Joc10219 PDF
Diunggah oleh
Francisco Tapia Román.Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Joc10219 PDF
Diunggah oleh
Francisco Tapia Román.Hak Cipta:
Format Tersedia
ORIGINAL CONTRIBUTION
The Role of Knee Alignment
in Disease Progression and Functional
Decline in Knee Osteoarthritis
Leena Sharma, MD Context Knee osteoarthritis (OA) is a leading cause of disability in older persons. Few
Jing Song, MS risk factors for disease progression or functional decline have been identified. Hip-
knee-ankle alignment influences load distribution at the knee; varus and valgus align-
David T. Felson, MD, MPH
ment increase medial and lateral load, respectively.
September Cahue, BS Objective To test the hypotheses that (1) varus alignment increases risk of medial knee
Eli Shamiyeh, MS OA progression during the subsequent 18 months, (2) valgus alignment increases risk
Dorothy D. Dunlop, PhD of subsequent lateral knee OA progression, (3) greater severity of malalignment is as-
sociated with greater subsequent loss of joint space, and (4) greater burden of malalign-
T
WELVE PERCENT OF THE US ment is associated with greater subsequent decline in physical function.
population aged 25 to 75 years Design and Setting Prospective longitudinal cohort study conducted March 1997
has symptoms and signs of os- to March 2000 at an academic medical center in Chicago, Ill.
teoarthritis (OA).1 Disability Participants A total of 237 persons recruited from the community with primary knee
due to OA is largely a result of knee or OA, defined by presence of definite tibiofemoral osteophytes and at least some dif-
hip involvement. The risk of disability ficulty with knee-requiring activity; 230 (97%) completed the study.
attributable to knee OA alone is as great Main Outcome Measures Progression of OA, defined as a 1-grade increase in
as that due to cardiac disease and greater severity of joint space narrowing on semiflexed, fluoroscopically confirmed knee ra-
than that due to any other medical con- diographs; change in narrowest joint space width; and change in physical function be-
dition in elderly persons.2 Knee OA also tween baseline and 18 months, compared by knee alignment at baseline.
substantially increases risk of disabil- Results Varus alignment at baseline was associated with a 4-fold increase in the odds
ity due to other medical conditions.3 In- of medial progression, adjusting for age, sex, and body mass index (adjusted odds ra-
creased awareness of the impact of knee tio [OR], 4.09; 95% confidence interval [CI], 2.20-7.62). Valgus alignment at base-
OA has provided impetus to acceler- line was associated with a nearly 5-fold increase in the odds of lateral progression (ad-
ate development of disease-modifying justed OR, 4.89; 95% CI, 2.13-11.20). Severity of varus correlated with greater medial
joint space loss during the subsequent 18 months (R=0.52; 95% CI, 0.40-0.62 in domi-
agents (ie, treatments that delay OA
nant knees), and severity of valgus correlated with greater subsequent lateral joint space
progression).4 At present, there are no loss (R=0.35; 95% CI, 0.21-0.47 in dominant knees). Having alignment of more than
disease-modifying drugs for OA. 5 (in either direction) in both knees at baseline was associated with significantly greater
Poor understanding of the natural functional deterioration during the 18 months than having alignment of 5 or less in
history of OA contributes to the slow both knees, after adjusting for age, sex, body mass index, and pain.
development of interventions that Conclusion This is, to our knowledge, the first demonstration that in primary knee OA
modify the course of the disease. This varus alignment increases risk of medial OA progression, that valgus alignment increases
deficiency of knowledge hinders de- risk of lateral OA progression, that burden of malalignment predicts decline in physical
velopment of novel interventions to tar- function, and that these effects can be detected after as little as 18 months of observation.
get factors responsible for disease pro- JAMA. 2001;286:188-195 www.jama.com
gression and functional decline; it also
clouds the ability to identify patients incidence (ie, new occurrence) of os- Author Affiliations: Northwestern University Medi-
cal School, Chicago, Ill (Drs Sharma and Dunlop, Mr
who are unlikely to benefit from inves- teoarthritic disease? (2) disease progres- Shamiyeh, and Mss Song and Cahue); and Boston Uni-
tigational treatments. sion in those who already have OA? and versity, Boston, Mass (Dr Felson).
In the investigation of a candidate risk (3) disability in those with OA? The lit- Corresponding Author and Reprints: Leena Sharma,
MD, Northwestern University Medical School, 303 E
factor in OA studies, 3 key questions erature on knee OA is weighted toward Chicago Ave, Ward Bldg 3-315, Chicago, IL 60611
arise. Does the factor contribute to (1) the first question. However, the second (e-mail: L-Sharma@northwestern.edu).
188 JAMA, July 11, 2001Vol 286, No. 2 (Reprinted) 2001 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ on 12/20/2014
KNEE ALIGNMENT AND KNEE OSTEOARTHRITIS
and third questions are crucial to the goal magnitude of intrinsic compressive load ficulty with knee-requiring activity. Ex-
of reducing the burden of knee OA. In on the medial compartment during clusion criteria were corticosteroid in-
a subset of individuals, knee OA re- gait.19 Varus-valgus alignment is a key jection within the previous 3 months or
mains in the mild state that character- determinant of this moment. history of avascular necrosis, rheuma-
izes newly developed OA; Dieppe5 has These mechanical effects of align- toid or other inflammatory arthritis, peri-
stated that in this subset, OA should not ment on load distribution make it bio- articular fracture, Paget disease, villo-
even be considered a diseaseOA that logically plausible that both varus and nodular synovitis, joint infection,
progresses beyond mild stages is respon- valgus alignment contribute to OA pro- ochronosis, neuropathic arthropathy, ac-
sible for the bulk of both individual and gression. Further support comes from romegaly, hemochromatosis, Wilson dis-
societal costs of OA. Knowledge of the animal studies17 as well as surgical stud- ease, osteochondromatosis, gout, pseu-
factors that lead to progression and func- ies, which identify knee alignment as dogout, or osteopetrosis. Approval was
tional decline will aid development of a predictor of knee procedure out- obtained from the Office for the Protec-
interventions to modify disease course comes. The question that has not been tion of Research SubjectsInstitutional
and patient-centered outcomes. answered is, does knee alignment in- Review Board of Northwestern Univer-
In the investigation of knee OA pro- fluence risk of structural progression sity. Written informed consent was ob-
gression, the recommended primary and functional decline in knee OA? tained from all participants.
outcome is joint space change, mea- In this study, we tested whether (1)
sured via radiographic images ac- varus alignment at baseline increases Alignment
quired using special protocols that risk of subsequent medial tibiofemo- To assess alignment, a single antero-
maximize accuracy and reliability.6-13 ral compartment OA progression, (2) posterior radiograph of the lower ex-
The sparse literature regarding progres- valgus alignment at baseline increases tremity was obtained. A 13036-cm
sion is limited by its reliance on con- risk of subsequent lateral compart- graduated grid cassette was used to in-
ventional, extended-knee radiogra- ment OA progression, (3) severity of clude the full limb of tall partici-
phy (ie, without the protocols now varus or valgus malalignment at base- pants.20 By filtering the x-ray beam in
considered essential). line is correlated with subsequent a graduated fashion, this cassette ac-
Osteoarthritis is widely believed to change in medial or lateral joint space counts for the unique soft tissue char-
be the result of local mechanical fac- width, respectively, and (4) greater bur- acteristics of the hip and ankle. Partici-
tors acting within the context of sys- den of malalignment at baseline is as- pants stood without footwear, with
temic susceptibility.14-16 Certain site- sociated with greater subsequent dete- tibial tubercles facing forward. The tibial
specific factors in the local joint rioration in physical function. tubercle, a knee-adjacent site not dis-
environment govern how load is dis- torted by OA, was used as positioning
tributed across the articular cartilage of METHODS landmark.21 The patella is often used to
a given joint. However, the effect of Participants position normal knees,20 but the pos-
such factors on OA progression or pa- The Mechanical Factors in Arthritis of sibility of patellofemoral OA pre-
tient-centered outcomes is largely un- the Knee (MAK) study is a longitudi- cluded this approach. The x-ray beam
examined. nal study of the contribution of me- was centered at the knee at a distance
At the knee, alignment (ie, the hip- chanical factors to disease progression of 2.4 m. A setting of 100 to 300 mA/s
knee-ankle angle) is a key determi- and functional decline in knee OA. Par- and 80-90 kV was used, depending on
nant of load distribution. In theory, any ticipants were recruited from the com- limb size and tissue characteristics.
