Bonn, Germany.
Copyright 2000 by Lippincott Williams & Wilkins
Crit Care Med 2000 Vol. 28, No. 10
higher IL-6 concentrations than all other groups throughout the
study period and showed a significant increase after femoral
nailing (preoperative IL-6, 570 21 pg/mL; IL-6 30 mins postinsertion, 690 24 pg/mL; p .003), whereas no perioperative
change was seen in group AF. The highest IL-6 increases were
associated with a longer ventilation time (group PTFF) and a
longer period of positive fluid balances (groups PTFF, IFF, THA).
The coagulatory variables demonstrated similar perioperative increases in groups IFF and THA, but not in groups PTFF and AF. The
IL-6 concentrations and the prothrombin fragments 1 2 concentrations correlated between groups THA and IFF at 30 mins
and at 1 hr after surgery (r2 .64, p < .02). In all patients the
clinical variables were stable perioperatively.
Conclusions: Major surgery of the lower extremity causes
changes to the inflammatory, fibrinolytic, and coagulatory cascades in patients with stable cardiopulmonary function. The inflammatory response induced by femoral nailing is biochemically
comparable to that induced by uncemented total hip arthroplasty.
In multiple trauma patients, increases, which occurred in addition
to those induced by the initial trauma, were measured. Definitive
primary femoral stabilization by intramedullary nailing imposes
an additional burden to the patient with blunt trauma. A careful
preoperative investigation is required to evaluate whether primary
definitive stabilization can be performed safely. (Crit Care Med
2000; 28:34413448)
KEY WORDS: systemic inflammatory response; interleukin-6; tumor necrosis factor-; hypercoagulability; blunt multiple trauma;
primary fracture fixation; femoral nailing
first hit and by the subsequent surgery
(second hit) continue to be debated (5, 6).
These patients frequently have long bone
fractures, which contribute significantly
to the subsequent morbidity (7, 8). Although primary operative stabilization of
these fractures reduce the overall frequency rate of posttraumatic complications (9), adverse changes in inflammatory mediators have been described with
respect to primary intramedullary stabilization of fractures (10, 11), and especially for reamed nails (12, 13). Among
the proinflammatory cytokines, it is recognized that IL-6 has a central role in
determining the insult induced both by
surgery and trauma (2, 5, 6). Likewise,
serum levels of fibrin degradation products and prothrombin fragments are regarded as sensitive indicators of responses in the fibrinolytic and coagulatory cascades, respectively (14, 15).
Sustained alterations in these markers
have been associated with systemic complications including organ failure (16),
but the magnitude and relevance of these
alterations in trauma patients who are
physiologically stable are not widely appreciated.
Although these markers represent
physiologic changes relevant to trauma
management, the magnitude of skeletal
injury and surgery have not been precisely defined. The aim of this study is to
3441
document perioperative changes for
these biological markers with lower limb
surgery in defined patient groups.
PATIENTS AND METHODS
This investigation was designed as a prospective, nonrandomized cohort study. It was
performed between November 1996 and September 1998, with approval of the ethical
board of our institution in accordance with
the standards of the Helsinki declaration
(1975).
The base population (group PTFF) consisted of consecutive patients with multiple
trauma (Injury Severity Score 18 points).
Injuries included a femoral shaft fracture stabilized with an unreamed femoral nail within
24 hrs after the accident. Our general protocol
for multiple trauma patients includes early
on-site intubation and ventilation. If the patient is in extremis, clinically unstable, or in
an uncertain clinical condition (borderline patient) (11), we use primary external fixation,
followed by conversion to internal fixation
within days thereafter (damage control orthopedics) (17, 18). In all stable patients, primary
stabilization by unreamed femoral nailing is
performed by the anterograde technique.
The comparative groups involved consecutive patients who fulfilled criteria regarding
premorbid conditions, type of injury, and surgery, as specified below. In addition, measurements were obtained from 20 healthy volunteers. Patients with an isolated femoral shaft
fracture (IFF) treated by an unreamed femoral
nail within 24 hrs after the accident were
group IFF. Patients who had osteoarthritis of
the hip treated with an elective uncemented
total hip arthroplasty (THA) were group THA.
Patients with an isolated closed ankle fracture
(AF) stabilized surgically within 24 hrs after
the initial injury were the control, group AF.
Inclusion Criteria. Inclusion criteria for all
patients were as follows: age ranging from 18
to 70 yrs; primary care and surgery at the
Department of Trauma Surgery, Hannover
Medical School; no preexisting pulmonary disease (chronic obstructive pulmonary disease,
malignancy, or previous thoracic trauma); no
preexisting coagulatory disorder; no pretreatment with anticoagulants; no local or systemic infection (pneumonia, sepsis, soft tissue
infection, acquired immunodeficiency syndrome, or tuberculosis etc.) at the time of
accident; and no history of liver disease.
Patients with penetrating trauma and with
lung contusions were also excluded. A lung
contusion was diagnosed if radiologic signs of
parenchymal localized pulmonary damage in
the absence of preexisting lung disease were
found on anteroposterior chest radiographs or
by chest computed tomography. Lung contusion was independently diagnosed by a radiologist on the basis of the initial chest radio-
3442
graph and the control at 24 hrs, thereafter
(19).
In trauma patients, the severity of injury
was categorized preoperatively by using the
Injury Severity Score (20). On arrival at the
operating room, each patient had arterial
blood gas measured and a central venous catheter inserted. Blood withdrawal was performed
according to a standardized schedule and sent
for laboratory analysis as described below (Table 1). Throughout the operations, electrocardiogram monitoring and a continuous temperature recording were performed by using a
rectal probe. Patients undergoing stabilization
of ankle fractures usually had an arterial thigh
tourniquet inflated to 250 mm Hg. Intraoperative blood loss describes the amount of blood
collected during the operative procedures (intramuscular nailing, THA, and ankle surgery).
In group PTFF, the amount of blood collected
during other surgical procedures was not included. During the postoperative period details on complications were recorded prospectively in a standardized form. No active
screening for thromboembolic complications
was performed, these were investigated on the
basis of clinical suspicion. The ventilation
time encompassed the period between intubation and extubation. The intensive care unit
stay summarizes the time from admission to
the intensive care unit until transfer to a normal ward. A positive fluid balance was diagnosed when the ratio of fluid input and output
exceeded 500 mL per 24 hrs. Multiple organ
failure, sepsis, and adult respiratory distress
syndrome were determined by scoring systems
(21, 22).
