Catatonia Farmacoterapia
Diunggah oleh
W Andrés S MedinaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Catatonia Farmacoterapia
Diunggah oleh
W Andrés S MedinaHak Cipta:
Format Tersedia
FEATURE ARTICLE
m Psychiatry. 20lO:17(4):41-47
The Pharmacotherapy of Catatonia
Brendan T. Carroll, MD, Joseph W.Y. Lee, MBBS, MRCPsych, FRANZCP, Francisco Appiani, MD,
and Christopher Thomas, PharmD, BCPP
ABSTRACT
FOCUS POINTS
Catatonia is an important clinical syndrome that occurs in affec-
Multiple pharmacologie agents have been used in the
tive, psychotic, autistic, developmental, and medical disorders. treatment ot catatonia,
The pharmacotherapy of catatonia is complex because of multiple The proposed pattiophysiology nt catatona involves gab-
aergic, dopaminergic. glutamatergic, and other neiiro-
and varied ttierapeutic agents. The proposed pathophysiology of
chemical systems.
catatonia includes: y-aminohutyric acid (GABA)/^ hypoactivity dopa- The primary treatments tor catatonia have mechanisms
mine-2 hypoactivity. glutamate W-methyl-o-aspartate hyperactivity. of action that involve one or more of these neurochemical
systems,
serotonin-2 hyperactivity. and choiinergic hyperactivity. The pharma-
The alternative pharmacologie treatments ot catatona are
cotherapy of catatonia includes henzodiazepines. CABA promoters. important when benzodiazepmes and electroconvulsive
certain anticonvulsants. glutamate inhibitors, and second-generation therapy are not ettective treatment options.
antipsychotics. The role of first-generation antipsychotics remains The application of pharmacologie treatment tor catatona
is illustrated in case vignettes.
unclear Catatonia. a treatable syndrome, occurs in a variety of psy-
chiatric, medical, and neurologic illnesses. Physicians may benefit
from learning about these pharmacologie treatment options. and is a constellation of symptoms reliably associated with
disturbance that Is functional, structural, neurochemical, or
neuropathologic in a circumscribed structural location or
INTRODUCTION neural circuit. The clinician is charged with the detection and
diagnosis of catatonia. Thus, when catatonia becomes the focus
The clinician should approach cataronia as a diagnosable oi treatment, there is an urgent need to explore the different
;iiid treatable disorder. One approach is that catatonia is a pharmacologie treatments. This heuristic approach may be
psychiatric disorder and the clinician should treat the primary helpfiil in many ca.ses where the clinician begins with treatment
psychiatric disorder.' However, another view is that, since cata- and works baekwards toward diagnosis.
tonia \s found in non-psychiatric medical disorders, it is a
neuropsychiatrie illness and treatment should focus on the
medical disorder' The authors of this article favor the concept
of catatonia as a neuropsychiatrie syndrome with an identified MECHANISMS OF CATATONIA
set of etiologies, core features, pathophysiology, and treatment There are multiple theories rq^arding the neuroehemical
response.* Catatonia constitutes a neurobiologie syndrome etiology for catatonia. This article provides a brief mechanistic
Or Carrol! is clinical assistant professor of Psychiatry 3t Ohio University College ot Ostopathie Medicine in Athens, arjd chief of Psychiatry Service at the Chlllicnthe Veteran's Aftairs (VA) Medical Center in Ohio,
Or I ee IS clinical associate pmfessoi al the University ct Western Australia m Perth. Or. Appian is assistant prnfessor ol Pharmacology at Universiriad de Buenos Aires. Facultad de Medicina, and Oirectai ot Ihe
Association tor the Study and Develogment of the Neumsciences m Buenos Aires. Afgentma Dr Thomas is clinical pharmacy specialist m Psychiatry at the Chillicothe VA Medical Center.
Oisnlosun;: Df Carroll is a consultant to Neurotepltc Malignant Syndrame tniormation Service; is on the speaker s bureaus ot AhbotI, AslraZeneca, Bnstol-Mycrs Squibb, Eli Lilly, Forest Laboratories, Pfi?er, and
tanssen. and leceives granl support from Ptizef. Or, Lee is consultant to EJi Lilly and Plizer. and is on the speaker s bureaus and receives grartt support tn3m Janssen-Cilag. Or. Appiani reports no attiliation mth
Of ttnancial interest m any organisation that ma/ pose a conflict of interest, Dr Thomas is on the speaker's bureau of AstraZeneca.
Please direct all correspondence tO: Brendan T Carroll, MO, Chief, Psychiatiy Service, MHCL, ChiKicothe VA Medical Center, 116A, 17273 State Route 104, Chillicothe, OH 45601, Tel 740-773-1141 i;7871:
Fax 740-772-7179; E-mail, btcartollI0cs.com.
Prtmary Psychiatry 41 AprtI 2010
B.T. Carroll, J.W.Y. Lee, F. Appiani, C. Thomas
overview of catatonia; a tnore cotnprehensive review of specific types. Patients who present in an acute psychiatric setting and
theories of catatonia can be found elsewhere.' In general, there fora follow-up appointment in an outpatient clinic may both
ate three major theories, naJiiely, dopaminc hypoactivity, y-aini- meet Diagnostic and Statistical Manual of Mental Disorders,
nobutyric acid {GABA) hypoactivity, and glutamate hyperactiv- Fourth Edition," criteria for the catatonia specifier. However,
ity,'' along with the two minor theories of serotonin hyperactivity there are differences in the level of functional impairment and
and cholinergic hyperactivity.'^ Dopamine (D) hypoactivity, the severity of the syndrome (Table I). This separation may
specifically at the Di receptor, is thought to be the predomi- help in selecting treatment for patients with catatonia.'