shift from a neutral or collinear align- munity through advertising in periodi- Alignment was measured as the angle
ment of the hip, knee, and ankle af- cals targeting elderly persons, 67 formed by the intersection of the me-
fects load distribution at the knee.17 The neighborhood organizations, letters to chanical axes of the femur (the line from
load-bearing axis is represented by a line members of the registry of the Buehler femoral head center to femoral inter-
drawn from mid femoral head to mid Center on Aging at Northwestern Uni- condylar notch center) and the tibia
ankle. In a varus knee, this line passes versity, Chicago, Ill, and local referrals. (the line from ankle talus center to the
medial to the knee and a moment arm Inclusion and exclusion criteria were center of the tibial spine tips).17,21,22 A
is created, which increases force across based on National Institute of Arthritis knee was defined as varus when align-
the medial compartment. In a valgus and Musculoskeletal and Skin Diseases/ ment was more than 0 in the varus di-
knee, the load-bearing axis passes lat- National Institute on Agingsponsored rection, valgus when it was more than
eral to the knee, and the resulting mo- multidisciplinary workshop recommen- 0 in the valgus direction, and neutral
ment arm increases force across the lat- dations for knee OA progression stud- when alignment was 0.20,22-24 The angle
eral compartment.17 Disproportionate ies.6 Inclusion criteria were definite tib- made by the femur and tibia on a knee
medial transmission of load results from iofemoral osteophyte presence (Kellgren/ x-ray was not used because it does not
a stance-phase adduction moment.18 Lawrence [K/L] radiographic grade 2) consider the proximal femur, femoral
This adduction moment reflects the of 1 or both knees and at least some dif- or tibial shafts, or ankle25; is highly vari-
2001 American Medical Association. All rights reserved. (Reprinted) JAMA, July 11, 2001Vol 286, No. 2 189
Downloaded From: http://jama.jamanetwork.com/ on 12/20/2014
KNEE ALIGNMENT AND KNEE OSTEOARTHRITIS
able as opposed to full-limb measure- sition, criteria for beam alignment rela- ment was measured using calipers with
ments22; and is not typically used in or- tive to knee center, radiopaque markers electronic readout.6,40,41 Joint space area
thopedic clinical or biomechanical to account for magnification, and mea- and midcompartment width are less
studies. surement landmarks were specified. All sensitive to change than narrowest joint
One experienced reader made all radiographs were obtained in the same space width.35
measurements. Reliability was high for unit by 2 trained technicians. Other approaches (ie, osteophyte
measurements of varus (intraclass cor- The standing semiflexed view of the grade, K/L grade) had limitations. Al-
relation coefficient [ICC], 0.99) and val- knee in this protocol is optimal for joint though osteophytes can be graded per
gus (ICC, 0.98) alignment. space assessment because it achieves su- compartment, they are often more
perimposition of the anterior and pos- prominent in the uninvolved compart-
Varus-Valgus Laxity terior joint margins.12,36,37 The knee was ment. The K/L grade provides a global
Because physical examination laxity flexed until the tibial plateau was hori- score without separate information for
tests are unreliable,26,27 a device to mea- zontal, parallel to the beam and per- the medial and lateral compartments
sure varus-valgus laxity was designed pendicular to the film. To control for (ie, 0 = normal; 1 = possible osteo-
by Thomas Buchanan, PhD.28,29 This de- rotation, the heel was fixed and the foot phytes; 2=definite osteophytes and pos-
vice and the measurement protocol ad- rotated until the tibial spines were cen- sible joint space narrowing; 3=moder-
dress sources of variation in knee lax- tral within the femoral notch. Knee po- ate/multiple osteophytes, definite
ity tests, ie, inadequate thigh and ankle sition was confirmed by fluoroscopy be- narrowing, some sclerosis, and pos-
immobilization, incomplete muscle re- fore films were taken. Foot maps made sible attrition; and 4 = large osteo-
laxation, variation of the knee flexion at baseline were used to standardize phytes, marked narrowing, severe scle-
angle, variation of load applied, and im- repositioning at 18 months. These rosis, and definite attrition).
precise measurement of rotation.26,27,30 protocol elements enhance accuracy One experienced reader assessed ra-
The system consists of a bench with and precision of joint space assess- diographs using an atlas.8 Reliability for
an arc-shaped, low-friction track run- ment.12,37 Even without fluoroscopic joint space grading ( coefficient, 0.80-
ning medially and laterally. The distal confirmation, the semiflexed view was 0.86) and measurement (ICC, 0.95-
shank is attached to a sled, which trav- superior to the extended or schuss 0.98) was very good. Reading of knee
els within the track. A handheld dyna- views38; the fluoroscopic approach, by and full-limb radiographs occurred in
mometer fits into the sled and is used confirming the same position in all ra- separate sessions. The reader was
to apply load. Participants assumed a diographs, further reduces variability. blinded to knee data when assessing
seated position, with the thigh and alignment and to alignment data when
ankle immobilized and the study knee Radiographic Progression assessing knee radiographs.
at 20 flexion.31 An auditory signal in- Joint space assessment is the widely rec-
dicates when a load of 40 newtons (12 ommended primary outcome for knee Physical Function and Pain
newtons/m) has been applied.32 OA progression studies9,11,39 and pro- Physical function was assessed using an
Laxity was measured as the angular vides a compartment-specific mea- observed measure, chair-stand perfor-
deviation at the sled after varus and val- sure, which was required in this study. mance (rate of chair stands per minute,
gus load. Total rotation, the sum of Medial and lateral progression were based on the time required to complete
varus and valgus rotation for each knee, defined as a 1-grade or greater in- 5 repetitions of rising from a chair and
was examined as previously de- crease in severity of joint space nar- sitting down), using the protocol of Gu-
scribed.32-34 All laxity measurements rowing in the medial and lateral com- ralnik et al42 and Seeman et al.43 The sit-
were performed by the same examiner partments, respectively. We used the stand transfer is closely linked to knee
and assistant. Our reliability with this 4-grade scale (ie, 0 = none; 1 = pos- status.44 Of the lower-extremity joints,
device was very good (within-session sible; 2 =definite; and 3=severe) with the knee often exhibits the greatest peak
ICC, 0.85-0.96; between-session ICC, atlas representations from Altman et al.8 torques during this task.45-47 Average pain
0.84-0.90). Joint space was also measured at the during the past week was recorded on
narrowest point in each compart- separate 0- to 100-mm visual analog
Knee Radiographs ment. The femoral boundary was the scales (VASs) for each knee.
For knee radiographs at baseline and distal convex margin of the condyles.
18 months, the Buckland-Wright pro- The tibial boundary was the line ex- Statistical Analysis
tocol35 was followed. This protocol tending from tibial spine to outer mar- For analyses of OA progression, knees
meets recommendations for knee OA gin, across the center of the articular not at risk of progressing (ie, those with
studies provided by multidisciplinary fossa, defined by the superior margin the highest grade of joint space nar-
workshops6 and the Task Force of the of the bright radiodense band of the rowing at baseline) were excluded. De-
Osteoarthritis Research Society Inter- subchondral cortex.35,40 The narrow- scriptive data (proportions) and cor-
national.9 Per this protocol, knee po- est interbone distance of each compart- relations were provided separately for
190 JAMA, July 11, 2001Vol 286, No. 2 (Reprinted) 2001 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ on 12/20/2014
KNEE ALIGNMENT AND KNEE OSTEOARTHRITIS
dominant and nondominant knees,
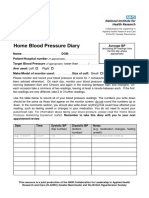
Table 1. Sample Participant Characteristics
with dominance ascertained using the
Study Sample Eligible Noncompleters
question, In order to kick a ball, which (n = 230) (n = 7)
leg would you use? All statistical tests Age, mean (SD), y 64.0 (11.1) 64.1 (13.0)
were conducted using a nominal level Body mass index, mean (SD), kg/m2 30.3 (5.8) 33.6 (9.0)
of .05. The risk of progression was ana- Sex, No.
lyzed from logistic regression, using Women 173 4
generalized estimating equations Men 57 3
(GEEs) to include data from 1 or both Osteoarthritis severity, No.*
Kellgren/Lawrence grade
knees of each participant. Odds ratios 0 1 0
(ORs) were calculated for medial and 1 14 0
lateral progression, first entering align- 2 108 3
ment (unadjusted OR), then adding age, 3 71 3
sex, and body mass index (BMI) (ad- 4 36 1
justed OR). Odds ratios were recalcu- Joint space narrowing grade
lated after additional adjustment for lax- 0 59 0
ity. The associated 95% confidence 1 63 3
intervals (CIs) were calculated; a 95% 2 66 2
CI of more than 1.00 indicates that 3 42 2
alignment is significantly associated Alignment, No.