Proinflammatory Cytokines. For determination of cytokine levels, central venous blood
was collected in sterile tubes containing glass
beads (Sarstedt, Hamburg, Germany). After
centrifugation for 10 mins at 2000 g, serum
was transferred into sterile 1.5 mL tubes, and
the samples were stored at 20C (4F)
until further analysis.
Serum concentrations of tumor necrosis
factor (TNF)- were determined by using a
sandwich ELISA technique. Recombinant
TNF- (Bissendorf, Hannover, Germany) was
used as a standard criterion. Polyclonal rabbit
antihuman TNF- was used as a capture anti-
body. To detect bound TNF-, a monoclonal
mouse antihuman TNF- Fab-fragment conjugated to peroxidase (Boehringer-Mannheim,
Mannheim, Germany) was applied to the samples. After washing, 3,3,5,5-tetramethylbenzidine was added to the complex as a substrate
for the peroxidase. After termination of the
reaction with 4 N sulfuric acid, the optical
density of the samples was measured at 450
nm by using an ELISA reader. The detection
level of this assay was 60 pg/mL.
Interleukin (IL)-6 was measured in serum
samples by means of a commercial solid
phase ELISA (WAK Medical, Bad Hamburg,
Germany). Recombinant IL-6 (BoehringerMannheim) was used to produce a standard
curve. The detection level was at 10 pg/mL.
Microtiter plates were coated with the monoclonal anti-IL-6 antibody BE-8 (7 g/mL in
phosphate buffered saline, pH 7.4). After a
24-hr incubation at 4C (39.2F), the plates
were washed with phosphate buffered saline
containing 0.02% (volume/volume) Tween-20.
A 60-min incubation was performed at room
temperature. Then, phosphate buffered saline
was substituted with 0.1% bovine serum albumin. After washing, serial dilutions of standard recombinant human IL-6 or serum samples were added to the wells and incubated for
1 hr at 37C (98.6F). A monoclonal biotinylated anti-IL-6 BE-4 was added to the wells for
60 mins at 37C (98.6F). To analyze the
amount of bound secondary antibody, 100 L
streptavidin horseradish peroxidase was added
to the samples for 45 mins at 37C (98.6F).
Orthophenyldiamine was used as a substrate
for the peroxidase. It was applied in a citric
acid buffer (pH 5.2) containing 0.003% hydrogen peroxide. Incubation was performed for 30
mins, then 4 N sulfuric acid was added for
termination of the reaction. The optical density of the samples was measured at 495 nm by
using an ELISA reader.
Coagulatory and Fibrinolytic Variables.
The investigation of coagulatory variables involved fresh samples. Platelet-poor plasma was
prepared from 4.5 mL of blood which was
mixed with 0.5 mL of 0.1 mol/L sodium citrate
in an 8 mL siliconized glass tube, which was
centrifuged at 2600 rpm for 20 mins. The
plasma was then centrifuged at 10,000 rpm for
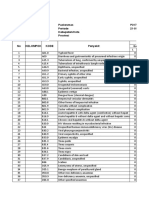
Table 1. Schedule of blood withdrawal and measurements from central venous blood as well as
hemodynamic measurements
Blood Withdrawal
Time
Instrumentation
II-6/TNF-
B
I
30 mins
1 hr
7 hrs
24 hrs
Baseline (skin incision)
Insertion of nail/THA/plate
30 mins after insertion
1 hr after insertion
7 hrs after insertion
24 hrs after insertion
D-Dimer/F1
II, interleukin; TNF, tumor necrosis factor; F, prothombin fragments; B, baseline; I, insertion of
the intramedullary nail; THA, total hip arthroplasty.
Crit Care Med 2000 Vol. 28, No. 10
20 mins at 4C (39.2F). Plasma samples were
aliquoted and snap-frozen in ethanol dry ice
before being stored at 70C (56F).
For measurements of prothrombin fragments 1 2 (F1 2), an enzyme-linked
immunoabsorbent assay (Behring Diagnostics, Marburg, Germany) was used. Prothrombin F1 2 were bound to monoclonal antibodies attached to a microtiter plate. After
several washing and incubation steps, the
samples were then incubated with a secondary
peroxidase-conjugated antibody that binds
specifically to other epitopes of the fibrin-split
products. The detection level is at 500 g/L.
D-dimer cross-linked fibrin degradation products in plasma were measured by using a Ddimer ELISA kit (Organon Technika, Eppelheim, Germany).
Statistics. Differences among patient
groups were determined by the Kruskal-Wallis
test and Wilcoxons two-sample test. For analysis of correlations among different variables,
the Spearmans correlation coefficient was
performed. A p .05 was considered significant.
RESULTS
Demographic Data, Perioperative
Condition, and Clinical Course. Of 115
multiple trauma patients, 105 patients
were studied prospectively. Two patients
had signs of lung contusion on initial
chest computed tomography and were excluded. Two patients developed typical
changes of lung contusion on the routine
plain chest radiograph at the 24-hr time
point and were excluded. Three patients
had been pretreated with anticoagulants;
three patients had preexisting chronic
obstructive pulmonary disease and were
excluded from the study.
All patients were initially brought to
our institution. The demographic data of
the patients included in the study are
demonstrated in Table 2. There were six
open tibial fractures and five compound
distal femoral fractures contralateral to
the side submitted to an unreamed intramedullary nail. The mean values of the
local injury severity determined by abbreviated injury scale (AIS) is as follows:
AISHead 2.8 0.2, AISFace 1.8 0.6, AISAbdomen 1.6 0.5, AISExtr 3.43 0.31, and
AISExternal 1.6 1.2. No patient required
craniotomy. In one patient, a laparotomy
was performed and a splenectomy done.
Five patients had pelvic injuries requiring
a supra-acetabular external fixateur. The
open tibial fractures were initially stabilized by using an unreamed tibial nail. In
9 of 21 patients of group AF, a tourniquet
was placed, but not inflated. One patient
had a left lower lobe lung contusion diCrit Care Med 2000 Vol. 28, No. 10
agnosed on chest computed tomography
on day 3 after the initial injury. This
patient belonged to group PTFF and required prolonged ventilatory support, but
did not develop acute respiratory distress
syndrome. There were no significant differences among the groups in patient
numbers or gender distribution. A tendency toward a higher patient age in
group THA compared with all other
groups was not significant. In group
PTFF, one patient developed deep venous
thrombosis which was detected 16 days
after the initial injury. In group THA, one
patient developed deep venous thrombosis 9 days after the operation. There were
no discernible differences among the patient groups in frequency rate of other
complications (Table 2). The group of
volunteers consisted of 20 healthy men
ranging in age from 22 to 26 yrs.