nate niechatiism that leads to catatonia. To flirther support the
hypoactive D-> receptor theory, several case reports exist that
demonstrate a relationship with high-potency typicaj antipsy- RATING SCALES FOR CATATONIA
chotics either causing or worsening catatonia. This phenomenon
is ioiown as neuroleptic-induced catatonia (NIC). The decrease Glinicians detect and diagnose catatonia with greater fre-
in activity at the Di receptor then causes an abundajit release quency with the use of a larger number of catatonic signs and
of glutamate, the major excitatory neurotransmitter, hence, the a rating scale for catatona.'" " Furthermore, the treatment of
physiologic attempt to increase dopamine activity via glutamate. caratonia is enhanced by the use of a rating scale handled by
Glutamate is known to regulating the catecholamine release and an experienced clinician with skill in administering the cho-
is directly involved in dopamine regulation. ' However, glutamate sen rating scale. Rating scales include: one by Rosebush and
is known to be excitotoxic, thereby, causing neuronal damage, colleagues,'- the Modified Rogers Scale,'* the Bush-Francis
and may produce symptoms similar to catatonia.'"' GABA, the Gatatonia Rating Scale,'' the Northoff Gatatonia Scale,''^
major inhibitory neurotransmirter in the central nervotis system, the Braunig Gatatonia Rating Scale,"' and the KANNER
has an inverse relationship wirh glutamate. In environments Gatatonia Rating Scalc.'^ Garroll and colleagues' provide a
with high glutamate, GABA acts ro shur down glutamate release. review of catatonia rating .scales. In North America, the Bush-
Therefore, to further support the high glutamate activity and Francis Gatatonia Rating Scale is used most frequently.''
hypodopamine receptor theory, drugs that potentiate GABA
(benzodiazepines) or act as GABA agonists (anticonvtilsants) will
have a benefit in treating catatonia. THE CATATONIC DILEMMA
These general neurochemicai theories are supported by
Gatatonic signs may appear or worsen with antip.sychotic
pharmacologie treatment because clinical studies of neuro-
pharmacotherapy."* This "catatonic dilemma" illustrates the
chemicai mechanisms are difficult to obtain in these patients.
role of dopamine blockers on the pathogenesis of catatonia.
These mechanisms will be reviewed further in the pharmaco-
NIG has been described with Hrsr-generation antipsychotics
therapy section of this article. Animal studies of catalepsy do
(FGAs) and, albeit less frequently, with second-generation
provide some information on the actions of pharmacologie
antipsychotics (SGAs). SGAs tend not to worsen catatonia
agents. However, there is no suitable model for catatonia in
and have been recommended. NIG may emerge during
humans. Electroconvulsive therapy has been a very important
pharmacologie treatment and can mimic acute or chronic
treatment for catatonia and also contributes to these neuro-
catatonia. Thus, the physician may need to obtain a history
chemicai theories.
Ftirthermore, catatonia is not a unitary syndrome and there
TABLE 1
may be subtypes that respond favorably to one type of medi-
cation. Gatatonia is probably a heterogeneous condition with ACUTE VS. CHRONIC CATATONIA
subtypes different in treatment responses and pathophysiol- Measure of moairment Acute Chronic
ogy. Therefore, multiple agents may be required to not only Catatonic signs Greater Fewer
treat acute catatonia, but maintain or prevent the reoccur-
Nutritional compromise More likely Less likely
rence of chronic catatonia.
Dehydration More likely Less likely
Autonomie instability More common Less common
TYPES OF CATATONIA Urgent status Inpatient Outpatient or residential
Gatatonia is derived from a term for "tension insanity" Medical complications More likely Less likely
by Kahlbaum and colleagues.*' Since this original descrip- Recent diagnostic procedures More likely Less likely
tion, additional signs have been observed and described by
Impairment in ADLs More severe Less severe
Dhossche and colleagues.^ Physicians working in different
settings may encounter different forms of catatonia. A heu- AOLs=activ!ties ot dailiy living.
ristic approach is to classify catatonia into acute and chronic Carroll BT. Lee JWY, Appiani F, Thomas C. Primary Psychiatry. Vol 17, No 4.200,
P^vchi^trv 42 April ?010
The Pharmacotherapy of Catatonia
of all mods administered and even toxicology for occult HGAs rate in chronic catatonia in schizophrenia with benzodiazx'pines
and SCiAs.''' This modetn "catatonic dilemma" must be con- was 8%, thus, a much lower response rate versus response in
sidered by the clinician in a case by case basis. acute catatonia. Response rates with amantadine, selegeline,
lithium, and SGAs occurred in nine of 13 (69%), yielding a
response rate similar to benzodiazepines in acute catatonia/'
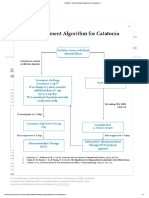
PHARMACOTHERAPY These diverse medications have been reported to help improve
catatonia ('lables 2-6; Figures 1-4). Ixirazepam and other
Carroll and colleagues-^" and Lee and Carroll'' reviewed GABA,\ promoters (ie, benzodiazepines, zolpideni) increase
several authoritative texts and review articles on the subject GABA activity as their mechanism of action. Anticoiivulsants
of catatonia response. They divided the drugs into their
may be helpful by increasing activity at GABA or modest anti-
known classes and identified their mechanism of action. They
gkitaminergic effects witb some reports of benefit from carbani-
also reviewed 49 cases that were rated with the Bush-Francis
azepine ;md valproic acid. In neuroleptic-induced catatonia an
Rating Scale as part of clinical care at a neuropsychiatrie
anticholinergic might be helpful, suggesting a role for the choHn-
institution between iyy5 and 2005/ Thirty-five patients
ergic system in catatonia. Clozapine and other SGAs have been
(66%) met the de.scription of schizophrenia with catatonic
reported to improve catatonia in psychosis, perhaps via a greater
features, l'en patients (19%) had catatonia due to a general
medical condition. Bipolar and unipolar mood disorders were "pass-though" of dopamine to the D? receptor. Perhaps the most
a minority (fout patients; 9%). Some improvement in catato- promising finding is that M methyl-D-aspa rtate antagonists may
nia and function occurred with medication treatment in 16 improve schizophrenia with catatonic featiLres.