Varus 117 5
with progression. The same approach Valgus 97 1
was taken to explore the relationship Neutral 16 1
between alignment and progression as- Laxity, mean (SD) 5.3 (2.0) 6.3 (1.8)
sessed using K/L grade. *Osteoarthritis severity is presented for dominant knees.
Next, the relationship between base-
line varus alignment (in degrees; varus We also explored the relationship be- valgus knees. Of 24 dominant knees with
as a positive value, neutral as 0, and val- tween baseline alignment group and lateral progression, 19 (79%) were val-
gus as a negative value) and change in functional decline, designated as at least gus. Mean valgus alignment was 3.21
medial joint space width from baseline 20% worsening in chair-stand rate. Lo- at baseline and 3.24 at 18 months. Re-
to 18 months, each as a continuous vari- gistic regression analysis was used to sults were similar in nondominant
able, was examined in dominant knees evaluate the unadjusted and adjusted knees.
using linear regression analysis. A de- odds of performance decline related to The average change in the compart-
crease in joint space was analyzed as a alignment group status. ment that was narrower at baseline was
positive value. Similarly, the relation- a loss of 0.45 mm over 18 months. Defi-
ship between baseline valgus alignment RESULTS nite joint space narrowing (grade 2)
(valgus as a positive value, neutral as 0, Of 237 participants at risk for progres- was present in either the medial or the
and varus as a negative value) and change sion in at least 1 knee, 7 (3%) did not lateral compartment but never in both.
in lateral joint space width from base- return at 18 months; 5 died and 2 could In no knee did both medial and lateral
line to 18 months was examined. not be reached. Selected characteristics progression occur; tibiofemoral pro-
For analyses of physical function, par- of these participants are presented in gression was a unicompartmental event.
ticipants whose chair-stand perfor- TABLE 1. No participant received therapy
mance could not further decline (ie, that might have affected the progres- Medial Progression
those who could not perform the test at sion rate. In GEE logistic regression analyses,
baseline) were excluded. Participants varus vs nonvarus (referent) align-
were divided into 3 alignment groups Radiographic Progression ment at baseline was associated with a
based on having 0, 1, or 2 knees with In dominant knees, medial OA progres- 5-fold increase in the odds of medial
baseline alignment of more than 5 from sion occurred in 28 (31%) of 89 varus progression during the subsequent 18
neutral (in either direction). Change vs 9 (9%) of 102 nonvarus knees. Of the months (TABLE 2). After adjustment for
from baseline to 18 months in chair- 37 dominant knees with medial progres- age, sex, and BMI, varus alignment was
stand rate was regressed on alignment sion, 28 (76%) were varus at baseline. still associated with a 4-fold increase in
group status to evaluate unadjusted and Mean varus alignment was 3.34 at base- the odds of medial progression.
age-, sex-, and BMI-adjusted differ- line and 3.82 at 18 months. Results were In calculating risk in varus vs non-
ences between groups. To explore the similar in nondominant knees. varus knees, we recognized that me-
mediating role of pain, further analyses Lateral OA progression occurred in 19 dial OA may be associated with varus,
additionally adjusted for pain. (22%) of 88 valgus vs 5 (5%) of 103 non- valgus, or neutral alignment. There-
2001 American Medical Association. All rights reserved. (Reprinted) JAMA, July 11, 2001Vol 286, No. 2 191
Downloaded From: http://jama.jamanetwork.com/ on 12/20/2014
KNEE ALIGNMENT AND KNEE OSTEOARTHRITIS
examined the relationship between
Table 2. Odds Ratios for Medial and Lateral Progression*
baseline alignment and K/L grade pro-
Odds Ratio (95% Confidence Interval)
gression (1-grade increase). How-
Unadjusted Adjusted ever, knees that progress by K/L grade
Varus Alignment and Medial Progression include some knees with medial pro-
Nonvarus 1.00 1.00 gression and other knees with lateral
Varus 5.00 (2.77-9.02) 4.09 (2.20-7.62)
progression. Therefore, this analysis
Neutral/mild valgus 1.00 1.00
Varus 3.54 (1.85-6.77) 2.98 (1.51-5.89) tests a different hypothesisdoes varus
alignment increase risk of progression
Valgus Alignment and Lateral Progression
in either the medial (mechanically
Nonvalgus 1.00 1.00
Valgus 3.88 (1.82-8.24) 4.89 (2.13-11.20) stressed by varus alignment) or the lat-
Neutral/mild varus 1.00 1.00 eral (not stressed) compartment, and
Valgus 3.23 (1.30-8.05) 3.42 (1.31-8.96) does valgus alignment increase risk of
*Knees with grade 3 joint space narrowing at baseline were excluded. For analyses involving nonvarus and neutral/
mild valgus reference groups, n = 381 and 281 knees, respectively. For analyses involving nonvalgus and neutral/
progression in either the medial (not
mild varus reference groups, n = 381 and 278 knees, respectively. Mild varus and mild valgus were defined as 2 stressed) or the lateral (stressed by val-
varus or valgus, respectively.
Adjusted for age, sex, and body mass index. gus alignment) compartment? Nota-
bly, there is no rationale to support a
link between varus alignment and lat-
fore, the risk associated with varus CI, 2.19-7.62). The OR for the rela- eral progression or between valgus
alignment was compared with the risk tionship between valgus alignment and alignment and medial progression.
conferred by any other possible align- lateral progression, adjusting for age, Even with this limitation of the K/L
ment for a given knee. To determine the sex, BMI, and laxity, was 4.78 (95% CI, grading system, valgus alignment was
progression risk associated with varus 2.08-11.02). associated with an increase in risk of
alignment when the comparison group Results of analyses of medial pro- K/L grade progression (OR, 2.51; 95%
was neutral or nearly neutral knees, we gression were not affected by exclud- CI, 0.91-6.89), and varus alignment was
repeated the analysis with a referent ing lateral progressors from the non- associated with a significant increase in
group consisting of neutral (0) or progressor group. Results of analyses risk of K/L grade progression (OR, 3.61;
mildly valgus (2) knees. Varus align- of lateral progression also were not af- 95% CI, 1.33-9.85), further attesting to
ment was still associated with a 3-fold fected by excluding medial progres- the strength of their effects. Finally, ab-
increase in risk of medial progression sors from the nonprogressor group. solute severity of malalignment as a
in adjusted analyses (Table 2). continuous variable was significantly as-
Malalignment Severity at Baseline sociated with K/L grade progression.