Table 3 documents the duration and
time of surgery and the intraoperative
and perioperative laboratory and physiologic data. A tendency toward a longer
duration of surgery in group PTFF was
found; this difference was not statistically
significant. The intraoperative blood loss
was significantly higher in group THA
than in all other groups (p .03 vs.
PTFF, p .03 vs. IFF, p .02 vs. AF).
The preoperative temperature was significantly lower in group PTFF compared
with the groups THA (p .03) and AF
(p .04). There was a tendency toward
an increased intraoperative loss of temperature in groups PTFF and IFF compared with group AF. This difference did
not reach statistical significance. The arterial blood pressure and the oxygenation
(PaO2/FIO2) were within physiologic normal ranges and remained stable in all
groups, perioperatively. Subgroups of patients were differentiated according to
the magnitude of perioperative IL-6 increases. Variables of the clinical course
are depicted in Table 4.
Inflammatory Variables. Table 5 demonstrates the serum concentrations of
TNF-. In group PTFF, these levels were
significantly higher than in all other
groups at all time points studied. There
was a tendency toward an increase in the
concentrations of TNF- in groups PTFF,
IFF, and THA, but these increases did not
reach statistical significance.
The central venous concentrations of
IL-6 in group PTFF were significantly
(p .0002) elevated compared with all
other groups during the entire study period. There was a statistically significant
increase compared with baseline levels at
30 mins, 1 hr, and 7 hrs after insertion of
the femoral nail. Group IFF demonstrated significantly elevated IL-6 concentrations compared with 20 healthy
volunteers (12 18 g/mL) and significantly higher levels (p .03) than patients of group AF in all comparative
samples throughout the study did. In
group IFF, a significant increase compared with baseline levels was found at
the time of insertion of the intramedullary nail, and 30 mins, thereafter. Statistically significant increases in comparison with baseline levels were also
determined in group THA at insertion of
the femoral component and at 30 mins
afterward. At 30 mins after insertion, the
measured increases of IL-6 concentrations showed a correlation between
groups IFF and THA (r .83; p .0004)
and were of comparable magnitude. In
group AF, IL-6 concentrations did not
Table 2. Demographic data and complications during the hospital course
Patient group
No. of patients
Age (yrs), mean SD
Gender (M/F)
ISS, mean SDa
Complications (no.)
Deep vein thrombosis
Local infection
Pneumonia
Sepsis
ARDS
MOF
PTFF
IFF
THA
AF
34
35 12
21/13
22.7 5.2
28
38 16
15/13
8.4 2.1
22
47 19
12/10
21
22 7
12/9
4.0 1.4
0
1
0
0
0
0
1
0
0
0
0
0
1
1
0
0
0
0
1
0
1
1
1
1
PTFF, multiply traumatized with femoral fracture; IFF, isolated femoral fracture; THA, total hip
arthroplasty; AF, ankle fracture; ISS, Injury Severity Score; , no injuries; ARDS, acute respiratory
distress syndrome; MOF, multiple organ failure.
a
p .02, PTFF vs. IFF and AF; p .003, PTFF vs. AF.
3443
Table 3. Variables of the perioperative clinical condition
Patient Group
PTFF
IFF
THA
AF
p Value
Rescue time (min)
Admission-surgery (min)
Time to surgery (min)
Duration of surgery (min)
Intra-OP blood loss femur (mB)
Intra-OP blood loss total (mB)
Total 24-hr blood loss (mB)
Pre-OP temperature (C)
Intra-OP loss of temperature (C)
Pre-OP systemic ABP (mm Hg)
Post-OP systemic ABP (mm Hg)
Pre-OP PaO2/FIO2
Post-OP PaO2/FIO2
Pre-OP platelets (1000/L)
Post-OP platelets (1000/L)
65 35
95 40
150 50
66 20
70 26
480 120
790 210
33.4 1.9a
1.2 0.5
110 15
110 20
330 335
310 30
140 45
120 55
95 60
65 30
160 40
62 24
91 29
91 29
120 60
35.9 1.4
1.5 0.7
120 15
110 25
350 45
330 55
160 35
150 45
55 19
210 51
210 51
250 80
36.1 0.6
0.8 0.7
140 20
130 25
310 30
290 40
190 40
180 40
220 40
40 30
260 70
47 32
38 15
38 15
38 15
36.0 1.0
0.4 0.3
125 20
120 15
350 20
345 40
180 25
190 35
.05 (AF vs. PTFF and IFF)
NS
NS
NS
.02 (THA vs. IFF and AF)
.01 (PTFF vs. all)
.01 (PTFF vs. all)
.04 (PTFF vs. AF)
NS
NS
NS
NS
NS
NS
NS
PTFF, multiply traumatized with femoral fracture; IFF, isolated femoral fracture; THA, total hip arthroplasty; AF, ankle fracture; Rescue time, time
between trauma and admission to the hospital; , no emergencies; Admission-surgery, time between admission to the hospital and skin incision; Time
to surgery, time between trauma and skin incision; OP, operative; ABP, arterial blood pressure.
a
Significant difference compared with group AF. There was a statistically higher amount of blood administered intraoperatively in group THA compared
with all other groups. The preoperative temperature was significantly lower in group PTFF compared with groups THA and AF.
Table 4. Variables of the clinical course in subgroups of patients selected according to the degree of perioperative cytokine secretion
Group
PTFF
H
L
IFF
H
L
THA
H
L
AF
H
L
Ventilation
(Days)
p Value
H vs. L
ICU Stay
(Days)
p Value
H vs. L
Positive I/O
(Days)
p Value
H vs. L
3.3 1.1
1.0 0.6
.04
4.9 1.3
1.8 0.9
.05
4.6 1.0
1.6 1.0
.03
1.2 0.7
0.7 0.4
NS
1.6 0.9
1.1 0.9
NS
1.7 0.7
0.5 0.4
.04
0.9 0.5
0.6 0.4
NS
1.3 0.8
0.9 0.7
NS
1.4 0.6
0.5 0.2
.05
0.1 0.02
0.1 0.05
NS
0
0
NS
0.01 0.01
0.01 0.01
NS
H, subgroup consisting of those six patients within one of the four groups who developed the highest perioperative increase in interleukin-6
concentrations; L, subgroup consisting of those six patients within one of the four groups who developed the lowest perioperative increase in interleukin-6
concentrations; ICU, intensive care unit; Positive I/O, duration of positive fluid balance (input/output 500 mL/24 hrs); PTFF, multiply traumatized with
femoral fracture; IFF, isolated femoral fracture; THA, total hip arthroplasty; AF, ankle fracture.