of the 49 cases. This included: SGAs (two), clozapine (two),
lorazepam (iour), broinocriptine (one), memantine (adjunct;
six), and memantine (monotherapy; one).*" CASES
Meanwhile, Lee and CarrolH' reviewed treatments used in
71 episodes of catatonia (58 acute, 13 chronic) with schizo-
phrenia (according to the DSM-IV; most of them were seen in
Case 1
two psychiatric intensive care facilities respectively irom 1996 Ihe authors describe the case ot a 64-year-old female
lo 2002).' All met restrictive criteria \ox catatonia according to patient who came for psychiatric treatment accompanied
Rosebush and colleagues" and Lohr and Wisenewski.'' They by her son. According to her son's description, the patient
were first treated with benzodiazepines {oral lorazepam or became mute. She could not perform her usual activities, and
inrianiuscular clona/.epani). I hose who failed benzodiazepines spent [learly the whole day in bed with akinesia. During this
icceived other treatments for their catatonic symptoms. The time the patient lost 15 Ib and ate once a day and only if she
efficacy of benzodiazepines in acute catatonia in schizophre- was assisted. The patient had a history of two depressive epi-
nia was seen in 40 of 58 episodes (69%). [Respite the decent sodes that, according to clinical records, were mild and pro-
icsponse In acute catatonia, this response was not sustained and duced by family conflicts. She was diagnosed by her former
catatonia returned in the majority of patients. The response psychiatrist with dysthymia and was treated with vcnlafaxiiie
TABLE 2
TREATMENT OF SCHIZOPHRENIA ANO CATATONIC FEATURES'^
Use Rationale Benefits Risks
FGAs Often usedtor Sciizopirenia Controls positive sympfoms, Well-established and less The catatoriic dilemma Catatonia is
such as hallucinations and expensive difficult to distinguish from NMS and may
delusions worsen catatonic symptoms (NIC)
SGAs Beneficial in catatonia Low D^ blockade is less likely Some series suggest greater The metabolic syndrome and agranulocyto-
to worsen catatonia efficacy sis with clozapine
BZDs Lrazepam and other 62Ds are Can be added to FGAs or SGAs Safe, first line treatment fof Respiratory compromise, incoordination,
helpful in acute catatonia catatonia sedation, potential for abuse
ECI Beneficial in malignant catatonia Effective in catatona and Less risk of NMS, useful lor Concerns with anesthesia, informed con-
treatment refractory catato- sent and availability
nia, rapid onset of action
FGAs=first-gefieration antipsychotics; NMS=neuroleptic malignant syndrome; NIC=neuroleptic-induced catatonia; SGAs=second-generation a nti psychotic s ; D=dopamine;
BZDs=benzod3zepines; ECT=e!ectroconvulsive therapy,
Carroll BT, Lee JWY, Appiani F, Thomas C. Primary Psyctiiatry. Vol 17, No i. 2010,
imary Psychiatry 43 April 2010
B.T. Carroll. J.W.Y. Lee, F. Appiani, C. Thomas
75 mg/day with partial response. At this time she was also arms. Head computerized tomography scan showed an old
under psychotherapy treatment. She had one venlafaxine- small infarct in the subcortical zone of the riglit frontal lobe,
induced manic episode. the diagnosis of NIC was made. After rhe initial evaluation,
This catatonic syndrome developed 10 days after the patient risperidone was stopped. Treatment with lorazepam began at
was started with risperidone 3 mg/day. In the clinical examina- 2.5 mg/day gradually titrated to 2.5 mg Bll). After 48 hours oi
tion, the patient had immobility, she answered questions only this pharmacologie treatment the catatonic symptoms began to
with 'yes" or "no", and she had a marked delay of many sec- resolve. This was especially seen in an increase on verbal fluency
onds to answer. Physical examination revealed no fever, blood and feeding habits. After 2 weeks of treatment, the patient was
pressure ot 125/75 Hg mm, and cardiac frequency oi 85 beats almost without catatonic symptoms, and in the physical exami-
per minute. She had catalepsy and cogwheel rigidity in both nation she had mild cogwheel in hoch arms. She was started on
quetiapine 25 mg/day titrated to 150 mg/day in a month. This
drug was given to treat bipolar disorder. W i tti tliib regitnen or
TABLE 3
Ul/l/f AUT
OTHER TREATMENTS FOR CATATONIA
TABLE 5
Anti- Anti-
GABA glutamate glutamate
OTHER TREATMENTS FOR CATATONIA: DOPAMINERGIC
Medication DOtenc\ f BABA effects potency effects Anti-
rlillr
Valproic Acid Strong + GABAB-P Modest Cerebral DA glutamate Anti-glutamate
a s prtate Medication potency DA effects potency effects
- GABAB - T/0
Carbidopa/ Strong DA precursor None None (worsens
-- GABA oy levodopa psychosis)
GAD, synthesis.
release and Bfomocriptine Strong D^ agonist None None (worsens
transaminase psychosis)
inhibition Amantadine Modest -t- DA trans- Weak NMDA antagonism
Carbamazepine Modest + GABAg - P Modest Inhibition ot mission (non-competitive)
glutamate (worsens psychosis)
release Memantine None None Modest NMDA antagonism
Top ira mate Modest Potentiates Strong Inhibition ot (non-cmpetitive)
GABA AMPA recep- Seiegeline Modest -t-DA Weak Possible NMDA
tors (possible via MAO-B attenuation
NMDA attenu-
ation) DA=dopamine and D? receploi subtype; -(--mcrease, NMDA=/i(-niethyl-D-aspartate (ylu-
tamate receptor subtype); MAO-B=monamine o)(idase-8 enzyme.
GABA=Y-aminobutyric acid (A and B receptor subtype); +=increase: ---decrease;
P=pfomotof. T/O=turnyEf. GAD=v-amJno decarboxylase^ AMPA=amino-3-hydroxy-5 Carroll BT, Lee JWY, Appiani F, Thomas C. Primary Psychiatry. Vol l No i. 210.
methyl-4 isoazole (glutamate receptor); NMDA=A'-mettiyl-D-a s prtale (glutamate recep-
tor subtype).
TABLE 6
Carroll BT. Lee JWY, Appiani F, Thomas C, Primary Psychiatry. Vol 17. No 4. 2010. OTHER TREATMENTS FOR CATATONIA: SGAs
Anti-Glutamate
TABLE 4 Medication OABinding DA Effects Anti-5-HT Effects
OTHER TREATMENTS FOR CATATONIA Clozapine Loose 5-HT22A Unclear
Medication GABA GABA effects Anti- Anti- Ouetiapine Loose 5-HT2,, Uncleai
notenc}! glutamate glutamate
Olanzapine Loose 5-HT22A Unclear
potency effects
Risperidone Tight 5-HT2,, Unclear
Lorazepam Strong -1- GABAA - P None None
Ziprasidone Tight 5-HT22S Unclear
Zolpidem Strong + GABAA None None
- a subunit Ar i pip razle Tight with partial 5-HT2,i Unclear
pass through agonist
Memafitri ' None ' None Modest NMDA antag-
onism (non- Amisulpride Loose D^, D3 None Unclear
competitive) (low dose)
GABA=Y-aminobutync acid (A and B receptor subtype); -(-=incr8ase; -=decfease; SGAs=secofid-genefation antipsychotics; DA-dopamirte and 2, D3 and Oj receptor sub-
P=promotor; NMDA=A(-methyl-D-aspanate (glutamate receptor subtype). type; 5-HT;,A-serotiim receptor (5-HT? subtype).