Lateral Progression and Change in Joint Space
In GEE logistic regression analyses, val- The relationship between baseline se- Burden of Knee Malalignment
gus vs nonvalgus (referent) alignment verity of varus alignment and change in at Baseline and Change
at baseline was associated with an al- medial joint space width from baseline in Physical Function
most 4-fold increase in the odds of lat- to 18 months, each as a continuous vari- Burden of malalignment at baseline pre-
eral progression during the subse- able, was examined in dominant knees. dicted deterioration in physical func-
quent 18 months (Table 2). This Greater varus alignment correlated with tion between baseline and 18 months.
relationship persisted after adjust- greater subsequent loss of joint space Participants were classified into 1 of
ment for age, sex, and BMI. (R=0.52; 95% CI, 0.40-0.62). 3 groups at baseline: those who had
When the referent group was neu- Similarly, the relationship between alignment of 5 or less in both knees
tral or nearly neutral (2 varus) knees, baseline severity of valgus and change in (n = 126), 1 knee with alignment of
valgus alignment was associated with lateral joint space width from baseline to more than 5 (n = 52), or both knees
a more than 3-fold increase in the odds 18 months was examined in dominant with alignment of more than 5 (n=37).
of subsequent lateral OA progression knees. Severity of valgus correlated with Physical functional outcome was ana-
in both unadjusted and adjusted analy- the magnitude of loss of lateral joint space lyzed as a continuous variable, ie,
ses (Table 2). width (R = 0.35; 95% CI, 0.21-0.47). change in chair-stand rate from base-
These logistic regression analyses These relationships persisted after ad- line to 18 months. Change did not dif-
were repeated after additionally con- justment for age, sex, BMI, and laxity. fer between the first 2 groups, but sig-
trolling for varus-valgus laxity, with nificantly greater deterioration in chair-
little effect on results. The OR for the Alignment at Baseline and stand performance was found in
relationship between varus alignment Progression of K/L Grade participants who had alignment of more
and medial progression, adjusting for Given the historical role of the K/L grad- than 5 in both knees vs participants
age, sex, BMI, and laxity, was 4.01 (95% ing system in knee OA studies, we also who had alignment of 5 or less in both
192 JAMA, July 11, 2001Vol 286, No. 2 (Reprinted) 2001 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ on 12/20/2014
KNEE ALIGNMENT AND KNEE OSTEOARTHRITIS
knees (TABLE 3). The difference be-
Table 3. Alignment Group Differences in Change in Chair-Stand Rate, Baseline to
tween these groups persisted after ad- 18 Months
justing for age, sex, and BMI. Difference Between Groups (95% Confidence Interval)*
We also explored the relationship be-
tween burden of malalignment and Age-, Sex-, and Age-, Sex-, BMI-,
Unadjusted BMI-Adjusted and Pain-Adjusted
functional decline, designating de- 1 Knee 5 vs 0.48 (1.40 to 2.36) 0.43 (1.44 to 2.31) 0.17 (1.66 to 2.01)
cline as at least 20% worsening in chair- both knees 5
stand rate. Thirty-four (16%) of the 215 Both knees 5 vs 2.88 (0.75 to 5.01) 2.73 (0.52 to 4.94) 2.23 (0.05 to 4.41)
participants able to perform the test at both knees 5
baseline had functional decline by this *BMI indicates body mass index. For each group, the change in chair-stand rate was determined, with positive values
indicating a decrease in rate. The chair-stand rate is the number of stands per minute, calculated from the time re-
definition, including 10% of the 126 quired to complete 5 chair stands.
with alignment in both knees of 5 or
less, 21% of the 52 with alignment of
more than 5 in 1 knee, and 27% of the 2 vs 0 knees) continued to be signifi- progression. The results of the cur-
37 with alignment of more than 5 in cantly associated with subsequent func- rent study, especially given the influ-
both knees. The odds of functional de- tional deterioration. ence of alignment on load distribu-
cline were doubled (OR, 2.33; 95% CI, tion, support this concept.
0.97-5.62) by having 1 knee with align- COMMENT The presence of a relationship be-
ment of more than 5 vs both knees with Varus alignment at baseline increased tween alignment and progression by 18
alignment of 5 or less and were tripled risk of medial knee OA progression over months underscores the importance of
by having alignment of more than 5 the 18 months of our study, and val- alignment as a risk factor. In knee OA
in both knees vs alignment of 5 or less gus alignment increased risk of subse- progression studies, 18 months is a rela-
in both knees (OR, 3.22; 95% CI, quent lateral knee OA progression. The tively early follow-up point, at which
1.28-8.12). This association persisted severity of varus malalignment at base- an effect may not as yet be detectable.
after adjusting for age, sex, and BMI. line correlated with the magnitude of The importance of alignment was fur-
medial joint space loss, and the base- ther demonstrated by the finding of a
Burden of Malalignment, line severity of valgus malalignment strong relationship with progression
Functional Deterioration, and Pain correlated with the magnitude of lat- even when the referent group in-
To explore whether pain is an interven- eral joint space loss. A greater burden cluded only neutral or nearly neutral
ing variable in the relationship be- of malalignment at baseline was linked knees. The alignment-associated odds
tween knee alignment and functional de- to greater decline in an observed mea- of progression may be even greater at
terioration, first we examined the sure of physical function. To our knowl- longer follow-up. The odds may be sub-
relationship between alignment and pain edge, this is the first demonstration that stantially greater if malalignment and
at baseline, then we examined whether alignment influences risk of subse- knee OA are in a vicious cycle.
the relationship between alignment and quent primary OA disease progres- Varus or valgus alignment may
functional deterioration was lost after ac- sion and decline in functional status and stretch the capsule and collateral liga-
counting for pain. Average pain in- that these effects can be detected after ments, increasing varus-valgus laxity,
creased as malalignment increased as little as 18 months of observation. a potential mechanism of the align-
(alignment 4=pain score of 25.2 mm In theory, varus and valgus align- ment effect. If laxity were playing this
on the VAS; alignment 4 but ment may each be a cause or result of role, then controlling for laxity should
8=pain score of 37.7 mm; and align- progressive knee OA; therefore, it was lead to a reduction in the alignment-
ment 8=pain score of 41.2 mm). Pain essential to examine alignment at the progression relationship. In our study,
severity was significantly associated with beginning of the period during which this did not occur, suggesting that an
malalignment severity. Specifically, the progression was evaluated. Varus or val- increase in laxity is not a major mecha-
GEE logistic regression analysis of align- gus alignment that predates knee OA nism for the alignment effect. Our study
ment and pain showed an average VAS may be due to genetic, developmen- had more women than men; this sex
increase of 10 mm in knee pain with tal, or posttraumatic factors. Animal distribution matches that of knee OA
each 5 of malalignment. This relation- model data support a link between pre- in the general population. The effects
ship persisted after adjustment for age, existing varus or valgus alignment and of alignment were independent of sex.
sex, and BMI. Next, we repeated the OA development.17 Knee alignment that Burden of malalignment influenced
analysis of the relationship between results from knee OA may be due to loss patient-centered outcome, physical func-
alignment group and change in chair- of cartilage and bone height. How- tion assessed by chair-stand perfor-
stand rate after additionally account- ever, even as a consequence of osteo- mance. In knee OA, risk factor profiles
ing for pain. As shown in Table 3, the arthritic disease, varus or valgus align- for structural disease progression and for
burden of malalignment at baseline (ie, ment may contribute to subsequent disability overlap but are not identical.
2001 American Medical Association. All rights reserved. (Reprinted) JAMA, July 11, 2001Vol 286, No. 2 193
Downloaded From: http://jama.jamanetwork.com/ on 12/20/2014
KNEE ALIGNMENT AND KNEE OSTEOARTHRITIS
It was necessary to specifically exam- ration and surgical outcome studies. phy, is not possible. In previous pro-
ine the relationship between alignment Testing the immediate or short-term me- gression studies, medial and lateral knee
and functional status. Longitudinal stud- chanical impact of a factor is not equiva- OA have been treated as a single con-
ies of patient-centered outcomes in knee lent to testing its impact on a long- dition, despite a belief that they differ
OA have been rare; knowledge about term structural outcome in a patient. The in rate of progression and risk factor
risk factors has been derived chiefly from stage of investigation represented by the profile. Our results provide evidence
cross-sectional studies. We explored current study was necessary, both to that tibiofemoral OA progresses asym-
whether pain was an intervening factor demonstrate and to quantify the long- metrically and illustrate that local risk
in the alignment effect on function. term effects of knee alignment on pa- factors are not only specific to joint but
While the strength of the alignment- tient outcomes. Several orthopedic also to compartment.