Table 5. Perioperative serum concentrations of tumor necrosis factor- (ng/mL)
Group
30 Mins
1 Hr
7 Hrs
24 Hrs
PTFF
IFF
THA
AF
1.0 0.3a
0.2 0.08
0.1 0.05
0.07 0.06
0.9 0.4a
0.2 0.09
0.12 0.1
0.08 0.08
1.1 0.3a
0.24 0.05
0.14 0.07
0.06 0.04
1.0 0.4a
0.2 0.11
0.17 0.12
0.1 0.06
1.1 0.24a
0.21 0.13
0.18 0.11
0.11 0.09
.2 0.3a
0.14 0.12
0.13 0.11
0.07 0.7
B, baseline; I, insertion of the intramedullary nail; PTFF, multiply traumatized with femoral fracture; IFF, isolated femoral fracture; THA, total hip
arthroplasty; AF, ankle fracture.
a
Significant difference between the groups PTFF and all other groups. No group demonstrated significant increases in the concentrations of tumor
necrosis factor- compared with baseline levels.
demonstrate a statistically significant difference compared with baseline levels or
with healthy volunteers (Fig. 1).
Fibrinolytic and Coagulatory Variables. The concentrations of cross-linked
fibrin degradation products in group
3444
PTFF were significantly higher than the
concentrations in all other groups at several times (baseline, at insertion, and 24
hrs after the initial injury). At 30 mins
and at 1 hr after intramedullary instrumentation, a significant difference was
present only in comparison with group
AF. In group IFF, the D-dimer levels were
significantly higher than the normal laboratory range during the entire study period. From baseline to insertion and to
the 30-min time point, group IFF DCrit Care Med 2000 Vol. 28, No. 10
dimer concentrations showed a significant (p .02) increase. In group THA, a
significant increase compared with baseline was found at 30 mins, 1 hr, and at 7
hrs after insertion (Fig. 2).
The prothrombin F1 2 in group
PTFF was significantly elevated (p .03)
throughout the study period. At 30 mins
and 1 hr postoperatively, the concentrations were not different from groups IFF
and THA. There was a statistically significant difference at 7 and 24 hrs after
surgery in these groups. Groups IFF and
THA also demonstrated a significant increase from baseline to 1 hr after surgery.
In group AF, no discernible increase in
prothrombin F1 2 was measured (Fig.
3). There was a positive correlation between the percentage change of baseline
IL-6 concentrations and the prothrombin
F1 2 concentrations in both groups
(THA and IFF) at 30 mins after insertion
(r .79; p .02).
DISCUSSION
In the present study, we document
significant inflammatory, coagulatory,
and fibrinolytic responses with respect to
the degree of trauma and subsequent surgery in clinically stable patients. Our
principal results demonstrate the following: activation of these cascades by femoral intramedullary nailing comparable
with that induced by a total hip arthroplasty; no such activation was measured
during operative fixation of ankle fractures; in multiple trauma patients, surgery added to the proinflammatory cytokine release induced by the initial injury;
Figure 1. Posttraumatic course of the central
venous concentration of the proinflammatory cytokine interleukin-6. All data were corrected for
hematocrit. The first (open) bar indicates the
mean value obtained from 20 healthy volunteers.
Significant (p .05) differences between group
PTFF and all other groups are marked by an
asterisk; significant differences to baseline (B)
are marked by a cross. PTFF, multiply traumatized with femoral fracture; IFF, isolated femoral
fracture; THA, total hip arthroplasty; AF, ankle
fracture.
Crit Care Med 2000 Vol. 28, No. 10
and in patients with the highest perioperative increases in IL-6 concentrations,
a longer ventilation time (group PTFF)
and a longer period of positive fluid balances (groups PTFF, IFF, THA) was found
when compared with those demonstrating the lowest perioperative increases of
this variable.
The fact there was no difference in the
frequency rate of acute respiratory distress syndrome or multiple organ failure
is most likely a result of patient selection.
In a previous study (11), we warned
against patients with unstable vital signs
and against borderline patients whose vital signs are stable but who have other
risk factors to develop posttraumatic
complications. Since then, we initially
stabilize the femoral shaft fracture by external fixation (damage control orthopedic surgery), if the clinical condition is
uncertain. In addition, we have replaced
reamed nailing by unreamed nailing of
the femur, which has less systemic effects
(6, 13). All patients submitted to primary
definitive femoral stabilization in our
study had stable vital signs before surgery
and no other abnormality in their laboratory findings that would indicate a borderline situation (17).
Previous studies (2, 11, 23) pointed
out that the sequelae of surgical procedures can be measured by biochemical
markers. This burden of surgery may become clinically relevant, if the patient has
a predisposition (hemorrhagic shock,
lung contusion etc.). We therefore hypothesize that similar surgical proce-
Figure 2. Central venous concentrations of fibrin
split products (D-dimer XDP, cross-linked fibrin
degradation products) in four different patient
groups (group PTFF, group IFF, group TPH,
group AF). The first (open) bar indicates the
mean value obtained from 20 healthy volunteers.
Significant (p .05) differences between group
PTFF and all other groups are marked by an
asterisk; significant differences to baseline (B)
are marked by a cross. PTFF, multiply traumatized with femoral fracture; IFF, isolated femoral
fracture; THA, total hip arthroplasty; AF, ankle
fracture.
dures performed in unstable patients
were associated with a higher frequency
rate of postoperative complications.
Our observations on the systemic release of proinflammatory cytokines concur with previous investigations (1, 2).
Giannoudis et al. (6) observed a similar increase in venous levels of IL-6 during reamed intramedullary nailing of the
femur, as seen in the present study.
Cruickshank et al. (5) reported that elective surgical procedures cause an acute
rise in venous levels of IL-6 in proportion
to the magnitude and duration of the
surgical procedure. However, this study
compares various types of surgical procedures and does not focus on skeletal operations. This study does not clearly define the types of surgical procedures
performed, and in particular, does not
address the issues of anticoagulants interfering with the assays of IL-6 in the
patients undergoing vascular surgery.
