Risk Factors of Surgical Site Infection at The Regional and Teaching Hospital Center of Borgou (Benin)
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Risk Factors of Surgical Site Infection at The Regional and Teaching Hospital Center of Borgou (Benin)
Hak Cipta:
Format Tersedia
Int J Clin and Biomed Res. 2017;3(1):01-04.
Journal homepage: www.ijcbr.com
Research article
RISK FACTORS OF SURGICAL SITE INFECTION AT THE REGIONAL AND TEACHING
HOSPITAL CENTER OF BORGOU (BENIN)
HODONOU M. ADRIEN1, ALLOD S ALEXANDRE1, TOBOM S ROMARIC1,3, HOUNKPONOU-AHOUINGNAN FANNY2,
FATIGBA O HOLDEN1, TAMOU SAMBO BIO1, MENSAH AD EMILE1, BANKOLE CHRISTELLE HE 3, ATAKPA FELIX4, MEHINTO K. DELPHIN5
AUTHOR DETAILS ABSTRACT
Received: 2nd Jan 2017 Introduction: The reduction of the SSI rate requires knowledge of its risk
Revised: 10th Jan 2017 factors. Objective: To analyze the risk factors of SSI occurrence at CHD-B
Accepted: 12th Jan 2017 Methods: Prospective, descriptive and analytical study involving 603 patients
undergoing general surgery (218) and obstetrics and gynecology (385) from
Author details: 1stJanuary to 31st July 2013. Results: 44 patients have developed SSI
1
Department of surgery and specialities, (7.3%). The SSI frequency was 12.8% in general surgery and 4.2% in
2
Department of mother and child, Faculty of gynecology-obstetrics (p significant). The mean age of patients developing SSI
medicine, University of Parakou, 3Saint Jean de was 30.7 15.8 years with a minimum and maximum 5 months and 70 years,
Dieu Hospital Center of Tanguieta, 4Department respectively; and for general surgery patients, there were 23 men and 5
of pharmacy, Regional and Teaching Hospital women (p not significant). The presence of preoperative infectious spot at
Center of Borgou, 5Department of surgery and admission (P = 0.003), the preoperative shaving of the site to be incised (p =
0.000), the ASA score (p = 0.000), the surgery contamination class (p = 0.000),
specialities, Faculty of Health Sciences,
and the NNIS score (p = 0.000) were all significantly related to SSI occurrence.
University of Abomey- Calavi.
Considering all these factors, the NNIS score 2 remained the predictive tool
Corresponding author:
by multiplying by 3.4 the risk of SSI occurrence. Conclusion: NNIS score is the
Hodonou M. Adrien best SSI prediction tool at CHD-B.
MD General surgery.
e-mail: hodasm98@gmail.com. KEYWORDS: Surgical site infection; Risk factor; NNIS score.
INTRODUCTION for this study. Since the study was observational, it was not
necessary to obtain the agreement of an ethical committee.
Despite advances in surgical technique, antibiotics and recent
therapeutic measures, infection is still a major problem in Sampling method and sample size: Sampling was consecutive
surgery [1]. Surgical site infections (SSI) are associated with and exhaustive. This allowed us to retain 603 patients.
high mortality and morbidity rates with an increase in the care Locus of study and time frame: The prospective data
cost; becoming a public health problem worldwide [2, 3]. In collection performed in two surgical services (General surgery
developing countries, SSI is one of the frequent infections and Gynecology & Obstetrics) of the Regional Hospital of
associated with care [4]. According to a recent prevalence Borgou February 1st to August 31st 2013. The Department of
study in the United States of America (USA), SSI was the most General Surgery has 33 hospital beds and accommodated all
common of all infections associated with hospitalized patients patients operated in the central operating room of the
[5]
. Nowadays, nosocomial infections, particularly the SSI, are
hospital by all specialized surgical services. The Department of
considered as a reflection of the care quality in hospitals [6, 7].
Gynecology and Obstetrics (maternity) has 53 beds and
The reduction of the SSI rate requires knowledge of its risk
accommodated only the female patients operated in the
factors. It is within this framework that the authors propose to
analyze the risk factors of the SSI at the Regional and Teaching maternity unit.