CarrollBT, Lee JWY. Appiani F, Thomas C. Primary Psychiatry. M 17. No 4 2010. Garroll BT, Lee JWY. Appiani F. Thomas C. Primary Psychiatry. Vof 17. No 4. 2010.
Primary Psychiatry 44 April 2010
The PharTTiacotherapy of Catatonia
qiietiiipinc 150 mg/day and lorazepam 5 mg/day the patient acted with increased suspiciou.sness, auditory hallucinations,
ifniained aiyiiipu)m.itic Un 6 months until she decided to stop and mystical delusions. She refused to drink and eat and had
taking lorazepam. Immediately after lorazepam discontinua- episodes of impulsivity without provocation. Weight loss was
tioti the patient developed a clinical state ot mutism, akinesia evident. The patient had no prior history of psychiatric disor-
with a narked anxiety state. Lorazepam was administered again der. She lived with her husband and three sons.
and symptom.s resolved in hours. The diagnosis of this episode Laboratory studies were normal range except for a mild
wa.s catatonic symptoms due to benzodiazepine withdrawal. anemia with hemoglobin 9.2 g/dl and hematocrit 32.1 %.
After this episode the patient remained sthle and continued A slow intravenous dose of lorazepam 2 mg was initiated.
with lorazepam S mg/day and quctiapine I "^O mg/day, witliout After 20 minutes of lorazepam administration the patient
catatonic symptoms. Lithium 600 mg/day was added tor the started to give brief delayed responses, with perseveration,
ireatment of the bipolar disorder, with a favorable response. movement improvement, exhibiting facial gestures, and giv-
ing minimal response to external stimuli.
Case 2
A 31-year-old female was admitted to a general hospital FIGURE 3
with immobility, waxy flexibility, negativism, mutism, rigid- GABA GLUTAMATE HYPOTHESIS THREE
ity, and decreased blinking. Her husband had reported that
10 days prior to the admission her behavior changed, she
Glutamate
FIGURE 1
Beiizodtazepmes
GABA GLUTAMATE HYPOTHESIS ONE Zolpidem
Valproate
^ Memantine
H_
CarbamazepinE ^,,-^ Amantadme
lopiramate ^,,,-^'^t Topi ram ate
L Clozapine
According to this hypothesis, pharmacologie treatment tend to restore GABA-glutamate
imbalance, decreasing glutamate transmission or increasing GABA transmission.
Decrease of dopaminergic transmission may act indireclly, increasing GABA-glutamate
In non-catatonic brain there is an equilibrium between GABA and glutimate concentrations. imbalance.
GABA-y-ammobutyric acid: CNS-central nervous system. GABA-f-aminobutyric acid; CNS=ceniral nervous system.
Carroll BT, Lee JWY, Appiani F. Thomas C, Primary Ps^iiiatiy. Vol 17, No 4.2010. Caffoll BT. Lee IWY. Appiani F, Thomas C. Primary Psychiatry. Vol 17, No 4. 2010.
FIGURE 2 FIGURE 4
GABA GLUTAMATE HYPOTHESIS TWO THE GABAA-GABAB CATATONIA HYPOTHESIS
In 3 catatonic bfain, the equilibfium between GA6A and glutamate is broken and there is According to this hypothesis, ttie GABA^-GABAB imbdlance Lould be restored by agonists of GABA^
a relative decrease of gabaergic transmission and a relative increase ot glutamate. receptor like lorazepam and zolpidem. or exacerbated y GABAu antagonists like bacioferi.
GABA-Y-aniinobu(yfic acid; CNS=central nervous system, GABA^-ammobutyric acid; CNS=central nervous system,
Carroll BT. Lee JWY. Appiani F, Thomas C. Primary Psychiatry. Vol 17, No 4. 2010. Carfoll BT. Lee JWY, Appiani F. Thomas C. Primary Psychiatry. Vol 17, No 4. 2010,
'rimary Psychiatry 45 April 2010
The Pharmacotherapy of Catatonia
12. Rosehusfi PI, Majurek MF Catatona re-awakening to a forgotten disorder. MovOisord. 1999:M(3)i395-397.
REFERENCES 13. LundCE.MortimerAM, Rogers D,McKenna PI Motor, voiilional and behavioural disorders m schizophre-
1. Abrams R, Taylor MA. Catatona A prospective clinical study Aich Gen Psychiatry. 1975;33(5);579'581. nia. I. flsse5smenl using ttie Modified Rogers Scale. Br I Psychiatry. 1991:158.323-32.333-336.
2. Ahmed I, Fu|ii D, eds. The Spectrum of Psychotic Disorders. Nembialogy: Etiology S Pethogenesis.fiefi 14. Bush G, Finh M. PetriQes G, Dowling F. Francis A Catatonia. I. Rating scale and standardized examina-
yorh, NY: Cambridp University Press; 2007 tion Ada Psychiafr Scand. 1996:93(21:129-136.
3. Barnes MP, Saunders M, Walls TJ, Sauners I, Kirk Cft, The syndrome of KafI Ludwig Kahfbaum, J Ueuio! 15. Northoff G, Koch A, Wenke J. el ai. Catatona as a psychomotor syndrome' a latmg scale and extrpyra-
Neurosiirg Psychiatry 1986;49[9h991-996. midal motor symptoms, lifov Disar. 1999;I4(3) 404-416.
4 Northnff G. What catatonia can tell us about "top-down madulatior" a neuropsychiatrie hypothesis. la. Brunig P, Krger S, Shugar G. HOffier I. Burner I. The catatonia rating scale l-development. teliability
Behav Brain Sei- 2002:25(51-555-577. and use. ComprPsychiatry. 2DDD:ill(21147-15S.