function relationship was reduced studies have demonstrated that knee The goal of this study was to exam-
slightly after accounting for pain, a sig- alignment is associated with surgical out- ine the influence of alignment on struc-
nificant relationship persisted, suggest- come (eg, arthroplasty,53 osteotomy,54 tural and functional outcomes in pa-
ing that at least some portion of the meniscectomy, 5 5 - 5 7 and meniscal tients with established OA. There is
alignment effect is independent of pain. debridement58). While extremely im- growing awareness that risk factors for
The results of this study are consis- portant, these data do not address the incident OA differ from risk factors for
tent with biomechanical studies that role played by knee alignment in the OA progression. It is likely that knee
have revealed that varus and valgus nonsurgical, natural evolution of knee alignment has a different effect on risk
alignment increase medial and lateral OA. In the operated knee, the develop- of incident OA from that shown here
load, respectively.17,48,49 During gait, the ment or progression of OA is linked to on risk of progression. The former ef-
impact of valgus on load distribution several factors not at play in natural pro- fect may be smaller, given the less vul-
may not be comparable with that of gression (eg, nature of surgery and stage nerable state of the healthy knee. How-
varus alignment. In the normally aligned of OA at time of surgery). ever, the effect on risk of incident OA
ambulating knee, load is disproportion- Investigation of the influence of cannot be inferred from these results
ately transmitted to the medial compart- alignment on natural structural or and should be specifically examined.
ment.50 Varus alignment further in- patient-centered outcomes in unse- These results suggest the need to de-
creases medial load during gait.22 Valgus lected populations has been rare. velop and test, in patients with knee OA,
alignment is associated with an in- Schouten et al 59 found that patient the effect of interventions that reduce the
crease in lateral compartment peak pres- recollection of bow-legs or knock- stresses imposed by a given alignment.
sures49; however, more load is still borne knees in childhood was associated Interventions that reduce load in the
medially until more severe valgus is pre- with a 5-fold increase in risk of OA stressed compartment on an ongoing ba-
sent.51,52 Therefore, we expected to find progression. Others found that pres- sis may have a disease-modifying ef-
that varus alignment had a stronger ef- ence of varus/valgus deformity, not fect. Interventions that may hold prom-
fect on medial progression risk than val- further defined, did not differ between ise (eg, unloading orthoses) have been
gus on lateral progression risk, but the those who progressed and those who examined in short-term studies; their
effects of varus and valgus were similar did not.60 In another study involving long-term tolerability and effect on
in magnitude. The severity of varus was patients who were selected from a symptoms have been minimally evalu-
similar to that of valgus; the lack of dif- hospital practice on the basis of not ated, and their effect on progression and
ference in potency could not be attrib- having undergone surgery, and in long-term functional outcomes is un-
uted to more severe valgus malalign- whom alignment was considered only known.
ment. Certainly, alignment in either at the end of follow-up, 50% of 35 In summary, varus alignment at base-
direction increases compartmental load, varus knees had progressive joint line increased risk of subsequent me-
giving credence to the concept that varus space narrowing.61 dial OA progression and valgus align-
and valgus alignment each may contrib- The proportion of participants whose ment at baseline increased risk of
ute to subsequent progression. Differ- OA progressed in the current study is subsequent lateral OA progression. Base-
ences between the magnitude of the ef- comparable with studies using similar line severity of malalignment was cor-
fects of varus and valgus alignment may recruitment methods.11,62 Also, an av- related with the magnitude of subse-
emerge with further follow-up. erage joint space loss of 0.45 mm was quent joint space loss. Burden of
A relationship between varus or val- detected over 18 months, or 0.30 mm malalignment at baseline was linked to
gus alignment and the natural progres- over 12 months. This rate falls within greater decline in physical function.
sion of primary knee OA has not previ- the range of annual joint space loss in
Author Contributions: Study concept and design:
ously been demonstrated. Beliefs the literature (0.12 to 0.62 mm/y). Sharma, Felson.
regarding this relationship have rested Comparison with population-based Acquisition of data: Sharma, Cahue.
Analysis and interpretation of data: Sharma, Song, Fel-
on biomechanical models and studies studies, which have tended to use con- son, Shamiyeh, Dunlop.
that are cross-sectional or of short du- ventional, extended-knee radiogra- Drafting of the manuscript: Sharma.
194 JAMA, July 11, 2001Vol 286, No. 2 (Reprinted) 2001 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ on 12/20/2014
KNEE ALIGNMENT AND KNEE OSTEOARTHRITIS
Critical revision of the manuscript for important intel- and Allied Conditions: A Textbook of Rheumatology. 40. Lequesne M. Quantitative measurements of joint
lectual content: Sharma, Song, Felson, Cahue, Shami- Baltimore, Md: Williams & Wilkins; 1997:1969-1984. space during progression of osteoarthritis: chondrom-
yeh, Dunlop. 17. Tetsworth K, Paley D. Malalignment and degen- etry. In: Kuettner KE, Goldberg VM, eds. Osteoar-
Statistical expertise: Song, Shamiyeh, Dunlop. erative arthropathy. Orthop Clin North Am. 1994;25: thritic Disorders. Rosemont, Ill: American Academy of
Obtained funding: Sharma. 367-377. Orthopaedic Surgeons; 1995:427-444.
Administrative, technical, or material support: Sharma, 18. Andriacchi TP. Dynamics of knee malalignment. Or- 41. Buckland-Wright JC, Macfarlane DG. Radioana-
Cahue. thop Clin North Am. 1994;25:395-403. tomic assessment of therapeutic outcome in osteoar-
Study supervision: Sharma. 19. Schipplein OD, Andriacchi TP. Interaction be- thritis. In: Kuettner KE, Goldberg VM, eds. Osteoar-
Funding/Support: This study was supported by NIH tween active and passive knee stabilizers during level thritic Disorders. Rosemont, Ill: American Academy of
grant AR-30692 and NIH/National Center for Re- walking. J Orthop Res. 1991;9:113-119. Orthopaedic Surgeons; 1995:51-65.
search Resources grant RR-00048. 20. Moreland JR, Bassett LW, Hanker GJ. Radio- 42. Guralnik JM, Ferrucci L, Simonsick EM, Salive ME,
Acknowledgment: We are very grateful to the indi- graphic analysis of the axial alignment of the lower ex- Wallace RB. Lower-extremity function in persons over
viduals in the MAK study cohort. tremity. J Bone Joint Surg Am. 1987;69:745-749. the age of 70 as a predictor of subsequent disability.
21. Chao EY, Neluheni EV, Hsu RW, Paley D. Biome- N Engl J Med. 1995;332:556-561.
chanics of malalignment. Orthop Clin North Am. 1994; 43. Seeman TE, Charpentier PA, Berkman LF, et al. Pre-
REFERENCES 25:379-386. dicting changes in physical performance in a high-
22. Hsu RW, Himeno S, Conventry MB, Chao EY. Nor- functioning elderly cohort: MacArthur studies of suc-
1. Lawrence RC, Helmick CG, Arnett FC, et al. Esti- mal axial alignment of the lower extremity and load- cessful aging. J Gerontol. 1994;49:M97-M108.
mates of the prevalence of arthritis and selected mus- bearing distribution at the knee. Clin Orthop. 1990; 44. Pai YC, Chang HJ, Chang RW, Sinacore JM, Lewis
culoskeletal disorders in the United States. Arthritis 255:215-227. JL. Alteration in multijoint dynamics in patients with bi-
Rheum. 1998;41:778-799. 23. Cooke TD, Li J, Scudamore RA. Radiographic as- lateral knee osteoarthritis. Arthritis Rheum. 1994;37:
2. Guccione AA, Felson DT, Anderson JJ, et al. The ef- sessment of bony contributions to knee deformity. Or- 1297-1304.
fects of specific medical conditions on the functional thop Clin North Am. 1994;25:387-393. 45. Fleckenstein SJ, Kirby RL, MacLeod DA. Effect of
limitations of elders in the Framingham Study. Am J Pub- 24. Hilding MB, Lanshammar H, Ryd L. A relationship limited knee-flexion range on peak hip moments of force
lic Health. 1994;84:351-358. between dynamic and static assessments of knee joint while transferring from sitting to standing. J Biomech.
3. Ettinger WH, Davis MA, Neuhaus JM, Mallon KP.
load. Acta Orthop Scand. 1995;66:317-320. 1988;21:915-918.
Long-term physical functioning in persons with knee
25. Goldberg VM, Kettelkamp DB, Coyler RA. Osteo- 46. Pai YC, Rogers MW. Speed variation and result-
osteoarthritis from NHANES I: effects of comorbid medi-
arthritis of the knee. In: Moskowitz RW, Howell DS, ant joint torques during sit-to-stand. Arch Phys Med
cal conditions. J Clin Epidemiol. 1994;47:809-815.