Hospital Center of Borgou. The cloths and the surgical material were treated and
sterilized in the same way. The anesthesis specialists worked
MATERIALS & METHODS in both two surgical departments. Patients received were
Study design: This was a descriptive and analytical study exhaustive and lasted 6 months from February 2013 to July
Ethics approval: the agreement of the authorities of the 2013, but patient monitoring continued for 1 month or one
hospital was acquired. The patient gave their consent. The year depending on whether the patients operated had
anonymity was respected. The data collected were used only benefited from implants or not. Thus, the last patients
Hodonou M. Adrien et al.,
Page 1
Int J Clin and Biomed Res. 2017;3(1):01-04.
operated in July 2013 without prosthetic equipment had been general surgery and gynecology-obstetrics at the Regional
followed till 31 August 2013 while those with implant had Health Center of Borgou (Table 1).
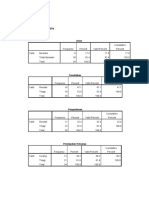
been followed till 31st August 2014. Table 1. Patients Distribution by Variables and Occurrence
Inclusion criteria: all the patients operated in both services of SSI
during the recruitment period were exhaustively included. Variables With SSI Without SSI P value
Exclusion criteria: when a patients consent was not given, he n (%) n (%)
Support service
was excluded. Those lost during the follow-up were excluded.
General surgery 28 (12.8%) 0.000***
And the patients who died in the follow-up period without SSI Gynaecology-obstetrics 16 (4.2%)
were also excluded. Infectious spot at
Methodology: For each patient, as soon as an operative admission 0.003***
Yes 11 (16.2%) 57 (83.8)
indication was given, we explained to him the purpose of the
No 33 (6.2%) 502 (93.8%)
current study and asked for his willingness to participate. In
Preoperative shaving of
the case of positive answer, we went further in the process. site to be incised
0.000***
When the patient was actually operated, we included him in Yes 28 (5.6%) 472 (94.4%)
the study by recording him in a database built for all patients No 16 (15.5%) 87 (84.5%)
Score ASA
operated during the study period. The surgical wound was
ASA1 17 (4.2%) 388 (95.8%)
followed for all patients operated during the monitoring ASA2 12 (12.4%) 85 (87.6%) 0.000***
period. When an SSI was declared, specific data about the ASA3 11 (12.4%) 78 (87.6%)
patient with SSI was then collected. The diagnostic criteria ASA4 4 (33.3%) 8 (66.6%)
Surgery contamination
were those of Centers for Disease Control and
class
Prevention/National Healthcare Safety Network (CDC/NHSN) Clean 6 (7.6%) 73 (92.4%)
of March 2009 [8]. Clean 20 (4.9%) 408 (95.1%) 0.000***
contaminated
Statistical analysis: Sample description was made possible by Contaminated 7 (13.0%) 47 (87.0%)
Durty infected 11 (26.2%) 31 (75.8%)
calculating the proportions and averages. Chi-square and
Score NNIS
Fisher tests (where Chi square was inappropriate) were used
NNIS0 16 (4.1%) 375 (95.9%)
to determine the significance level studied variables. Factors NNIS1 12 (7.1%) 157 (92.9%) 0.000***
associated with SSI occurrence were analyzed by performing NNIS2 15 (37.5%) 25 (62.5%)
logistic regression. The Odds Ratio (OR) was calculated and the NNIS3 1 (33.3%) 2 (66.7%)
risk of error was set at 5%. *** = significant (p<0.05).
RESULTS Risk factors determining SSI occurrence in general surgery and
in Gynecology-Obstetrics at CHD-B was identified by
From February 1st to July 31st 2013, 603 patients (218 in
performing logistic regression (Table 2).