Also, the possibility of activation of inflammatory mediators by methylmethacrylate (24) in the patient group submitted
to THA is not considered (5). Moreover,
both these latter studies do not indicate
the site of sampling of venous blood for
IL-6 assays (5, 6). The question whether
central or peripheral venous blood was
obtained is important, because the lung
acts as a filter, and the determination of
cytokine levels from central venous blood
is more relevant than that obtained from
peripheral venous blood (25, 26). We feel
that our study provides more reliable
quantitative information regarding the
IL-6 concentrations, because we consistently used central venous samples. This
Figure 3. The perioperative sequence of the central venous concentrations of prothrombin fragments 1 2 during and after surgical intervention. The first (open) bar indicates the mean
value obtained from 20 healthy volunteers. Significant (p .05) differences between group
PTFF and all other groups are marked by an
asterisk; significant differences to baseline (B)
are marked by a cross. PTFF, multiply traumatized with femoral fracture; IFF, isolated femoral
fracture; THA, total hip arthroplasty; AF, ankle
fracture.
3445
lthough the clinical condition may
appear stable, we
feel it is prudent to respect
the subclinical evidence of
activation of cascade systems that may further harm
the patient. The indication
for major surgery of the
lower extremity, namely intramedullary femur fixation
as primary definitive treatment, should be carefully
evaluated in this light.
factor may explain the more acute rise in
IL-6 found in our study compared with
other studies (5).
Our values for IL-6 concentrations in
peripheral venous blood in 20 normal
volunteers (12 18 pg/mL) concurred
with those measured in other studies
(16 10 pg/mL) (27). Also, our study
defines the surgical and traumatic insult
in terms of well-appreciated levels of injury and standardized surgical procedures. In our multiple trauma group, the
issue of further surgery has not been addressed and may have influenced the results. However, the femoral nailing was
always the first procedure carried out.
Therefore, it is likely that the perioperative information truly reflects the effect
of femoral intramedullary nailing.
Cruickshank et al. (5) argued whether
anesthesia may induce changes in proinflammatory cytokines. However, in our
study the observed changes occurred after the femoral instrumentation and decreased before the end of surgery and
artificial ventilation. In view of the short
half-life of IL-6 (28), the occurrence of
peak concentrations at 30 mins after instrumentation suggests that this was not
an effect of induction of anesthesia.
Moreover, the subsequent decline before
the end of surgery in groups PTFF, IFF,
and THA, imply that the changes mea3446
sured are not caused by maintenance anesthetics or mechanical ventilatory support.
Our results discount the value of the
measurement of systemic TNF- concentrations as an acute marker of trauma
and surgery. This effect is unlikely to be
caused by the timing of blood collection,
as previously investigated (29). The serum levels of TNF- have also not correlated with the development of multiple
organ failure and septic shock in trauma
patients (30). Although the role of TNF-
as an inflammatory mediator is recognized in many patient groups, in trauma
patients, binding of serum TNF- to its
shed soluble receptors (31) may interfere
with measurement of its serum levels
(32), which would explain our negative
findings.
Activation of the coagulation and fibrinolytic systems is a normal physiologic response after trauma, sepsis,
burns, surgery, and shock. D-dimer crosslinked fibrin degradation products are accepted as specific markers of fibrinolysis
(15), and indicate the magnitude of soft
tissue (33) and bony injury (34). Our results demonstrate a perioperative induction of this marker for groups IFF and
THA. This effect was not seen in patients
with ankle fractures (group AF) nor in
patients with multiple injuries (group
PTFF). The latter group demonstrated increased fibrinolytic activity before surgery, but no detectable influence of fracture fixation. We suggest that the
magnitude of surgery was not enough to
activate this system in group AF, whereas
in the multiple trauma group the lack of
a perioperative response may have been
caused by a ceiling effect or the fact that
the trauma-induced stimulation outweighs the effect of the surgical procedure. The first assumption is unlikely.
Our maximum D-dimer levels were 15
ng/mL. Enderson et al. (35) describe
higher levels in patients with multisystem trauma, and Gando et al. (36) show a
further increase if trauma is complicated
by disseminated intravascular coagulation. The second assumption may play a
more important role. Even massively increased D-dimer levels were reduced by
half within 48 hrs (4, 36), therefore, the
increase induced by a surgical procedure
may be mimicked by a normal physiologic reduction of D-dimer levels. In our
study, the observed increases of 3
ng/mL in D-dimer cross-linked fibrin degradation products in groups IFF and THA
were only calculated to be statistically
relevant if low baseline values were
present, as seen in groups IFF and THA.
Group PTFF demonstrated massively increased D-dimer levels early after trauma,
and a tendency toward a further increase
after nailing occurred, which was not significant.
We assume that intravasation of intramedullary contents, which contain
high levels of procoagulant factors (7), by
increased intramedullary pressure during
instrumentation (17, 37) is responsible
for the observed increases in F1 2. This
increase might also be caused by passage
into the lung of platelets that aggregate
around fat emboli (38), thus inducing a
systemic coagulatory response (39). We
propose that these effects are probably
aggravated by intramedullary reaming
(8), and by the presence of other associated injuries (34).
It has also been suggested that the
inflammatory response might be responsible for inducing the coagulatory cascade. IL-6 stimulates the production of
C-reactive protein, fibrinogen, and -1
antitrypsin in hepatocytes (40). Clinical
studies demonstrated that elevations of
systemic cytokine levels are more sustained in patients in whom the coagulatory system is altered. Gando et al. (36)
discuss a relationship among increased
proinflammatory cytokines, the coagulatory system, and multiple organ failure.
In our study, a positive correlation between the change in IL-6 and the prothrombin F1 2 concentrations was
measured. This finding supports the idea
of an interaction between the inflammatory and the coagulatory cascade system.
Clinical Implications. Alterations of
proinflammatory cytokines as determined in our study should be considered
a serious insult (16). We hypothesize that
the selection of clinically stable patients
was one reason why no adverse outcome
was found if organ dysfunction was chosen as an end point. Instead, we found
subtle clinical sequelae (duration of ventilation and of positive fluid balance) in
association with high elevations of IL-6
concentrations. Other studies emphasized the role of IL-6 as an indicator of
infectious complications (41), burn injuries (42), and organ dysfunction (2, 43).
Moreover, previous investigations from
our laboratory confirmed that IL-6 serum
concentrations exceeding 800 pg/mL at admission are predictive of later organ failure
(44).
With regard to multiple trauma patients, there is ongoing discussion concerning the optimal time and method of
Crit Care Med 2000 Vol. 28, No. 10
femur fractures. Although Bone et al.
(45) and Bosse et al. (46) advocate early
total care for all such patients, a variety of
studies (5, 6, 9, 12, 47) have demonstrated that the duration and the type of
stabilization definitively alter the clinical
patient condition. Primary surgery of 6
hrs duration was associated with a higher
rate of organ failure (48). Likewise, Friedl
et al. (49) strictly avoided primary nailing
in patients with severe trauma, defined as
an Injury Severity Score of 40 points.