Goldberg VM, Mankin HJ, eds. Osteoarthritis: Diag- Rehabil. 1991;72:881-885.
4. National Institute of Arthritis and Musculoskeletal
nosis and Medical/Surgical Management. Philadel- 47. Schultz AB, Alexander NB, Ashton-Miller JA. Bio-
and Skin Diseases. The Osteoarthritis Initiative. Avail-
phia, Pa: WB Saunders Co; 1992:599-620. mechanics analysis of rising from a chair. J Biomech.
able at: http://www.nih.gov/niams/news/oisg/index
26. Cushnaghan J, Cooper C, Dieppe P, et al. Clinical 1992;25:1383-1391.
.htm. Accessed February 6, 2001.
assessment of osteoarthritis of the knee. Ann Rheum 48. McKellop HA, Llinas A, Sarmiento A. Effects of tibial
5. Dieppe P. Theories on the pathogenesis of OA. Pre-
Dis. 1990;49:768-770. malalignment on the knee and ankle. Orthop Clin North
sented at: Stepping Away From OA: A Scientific Con-
27. Noyes FR, Cummings JF, Grood ES, et al. The di- Am. 1994;25:415-423.
ference on the Prevention of Onset, Progression, and
Disability of Osteoarthritis; July 23-24, 1999; Bethesda, agnosis of knee motion limits, subluxations, and liga- 49. Bruns J, Volkmer, M, Luessenhop S. Pressure dis-
Md. Summary available at: http://www.nih.gov/niams ment injury. Am J Sports Med. 1991;19:163-171. tribution at the knee joint. Arch Orthop Trauma Surg.
/reports/oa/oaconfsumsc.htm. Accessed February 6, 28. Sharma L, Lou C, Felson DT, et al. Laxity in healthy 1993;133:12-19.
2001. and osteoarthritic knees. Arthritis Rheum. 1999;42: 50. Morrison JB. The mechanics of the knee joint in re-
6. Dieppe P, Altman RD, Buckwalter JA, et al. Stan- 861-870. lation to normal walking. J Biomech. 1970;3:51-61.
dardization of methods used to assess the progression 29. Sharma L, Hayes KW, Felson DT, et al. Does lax- 51. Johnson F, Leitl S, Waugh W. The distribution of
of osteoarthritis of the hip or knee joints. In: Kuettner ity alter the relationship between strength and physi- load across the knee. J Bone Joint Surg Br. 1980;62:
KE, Goldberg VM, eds. Osteoarthritic Disorders. Rose- cal function in knee osteoarthritis? Arthritis Rheum. 346-349.
mont, Ill: American Academy of Orthopaedic Sur- 1999;42:25-32. 52. Harrington IJ. Static and dynamic loading pat-
geons; 1995:481-496. 30. Markolf KL, Graff-Radford A, Amstutz HC. In vivo terns in knee joints with deformities. J Bone Joint Surg
7. Mazzuca SA, Brandt KD. Plain radiography as an out- knee stability. J Bone Joint Surg Am. 1978;60:664- Am. 1983;65:247-259.
come measure in clinical trials involving patients with 674. 53. Ritter MA, Faris PM, Keating EM, Meding JB. Post-
knee osteoarthritis. Rheum Dis Clin North Am. 1999; 31. Markolf KL, Bargar WL, Shoemaker SC, Amstutz operative alignment of total knee replacement. Clin Or-
25:467-480. HC. The role of joint load in knee stability. J Bone Joint thop. 1994;299:153-156.
8. Altman RD, Hochberg M, Murphy WA, Wolfe F, Surg Am. 1981;63:570-585. 54. Yasuda K, Majima T, Tsuchida T, Kaneda K. A ten-
Lequesne M. Atlas of individual radiographic features 32. Brage ME, Draganich LF, Pottenger LA, Curran JJ. to 15-year follow-up observation of high tibial oste-
in osteoarthritis. Osteoarthritis Cartilage. 1995;3:3-70. Knee laxity in symptomatic osteoarthritis. Clin Or- otomy in medial compartment osteoarthritis. Clin Or-
9. Task Force of the Osteoarthritis Research Society. De- thop. 1994;304:184-189. thop. 1992;282:186-195.
sign and conduct of clinical trials in patients with osteo- 33. Pottenger LA, Phillips FM, Draganich LF. The ef- 55. Allen PR, Denham RA, Swan AV. Late degenera-
arthritis. Osteoarthritis Cartilage. 1996;4:217-244. fect of marginal osteophytes on reduction of varus- tive changes after meniscectomy. J Bone Joint Surg Br.
10. Mazzuca SA, Brandt KD, Katz BP. Is conventional valgus instability in osteoarthritic knees. Arthritis Rheum. 1984;66:666-671.
radiography suitable for evaluation of a disease- 1990;33:853-858. 56. Neyret P, Donell ST, Dejour H. Results of partial
modifying drug in patients with knee osteoarthritis? Os- 34. Wada M, Imura S, Baba H, Shimada S. Knee lax- meniscectomy related to the state of the anterior cru-
teoarthritis Cartilage. 1997;5:217-226. ity in patients with osteoarthritis and rheumatoid ar- ciate ligament. J Bone Joint Surg Br. 1993;75:36-40.
11. Ravaud P, Giraudeau B, Auleley GR, et al. Radio- thritis. Br J Rheumatol. 1996;35:560-563. 57. Boe S, Hansen H. Arthroscopic partial meniscec-
graphic assessment of knee OA: reproducibility and sen- 35. Buckland-Wright CB. Protocols for precise radio- tomy in patients aged over 50. J Bone Joint Surg Br.
sitivity to change. J Rheumatol. 1996;23:1756-1764. anatomical positioning of the tibiofemoral and patel- 1986;68:707.
12. Buckland-Wright JC, Macfarlane DG, Lynch JA, Jas- lofemoral compartments of the knee. Osteoarthritis Car- 58. Ogilvie-Harris DJ, Fitsialos DP. Arthroscopic man-
ani MK, Bradshaw CR. Joint space width measures car- tilage. 1995;3(suppl A):71-80. agement of the degenerative knee. Arthroscopy. 1991;
tilage thickness in osteoarthritis of the knee. Ann Rheum 36. Messieh SS, Fowler PJ, Munro T. Anteroposterior 7:151-157.
Dis. 1995;54:263-268. radiographs of the osteoarthritic knee. J Bone Joint Surg 59. Schouten JS, van den Ouweland FA, Valkenburg
13. Buckland-Wright JC. Quantitative radiography of Br. 1990;72:639-640. HA. A 12-year follow up study in the general popula-
osteoarthritis. Ann Rheum Dis. 1994;53:268-275. 37. Buckland-Wright JC, Macfarlane DG, Williams SA, tion on prognostic factors of cartilage loss in osteoar-
14. Dieppe P. The classification and diagnosis of os- Ward RJ. Accuracy and precision of joint space width thritis of the knee. Ann Rheum Dis. 1992;51:932-937.
teoarthritis. In: Kuettner KE, Goldberg VM, eds. Os- measurements in standard and macroradiographs of os- 60. Dougados M, Gueguen A, Nguyen M, et al. Lon-
teoarthritic Disorders. Rosemont, Ill: American Acad- teoarthritic knees. Ann Rheum Dis. 1995;54:872-880. gitudinal radiologic evaluation of osteoarthritis of the
emy of Orthopaedic Surgeons; 1995:7. 38. Buckland-Wright JC, Wolfe F, Ward RJ, Flowers knee. J Rheumatol. 1992;19:378-384.
15. Kuettner KE, Goldberg VM. Introduction. In: N, Hayne C. Substantial superiority of semiflexed (MTP) 61. Miller R, Kettelkamp DB, Laubenthal KN, et al.
Kuettner KE, Goldberg VM, eds. Osteoarthritic Disor- views in knee osteoarthritis. J Rheumatol. 1999;26: Quantitative correlations in degenerative arthritis of the
ders. Rosemont, Ill: American Academy of Orthopae- 2664-2674. knee. J Bone Joint Surg Am. 1973;55:956-962.
dic Surgeons; 1995:xxi-xxv. 39. Altman RD, Fries JF, Bloch DA, Carstens J, et al. 62. Ledingham J, Regan M, Jones A, Doherty M. Fac-
16. Pelletier JP, Martel-Pelletier J, Howell DS. Etiopatho- Radiographic assessment of progression in osteoarthri- tors affecting radiographic progression of knee osteo-
genesis of osteoarthritis. In: Koopman WJ, ed. Arthritis tis. Arthritis Rheum. 1987;30:1214-1225. arthritis. Ann Rheum Dis. 1995;54:53-58.