5. Yeh AW, Lee IW, Cheng TC, Wen JK. Chen WH, Clorapme mthdrawa) catatonia associated with cholinefEic 17. Carroll BT, Kirlihartft,Ahu|a N, et al. Katatonia a new conceolual understanding of catatona and a new
and seretonefgic rebound hyperactivity: a case report Clm Neuwptiamacol. 2DD4;27(5);216-218. rating scale. Psychiatry (Edgemontl. 2DD8:5(12):42-50.
6. Kahlbaum KL: Leui) Y, Ptidon T. trans. Catatiiia Baltimore. MD lohns Hopkins University Press: 1973. 18. Brenner I. RtieubanWJ The catatonic dilemma Am J Acta Psychiatiy 1978;135(1D1:1242-1243
7. Dhossche DM. Wilson C, Wachtel LE. Catatonia in childhood and adolescence: implications foi the 19. Lee JW Ne uro le ptic-induced catatona: clinical presentation, response to benzodiazepines. and lelation-
DSM-5. Primary Psychiatry. ?010,17(4):35-39 ship to neuroleptic malignant syndrome, yC/in Psycttopharmacol. 20!0,3Dtll:3-lP.
8. Diagnostic and Statistical Manual of tienta! Disorders. 4th ed. Washinton, DC American Psychiatric 2D. Carroli BT, Cairoll TD, Lee JW, et al. Why are some medications effective against catatonia? tnt I
Association: 1994 Neiiropsychopharmacalogy 2QQ6:9(suppl !1:S253.
9. llngvari GS, Chiu HF. Chow LY, Lau BS, Tang WK Lorazepam lor chronic catatona: a randomized, dautile- 21. Lee M , Cafroll BT Amantadine in the treatment of cbronic catatonic schizophren i a Int J
blind, placebo-controlled cross-ouer study Psychopharmacalogy (Berl). l999;142l4):393-398. tempsychopharmacology. 206:9lsuppl 11:S27O
ID. van der Keijen F. Turnier S, Arts N. Hoogendoorn M, Katin R, Vethoeven W. CatatoniS: disappeared or 22. Rosebush Pi. Hiidebrand AM, Furiong BG Mazurek MR Catatonic syndrome m a general psychiatric popula-
tion: frequency, clinical presentation, and response to lorazepam. J Ctiri Psychiatry. 1990.51 9j:357-362.
under-diagnosed' Psyctiopathology. 2005:38(11:3-8
23. Lohr IB, Wisenewski AA. Movement Disorders A Neuropsychiatrie Approaett. New York, NY. Guillord
11. Slompe T. Ortwein-Stvoboda G. Ritter K, Schanda H, Friedmans A. Are we witnessing the disappearance Press: 1987.
of calatonic schizophrenia? CmprPsyc/iJ3/f>'20D2:43(3 16M74.
Now Available @ www.primarypsychiatry.com
An Expert Panel Review of Clinical Challenges
in Primary Care and Psychiatry
Recognition and Treatment Strategies for Bipolar
Disorder Across the Life Cycle
j Authors: Joseph F. Goldberg, MD CMEP
Charles L Bowden, MD
^^^ Claudia Baldassano, MD
Noreen Reilly-Harrington, PhD
Funding for ttiis activity has been provided by educational grants from Bristol-Myers Squibb and Pfizer.
Primary Psychiatry 47 April 2010
The Pharmacotherapy of Catatonia
REFERENCES 1?. Rosebush PL Hazurek MF. Cataloraa: re-awakening ro a tcrgctteti disorder MmDisan!. 1999: L4(3):395-397
13. Lund CE, Mortimer AM. Rogers D. McKenna PI. Motor, volitional and behavioural disoiders m scfiwophre-
1. Abfams R, Taylot MA Catatona A prospective clinical sludy. Arch Gen Psychiatry. 1976;33(5):579-58I. nia. I Assessment using the Modified Rogers Scale Br J Psychiatry. 1991:158.323-327.333-336.
2. Ahmed I, FLI|M 0, eds. It)e Spectrum ol Psyct!olic Disorders. Nmotiiolm Etiology & Pattiogenesis. New 14. Bush G. Fink M. Petrides G, Dcwiing F. Francis A. Catatona I. Rating scale and standafdiied Kamma-
York, KY Cambridge Umuersily Pressa 2007 tion. Acta Psychiatr Scand. 1996:93(2). 129-136.
3. Barnes MP, Saiiniters M Walls IJ, Saunders I, Kirk CA. fhe syndrome ot Karl Ludwtg Kshlbaum. I Neuroi 15. fiarthoff G, Kacti A, Wenke I, et at. Catatona as a psychomotor syndrome, a rating scale and oxfipyra-
timirosurg Psychialiy 19a6,49(9).991-996. midal motor symptoms hovDmrr. 1999:14(3):4Q4-416,
'I Northoff G. What catatona can tell us about "tap-dawn maduiation": a neuropsychiatrie hypothesis. IB. Sraunig P. Krger S, Shugar G, Hffler I. Bmei I. The catatona rating scale l--development. reliability
M t o S 2O225(5)555577 and use. ConiptPsychiatry. 2000:4I(2).147-158.
Ypti AW, l.ee M, Cheng TC. Wen )K, Chen WH. Cloiapine withdrawal catatonia associated with cholinergic 17. Carroll BT. Kirkhad R, Ahuja N. et al. Katatonia: a new conceptual understanding of catatona and a new
,ird serotoneigic reboimd hypeiactiuity a case report ClmNeuraptiarmacot. 200i.27h).2le-2\. rating scale. Psyctiiatry tEdgemont) 208:5(12):42-50.
Kahlbaum KL, Levii Y, Pndon f. tars. Catatona. Bait/more, MD. Johns Hophins University Press; 1973. IB. Brenner I, Rheuban WJ The catatonc dilemma. Am J Acta Psychiatry 1978:135(10). 242-1243.
Dhosshe DM. Wilson C. Wachtel lE. Catatona m childhood and adolescence: implications for the 19. LeelW. Neuroleplic-mduijed catatona: cliiiical presentation, response to ben zod ta repines, and relation-
DSM-S Primary Psyvfiistiy. 2010;l/(4).35-39. ship to neuroleptic malignant syndrome, JClin Psychophaimacol. 2l0;30(l)i3-10.