Moreover, the method of stabilization is
known to play a role. Clinical and experimental studies demonstrate that unreamed nailing imposes a less systemic
burden than the reamed procedure (32),
but its impact should not be underestimated (50).
We previously differentiated between
patients who are clinically unstable, even
after resuscitation (systolic blood pressure 100 mm Hg; PaO2/FIO2 200) and
patients who are apparently stable but
have an increased risk to develop postoperative complications. In the first patient
group, we avoided primary definitive stabilization by intramedullary nailing and
used external fixation to stabilize the
fracture. The second group of patients,
who have stable vital signs but have other
reasons to be at high risk of organ failure
was termed, borderline (11). This status
may be present, if a lung contusion is
diagnosed, or if alterations in the coagulatory response, in serum lactate concentrations, and in the fluid balance are
present. We have also recommended
avoidance of primary major operative
surgery in these patients, because we feel
that the operative burden represents a
risk for postoperative complications. According to our experience, most patients
regarded not eligible for primary definitive treatment of the long bone fracture
had other clinical causes preventing their
benefit from early total care.
CONCLUSIONS
The activation of inflammatory, coagulatory, and fibrinolytic cascades by
trauma and surgery may have important
consequences for the trauma patient. Although the clinical condition may appear
stable, we feel it is prudent to respect the
subclinical evidence of activation of cascade systems that may further harm the
patient. The indication for major surgery
of the lower extremity, namely intramedullary femur fixation as primary definitive
Crit Care Med 2000 Vol. 28, No. 10
treatment, should be carefully evaluated
in this light.
REFERENCES
1. Ayala A, Wang P, Ba ZF, et al: Differential
alterations in plasma IL-6 and TNF levels
after trauma and hemorrhage. Am J Physiol
1991; 260:R167R171
2. Roumen RM, Hendrijks T, ven der VenJongekrijg, et al: Cytokine patterns in patients after major vascular surgery, hemorrhagic shock, and severe blunt trauma:
Relation with subsequent adult respiratory
distress syndrome and multiple organ failure. Ann Surg 1993; 218:769 776
3. Murphy WG, Davies MJ, Eduardo A: The hemostatic response to surgery and trauma.
Br J Anesth 1993; 70:205213
4. Gando S, Tedo I, Kubota M: Posttrauma coagulation and fibrinolysis. Crit Care Med
1992; 20:594 600
5. Cruickshank AM, Fraser WD, Bruns HJG, et
al: Response of serum interleukin-6 in patients undergoing elective surgery of varying
severity. Clin Sci (Colch) 1990; 79:161165
6. Giannoudis PV, Smith RM, Bellamy MC, et
al: Stimulation of the inflammatory system
by reamed and unreamed nailing of femoral
fractures. JBJS-B 1999; 81:356 361
7. Riseborough EJ, Herndon J: Alterations in
pulmonary function, coagulation and fat metabolism in patients with fractures of the
lower limbs. Clin Orthop Rel Res 1976; 115:
248 266
8. Kuntscher G: Dangers of intramedullary
nailing. In: Practice of Intramedullary Nailing. Kuntscher G (Ed). Springfield, Illinois,
Charles C Thomas, 1962, pp 36 51
9. Seibel R, LaDuca J, Hassett JM, et al: Blunt
multiple trauma (ISS 36), femur traction and
the pulmonary failure septic state. Ann Surg
1985; 202:283293
10. Nast-Kolb D, Waydhas C, Jochum M, et al: [Is
there a favorable time for the management of
femoral shaft fracture in polytrauma?] German. Chirurg 1990; 61:259 264
11. Pape H-C, AufmKolk M, Paffrath T, et al:
Primary intramedullary fixation in polytrauma patients with associated lung contusion: A cause of posttraumatic ARDS?
J Trauma 1993; 34:540 548
12. Pell AC, Christie J, Keating JF, et al: The
detection of fat embolism by transesophageal
echocardiography during reamed intramedullary nailing: A study of 24 patients with
femoral and tibial fractures. JBJS-B, 1995;
75:921923
13. Pape H-C, Dwenger A, Regel G, et al: Pulmonary damage due to intramedullary femoral
nailing in severe trauma in sheep: Is there an
effect from different nailing methods?
J Trauma 1992; 33:574 578
14. Hogevold HE, Lyberg T, Kierulf P, et al:
Generation of procoagulant and plasminogen
activator activities in peripheral blood monocytes after total hip replacement surgery.
Thromb Res 1991; 62:449 457
15. Jorgensen LN, Lind B, Hauch O, et al:
Thrombin-antithrombin III-complex and fibrin degradation products in plasma: Surgery and postoperative deep venous thrombosis. Thromb Res 1990; 59:69 76
16. Nast-Kolb D, Waydhas C, Gippner-Steppert
C, et al: Indicators of the posttraumatic inflammatory response correlate with organ
failure in patients with multiple injuries.
J Trauma 1997; 42:446 455
17. Pape H-C, Regel G, Tscherne H: Local and
systemic effects of fat embolization after intra-medullary reaming and its influence by
cofactors. Tech Orthop 1996; 11:213
18. Pape H-C, Regel G, Tscherne H: Controversies regarding early musculoskeletal management in the multiple trauma patient.
Curr Opin Crit Care 1996; 2:295303
19. Tyburski JG, Collinge JD, Wilson RF, et al:
Pulmonary contusions: Quantifying the lesions on chest x-ray films and the factors
affecting prognosis. J Trauma 1999; 46:5:
833 838
20. Baker SP, ONeill B, Haddon W, et al: The
injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974; 14:
187196
21. Bone RB, et al: Consensus conference, Am
College of Chest Physicians/Society of Critical Care Medicine (ACCP/SCCM) Crit Care
Med 1992; 20:864 873
22. Bernard GR, et al: Consensus conference on
ARDS. Am J Respir Crit Care Med 1994;
149:818 824
23. Roumen R, Redl H, Schlag G, et al: Inflammatory mediators in relation to the development of multiple organ failure in patients
after severe blunt trauma. Crit Care Med
1995; 23:474 480
24. Johansen I, Benumof JL: Methylmethacrylate: A myocardial depressant and peripheral
dilator. Anesthesiology 1979; 51:77 84
25. Meek RN, Woodruff B, Allardyce DB: Source
of fat macroglobules in fractures of the lower
extremity. J Trauma 1972; 12:432 434
26. Strecker W: Thromboxane: Cofactor of pulmonary disturbance in intramedullary nailing. Injury 1993; 24:68 72
27. Schluter B, Konig B, Bergmann U, et al:
Interleukin-6: A potential mediator of lethal
sepsis after major thermal traumaEvidence for increased IL-6 production by peripheral blood mononuclear cells. J Trauma
1991; 31:16631670
28. Castell JV, Geiger T, Gross V, et al: Plasma
clearance, organ distribution and target cells
of interleukin-6/hepatocyte stimulating factor in the rat. Eur J Biochem 1988; 177:
357363
29. Rabinovici R, Yue TL, Farhat M, et al: Platelet
activating factor and tumor necrosis factor
interactions in endotoxemic shock: Studies
with BN 50739, a novel PAF antagonist.