2001 American Medical Association. All rights reserved. (Reprinted) JAMA, July 11, 2001Vol 286, No. 2 195
Downloaded From: http://jama.jamanetwork.com/ on 12/20/2014
Anda mungkin juga menyukai
- Proximal Humerus Fractures: Evaluation and ManagementDari EverandProximal Humerus Fractures: Evaluation and ManagementLynn A. CrosbyBelum ada peringkat
- Joelho Valgoe VaroDokumen13 halamanJoelho Valgoe VaroTiago BrandalizeBelum ada peringkat
- Jurnal 1Dokumen8 halamanJurnal 1Andre PratamaBelum ada peringkat
- Osteoarthritis: in The ClinicDokumen16 halamanOsteoarthritis: in The ClinicKurosaki IchigoBelum ada peringkat
- 2013 Article 9164Dokumen6 halaman2013 Article 9164iosif iliaBelum ada peringkat
- Relationship Between Knee and Ankle Degeneration in A Population of Organ DonorsDokumen11 halamanRelationship Between Knee and Ankle Degeneration in A Population of Organ DonorsNguyễn HùngBelum ada peringkat
- Minis CoDokumen6 halamanMinis CoNaara LibBelum ada peringkat
- Researc OrofasdialDokumen18 halamanResearc OrofasdialREANANDA MUBARAK SUGIARTOBelum ada peringkat
- Review Femoroacetabular ImpingementDokumen11 halamanReview Femoroacetabular ImpingementwladjaBelum ada peringkat
- Nisha - OA 3Dokumen6 halamanNisha - OA 3JeveraBelum ada peringkat
- Physiotherapy Management of Hip OsteoarthritisDokumen14 halamanPhysiotherapy Management of Hip Osteoarthritisaraaela 25Belum ada peringkat
- The Prevalence of in The Knee Osteoarthritis ElderlyDokumen5 halamanThe Prevalence of in The Knee Osteoarthritis Elderlyqurrat ul ann haiderBelum ada peringkat
- Physiotherapy Management of Hip Osteoarthritis: Kim BennellDokumen13 halamanPhysiotherapy Management of Hip Osteoarthritis: Kim BennellAndrei R LupuBelum ada peringkat
- MRI, Força de ExtensoresDokumen16 halamanMRI, Força de ExtensoresRosaneLacerdaBelum ada peringkat
- Oa Glyn-Jones2015Dokumen12 halamanOa Glyn-Jones2015Azmia TabahBelum ada peringkat
- The Association of Spinal Osteoarthritis With Lumbar LordosisDokumen7 halamanThe Association of Spinal Osteoarthritis With Lumbar LordosisPatricio Fernando Garay GallardoBelum ada peringkat
- NIH Public Access: Author ManuscriptDokumen15 halamanNIH Public Access: Author Manuscriptfidatahir93Belum ada peringkat
- Epidemiologyofosteoarthritis: Tuhina Neogi,, Yuqing ZhangDokumen19 halamanEpidemiologyofosteoarthritis: Tuhina Neogi,, Yuqing ZhangIkmal ShahromBelum ada peringkat
- Vertebral Fractures: Clinical PracticeDokumen9 halamanVertebral Fractures: Clinical PracticeIndraYudhiBelum ada peringkat
- Brazilian Journal of Physical TherapyDokumen8 halamanBrazilian Journal of Physical TherapyLina M GarciaBelum ada peringkat
- Effects of Exercise and Physical Activity On Knee OsteoarthritisDokumen9 halamanEffects of Exercise and Physical Activity On Knee OsteoarthritisJoseph LimBelum ada peringkat
- JBMR2014 HKFXDokumen8 halamanJBMR2014 HKFXIfon poppy yosefBelum ada peringkat
- The Female Acl: Why Is It More Prone To Injury?: SciencedirectDokumen4 halamanThe Female Acl: Why Is It More Prone To Injury?: SciencedirectmasonBelum ada peringkat
- InTech-Knee Pain in Adults Adolescents Diagnosis and TreatmentDokumen32 halamanInTech-Knee Pain in Adults Adolescents Diagnosis and Treatmentevil freakBelum ada peringkat
- Predicting Knee OADokumen12 halamanPredicting Knee OAMoustafa AnwarBelum ada peringkat
- Obesity & Osteoarthritis PDFDokumen9 halamanObesity & Osteoarthritis PDFTaufik Ramadhan BiyaBelum ada peringkat
- Preventive Osteopathic Manipulative Treatment and Stress Fracture Incidence Among Collegiate Cross-Country AthletesDokumen9 halamanPreventive Osteopathic Manipulative Treatment and Stress Fracture Incidence Among Collegiate Cross-Country AthletesAlejandro OrduzBelum ada peringkat
- Ymj 59 317Dokumen8 halamanYmj 59 317ItaloLozanoPalominoBelum ada peringkat
- Tennis Elbow JOSPT ArticleDokumen11 halamanTennis Elbow JOSPT ArticleHasan RahmanBelum ada peringkat
- Research Report: Plantar Fasciitis: Are Pain and Fascial Thickness Associated With Arch Shape and Loading?Dokumen7 halamanResearch Report: Plantar Fasciitis: Are Pain and Fascial Thickness Associated With Arch Shape and Loading?fabiosm17Belum ada peringkat
- Osteoarthritis: Epidemiology, Risk Factors, and PathophysiologyDokumen10 halamanOsteoarthritis: Epidemiology, Risk Factors, and PathophysiologyMaryama AflahaBelum ada peringkat
- HHS Public Access: Diagnosis and Treatment of Hip and Knee Osteoarthritis: A ReviewDokumen25 halamanHHS Public Access: Diagnosis and Treatment of Hip and Knee Osteoarthritis: A ReviewJose PerezBelum ada peringkat
- Fijcmr 650 May 31 2Dokumen3 halamanFijcmr 650 May 31 2khusnulBelum ada peringkat
- Knee Osteoarthritis: An Overview of Recent Interventions: Bijeet Bardoloi, Chungki Bhutia, Dinesh Bhatia, Sudip PaulDokumen18 halamanKnee Osteoarthritis: An Overview of Recent Interventions: Bijeet Bardoloi, Chungki Bhutia, Dinesh Bhatia, Sudip PaultiaanastaBelum ada peringkat
- Balneo 305Dokumen6 halamanBalneo 305Nicoleta TudorachiBelum ada peringkat
- Dynapenia and Aging An UpdateDokumen13 halamanDynapenia and Aging An UpdatehattorijuniorBelum ada peringkat
- Rothenfluh ASDDokumen8 halamanRothenfluh ASDMichael GBelum ada peringkat
- Body Mass Index and Susceptibility To Knee Osteoarthritis: A Systematic Review and Meta-AnalysisDokumen7 halamanBody Mass Index and Susceptibility To Knee Osteoarthritis: A Systematic Review and Meta-AnalysisAmalia RosaBelum ada peringkat
- Baseline Articular Contact Stress Tingkats Predict Incident Symptomatic Knee Osteoarthritis Development in The MOST CohortDokumen7 halamanBaseline Articular Contact Stress Tingkats Predict Incident Symptomatic Knee Osteoarthritis Development in The MOST CohortSTAF OSCEBelum ada peringkat
- 2Dokumen6 halaman2Rashmi GodeshwerBelum ada peringkat
- Osteoarthritis in Women: Effects of Estrogen, Obesity and Physical ActivityDokumen15 halamanOsteoarthritis in Women: Effects of Estrogen, Obesity and Physical ActivitypakemainmainBelum ada peringkat
- 1-Disease MechanismsDokumen5 halaman1-Disease MechanismsMarian Dane PunzalanBelum ada peringkat
- Correlation Between Metabolic Syndrome and Knee Osteoarthritis: Data From The Korean National Health and Nutrition Examination Survey (Knhanes)Dokumen8 halamanCorrelation Between Metabolic Syndrome and Knee Osteoarthritis: Data From The Korean National Health and Nutrition Examination Survey (Knhanes)Agatha GeraldyneBelum ada peringkat