Diagnostic and Statistical Manual of Mental Oisorders. 4th e<S. Washinton. DC: American Psychiatric 20. Carroll BT. Carroll TD, lee JW. el al. Why are some medications elfective against catatonia' Int J
Association, 1994 Neuropsychopharmacology. 2006:9(siippI 1)-S253,
llngvaii GS, Chiu HF. Chaw LY. Lau BS. Tang WK Lorazepam lar chronic catatonia a randomized, dauble- 21. Lee JW, Carroll BT. Amantadme in the treatment of chronic catatonic schiiophtenia. Int J
lilind. placebp-controlled cnDss over study. Psychopharmacology Berll 1999;!42(4):393-398. tieuropsychopharmacotogy. 2006:9(Suppl 1):S27O.
van der Heijden F, Tuimer S. Arts N, Hoogendoorn M. Kahn R. Verhven W. Catatona: disappeared 0( 22. Rosebush PI, Hildebrand AM, Furlcng BG, Mazurek MF. Catatonic syndrome in a gerteral psychiatric popula-
imder-diagnpsed? hyclioeattiology 2005:38(11:3-8. tion: frequency, clinical presentatiun, and response to lorazepam J Ctm Psychiatry. 199l):!)l(9)3Si-3G2
Stompe T, Orlwem-Swaoda G. Ritter K, Schanda H. Friedmann A. Are we wlfnessmg ttie disappeafance 23 Lohr JS, Wisenewsht AA. Movement Oisotders: A tieumsychiatric Approacti. New York, NY: Guilford
f calatpnicschiiophrenia? CmprPsychiatry 2002.43(3) 167-1/4. Press: 1987.
Now Available at www.DrimarvDsvchiatrv.com
ONLINE INTERACTIVE CASE STUDIES
A CLINICAL CASE DISCUSSION OF CHALLENGES IN PRIMARY CARE AND PSYCHIATRY
Fibromyalgia FACTS: Foundations for
Assessment, Care, and Treatment Strategies
Philip J. Mease, MD. Roland Staud, MO. and David A. Williams PhD
This activity is designed to meet the continuing eULtionai needs of
CME
.75
primary care physicians and psychiatrists
who care for patients with fibromyaigia.
The Mount Sinai School of Medicine designates this interactive online activity for a maximum of
0.75 AMA PRA Category I Credits. The Mount Sinai School of Medicine is accredited by the
Accreditation Council for Continuing Medical Education to provide continuing
medical education for physicians.
This activity is supported by an educational grant from Pfizer Inc.
Primary Psychiatry 47 April 2010
Copyright of Primary Psychiatry is the property of MBL Communications and its content may not be copied or
emailed to multiple sites or posted to a listserv without the copyright holder's express written permission.
However, users may print, download, or email articles for individual use.
Anda mungkin juga menyukai
- Catatonia - Pathophysiology, Diagnosis and ManagementDokumen17 halamanCatatonia - Pathophysiology, Diagnosis and ManagementFahrunnisa NurdinBelum ada peringkat
- Psycho P HarmDokumen84 halamanPsycho P HarmEliBelum ada peringkat
- AkathisiaDokumen4 halamanAkathisiaRindayu Julianti NurmanBelum ada peringkat
- Apt Aka 2015Dokumen3 halamanApt Aka 2015dzakiyah nurul israBelum ada peringkat
- Pe 2 3 36Dokumen6 halamanPe 2 3 36Oslo SaputraBelum ada peringkat
- Anest Implication of PsikoaktifDokumen5 halamanAnest Implication of PsikoaktifjilieBelum ada peringkat
- ParkinsonDokumen9 halamanParkinsonSOCIETE S.T.HBelum ada peringkat
- The Subjective Effects of Psychedelics May Not Be Necessary For Their Enduring Therapeutic EffectsDokumen5 halamanThe Subjective Effects of Psychedelics May Not Be Necessary For Their Enduring Therapeutic EffectsAnka StBelum ada peringkat
- Psychedelic Medicine - A Re-Emerging Therapeutic ParadigmDokumen6 halamanPsychedelic Medicine - A Re-Emerging Therapeutic ParadigmIago LôboBelum ada peringkat
- Geddes2013 PDFDokumen11 halamanGeddes2013 PDFalfredoibcBelum ada peringkat
- Trends in Anaesthesia and Critical Care: Jamie Sleigh, Martyn Harvey, Logan Voss, Bill DennyDokumen6 halamanTrends in Anaesthesia and Critical Care: Jamie Sleigh, Martyn Harvey, Logan Voss, Bill DennyAnonymous ORleRrBelum ada peringkat
- Advances in The PharmacologicalDokumen12 halamanAdvances in The PharmacologicalpaijosusenoBelum ada peringkat
- Tourette 1Dokumen8 halamanTourette 1Meli FernándezBelum ada peringkat
- Crow Et Al-2009-International Journal of Eating DisordersDokumen8 halamanCrow Et Al-2009-International Journal of Eating DisordersRosarioBelum ada peringkat
- Treatment of Mania, Mixed State, and Rapid CyclingDokumen9 halamanTreatment of Mania, Mixed State, and Rapid CyclingFernando PerezBelum ada peringkat
- BMJ 334 7595 CR 00686Dokumen10 halamanBMJ 334 7595 CR 00686samiratumananBelum ada peringkat
- The Neurobiology of Addictive DisordersDokumen8 halamanThe Neurobiology of Addictive DisordersDee DeeBelum ada peringkat
- Dic 212257Dokumen10 halamanDic 212257Agustina ZairidaBelum ada peringkat
- The Detection and Measurement of Catatonia: (Review)Dokumen5 halamanThe Detection and Measurement of Catatonia: (Review)Imon PaulBelum ada peringkat
- N-Acetylcysteine in The Treatment of Psychiatric Disorders: Current Status and Future ProspectsDokumen51 halamanN-Acetylcysteine in The Treatment of Psychiatric Disorders: Current Status and Future ProspectsRavennaBelum ada peringkat
- Schizophrenia: Recent Advances and Future Hopes: by Ahmad Al-Dabbas Resident in PsychiatryDokumen25 halamanSchizophrenia: Recent Advances and Future Hopes: by Ahmad Al-Dabbas Resident in PsychiatryAhmad DabbasBelum ada peringkat