J Pharmacol Exp Ther 1990; 255:256 259
30. Rabinovici R, John R, Esser K, et al: Serum
tumor necrosis factor-alpha profile in
trauma patients. J Trauma 1993; 35:698 702
3447
31. Engelbarts I, Stephens S, Francot GJM, et al:
Evidence for different effects of soluble
TNF- receptors on various TN measurements in human biological fluids. Lancet
1991; 2:515518
32. Tan LR, Waxman K, Scannell G, et al:
Trauma causes early release of soluble receptors for tumor necrosis factor. J Trauma
1993; 34:634 647
33. Kwan HC: Role of fibrinolysis in disease processes. Semin Thromb Haemostas 1984; 10:
719
34. Dahl O, Aspelin T, Lyberg T: The role of bone
traumatization in the initiation of proximal
DVT during cemented hip replacement surgery in pigs. Blood Coagul Fibrinolysis 1995;
6:709 717
35. Enderson B, Chen JP, Robinson R: Fibrinolysis in multisystem trauma patients.
J Trauma 1991; 31:1240 1246
36. Gando S, Nakanishi Y, Tedo I: Cytokines and
plasminogen activator inhibitor-1 in posttrauma disseminated intravascular coagulation: Relationship to multiple organ dysfunction syndrome. Crit Care Med 1995; 23:
18351842
37. Pape H-C, Bartels M, Pohlemann T, et al:
Coagulatory response after femoral instrumentation after severe trauma in sheep.
J Trauma 1998; 45:720 728
3448
38. Wenda K, Ritter G, Degreif J, et al: Zur genese pulmonaler komplikationen nach
marknagelosteosynthesen. Unfallchirurg
1988; 91:432 437
39. Heim D, Regazzoni P, Tsakiris DA, et al:
Intramedullary nailing and pulmonary embolism: Does unreamed nailing prevent embolization? J Trauma 1995; 38:899 906
40. Gauldie J, Richards C, Harnish D, et al: Interferon 2/B-cell stimulatory factor type 2
shares identity with monocyte derived hepatocyte-stimulating factor and regulates the
major acute phase protein response in liver
cells. Proc Natl Acad Sci U S A 1987; 84:
721725
41. Damas P, Ledoux D, Nys M, et al: Cytokine
serum level during severe sepsis in human
IL-6 as a marker of severity. Ann Surg 1992;
215:356 362
42. Nijsten MWN, Hack CE, Helle M, et al: Interleukin-6 and its relation to the humoral immune response and clinical variables in
burned patients. Surgery 1991; 109:761767
43. Pape H-C, Remmers D, Grotz M, et al: Reticuloendothelial system activity and organ
failure in multiply injured patients. Arch
Surg 1999; 134:421 427
44. Pape H-C, Remmers D, Grotz M, et al: Levels
of antibodies to endotoxin and cytokine release in patients with severe trauma: Does
45.
46.
47.
48.
49.
50.
posttraumatic dysergy contribute to organ
failure? J Trauma 1999; 46:907912
Bone LB, Babikian G, Stegemann P: Femoral
canal reaming in the polytrauma patient
with chest injury. Clin Orthop Rel Res 1995;
318:9194
Bosse MJ, MacKenzie E, Riemer BL, et al:
Adult respiratory distress syndrome, pneumonia, and mortality following thoracic injury and a femoral fracture treated either
with intramedullary nailing with reaming or
with a plate. JBJS-A 1997; 79:799 809
Pape H-C, Regel G, Dwenger A, et al: Influences of different methods of intramedullary
femoral nailing on lung function in patients
with multiple trauma. J Trauma 1993; 35:
709 715
Pape H-C, Stalp M, Dahlweid M, et al: Optimal duration of primary surgery with regards
to a borderline situation in polytrauma patients. Unfallchirurg 1999; 102:861 869
Friedl HP, Stocker R, Czermack B, et al:
Primary fixation and delayed nailing of long
bone fractures in severe trauma. Tech
Orthop 1996; 11:59 66
Pape H-C, Meier R, Glinski S, et al: Pulmonary dysfunction following bilateral femoral
nailing: A case report. Int Care Med 1999;
25:547548
Crit Care Med 2000 Vol. 28, No. 10
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- (IMCI) Integrated Management of Childhood IllnessDokumen34 halaman(IMCI) Integrated Management of Childhood Illnessɹǝʍdןnos97% (34)
- Nonoperative Treatment of The Medial Malleolus in Bimalleolar and Trimalleolar Ankle Fractures, A Randomized Controlled TrialDokumen5 halamanNonoperative Treatment of The Medial Malleolus in Bimalleolar and Trimalleolar Ankle Fractures, A Randomized Controlled TrialDiego Cruces OrdoñezBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- 2017 Is Humidified Better Than Non-Humidified Low Flow Oxygen Therapy, A Systematic Review and Meta-AnalysisDokumen35 halaman2017 Is Humidified Better Than Non-Humidified Low Flow Oxygen Therapy, A Systematic Review and Meta-AnalysisDiego Cruces OrdoñezBelum ada peringkat
- Manual Therapy: Hiroshi Takasaki, Takeshi Iizawa, Toby Hall, Takuo Nakamura, Shouta KanekoDokumen6 halamanManual Therapy: Hiroshi Takasaki, Takeshi Iizawa, Toby Hall, Takuo Nakamura, Shouta KanekoDiego Cruces OrdoñezBelum ada peringkat
- Recruitment Maneuvers and PEEP TitrationDokumen17 halamanRecruitment Maneuvers and PEEP TitrationDiego Cruces OrdoñezBelum ada peringkat
- Neck Musculature Fatigue Affects Specific Frequency Bands of Postural Dynamics During Quiet StandingDokumen7 halamanNeck Musculature Fatigue Affects Specific Frequency Bands of Postural Dynamics During Quiet StandingDiego Cruces OrdoñezBelum ada peringkat