- HHS Public Access: Imaging of Osteoarthritis in Geriatric PatientsDokumen16 halamanHHS Public Access: Imaging of Osteoarthritis in Geriatric PatientsNaufal K. YurnadiBelum ada peringkat
- Vertebral Fracture Risk (VFR) Score For Fracture Prediction in Postmenopausal WomenDokumen11 halamanVertebral Fracture Risk (VFR) Score For Fracture Prediction in Postmenopausal WomenAdhiatma DotBelum ada peringkat
- Morel Lavellee Lession DiagnosisDokumen10 halamanMorel Lavellee Lession DiagnosisGuillermo Chacon AcevedoBelum ada peringkat
- Palmieri Smith2009Dokumen7 halamanPalmieri Smith2009R HariBelum ada peringkat
- 1756-185X.13082) Huang, Lanfeng Guo, Bin Xu, Feixiang Zhao, Jinsong - Effects of Quadriceps Functional Exercise With IsDokumen8 halaman1756-185X.13082) Huang, Lanfeng Guo, Bin Xu, Feixiang Zhao, Jinsong - Effects of Quadriceps Functional Exercise With IsTrisna ArinataBelum ada peringkat
- Diagnosis Management Pelvic FracturesDokumen11 halamanDiagnosis Management Pelvic FracturesIstari PutriBelum ada peringkat
- Theepidemiology Ofdistalradius Fractures: Kate W. Nellans,, Evan Kowalski,, Kevin C. ChungDokumen13 halamanTheepidemiology Ofdistalradius Fractures: Kate W. Nellans,, Evan Kowalski,, Kevin C. Chungreza rivaldy azaBelum ada peringkat
- Seyed Esmaeel Shafiei2016Dokumen4 halamanSeyed Esmaeel Shafiei2016xavi5_5Belum ada peringkat
- Musculoskeletal Disorders Associated With Obesity: A Biomechanical PerspectiveDokumen12 halamanMusculoskeletal Disorders Associated With Obesity: A Biomechanical Perspectiveprofessor do valeBelum ada peringkat
- Medicine The American Journal of SportsDokumen7 halamanMedicine The American Journal of SportsJohann Sebastian CruzBelum ada peringkat
- Prevalence of Flatfoot and Its Correlation With Age, Gender and BMI Among Undergraduates at The Faculty of Allied Health Sciences, General Sir John Kotelawela Defence UniversityDokumen5 halamanPrevalence of Flatfoot and Its Correlation With Age, Gender and BMI Among Undergraduates at The Faculty of Allied Health Sciences, General Sir John Kotelawela Defence UniversitySabrina JonesBelum ada peringkat
- Bir RellDokumen12 halamanBir RellGaudeamus IgiturBelum ada peringkat
- Abductor Strenght in Relation With Sports InjuriesDokumen7 halamanAbductor Strenght in Relation With Sports InjuriespetrBelum ada peringkat
- A Naturally Aging Knee or Development of Early KN - 2018 - Osteoarthritis and CDokumen6 halamanA Naturally Aging Knee or Development of Early KN - 2018 - Osteoarthritis and CVanessa MartinsBelum ada peringkat
- Theburdenofosteoarthritis Inolderadults: Gillian A. Hawker,, Lauren K. KingDokumen12 halamanTheburdenofosteoarthritis Inolderadults: Gillian A. Hawker,, Lauren K. KingabdulfatahalhemeryBelum ada peringkat
- An Emerging Pattern of Subtrochanteric Stress FracturesDokumen6 halamanAn Emerging Pattern of Subtrochanteric Stress FracturesAlejandro OrduzBelum ada peringkat
- Hewett2006 PDFDokumen13 halamanHewett2006 PDFhectorBelum ada peringkat
- ReseachDokumen3 halamanReseachWen TingBelum ada peringkat
- Molar Uprighting Simple TechniqueDokumen4 halamanMolar Uprighting Simple TechniqueMariem DelmasBelum ada peringkat
- p2418 Chapter2 PDFDokumen10 halamanp2418 Chapter2 PDFLiz TaylorBelum ada peringkat
- PEMF To Support Heavy Metal Detoxification (Truly Heal)Dokumen50 halamanPEMF To Support Heavy Metal Detoxification (Truly Heal)Vas Ra100% (5)
- EAD Irst: The Ob/Gyn Clerk's CompanionDokumen32 halamanEAD Irst: The Ob/Gyn Clerk's CompanionEmerald Holly TagoBelum ada peringkat
- Roger Perron - Idea/RepresentationDokumen5 halamanRoger Perron - Idea/RepresentationAustin E BeckBelum ada peringkat
- Blood Transfusion NotesDokumen1 halamanBlood Transfusion NotesShreyas WalvekarBelum ada peringkat
- Home Blood Pressure DiaryDokumen2 halamanHome Blood Pressure DiaryCherieBelum ada peringkat
- Aggressivity, Narcissism, and Self-Destructiveness in The Psychotherapeutic Relationship - Otto KernbergDokumen27 halamanAggressivity, Narcissism, and Self-Destructiveness in The Psychotherapeutic Relationship - Otto Kernbergvgimbe100% (1)
- Evidence-Based Nursing: The 5 Steps of EBNDokumen13 halamanEvidence-Based Nursing: The 5 Steps of EBNRanjith RgtBelum ada peringkat
- Chapter 6 NeuroemergencyDokumen21 halamanChapter 6 NeuroemergencyEdo FebrianBelum ada peringkat
- Drug Study - DiazepamDokumen2 halamanDrug Study - DiazepamCerie Anne Olay40% (5)
- Thesis PoDokumen5 halamanThesis PoJane SandovalBelum ada peringkat
- Green Back TanjyDokumen20 halamanGreen Back TanjymymicroBelum ada peringkat
- Solving Math Word Problems: Steps Tips For Success ExampleDokumen3 halamanSolving Math Word Problems: Steps Tips For Success ExampleDhiman NathBelum ada peringkat
- PeriopConceptsDokumen43 halamanPeriopConceptsKysha Huang100% (1)
- Recurrent Pregnancy LossDokumen40 halamanRecurrent Pregnancy LossJagannath MaaleBelum ada peringkat
- Blood DetailsDokumen13 halamanBlood DetailsKishore Babu PvrBelum ada peringkat
- FenofibrateDokumen7 halamanFenofibrateVikas Karande100% (1)
- Health Claim Form Part BDokumen3 halamanHealth Claim Form Part BShubham PandeyBelum ada peringkat
- Educational Training Manual: Certification Board, IncDokumen58 halamanEducational Training Manual: Certification Board, IncAlexander MaukinBelum ada peringkat
- Manual For Charge NursesDokumen99 halamanManual For Charge NursesHazelina Villamor100% (1)
- Bladder CancerDokumen35 halamanBladder CancerHealth Education Library for PeopleBelum ada peringkat
- Komplikasi Trauma Muskuloskeletal-YudisDokumen12 halamanKomplikasi Trauma Muskuloskeletal-YudisFrans 'cazper' SihombingBelum ada peringkat
- Health Problem Family Nursing Problem Goal of Care Objectives of Care Intervention PlanDokumen2 halamanHealth Problem Family Nursing Problem Goal of Care Objectives of Care Intervention PlanCarol MalcoBelum ada peringkat
- Contract Research Organizations An Industry AnalysisDokumen25 halamanContract Research Organizations An Industry AnalysisJürgen FleischerBelum ada peringkat
- Modified Early Obstetric Warning Score MEOWS MID33 AO13 v4.2Dokumen9 halamanModified Early Obstetric Warning Score MEOWS MID33 AO13 v4.2indirinoor5Belum ada peringkat
- Nxlex 6Dokumen50 halamanNxlex 6Arvin CamposBelum ada peringkat
- Gynae & Obstetrics Monitoring - IoMT - PhilipsDokumen10 halamanGynae & Obstetrics Monitoring - IoMT - PhilipsAnuj MehrotraBelum ada peringkat
- Multiapproach Orthopaedic ManagementDokumen68 halamanMultiapproach Orthopaedic ManagementDz PutraBelum ada peringkat