general surgery and 385 in gynecology and obstetrics)
underwent surgery and 44 (7.3%) have developed SSI Table 2. Identification of factors determining SSI occurrence
depending on the defined case; 559 (92.7%) did not develop with logistic regression
SSI. Considering each service, the SSI frequency was 12.8% in 95%
general surgery and 4.2% in gynecology-obstetrics, Associated Odds
Coefficients P value Confident
respectively (Table 1) with a p = 0.000 (significant). The mean factors Ratio
Interval
age of patients with SSI was 30.7 15.8 years with a minimum Surgery [0.433;
and maximum of 5 months and 70 years; and for general 0.1369435 0.783 ns 1.146763
care 3.0383]
surgery patients, there were 23 men and 5 women (p = 0.17, [0.937;
not significant). No shaving 0.7239679 0.072 ns 2.062601
4.541]
Of the 57 patients with infectious spot at admission and [1.458;
NNIS score 1.219072 0.005*** 3.384046
operated, 11 (16.2%) have developed later SSI (Table I) with p 7.852]
= 0.003 (significant). The absence of pre-operative shaving of Constant -3.216274 0.000*** - -
the incising site (p = 0.000), the American Society of
Anesthesiologists (ASA) score [9] (p = 0.000), the surgical ns = not significant; *** = significant (p<0.05).
contamination class according to [10] (p = 0.000) and the score
of National Nosocomial Infections Surveillance (NNIS) DISCUSSION
according to CDC/NHSN surveillance denition of health
This study reports that the overall frequency of SSI at Regional
careassociated infection and criteria for specic types of
and Teaching Hospital of Borgou, which was 7.3%, was similar
infections in the acute care setting[8] (P = 0.000) were
significantly associated with the occurrence of the SSI in to that reported (7.3%) by Bibi et al. [11] on the one hand and
Hodonou M. Adrien et al.,
Page 2
Int J Clin and Biomed Res. 2017;3(1):01-04.
Giri et al. [12] on the other hand. This frequency is higher than 3. Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC
the 2.0% reported by Oni et al. [13]; to 0.9% in France definitions of nosocomial surgical site infections, 1992: a
[14]
modification of CDC definitions of surgical wound infections.
. However, it was much lower than the 10.1% obtained by Infect Control Hosp Epidemiol 1992;13(10):606-8.
Mankoutod et al. [15]; to 30.7% reported by Umesh et 4. Aiken AM, Wanyoro AK, Mwangi J, Mulingwa P, Mulingwa P,
al. [16]. There was significantly more SSI in general surgery Wanjohi J, et al. Evaluation of surveillance for surgical site
infections in Thika Hospital, Kenya. J Hosp Infect 2013;83(2):140-
(28/218, 12.8% of the operated patients) than in gynecology-
5.
obstetrics (16/385, 4.2% of operated patient). This same 5. Magill SS, Hellinger W, Cohen J, Kay R, Bailey C, Boland B, et al.
observation was made in the 2009-2010 SSI monitoring report Prevalence of healthcare-associated infections in acute care
in France [17]. The difference in rates between these two hospitals in Jacksonville, Florida. Infect Control Hosp Epidemiol
2012;33(3):283-91.
services could be attributed to several factors, three of which 6. Walter PW, Marcel Z, Stefan R, Chantal F-M, Heidi M, Rachel R,
are important:- the ASA score: the majority of patients with a et al. Infect Control and Hosp Epidemiol 2008;29(17):623-9.
poor ASA score (ASA3, ASA4 or ASA5) were in general surgery; 7. Satyanarayana V, Prashanth H V, Basavaraj B, Kavyashree A N.
Study of surgical site infections in abdominal surgeries. Journal
-the surgery contamination class: the operations of
of Clinical and Diagnostic Research 2011;29(17):935-9.
contaminated surgery were less practiced in gynecology- 8. Horan TC, Andrus M, Dudeck M A. CDC/NHSN surveillance
obstetrics compared to the general surgery service; Also, all denition of health careassociated infection and criteria for
the operations with dirty infected surgery have been carried specic types of infections in the acute care setting. Am J Infect
Control 2008;36(15):309-32.
out in the latter service. 9. Owens WD, Felts JA, Spitznagel EL. ASA physical status
The ASA score between 3 and 5 predisposed the patient to an classification: A study of consistency of ratings. J Anesth
SSI [17, 18]. In our study, the higher the ASA score was, the higher 1978;49(4):239-43.
the SSI rate was. Thus, the SSI rate rose from 4.2% for patients 10. Altemeier WA, Burke JF, Puitt BA, Sandusky WR. Manual on
control of infection in surgical patients. Philadelphia: JB
with an ASA score of 1 to 33.3% for those with an ASA score Lippincott 2nd edition; 1984:29p.