- A Comprehensive Review of Prone Position in ARDS PDFDokumen28 halamanA Comprehensive Review of Prone Position in ARDS PDFDiego Cruces OrdoñezBelum ada peringkat
- Neuromuscular Adaptation in Experimental and Clinical Neck Pain PDFDokumen7 halamanNeuromuscular Adaptation in Experimental and Clinical Neck Pain PDFDiego Cruces OrdoñezBelum ada peringkat
- The Role of Physiotherapy in The Prevention and Treatment of OsteoporosisDokumen16 halamanThe Role of Physiotherapy in The Prevention and Treatment of OsteoporosisDiego Cruces OrdoñezBelum ada peringkat
- Strength Versus Stability - Part 1 Concept and Terms PDFDokumen11 halamanStrength Versus Stability - Part 1 Concept and Terms PDFDiego Cruces OrdoñezBelum ada peringkat
- Drugs Name of Heterocyclic CompoundsDokumen4 halamanDrugs Name of Heterocyclic CompoundsNAZIM10728233% (6)
- Ayurveda PPT (1) - 1Dokumen91 halamanAyurveda PPT (1) - 1Sabir Kumar Sahu0% (1)
- StentsDokumen4 halamanStentsChitresh MotwaniBelum ada peringkat
- Rajiv Gandhi University of Health Sciences, Karnataka, BangaloreDokumen27 halamanRajiv Gandhi University of Health Sciences, Karnataka, BangaloreJyotiBelum ada peringkat
- Prediction of Pulmonary Embolism in The Emergency DepartmentDokumen10 halamanPrediction of Pulmonary Embolism in The Emergency DepartmenttechiemedicBelum ada peringkat
- INTELLECTUAL - REVOLUTION - THAT - DEFINES - SOCIETY - WPS PDF ConvertDokumen32 halamanINTELLECTUAL - REVOLUTION - THAT - DEFINES - SOCIETY - WPS PDF ConvertEloisa Karen MonatoBelum ada peringkat
- UNCC300 Assesment TAsk 2Dokumen2 halamanUNCC300 Assesment TAsk 2Spandan DahalBelum ada peringkat
- Swine Influenza, Also Called Pig Influenza, Swine Flu, Hog Flu and Pig Flu, Is An Infection by AnyDokumen13 halamanSwine Influenza, Also Called Pig Influenza, Swine Flu, Hog Flu and Pig Flu, Is An Infection by AnyKaran AgrawalBelum ada peringkat
- COVID Testing Labs 26042021Dokumen167 halamanCOVID Testing Labs 26042021suresh10526_71653021Belum ada peringkat
- Workplace Health Longterm Sickness Absence and Capability To Work PDFDokumen38 halamanWorkplace Health Longterm Sickness Absence and Capability To Work PDFFuzail AyazBelum ada peringkat
- The Science of SingingDokumen18 halamanThe Science of SingingK100% (2)
- A Giant Juvenile Fibroadenoma of BreastDokumen2 halamanA Giant Juvenile Fibroadenoma of BreastIOSRjournalBelum ada peringkat
- Laporan Bulanan Lb1: 0-7 HR Baru LDokumen20 halamanLaporan Bulanan Lb1: 0-7 HR Baru LOla SarlinaBelum ada peringkat
- Baxter (Flo-Gard 6201) Volumetric Infusion Pump Flow Rate Accuracy - Test Design and Performance VerificationDokumen21 halamanBaxter (Flo-Gard 6201) Volumetric Infusion Pump Flow Rate Accuracy - Test Design and Performance VerificationKousha TalebianBelum ada peringkat
- Pathophysiology On Cellulitis On Left Facial AreaDokumen9 halamanPathophysiology On Cellulitis On Left Facial AreaAdiBelum ada peringkat
- PGIMER Chandigarh Recruitment 2022 Notification Group A B C PostsDokumen36 halamanPGIMER Chandigarh Recruitment 2022 Notification Group A B C PostsGourav KadianBelum ada peringkat
- Modified Radical Mastectomy - 3B ABLOGDokumen45 halamanModified Radical Mastectomy - 3B ABLOGDafny CzarinaBelum ada peringkat
- Lower Gastrointestinal Series (Colonoscopy) : Nursing Skills Output (Nso)Dokumen3 halamanLower Gastrointestinal Series (Colonoscopy) : Nursing Skills Output (Nso)Grant Wynn ArnucoBelum ada peringkat
- Renal System and Its Disorders: Key PointsDokumen19 halamanRenal System and Its Disorders: Key PointsskBelum ada peringkat
- Use of Pallada in The Treatment of Allergic Conjunctivitis, Adenovirus Keratoconjunctivitis and KeratoconusDokumen4 halamanUse of Pallada in The Treatment of Allergic Conjunctivitis, Adenovirus Keratoconjunctivitis and KeratoconusCentral Asian StudiesBelum ada peringkat
- SEP. 2015 RECALLS MRCOG P2 DR HAMADA Aboromuh PDFDokumen95 halamanSEP. 2015 RECALLS MRCOG P2 DR HAMADA Aboromuh PDFuzairBelum ada peringkat
- Answer Key EXAM DRILL 1 - Community Health Nursing Nursing Practice Ii - CHN and Care of The Mother and ChildDokumen11 halamanAnswer Key EXAM DRILL 1 - Community Health Nursing Nursing Practice Ii - CHN and Care of The Mother and Childbetiful100% (5)
- ECHS Hosp Latest ListDokumen45 halamanECHS Hosp Latest Listyksingh25100% (1)
- (PDF) Diabetes Causes, Symptoms and TreatmentsDokumen1 halaman(PDF) Diabetes Causes, Symptoms and TreatmentsBakaro ShafiBelum ada peringkat
- Catalog Tracoe 2014 PDFDokumen94 halamanCatalog Tracoe 2014 PDFLiudmila RailescuBelum ada peringkat
- Regional Anesthesia in The Patient Receiving Antithrombotic or Thrombolytic TherapyDokumen64 halamanRegional Anesthesia in The Patient Receiving Antithrombotic or Thrombolytic TherapyAlejandro CespedesBelum ada peringkat
- Introduction To BioethicsDokumen33 halamanIntroduction To BioethicsReymart BolagaoBelum ada peringkat
- PDF Book UrduDokumen4 halamanPDF Book UrduMuhammad KamranBelum ada peringkat
- Nursing Care Plan For A Patient With SchizophreniaDokumen14 halamanNursing Care Plan For A Patient With SchizophreniaJerilee SoCute WattsBelum ada peringkat