- PsychologyDokumen7 halamanPsychologyHarish KumarBelum ada peringkat
- Dopamine Theory Considerations in SchizophreniaDokumen14 halamanDopamine Theory Considerations in SchizophreniaSantos Justine PBelum ada peringkat
- Fphar 12 604040Dokumen28 halamanFphar 12 604040biblioteka1.mzlBelum ada peringkat
- AKATHASIADokumen7 halamanAKATHASIAWanda AprilliaBelum ada peringkat
- NIH Public Access: Effects of Ketamine in Treatment-Refractory Obsessive-Compulsive DisorderDokumen13 halamanNIH Public Access: Effects of Ketamine in Treatment-Refractory Obsessive-Compulsive DisordermazsamBelum ada peringkat
- Current Pharmacological and Non Pharmacological Treatments For Obsessive-Compulsive DisorderDokumen14 halamanCurrent Pharmacological and Non Pharmacological Treatments For Obsessive-Compulsive DisorderKelvin PangestuBelum ada peringkat
- Movement Disorders in Catatonia: Subhashie Wijemanne, Joseph JankovicDokumen9 halamanMovement Disorders in Catatonia: Subhashie Wijemanne, Joseph JankovicTri Santi GhozaliBelum ada peringkat
- Emergency Presentations of MDDokumen10 halamanEmergency Presentations of MDGustavo PestanaBelum ada peringkat
- AnticonvulsantsPsychosisReview CITROME JCPVisuals2001Dokumen10 halamanAnticonvulsantsPsychosisReview CITROME JCPVisuals2001Leslie CitromeBelum ada peringkat
- The Many Varieties of Catatonia: Max Fink Michael A. TaylorDokumen7 halamanThe Many Varieties of Catatonia: Max Fink Michael A. TaylorRoy FloresBelum ada peringkat
- Kleptomania After Head Trauma: Two Case Reports and Combination Treatment StrategiesDokumen5 halamanKleptomania After Head Trauma: Two Case Reports and Combination Treatment StrategiesChloe AnnBelum ada peringkat
- Catatonia: FeaturesDokumen6 halamanCatatonia: FeaturesfirehuBelum ada peringkat
- Clincal Practice Guidelines For ECT IJP-23Dokumen26 halamanClincal Practice Guidelines For ECT IJP-23JagadishaThirthalliBelum ada peringkat
- How Do Psychoactive Drugs WorkDokumen1 halamanHow Do Psychoactive Drugs WorkErasmus CudjoeBelum ada peringkat
- Current Approaches and New Developments in The Pharmacological Management of Tourette SyndromeDokumen13 halamanCurrent Approaches and New Developments in The Pharmacological Management of Tourette SyndromedorinatcaciBelum ada peringkat
- Zhang Revision Efectividad y Efectos SecundariosDokumen40 halamanZhang Revision Efectividad y Efectos SecundariosJAIME CARMONA huertaBelum ada peringkat
- Antipsychotic Polypharmacy For The Management of SchizophreniaDokumen12 halamanAntipsychotic Polypharmacy For The Management of SchizophreniaAlondra CastilloBelum ada peringkat
- Psych 3Dokumen2 halamanPsych 3Jacquelyn HasiandaBelum ada peringkat
- Akathisia After Chronic Usage of Synthetic CathinonesDokumen7 halamanAkathisia After Chronic Usage of Synthetic CathinonesAram SBelum ada peringkat
- Ijms 23 08493Dokumen17 halamanIjms 23 08493Angieda SoepartoBelum ada peringkat
- Introduction To Psychedelic Neuroscience. Review 2018Dokumen23 halamanIntroduction To Psychedelic Neuroscience. Review 2018Luis Henrique SalesBelum ada peringkat
- Case Report On Antipsychotic Induced Catatonia in An Incarcerated PatientDokumen7 halamanCase Report On Antipsychotic Induced Catatonia in An Incarcerated Patientazadparis66Belum ada peringkat
- Revision Antipsicoticos Alteraciones Metabolicas OJO Imagenes 2019Dokumen10 halamanRevision Antipsicoticos Alteraciones Metabolicas OJO Imagenes 2019siralkBelum ada peringkat
- Complex Combination Pharmacotherapy For Bipolar Disorder: Knowing When Less Is More or More Is BetterDokumen14 halamanComplex Combination Pharmacotherapy For Bipolar Disorder: Knowing When Less Is More or More Is Bettermarc_2377Belum ada peringkat
- Approach Considerations: Nita V Bhatt, MD, MPH Clinical Instructor, Resident Physician, Department ofDokumen7 halamanApproach Considerations: Nita V Bhatt, MD, MPH Clinical Instructor, Resident Physician, Department ofHiLmy ZakiyahBelum ada peringkat
- Quetiapine or Haloperidol As Monotherapy For Bipolar Mania A 12week Doubleblind Randomised Placebo Controlled Trial - Europ Neuropsych 2005Dokumen13 halamanQuetiapine or Haloperidol As Monotherapy For Bipolar Mania A 12week Doubleblind Randomised Placebo Controlled Trial - Europ Neuropsych 2005Pedro GargoloffBelum ada peringkat
- Piis0166223611001962 PDFDokumen11 halamanPiis0166223611001962 PDFmaghfiraniBelum ada peringkat
- Neurobiologia de La Abstinencia de OpioidesDokumen9 halamanNeurobiologia de La Abstinencia de OpioidesWidad LeivaBelum ada peringkat
- Case StudyDokumen15 halamanCase Studyapi-589548099Belum ada peringkat
- C102 1461-1474 PDFDokumen14 halamanC102 1461-1474 PDFstein godoy pachecoBelum ada peringkat
- Catatonia Revived. A Unique Syndrome UpdatedDokumen10 halamanCatatonia Revived. A Unique Syndrome UpdatedElisa PavezBelum ada peringkat
- From Apathy To Addiction Insights From Neurology and PsychiatryDokumen13 halamanFrom Apathy To Addiction Insights From Neurology and PsychiatryAlane SilveiraBelum ada peringkat