equal to 4. The risk of SSI occurrence was significantly related 11. Bibi S, Channa GA, Siddiqui TR, Ahmed W. Frequency and risk
to the degree of surgical dirt (p0.05) as the SSI rate increased factors of surgical site infections in general surgery ward of a
tertiary care hospital of Karachi, Pakistan. Int J Infect Control
by 7.6% for clean surgery and by 26.2% for infected dirty
2011;7(3):1-5.
surgery. Similar results were reported by several authors [7, 11]. 12. Giri BR, Pant HP, Sreeramareddy CT, Sen PK. Surgical site
However, most of the procedures performed in general infection and antibiotics use pattern in a tertiary care hospital in
surgery in our study were done for infectious diseases. For the Nepal. P Pak Med Asso 2008;58(3):148-51.
13. Oni A A, Ewete AF, Gbadja AT, Kolade AF, Mutiu WB, Adeyemo
CDC Expert Committee [19], it is necessary to know the patient's DA, et al. Nosocomial infections: surgical site infection in UCH
surgery class in order to give a suitable prophylactic antibiotic Ibadan (Nigeria). Nigerian Journal of Surgical Research
therapy. 2006;8(1-2):19-23.
14. Rseau dAlerte dinvestigation et de Surveillance des Infections
The SSI rate in our study increased significantly with the NNIS
Nosocomiales, Centres de Coordination de la Lutte contre les
score from 4.1% for an NNIS equal to 0 to 33.3% for an NNIS Infections Nosocomiales Est, Centres de Coordination de la Lutte
of 3 (p0.05). Indeed, the calculation of the NNIS score took contre les Infections Nosocomiales Ouest, et al. Surveillance des
into account the ASA score, the surgical class according to Infections du site opratoire France 2011 : Rsultats. [online].
Altemeier and the duration of surgical intervention. The NNIS Accessed online 08/02/2013,
score could then predict the occurrence of SSI. Indeed, in our http://www.invs.sante.fr/content/download/48611/209686/ve
study, this score of 2 or 3 multiplies by 3.4 the risk of SSI rsion/5/file/Rapport_Surveillance_infections_site_op%C3%A9r
occurrence. The same observation was done by several atoire_2011_iso_raisin.pdf.
15. Makoutod M, Birintanya N, Djigbnoud O, Paraso NM,
authors [18]; Atif et al. [20]; Hernandez et al. [21]; Alberto et al. Ouendo E-M, Agueh V. Etude de l'incidence de l'infection des
[22]
. All these authors confirmed the suitability of the NNIS plaies post-opratoires au centre hospitalier dpartemental de
score for assessing the SSI risk. l'Oum et du Plateau au Bnin. Le Bnin Mdical 2002;21:59-
62.
CONCLUSION 16. Umesh SK, Fereirra AMA, Kulkarni MS, Motghare DD. A
prospective study of surgical site infections in a teaching hospital
The NNIS score is a sound tool for predicting SSI and its actual in Goa. Indian J Surg 2008;70(3):120-4.
use as well as the rigorous practice of aseptic rules could 17. Rseau dAlerte dinvestigation et de Surveillance des Infections
contribute to a reduction of the SSI rate in general surgery and Nosocomiales, Centres de Coordination de la Lutte contre les
gynaecology-obstetrics at the Health Center of Borgou. Infections Nosocomiales Est, Centres de Coordination de la Lutte
contre les Infections Nosocomiales Ouest, et al. Surveillance des
REFERENCES Infection du site opratoire en France en 1999 et 2000 Rsultats.
[online]. accessed on 05/02/13,
1. Ruef C, Pittet D. pidmiologie et prvention des infections du http://www.invs.sante.fr/publications/2003/raisin_2002/index.
site chirurgical: progrs et problmes. Md et Hyg html.
1998;56(2225):1846-52. 18. Campos ML, Cipriani ZM, Freitas PF. Suitability of the NNIS Index
2. Francoli P, Nahimana I, Widmer A. Infections du site chirurgical. for estimating surgical-site infection risk at a small University
Swiss- NOSO 1996;3(1):1-15. Hospital in Brazil. Infect Control Hosp Epidemiol
2001;22(15):268-72.