- Anticonvulsivantes e Antipsicóticos No Tratamento Do Transtorno BipolarDokumen7 halamanAnticonvulsivantes e Antipsicóticos No Tratamento Do Transtorno BipolarAzerax PLAYBelum ada peringkat
- Preclinical and Clinical Evidence of Therapeutic Agents For Paclitaxel Induced Peripheral NeuropathyDokumen29 halamanPreclinical and Clinical Evidence of Therapeutic Agents For Paclitaxel Induced Peripheral NeuropathyMahmoud gharibBelum ada peringkat
- The Diagnosis and Treatment of CatatoniaDokumen4 halamanThe Diagnosis and Treatment of Catatonia崔雍建Belum ada peringkat
- Quetiapine Doe Primary Insomnia Consider The RiskDokumen9 halamanQuetiapine Doe Primary Insomnia Consider The RiskFlorence Matthew T BesaresBelum ada peringkat
- Serotonin and Beyond: Therapeutics For Major Depression: ReviewDokumen7 halamanSerotonin and Beyond: Therapeutics For Major Depression: ReviewmarielaBelum ada peringkat
- AkathisiaDokumen5 halamanAkathisiaRindayu Julianti NurmanBelum ada peringkat
- Pedophilia JAMA 2002 Review TherapyDokumen8 halamanPedophilia JAMA 2002 Review TherapyW Andrés S MedinaBelum ada peringkat
- Carel-Phenomenology and PatientsDokumen18 halamanCarel-Phenomenology and PatientsW Andrés S MedinaBelum ada peringkat
- The Icarus Project: A Counter Narrative For Psychic DiversityDokumen15 halamanThe Icarus Project: A Counter Narrative For Psychic DiversityW Andrés S MedinaBelum ada peringkat
- Occasional Review: Penis Captivus-Did Occur?Dokumen2 halamanOccasional Review: Penis Captivus-Did Occur?W Andrés S MedinaBelum ada peringkat
- Catatonía HistoriaDokumen48 halamanCatatonía HistoriaW Andrés S MedinaBelum ada peringkat
- Antimicrobials and AstringentsDokumen52 halamanAntimicrobials and AstringentsApril Mergelle LapuzBelum ada peringkat
- Abdullahi V Pfizer PaperDokumen2 halamanAbdullahi V Pfizer PaperTeam2KissBelum ada peringkat
- Drug Guideline Title: Sodium Bicarbonate: SummaryDokumen4 halamanDrug Guideline Title: Sodium Bicarbonate: SummaryLoreine Jane ClaritoBelum ada peringkat
- Vastarel MRDokumen1 halamanVastarel MRianecunar100% (2)
- Ranbaxy Dissertation June 2010Dokumen40 halamanRanbaxy Dissertation June 2010NabinSundar NayakBelum ada peringkat
- New Zealand Healthcare Pharmacists' Association Compounding Nutrition & Oncology SIGDokumen31 halamanNew Zealand Healthcare Pharmacists' Association Compounding Nutrition & Oncology SIGcleanroom100% (1)
- Edibles List Magazine Issue 38 Featuring Montel WilliamsDokumen35 halamanEdibles List Magazine Issue 38 Featuring Montel WilliamsEdibles MagazineBelum ada peringkat
- Bin Card Coc Level 4Dokumen19 halamanBin Card Coc Level 4Kaleb Tilahun100% (1)
- Dirhea and IBSDokumen6 halamanDirhea and IBSDavid HosamBelum ada peringkat
- ICH GuidelinesDokumen35 halamanICH GuidelinesMounica Bollu50% (4)
- The 6 Most Effective Diarrhea RemediesDokumen6 halamanThe 6 Most Effective Diarrhea RemediesCatarina Baccay CauilanBelum ada peringkat
- Stock SekarangDokumen26 halamanStock SekarangNita FitriBelum ada peringkat
- Ich GuidelinesDokumen6 halamanIch GuidelinesVijay RavindranathBelum ada peringkat
- Drugs and Doping in SportDokumen39 halamanDrugs and Doping in SportAbhijit Sharma100% (1)
- Metabolism, Pharmacokinetics and Toxicity of Functional GroupsDokumen545 halamanMetabolism, Pharmacokinetics and Toxicity of Functional GroupsDenisa Nițu100% (1)
- Berno 19032019Dokumen70 halamanBerno 19032019Antocsm CisagaBelum ada peringkat
- Self Assessment Toolkit 3RD EDITION - DR Ramesh Babu, ErodeDokumen47 halamanSelf Assessment Toolkit 3RD EDITION - DR Ramesh Babu, ErodeRamesh Babu Balasubramaniam100% (1)
- Manual MesoterapiaDokumen95 halamanManual MesoterapiaDiana Mesquita100% (5)
- Methylprednisolone AlphapharmDokumen5 halamanMethylprednisolone AlphapharmMarthin TheservantBelum ada peringkat
- Ats SorowakoDokumen12 halamanAts SorowakoFirmanBelum ada peringkat
- HyphemaDokumen24 halamanHyphemaKaisun TeoBelum ada peringkat
- Integrase Inhibitor RaltegravirDokumen15 halamanIntegrase Inhibitor RaltegravirNovi SilitongaBelum ada peringkat
- Drugs in Neurology - OXFORD 2017Dokumen677 halamanDrugs in Neurology - OXFORD 2017athenea89100% (1)
- Dinesh Dhumal Formatted CVDokumen9 halamanDinesh Dhumal Formatted CVManoharBelum ada peringkat
- Remdesivir Distributor ListDokumen15 halamanRemdesivir Distributor Listbasit.000Belum ada peringkat
- Antimicrobial Stewardship Manual of Procedures For Hospitals 2016 v2Dokumen82 halamanAntimicrobial Stewardship Manual of Procedures For Hospitals 2016 v2kBelum ada peringkat
- Ratiu Ileana Andreea enDokumen48 halamanRatiu Ileana Andreea enAura MateiuBelum ada peringkat
- Administering An Intramuscular InjectionDokumen3 halamanAdministering An Intramuscular Injectionapi-26570979100% (4)
- Overview of Randomized Controlled Trials: Review ArticleDokumen7 halamanOverview of Randomized Controlled Trials: Review ArticleCut Sinta BeliaBelum ada peringkat
- Census August 14 - August 15, 2020Dokumen6 halamanCensus August 14 - August 15, 2020Patrick JohnBelum ada peringkat