Hodonou M. Adrien et al.,
Page 3
Int J Clin and Biomed Res. 2017;3(1):01-04.
19. [19] Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. 21. Hernandez K, Elizabeth R, Carlos S, German H, Eduardo G.
Guideline for prevention of surgical site infection, 1999. Hospital Incidence of and risk factors for Surgical-site Infections in a
Infection Control Practices Advisory Committee. Infect Control Peruvian Hospital. Infect Control Hosp Epidemiol
Hosp Epidemiol 1999;20(4):250-80. 2005;26(15):473-7.
20. Atif ML, Bouadda N, Bezzaoucha A, Azouaou A, Bendali L, 22. Alberto DL, Silvano P, Francesco R, Alberto M, Elena P, Vincenzo
Boubechou N, Bellouni R. Incidence of surgical cite infections P, et al. Surgical site infection in an Italian surgical ward: A
and accompanying risk factors in Algerian patients. Int J Infect prospective study. Surgical Infections 2009;10(16):533-8.
Control 2007;3(1):1-3.
Hodonou M. Adrien et al.,
Page 4
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Sanet ST 0199751765 PDFDokumen481 halamanSanet ST 0199751765 PDFRoman PBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Basic Statistics For Health SciencesDokumen361 halamanBasic Statistics For Health Sciencesgeofflilley89% (9)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Employee RetentionDokumen96 halamanEmployee RetentionsathishBelum ada peringkat
- Application of Statistics in The Business Research PDFDokumen5 halamanApplication of Statistics in The Business Research PDFAby Abdul Rabb87% (23)
- Non-Parametric TestsDokumen55 halamanNon-Parametric TestsMya Sumitra100% (1)
- Nelson Et Al-2010-Journal of Applied Social PsychologyDokumen14 halamanNelson Et Al-2010-Journal of Applied Social PsychologyclayBelum ada peringkat
- Statistics For Management - Assignments SolvedDokumen9 halamanStatistics For Management - Assignments Solvednitin_bslBelum ada peringkat
- Ore Body Modelling: Concepts and TechniquesDokumen33 halamanOre Body Modelling: Concepts and Techniquesفردوس سليمانBelum ada peringkat
- Utility of Salivary Ca-125 and LDH As A Tumor Marker in Oral MalignancyDokumen5 halamanUtility of Salivary Ca-125 and LDH As A Tumor Marker in Oral MalignancyInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Variations of Origin and Distance of Axillary Nerve: A Descriptive StudyDokumen4 halamanVariations of Origin and Distance of Axillary Nerve: A Descriptive StudyInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Protective Effect of Diosgenin Against Carbon Tetrachloride and Cisplatin Induced Hepatotoxicity in RatsDokumen7 halamanProtective Effect of Diosgenin Against Carbon Tetrachloride and Cisplatin Induced Hepatotoxicity in RatsInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Feasibility Study On Blood Cell Counting Using Mobile Phone-Based Portable MicroscopeDokumen4 halamanFeasibility Study On Blood Cell Counting Using Mobile Phone-Based Portable MicroscopeInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Alarming Signals of Drug Addiction Among The Southern Youths in Bangladesh: A Survey Based ResearchDokumen6 halamanAlarming Signals of Drug Addiction Among The Southern Youths in Bangladesh: A Survey Based ResearchInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Awareness About The Concept of Green Corridor Among Medical Student and Doctors in A Rural Medical College of Maharashtra, IndiaDokumen6 halamanAwareness About The Concept of Green Corridor Among Medical Student and Doctors in A Rural Medical College of Maharashtra, IndiaInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Perspectives of Medical Students & Teachers Regarding The Use of Different Lecture MethodsDokumen4 halamanPerspectives of Medical Students & Teachers Regarding The Use of Different Lecture MethodsInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Evaluation of Immunomodulatory Activity of Diosgenin in RatsDokumen6 halamanEvaluation of Immunomodulatory Activity of Diosgenin in RatsInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Pelvic Inflammatory Disease (Pid) : A Cross Sectional Prospective Study at A Tertiary Care CentreDokumen4 halamanPelvic Inflammatory Disease (Pid) : A Cross Sectional Prospective Study at A Tertiary Care CentreInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Assessment of Serum Paraoxonase-1 Enzyme Activity, Malondialdehyde and Vitamin-C in Oral PremalignanciesDokumen6 halamanAssessment of Serum Paraoxonase-1 Enzyme Activity, Malondialdehyde and Vitamin-C in Oral PremalignanciesInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Comparative Study of Lithotripsy and Miniperc in 11 To 18 MM Impacted Puj CalculiDokumen5 halamanComparative Study of Lithotripsy and Miniperc in 11 To 18 MM Impacted Puj CalculiInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Antibiotic Use in Pediatric Infections A Study in Tertiary Care HospitalDokumen7 halamanAntibiotic Use in Pediatric Infections A Study in Tertiary Care HospitalInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Synthesis of Novel Heterocyclic Quinolone Compound For Anti - Tubercular ActivityDokumen6 halamanSynthesis of Novel Heterocyclic Quinolone Compound For Anti - Tubercular ActivityInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Assessment of Ionized Calcium Status in Febrile SeizuresDokumen3 halamanAssessment of Ionized Calcium Status in Febrile SeizuresInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Pseudocholinesterase As A Predictor Marker in Hypothyroid PatientsDokumen3 halamanPseudocholinesterase As A Predictor Marker in Hypothyroid PatientsInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Electromyographic Activity of Various Muscles During Sit-To-Stand in Patients With Stroke: A Meta-AnalysisDokumen7 halamanElectromyographic Activity of Various Muscles During Sit-To-Stand in Patients With Stroke: A Meta-AnalysisInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- A Comparative Study of Topical Betaxalol and Timolol For Their Efficacy and Side EffectsDokumen4 halamanA Comparative Study of Topical Betaxalol and Timolol For Their Efficacy and Side EffectsInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Identification of Megaloblastic Anemia Cells Through The Use of Image Processing TechniquesDokumen5 halamanIdentification of Megaloblastic Anemia Cells Through The Use of Image Processing TechniquesInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Comparison of Cervical Biopsy Using Punch Biopsy Forceps Versus Loop ElectrodeDokumen7 halamanComparison of Cervical Biopsy Using Punch Biopsy Forceps Versus Loop ElectrodeInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Road Traffic Accidents in India: An OverviewDokumen3 halamanRoad Traffic Accidents in India: An OverviewInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Ethical Issues in Epidemiological StudiesDokumen3 halamanEthical Issues in Epidemiological StudiesInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- A Rare Case of Space Occupying Lesion of Brainstem in An Elderly Male PatientDokumen3 halamanA Rare Case of Space Occupying Lesion of Brainstem in An Elderly Male PatientInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Comparison Between Racemic Bupivacaine and Levobupivacaine Both Combined With Low Dose Fentanyl, Through Intrathecal Route For Transurethral Resection of ProstateDokumen4 halamanComparison Between Racemic Bupivacaine and Levobupivacaine Both Combined With Low Dose Fentanyl, Through Intrathecal Route For Transurethral Resection of ProstateInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Immediate Effect of Incentive Spirometry On Arterial Blood Gases Analysis After Coronary Bypass Graft Surgery PatientsDokumen3 halamanImmediate Effect of Incentive Spirometry On Arterial Blood Gases Analysis After Coronary Bypass Graft Surgery PatientsInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Clinical Outcome of Patients With Acute Scrotal Pain at A Tertiary Rural Centre in MaharashtraDokumen3 halamanClinical Outcome of Patients With Acute Scrotal Pain at A Tertiary Rural Centre in MaharashtraInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Effect of Lead On Male Reproduction in Experimental Animal ModelDokumen4 halamanEffect of Lead On Male Reproduction in Experimental Animal ModelInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Preparation and Evaluation of Transnasal Microemulsion of VigabatrinDokumen6 halamanPreparation and Evaluation of Transnasal Microemulsion of VigabatrinInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Influence of Distractions On Audio and Visual Reaction Time in Young Healthy Individual of 19-26 YearsDokumen5 halamanInfluence of Distractions On Audio and Visual Reaction Time in Young Healthy Individual of 19-26 YearsInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Dexmedetomidine Premedication With Ketamine and Propofol During Burns Debridement and DressingsDokumen5 halamanDexmedetomidine Premedication With Ketamine and Propofol During Burns Debridement and DressingsInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- Anti Inflammatory Effect of Ciprofloxacin, Azithromycin and Diclofenac Sodium On Carrageenan Induced Hind Paw Edema in MiceDokumen4 halamanAnti Inflammatory Effect of Ciprofloxacin, Azithromycin and Diclofenac Sodium On Carrageenan Induced Hind Paw Edema in MiceInternational Journal of Clinical and Biomedical Research (IJCBR)Belum ada peringkat
- DataPower Training TutorialDokumen394 halamanDataPower Training TutorialSorina StoianBelum ada peringkat
- Traffic Flow Distribution and Predicting Short Time Traffic Flow Composition Using Monte Carlo SimulationDokumen7 halamanTraffic Flow Distribution and Predicting Short Time Traffic Flow Composition Using Monte Carlo SimulationArif HasnatBelum ada peringkat
- Confidence Interval Estimation MultipleDokumen31 halamanConfidence Interval Estimation MultipleHuma RehmanBelum ada peringkat
- Metro Rail DhakaDokumen20 halamanMetro Rail DhakaKaushal ChapagainBelum ada peringkat
- Textile Engineering Course Overview - I & II Semester SubjectsDokumen34 halamanTextile Engineering Course Overview - I & II Semester SubjectsSiva Jagadish Kumar MBelum ada peringkat
- Lec12 Application of Mendel's PrincipleDokumen62 halamanLec12 Application of Mendel's PrincipleSITI BAZILAH BINTI BILAK KPM-GuruBelum ada peringkat
- LampiranDokumen16 halamanLampiranKus Patricia BrillianBelum ada peringkat
- AP Stat Free Response QuestionsDokumen22 halamanAP Stat Free Response QuestionsLOUELLA JADE SUAREZBelum ada peringkat
- GriesDokumen44 halamanGriesMagui SerriBelum ada peringkat
- Distribución de clientesDokumen5 halamanDistribución de clienteskeny ynekBelum ada peringkat
- A Vector Auto-Regressive (VAR) ModelDokumen21 halamanA Vector Auto-Regressive (VAR) Modelmeagon_cjBelum ada peringkat
- Socio-economic Impact of Guinness Brewery on Ikeja ResidentsDokumen19 halamanSocio-economic Impact of Guinness Brewery on Ikeja ResidentsMorrison Omokiniovo Jessa SnrBelum ada peringkat
- Chi Square Test - Apr 24 2015Dokumen30 halamanChi Square Test - Apr 24 2015Sneha Arora100% (1)
- Crystal Structure Refinement - TUTORIALDokumen83 halamanCrystal Structure Refinement - TUTORIALJuanBelum ada peringkat
- Merkle You Preacher 2016Dokumen13 halamanMerkle You Preacher 2016wuriBelum ada peringkat
- CB 6Dokumen24 halamanCB 6Himanshu SagarBelum ada peringkat
- Fixed Versus Random Effects Models for Multilevel and Longitudinal Data AnalysisDokumen82 halamanFixed Versus Random Effects Models for Multilevel and Longitudinal Data Analysisdanixh HameedBelum ada peringkat
- Deva Project Final Version-1Dokumen74 halamanDeva Project Final Version-1Saranya ManojBelum ada peringkat
- The Learning Environment As A Mediating Variable Between Self-Directed Learning ReadinessDokumen6 halamanThe Learning Environment As A Mediating Variable Between Self-Directed Learning ReadinessMagno AquinoBelum ada peringkat
- A R S C P T M-C: Esearch To Tudy The Onsumer Erception Owards OmmerceDokumen43 halamanA R S C P T M-C: Esearch To Tudy The Onsumer Erception Owards OmmerceSaransh AggarwalBelum ada peringkat
- Relationship between snack consumption and dental caries among studentsDokumen6 halamanRelationship between snack consumption and dental caries among studentsprimaBelum ada peringkat
- BTHBSC... 301 Mathematics-III 2023-24Dokumen3 halamanBTHBSC... 301 Mathematics-III 2023-24Diza N.SultanaA44Belum ada peringkat